Serum Neuron-Specific Enolase as a Biomarker of Neonatal Brain Injury—New Perspectives for the Identification of Preterm Neonates at High Risk for Severe Intraventricular Hemorrhage
Abstract
1. Introduction
2. Materials and Methods
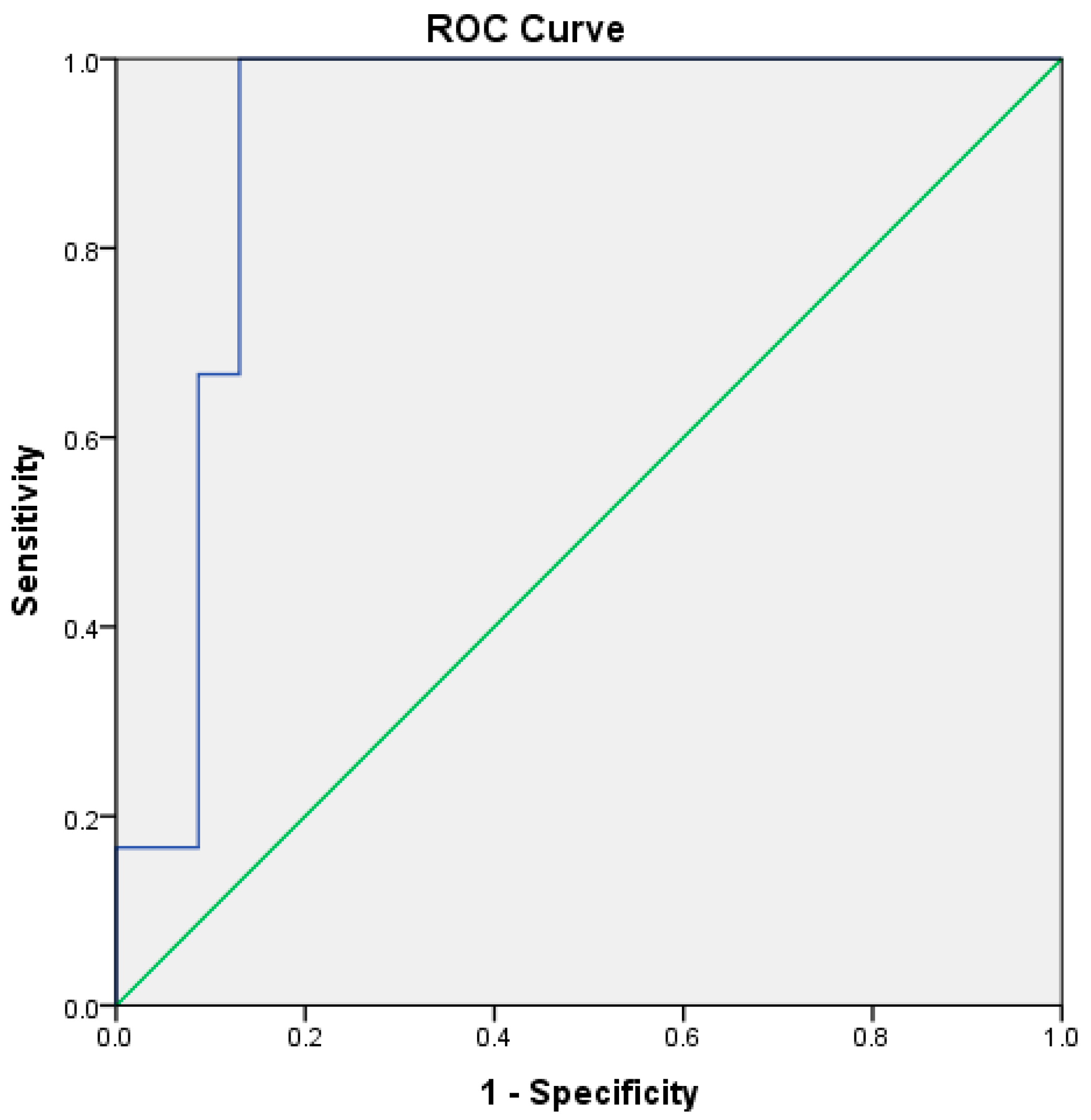
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Collins, K.A.; Popek, E. Birth injury: Birth Asphyxia and Birth Trauma. Acad. Forensic Pathol. 2018, 8, 788–864. [Google Scholar] [CrossRef] [PubMed]
- Aslam, S.; Strickland, T.; Molloy, E.J. Neonatal Encephalopathy: Need for Recognition of Multiple Etiologies for Optimal Management. Front. Pediatr. 2019, 7, 142. [Google Scholar] [CrossRef] [PubMed]
- Suppiej, A.; Franzoi, M.; Gentilomo, C.; Battistella, P.A.; Drigo, P.; Gavasso, S.; Laverda, A.M.; Simioni, P. High prevalence of inherited thrombophilia in ‘presumed peri-neonatal’ ischemic stroke. Eur. J. Haematol. 2008, 80, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Tataranno, M.L.; Vijlbrief, D.C.; Dudink, J.; Benders, M.J.N.L. Precision Medicine in Neonates: A Tailored Approach to Neonatal Brain Injury. Front. Pediatr. 2021, 9, 634092. [Google Scholar] [CrossRef] [PubMed]
- Metallinou, D.; Karampas, G.; Nyktari, G.; Iacovidou, N.; Lykeridou, K.; Rizos, D. S100B as a biomarker of brain injury in premature neonates. A prospective case–control longitudinal study. Clin. Chim. Acta 2020, 510, 781–786. [Google Scholar] [CrossRef] [PubMed]
- Ahya, K.P.; Suryawanshi, P. Neonatal periventricular leukomalacia: Current perspectives. Res. Rep. Neonatol. 2018, 2018, 8. [Google Scholar] [CrossRef]
- Coskun, Y.; Isik, S.; Bayram, T.; Urgun, K.; Sakarya, S.; Akman, I. A clinical scoring system to predict the development of intraventricular hemorrhage (IVH) in premature infants. Childs Nerv. Syst. 2018, 34, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Russ, J.B.; Simmons, R.; Glass, H.C. Neonatal Encephalopathy: Beyond Hypoxic-Ischemic Encephalopathy. Neoreviews 2021, 22, e148–e162. [Google Scholar] [CrossRef] [PubMed]
- Tenovuo, O.; Janigro, D.; Sanchez, J.C.; Undén, J. Biomarkers of Brain Damage—A Complex Challenge with Great Potential. Front. Neurol. 2021, 12, 664445. [Google Scholar] [CrossRef]
- Wassink, G.; Harrison, S.; Dhillon, S.; Bennet, B.; Gunn, A.J. Prognostic Neurobiomarkers in Neonatal Encephalopathy. Dev. Neurosci. 2022, 44, 331–343. [Google Scholar] [CrossRef]
