Hyaluronic Acid in Topical Applications: The Various Forms and Biological Effects of a Hero Molecule in the Cosmetics Industry
Abstract
1. Introduction
2. Methods
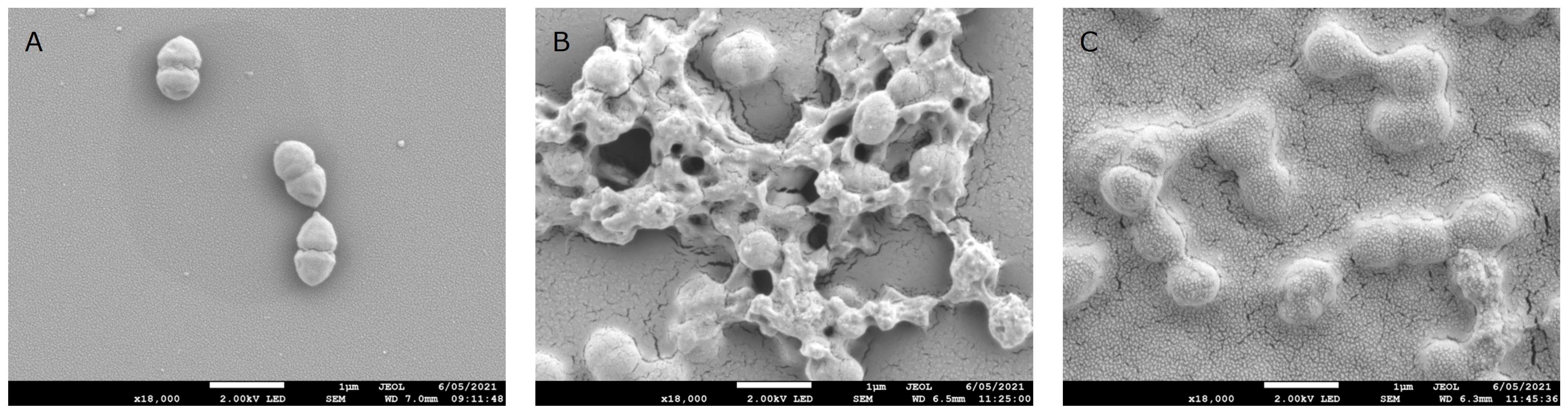
3. Biological Functions of HA in Human Skin
3.1. Structural and Physico-Chemical Properties
3.2. Localization, Synthesis, Degradation, and Cell Surface Receptors
3.3. Roles of HA in Human Skin
3.4. HA in Aging
4. The Different Forms of HA-Based Ingredients, Their Safety, and Interaction with Skin
4.1. The Molecules Behind the Term HA
4.2. Safety of HA in Topical Use
4.3. Interaction of HA with Skin Microbiota
4.4. Skin Penetration
| Reference | HA MW (kDa) | HA Concentration | Dose | Formula | Method | Model | Observation |
|---|---|---|---|---|---|---|---|
| [68] | 3 | 3% | 643 µg/cm2 | Aqueous solution | Raman spectroscopy | Skin explants | HA penetrates up to 60 µm |
| [78] | 400 | 3–13.4 mg.g−1 | 56.3 mg/1.8 cm2 | Water, benzyl alcohol 0.5% (v/v) | HA Radiolabeling, biopsy, imaging | In vivo, forearm | HA is absorbed up to the dermis |
| [83] | 200–325 | 1 mg.mL−1 | 200 µL/1.77 cm2 | Phosphate buffer saline solution (50 mM, pH 4) | Franz diffusion cell | Full-thickness abdominal skin | HA penetrates up to the dermis but only 2–3% of the applied dose enters the skin |
| [79] | 6.5 185 | 2% | - | Aqueous solution | Franz diffusion cell Confocal microscopy of fluorescein-labelled HA | Stratum corneum with epidermis isolated from abdominal skin | Fluorescein-labelled HA permeate the stratum corneum and epidermis, depending on MW |
| [80] | 1000–1400 100–300 20–50 | 1% | 300 µL/0.79 cm2 | Aqueous solution | Raman spectroscopy | Dermatomed skin from abdominal skin | HA 1000–1400 kDa did not permeate skin, HA 20–300 kDa fully permeates the stratum corneum, and 20–50 kDa HA reaches the deeper epidermis |
| [84] | 2.044 | 0.34% | Serum | Quantification of HA released in culture medium | Epidermal barrier model | HA crossed the multilayer of keratinocytes | |
| [85] | 10 | - | 2 mg/cm2 | Cosmetic formula | Matrix-assisted laser desorption/ionization mass spectrometry imaging | Skin explants from abdominoplasty | HA was detected in each skin layer |
| [86] | 2 1000 | 0.1% | - | - | Franz type diffusion cell, Fluorescein labelling, Fluorescence microscopy | Dermatomed abdominal skin in Franz-type cell chamber | 2 kDa fluorescein-labelled HA penetrated up to the dermis while 1000 kDa HA did not pass through the stratum corneum |
| [82] | 1000–1400 20–50 | 0.5% 100–1400 kDa–1% 20–50 kDa | About 112 mg HA in 56 cm2 | Emulsion | Tape stripping and quantification by Elisa assay | Clinical study, forearm | HA diffuse and accumulate in the stratum corneum following repeated application |
| [81] | 10 400–1000 | 2 mg.mL−1 | 200 µL | Aqueous solution | Rhenium-tricarbonyl labeling, infrared microscopy, and fluorescence imaging | Skin biopsies in Franz cell chamber | After 24 h, the rhenium-tricarbonyl-labelled 10 kDa HA is homogeneously distributed in the stratum corneum with very weak amount detected in the viable epidermis |
5. Beneficial Effects of Topical HA in Skin: Clinical Efficacy and Mechanisms
5.1. Native and Hydrolysed HA
| Application | Reference | HA (Type, Trade Name, Molecular Weight) | Study Parameters (Cohort Size, Age Range, Body Site, Placebo Availability, Formula) | Findings |
|---|---|---|---|---|
| Anti-Aging | [99] | Hydrolyzed sodium hyaluronate HAbooster™ 2 kDa | n = 21 (41–60 years), face, placebo controlled, HA 0.1% in lotion | Reduction in facial pigmented spots, eyebag sagging, and pore volume. |
| [86] | Hydrolyzed sodium hyaluronate HAbooster™ 2 kDa | n = 8 (26–39 years), forearm and face, placebo controlled, HA 0.1% in lotion | Increase in dermal collagen score, skin elasticity, and water content. Reduction of sagging and crow’s feet/nasolabial wrinkle depth. | |
| [100] | Sodium hyaluronate PrincipHyal® | n = 75 (average age 55.8 years), face, placebo controlled, HA 0.5% in cream | Formula well tolerated. Increase in moisturization, elasticity, firmness, and smoothness. Decrease in wrinkle depth. | |
| [101] | Sodium hyaluronate in novel conformation 1200 kDA | n = 22 (average age 52.2 years), face, HA 0.5% in aqueous solution | Increase in skin hydration, elasticity, and density. Reduction in transepidermal water loss, roughness in the eye contour, and facial sagging. | |
| [97] | Sodium hyaluronate 50, 130, 300, 800, 2000 kDa (comparison) | n = 76 (30–60 years), face, placebo controlled, HA 0.1% in cream | All HA increased skin moisture and elasticity. Wrinkle depth was significantly reduced by 130 and 50 kDa. | |
| Moisturization | [91] | HA 5, 8, 42, 360, 920, 1770 kDa (comparison) | n = 3 (20–25 years), arm, HA 0.1% in solution | Hydration level increase with decreasing molecular weight. |
| Dry skin (xerosis) | [98] | 7 kDa 1800 kDa (comparison) | n = 36 (60–80 years), leg, 0.1% 7 kDa HA or 0.1% 1800 kDa in lotion, placebo controlled | Both HA increased skin capacitance with a significantly better effect of the 7 kDa compared to the 1800 kDa. No modification of transepidermal water loss or specified symptom sum score. |
| Seborrheic dermatitis | [102] | LMWHA Bionect Hydrogel | n = 13 (18–75 years), face, HA 0.2% in gel | Excellent tolerability. Reduction in erythema and pruritus. |
| Rosacea | [103] | LMWHA Bionect Hydrogel | n = 14 (18–75 years), face, HA 0.2% in gel | Excellent tolerability. Reduction in papules, erythema and dryness. |
| Application | Reference | HA (Type, Trade Name, Molecular Weight) | Study Parameters (Cohort Size, Age Range, Body Site, Placebo Availability, Formula) | Findings |
|---|---|---|---|---|
| Anti-Aging | [104] | Jalubalance® | n = 91 (average age 43 years), face, HA in cream | Reduction in wrinkles and hyperpigmentation. Improvement in skin elasticity and uniformity. |
| [105] | Sodium hyaluronate | n = 44 (average age 48 years), face, HA in formula with niacinamide n = 30 (35–55 years old), arm, HA in formula with niacinamide, biopsy | Improvement of fine lines, wrinkles, luminosity, smoothness, homogeneity, and plumpness. Biopsies revealed 101 mRNAs and 13 miRNAs differentially expressed compared to untreated skin. Senescence-associated secretory phenotype genes were down-regulated. | |
| [106] | Hydrolyzed HA Primalhyal™ 50 20–50 kDa Vectorized HA Hyalusphere™ PF 1000–1400 kDa | HA 0.5% in formula | Formula well tolerated. Wrinkle depth and length in the periorbital area were significantly reduced. | |
| [107] | Sodium hyaluronate Sodium Hyaluronate crosspolymer | n = 46 (average age 43.6 years), face, HA in serum | Increase in skin hydration. Decrease in wrinkles and erythema. Biopsies showed CD44 increase and improvement of solar elastosis. | |
