Cardiovascular–Endocrine–Metabolic Medicine: Proposing a New Clinical Sub-Specialty Amid the Cardiometabolic Pandemic
Abstract
1. Introduction
- ■
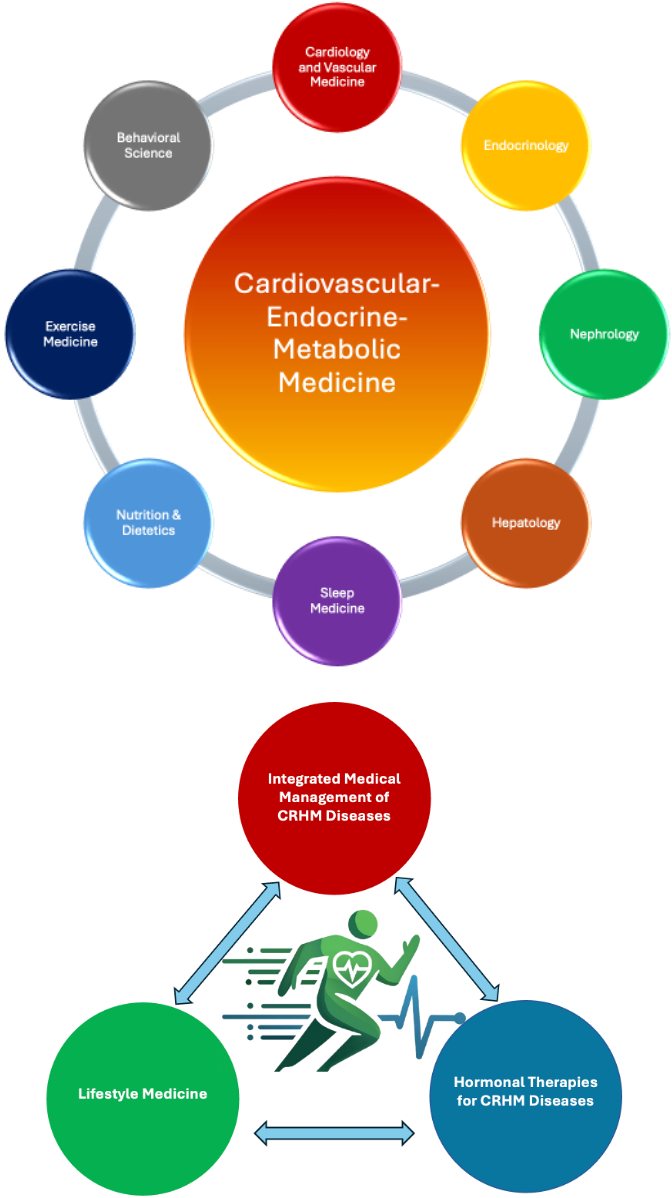
- Lifestyle Medicine: Incorporating evidence-based strategies, this pillar focuses on the integration of nutritional, exercise, and behavioral interventions to prevent and manage CRHM diseases. Inspired by principles observed in longevity-focused so-called Blue Zones and the pillars of lifestyle medicine described in our previous manuscript, this approach seeks to modify key lifestyle factors such as diet, physical activity, sleep, stress management, and smoking–alcohol cessation to enhance both health span and life span [58].
- ■
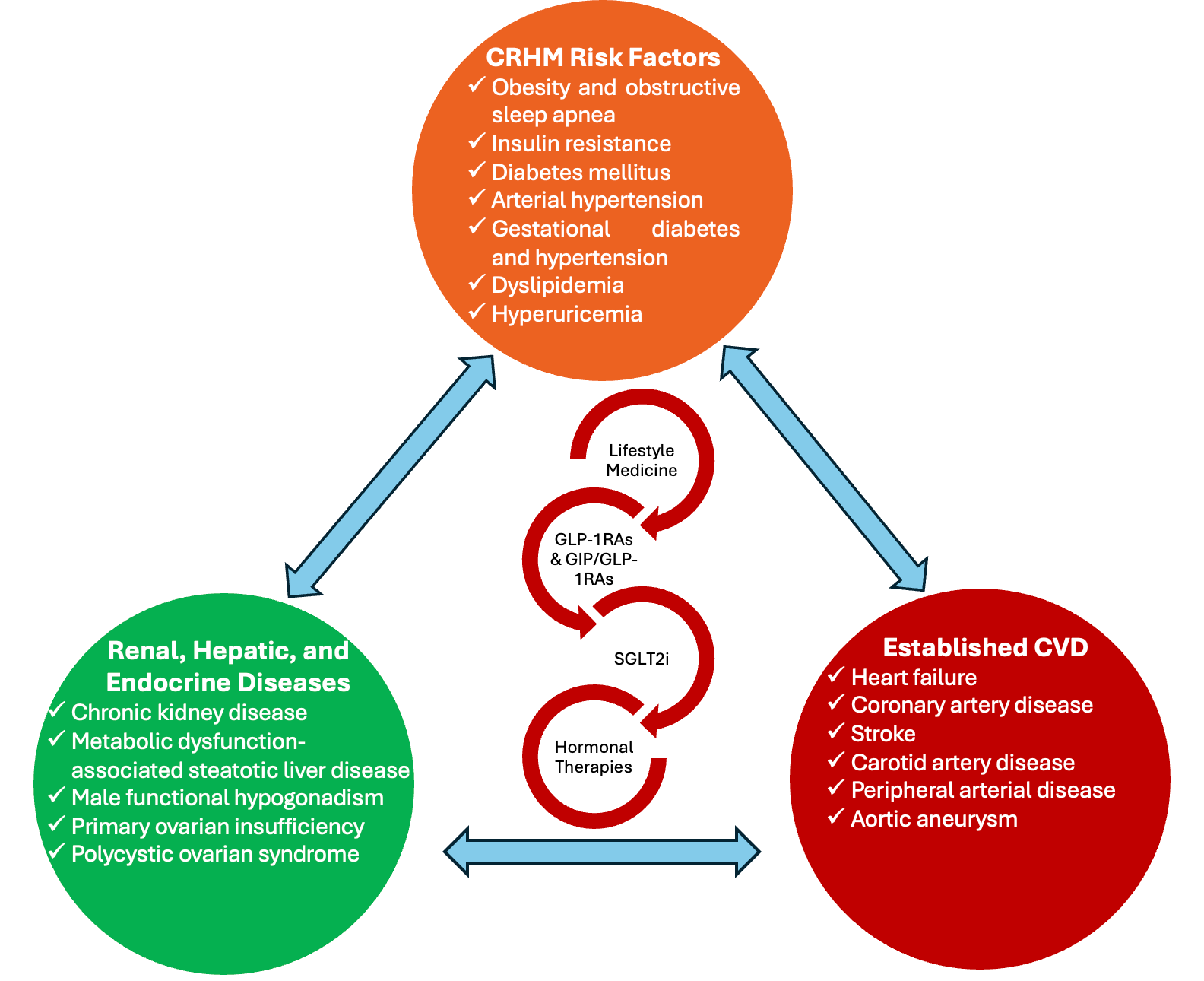
- Integrated Medical Management of CRHM Diseases: This pillar focuses on the optimization of the medical management of the cardiometabolic spectrum, including obesity, insulin resistance, T2DM, arterial hypertension, dyslipidemia, cardiometabolic HFpEF, early-stage CKD, MASLD, OSA, FHH, and polycystic ovarian syndrome (PCOS). Recognizing the shared pathophysiology and overlapping therapeutic strategies, this framework promotes an integrated approach to diagnosis, prevention, and treatment.
- ■
- Hormonal Therapies for CRHM: This research involves hormonal therapies for HF, integration of TTh for men with FHH and CRHM diseases, and optimized care for women with premature ovarian insufficiency (POI).