- Bersani, I.; Pluchinotta, F.; Dotta, A.; Savarese, I.; Campi, F.; Auriti, C.; Chuklantseva, N.; Piersigilli, F.; Gazzolo, F.; Varrica, A.; et al. Early predictors of perinatal brain damage: The role of neurobiomarkers. Clin. Chem. Lab. Med. 2020, 58, 471–486. [Google Scholar] [CrossRef] [PubMed]
- Gazzolo, D.; Pluchinotta, F.; Bashir, M.; Aboulgar, H.; Said, H.M.; Iman, I.; Ivani, G.; Conio, A.; Tina, L.G.; Nigro, F.; et al. Neurological abnormalities in full-term asphyxiated newborns and salivary S100B testing: The “Cooperative Multitask against Brain Injury of Neonates” (CoMBINe) international study. PLoS ONE 2015, 10, e0115194. [Google Scholar] [CrossRef] [PubMed]
- Murray, D.M. Biomarkers in neonatal hypoxic–ischemic encephalopathy—Review of the literature to date and future directions for research. Handb. Clin. Neurol. 2019, 162, 281–293. [Google Scholar] [CrossRef] [PubMed]
- Metallinou, D.; Lazarou, E.; Lykeridou, A. Pharmacological and Non-Pharmacological Brain-Focused Clinical Practices for Premature Neonates at High Risk of Neuronal Injury. Maedica 2021, 16, 281–290. [Google Scholar] [CrossRef]
- Garcia-Alix, A.; Arnaez, J. Neuron-specific enolase in cerebrospinal fluid as a biomarker of brain damage in infants with hypoxic-ischemic encephalopathy. Neural Regen. Res. 2022, 17, 318–319. [Google Scholar] [CrossRef]
- Huang, H.Z.; Hu, X.F.; Wen, X.H.; Yang, L.Q. Serum neuron-specific enolase, magnetic resonance imaging, and electrophysiology for predicting neurodevelopmental outcomes of neonates with hypoxic-ischemic encephalopathy: A prospective study. BMC Pediatr. 2022, 22, 290. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.M.; Luo, Y.L.; Li, S.; Li, Z.X.; Jiang, L.; Zhang, G.X.; Owusu, L.; Chen, H.L. Multifunctional neuron-specific enolase: Its role in lung diseases. Biosci. Rep. 2019, 39, BSR20192732. [Google Scholar] [CrossRef]
- Haque, A.; Polcyn, R.; Matzelle, D.; Banik, N.L. New Insights into the Role of Neuron-Specific Enolase in Neuro-Inflammation, Neurodegeneration, and Neuroprotection. Brain Sci. 2018, 8, 33. [Google Scholar] [CrossRef] [PubMed]
- Metallinou, D.; Karampas, G.; Nyktari, G.; Iacovidou, N.; Lykeridou, K.; Rizos, D. Serum glial fibrillary acidic protein as a biomarker of brain injury in premature neonates. Bosn. J. Basic. Med. Sci. 2022, 22, 46–53. [Google Scholar] [CrossRef]
- Gotoh, Y.; Hashimoto, K.; Tada, K. Urine neuron-specific enolase and its clinical implication in patients with neuroblastoma. Tohoku J. Exp. Med. 1986, 149, 67–72. [Google Scholar] [CrossRef]