| [108] | Hydrolyzed HA Sodium hyaluronate | n = 40 (30–65 years), face, HA in serum | Formula had excellent tolerability confirmed by no increase in IL-1a. Improvement in smoothness, plumping, and hydration. Decrease in fine lines and wrinkles. | |
| [109] | Nano HA Hyalogy® Skincare | n = 33 (average age 45.2 years), face, HA formulated in cream, serum, and lotion | Increase in skin moisture and skin elasticity. | |
| [110] | Sodium hyaluronate cross polymer, and blend of 6 HA/sodium hyaluronate/hydrolyzed sodium hyaluronate Fillerina® 1,5, 50, 200, 2000 kDa (mix) | n = 40 (25–55 years), face, placebo controlled, HA incorporated in 5 formula | Lip/cheekbone volume increase, decrease in skin sagging in face/cheekbone contour, decrease in wrinkle volume and depth. | |
| Dermatoses (rosacea, sensitive skin, reactive skin) | [111,112] | Sodium hyaluronate | n = 510 (18–88 years), face, HA in formula (M89 Vichy) | The formula decreased the symptom scores of dryness, burning sensation, itching, and stinging/tingling. The prevalence of subjects with severe clinical signs (erythema, desquamation, irritation) decreased. |
| Dry skin related dermatoses | [113] | Sodium hyaluronate | n = 47 (average age 40.9 years), face, HA in formula (M89 Vichy) | The formula decreased the sensation of burning, itching, and stinging/tingling and improved skin dryness in dermatoses related to compromised barriers. |
| Biological Effect | Ref. | Model | HA Characteristics | Findings |
|---|---|---|---|---|
| Fibroblasts Extracellular matrix | [86] | Full-thickness 3D skin model | 2 kDa | Promotion of collagen-type 1A1 and matrix metalloproteinase 1. |
| [119] | Human dermal fibroblasts | 10 kDa 1600 kDa | HA decreased total protein synthesis; did not modify collagen or HA content. | |
| [117] | Human dermal fibroblasts | 30 kDa | Reduction in matrix metalloproteinase 1 expression. | |
| [115,116] | Normal human dermal fibroblasts | 20–50 kDa | HA modified sphingolipids composition. Several pathways were impacted by HA: proliferation and growth, extracellular matrix reorganization, proteoglycans biosynthesis, mitochondrial activity, cell adhesion, wound healing, immune response. | |
| [120] | Human dermal fibroblasts (2D, 3D) | 900 kDa 2300 kDa | 900 kDa > 2300 kDa HA in stimulating fibroblast proliferation. | |
| [118] | Human dermal fibroblasts | 1700 kDa HA12 fragment of 12 saccharide units HA 880 fragment of 880 saccharide units | Increase in matrix metalloproteinase 1 and 3 gene expression. HA12 enhanced collagen 1 expression and transforming growth factor-β1. HA12 and 1700 kDa stimulated type III collagen and transforming growth factor-β 3. | |
| [121] | Normal human dermal fibroblasts (monolayer and in 3D collagen gel) | 750 kDa 2700 kDa | Independently of the molecular weight, HA modified actin cytoskeleton organization. | |
| Epidermal-dermal junction, epidermal development | [122] | Reconstructed epidermis | 50 kDa 800 kDa (topical) | 50 kDa > 800 kDa in up-regulating the expression of several genes involved in Epidermal-dermal junction (tight junction, claudin, ZO1, ZO2, cadherin…), epidermal differentiation (kallikrein, repetin, keratin), and delaying aging (sirtuin). |
| Barrier function | [123] | Keratinocytes (HaCaT) | <100 kDa >500 kDa | Increase in the protein expression of claudin-3, claudin-4 involved in tight junction formation, and of JAM-A, a junctional adhesion molecule. |
| Epidermal homeostasis | [124] | Epidermis 3D model | LMWHA (topical) | Up-regulation of pro-filaggrin gene expression; increase in filaggrin protein content and caspase 14 activity, suggesting improvement in hydration through natural moisture factor enhancement. |
| Epidermal differentiation | [125] | Normal human epidermal keratinocytes | 0.776 kDa >1200 kDa | Increase in differentiation markers gene and protein expression by both HA. HA4 increased CD44-phosphorylated protein and intracellular calcium concentration. |
| Epidermal differentiation | [126] | Mouse Human | Mix of 1 to 50 kDa (topical) | HA induced keratinocyte proliferation involving CD44 and induced hyperplasia in atrophic human skin. Increase in HA synthase and hyaluronidase expression not mediated by CD44. |
| Epidermal differentiation | [127] | Skin equivalent model | oligosaccharide | Epidermis thickening and promotion of epidermal differentiation. |
| Inflammation | [99] | Normal human epidermal keratinocytes | 2 kDa | Reduction in H2O2-induced gene expression of TNF-α and IL1-β and improvement in cell viability. Autophagy and cell renewal markers increased secretion. |
| Inflammation and barrier function in rosacea | [128] | Normal human keratinocytes and BALB/c mouse model treated with rosacea inducer LL-37 | 0.776 kDa | Decrease in LL-37-induced pro-inflammatory cytokines in keratinocytes. In mice, decrease in inflammatory cell infiltration, interleukin 17A, and kallikrein 5, as well as increase in CD44 and filaggrin expression. |
| UV response | [129] | Keratinocytes (HaCat cells) | 970 kDa | Suppression of UVB-induced pro-inflammatory cytokines and cell viability maintenance |
| [130] | Keratinocytes (HaCat cells, normal human epidermal keratinocytes) | 0.8 kDa 1200 kDa | 0.8 kDa HA decreased UVB-induced interleukin 6 secretion by binding the receptor TLR4. The 1200 kDa also decreased the interleukin 6. | |
| [131] | Skin explants | HA in formula | Prevent the decrease in expression of skin barrier markers and the induction of inflammasome. |
5.2. Functionalized HA
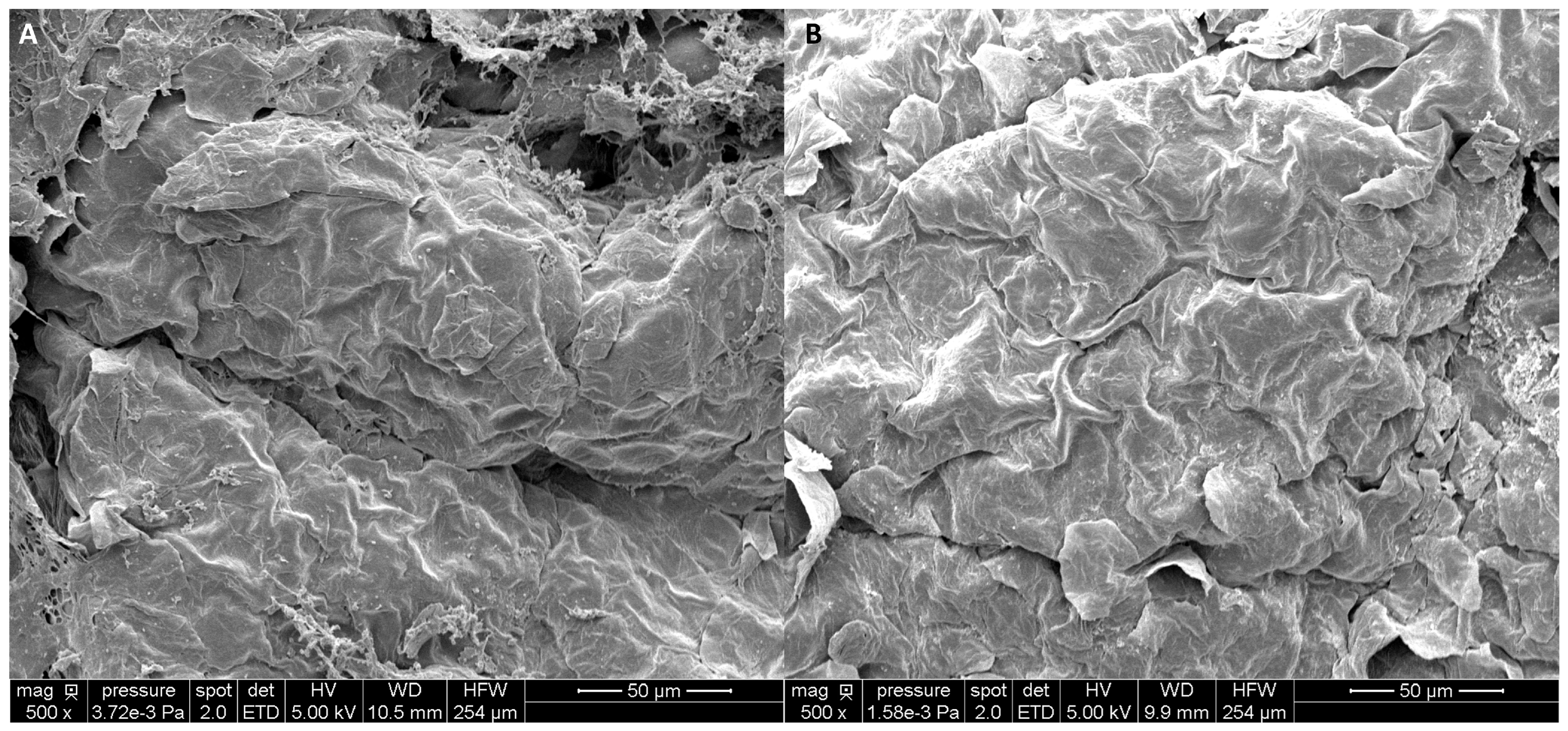
5.3. Enhanced Delivery and Biological Benefits of HMWHA
6. HA in Hair Care
7. Conclusions and Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CD44 | Cluster of differentiation 44 |
| CEMIP | Cell migration-inducing hyaluronidase |
| FDA | Food drug administration |
| HA | Hyaluronic acid |
| HAS | Hyaluronan synthase |
| HMWHA | High-molecular-weight hyaluronic acid |
| HYAL | Hyaluronidase |
| ISO | International standard organization |
| LMWHA | Low-molecular-weight hyaluronic acid |
| LYVE1 | Lymphatic vessel endothelial hyaluronan receptor-1 |
| MMWHA | Medium molecular weight hyaluronic acid |
| P2X7 | Purinergic receptor P2X7 |
| RHAMM | Receptor for hyaluronan-mediated motility |
| SEM | Scanning electron microscopy |
| TLR | Toll-like receptor |
| TMEM2 | Transmembrane protein 2 |
| UV | Ultraviolet |
References
- Meyer, K.; Palmer, J.W. On the Nature of the Ocular Fluids. Am. J. Ophthalmol. 1936, 19, 859–865. [Google Scholar] [CrossRef]
- Laurent, T.C.; Fraser, J.R.E. Hyaluronan. FASEB J. 1992, 6, 2397–2404. [Google Scholar] [CrossRef]
- Wang, S.T.; Neo, B.H.; Betts, R.J. Glycosaminoglycans: Sweet as Sugar Targets for Topical Skin Anti-Aging. Clin. Cosmet. Investig. Dermatol. 2021, 14, 1227–1246. [Google Scholar] [CrossRef] [PubMed]
