Gasdermin D: A Potential New Auxiliary Pan-Biomarker for the Detection and Diagnosis of Diseases
Abstract
:1. Introduction
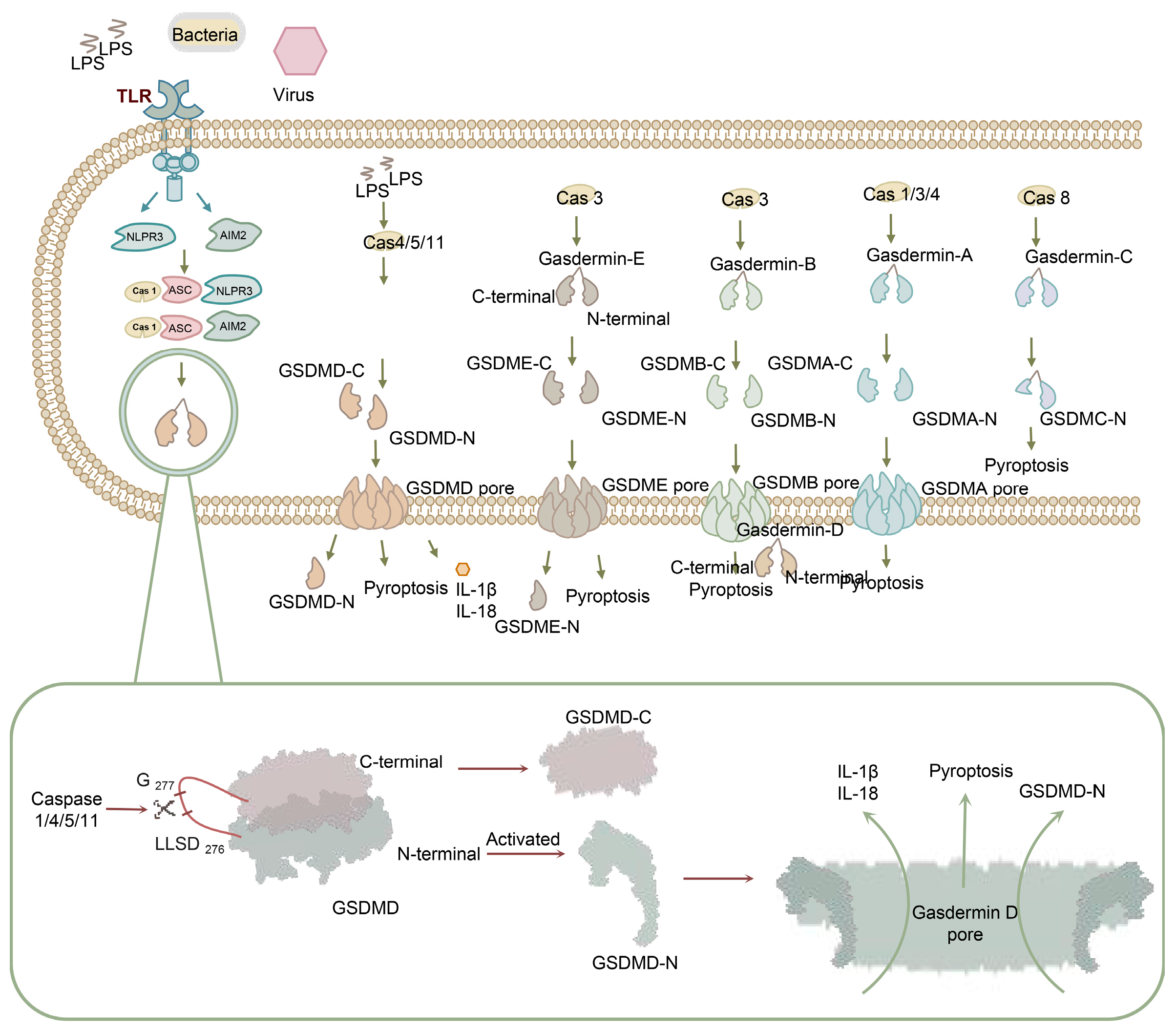
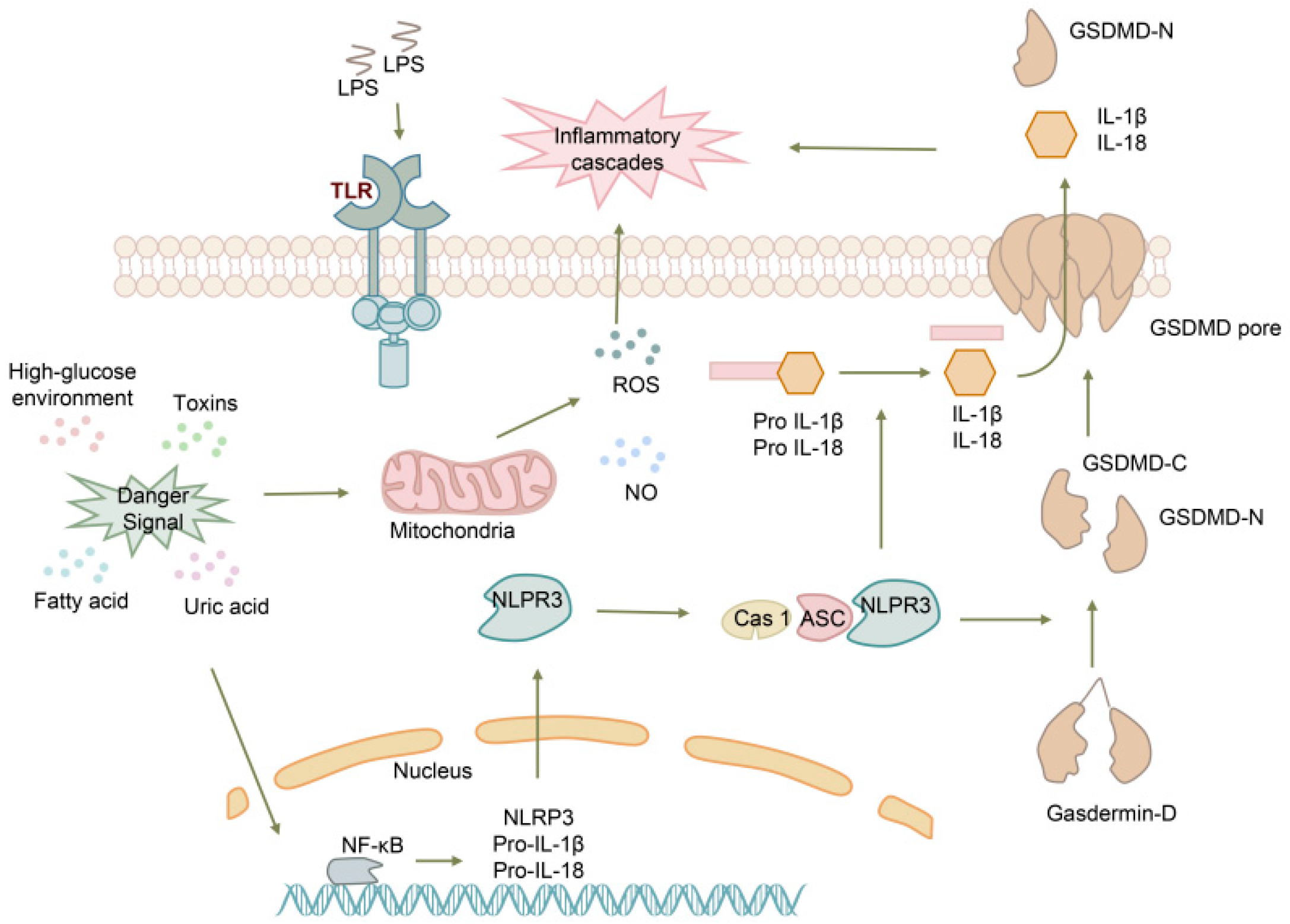
2. The Process of Pyroptosis
3. GSDMD as a Potential Biomarker for the Early Diagnosis of Infectious Diseases
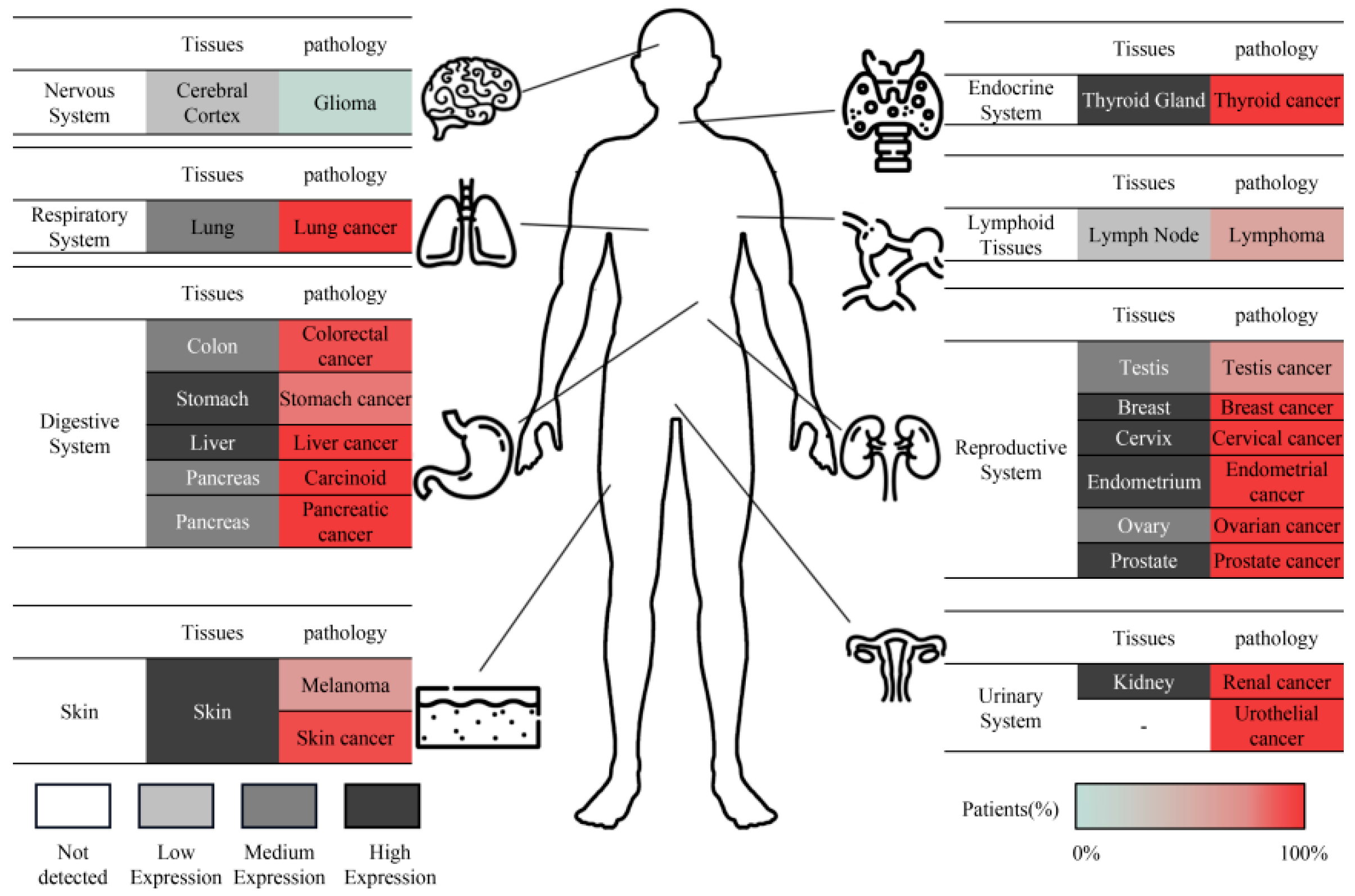
3.1. Respiratory System
3.2. The Reproductive System
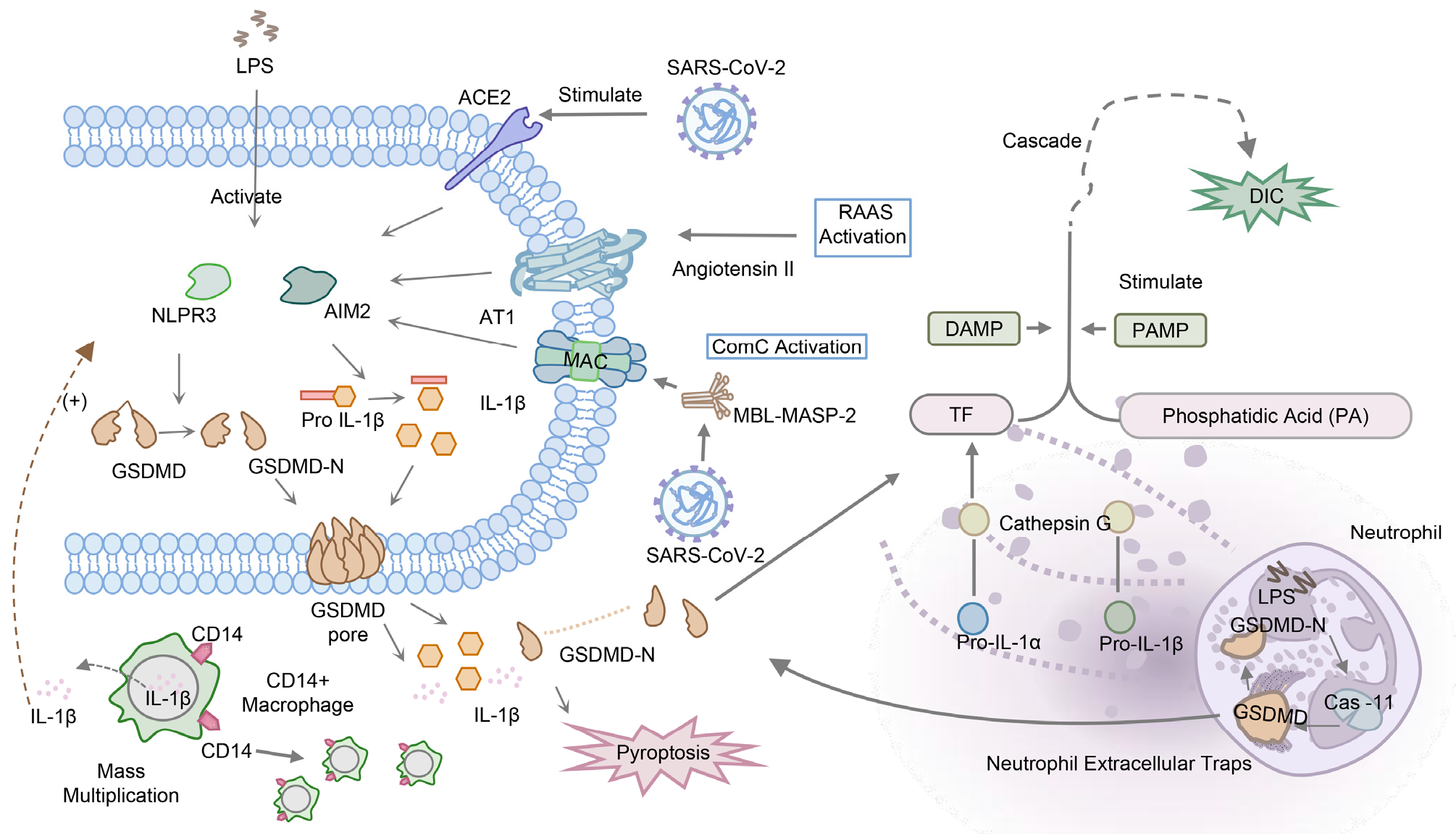
3.3. Systemic Infectious Disease
3.3.1. Sepsis
3.3.2. Disseminated Intravascular Coagulation
3.4. Liver Disease
3.4.1. Non-Alcoholic Fatty Liver Disease
3.4.2. Viral Hepatitis
4. GSDMD Has Potential as a Novel Biomarker for the Diagnosis of Non-Infectious Diseases
Nervous System
5. GSDMD Has Emerged as a Potential Novel Biomarker for Prognosis or as a Predictive Biomarker in Cancer, including Colorectal Cancer (CRC) and Brain Lower-Grade Glioma
5.1. Colorectal Cancer
5.2. Brain Lower-Grade Glioma
5.3. Pancreatic Cancer
5.4. Other Cancers
6. Evaluation of Treatment
7. GSDMD Inhibitors: Therapeutic Potential, Benefits, and Adverse Effects
7.1. Disulfiram
7.2. Necrosulfonamide
8. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Cookson, B.T.; Brennan, M.A. Pro-inflammatory programmed cell death. Trends Microbiol. 2001, 9, 113–114. [Google Scholar] [CrossRef]
- Jorgensen, I.; Miao, E.A. Pyroptotic cell death defends against intracellular pathogens. Immunol. Rev. 2015, 265, 130–142. [Google Scholar] [CrossRef]
- Hadian, K.; Stockwell, B.R. The therapeutic potential of targeting regulated non-apoptotic cell death. Nat. Rev. Drug Discov. 2023, 22, 723–742. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Mo, F.; Wang, Y.; Li, W.; Chen, Y.; Liu, J.; Chen-Mayfield, T.-J.; Hu, Q. Enhancing Gasdermin-induced tumor pyroptosis through preventing ESCRT-dependent cell membrane repair augments antitumor immune response. Nat. Commun. 2022, 13, 6321. [Google Scholar] [CrossRef]
- Tang, S.; Yang, C.; Li, S.; Ding, Y.; Zhu, D.; Ying, S.; Sun, C.; Shi, Y.; Qiao, J.; Fang, H. Genetic and pharmacological targeting of GSDMD ameliorates systemic inflammation in macrophage activation syndrome. J. Autoimmun. 2022, 133, 102929. [Google Scholar] [CrossRef]
- Fang, Y.; Tian, S.; Pan, Y.; Li, W.; Wang, Q.; Tang, Y.; Yu, T.; Wu, X.; Shi, Y.; Ma, P.; et al. Pyroptosis: A new frontier in cancer. Biomed. Pharmacother. 2019, 121, 109595. [Google Scholar] [CrossRef] [PubMed]
- De Schutter, E.; Roelandt, R.; Riquet, F.B.; Van Camp, G.; Wullaert, A.; Vandenabeele, P. Punching Holes in Cellular Membranes: Biology and Evolution of Gasdermins. Trends Cell Biol. 2021, 31, 500–513. [Google Scholar] [CrossRef] [PubMed]