- Wijnberger, L.D.; Nikkels, P.G.; Van Dongen, A.J.; Noorlander, C.W.; Mulder, E.J.; Schrama, L.H.; Visser, G.H. Expression in the Placenta of Neuronal Markers for Perinatal Brain Damage. Pediatr. Res. 2002, 51, 492–496. [Google Scholar] [CrossRef]
- Attia, H.; Holayl, M.; El-Sheikh, A.E.R.; Abo-Elmagde, Y. Prognostic value of neuron specific enolase in serum for outcome of infants with birth asphyxia. ZUMJ 2016, 22, 269–275. [Google Scholar] [CrossRef]
- Perrone, S.; Grassi, F.; Caporilli, C.; Boscarino, G.; Carbone, G.; Petrolini, C.; Gambini, L.M.; Di Peri, A.; Moretti, S.; Buonocore, G.; et al. Brain Damage in Preterm and Full-Term Neonates: Serum Biomarkers for the Early Diagnosis and Intervention. Antioxidants 2023, 12, 309. [Google Scholar] [CrossRef]
- Kelen, D.; Andorka, C.; Szabó, M.; Alafuzoff, A.; Kaila, K.; Summanen, M. Serum copeptin and neuron specific enolase are markers of neonatal distress and long-term neurodevelopmental outcome. PLoS ONE 2017, 12, e0184593. [Google Scholar] [CrossRef] [PubMed]
- Abbasoglu, A.; Sarialioglu, F.; Yazici, N.; Bayraktar, N.; Haberal, A.; Erbay, A. Serum neuron-specific enolase levels in preterm and term newborns and in infants 1–3 months of age. Pediatr. Neonatol. 2015, 56, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Tian, X.; Ma, J.; Zheng, J. Clinical efficacy of gangliosides on premature infants suffering from white matter damage and its effect on the levels of IL-6, NSE and S100β. Exp. Ther. Med. 2019, 18, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Efstathiou, N.; Soubasi, V.; Koliakos, G.; Kyriazis, G.; Zafeiriou, D.I.; Slavakis, A.; Kantziou, K.; Pozotou, T.; Chatzizisi, O.; Drosou-Agakidou, V. Mobilization of circulating progenitor cells following brain injury in premature neonates could be indicative of an endogenous repair process. A pilot study. Hippokratia 2015, 19, 141–147. [Google Scholar]
- Metallinou, D.; Karampas, G.; Lazarou, E.; Iacovidou, N.; Pervanidou, P.; Lykeridou, K.; Mastorakos, G.; Rizos, D. Serum Activin A as Brain Injury Biomarker in the First Three Days of Life. A Prospective Case—Control Longitudinal Study in Human Premature Neonates. Brain Sci. 2021, 11, 1243. [Google Scholar] [CrossRef]
- European Foundation for the Care of Newborn Infants. Available online: https://newborn-health-standards.org/standards/standards-english/medical-care-clinical-practice/neurological-monitoring-in-the-high-risk-infant-ultrasound-and-mri-scanning/ (accessed on 19 March 2024).