- Chylińska, N.; Maciejczyk, M. Hyaluronic Acid and Skin: Its Role in Aging and Wound-Healing Processes. Gels 2025, 11, 281. [Google Scholar] [CrossRef] [PubMed]
- Abatangelo, G.; Vindigni, V.; Avruscio, G.; Pandis, L.; Brun, P. Hyaluronic Acid: Redefining Its Role. Cells 2020, 9, 1743. [Google Scholar] [CrossRef]
- Casale, M.; Moffa, A.; Vella, P.; Sabatino, L.; Capuano, F.; Salvinelli, B.; Lopez, M.A.; Carinci, F.; Salvinelli, F. Hyaluronic Acid: Perspectives in Dentistry. A Systematic Review. Int. J. Immunopathol. Pharmacol. 2016, 29, 572–582. [Google Scholar] [CrossRef]
- Yasin, A.; Ren, Y.; Li, J.; Sheng, Y.; Cao, C.; Zhang, K. Advances in Hyaluronic Acid for Biomedical Applications. Front. Bioeng. Biotechnol. 2022, 10, 910290. [Google Scholar] [CrossRef]
- Waggett, S.; Lyles, E.; Schlesinger, T. Update on Low-Molecular Weight Hyaluronic Acid in Dermatology: A Scoping Review. EMJ Dermatol. 2024, 12, 134–146. [Google Scholar] [CrossRef]
- Al-Halaseh, L.K.; Al-Jawabri, N.A.; Tarawneh, S.K.; Al-Qdah, W.K.; Abu-Hajleh, M.N.; Al-Samydai, A.M.; Ahmed, M.A. A Review of the Cosmetic Use and Potentially Therapeutic Importance of Hyaluronic Acid. J. Appl. Pharm. Sci. 2022, 12, 34–41. [Google Scholar] [CrossRef]
- Fallacara, A.; Baldini, E.; Manfredini, S.; Vertuani, S. Hyaluronic Acid in the Third Millennium. Polymers 2018, 10, 701. [Google Scholar] [CrossRef]
- Bravo, B.; Correia, P.; Gonçalves, J.E., Jr.; Sant’Anna, B.; Kerob, D. Benefits of Topical Hyaluronic Acid for Skin Quality and Signs of Skin Aging: From Literature Review to Clinical Evidence. Dermatol. Ther. 2022, 35, e15903. [Google Scholar] [CrossRef]
- Cowman, M.K.; Lee, H.-G.; Schwertfeger, K.L.; McCarthy, J.B.; Turley, E.A. The Content and Size of Hyaluronan in Biological Fluids and Tissues. Front. Immunol. 2015, 6, 261. [Google Scholar] [CrossRef]
- Wu, Y.; Zhao, S.; Wang, J.; Chen, Y.; Li, H.; Li, J.; Kan, Y.; Zhang, T. Methods for Determining the Structure and Physicochemical Properties of Hyaluronic Acid and Its Derivatives: A Review. Int. J. Biol. Macromol. 2024, 282, 137603. [Google Scholar] [CrossRef] [PubMed]
- Grabowski, M.; Gmyrek, D.; Żurawska, M.; Trusek, A. Hyaluronic Acid: Production Strategies, Gel-Forming Properties, and Advances in Drug Delivery Systems. Gels 2025, 11, 424. [Google Scholar] [CrossRef] [PubMed]
- Di Meo, C.; Stellavato, A.; d’Agostino, M.; D’Agostino, A.; Schiraldi, C.; La Gatta, A. Hyaluronan Size and Concentration: Effect on Key Biophysical and Biochemical Features. Int. J. Biol. Macromol. 2024, 282, 137125. [Google Scholar] [CrossRef]
- Meunier, M.; De Tollenaere, M.; Chapuis, E.; Bracq, M.; Lapierre, L.; Tiguemounine, J.; Scandolera, A.; Joset, N.; Reynaud, R. Cationic Hyaluronic Acid Improves Dry Skin Condition and Opens New Use in Rinse-Off Application. JOJ Dermatol. Cosmet. 2025, 6, 555695. [Google Scholar] [CrossRef]
- Evrard, C.; Lambert de Rouvroit, C.; Poumay, Y. Epidermal Hyaluronan in Barrier Alteration-Related Disease. Cells 2021, 10, 3096. [Google Scholar] [CrossRef]
- Tammi, R.; Ripellino, J.A.; Margolis, R.U.; Tammi, M. Localization of Epidermal Hyaluronic Acid Using the Hyaluronate Binding Region of Cartilage Proteoglycan as a Specific Probe. J. Investig. Dermatol. 1988, 90, 412–414. [Google Scholar] [CrossRef]
- Anderegg, U.; Simon, J.C.; Averbeck, M. More than Just a Filler—The Role of Hyaluronan for Skin Homeostasis. Exp. Dermatol. 2014, 23, 295–303. [Google Scholar] [CrossRef]
- Skandalis, S.S.; Karalis, T.; Heldin, P. Intracellular Hyaluronan: Importance for Cellular Functions. Semin. Cancer Biol. 2020, 62, 20–30. [Google Scholar] [CrossRef]
- Žádníková, P.; Šínová, R.; Pavlík, V.; Šimek, M.; Šafránková, B.; Hermannová, M.; Nešporová, K.; Velebný, V. The Degradation of Hyaluronan in the Skin. Biomolecules 2022, 12, 251. [Google Scholar] [CrossRef]
- Muto, J.; Sayama, K.; Gallo, R.L.; Kimata, K. Emerging Evidence for the Essential Role of Hyaluronan in Cutaneous Biology. J. Dermatol. Sci. 2019, 94, 190–195. [Google Scholar] [CrossRef]
- Papakonstantinou, E.; Roth, M.; Karakiulakis, G. Hyaluronic Acid: A Key Molecule in Skin Aging. Derm.-Endocrinol. 2012, 4, 253–258. [Google Scholar] [CrossRef]
- Robert, L. Hyaluronan, a Truly “Youthful” Polysaccharide. Its Medical Applications. Pathol. Biol. 2015, 63, 32–34. [Google Scholar] [CrossRef]
- Choi, J.W.; Kwon, S.H.; Huh, C.H.; Park, K.C.; Youn, S.W. The Influences of Skin Visco-Elasticity, Hydration Level and Aging on the Formation of Wrinkles: A Comprehensive and Objective Approach. Skin. Res. Technol. 2013, 19, e349–e355. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Cai, W.; Shao, X. Regulation of Aquaporin-3 Water Permeability by Hyaluronan. Phys. Chem. Chem. Phys. 2021, 23, 25706–25711. [Google Scholar] [CrossRef] [PubMed]
- Krasiński, R.; Tchórzewski, H.; Lewkowicz, P. Antioxidant Effect of Hyaluronan on Polymorphonuclear Leukocyte-Derived Reactive Oxygen Species Is Dependent on Its Molecular Weight and Concentration and Mainly Involves the Extracellular Space. Postep. Hig. Med. Dosw. 2009, 63, 205–212. [Google Scholar]
- Shukla, P.; Srivastava, P.; Mishra, A. On the Potential Activity of Hyaluronic Acid as an Antimicrobial Agent: Experimental and Computational Validations. Bioprocess. Biosyst. Eng. 2025, 48, 27–42. [Google Scholar] [CrossRef] [PubMed]
- Chmielewski, R.; Lesiak, A. Mitigating Glycation and Oxidative Stress in Aesthetic Medicine: Hyaluronic Acid and Trehalose Synergy for Anti-AGEs Action in Skin Aging Treatment. CCID Clin. Cosmet. Investig. Dermatol. 2024, 17, 2701–2712. [Google Scholar] [CrossRef]
- Litwiniuk, M.; Krejner, A.; Speyrer, M.S.; Gauto, A.R.; Grzela, T. Hyaluronic Acid in Inflammation and Tissue Regeneration. Wounds 2016, 28, 78–88. [Google Scholar]
- Kwon, S.-H.; Park, K.-C. Antioxidants as an Epidermal Stem Cell Activator. Antioxidants 2020, 9, 958. [Google Scholar] [CrossRef]
- Zhang, M.; Shi, D.; Cui, M.; Li, J.; Cheng, W.; Pu, C.; Zhang, J.; Wang, C. Saccharomyces Cerevisiae Fermentation of High Molecular Weight Hyaluronic Acid Enhanced the Antioxidant Capacity in Skin Fibroblasts. Arch. Microbiol. 2025, 207, 66. [Google Scholar] [CrossRef] [PubMed]
- Shang, L.; Li, M.; Xu, A.; Zhuo, F. Recent Applications and Molecular Mechanisms of Hyaluronic Acid in Skin Aging and Wound Healing. Med. Nov. Technol. Devices 2024, 23, 100320. [Google Scholar] [CrossRef]
- Ghazi, K.; Deng-Pichon, U.; Warnet, J.-M.; Rat, P. Hyaluronan Fragments Improve Wound Healing on In Vitro Cutaneous Model through P2X7 Purinoreceptor Basal Activation: Role of Molecular Weight. PLoS ONE 2012, 7, e48351. [Google Scholar] [CrossRef]