- Feng, S.; Fox, D.; Man, S.M. Mechanisms of Gasdermin Family Members in Inflammasome Signaling and Cell Death. J. Mol. Biol. 2018, 430, 3068–3080. [Google Scholar] [CrossRef]
- Katoh, M.; Katoh, M. Identification and Characterization of Human Dfna5L, Mouse Dfna5L, and Rat Dfna5L Genes in Silico. Int. J. Oncol. 2004, 25, 765–770. [Google Scholar] [CrossRef]
- Zahid, A.; Ismail, H.; Jin, T. Molecular and structural aspects of gasdermin family pores and insights into gasdermin-elicited programmed cell death. Biochem. Soc. Trans. 2021, 49, 2697–2710. [Google Scholar] [CrossRef]
- Tamura, M.; Tanaka, S.; Fujii, T.; Aoki, A.; Komiyama, H.; Ezawa, K.; Sumiyama, K.; Sagai, T.; Shiroishi, T. Members of a novel gene family, Gsdm, are expressed exclusively in the epithelium of the skin and gastrointestinal tract in a highly tissue-specific manner. Genomics 2007, 89, 618–629. [Google Scholar] [CrossRef] [PubMed]
- Kuang, S.; Zheng, J.; Yang, H.; Li, S.; Duan, S.; Shen, Y.; Ji, C.; Gan, J.; Xu, X.-W.; Li, J. Structure insight of GSDMD reveals the basis of GSDMD autoinhibition in cell pyroptosis. Proc. Natl. Acad. Sci. USA 2017, 114, 10642–10647. [Google Scholar] [CrossRef]
- Ding, J.; Wang, K.; Liu, W.; She, Y.; Sun, Q.; Shi, J.; Sun, H.; Wang, D.C.; Shao, F. Pore-forming activity and structural autoinhibition of the gasdermin family. Nature 2016, 535, 111–116. [Google Scholar] [CrossRef]
- Liu, X.; Zhang, Z.; Ruan, J.; Pan, Y.; Magupalli, V.G.; Wu, H.; Lieberman, J. Inflammasome-activated gasdermin D causes pyroptosis by forming membrane pores. Nature 2016, 535, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Wang, C.; Rathkey, J.K.; Yang, J.; Dubyak, G.R.; Abbott, D.W.; Xiao, T.S. Structures of the Gasdermin D C-Terminal Domains Reveal Mechanisms of Autoinhibition. Structure 2018, 26, 778–784.e3. [Google Scholar] [CrossRef]
- Liu, Z.; Wang, C.; Yang, J.; Chen, Y.; Zhou, B.; Abbott, D.W.; Xiao, T.S. Caspase-1 Engages Full-Length Gasdermin D through Two Distinct Interfaces that Mediate Caspase Recruitment and Substrate Cleavage. Immunity 2020, 53, 106–114.e5. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Gan, L.; Xu, Y.; Luo, D.; Ren, Q.; Wu, S.; Sun, C. Melatonin Alleviates Inflammasome-Induced Pyroptosis through Inhibiting Nf-Kappab/Gsdmd Signal in Mice Adipose Tissue. J. Pineal Res. 2017, 63, e12414. [Google Scholar] [CrossRef]
- Zhang, D.; Mao, F.; Wang, S.; Wu, H.; Wang, S.; Liao, Y. Role of Transcription Factor Nrf2 in Pyroptosis in Spinal Cord Injury by Regulating GSDMD. Neurochem. Res. 2022, 48, 172–187. [Google Scholar] [CrossRef]
- Kayagaki, N.; Lee, B.L.; Stowe, I.B.; Kornfeld, O.S.; O’Rourke, K.; Mirrashidi, K.M.; Haley, B.; Watanabe, C.; Roose-Girma, M.; Modrusan, Z.; et al. IRF2 transcriptionally induces GSDMD expression for pyroptosis. Sci. Signal. 2019, 12, eaax4917. [Google Scholar] [CrossRef]