2. The Cardiometabolic Pandemic
3. First Pillar: Lifestyle Medicine
3.1. Nutrition
3.2. Physical Activity and Exercise
3.3. Weight Management
3.4. Smoking, Alcohol and Caffeine
3.5. Integrating Lifestyle Medicine into Cardiovascular–Endocrine–Metabolic Medicine
4. Second Pillar: Integrated Medical Management of Cardiovascular–Renal–Hepatic–Metabolic Diseases
4.1. Obesity, T2DM, Arterial Hypertension, and Dyslipidemia
4.2. SGLT2i and GLP-1RAs: A Wide Repertoire of Indications
5. Third Pillar: Hormonal Therapies for CRHM Diseases
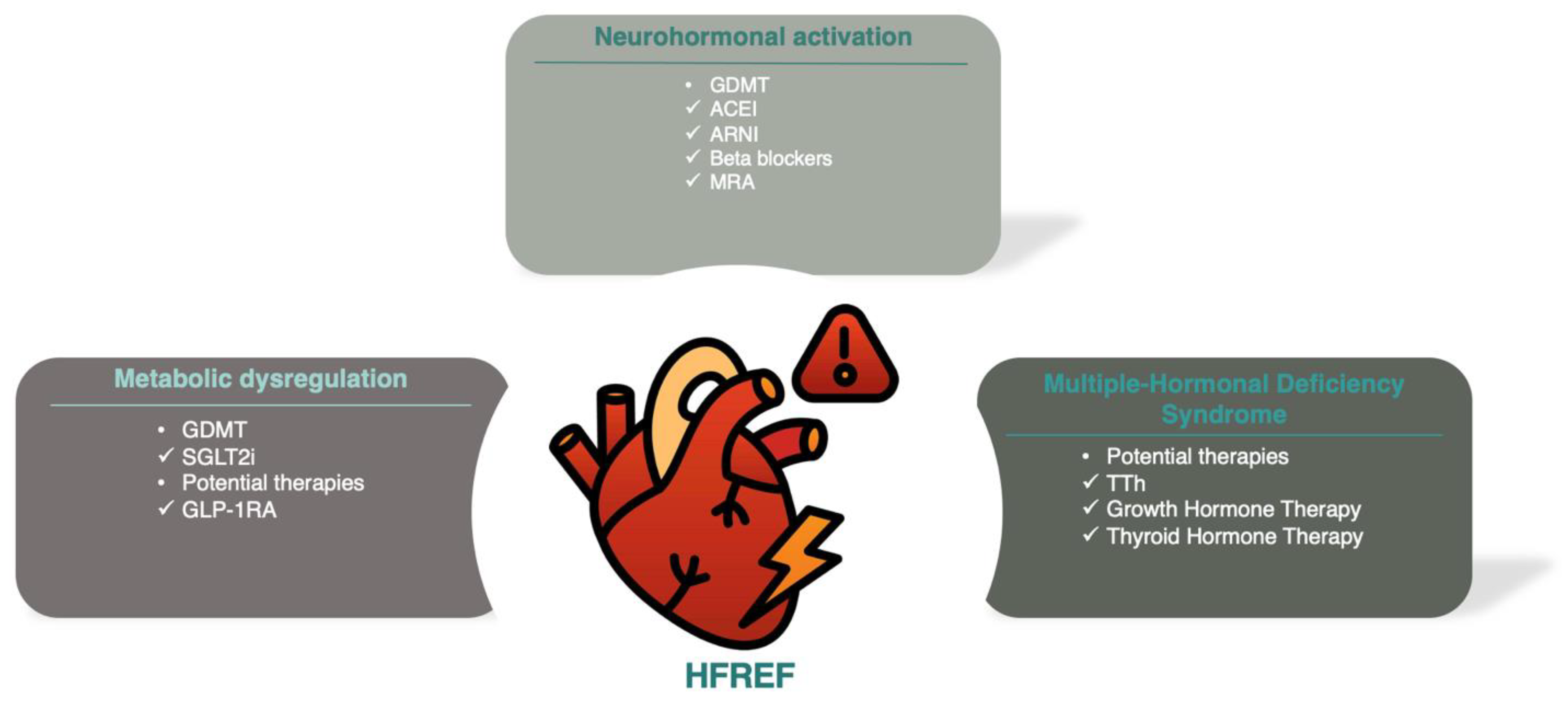
5.1. HF and Multiple Hormonal Deficiency Syndrome
5.2. Male FHH
5.3. Estrogen Deficiency: Premature Ovarian Insufficiency
6. Proposed Training Curriculum in Cardiovascular–Endocrine–Metabolic Medicine
6.1. Cardiology and Vascular Medicine
- ■
- Core Competencies
- ○
- Cardiovascular risk stratification.
- ○
- Etiology, diagnosis, prevention, and management of arterial hypertension, including resistant hypertension, gestational hypertension, and pre-eclampsia.
- ○
- Etiology, diagnosis, prevention, and management of dyslipidemia, including genetic lipid disorders and LDL apheresis.
- ○
- Etiology, pathophysiology, prevention, and diagnosis of ASCVD.
- ○
- Etiology, pathophysiology, diagnosis, prevention, and management of cardiometabolic HFpEF.
- ○
- The basics of interpreting ECG, transthoracic echocardiography, arterial and venous color Doppler studies, coronary computed tomography, functional ischemic tests, and coronary angiography.
- ○
- Emerging hormonal therapies in HF.
- ○
- Research and leadership.
- ■
- Exclusions: Anything outside the above, including but not limited to HFrEF, cardiac amyloidosis, cardiac transplantation, the management of ASCVD, interventional cardiology, arrhythmias, electrophysiology, and cardio-oncology, remain outside our scope.
- ■
- Clinical Training
- ○
- Preventive Cardiology of outpatient clinics.
- ○
- HF outpatient clinics.
- ○
- Echocardiography labs.
- ○
- General cardiology wards.
6.2. Endocrinology
- ■
- Core Competencies
- ○
- Etiology, pathophysiology, diagnosis, prevention, and medical management of obesity, including indications for bariatric surgery.
- ○
- Etiology, pathophysiology, diagnosis, prevention, and management of diabetes mellitus (including oral agents, GLP-1RAs, GIP/GLP-1RAs, insulin therapy, acute and chronic complications, and gestational diabetes).
- ○
- Investigation and medical management of endocrine causes behind secondary arterial hypertension.
- ○
- Key considerations for the management of thyroid disorders in patients with CVD.
- ○
- Etiology, diagnosis, and management of male FHH, POI, and PCOS.
- ○
- Research and leadership.
- ■
- Exclusions: Anything outside the above, including but not limited to complex endocrine disorders (e.g., pituitary, thyroid, parathyroid, adrenal glands), disorders of bone metabolism, and hereditary metabolic disorders, remain outside our scope.
- ■
- Clinical Training
- ○
- Obesity outpatient clinics, including rotations in follow-up post-bariatric surgery.
- ○
- Diabetes mellitus outpatient clinics (type 1 diabetes, type 2 diabetes, and diabetes in pregnancy).
- ○
- Male and female reproduction outpatient clinics.
6.3. Nephrology
- ■
- Core Competencies
- ○
- Etiology, diagnosis, prevention, and medical management of CKD stages I to III.
- ○
- Investigation and medical management of renal and renovascular secondary hypertension.
- ■
- Exclusions: Anything outside the above, including but not limited to stage IV or V CKD, renal replacement therapy, renal transplantation, or glomerular diseases, remains outside our scope.
- ■
- Clinical Training
- ○
- CKD outpatient clinics.
6.4. Hepatology
- ■
- Core Competencies
- ○
- Etiology, pathophysiology, diagnosis, prevention, and management of MASLD.
- ■
- Exclusions: Topics, including but not limited to autoimmune hepatitis, viral hepatitis, liver cirrhosis, and renal transplantation, remain outside our scope.