- Kawano, Y.; Patrulea, V.; Sublet, E.; Borchard, G.; Iyoda, T.; Kageyama, R.; Morita, A.; Seino, S.; Yoshida, H.; Jordan, O.; et al. Wound Healing Promotion by Hyaluronic Acid: Effect of Molecular Weight on Gene Expression and In Vivo Wound Closure. Pharmaceuticals 2021, 14, 301. [Google Scholar] [CrossRef]
- Quan, T. Molecular Insights of Human Skin Epidermal and Dermal Aging. J. Dermatol. Sci. 2023, 112, 48–53. [Google Scholar] [CrossRef]
- Chin, T.; Lee, X.E.; Ng, P.Y.; Lee, Y.; Dreesen, O. The Role of Cellular Senescence in Skin Aging and Age-Related Skin Pathologies. Front. Physiol. 2023, 14, 1297637. [Google Scholar] [CrossRef] [PubMed]
- Röck, K.; Tigges, J.; Sass, S.; Schütze, A.; Florea, A.-M.; Fender, A.C.; Theis, F.J.; Krutmann, J.; Boege, F.; Fritsche, E.; et al. miR-23a-3p Causes Cellular Senescence by Targeting Hyaluronan Synthase 2: Possible Implication for Skin Aging. J. Investig. Dermatol. 2015, 135, 369–377. [Google Scholar] [CrossRef]
- Šínová, R.; Pavlík, V.; Ondrej, M.; Velebný, V.; Nešporová, K. Hyaluronan: A Key Player or Just a Bystander in Skin Photoaging? Exp. Dermatol. 2022, 31, 442–458. [Google Scholar] [CrossRef]
- Draelos, Z.; Bogdanowicz, P.; Saurat, J.-H. Top Weapons in Skin Aging and Actives to Target the Consequences of Skin Cell Senescence. J. Eur. Acad. Dermatol. Venereol. 2024, 38, 15–22. [Google Scholar] [CrossRef]
- Yoshida, H.; Aoki, M.; Komiya, A.; Endo, Y.; Kawabata, K.; Nakamura, T.; Sakai, S.; Sayo, T.; Okada, Y.; Takahashi, Y. HYBID (Alias KIAA1199/CEMIP) and Hyaluronan Synthase Coordinately Regulate Hyaluronan Metabolism in Histamine-Stimulated Skin Fibroblasts. J. Biol. Chem. 2020, 295, 2483–2494. [Google Scholar] [CrossRef]
- Valcarcel, J.; García, M.R.; Varela, U.R.; Vázquez, J.A. Hyaluronic Acid of Tailored Molecular Weight by Enzymatic and Acid Depolymerization. Int. J. Biol. Macromol. 2020, 145, 788–794. [Google Scholar] [CrossRef]
- Becker, L.C.; Bergfeld, W.F.; Belsito, D.V.; Klaassen, C.D.; Marks, J.G.; Shank, R.C.; Slaga, T.J.; Snyder, P.W.; Cosmetic Ingredient Review Expert Panel; Andersen, F.A. Final Report of the Safety Assessment of Hyaluronic Acid, Potassium Hyaluronate, and Sodium Hyaluronate. Int. J. Toxicol. 2009, 28, 5–67. [Google Scholar] [CrossRef]
- CIR Portal Ingredient Status Report—Starter. Available online: https://cir-reports.cir-safety.org/cir-ingredient-status-report/?id=57efb38d-7d49-ed11-bba2-00224824e39e (accessed on 15 March 2025).
- Salwowska, N.M.; Bebenek, K.A.; Żądło, D.A.; Wcisło-Dziadecka, D.L. Physiochemical Properties and Application of Hyaluronic Acid: A Systematic Review. J. Cosmet. Dermatol. 2016, 15, 520–526. [Google Scholar] [CrossRef] [PubMed]
- Callejas-Quijada, G.; Escobar-Chavez, J.J.; Campos-Lozada, G.; Perez-Marroquin, X.A.; Aguirre-Alvarez, G. Hyaluronic Acid—Extraction Methods, Sources and Applications. Polymers 2023, 15, 3473. [Google Scholar] [CrossRef] [PubMed]
- Shiedlin, A.; Bigelow, R.; Christopher, W.; Arbabi, S.; Yang, L.; Maier, R.V.; Wainwright, N.; Childs, A.; Miller, R.J. Evaluation of Hyaluronan from Different Sources: Streptococcus Zooepidemicus, Rooster Comb, Bovine Vitreous, and Human Umbilical Cord. Biomacromolecules 2004, 5, 2122–2127. [Google Scholar] [CrossRef]
- Dong, Y.; Arif, A.; Olsson, M.; Cali, V.; Hardman, B.; Dosanjh, M.; Lauer, M.; Midura, R.J.; Hascall, V.C.; Brown, K.L.; et al. Endotoxin Free Hyaluronan and Hyaluronan Fragments Do Not Stimulate TNF-α, Interleukin-12 or Upregulate Co-Stimulatory Molecules in Dendritic Cells or Macrophages. Sci. Rep. 2016, 6, 36928. [Google Scholar] [CrossRef]
- Kass, E.H.; Seastone, C.V. The Role of the Mucoid Polysaccharide (Hyaluronic Acid) in the Virulence of Group A Hemolytic Streptococci. J. Exp. Med. 1944, 79, 319–330. [Google Scholar] [CrossRef]
- Akasaka, H.; Komasaki, H.; Arai, T. Fermentation Method for Producing Hyaluronic Acid. U.S. Patent 4,801,539A, 9 May 1989. [Google Scholar]
- Serra, M.; Casas, A.; Toubarro, D.; Barros, A.N.; Teixeira, J.A. Microbial Hyaluronic Acid Production: A Review. Molecules 2023, 28, 2084. [Google Scholar] [CrossRef] [PubMed]
- Ucm, R.; Aem, M.; Lhb, Z.; Kumar, V.; Taherzadeh, M.J.; Garlapati, V.K.; Chandel, A.K. Comprehensive Review on Biotechnological Production of Hyaluronic Acid: Status, Innovation, Market and Applications. Bioengineered 2022, 13, 9645–9661. [Google Scholar] [CrossRef]
- Qiu, Y.; Ma, Y.; Huang, Y.; Li, S.; Xu, H.; Su, E. Current Advances in the Biosynthesis of Hyaluronic Acid with Variable Molecular Weights. Carbohydr. Polym. 2021, 269, 118320. [Google Scholar] [CrossRef]
- Marcellin, E.; Steen, J.A.; Nielsen, L.K. Insight into Hyaluronic Acid Molecular Weight Control. Appl. Microbiol. Biotechnol. 2014, 98, 6947–6956. [Google Scholar] [CrossRef]
- Meunier, M.; Scandolera, A.; Chapuis, E.; Lapierre, L.; Sandré, J.; Brunner, G.; Lovchik, M.; Reynaud, R. The Anti-Wrinkles Properties of Sodium Acetylated Hyaluronate. J. Cosmet. Dermatol. 2022, 21, 2749–2762. [Google Scholar] [CrossRef]
- Sundaram, H.; Cegielska, A.; Wojciechowska, A.; Delobel, P. Prospective, Randomized, Investigator-Blinded, Split-Face Evaluation of a Topical Crosslinked Hyaluronic Acid Serum for Post-Procedural Improvement of Skin Quality and Biomechanical Attributes. J. Drugs Dermatol. 2018, 17, 442–450. [Google Scholar]
- Zhang, M.; Dong, Q.; Yang, K.; Chen, R.; Zhang, J.; Xiao, P.; Zhou, Y. Hyaluronic Acid Hydrogels with Excellent Self-Healing Capacity and Photo-Enhanced Mechanical Properties for Wound Healing. Int. J. Biol. Macromol. 2024, 267, 131235. [Google Scholar] [CrossRef]
- Gui, H.; Liu, H.; Cai, Y.; Nian, J.; Liu, L.; Song, Y.; Kye, S.; Zuo, S.; Yao, C. Hyaluronic Acid-Grafted Titanium Dioxide Nanoparticles for Moisture-Retentive and Non-Cytotoxic Sunscreen Creams. Int. J. Biol. Macromol. 2025, 311, 143957. [Google Scholar] [CrossRef] [PubMed]
- Huerta-Ángeles, G.; Brandejsová, M.; Štěpán, P.; Pavlík, V.; Starigazdová, J.; Orzol, P.; Kopecká, K.; Halamková, P.; Kulhánek, J.; Velebný, V. Retinoic Acid Grafted to Hyaluronan for Skin Delivery: Synthesis, Stability Studies, and Biological Evaluation. Carbohydr. Polym. 2020, 231, 115733. [Google Scholar] [CrossRef]
- Hintze, V.; Schnabelrauch, M.; Rother, S. Chemical Modification of Hyaluronan and Their Biomedical Applications. Front. Chem. 2022, 10, 830671. [Google Scholar] [CrossRef] [PubMed]
- Juncan, A.M.; Moisă, D.G.; Santini, A.; Morgovan, C.; Rus, L.-L.; Vonica-Țincu, A.L.; Loghin, F. Advantages of Hyaluronic Acid and Its Combination with Other Bioactive Ingredients in Cosmeceuticals. Molecules 2021, 26, 4429. [Google Scholar] [CrossRef] [PubMed]
- Bukhari, S.N.A.; Roswandi, N.L.; Waqas, M.; Habib, H.; Hussain, F.; Khan, S.; Sohail, M.; Ramli, N.A.; Thu, H.E.; Hussain, Z. Hyaluronic Acid, a Promising Skin Rejuvenating Biomedicine: A Review of Recent Updates and Pre-Clinical and Clinical Investigations on Cosmetic and Nutricosmetic Effects. Int. J. Biol. Macromol. 2018, 120, 1682–1695. [Google Scholar] [CrossRef]