- Shao, F.; Fitzgerald, K.A. Molecular mechanisms and functions of pyroptosis. J. Mol. Biol. 2022, 434, 167461. [Google Scholar] [CrossRef]
- Liu, X.; Xia, S.; Zhang, Z.; Wu, H.; Lieberman, J. Channelling inflammation: Gasdermins in physiology and disease. Nat. Rev. Drug Discov. 2021, 20, 384–405. [Google Scholar] [CrossRef]
- Qiu, S.; Liu, J.; Xing, F. ‘Hints’ in the killer protein gasdermin D: Unveiling the secrets of gasdermins driving cell death. Cell Death Differ. 2017, 24, 588–596. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Zhao, Y.; Wang, K.; Shi, X.; Wang, Y.; Huang, H.; Zhuang, Y.; Cai, T.; Wang, F.; Shao, F. Cleavage of GSDMD by inflammatory caspases determines pyroptotic cell death. Nature 2015, 526, 660–665. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Chen, C.; Lu, Y.; Fang, L.; Cao, B.; Hu, X.; Qiu, W.; Shu, Y. Association of Serum Gasdermin D with Anti-N-Methyl-D-Aspartate Receptor Encephalitis. J. Neurochem. 2021, 159, 923–930. [Google Scholar] [CrossRef]
- Wang, Y.-Y.; Liu, X.-L.; Zhao, R. Induction of Pyroptosis and Its Implications in Cancer Management. Front. Oncol. 2019, 9, 971. [Google Scholar] [CrossRef] [PubMed]
- Ratajczak, M.Z.; Kucia, M. SARS-CoV-2 Infection and Overactivation of Nlrp3 Inflammasome as a Trigger of Cytokine “Storm” and Risk Factor for Damage of Hematopoietic Stem Cells. Leukemia 2020, 34, 1726–1729. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Kong, L.; Huang, H.; Luan, S.; Jin, R.; Wu, F. ASIC1a inhibits cell pyroptosis induced by acid-induced activation of rat hepatic stellate cells. FEBS Open Bio 2020, 10, 1044–1055. [Google Scholar] [CrossRef]
- Carl-McGrath, S.; Schneider-Stock, R.; Ebert, M.; Röcken, C. Differential expression and localisation of gasdermin-like (GSDML), a novel member of the cancer-associated GSDMDC protein family, in neoplastic and non-neoplastic gastric, hepatic, and colon tissues. Pathology 2008, 40, 13–24. [Google Scholar] [CrossRef]
- Karmakar, M.; Minns, M.; Greenberg, E.N.; Diaz-Aponte, J.; Pestonjamasp, K.; Johnson, J.L.; Rathkey, J.K.; Abbott, D.W.; Wang, K.; Shao, F.; et al. N-GSDMD trafficking to neutrophil organelles facilitates IL-1β release independently of plasma membrane pores and pyroptosis. Nat. Commun. 2020, 11, 2212. [Google Scholar] [CrossRef]
- Wang, D.; Zhan, X.; Wu, R.; You, Y.; Chen, W.; Duan, L. Assessment of Pyroptosis-Related Indicators as Potential Biomarkers and Their Association with Severity in Patients with Liver Cirrhosis. J. Inflamm. Res. 2021, 14, 3185–3196. [Google Scholar] [CrossRef]
- The Human Protein Atlas. Available online: http://www.proteinatlas.org/ (accessed on 26 October 2023).