- ■
- Clinical Training
- ○
- Hepatology outpatient clinics.
6.5. Sleep Medicine
- ■
- Core Competencies
- ○
- Etiology, pathophysiology, prevention diagnosis, and basics of the management of OSA in the context of obesity.
- ■
- Exclusions: Competencies beyond those listed above, including advanced management of OSA, remain out of our scope.
- ■
- Clinical Training
- ○
- Polysomnography laboratory.
6.6. Lifestyle Medicine
- ■
- Core Competencies
- ○
- Clinical nutrition;
- ○
- Exercise prescription;
- ○
- Smoking–alcohol cessation;
- ○
- Behavioral counseling, including motivational interviewing.
- ■
- Clinical Training
- ○
- Nutrition–dietetic outpatient clinics, including in-patient consultations.
- ○
- Familiarity with quantitative exercise physiology laboratory assessments, e.g., measurement of VO2 max.
- ○
- Smoking–alcohol cessation and behavioral counseling clinics.
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACC | American College of Cardiology |
| ADA | American Diabetes Association |
| AHI | Apnea–hypopnea index |
| AHA | American Heart Association |
| ASCVD | Atherosclerotic cardiovascular disease |
| ASMR | Age-standardized mortality rate |
| BMD | Bone mineral density |
| BMI | Body mass index |
| BP | Blood pressure |
| CAD | Coronary artery disease |
| CVD | Cardiovascular disease |
| CKD | Chronic kidney disease |
| CRHM | Cardiovascular–Renal–Hepatic–Metabolic syndrome |
| DASH | Dietary approaches to stop hypertension |
| DPP4i | Dipeptidyl peptidase-4 inhibitors |
| EAPC | European Association of Preventive Cardiology |
| EASD | European Association for the Study of Diabetes |
| EASO | European Association for the Study of Obesity |
| ECG | Electrocardiogram |
| ESC | European Society of Cardiology |
| FHH | Functional hypogonadotropic hypogonadism |
| GDMT | Guideline-directed medical therapy |
| GIP | Glucose-dependent insulinotropic polypeptide |
| GLP-1RA | Glucagon-like peptide-1 receptor agonist |
| HbA1c | Glycated hemoglobin |
| HF | Heart failure |
| HFpEF | Heart failure with preserved ejection fraction |
| HFrEF | Heart failure with reduced ejection fraction |
| HIF-1α | Hypoxia-inducible factor 1-alpha |
| HR | Hazard ratio |
| IGF-I | Insulin-like growth factor-I |
| LDL-C | Low-density lipoprotein cholesterol |
| MASLD | Metabolic dysfunction-associated steatotic liver disease |
| MHT | Menopausal hormone therapy |
| MHDS | Multiple hormonal and metabolic deficiency syndrome |
| NAFLD | Non-alcoholic fatty liver disease |
| NASH | Non-alcoholic steatohepatitis |
| NT-proBNP | N-terminal prohormone of brain natriuretic peptide |
| OSA | Obstructive sleep apnea |
| PAD | Peripheral artery disease |
| PCOS | Polycystic Ovary Syndrome |
| PCSK9 | Proprotein convertase subtilisin/kexin type 9 |
| PAP | Positive airway pressure |
| POI | Primary Ovarian Insufficiency |
| RCT | Randomized controlled trial |
| RMR | Resting metabolic rate |
| SGLT2i | Sodium-glucose cotransporter-2 inhibitors |
| siRNA | Small interfering RNA |
| T2DM | Type 2 diabetes mellitus |
| TTh | Testosterone therapy |
| TZD | Thiazolidinedione |
| VO2 max | Maximum oxygen consumption |
References
- Theodorakis, N.; Nikolaou, M. Integrated Management of Cardiovascular-Renal-Hepatic-Metabolic Syndrome: Expanding Roles of SGLT2is, GLP-1RAs, and GIP/GLP-1RAs. Biomedicines 2025, 13, 135. [Google Scholar] [CrossRef]
- Capone, F.; Vettor, R.; Schiattarella, G.G. Cardiometabolic HFpEF: NASH of the Heart. Circulation 2023, 147, 451–453. [Google Scholar] [CrossRef] [PubMed]
- Anker, S.D.; Butler, J.; Filippatos, G.; Ferreira, J.P.; Bocchi, E.; Böhm, M.; Brunner-La Rocca, H.P.; Choi, D.J.; Chopra, V.; Chuquiure-Valenzuela, E.; et al. Empagliflozin in Heart Failure with a Preserved Ejection Fraction. N. Engl. J. Med. 2021, 385, 1451–1461. [Google Scholar] [CrossRef]
- Packer, M.; Anker, S.D.; Butler, J.; Filippatos, G.; Pocock, S.J.; Carson, P.; Januzzi, J.; Verma, S.; Tsutsui, H.; Brueckmann, M.; et al. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. N. Engl. J. Med. 2020, 383, 1413–1424. [Google Scholar] [CrossRef] [PubMed]
- Solomon, S.D.; McMurray, J.J.V.; Claggett, B.; de Boer, R.A.; DeMets, D.; Hernandez, A.F.; Inzucchi, S.E.; Kosiborod, M.N.; Lam, C.S.P.; Martinez, F.; et al. Dapagliflozin in Heart Failure with Mildly Reduced or Preserved Ejection Fraction. N. Engl. J. Med. 2022, 387, 1089–1098. [Google Scholar] [CrossRef]
- McMurray, J.J.V.; Solomon, S.D.; Inzucchi, S.E.; Køber, L.; Kosiborod, M.N.; Martinez, F.A.; Ponikowski, P.; Sabatine, M.S.; Anand, I.S.; Bělohlávek, J.; et al. Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N. Engl. J. Med. 2019, 381, 1995–2008. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, D.L.; Szarek, M.; Steg, P.G.; Cannon, C.P.; Leiter, L.A.; McGuire, D.K.; Lewis, J.B.; Riddle, M.C.; Voors, A.A.; Metra, M.; et al. Sotagliflozin in Patients with Diabetes and Recent Worsening Heart Failure. N. Engl. J. Med. 2021, 384, 117–128. [Google Scholar] [CrossRef]
- Vaduganathan, M.; Docherty, K.F.; Claggett, B.L.; Jhund, P.S.; de Boer, R.A.; Hernandez, A.F.; Inzucchi, S.E.; Kosiborod, M.N.; Lam, C.S.P.; Martinez, F.; et al. SGLT-2 inhibitors in patients with heart failure: A comprehensive meta-analysis of five randomised controlled trials. Lancet 2022, 400, 757–767. [Google Scholar] [CrossRef]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2023 Focused Update of the 2021 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure. Eur. Heart J. 2023, 44, 3627–3639. [Google Scholar] [CrossRef]