- Allen, J.; Dodou, K. Current Knowledge and Regulatory Framework on the Use of Hyaluronic Acid for Aesthetic Injectable Skin Rejuvenation Treatments. Cosmetics 2024, 11, 54. [Google Scholar] [CrossRef]
- Miller, L.E.; Bhattacharyya, S.; Parrish, W.R.; Fredericson, M.; Bisson, B.; Altman, R.D. Safety of Intra-Articular Hyaluronic Acid for Knee Osteoarthritis: Systematic Review and Meta-Analysis of Randomized Trials Involving More than 8,000 Patients. Cartilage 2021, 13, 351S–363S. [Google Scholar] [CrossRef]
- Iaconisi, G.N.; Lunetti, P.; Gallo, N.; Cappello, A.R.; Fiermonte, G.; Dolce, V.; Capobianco, L. Hyaluronic Acid: A Powerful Biomolecule with Wide-Ranging Applications-A Comprehensive Review. Int. J. Mol. Sci. 2023, 24, 10296. [Google Scholar] [CrossRef]
- Cassuto, D.; Delledonne, M.; Zaccaria, G.; Illiano, I.; Giori, A.M.; Bellia, G. Safety Assessment of High- and Low-Molecular-Weight Hyaluronans (Profhilo®) as Derived from Worldwide Postmarketing Data. Biomed. Res. Int. 2020, 2020, 8159047. [Google Scholar] [CrossRef] [PubMed]
- EC No. 1223/2009; Regulation (EC) of the European Parliament and of the Council of 30 November 2009 on Cosmetic Products (Recast) (Text with EEA Relevance). European Union: Brussels, Belgium, 2025.
- Corriou, A. P07-12 Toxicological Evaluation and Skin Acceptability of a Very Low Molecular Weight Hyaluronic Acid (LMW-HA) for Cosmetic Applications. Toxicol. Lett. 2025, 411, S103–S104. [Google Scholar] [CrossRef]
- Lee, H.J.; Jeong, S.E.; Lee, S.; Kim, S.; Han, H.; Jeon, C.O. Effects of Cosmetics on the Skin Microbiome of Facial Cheeks with Different Hydration Levels. Microbiol. Open 2018, 7, e00557. [Google Scholar] [CrossRef]
- Meunier, M.; Scandolera, A.; Chapuis, E.; Lambert, C.; Jarrin, C.; Robe, P.; Chajra, H.; Auriol, D.; Reynaud, R. From Stem Cells Protection to Skin Microbiota Balance: Orobanche Rapum Extract, a New Natural Strategy. J. Cosmet. Dermatol. 2019, 18, 1140–1154. [Google Scholar] [CrossRef] [PubMed]
- Tollenaere, M.D.; Boira, C.; Chapuis, E.; Lapierre, L.; Jarrin, C.; Robe, P.; Zanchetta, C.; Vilanova, D.; Sennelier-Portet, B.; Martinez, J.; et al. Action of Mangifera Indica Leaf Extract on Acne-Prone Skin through Sebum Harmonization and Targeting C. Acnes. Molecules 2022, 27, 4769. [Google Scholar] [CrossRef]
- Robe, P.; Jarrin, C.; Zanchetta, C.; Dupont, J.; Chapuis, E.; Scandolera, A.; Auriol, D.; Reynaud, R. Rehabilitation of Skin Bacterial Counts to Assess the Short-Term Impact of Ingredients in Topical Applications—Presenting a Culture-Based Viability Score. Cosmetics 2023, 10, 50. [Google Scholar] [CrossRef]
- He, C.; Yue, Y.; Li, R.; Huang, Y.; Shu, L.; Lv, H.; Wang, J.; Zhang, Z. Sodium Hyaluronates Applied in the Face Affects the Diversity of Skin Microbiota in Healthy People. Int. J. Cosmet. Sci. 2023, 45, 373–386. [Google Scholar] [CrossRef]
- Zanchetta, C.; Fleury, M. Unique Active Ingredients Balancing the Skin Microbiome to Solve the Fourth Most Common Skin Issue. Available online: https://sofw.com/en/sofw-journal/articles-en/48-personal-care/3735-unique-active-ingredients-balancing-the-skin-microbiome-to-solve-the-fourth-most-common-skin-issue (accessed on 8 September 2025).
- Zhao, R.; Zhang, C.; Yu, L.; Zhang, C.; Zhao, J.; Narbad, A.; Zhai, Q.; Tian, F. In Vitro Fermentation of Hyaluronan with Different Molecular Weights by Human Gut Microbiota: Differential Effects on Gut Microbiota Structure and Metabolic Function. Polymers 2023, 15, 2103. [Google Scholar] [CrossRef]
- Šimek, M.; Turková, K.; Schwarzer, M.; Nešporová, K.; Kubala, L.; Hermannová, M.; Foglová, T.; Šafránková, B.; Šindelář, M.; Šrůtková, D.; et al. Molecular Weight and Gut Microbiota Determine the Bioavailability of Orally Administered Hyaluronic Acid. Carbohydr. Polym. 2023, 313, 120880. [Google Scholar] [CrossRef]
- Scott, J.E. Secondary Structures in Hyaluronan Solutions: Chemical and Biological Implications. In Ciba Foundation Symposium 143—The Biology of Hyaluronan; Wiley: Hoboken, NJ, USA, 1989; pp. 281–285. [Google Scholar] [CrossRef]
- Brown, T.J.; Alcorn, D.; Fraser, J.R.E. Absorption of Hyaluronan Applied to the Surface of Intact Skin. J. Investig. Dermatol. 1999, 113, 740–746. [Google Scholar] [CrossRef] [PubMed]
- Cilurzo, F.; Vistoli, G.; Gennari, C.G.M.; Selmin, F.; Gardoni, F.; Franzè, S.; Campisi, M.; Minghetti, P. The Role of the Conformational Profile of Polysaccharides on Skin Penetration: The Case of Hyaluronan and Its Sulfates. Chem. Biodivers. 2014, 11, 551–561. [Google Scholar] [CrossRef] [PubMed]
- Essendoubi, M.; Gobinet, C.; Reynaud, R.; Angiboust, J.F.; Manfait, M.; Piot, O. Human Skin Penetration of Hyaluronic Acid of Different Molecular Weights as Probed by Raman Spectroscopy. Skin. Res. Technol. 2016, 22, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Henry, L.; Delsuc, N.; Laugel, C.; Lambert, F.; Sandt, C.; Hostachy, S.; Bernard, A.-S.; Bertrand, H.C.; Grimaud, L.; Baillet-Guffroy, A.; et al. Labeling of Hyaluronic Acids with a Rhenium-Tricarbonyl Tag and Percutaneous Penetration Studied by Multimodal Imaging. Bioconjug Chem. 2018, 29, 987–991. [Google Scholar] [CrossRef]
- Grégoire, S.; Man, P.D.; Maudet, A.; Le Tertre, M.; Hicham, N.; Changey, F.; Gaëlle, B.-S.; Tran, C.; Laurence, V. Hyaluronic Acid Skin Penetration Evaluated by Tape Stripping Using ELISA Kit Assay. J. Pharm. Biomed. Anal. 2023, 224, 115205. [Google Scholar] [CrossRef]
- Chen, M.; Gupta, V.; Anselmo, A.C.; Muraski, J.A.; Mitragotri, S. Topical Delivery of Hyaluronic Acid into Skin Using SPACE-Peptide Carriers. J. Control Release 2014, 173, 67–74. [Google Scholar] [CrossRef]
- Nashchekina, Y.A.; Raydan, M. Noninvasive Penetration of 5 Nm Hyaluronic Acid Molecules across the Epidermal Barrier (in Vitro) and Its Interaction with Human Skin Cells. Skin. Res. Technol. 2018, 24, 129–134. [Google Scholar] [CrossRef]
- Legouffe, R.; Jeanneton, O.; Gaudin, M.; Tomezyk, A.; Gerstenberg, A.; Dumas, M.; Heusèle, C.; Bonnel, D.; Stauber, J.; Schnebert, S. Hyaluronic Acid Detection and Relative Quantification by Mass Spectrometry Imaging in Human Skin Tissues. Anal. Bioanal. Chem. 2022, 414, 5781–5791. [Google Scholar] [CrossRef]
- Abe, Y.; Seino, S.; Kurihara, H.; Kage, M.; Tokudome, Y. 2-kDa Hyaluronan Ameliorates Human Facial Wrinkles through Increased Dermal Collagen Density Related to Promotion of Collagen Remodeling. J. Cosmet. Dermatol. 2023, 22, 320–327. [Google Scholar] [CrossRef]
- Kozaka, S.; Kashima, A.; Wakabayashi, R.; Nakata, T.; Ueda, T.; Goto, M. Effective Transcutaneous Delivery of Hyaluronic Acid Using an Easy-to-Prepare Reverse Micelle Formulation. Cosmetics 2020, 7, 52. [Google Scholar] [CrossRef]