- Jany, B.; Welte, T. Pleural Effusion in Adults—Etiology, Diagnosis, and Treatment. Dtsch. Arztebl. Int. 2019, 116, 377–386. [Google Scholar] [CrossRef] [PubMed]
- Walker, S.P.; Morley, A.J.; Stadon, L.; De Fonseka, D.; Arnold, D.T.; Medford, A.; Maskell, N.A. Nonmalignant Pleural Effusions: A Prospective Study of 356 Consecutive Unselected Patients. Chest 2017, 151, 1099–1105. [Google Scholar] [CrossRef]
- Desai, N.R.; Lee, H.J. Diagnosis and management of malignant pleural effusions: State of the art in 2017. J. Thorac. Dis. 2017, 9, S1111–S1122. [Google Scholar] [CrossRef] [PubMed]
- Huo, Z.; Yang, M.; Chen, J.; Peng, L. Improved early diagnosis of difficult cases of tuberculous pleural effusion by combination of thoracoscopy with immunological tests. Int. J. Infect. Dis. 2019, 81, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Ma, L.; Qiao, X.; Zhang, X.; Dong, S.-F.; Wu, M.-T.; Zhai, K.; Shi, H.-Z. Salivary microRNAs show potential as biomarkers for early diagnosis of malignant pleural effusion. Transl. Lung Cancer Res. 2020, 9, 1247–1257. [Google Scholar] [CrossRef]
- Li, P.; Shi, J.; Zhou, L.; Wang, B.; Zhang, L.J.; Duan, L.; Hu, Q.; Zhou, X.; Yuan, Y.; Li, D.; et al. Pleural Fluid GSDMD Is a Novel Biomarker for the Early Differential Diagnosis of Pleural Effusion. Front. Microbiol. 2021, 12, 620322. [Google Scholar] [CrossRef]
- Filipek, A.; Jurewicz, E. Preeclampsia—A Disease of Pregnant Women. Postepy Biochem. 2018, 64, 229–232. [Google Scholar]
- Correa, P.J.; Palmeiro, Y.; Soto, M.J.; Ugarte, C.; Illanes, S.E. Etiopathogenesis, Prediction, and Prevention of Preeclampsia. Hypertens. Pregnancy 2016, 35, 280–294. [Google Scholar] [CrossRef]
- Cheng, S.-B.; Nakashima, A.; Huber, W.J.; Davis, S.; Banerjee, S.; Huang, Z.; Saito, S.; Sadovsky, Y.; Sharma, S. Pyroptosis is a critical inflammatory pathway in the placenta from early onset preeclampsia and in human trophoblasts exposed to hypoxia and endoplasmic reticulum stressors. Cell Death Dis. 2019, 10, 927. [Google Scholar] [CrossRef]
- Nunes, P.R.; Mattioli, S.V.; Sandrim, V.C. NLRP3 Activation and Its Relationship to Endothelial Dysfunction and Oxidative Stress: Implications for Preeclampsia and Pharmacological Interventions. Cells 2021, 10, 2828. [Google Scholar] [CrossRef]
- Pan, Y.-J.; Zhang, M.-Z.; He, L.-H.; Feng, J.; Zhang, A.-H. Expression of urotensin II is positively correlated with pyroptosis-related molecules in patients with severe preeclampsia. Clin. Exp. Hypertens. 2020, 43, 295–304. [Google Scholar] [CrossRef]
- Zhang, X.; Chen, G.; Yin, J.; Li, L.; Huang, K.; Du, Q.; Tong, D.; Huang, Y. Pseudorabies virus infection activates the NLRP3 and IFI16 inflammasomes to trigger pyroptosis. Vet. Microbiol. 2023, 284, 109826. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; Zeng, Q.; Xiao, J.; Qin, S.; Wang, Y.; Shan, T.; Hu, D.; Zhu, Y.; Liu, K.; Zheng, K.; et al. Herpes Simplex Virus 1 Induces Microglia Gasdermin D-Dependent Pyroptosis through Activating the NLR Family Pyrin Domain Containing 3 Inflammasome. Front. Microbiol. 2022, 13, 838808. [Google Scholar] [CrossRef] [PubMed]
- Yamaoka, Y.; Matsunaga, S.; Jeremiah, S.S.; Nishi, M.; Miyakawa, K.; Morita, T.; Khatun, H.; Shimizu, H.; Okabe, N.; Kimura, H.; et al. Zika virus protease induces caspase-independent pyroptotic cell death by directly cleaving gasdermin D. Biochem. Biophys. Res. Commun. 2020, 534, 666–671. [Google Scholar] [CrossRef] [PubMed]
- Selva, K.J.; Chung, A.W. Insights into How SARS-CoV2 Infection Induces Cytokine Storms. Trends Immunol. 2022, 43, 417–419. [Google Scholar] [CrossRef] [PubMed]
- Vora, S.M.; Lieberman, J.; Wu, H. Inflammasome activation at the crux of severe COVID-19. Nat. Rev. Immunol. 2021, 21, 694–703. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Li, Y.; Wu, J.; Li, G.; Tao, X.; Lai, K.; Yuan, Y.; Zhang, X.; Zou, Z.; Xu, Y. RIPK3 collaborates with GSDMD to drive tissue injury in lethal polymicrobial sepsis. Cell Death Differ. 2020, 27, 2568–2585. [Google Scholar] [CrossRef]
- Silva, C.M.S.; Wanderley, C.W.S.; Veras, F.P.; Gonçalves, A.V.; Lima, M.H.F.; Toller-Kawahisa, J.E.; Gomes, G.F.; Nascimento, D.C.; Monteiro, V.V.S.; Paiva, I.M.; et al. Gasdermin-D Activation by SARS-CoV-2 Triggers Net and Mediate COVID-19 Immunopathology. Crit Care 2022, 26, 206. [Google Scholar] [CrossRef]
- Silva, C.M.S.; Wanderley, C.W.S.; Veras, F.P.; Sonego, F.; Nascimento, D.C.; Gonçalves, A.V.; Martins, T.V.; Cólon, D.F.; Borges, V.F.; Brauer, V.S.; et al. Gasdermin D inhibition prevents multiple organ dysfunction during sepsis by blocking NET formation. Blood 2021, 138, 2702–2713. [Google Scholar] [CrossRef]
- Iba, T.; Levy, J.H. Sepsis-induced Coagulopathy and Disseminated Intravascular Coagulation. Anesthesiology 2020, 132, 1238–1245. [Google Scholar] [CrossRef]
- Levi, M.; Sivapalaratnam, S. Disseminated intravascular coagulation: An update on pathogenesis and diagnosis. Expert Rev. Hematol. 2018, 11, 663–672. [Google Scholar] [CrossRef] [PubMed]
- Mammen, E.F. Disseminated Intravascular Coagulation (Dic). Clin. Lab. Sci. 2000, 13, 239–245. [Google Scholar] [PubMed]
- Kidokoro, A.; Iba, T.; Hong, J. Role of DIC in multiple organ failure. Int. J. Surg. Investig. 2000, 2, 73–80. [Google Scholar]
- Yang, X.; Cheng, X.; Tang, Y.; Qiu, X.; Wang, Y.; Kang, H.; Wu, J.; Wang, Z.; Liu, Y.; Chen, F.; et al. Bacterial Endotoxin Activates the Coagulation Cascade through Gasdermin D-Dependent Phosphatidylserine Exposure. Immunity 2019, 51, 983–996.e6. [Google Scholar] [CrossRef]
- Peng, Y.; Gao, M.; Liu, Y.; Qiu, X.; Cheng, X.; Yang, X.; Chen, F.; Wang, E. Bacterial outer membrane vesicles induce disseminated intravascular coagulation through the caspase-11-gasdermin D pathway. Thromb. Res. 2020, 196, 159–166. [Google Scholar] [CrossRef]
- Wu, C.; Lu, W.; Zhang, Y.; Zhang, G.; Shi, X.; Hisada, Y.; Grover, S.P.; Zhang, X.; Li, L.; Xiang, B.; et al. Inflammasome Activation Triggers Blood Clotting and Host Death through Pyroptosis. Immunity 2019, 50, 1401–1411.e4. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Peng, Y.; Wang, L.; Wang, X. Sevoflurane Attenuates Cognitive Dysfunction and Nlrp3-Dependent Caspase-1/11-Gsdmd Pathway-Mediated Pyroptosis in the Hippocampus via Upregulation of Sirt1 in a Sepsis Model. Arch. Physiol. Biochem. 2020, 128, 1413–1420. [Google Scholar] [CrossRef]