- Papile, L.A.; Burstein, J.; Burstein, R.; Koffler, H. Incidence and evolution of subependymal and intraventricular hemorrhage: A study of infants with birth weights less than 1500 gm. J. Pediatr. 1978, 92, 529–534. [Google Scholar] [CrossRef]
- Romero-Guzman, G.J.; Lopez-Munoz, F. Prevalence and risk factors for periventricular leukomalacia in preterm infants. A systematic review. Rev. Neurol. 2017, 65, 57–62. [Google Scholar]
- Efstathiou, N.; Kyriazis, G.; Bougiouklis, D.; Drossou, V.; Soumbasi, V. Circulating progenitor cells in preterm neonates with CNS injury—A preliminary report. In Proceedings of the 4th Congress of the European Academy of Paediatric Societies (EAPS), Istanbul, Turkey, 5–9 October 2012. [Google Scholar] [CrossRef]
- Verina, T.; Fatemi, A.; Johnston, M.V.; Comi, A.M. Pluripotent possibilities: Human umbilical cord blood cell treatment after neonatal brain injury. Pediatr. Neurol. 2013, 48, 346–354. [Google Scholar] [CrossRef] [PubMed]
- Dhama, K.; Latheef, S.K.; Dadar, M.; Samad, H.A.; Munjal, A.; Khandia, R.; Karthik, K.; Tiwari, R.; Yatoo, M.; Bhatt, P.; et al. Biomarkers in Stress Related Diseases/Disorders: Diagnostic, Prognostic, and Therapeutic Values. Front. Mol. Biosci. 2019, 6, 91. [Google Scholar] [CrossRef] [PubMed]
- Paliwal, M.N.; Paliwal, P.; Varma, M.; Shaikh, M.K.; Mulye, S. Study of neuron specific enolase (NSE) in perinatal asphyxia & its role as an early marker of brain injury. J. Evid. Based Med. Healthc. 2016, 3, 3640–3643. [Google Scholar] [CrossRef]
- Smyser, C.D.; Wheelock, M.D.; Limbrick, D.D., Jr.; Neil, J.J. Neonatal brain injury and aberrant connectivity. Neuroimage 2019, 185, 609–623. [Google Scholar] [CrossRef] [PubMed]
- Hinojosa-Rodríguez, M.; Harmony, T.; Carrillo-Prado, C.; Van Horn, J.D.; Irimia, A.; Torgerson, C.; Jacokes, Z. Clinical neuroimaging in the preterm infant: Diagnosis and prognosis. Neuroimage Clin. 2017, 16, 355–368. [Google Scholar] [CrossRef] [PubMed]
- Ment, L.R.; Bada, H.S.; Barnes, P.; Grant, P.E.; Hirtz, D.; Papile, L.A.; Pinto-Martin, J.; Rivkin, M.; Slovis, T.L. Practice parameter: Neuroimaging of the neonate: Report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology 2002, 58, 1726–1738. [Google Scholar] [CrossRef]
- Sewell, E.K.; Andescavage, N.N. Neuroimaging for Neurodevelopmental Prognostication in High-Risk Neonates. Clin. Perinatol. 2018, 45, 421–437. [Google Scholar] [CrossRef]

| N | Control Group | Case Group | p-Value |
|---|---|---|---|
| 29 | 29 | ||
| Admission Mean (±SD) | 5.91 (±3.68) | 5.62 (±3.11) | 0.904 |
| 2nd day Mean (±SD) | 4.92 (±2.14) | 5.12 (±2.8) | 0.521 |
| 3rd day Mean (±SD) | 3.86 (±1.68) 1 | 5.06 (±3.49) | 0.124 |
| N | Control Group | PVL | IVH | p-Value |
|---|---|---|---|---|
| 29 | 17 | 12 | ||