- Witting, M.; Boreham, A.; Brodwolf, R.; Vávrová, K.; Alexiev, U.; Friess, W.; Hedtrich, S. Interactions of Hyaluronic Acid with the Skin and Implications for the Dermal Delivery of Biomacromolecules. Mol. Pharm. 2015, 12, 1391–1401. [Google Scholar] [CrossRef]
- Knorr, F.; Lademann, J.; Patzelt, A.; Sterry, W.; Blume-Peytavi, U.; Vogt, A. Follicular Transport Route--Research Progress and Future Perspectives. Eur. J. Pharm. Biopharm. 2009, 71, 173–180. [Google Scholar] [CrossRef]
- De Tollenaere, M.; Meunier, M.; Lapierre, L.; Chapuis, E.; Guilleret, A.; Harrison, I.; Jean, T.; Rannou, A.; Scandolera, A.; Reynaud, R. High Molecular Weight Hyaluronic Acid Vectorised with Clay Provides Long-Term Hydration and Reduces Skin Brightness. Skin. Res. Technol. 2024, 30, e13672. [Google Scholar] [CrossRef] [PubMed]
- Ni, C.; Zhang, Z.; Wang, Y.; Zhang, Z.; Guo, X.; Lv, H. Hyaluronic Acid and HA-Modified Cationic Liposomes for Promoting Skin Penetration and Retention. J. Control. Release 2023, 357, 432–443. [Google Scholar] [CrossRef]
- Nakamura, M.; Hikida, M.; Nakano, T.; Ito, S.; Hamano, T.; Kinoshita, S. Characterization of Water Retentive Properties of Hyaluronan. Cornea 1993, 12, 433–436. [Google Scholar] [CrossRef] [PubMed]
- Snetkov, P.; Zakharova, K.; Morozkina, S.; Olekhnovich, R.; Uspenskaya, M. Hyaluronic Acid: The Influence of Molecular Weight on Structural, Physical, Physico-Chemical, and Degradable Properties of Biopolymer. Polymers 2020, 12, 1800. [Google Scholar] [CrossRef] [PubMed]
- Jouon, N.; Rinaudo, M.; Milas, M.; Desbrières, J. Hydration of Hyaluronic Acid as a Function of the Counterion Type and Relative Humidity. Carbohydr. Polym. 1995, 26, 69–73. [Google Scholar] [CrossRef]
- Průšová, A.; Šmejkalová, D.; Chytil, M.; Velebný, V.; Kučerík, J. An Alternative DSC Approach to Study Hydration of Hyaluronan. Carbohydr. Polym. 2010, 82, 498–503. [Google Scholar] [CrossRef]
- Kučerík, J.; Průšová, A.; Rotaru, A.; Flimel, K.; Janeček, J.; Conte, P. DSC Study on Hyaluronan Drying and Hydration. Thermochim. Acta 2011, 523, 245–249. [Google Scholar] [CrossRef]
- Pavicic, T.; Gauglitz, G.G.; Lersch, P.; Schwach-Abdellaoui, K.; Malle, B.; Korting, H.C.; Farwick, M. Efficacy of Cream-Based Novel Formulations of Hyaluronic Acid of Different Molecular Weights in Anti-Wrinkle Treatment. J. Drugs Dermatol. 2011, 10, 990–1000. [Google Scholar] [PubMed]
- Muhammad, P.; Novianto, E.; Setyorini, M.; Legiawati, L.; Yusharyahya, S.N.; Menaldi, S.L.; Budianti, W.K. Effectiveness of Topical Hyaluronic Acid of Different Molecular Weights in Xerosis Cutis Treatment in Elderly: A Double-Blind, Randomized Controlled Trial. Arch. Dermatol. Res. 2024, 316, 329. [Google Scholar] [CrossRef]
- Ito, S.; Kurihara, H.; Kuriyama, K.; Kimura, M.; Tokudome, Y. 2 kDa Hyaluronic Acid Reduces Blemishes and Sagging in Human Facial Skin. CCID Clin. Cosmet. Investig. Dermatol. 2025, 18, 805–816. [Google Scholar] [CrossRef]
- Carlomagno, F.; Roveda, G.; Michelotti, A.; Ruggeri, F.; Tursi, F. Anti-Skin-Aging Effect of a Treatment with a Cosmetic Product and a Food Supplement Based on a New Hyaluronan: A Randomized Clinical Study in Healthy Women. Cosmetics 2022, 9, 54. [Google Scholar] [CrossRef]
- Nam, G.; Lee, H.W.; Jang, J.; Kim, C.H.; Kim, K.-H. Novel Conformation of Hyaluronic Acid with Improved Cosmetic Efficacy. J. Cosmet. Dermatol. 2023, 22, 1312–1320. [Google Scholar] [CrossRef]
- Schlesinger, T.; Rowland Powell, C. Efficacy and Safety of a Low Molecular Weight Hyaluronic Acid Topical Gel in the Treatment of Facial Seborrheic Dermatitis Final Report. J. Clin. Aesthet. Dermatol. 2014, 7, 15–18. [Google Scholar]
- Schlesinger, T.E.; Powell, C.R. Efficacy and Tolerability of Low Molecular Weight Hyaluronic Acid Sodium Salt 0.2% Cream in Rosacea. J. Drugs Dermatol. 2013, 12, 664–667. [Google Scholar]
- Rigoni, C.; Cantù, A.M.; Annunziata, M.C.; Bordin, C.; Farina, S.; Forgione, P.; Foti, C.; Lorenzi, S.; Negosanti, F.; Praticò, M.; et al. Clinical and Instrumental Evaluation of the Anti-Aging Effectiveness of a Cream Based on Hyaluronic Acid and a Cream Based on Hyaluronic Acid and Vitamin C: A Prospective, Multicenter, 8-Week, Parallel-Group Randomized Study on 91 Subjects. Cosmetics 2025, 12, 177. [Google Scholar] [CrossRef]
- Bogdanowicz, P.; Bensadoun, P.; Noizet, M.; Béganton, B.; Philippe, A.; Alvarez-Georges, S.; Doat, G.; Tourette, A.; Bessou-Touya, S.; Lemaitre, J.-M.; et al. Senomorphic Activity of a Combination of Niacinamide and Hyaluronic Acid: Correlation with Clinical Improvement of Skin Aging. Sci. Rep. 2024, 14, 16321. [Google Scholar] [CrossRef]
- Juncan, A.M.; Morgovan, C.; Rus, L.-L.; Loghin, F. Development and Evaluation of a Novel Anti-Ageing Cream Based on Hyaluronic Acid and Other Innovative Cosmetic Actives. Polymers 2023, 15, 4134. [Google Scholar] [CrossRef] [PubMed]
- Robinson, D.M.; Vega, J.; Palm, M.D.; Bell, M.; Widgerow, A.D.; Giannini, A. Multicenter Evaluation of a Topical Hyaluronic Acid Serum. J. Cosmet Dermatol 2022, 21, 3848–3858. [Google Scholar] [CrossRef]
- Draelos, Z.D.; Diaz, I.; Namkoong, J.; Wu, J.; Boyd, T. Efficacy Evaluation of a Topical Hyaluronic Acid Serum in Facial Photoaging. Dermatol. Ther. 2021, 11, 1385–1394. [Google Scholar] [CrossRef] [PubMed]
- Jegasothy, S.M.; Zabolotniaia, V.; Bielfeldt, S. Efficacy of a New Topical Nano-Hyaluronic Acid in Humans. J. Clin. Aesthet. Dermatol. 2014, 7, 27–29. [Google Scholar] [PubMed]
- Nobile, V.; Buonocore, D.; Michelotti, A.; Marzatico, F. Anti-Aging and Filling Efficacy of Six Types Hyaluronic Acid Based Dermo-Cosmetic Treatment: Double Blind, Randomized Clinical Trial of Efficacy and Safety. J. Cosmet. Dermatol. 2014, 13, 277–287. [Google Scholar] [CrossRef]
- Tan, J.; Spada, J.; Kerscher, M.; Anfilova, M.; Abdulla, S.; Altmeyer, A.; Delva, C.; Kerob, D.; Araviiskaia, E. 26268 M89, a Combination of 89% of Vichy Volcanic Mineralizing Water and Hyaluronic Acid Improves Signs and Symptoms of Subjects with Rosacea/Sensitive/Reactive Skin: Results from an Open-Label, Observational, International Study. J. Am. Acad. Dermatol. 2021, 85, AB93. [Google Scholar] [CrossRef]
- Tan, J.; Spada, J.; Orlandi, C.; Kerscher, M.; Anfilova, M.; Abdulla, S.; Floriánová, A.; Preisz, K.; Altmayer, A.; Delva, C.; et al. Vichy Mineralizing Water with Hyaluronic Acid Is Effective and Well Tolerated as an Adjunct to the Management of Various Dermatoses and after Esthetic Procedures. J. Cosmet. Dermatol. 2020, 19, 682–688. [Google Scholar] [CrossRef]