- Voors, A.A.; Angermann, C.E.; Teerlink, J.R.; Collins, S.P.; Kosiborod, M.; Biegus, J.; Ferreira, J.P.; Nassif, M.E.; Psotka, M.A.; Tromp, J.; et al. The SGLT2 inhibitor empagliflozin in patients hospitalized for acute heart failure: A multinational randomized trial. Nat. Med. 2022, 28, 568–574. [Google Scholar] [CrossRef]
- The EMPA-KIDNEY Collaborative Group; Herrington, W.G.; Staplin, N.; Wanner, C.; Green, J.B.; Hauske, S.J.; Emberson, J.R.; Preiss, D.; Judge, P.; Mayne, K.J.; et al. Empagliflozin in Patients with Chronic Kidney Disease. N. Engl. J. Med. 2023, 388, 117–127. [Google Scholar] [CrossRef]
- Heerspink, H.J.L.; Stefánsson, B.V.; Correa-Rotter, R.; Chertow, G.M.; Greene, T.; Hou, F.F.; Mann, J.F.E.; McMurray, J.J.V.; Lindberg, M.; Rossing, P.; et al. Dapagliflozin in Patients with Chronic Kidney Disease. N. Engl. J. Med. 2020, 383, 1436–1446. [Google Scholar] [CrossRef] [PubMed]
- Bakris, G.L.; Agarwal, R.; Anker, S.D.; Pitt, B.; Ruilope, L.M.; Rossing, P.; Kolkhof, P.; Nowack, C.; Schloemer, P.; Joseph, A.; et al. Effect of Finerenone on Chronic Kidney Disease Outcomes in Type 2 Diabetes. N. Engl. J. Med. 2020, 383, 2219–2229. [Google Scholar] [CrossRef] [PubMed]
- Pitt, B.; Filippatos, G.; Agarwal, R.; Anker, S.D.; Bakris, G.L.; Rossing, P.; Joseph, A.; Kolkhof, P.; Nowack, C.; Schloemer, P.; et al. Cardiovascular Events with Finerenone in Kidney Disease and Type 2 Diabetes. N. Engl. J. Med. 2021, 385, 2252–2263. [Google Scholar] [CrossRef]
- Agarwal, R.; Filippatos, G.; Pitt, B.; Anker, S.D.; Rossing, P.; Joseph, A.; Kolkhof, P.; Nowack, C.; Gebel, M.; Ruilope, L.M.; et al. Cardiovascular and Kidney Outcomes with Finerenone in Patients with Type 2 Diabetes and Chronic Kidney Disease: The FIDELITY Pooled Analysis. Eur. Heart J. 2022, 43, 474–484. [Google Scholar] [CrossRef]
- Solomon, S.D.; McMurray, J.J.V.; Vaduganathan, M.; Claggett, B.; Jhund, P.S.; Desai, A.S.; Henderson, A.D.; Lam, C.S.P.; Pitt, B.; Senni, M.; et al. Finerenone in Heart Failure with Mildly Reduced or Preserved Ejection Fraction. N. Engl. J. Med. 2024, 391, 1475–1485. [Google Scholar] [CrossRef]
- Vaduganathan, M.; Filippatos, G.; Claggett, B.L.; Desai, A.S.; Jhund, P.S.; Henderson, A.; Brinker, M.; Kolkhof, P.; Schloemer, P.; Lay-Flurrie, J.; et al. Finerenone in Heart Failure and Chronic Kidney Disease with Type 2 Diabetes: FINE-HEART Pooled Analysis of Cardiovascular, Kidney and Mortality Outcomes. Nat. Med. 2024, 30, 1–7. [Google Scholar] [CrossRef]
- Jhund, P.S.; Talebi, A.; Henderson, A.D.; Claggett, B.L.; Vaduganathan, M.; Desai, A.S.; Lam, C.S.P.; Pitt, B.; Senni, M.; Shah, S.J.; et al. Mineralocorticoid Receptor Antagonists in Heart Failure: An Individual Patient-Level Meta-Analysis. Lancet 2024, 404, 1119–1131. [Google Scholar] [CrossRef] [PubMed]
- Wilding, J.P.H.; Batterham, R.L.; Calanna, S.; Davies, M.; Van Gaal, L.F.; Lingvay, I.; McGowan, B.M.; Rosenstock, J.; Tran, M.T.D.; Wadden, T.A.; et al. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N. Engl. J. Med. 2021, 384, 989–1002. [Google Scholar] [CrossRef]
- Davies, M.; Færch, L.; Jeppesen, O.K.; Pakseresht, A.; Pedersen, S.D.; Perreault, L.; Rosenstock, J.; Shimomura, I.; Viljoen, A.; Wadden, T.A.; et al. Semaglutide 2.4 mg Once a Week in Adults with Overweight or Obesity, and Type 2 Diabetes (STEP 2): A Randomised, Double-Blind, Double-Dummy, Placebo-Controlled, Phase 3 Trial. Lancet 2021, 397, 971–984. [Google Scholar] [CrossRef]
- Sattar, N.; Lee, M.M.Y.; Kristensen, S.L.; Branch, K.R.H.; Del Prato, S.; Khurmi, N.S.; Lam, C.S.P.; Lopes, R.D.; McMurray, J.J.V.; Pratley, R.E.; et al. Cardiovascular, Mortality, and Kidney Outcomes with GLP-1 Receptor Agonists in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomised Trials. Lancet Diabetes Endocrinol. 2021, 9, 653–662. [Google Scholar] [CrossRef] [PubMed]
- McGuire, D.K.; Shih, W.J.; Cosentino, F.; Charbonnel, B.; Cherney, D.Z.I.; Dagogo-Jack, S.; Pratley, R.; Greenberg, M.; Wang, S.; Huyck, S.; et al. Association of SGLT2 Inhibitors with Cardiovascular and Kidney Outcomes in Patients with Type 2 Diabetes: A Meta-Analysis. JAMA Cardiol. 2021, 6, 148–158. [Google Scholar] [CrossRef] [PubMed]
- Marx, N.; Federici, M.; Schütt, K.; Müller-Wieland, D.; Ajjan, R.A.; Antunes, M.J.; Christodorescu, R.M.; Crawford, C.; Di Angelantonio, E.; Eliasson, B.; et al. 2023 ESC Guidelines for the Management of Cardiovascular Disease in Patients with Diabetes. Eur. Heart J. 2023, 44, 4043–4140. [Google Scholar] [CrossRef]
- Kosiborod, M.N.; Abildstrøm, S.Z.; Borlaug, B.A.; Butler, J.; Rasmussen, S.; Davies, M.; Hovingh, G.K.; Kitzman, D.W.; Lindegaard, M.L.; Møller, D.V.; et al. Semaglutide in Patients with Heart Failure with Preserved Ejection Fraction and Obesity. N. Engl. J. Med. 2023, 389, 1069–1084. [Google Scholar] [CrossRef]
- Kosiborod, M.N.; Petrie, M.C.; Borlaug, B.A.; Butler, J.; Davies, M.J.; Hovingh, G.K.; Kitzman, D.W.; Møller, D.V.; Treppendahl, M.B.; Verma, S.; et al. Semaglutide in Patients with Obesity-Related Heart Failure and Type 2 Diabetes. N. Engl. J. Med. 2024, 390, 1394–1407. [Google Scholar] [CrossRef] [PubMed]