- Evavold, C.L.; Ruan, J.; Tan, Y.; Xia, S.; Wu, H.; Kagan, J.C. The Pore-Forming Protein Gasdermin D Regulates Interleukin-1 Secretion from Living Macrophages. Immunity 2017, 48, 35–44.e6. [Google Scholar] [CrossRef]
- Zhang, Y.; Wu, C.; Li, L.; Pandeya, A.; Zhang, G.; Cui, J.; Kirchhofer, D.; Wood, J.P.; Smyth, S.S.; Wei, Y.; et al. Extracellular Histones Trigger Disseminated Intravascular Coagulation by Lytic Cell Death. Int. J. Mol. Sci. 2022, 23, 6800. [Google Scholar] [CrossRef]
- Rosell, A.; Havervall, S.; Von Meijenfeldt, F.; Hisada, Y.; Aguilera, K.; Grover, S.P.; Lisman, T.; Mackman, N.; Thålin, C. Patients with COVID-19 Have Elevated Levels of Circulating Extracellular Vesicle Tissue Factor Activity that Is Associated with Severity and Mortality—Brief Report. Arterioscler. Thromb. Vasc. Biol. 2021, 41, 878–882. [Google Scholar] [CrossRef]
- Satış, H.; Özger, H.S.; Yıldız, P.A.; Hızel, K.; Gulbahar, Ö.; Erbaş, G.; Aygencel, G.; Tunccan, O.G.; Öztürk, M.A.; Dizbay, M.; et al. Prognostic value of interleukin-18 and its association with other inflammatory markers and disease severity in COVID-19. Cytokine 2020, 137, 155302. [Google Scholar] [CrossRef] [PubMed]
- Mierzchala-Pasierb, M.; Krzystek-Korpacka, M.; Lesnik, P.; Adamik, B.; Placzkowska, S.; Serek, P.; Gamian, A.; Lipinska-Gediga, M. Interleukin-18 serum levels in sepsis: Correlation with disease severity and inflammatory markers. Cytokine 2019, 120, 22–27. [Google Scholar] [CrossRef] [PubMed]
- Peverill, W.; Powell, L.W.; Skoien, R. Evolving Concepts in the Pathogenesis of NASH: Beyond Steatosis and Inflammation. Int. J. Mol. Sci. 2014, 15, 8591–8638. [Google Scholar] [CrossRef] [PubMed]
- Henao-Mejia, J.; Elinav, E.; Jin, C.; Hao, L.; Mehal, W.Z.; Strowig, T.; Thaiss, C.A.; Kau, A.L.; Eisenbarth, S.C.; Jurczak, M.J.; et al. Inflammasome-mediated dysbiosis regulates progression of NAFLD and obesity. Nature 2012, 482, 179–185. [Google Scholar] [CrossRef]
- Szabo, G.; Iracheta-Vellve, A. Inflammasome activation in the liver: Focus on alcoholic and non-alcoholic steatohepatitis. Clin. Res. Hepatol. Gastroenterol. 2015, 39, S18–S23. [Google Scholar] [CrossRef]
- Szabo, G.; Csak, T. Inflammasomes in liver diseases. J. Hepatol. 2012, 57, 642–654. [Google Scholar] [CrossRef]
- Wu, J.; Lin, S.; Wan, B.; Velani, B.; Zhu, Y. Pyroptosis in Liver Disease: New Insights into Disease Mechanisms. Aging Dis. 2019, 10, 1094–1108. [Google Scholar] [CrossRef]
- Xu, B.; Jiang, M.; Chu, Y.; Wang, W.; Chen, D.; Li, X.; Zhang, Z.; Zhang, D.; Fan, D.; Nie, Y.; et al. Gasdermin D plays a key role as a pyroptosis executor of non-alcoholic steatohepatitis in humans and mice. J. Hepatol. 2018, 68, 773–782. [Google Scholar] [CrossRef]
- Xie, W.-H.; Ding, J.; Xie, X.-X.; Yang, X.-H.; Wu, X.-F.; Chen, Z.-X.; Guo, Q.-L.; Gao, W.-Y.; Wang, X.-Z.; Li, D. Hepatitis B virus X protein promotes liver cell pyroptosis under oxidative stress through NLRP3 inflammasome activation. Inflamm. Res. 2020, 69, 683–696. [Google Scholar] [CrossRef]
- Wang, Y.; Li, X.; Chen, Q.; Jiao, F.; Shi, C.; Pei, M.; Wang, L.; Gong, Z. The relationship between liver pathological inflammation degree and pyroptosis in chronic hepatitis B patients. J. Med. Virol. 2021, 93, 6229–6235. [Google Scholar] [CrossRef]
- Yu, Y.; Dong, H.; Sun, J.; Li, B.; Chen, Y.; Feng, M.; Yang, X.; Jiang, W. Hepatitis B Virus X mediates podocyte pyroptosis by regulating the ROS/NLRP3 signaling pathway in hepatitis B virus-associated glomerulonephritis. Iran J. Basic Med. Sci. 2022, 25, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Eisfeld, H.S.; Simonis, A.; Winter, S.; Chhen, J.; Ströh, L.J.; Krey, T.; Koch, M.; Theobald, S.J.; Rybniker, J. Viral Glycoproteins Induce NLRP3 Inflammasome Activation and Pyroptosis in Macrophages. Viruses 2021, 13, 2076. [Google Scholar] [CrossRef] [PubMed]
- Scheltens, P.; De Strooper, B.; Kivipelto, M.; Holstege, H.; Chételat, G.; Teunissen, C.E.; Cummings, J.; van der Flier, W.M. Alzheimer’s Disease. Lancet 2021, 397, 1577–1590. [Google Scholar] [CrossRef]
- Leng, F.; Edison, P. Neuroinflammation and Microglial Activation in Alzheimer Disease: Where Do we Go from Here? Nat. Rev. Neurol. 2021, 17, 157–172. [Google Scholar] [CrossRef] [PubMed]
- Zhao, N.; Sun, C.; Zheng, M.; Liu, S.; Shi, R. Amentoflavone suppresses amyloid β1–42 neurotoxicity in Alzheimer’s disease through the inhibition of pyroptosis. Life Sci. 2019, 239, 117043. [Google Scholar] [CrossRef]
- Han, C.; Guo, L.; Yang, Y.; Guan, Q.; Shen, H.; Sheng, Y.; Jiao, Q. Mechanism of Microrna-22 in Regulating Neuroinflammation in Alzheimer’s Disease. Brain Behav. 2020, 10, e1627. [Google Scholar] [CrossRef]
- Rui, W.; Xiao, H.; Fan, Y.; Ma, Z.; Xiao, M.; Li, S.; Shi, J. Systemic inflammasome activation and pyroptosis associate with the progression of amnestic mild cognitive impairment and Alzheimer’s disease. J. Neuroinflamm. 2021, 18, 280. [Google Scholar] [CrossRef]
- Poh, L.; Razak, S.M.B.A.; Lim, H.M.; Lai, M.K.; Chen, C.L.-H.; Lim, L.H.; Arumugam, T.V.; Fann, D.Y. AIM2 inflammasome mediates apoptotic and pyroptotic death in the cerebellum following chronic hypoperfusion. Exp. Neurol. 2021, 346, 113856. [Google Scholar] [CrossRef]
- Liu, L.; Wang, N.; Kalionis, B.; Xia, S.; He, Q. HMGB1 plays an important role in pyroptosis induced blood brain barrier breakdown in diabetes-associated cognitive decline. J. Neuroimmunol. 2021, 362, 577763. [Google Scholar] [CrossRef]
- Shen, H.; Han, C.; Yang, Y.; Guo, L.; Sheng, Y.; Wang, J.; Li, W.; Zhai, L.; Wang, G.; Guan, Q. Pyroptosis executive protein GSDMD as a biomarker for diagnosis and identification of Alzheimer’s disease. Brain Behav. 2021, 11, e02063. [Google Scholar] [CrossRef]
- Colombo, F.; Illescas, O.; Noci, S.; Minnai, F.; Pintarelli, G.; Pettinicchio, A.; Vannelli, A.; Sorrentino, L.; Battaglia, L.; Cosimelli, M.; et al. Gut microbiota composition in colorectal cancer patients is genetically regulated. Sci. Rep. 2022, 12, 11424. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; Tian, C.; Zhao, Y.; Guo, Y.; Chen, S. Prognostic prediction of systemic immune-inflammation status for patients with colorectal cancer: A novel pyroptosis-related model. World J. Surg. Oncol. 2022, 20, 234. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Kang, Y.; Li, Y.; Sun, L.; Zhang, J.; Qian, S.; Luo, K.; Jiang, Y.; Sun, L.; Xu, F. Gasdermin D in Different Subcellular Locations Predicts Diverse Progression, Immune Microenvironment and Prognosis in Colorectal Cancer. J. Inflamm. Res. 2021, 14, 6223–6235. [Google Scholar] [CrossRef] [PubMed]