- Hong, C.-H.; Schachter, J.; Sutton, A.B.; Salsberg, J.M.; Li, M.K.; Humphrey, S.D.; Dayeh, N.R. 89% Vichy Mineralizing Water with Hyaluronic Acid Is a Well-Tolerated Adjunct Treatment That Helps Restore Skin Barrier Function in Dry Skin-Related Inflammatory Dermatoses and Post-Procedure Skin Care: A Canadian Study. J. Cosmet. Dermatol. 2021, 20, 2148–2155. [Google Scholar] [CrossRef]
- Endo, Y.; Yoshida, H.; Akazawa, Y.; Yamazaki, K.; Ota, Y.; Sayo, T.; Takahashi, Y. Antiwrinkle Efficacy of 1-Ethyl-β-N-Acetylglucosaminide, an Inducer of Epidermal Hyaluronan Production. Skin. Res. Technol. 2022, 28, 58–65. [Google Scholar] [CrossRef]
- Radrezza, S.; Aiello, G.; Baron, G.; Aldini, G.; Carini, M.; D’Amato, A. Integratomics of Human Dermal Fibroblasts Treated with Low Molecular Weight Hyaluronic Acid. Molecules 2021, 26, 5096. [Google Scholar] [CrossRef]
- Radrezza, S.; Baron, G.; Nukala, S.B.; Depta, G.; Aldini, G.; Carini, M.; D’Amato, A. Advanced Quantitative Proteomics to Evaluate Molecular Effects of Low-Molecular-Weight Hyaluronic Acid in Human Dermal Fibroblasts. J. Pharm. Biomed. Anal. 2020, 185, 113199. [Google Scholar] [CrossRef]
- Chen, F.; Guo, X.; Wu, Y. Skin Antiaging Effects of a Multiple Mechanisms Hyaluronan Complex. Skin. Res. Technol. 2023, 29, e13350. [Google Scholar] [CrossRef]
- David-Raoudi, M.; Tranchepain, F.; Deschrevel, B.; Vincent, J.-C.; Bogdanowicz, P.; Boumediene, K.; Pujol, J.-P. Differential Effects of Hyaluronan and Its Fragments on Fibroblasts: Relation to Wound Healing. Wound Repair. Regen. 2008, 16, 274–287. [Google Scholar] [CrossRef]
- Croce, M.A.; Dyne, K.; Boraldi, F.; Quaglino, D.; Cetta, G.; Tiozzo, R.; Pasquali Ronchetti, I. Hyaluronan Affects Protein and Collagen Synthesis by in Vitro Human Skin Fibroblasts. Tissue Cell 2001, 33, 326–331. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Gu, H.; Burd, A. A Reappraisal of the Biological Effects of Hyaluronan on Human Dermal Fibroblast. J. Biomed. Mater. Res. A 2009, 90A, 1177–1185. [Google Scholar] [CrossRef]
- Boraldi, F.; Croce, M.A.; Quaglino, D.; Sammarco, R.; Carnevali, E.; Tiozzo, R.; Pasquali-Ronchetti, I. Cell–Matrix Interactions of in Vitro Human Skin Fibroblasts upon Addition of Hyaluronan. Tissue Cell 2003, 35, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Farwick, M.; Gauglitz, G.; Pavicic, T.; Köhler, T.; Wegmann, M.; Schwach-Abdellaoui, K.; Malle, B.; Tarabin, V.; Schmitz, G.; Korting, H.C. Fifty-kDa Hyaluronic Acid Upregulates Some Epidermal Genes without Changing TNF-α Expression in Reconstituted Epidermis. Skin. Pharmacol. Physiol. 2011, 24, 210–217. [Google Scholar] [CrossRef]
- Park, H.-Y.; Kweon, D.-K.; Kim, J.-K. Upregulation of Tight Junction-Related Proteins by Hyaluronic Acid in Human HaCaT Keratinocytes. Bioact. Carbohydr. Diet. Fibre 2023, 30, 100374. [Google Scholar] [CrossRef]
- Hashimoto, M.; Maeda, K. New Functions of Low-Molecular-Weight Hyaluronic Acid on Epidermis Filaggrin Production and Degradation. Cosmetics 2021, 8, 118. [Google Scholar] [CrossRef]
- Kage, M.; Tokudome, Y.; Matsunaga, Y.; Hariya, T.; Hashimoto, F. Effect of hyaluronan tetrasaccharides on epidermal differentiation in normal human epidermal keratinocytes. Int. J. Cosmet. Sci. 2014, 36, 109–115. [Google Scholar] [CrossRef]
- Kaya, G.; Tran, C.; Sorg, O.; Hotz, R.; Grand, D.; Carraux, P.; Didierjean, L.; Stamenkovic, I.; Saurat, J.-H. Hyaluronate Fragments Reverse Skin Atrophy by a CD44-Dependent Mechanism. PLoS Med. 2006, 3, e493. [Google Scholar] [CrossRef]
- Choi, H.-R.; Kang, Y.-A.; Na, J.-I.; Huh, S.Y.; Huh, C.-H.; Kim, K.H.; Park, K.-C. Oligosaccharides of Hyaluronic Acid Increased Epidermal Cell Stemness by Modulation of Integrin Expression. J. Cosmet. Dermatol. 2012, 11, 290–296. [Google Scholar] [CrossRef]
- Lee, S.G.; Yoon, M.S.; Kim, D.H.; Shin, J.U.; Lee, H.J. Hyaluronan Oligosaccharides Improve Rosacea-Like Phenotype through Anti-Inflammatory and Epidermal Barrier-Improving Effects. Ann. Dermatol. 2020, 32, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Hašová, M.; Crhák, T.; Šafránková, B.; Dvořáková, J.; Muthný, T.; Velebný, V.; Kubala, L. Hyaluronan Minimizes Effects of UV Irradiation on Human Keratinocytes. Arch. Dermatol. Res. 2011, 303, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Hu, L.; Nomura, S.; Sato, Y.; Takagi, K.; Ishii, T.; Honma, Y.; Watanabe, K.; Mizukami, Y.; Muto, J. Anti-Inflammatory Effects of Differential Molecular Weight Hyaluronic Acids on UVB-Induced Calprotectin-Mediated Keratinocyte Inflammation. J. Dermatol. Sci. 2022, 107, 24–31. [Google Scholar] [CrossRef]
- Benedusi, M.; Kerob, D.; Guiotto, A.; Cervellati, F.; Ferrara, F.; Pambianchi, E. Topical Application of M89PF Containing Vichy Mineralising Water and Probiotic Fractions Prevents Cutaneous Damage Induced by Exposure to UV and O3. Clin. Cosmet. Investig. Dermatol. 2023, 16, 1769–1776. [Google Scholar] [CrossRef]
- Malaisse, J.; Pendaries, V.; Hontoir, F.; Glas, V.D.; Vlaender, D.V.; Simon, M.; de Rouvroit, C.L.; Poumay, Y.; Flamion, B. Hyaluronan Does Not Regulate Human Epidermal Keratinocyte Proliferation and Differentiation *. J. Biol. Chem. 2016, 291, 6347–6358. [Google Scholar] [CrossRef]
- Endo, Y.; Yoshida, H.; Ota, Y.; Akazawa, Y.; Sayo, T.; Hanai, U.; Imagawa, K.; Sasaki, M.; Takahashi, Y. Accelerated Human Epidermal Turnover Driven by Increased Hyaluronan Production. J. Dermatol. Sci. 2021, 101, 123–133. [Google Scholar] [CrossRef]
- Choi, E.H. Aging of the Skin Barrier. Clin. Dermatol. 2019, 37, 336–345. [Google Scholar] [CrossRef] [PubMed]
- Biniek, K.; Levi, K.; Dauskardt, R.H. Solar UV Radiation Reduces the Barrier Function of Human Skin. Proc. Natl. Acad. Sci. USA 2012, 109, 17111–17116. [Google Scholar] [CrossRef]
- Vistejnova, L.; Safrankova, B.; Nesporova, K.; Slavkovsky, R.; Hermannova, M.; Hosek, P.; Velebny, V.; Kubala, L. Low Molecular Weight Hyaluronan Mediated CD44 Dependent Induction of IL-6 and Chemokines in Human Dermal Fibroblasts Potentiates Innate Immune Response. Cytokine 2014, 70, 97–103. [Google Scholar] [CrossRef]
- D’Agostino, A.; Stellavato, A.; Corsuto, L.; Diana, P.; Filosa, R.; La Gatta, A.; De Rosa, M.; Schiraldi, C. Is Molecular Size a Discriminating Factor in Hyaluronan Interaction with Human Cells? Carbohydr. Polym. 2017, 157, 21–30. [Google Scholar] [CrossRef] [PubMed]
- Han, W.; Lv, Y.; Sun, Y.; Wang, Y.; Zhao, Z.; Shi, C.; Chen, X.; Wang, L.; Zhang, M.; Wei, B.; et al. The Anti-Inflammatory Activity of Specific-Sized Hyaluronic Acid Oligosaccharides. Carbohydr. Polym. 2022, 276, 118699. [Google Scholar] [CrossRef] [PubMed]
- Antoszewska, M.; Sokolewicz, E.M.; Barańska-Rybak, W. Wide Use of Hyaluronic Acid in the Process of Wound Healing—A Rapid Review. Sci. Pharm. 2024, 92, 23. [Google Scholar] [CrossRef]