- Butler, J.; Shah, S.J.; Petrie, M.C.; Borlaug, B.A.; Abildstrøm, S.Z.; Davies, M.J.; Hovingh, G.K.; Kitzman, D.W.; Møller, D.V.; Verma, S.; et al. Semaglutide Versus Placebo in People with Obesity-Related Heart Failure with Preserved Ejection Fraction: A Pooled Analysis of the STEP-HFpEF and STEP-HFpEF DM Randomised Trials. Lancet 2024, 403, 1635–1648. [Google Scholar] [CrossRef]
- Lincoff, A.M.; Brown-Frandsen, K.; Colhoun, H.M.; Deanfield, J.; Emerson, S.S.; Esbjerg, S.; Hardt-Lindberg, S.; Hovingh, G.K.; Kahn, S.E.; Kushner, R.F.; et al. Semaglutide and Cardiovascular Outcomes in Obesity without Diabetes. N. Engl. J. Med. 2023, 389, 2221–2232. [Google Scholar] [CrossRef]
- Deanfield, J.; Verma, S.; Scirica, B.M.; Kahn, S.E.; Emerson, S.S.; Ryan, D.; Lingvay, I.; Colhoun, H.M.; Plutzky, J.; Kosiborod, M.N.; et al. Semaglutide and Cardiovascular Outcomes in Patients with Obesity and Prevalent Heart Failure: A Prespecified Analysis of the SELECT Trial. Lancet 2024, 404, 773–786. [Google Scholar] [CrossRef]
- Perkovic, V.; Tuttle, K.R.; Rossing, P.; Mahaffey, K.W.; Mann, J.F.E.; Bakris, G.; Baeres, F.M.M.; Idorn, T.; Bosch-Traberg, H.; Lausvig, N.L.; et al. Effects of Semaglutide on Chronic Kidney Disease in Patients with Type 2 Diabetes. N. Engl. J. Med. 2024, 391, 109–121. [Google Scholar] [CrossRef]
- Kosiborod, M.N.; Deanfield, J.; Pratley, R.; Borlaug, B.A.; Butler, J.; Davies, M.J.; Emerson, S.S.; Kahn, S.E.; Kitzman, D.W.; Lingvay, I.; et al. Semaglutide versus Placebo in Patients with Heart Failure and Mildly Reduced or Preserved Ejection Fraction: A Pooled Analysis of the SELECT, FLOW, STEP-HFpEF, and STEP-HFpEF DM Randomised Trials. Lancet 2024, 404, 949–961. [Google Scholar] [CrossRef]
- Jastreboff, A.M.; Aronne, L.J.; Ahmad, N.N.; Wharton, S.; Connery, L.; Alves, B.; Kiyosue, A.; Zhang, S.; Liu, B.; Bunck, M.C.; et al. Tirzepatide Once Weekly for the Treatment of Obesity. N. Engl. J. Med. 2022, 387, 205–216. [Google Scholar] [CrossRef] [PubMed]
- Garvey, W.T.; Frias, J.P.; Jastreboff, A.M.; le Roux, C.W.; Sattar, N.; Aizenberg, D.; Mao, H.; Zhang, S.; Ahmad, N.N.; Bunck, M.C.; et al. Tirzepatide Once Weekly for the Treatment of Obesity in People with Type 2 Diabetes (SURMOUNT-2): A Double-Blind, Randomised, Multicentre, Placebo-Controlled, Phase 3 Trial. Lancet 2023, 402, 613–626. [Google Scholar] [CrossRef] [PubMed]
- Jastreboff, A.M.; le Roux, C.W.; Stefanski, A.; Aronne, L.J.; Halpern, B.; Wharton, S.; Wilding, J.P.H.; Perreault, L.; Zhang, S.; Battula, R.; et al. Tirzepatide for Obesity Treatment and Diabetes Prevention. N. Engl. J. Med. 2024. [Google Scholar] [CrossRef] [PubMed]
- Jastreboff, A.M.; Kaplan, L.M.; Frías, J.P.; Wu, Q.; Du, Y.; Gurbuz, S.; Coskun, T.; Haupt, A.; Milicevic, Z.; Hartman, M.L.; et al. Triple-Hormone-Receptor Agonist Retatrutide for Obesity—A Phase 2 Trial. N. Engl. J. Med. 2023, 389, 514–526. [Google Scholar] [CrossRef]
- Newsome, P.N.; Buchholtz, K.; Cusi, K.; Linder, M.; Okanoue, T.; Ratziu, V.; Sanyal, A.J.; Sejling, A.S.; Harrison, S.A.; NN9931-4296 Investigators. A Placebo-Controlled Trial of Subcutaneous Semaglutide in Nonalcoholic Steatohepatitis. N. Engl. J. Med. 2021, 384, 1113–1124. [Google Scholar] [CrossRef]
- Loomba, R.; Abdelmalek, M.F.; Armstrong, M.J.; Jara, M.; Kjær, M.S.; Krarup, N.; Lawitz, E.; Ratziu, V.; Sanyal, A.J.; Schattenberg, J.M.; et al. Semaglutide 2.4 mg Once Weekly in Patients with Non-Alcoholic Steatohepatitis-Related Cirrhosis: A Randomised, Placebo-Controlled Phase 2 Trial. Lancet Gastroenterol. Hepatol. 2023, 8, 511–522. [Google Scholar] [CrossRef]
- Loomba, R.; Hartman, M.L.; Lawitz, E.J.; Vuppalanchi, R.; Boursier, J.; Bugianesi, E.; Yoneda, M.; Behling, C.; Cummings, O.W.; Tang, Y.; et al. Tirzepatide for Metabolic Dysfunction-Associated Steatohepatitis with Liver Fibrosis. N. Engl. J. Med. 2024, 391, 299–310. [Google Scholar] [CrossRef]
- Malhotra, A.; Bednarik, J.; Chakladar, S.; Dunn, J.P.; Weaver, T.; Grunstein, R.; Fietze, I.; Redline, S.; Azarbarzin, A.; Sands, S.A.; et al. Tirzepatide for the Treatment of Obstructive Sleep Apnea: Rationale, Design, and Sample Baseline Characteristics of the SURMOUNT-OSA Phase 3 Trial. Contemp. Clin. Trials 2024, 141, 107516. [Google Scholar] [CrossRef]
- Wittert, G.; Bracken, K.; Robledo, K.P.; Grossmann, M.; Yeap, B.B.; Handelsman, D.J.; Stuckey, B.; Conway, A.; Inder, W.; McLachlan, R.; et al. Testosterone Treatment to Prevent or Revert Type 2 Diabetes in Men Enrolled in a Lifestyle Programme (T4DM): A Randomised, Double-Blind, Placebo-Controlled, 2-Year, Phase 3b Trial. Lancet Diabetes Endocrinol. 2021, 9, 32–45. [Google Scholar] [CrossRef]
- Muraleedharan, V.; Marsh, H.; Kapoor, D.; Channer, K.S.; Jones, T.H. Testosterone Deficiency is Associated with Increased Risk of Mortality and Testosterone Replacement Improves Survival in Men with Type 2 Diabetes. Eur. J. Endocrinol. 2013, 169, 725–733. [Google Scholar] [CrossRef]
- Lincoff, A.M.; Bhasin, S.; Flevaris, P.; Mitchell, L.M.; Basaria, S.; Boden, W.E.; Cunningham, G.R.; Granger, C.B.; Khera, M.; Thompson, I.M., Jr.; et al. Cardiovascular Safety of Testosterone-Replacement Therapy. N. Engl. J. Med. 2023, 389, 107–117. [Google Scholar] [CrossRef] [PubMed]
- Cittadini, A.; Salzano, A.; Iacoviello, M.; Triggiani, V.; Rengo, G.; Cacciatore, F.; Maiello, C.; Limongelli, G.; Masarone, D.; Perticone, F.; et al. Multiple Hormonal and Metabolic Deficiency Syndrome Predicts Outcome in Heart Failure: The T.O.S.CA. Registry. Eur. J. Prev. Cardiol. 2021, 28, 1691–1700. [Google Scholar] [CrossRef]