- Mu, M.; Yu, Q.; Zhang, Q.; Guo, J.; Wang, X.; Sun, X.; Yu, J. A pan-cancer analysis of molecular characteristics and oncogenic role of gasdermins. Cancer Cell Int. 2022, 22, 80. [Google Scholar] [CrossRef]
- Wu, L.-S.; Liu, Y.; Wang, X.-W.; Xu, B.; Lin, Y.-L.; Song, Y.; Dong, Y.; Liu, J.-L.; Wang, X.-J.; Liu, S.; et al. LPS Enhances the Chemosensitivity of Oxaliplatin in HT29 Cells via GSDMD-Mediated Pyroptosis. Cancer Manag. Res. 2020, 12, 10397–10409. [Google Scholar] [CrossRef]
- Wang, Q.; Wang, Y.; Ding, J.; Wang, C.; Zhou, X.; Gao, W.; Huang, H.; Shao, F.; Liu, Z. A bioorthogonal system reveals antitumour immune function of pyroptosis. Nature 2020, 579, 421–426. [Google Scholar] [CrossRef]
- Tarassishin, L.; Casper, D.; Lee, S.C. Aberrant Expression of Interleukin-1β and Inflammasome Activation in Human Malignant Gliomas. PLoS ONE 2014, 9, e103432. [Google Scholar] [CrossRef]
- Jiang, Z.; Yao, L.; Ma, H.; Xu, P.; Li, Z.; Guo, M.; Chen, J.; Bao, H.; Qiao, S.; Zhao, Y.; et al. miRNA-214 Inhibits Cellular Proliferation and Migration in Glioma Cells Targeting Caspase 1 Involved in Pyroptosis. Oncol. Res. 2017, 25, 1009–1019. [Google Scholar] [CrossRef]
- Sharma, N.; Saxena, S.; Agrawal, I.; Singh, S.; Srinivasan, V.; Arvind, S.; Epari, S.; Paul, S.; Jha, S. Differential Expression Profile of NLRs and AIM2 in Glioma and Implications for NLRP12 in Glioblastoma. Sci. Rep. 2019, 9, 8480. [Google Scholar] [CrossRef]
- Lim, J.; Kim, M.J.; Park, Y.; Ahn, J.W.; Hwang, S.J.; Moon, J.-S.; Cho, K.G.; Kwack, K. Upregulation of the NLRC4 inflammasome contributes to poor prognosis in glioma patients. Sci. Rep. 2019, 9, 7895. [Google Scholar] [CrossRef]
- Shen, L.; Li, Y.; Li, N.; Zhao, Y.; Zhou, Q.; Shen, L.; Li, Z. Integrative analysis reveals the functional implications and clinical relevance of pyroptosis in low-grade glioma. Sci. Rep. 2022, 12, 4527. [Google Scholar] [CrossRef] [PubMed]
- Qiu, S.; Hu, Y.; Dong, S. Pan-cancer analysis reveals the expression, genetic alteration and prognosis of pyroptosis key gene GSDMD. Int. Immunopharmacol. 2021, 101, 108270. [Google Scholar] [CrossRef] [PubMed]
- McGuigan, A.; Kelly, P.; Turkington, R.C.; Jones, C.; Coleman, H.G.; McCain, R.S. Pancreatic cancer: A review of clinical diagnosis, epidemiology, treatment and outcomes. World J. Gastroenterol. 2018, 24, 4846–4861. [Google Scholar] [CrossRef]
- Kamisawa, T.; Wood, L.D.; Itoi, T.; Takaori, K. Pancreatic Cancer. Lancet 2016, 388, 73–85. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Deng, Z.; Xiao, Z.; Zou, W.; Liu, R. Analysis of Pyroptosis-Related Signature for Predicting Prognosis and Tumor Immune Microenvironment in Pancreatic Cancer. Front. Oncol. 2022, 12, 770005. [Google Scholar] [CrossRef] [PubMed]
- Janowski, A.M.; Kolb, R.; Zhang, W.; Sutterwala, F.S. Beneficial and Detrimental Roles of NLRs in Carcinogenesis. Front. Immunol. 2013, 4, 370. [Google Scholar] [CrossRef]
- Broz, P.; Pelegrín, P.; Shao, F. The gasdermins, a protein family executing cell death and inflammation. Nat. Rev. Immunol. 2019, 20, 143–157. [Google Scholar] [CrossRef]
- Feng, Z.; Shi, M.; Li, K.; Ma, Y.; Jiang, L.; Chen, H.; Peng, C. Development and validation of a cancer stem cell-related signature for prognostic prediction in pancreatic ductal adenocarcinoma. J. Transl. Med. 2020, 18, 360. [Google Scholar] [CrossRef]
- Santofimia-Castaño, P.; Iovanna, J. Combating pancreatic cancer chemoresistance by triggering multiple cell death pathways. Pancreatology 2021, 21, 522–529. [Google Scholar] [CrossRef]
- Tang, R.; Xu, J.; Zhang, B.; Liu, J.; Liang, C.; Hua, J.; Meng, Q.; Yu, X.; Shi, S. Ferroptosis, necroptosis, and pyroptosis in anticancer immunity. J. Hematol. Oncol. 2020, 13, 110. [Google Scholar] [CrossRef]
- Xi, G.; Gao, J.; Wan, B.; Zhan, P.; Xu, W.; Lv, T.; Song, Y. GSDMD is required for effector CD8+ T cell responses to lung cancer cells. Int. Immunopharmacol. 2019, 74, 105713. [Google Scholar] [CrossRef]
- Gao, J.; Qiu, X.; Xi, G.; Liu, H.; Zhang, F.; Lv, T.; Song, Y. Downregulation of GSDMD attenuates tumor proliferation via the intrinsic mitochondrial apoptotic pathway and inhibition of EGFR/Akt signaling and predicts a good prognosis in non-small cell lung cancer. Oncol. Rep. 2018, 40, 1971–1984. [Google Scholar] [CrossRef]
- Wang, W.J.; Chen, D.; Jiang, M.Z.; Xu, B.; Li, X.W.; Chu, Y.; Zhang, Y.J.; Mao, R.; Liang, J.; Fan, D.M. Downregulation of gasdermin D promotes gastric cancer proliferation by regulating cell cycle-related proteins. J. Dig. Dis. 2018, 19, 74–83. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Mao, X.; Huang, Y.; Zhu, Q.; Guan, J.; Wu, L. Original Detection of proteins associated with the pyroptosis signaling pathway in breast cancer tissues and their significance. Int. J. Clin. Exp. Pathol. 2020, 13, 1408–1414. [Google Scholar]
- Xu, J.; Núñez, G. The NLRP3 inflammasome: Activation and regulation. Trends Biochem. Sci. 2022, 48, 331–344. [Google Scholar] [CrossRef] [PubMed]
- Gao, L.; Ying, F.; Cai, J.; Peng, M.; Xiao, M.; Sun, S.; Zeng, Y.; Xiong, Z.; Cai, L.; Gao, R.; et al. Identification and validation of pyroptosis-related gene landscape in prognosis and immunotherapy of ovarian cancer. J. Ovarian Res. 2023, 16, 27. [Google Scholar] [CrossRef] [PubMed]
- Qi, L.; Wang, L.; Jin, M.; Jiang, M.; Li, L.; Li, Y. Caspase-6 is a key regulator of cross-talk signal way in PANoptosis in cancer. Immunology 2023, 169, 245–259. [Google Scholar] [CrossRef]
- Jiang, M.; Qi, L.; Li, L.; Wu, Y.; Song, D.; Li, Y. Caspase-8: A Key Protein of Cross-Talk Signal Way in “Panoptosis” in Cancer. Int. J. Cancer 2021, 149, 1408–1420. [Google Scholar] [CrossRef]
- Wu, Q.; Guo, J.; Liu, Y.; Zheng, Q.; Li, X.; Wu, C.; Fang, D.; Chen, X.; Ma, L.; Xu, P.; et al. YAP drives fate conversion and chemoresistance of small cell lung cancer. Sci. Adv. 2021, 7, eabg1850. [Google Scholar] [CrossRef]
- Zhang, Z.; Li, X.; Wang, Y.; Wei, Y.; Wei, X. Involvement of inflammasomes in tumor microenvironment and tumor therapies. J. Hematol. Oncol. 2023, 16, 24. [Google Scholar] [CrossRef]
- Ning, H.; Huang, S.; Lei, Y.; Zhi, R.; Yan, H.; Jin, J.; Hu, Z.; Guo, K.; Liu, J.; Yang, J.; et al. Enhancer Decommissioning by Mll4 Ablation Elicits Dsrna-Interferon Signaling and Gsdmd-Mediated Pyroptosis to Potentiate Anti-Tumor Immunity. Nat. Commun. 2022, 13, 6578. [Google Scholar] [CrossRef] [PubMed]