- Saturnino, C.; Sinicropi, M.S.; Parisi, O.I.; Iacopetta, D.; Popolo, A.; Marzocco, S.; Autore, G.; Caruso, A.; Cappello, A.R.; Longo, P.; et al. Acetylated Hyaluronic Acid: Enhanced Bioavailability and Biological Studies. Biomed. Res. Int. 2014, 2014, 921549. [Google Scholar] [CrossRef] [PubMed]
- Ha, N.G.; Lee, S.H.; Lee, E.H.; Chang, M.; Yoo, J.; Lee, W.J. Safety and Efficacy of a New Hydrogel Based on Hyaluronic Acid as Cosmeceutical for Xerosis. J. Cosmet. Dermatol. 2022, 21, 6840–6849. [Google Scholar] [CrossRef]
- Galvan, A.; Lacavalla, M.A.; Boschi, F.; Cisterna, B.; Dalla Pozza, E.; Vigato, E.; Carton, F.; Malatesta, M.; Calderan, L. A Fluid Dynamic In Vitro System to Study the Effect of Hyaluronic Acid Administration on Collagen Organization in Human Skin Explants. Int. J. Mol. Sci. 2025, 26, 5397. [Google Scholar] [CrossRef]
- Sundaram, H.; Mackiewicz, N.; Burton, E.; Peno-Mazzarino, L.; Lati, E.; Meunier, S. Pilot Comparative Study of the Topical Action of a Novel, Crosslinked Resilient Hyaluronic Acid on Skin Hydration and Barrier Function in a Dynamic, Three-Dimensional Human Explant Model. J. Drugs Dermatol. 2016, 15, 434–441. [Google Scholar]
- Cheong, K.-L.; Chen, Q.; Aweya, J.J.; Ji, X.L.; Zhong, S.; Tan, K. Trends in Polysaccharide-Based Hydrogels for Skin Anti-Aging and Skin Antioxidant. Int. J. Biol. Macromol. 2025, 319, 145366. [Google Scholar] [CrossRef]
- Baspinar, Y.; Borchert, H.-H. Penetration and Release Studies of Positively and Negatively Charged Nanoemulsions--Is There a Benefit of the Positive Charge? Int. J. Pharm. 2012, 430, 247–252. [Google Scholar] [CrossRef]
- Blanc Catala, J.; Zanchetta, C.; François, C.; Chapuis, E.; Joset, N.; Meunier, M.; Loeser, F.; Godbille, S.; Scandolera, A.; Reynaud, R.; et al. Evaluation of the Hydrating Benefits of a Cationic Hyaluronic Acid: From Biological Evaluation to Consumer Home Use Trial. Int. J. Cosmet. Sci. 2024, 46, 795–805. [Google Scholar] [CrossRef]
- Starace, M.; Granger, C.; Carpanese, M.A.; Alessandrini, A.; Bruni, F.; Piraccini, B.M. Review of the Literature on the Efficacy and Safety of a New Cosmetic Topical Treatment Containing Pistacia Lentiscus and Hyaluronic Acid for the Treatment of Nail Plate Damages. J. Cosmet. Dermatol. 2022, 21, 5514–5518. [Google Scholar] [CrossRef] [PubMed]
- Pavlík, V.; Machalová, V.; Čepa, M.; Šínová, R.; Šafránková, B.; Kulhánek, J.; Drmota, T.; Kubala, L.; Huerta-Ángeles, G.; Velebný, V.; et al. Retinoic Acid Grafted to Hyaluronic Acid Activates Retinoid Gene Expression and Removes Cholesterol from Cellular Membranes. Biomolecules 2022, 12, 200. [Google Scholar] [CrossRef]
- Jiang, F.-R.; Wang, S.; Han, D.; Wei, J.; Wu, Y.-N.; Liu, Z. Glutamic-Acid Grafted Hyaluronic Acid Inhibits Inflammatory Factors via Fibroblast and Skin Model Tests. Skin. Res. Technol. 2024, 30, e13548. [Google Scholar] [CrossRef] [PubMed]
- Fujii, M.Y.; Okishima, A.; Ichiwata, H.S.; Oka, T. Biocompatible Topical Delivery System of High-Molecular-Weight Hyaluronan into Human Stratum Corneum Using Magnesium Chloride. Sci. Rep. 2023, 13, 10782. [Google Scholar] [CrossRef]
- Shigefuji, M.; Tokudome, Y. Nanoparticulation of Hyaluronic Acid: A New Skin Penetration Enhancing Polyion Complex Formulation: Mechanism and Future Potential. Materialia 2020, 14, 100879. [Google Scholar] [CrossRef]
- Xing, H.; Pan, X.; Hu, Y.; Yang, Y.; Zhao, Z.; Peng, H.; Wang, J.; Li, S.; Hu, Y.; Li, G.; et al. High Molecular Weight Hyaluronic Acid-Liposome Delivery System for Efficient Transdermal Treatment of Acute and Chronic Skin Photodamage. Acta Biomater. 2024, 182, 171–187. [Google Scholar] [CrossRef] [PubMed]
- Pavlichko, J.P.; Goddard, E.D.; Band, P.A.; Leschiner, A. Enhanced Substantivity of Hyaluronic Acid on Keratin Substrates via Polymer Complexation. Int. J. Cosmet. Sci. 1994, 16, 227–234. [Google Scholar] [CrossRef]
- Sionkowska, A.; Kaczmarek, B.; Michalska, M.; Lewandowska, K.; Grabska, S. Preparation and Characterization of Collagen/Chitosan/Hyaluronic Acid Thin Films for Application in Hair Care Cosmetics. Pure Appl. Chem. 2017, 89, 1829–1839. [Google Scholar] [CrossRef]
- Cruz, C.F.; Martins, M.; Egipto, J.; Osório, H.; Ribeiro, A.; Cavaco-Paulo, A. Changing the Shape of Hair with Keratin Peptides. RSC Adv. 2017, 7, 51581–51592. [Google Scholar] [CrossRef]
- Essendoubi, M.; Meunier, M.; Scandolera, A.; Gobinet, C.; Manfait, M.; Lambert, C.; Auriol, D.; Reynaud, R.; Piot, O. Conformation Changes in Human Hair Keratin Observed Using Confocal Raman Spectroscopy after Active Ingredient Application. Int. J. Cosmet. Sci. 2019, 41, 203–212. [Google Scholar] [CrossRef]
- Qu, W.; Guo, X.; Xu, G.; Zou, S.; Wu, Y.; Hu, C.; Chang, K.; Wang, J. Improving the Mechanical Properties of Damaged Hair Using Low-Molecular Weight Hyaluronate. Molecules 2022, 27, 7701. [Google Scholar] [CrossRef]
- Boira, C.; Essendoubi, M.; Meunier, M.; Lambert, C.; Auriol, D.; Manfait, M.; Piot, O.; Scandolera, A.; Reynaud, R. Hyaluronic Acid: Elucidating Its Penetration into, and Effect on Hair Fibers Using Confocal Raman Spectroscopy and Biometric Techniques. J. Phys. Chem. Biophys. 2024, 14, 1000373. [Google Scholar] [CrossRef]
- Zerbinati, N.; Sommatis, S.; Maccario, C.; Capillo, M.C.; Di Francesco, S.; Rauso, R.; Protasoni, M.; D’Este, E.; Gasperina, D.D.; Mocchi, R. In Vitro Hair Growth Promoting Effect of a Noncrosslinked Hyaluronic Acid in Human Dermal Papilla Cells. Biomed. Res. Int. 2021, 2021, 5598110. [Google Scholar] [CrossRef] [PubMed]
- Lourenço, C.B.; Fava, A.L.M.; dos Santos, É.M.; de Macedo, L.M.; Tundisi, L.L.; Ataide, J.A.; Mazzola, P.G. Brief Descriptions of the Principles of Prominent Methods Used to Study the Penetration of Materials into Human Hair and a Review of Examples of Their Use. Int. J. Cosmet. Sci. 2021, 43, 113–122. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zanchetta, C.; Scandolera, A.; Reynaud, R. Hyaluronic Acid in Topical Applications: The Various Forms and Biological Effects of a Hero Molecule in the Cosmetics Industry. Biomolecules 2025, 15, 1656. https://doi.org/10.3390/biom15121656
Zanchetta C, Scandolera A, Reynaud R. Hyaluronic Acid in Topical Applications: The Various Forms and Biological Effects of a Hero Molecule in the Cosmetics Industry. Biomolecules. 2025; 15(12):1656. https://doi.org/10.3390/biom15121656
Chicago/Turabian StyleZanchetta, Catherine, Amandine Scandolera, and Romain Reynaud. 2025. "Hyaluronic Acid in Topical Applications: The Various Forms and Biological Effects of a Hero Molecule in the Cosmetics Industry" Biomolecules 15, no. 12: 1656. https://doi.org/10.3390/biom15121656
APA StyleZanchetta, C., Scandolera, A., & Reynaud, R. (2025). Hyaluronic Acid in Topical Applications: The Various Forms and Biological Effects of a Hero Molecule in the Cosmetics Industry. Biomolecules, 15(12), 1656. https://doi.org/10.3390/biom15121656