- Park, S.; Gale, S.E.; Watson, K. The Role of Testosterone in Patients with Heart Failure: A Systematic Review. Cardiol. Rev. 2021, 29, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Theodorakis, N.; Kreouzi, M.; Hitas, C.; Anagnostou, D.; Nikolaou, M. Growth Hormone and Heart Failure: Implications for Patient Stratification, Prognosis, and Precision Medicine. Diagnostics 2024, 14, 2831. [Google Scholar] [CrossRef] [PubMed]
- Theodorakis, N.; Feretzakis, G.; Kreouzi, M.; Anagnostou, D.; Hitas, C.; Verykios, V.S.; Nikolaou, M. Growth Hormone Therapy in Chronic Heart Failure: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Clin. Endocrinol. Metab. 2024, dgae814. [Google Scholar] [CrossRef]
- Shi, C.; Bao, Y.; Chen, X.; Tian, L. The Effectiveness of Thyroid Hormone Replacement Therapy on Heart Failure and Low-Triiodothyronine Syndrome: An Updated Systematic Review and Meta-Analysis of Randomized Controlled Trials. Endocr. Pract. 2022, 28, 1178–1186. [Google Scholar] [CrossRef]
- Theodorakis, N.; Feretzakis, G.; Kreouzi, M.; Anagnostou, D.; Hitas, C.; Verykios, V.S.; Nikolaou, M. Ghrelin: An Emerging Therapy for Heart Failure. Clin. Endocrinol. 2025, 102, 403–412. [Google Scholar] [CrossRef]
- Theodorakis, N.; Feretzakis, G.; Vamvakou, G.; Verykios, V.S.; Polymeris, A.; Nikolaou, M. Testosterone Therapy for Functional Hypogonadism in Middle-Aged and Elderly Males: Current Evidence and Future Perspectives. Hormones 2024, 23, 801–817. [Google Scholar] [CrossRef]
- Kern, L.M.; Bynum, J.P.W.; Pincus, H.A. Care Fragmentation, Care Continuity, and Care Coordination—How They Differ and Why It Matters. JAMA Intern. Med. 2024, 184, 236–237. [Google Scholar] [CrossRef]
- Joo, J.Y. Fragmented Care and Chronic Illness Patient Outcomes: A Systematic Review. Nurs. Open 2023, 10, 3460–3473. [Google Scholar] [CrossRef]
- John, M. Fragmentation of Care in Diabetes and Endocrinology—What is the Way Forward? Chron. Diabetes Res. Pract. 2022, 1, 43–46. [Google Scholar] [CrossRef]
- Colvin, C.L.; Akinyelure, O.P.; Rajan, M.; Safford, M.M.; Carson, A.P.; Muntner, P.; Colantonio, L.D.; Kern, L.M. Diabetes, Gaps in Care Coordination, and Preventable Adverse Events. Am. J. Manag. Care 2023, 29, e162–e168. [Google Scholar] [CrossRef] [PubMed]
- Tan, G.D.; Kozlowska, O.; Rea, R.D. Integrated Care and Diabetes: Challenges, Principles, and Opportunities. Clin. Integr. Care 2021, 4, 100037. [Google Scholar] [CrossRef]
- Shapiro, M.D.; Maron, D.J.; Morris, P.B.; Kosiborod, M.; Sandesara, P.B.; Virani, S.S.; Khera, A.; Ballantyne, C.M.; Baum, S.J.; Sperling, L.S.; et al. Preventive Cardiology as a Subspecialty of Cardiovascular Medicine: JACC Council Perspectives. J. Am. Coll. Cardiol. 2019, 74, 1926–1942. [Google Scholar] [CrossRef]
- Wilhelm, M.; Abreu, A.; Adami, P.E.; Ambrosetti, M.; Antonopoulou, M.; Biffi, A.; Cavarretta, E.; D’Ascenzi, F.; Gibson, I.; Grobbee, D.E.; et al. EAPC Core Curriculum for Preventive Cardiology. Eur. J. Prev. Cardiol. 2022, 29, 251–274. [Google Scholar] [CrossRef] [PubMed]
- Saxon, D.R.; Reiter-Brennan, C.; Blaha, M.J.; Eckel, R.H. Cardiometabolic Medicine: Development of a New Subspecialty. J. Clin. Endocrinol. Metab. 2020, 105, dgaa261. [Google Scholar] [CrossRef]
- Soroosh, G.P.; Dzaye, O.; Reiter-Brennan, C.; Blaha, M.J. Cardiometabolic Medicine: A Review of the Current Proposed Approaches to Revamped Training in the United States. Cardiovasc. Endocrinol. Metab. 2021, 10, 168–174. [Google Scholar] [CrossRef]
- Kreouzi, M.; Theodorakis, N.; Constantinou, C. Lessons Learned from Blue Zones, Lifestyle Medicine Pillars, and Beyond: An Update on the Contributions of Behavior and Genetics to Wellbeing and Longevity. Am. J. Lifestyle Med. 2022, 18, 750–765. [Google Scholar] [CrossRef]
- Nikolaou, M.; Theodorakis, N.; Feretzakis, G.; Vamvakou, G.; Hitas, C.; Kalantzi, S.; Spyridaki, A.; Apostolos, A.; Verykios, V.S.; Toutouzas, K. Nationwide Mortality Trends from 2001 to 2020 in Greece: Health Policy Implications under the Scope of Aging Societies. Hellenic J. Cardiol. 2024. [Google Scholar] [CrossRef]
- Woodruff, R.C.; Tong, X.; Khan, S.S.; Shah, N.S.; Jackson, S.L.; Loustalot, F.; Vaughan, A.S. Trends in Cardiovascular Disease Mortality Rates and Excess Deaths, 2010–2022. Am. J. Prev. Med. 2024, 66, 582–589. [Google Scholar] [CrossRef]
- Conrad, N.; Molenberghs, G.; Verbeke, G.; Zaccardi, F.; Lawson, C.; Friday, J.M.; Su, H.; Jhund, P.S.; Sattar, N.; Rahimi, K.; et al. Trends in Cardiovascular Disease Incidence Among 22 Million People in the UK Over 20 Years: Population-Based Study. BMJ 2024, 385, e078523. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Obesity and Overweight; WHO: Geneva, Switzerland, 2024. [Google Scholar]
- European Commission. Overweight and Obesity—BMI Statistics; Eurostat: Luxembourg, 2024. [Google Scholar]
- Khan, M.A.B.; Hashim, M.J.; King, J.K.; Govender, R.D.; Mustafa, H.; Al Kaabi, J. Epidemiology of Type 2 Diabetes—Global Burden of Disease and Forecasted Trends. J. Epidemiol. Glob. Health 2020, 10, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Gavina, C.; Carvalho, D.S.; Valente, F.; Bernardo, F.; Dinis-Oliveira, R.J.; Santos-Araújo, C.; Taveira-Gomes, T. 20 Years of Real-World Data to Estimate the Prevalence of Heart Failure and Its Subtypes in an Unselected Population of Integrated Care Units. J. Cardiovasc. Dev. Dis. 2022, 9, 149. [Google Scholar] [CrossRef]