- Fischer, F.A.; Chen, K.W.; Bezbradica, J.S. Posttranslational and Therapeutic Control of Gasdermin-Mediated Pyroptosis and Inflammation. Front. Immunol. 2021, 12, 661162. [Google Scholar] [CrossRef]
- Lu, Y.; Xu, F.; Wang, Y.; Shi, C.; Sha, Y.; He, G.; Yao, Q.; Shao, K.; Sun, W.; Du, J.; et al. Cancer immunogenic cell death via photo-pyroptosis with light-sensitive Indoleamine 2,3-dioxygenase inhibitor conjugate. Biomaterials 2021, 278, 121167. [Google Scholar] [CrossRef] [PubMed]
- Flores, J.; Noël, A.; Foveau, B.; Lynham, J.; Lecrux, C.; LeBlanc, A.C. Caspase-1 inhibition alleviates cognitive impairment and neuropathology in an Alzheimer’s disease mouse model. Nat. Commun. 2018, 9, 3916. [Google Scholar] [CrossRef]
- Youm, Y.-H.; Nguyen, K.Y.; Grant, R.W.; Goldberg, E.L.; Bodogai, M.; Kim, D.; D’Agostino, D.; Planavsky, N.; Lupfer, C.; Kanneganti, T.-D.; et al. The ketone metabolite β-hydroxybutyrate blocks NLRP3 inflammasome–mediated inflammatory disease. Nat. Med. 2015, 21, 263–269. [Google Scholar] [CrossRef]
- Zhao, W.; Yang, H.; Lyu, L.; Zhang, J.; Xu, Q.; Jiang, N.; Liu, G.; Wang, L.; Yan, H.; Che, C. Gsdmd, an Executor of Pyroptosis, is Involved in Il-1Β Secretion in Aspergillus Fumigatus Keratitis. Exp. Eye Res. 2021, 202, 108375. [Google Scholar] [CrossRef] [PubMed]
- Skrott, Z.; Mistrik, M.; Andersen, K.K.; Friis, S.; Majera, D.; Gursky, J.; Ozdian, T.; Bartkova, J.; Turi, Z.; Moudry, P.; et al. Alcohol-abuse drug disulfiram targets cancer via p97 segregase adaptor NPL4. Nature 2017, 552, 194–199. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.C.; Taabazuing, C.Y.; Okondo, M.C.; Chui, A.J.; Rao, S.D.; Brown, F.C.; Reed, C.; Peguero, E.; de Stanchina, E.; Kentsis, A.; et al. Dpp8/Dpp9 Inhibitor-Induced Pyroptosis for Treatment of Acute Myeloid Leukemia. Nat. Med. 2018, 24, 1151–1156. [Google Scholar] [CrossRef]
- Wu, D.; Wang, S.; Yu, G.; Chen, X. Cell Death Mediated by the Pyroptosis Pathway with the Aid of Nanotechnology: Prospects for Cancer Therapy. Angew. Chem. Int. Ed. 2020, 60, 8018–8034. [Google Scholar] [CrossRef]
- Lu, L.; Zhang, Y.; Tan, X.; Merkher, Y.; Leonov, S.; Zhu, L.; Deng, Y.; Zhang, H.; Zhu, D.; Tan, Y.; et al. Emerging mechanisms of pyroptosis and its therapeutic strategy in cancer. Cell Death Discov. 2022, 8, 338. [Google Scholar] [CrossRef]
- Zhang, Z.; Zhang, Y.; Xia, S.; Kong, Q.; Li, S.; Liu, X.; Junqueira, C.; Meza-Sosa, K.F.; Mok, T.M.Y.; Ansara, J.; et al. Gasdermin E suppresses tumour growth by activating anti-tumour immunity. Nature 2020, 579, 415–420. [Google Scholar] [CrossRef] [PubMed]
- Tsao, C.-C.; Wu, H.-H.; Wang, Y.-F.; Shen, P.-C.; Wu, W.-T.; Chen, H.-Y.; Dai, Y.-H. Novel Inflammasome-Based Risk Score for Predicting Survival and Efficacy to Immunotherapy in Early-Stage Non-Small Cell Lung Cancer. Biomedicines 2022, 10, 1539. [Google Scholar] [CrossRef]
- Zhang, Q.; Tan, Y.; Zhang, J.; Shi, Y.; Qi, J.; Zou, D.; Ci, W. Pyroptosis-Related Signature Predicts Prognosis and Immunotherapy Efficacy in Muscle-Invasive Bladder Cancer. Front. Immunol. 2022, 13, 782982. [Google Scholar] [CrossRef] [PubMed]
- Lv, Y.; Sun, B.; Lu, X.X.; Liu, Y.L.; Li, M.; Xu, L.X.; Feng, C.X.; Ding, X.; Feng, X. The Role of Microglia Mediated Pyroptosis in Neonatal Hypoxic-Ischemic Brain Damage. Biochem. Biophys. Res. Commun. 2020, 521, 933–938. [Google Scholar] [CrossRef]
- Zhang, H.; Du, Y.; Guo, Y.; Wang, Z.; Li, H.; Lv, Z.; Zeng, L.; Chen, Y.; Xie, Z.; Li, R.; et al. Tlr4-Nlrp3-Gsdmd-Mediated Pyroptosis Plays an Important Role in Aggravated Liver Injury of Cd38(-/-) Sepsis Mice. J. Immunol. Res. 2021, 2021, 6687555. [Google Scholar] [CrossRef]
- Mo, R.; Zhang, J.; Chen, Y.; Ding, Y. Nicotine promotes chronic obstructive pulmonary disease via inducing pyroptosis activation in bronchial epithelial cells. Mol. Med. Rep. 2022, 25, 92. [Google Scholar] [CrossRef] [PubMed]
- Junqueira, C.; Crespo, Â.; Ranjbar, S.; Lewandrowski, M.; Ingber, J.; de Lacerda, L.B.; Parry, B.; Ravid, S.; Clark, S.; Ho, F.; et al. SARS-CoV-2 Infects Blood Monocytes to Activate Nlrp3 and Aim2 Inflammasomes, Pyroptosis and Cytokine Release. medRxiv 2021. [Google Scholar] [CrossRef]
- Jin, Y.; Sun, M.; Jiang, X.; Zhang, Q.; Feng, D.; Wen, Z. Extracellular histones aggravate acute respiratory distress syndrome by inducing peripheral blood mononuclear cells pyroptosis. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue 2019, 31, 1357–1362. [Google Scholar]
- Hou, C.-C.; Ma, H.-F.; Ye, J.-F.; Luo, D.; Bao, H.-F.; Guan, J.-L. Plasma exosomes derived from patients with intestinal Behçet’s syndrome induce intestinal epithelial cell pyroptosis. Clin. Rheumatol. 2021, 40, 4143–4155. [Google Scholar] [CrossRef]
- Wang, Y.; Zhou, X.; Zou, K.; Chen, G.; Huang, L.; Yang, F.; Pan, W.; Xu, H.; Xu, Z.; Chen, H.; et al. Monocarboxylate Transporter 4 Triggered Cell Pyroptosis to Aggravate Intestinal Inflammation in Inflammatory Bowel Disease. Front. Immunol. 2021, 12, 644862. [Google Scholar] [CrossRef]
- Liu, Y.; He, M.; Xiong, H.; Yuan, F. Induction of Pyroptosis in Renal Tubular Epithelial Cells Using High Glucose. Front. Med. 2022, 9, 874916. [Google Scholar] [CrossRef] [PubMed]
- Yuan, S.; Wang, Y.; Li, Z.; Chen, X.; Song, P.; Chen, A.; Qu, Z.; Wen, S.; Liu, H.; Zhu, X. Gasdermin D is involved in switching from apoptosis to pyroptosis in TLR4-mediated renal tubular epithelial cells injury in diabetic kidney disease. Arch. Biochem. Biophys. 2022, 727, 109347. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhu, X.; Yuan, S.; Wen, S.; Liu, X.; Wang, C.; Qu, Z.; Li, J.; Liu, H.; Sun, L.; et al. Tlr4/Nf-Κb Signaling Induces Gsdmd-Related Pyroptosis in Tubular Cells in Diabetic Kidney Disease. Front. Endocrinol. 2019, 10, 603. [Google Scholar] [CrossRef] [PubMed]
- Cao, H.; Liang, J.; Liu, J.; He, Y.; Ke, Y.; Sun, Y.; Jiang, S.; Lin, J. Novel Effects of Combination Therapy through Inhibition of Caspase-1/Gasdermin D Induced-Pyroptosis in Lupus Nephritis. Front. Immunol. 2021, 12, 720877. [Google Scholar] [CrossRef] [PubMed]
- Berkel, C.; Cacan, E. Differential Expression and Copy Number Variation of Gasdermin (GSDM) Family Members, Pore-Forming Proteins in Pyroptosis, in Normal and Malignant Serous Ovarian Tissue. Inflammation 2021, 44, 2203–2216. [Google Scholar] [CrossRef]
- Zhu, D.; Zou, H.; Liu, J.; Wang, J.; Ma, C.; Yin, J.; Peng, X.; Li, D.; Yang, Y.; Ren, Y.; et al. Inhibition of HMGB1 Ameliorates the Maternal-Fetal Interface Destruction in Unexplained Recurrent Spontaneous Abortion by Suppressing Pyroptosis Activation. Front. Immunol. 2021, 12, 782792. [Google Scholar] [CrossRef]