| Admission Mean (±SD) | 5.91 (±3.68) | 5.66 (±3.15) | 5.57 (±3.21) | NS |
| 2nd day Mean (±SD) | 4.92 (±2.14) | 4.19 (±2.29) | 6.38 (±3.03) | NS |
| 3rd day Mean (±SD) | 3.86 (±1.68) 1 | 3.91 (±2.78) | 6.62 (±3.87) | 0.014 2 0.033 3 |
| N | All Other (Controls and PVL) | IVH | p-Value |
|---|---|---|---|
| 46 | 12 | ||
| Admission Mean (±SD) | 5.82 (±3.46) | 5.57 (±3.21) | 0.592 |
| 2nd day Mean (±SD) | 4.65 (±2.21) | 6.38 (±3.03) | 0.083 |
| 3rd day Mean (±SD) | 3.88 (±2.12) | 6.62 (±3.87) | 0.003 |
| N | All Other (Controls and PVL) | II–IV Degree IVH | p-Value |
|---|---|---|---|
| 50 | 8 | ||
| Admission Mean (±SD) | 5.83 (±3.38) | 5.34 (±3.65) | 0.715 |
| 2nd day Mean (±SD) | 4.81 (±2.19) | 6.64 (±3.98) | 0.146 |
| 3rd day Mean (±SD) | 4.06 (±2.43) | 7.52 (±3.57) | 0.003 |
| N | Control Group | Deaths | p-Value |
|---|---|---|---|
| 29 | 5 | ||
| Admission Mean (±SD) | 5.91 (±3.68) | 2.79 (±1.24) | 0.311 |
| 2nd day Mean (±SD) | 4.92 (±2.14) | 3.46 (±1.21) | 0.266 |
| 3rd day Mean (±SD) | 3.86 (±1.68) | 6.62 (±0.25) | 0.023 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Metallinou, D.; Karampas, G.; Pavlou, M.-L.; Louma, M.-I.; Mantzou, A.; Sarantaki, A.; Nanou, C.; Gourounti, K.; Tzeli, M.; Pantelaki, N.; et al. Serum Neuron-Specific Enolase as a Biomarker of Neonatal Brain Injury—New Perspectives for the Identification of Preterm Neonates at High Risk for Severe Intraventricular Hemorrhage. Biomolecules 2024, 14, 434. https://doi.org/10.3390/biom14040434
Metallinou D, Karampas G, Pavlou M-L, Louma M-I, Mantzou A, Sarantaki A, Nanou C, Gourounti K, Tzeli M, Pantelaki N, et al. Serum Neuron-Specific Enolase as a Biomarker of Neonatal Brain Injury—New Perspectives for the Identification of Preterm Neonates at High Risk for Severe Intraventricular Hemorrhage. Biomolecules. 2024; 14(4):434. https://doi.org/10.3390/biom14040434
Chicago/Turabian StyleMetallinou, Dimitra, Grigorios Karampas, Maria-Loukia Pavlou, Maria-Ioanna Louma, Aimilia Mantzou, Antigoni Sarantaki, Christina Nanou, Kleanthi Gourounti, Maria Tzeli, Nikoletta Pantelaki, and et al. 2024. "Serum Neuron-Specific Enolase as a Biomarker of Neonatal Brain Injury—New Perspectives for the Identification of Preterm Neonates at High Risk for Severe Intraventricular Hemorrhage" Biomolecules 14, no. 4: 434. https://doi.org/10.3390/biom14040434
APA StyleMetallinou, D., Karampas, G., Pavlou, M.-L., Louma, M.-I., Mantzou, A., Sarantaki, A., Nanou, C., Gourounti, K., Tzeli, M., Pantelaki, N., Tzamakos, E., Boutsikou, T., Lykeridou, A., & Iacovidou, N. (2024). Serum Neuron-Specific Enolase as a Biomarker of Neonatal Brain Injury—New Perspectives for the Identification of Preterm Neonates at High Risk for Severe Intraventricular Hemorrhage. Biomolecules, 14(4), 434. https://doi.org/10.3390/biom14040434