- Simonsmeier, B.A.; Flaig, M.; Simacek, T.; Schneider, M. What Sixty Years of Research Says About the Effectiveness of Patient Education on Health: A Second-Order Meta-Analysis. Health Psychol. Rev. 2022, 16, 450–474. [Google Scholar] [CrossRef]
- McEvoy, J.W.; McCarthy, C.P.; Bruno, R.M.; Brouwers, S.; Canavan, M.D.; Ceconi, C.; Christodorescu, R.M.; Daskalopoulou, S.S.; Ferro, C.J.; Gerdts, E.; et al. 2024 ESC Guidelines for the Management of Elevated Blood Pressure and Hypertension. Eur. Heart J. 2024, 45, 3912–4018. [Google Scholar] [CrossRef]
- Zeitouni, M.; Sabouret, P.; Kerneis, M.; Silvain, J.; Collet, J.P.; Bruckert, E.; Montalescot, G. 2019 ESC/EAS Guidelines for Management of Dyslipidaemia: Strengths and Limitations. Eur. Heart J. Cardiovasc. Pharmacother. 2021, 7, 324–333. [Google Scholar] [CrossRef]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.M.; Capodanno, D.; et al. 2021 ESC Guidelines on Cardiovascular Disease Prevention in Clinical Practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef] [PubMed]
- He, F.J.; Tan, M.; Ma, Y.; MacGregor, G.A. Salt Reduction to Prevent Hypertension and Cardiovascular Disease: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2020, 75, 632–647. [Google Scholar] [CrossRef]
- Hanssen, H.; Boardman, H.; Deiseroth, A.; Moholdt, T.; Simonenko, M.; Kränkel, N.; Niebauer, J.; Tiberi, M.; Abreu, A.; Solberg, E.E.; et al. Personalized Exercise Prescription in the Prevention and Treatment of Arterial Hypertension: A Consensus Document from the European Association of Preventive Cardiology (EAPC) and the ESC Council on Hypertension. Eur. J. Prev. Cardiol. 2022, 29, 205–215. [Google Scholar] [CrossRef]
- Van Hoof, R.; Hespel, P.; Fagard, R.; Lijnen, P.; Staessen, J.; Amery, A. Effect of Endurance Training on Blood Pressure at Rest, During Exercise, and During 24 Hours in Sedentary Men. Am. J. Cardiol. 1989, 63, 945–949. [Google Scholar] [CrossRef] [PubMed]
- Church, T.S.; Blair, S.N.; Cocreham, S.; Johannsen, N.; Johnson, W.; Kramer, K.; Mikus, C.R.; Myers, V.; Nauta, M.; Rodarte, R.Q.; et al. Effects of Aerobic and Resistance Training on Hemoglobin A1c Levels in Patients with Type 2 Diabetes: A Randomized Controlled Trial. JAMA 2010, 304, 2253–2262. [Google Scholar] [CrossRef] [PubMed]
- Sluik, D.; Buijsse, B.; Muckelbauer, R.; Kaaks, R.; Teucher, B.; Johnsen, N.F.; Tjønneland, A.; Overvad, K.; Ostergaard, J.N.; Amiano, P.; et al. Physical Activity and Mortality in Individuals with Diabetes Mellitus: A Prospective Study and Meta-Analysis. Arch. Intern. Med. 2012, 172, 1285–1295. [Google Scholar] [CrossRef]
- Neter, J.E.; Stam, B.E.; Kok, F.J.; Grobbee, D.E.; Geleijnse, J.M. Influence of Weight Reduction on Blood Pressure: A Meta-Analysis of Randomized Controlled Trials. Hypertension 2003, 42, 878–884. [Google Scholar] [CrossRef] [PubMed]
- Harris, E. Study Examines Intermittent Fasting and Cardiovascular Mortality. JAMA 2024, 331, 1440. [Google Scholar] [CrossRef]
- Patel, R.B.; Al Rifai, M.; McEvoy, J.W.; Vaduganathan, M. Implications of Specialist Density for Diabetes Care in the United States. JAMA Cardiol. 2019, 4, 1174–1175. [Google Scholar] [CrossRef]
- de Freminville, J.B.; Amar, L.; Azizi, M.; Mallart-Riancho, J. Endocrine Causes of Hypertension: Literature Review and Practical Approach. Hypertens. Res. 2023, 46, 2679–2692. [Google Scholar] [CrossRef]
- De Bhailis, Á.M.; Kalra, P.A. Hypertension and the Kidneys. Br. J. Hosp. Med. 2022, 83, 1–11. [Google Scholar] [CrossRef]
- Newman, C.B.; Blaha, M.J.; Boord, J.B.; Cariou, B.; Chait, A.; Fein, H.G.; Ginsberg, H.N.; Goldberg, I.J.; Murad, M.H.; Subramanian, S.; et al. Lipid Management in Patients with Endocrine Disorders: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2020, 105, dgaa674. [Google Scholar] [CrossRef]
- O’Donoghue, M.L.; Rosenson, R.S.; Gencer, B.; López, J.A.G.; Lepor, N.E.; Baum, S.J.; Stout, E.; Gaudet, D.; Knusel, B.; Kuder, J.F.; et al. Small Interfering RNA to Reduce Lipoprotein(a) in Cardiovascular Disease. N. Engl. J. Med. 2022, 387, 1855–1864. [Google Scholar] [CrossRef]
- Vrints, C.; Andreotti, F.; Koskinas, K.C.; Rossello, X.; Adamo, M.; Ainslie, J.; Banning, A.P.; Budaj, A.; Buechel, R.R.; Chiariello, G.A.; et al. 2024 ESC Guidelines for the Management of Chronic Coronary Syndromes. Eur. Heart J. 2024, 45, 3415–3537. [Google Scholar] [CrossRef]
- Packer, M.; Zile, M.R.; Kramer, C.M.; Baum, S.J.; Litwin, S.E.; Menon, V.; Ge, J.; Weerakkody, G.J.; Ou, Y.; Bunck, M.C.; et al. Tirzepatide for Heart Failure with Preserved Ejection Fraction and Obesity. N. Engl. J. Med. 2024, 392, 427–437. [Google Scholar] [CrossRef] [PubMed]
- Newsome, P.N.; Sanyal, A.J.; Engebretsen, K.A.; Kliers, I.; Østergaard, L.; Vanni, D.; Bugianesi, E.; Rinella, M.E.; Roden, M.; Ratziu, V. Semaglutide 2.4 mg in Participants with Metabolic Dysfunction-Associated Steatohepatitis: Baseline Characteristics and Design of the Phase 3 ESSENCE Trial. Aliment. Pharmacol. Ther. 2024, 60, 1525–1533. [Google Scholar] [CrossRef] [PubMed]
- Adhikari, R.; Jha, K.; Dardari, Z.; Heyward, J.; Blumenthal, R.S.; Eckel, R.H.; Alexander, G.C.; Blaha, M.J. National Trends in Use of Sodium-Glucose Cotransporter-2 Inhibitors and Glucagon-Like Peptide-1 Receptor Agonists by Cardiologists and Other Specialties, 2015 to 2020. J. Am. Heart Assoc. 2022, 11, e023811. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee. 9. Pharmacologic Approaches to Glycemic Treatment: Standards of Care in Diabetes-2024. Diabetes Care 2024, 47, S158–S178. [Google Scholar] [CrossRef] [PubMed]
- Cai, C.X.; Hribar, M.; Baxter, S.; Goetz, K.; Swaminathan, S.S.; Flowers, A.; Brown, E.N.; Toy, B.; Xu, B.; Chen, J.; et al. Semaglutide and Nonarteritic Anterior Ischemic Optic Neuropathy. JAMA Ophthalmol. 2025. Online ahead of print. [Google Scholar] [CrossRef]
- Hartupee, J.; Mann, D.L. Neurohormonal Activation in Heart Failure with Reduced Ejection Fraction. Nat. Rev. Cardiol. 2017, 14, 30–38. [Google Scholar] [CrossRef]
- Xie, Y.; Wei, Y.; Li, D.; Pu, J.; Ding, H.; Zhang, X. Mechanisms of SGLT2 Inhibitors in Heart Failure and Their Clinical Value. J. Cardiovasc. Pharmacol. 2023, 81, 4–14. [Google Scholar] [CrossRef]
- Cannarella, R.; Barbagallo, F.; Crafa, A.; Mongioì, L.M.; Aversa, A.; Greco, E.; Condorelli, R.A.; La Vignera, S.; Calogero, A.E. Testosterone Replacement Therapy in Hypogonadal Male Patients with Hypogonadism and Heart Failure: A Meta-Analysis of Randomized Controlled Studies. Minerva Urol. Nephrol. 2022, 74, 418–427. [Google Scholar] [CrossRef]
- Toma, M.; McAlister, F.A.; Coglianese, E.E.; Vidi, V.; Vasaiwala, S.; Bakal, J.A.; Armstrong, P.W.; Ezekowitz, J.A. Testosterone Supplementation in Heart Failure: A Meta-Analysis. Circ. Heart Fail. 2012, 5, 315–321. [Google Scholar] [CrossRef]
- Theodorakis, N.; Kreouzi, M.; Hitas, C.; Anagnostou, D.; Nikolaou, M. Adipokines and Cardiometabolic Heart Failure with Preserved Ejection Fraction: A State-of-the-Art Review. Diagnostics 2024, 14, 2677. [Google Scholar] [CrossRef]
- Michos, E.D.; Budoff, M.J. Testosterone: Therapeutic or Toxic for the Cardiovascular Health of Men? Lancet Healthy Longev. 2022, 3, e368–e369. [Google Scholar] [CrossRef]
- Hackett, G. Metabolic Effects of Testosterone Therapy in Men with Type 2 Diabetes and Metabolic Syndrome. Sex. Med. Rev. 2019, 7, 476–490. [Google Scholar] [CrossRef]
- Fallara, G.; Pozzi, E.; Belladelli, F.; Corsini, C.; Boeri, L.; Capogrosso, P.; Montorsi, F.; Salonia, A. Cardiovascular Morbidity and Mortality in Men—Findings from a Meta-Analysis on the Time-Related Measure of Risk of Exogenous Testosterone. J. Sex. Med. 2022, 19, 1243–1254. [Google Scholar] [CrossRef] [PubMed]
- Hackett, G.I. Testosterone Replacement Therapy and Mortality in Older Men. Drug Saf. 2016, 39, 117–130. [Google Scholar] [CrossRef]
- Touraine, P.; Chabbert-Buffet, N.; Plu-Bureau, G.; Duranteau, L.; Sinclair, A.H.; Tucker, E.J. Premature Ovarian Insufficiency. Nat. Rev. Dis. Primers 2024, 10, 63. [Google Scholar] [CrossRef] [PubMed]
- Chon, S.J.; Umair, Z.; Yoon, M.S. Premature Ovarian Insufficiency: Past, Present, and Future. Front. Cell Dev. Biol. 2021, 9, 672890. [Google Scholar] [CrossRef] [PubMed]
- Panay, N.; Anderson, R.A.; Bennie, A.; Cedars, M.; Davies, M.; Ee, C.; Gravholt, C.H.; Kalantaridou, S.; Kallen, A.; Kim, K.Q.; et al. Evidence-Based Guideline: Premature Ovarian Insufficiency. Hum. Reprod. Open 2024, 2024, hoae065. [Google Scholar] [CrossRef]
- Honigberg, M.C.; Zekavat, S.M.; Aragam, K.; Finneran, P.; Klarin, D.; Bhatt, D.L.; Januzzi, J.L., Jr.; Scott, N.S.; Natarajan, P. Association of Premature Natural and Surgical Menopause with Incident Cardiovascular Disease. JAMA 2019, 322, 2411–2421. [Google Scholar] [CrossRef]
- Liu, J.; Jin, X.; Liu, W.; Chen, W.; Wang, L.; Feng, Z.; Huang, J. The Risk of Long-Term Cardiometabolic Disease in Women with Premature or Early Menopause: A Systematic Review and Meta-Analysis. Front. Cardiovasc. Med. 2023, 10, 1131251. [Google Scholar] [CrossRef] [PubMed]
- Mishra, G.D.; Davies, M.C.; Hillman, S.; Chung, H.F.; Roy, S.; Maclaran, K.; Hickey, M. Optimising Health After Early Menopause. Lancet 2024, 403, 958–968. [Google Scholar] [CrossRef] [PubMed]

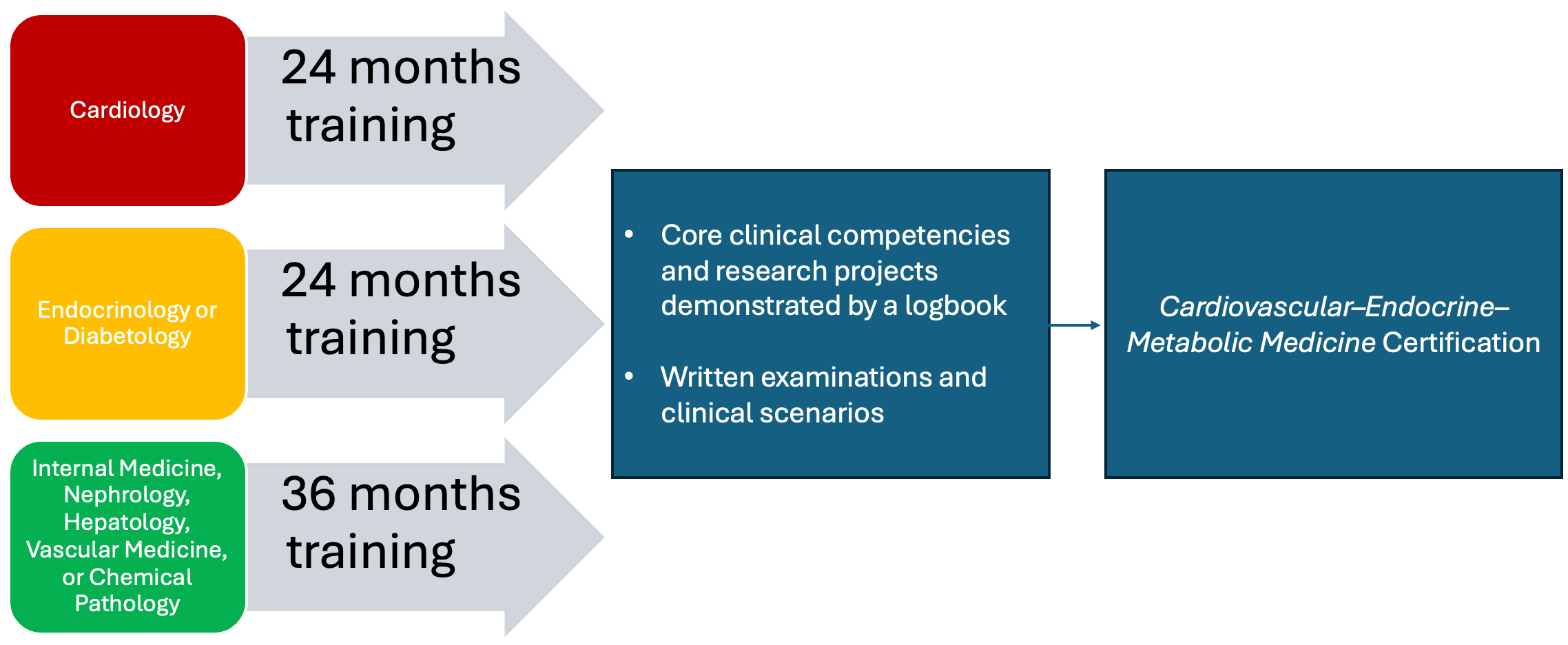
| Training Areas | Cardiology Entry Path (24 Months) | Endocrinology or Diabetology Entry Path (24 Months) | Internal Medicine, Vascular Medicine, Nephrology, Hepatology, or Chemical Pathology Entry Path (36 Months) |
|---|---|---|---|
| Cardiology | N/A | 12 months | 12 months |
| Endocrinology | 12 months | N/A | 12 months |
| Nephrology and Hepatology | 5 months | 5 months | 5 months |
| Lifestyle Medicine | 6 months | 6 months | 6 months |
| Sleep Medicine | 1 month | 1 month | 1 month |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Theodorakis, N.; Nikolaou, M.; Krentz, A. Cardiovascular–Endocrine–Metabolic Medicine: Proposing a New Clinical Sub-Specialty Amid the Cardiometabolic Pandemic. Biomolecules 2025, 15, 373. https://doi.org/10.3390/biom15030373
Theodorakis N, Nikolaou M, Krentz A. Cardiovascular–Endocrine–Metabolic Medicine: Proposing a New Clinical Sub-Specialty Amid the Cardiometabolic Pandemic. Biomolecules. 2025; 15(3):373. https://doi.org/10.3390/biom15030373
Chicago/Turabian StyleTheodorakis, Nikolaos, Maria Nikolaou, and Andrew Krentz. 2025. "Cardiovascular–Endocrine–Metabolic Medicine: Proposing a New Clinical Sub-Specialty Amid the Cardiometabolic Pandemic" Biomolecules 15, no. 3: 373. https://doi.org/10.3390/biom15030373
APA StyleTheodorakis, N., Nikolaou, M., & Krentz, A. (2025). Cardiovascular–Endocrine–Metabolic Medicine: Proposing a New Clinical Sub-Specialty Amid the Cardiometabolic Pandemic. Biomolecules, 15(3), 373. https://doi.org/10.3390/biom15030373