- Hou, J.; Wang, C.; Ma, D.; Chen, Y.; Jin, H.; An, Y.; Jia, J.; Huang, L.; Zhao, H. The Cardioprotective and Anxiolytic Effects of Chaihujialonggumuli Granule On Rats with Anxiety After Acute Myocardial Infarction is Partly Mediated by Suppression of Cxcr4/Nf-Κb/Gsdmd Pathway. Biomed. Pharmacother. 2021, 133, 111015. [Google Scholar] [CrossRef]
- Wang, S.-H.; Cui, L.-G.; Su, X.-L.; Komal, S.; Ni, R.-C.; Zang, M.-X.; Zhang, L.-R.; Han, S.-N. GSK-3β-mediated activation of NLRP3 inflammasome leads to pyroptosis and apoptosis of rat cardiomyocytes and fibroblasts. Eur. J. Pharmacol. 2022, 920, 174830. [Google Scholar] [CrossRef]
- Wang, X.; Li, X.; Liu, S.; Brickell, A.N.; Zhang, J.; Wu, Z.; Zhou, S.; Ding, Z. PCSK9 regulates pyroptosis via mtDNA damage in chronic myocardial ischemia. Basic Res. Cardiol. 2020, 115, 66. [Google Scholar] [CrossRef]
- Sun, W.; Lu, H.; Dong, S.; Li, R.; Chu, Y.; Wang, N.; Zhao, Y.; Zhang, Y.; Wang, L.; Sun, L.; et al. Beclin1 controls caspase-4 inflammsome activation and pyroptosis in mouse myocardial reperfusion-induced microvascular injury. Cell Commun. Signal. 2021, 19, 107. [Google Scholar] [CrossRef]
- Pan, J.; Han, L.; Guo, J.; Wang, X.; Liu, D.; Tian, J.; Zhang, M.; An, F. Aim2 Accelerates the Atherosclerotic Plaque Progressions in Apoe-/- Mice. Biochem. Biophys. Res. Commun. 2018, 498, 487–494. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Pan, J.; Liu, H.; Zhang, M.; Liu, D.; Lu, L.; Tian, J.; Liu, M.; Jin, T.; An, F. AIM2 gene silencing attenuates diabetic cardiomyopathy in type 2 diabetic rat model. Life Sci. 2019, 221, 249–258. [Google Scholar] [CrossRef]
- Hu, J.J.; Liu, X.; Xia, S.; Zhang, Z.; Zhang, Y.; Zhao, J.; Ruan, J.; Luo, X.; Lou, X.; Bai, Y.; et al. FDA-approved disulfiram inhibits pyroptosis by blocking gasdermin D pore formation. Nat. Immunol. 2020, 21, 736–745. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Feng, Y.; Chen, L.; Wang, Z.; Chen, J.; Ni, Q.; Guo, X.; Zhang, L.; Xue, G. Disulfiram Accelerates Diabetic Foot Ulcer Healing by Blocking Net Formation Via Suppressing the Nlrp3/Caspase-1/Gsdmd Pathway. Transl. Res. 2023, 254, 115–127. [Google Scholar] [CrossRef] [PubMed]
- Miao, N.; Wang, Z.; Wang, Q.; Xie, H.; Yang, N.; Wang, Y.; Kang, H.; Bai, W.; Wang, Y.; He, R.; et al. Oxidized mitochondrial DNA induces gasdermin D oligomerization in systemic lupus erythematosus. Nat. Commun. 2023, 14, 872. [Google Scholar] [CrossRef] [PubMed]
- Yao, F.; Jin, Z.; Zheng, Z.; Lv, X.; Ren, L.; Yang, J.; Chen, D.; Wang, B.; Yang, W.; Chen, L.; et al. Hdac11 Promotes Both Nlrp3/Caspase-1/Gsdmd and Caspase-3/Gsdme Pathways Causing Pyroptosis via Erg in Vascular Endothelial Cells. Cell Death Discov. 2022, 8, 112. [Google Scholar] [CrossRef]
- Wang, C.; Yang, T.; Xiao, J.; Xu, C.; Alippe, Y.; Sun, K.; Kanneganti, T.-D.; Monahan, J.B.; Abu-Amer, Y.; Lieberman, J.; et al. NLRP3 inflammasome activation triggers gasdermin D–independent inflammation. Sci. Immunol. 2021, 6, eabj3859. [Google Scholar] [CrossRef]
- Yang, W.; Tao, K.; Wang, Y.; Huang, Y.; Duan, C.; Wang, T.; Li, C.; Zhang, P.; Yin, Y.; Gao, J.; et al. Necrosulfonamide ameliorates intestinal inflammation via inhibiting GSDMD-medicated pyroptosis and MLKL-mediated necroptosis. Biochem. Pharmacol. 2022, 206, 115338. [Google Scholar] [CrossRef]
- Zhang, J.; Wei, K. Necrosulfonamide Reverses Pyroptosis-Induced Inhibition of Proliferation and Differentiation of Osteoblasts through the Nlrp3/Caspase-1/Gsdmd Pathway. Exp. Cell Res. 2021, 405, 112648. [Google Scholar] [CrossRef]
- Rathkey, J.K.; Zhao, J.; Liu, Z.; Chen, Y.; Yang, J.; Kondolf, H.C.; Benson, B.L.; Chirieleison, S.M.; Huang, A.Y.; Dubyak, G.R.; et al. Chemical disruption of the pyroptotic pore-forming protein gasdermin D inhibits inflammatory cell death and sepsis. Sci. Immunol. 2018, 3, eaat2738. [Google Scholar] [CrossRef]
- Wu, Y.-L.; Ou, W.-J.; Zhong, M.; Lin, S.; Zhu, Y.-Y. Gasdermin D Inhibitor Necrosulfonamide Alleviates Lipopolysaccharide/D-galactosamine-induced Acute Liver Failure in Mice. J. Clin. Transl. Hepatol. 2022, 10, 1148–1154. [Google Scholar] [CrossRef] [PubMed]
- Qiao, Y.-L.; Zhu, M.-W.; Xu, S.; Jiao, W.-E.; Ni, H.-F.; Tao, Z.-Z.; Chen, S.-M. Allergen-induced CD11c + dendritic cell pyroptosis aggravates allergic rhinitis. Cell Commun. Signal. 2023, 21, 281. [Google Scholar] [CrossRef] [PubMed]

| Diseases | Expression | Sample Source | Sample Size | Technique | Prognosis | Results | Refs | |
|---|---|---|---|---|---|---|---|---|
| Nervous system | Brain lower-grade glioma | ↑ | Human tumor tissues | 530 | Data analysis | Poor | The GSDMD model had good predictive ability in the survival of LGG (AUC for 1 year: 0.781; 3 years: 0.754; 5 years: 0.680) | [93] |
| Endocrine system | Adrenocortical carcinoma | ↑ | Human tumor tissues | 92 | Data analysis | Poor | The GSDMD model had good predictive ability in the survival of ACC (AUC for 1 year: 0.740; 3 years: 0.708; 5 years: 0.714) | [93] |
| Respiratory system | Lung adeno- carcinoma | ↑ | Human NSCLC tissues | 162 | Immuno- histochemistry | Poor | The GSDMD protein level was an independent, poor prognostic factor of LUAD | [103] |
| Liver hepato- cellular carcinoma | ↑ | Tumor tissues | - | Data analysis | Poor | GSDMD was highly expressed in LIHC, leading to a poor prognosis (AUC for 1 year: 0.569; 3 years: 0.520; 5 years: 0.604) | [93] | |
| Digestive system | Rectum adeno- carcinoma | ↓ | Tumor tissues | - | Data analysis | Good | High expression of GSDMD improved the survival time of patients with READ (AUC for 1 year: 0.513; 3 years: 0.408; 5 years: 0.269) | [93] |
| Colorectal cancer | - | Human peripheral blood and tumor tissues | 178 | Immuno- histochemistry | Poor | High expression of cytoplasmic GSDMD was an independent favorable indicator for prognosis | [84,86] | |
| Gastric cancer | ↓ | Tumor tissues | 61 | Western blotting and qRT-PCR | Poor | GSDMD expression was decreased in GC (specificity: 0.735; sensitivity: 0.672), promoting the proliferation of tumors | [104] | |
| Urinary system | Kidney renal clear cell carcinoma | ↑ | Human tumor tissues | - | Data analysis | Poor | (AUC for 1 year: 0.513; 3 years: 0.408; 5 years: 0.269) | [93] |
| Reproductive system | Breast cancer | ↑ | Human tumor tissues | 108 | Immuno- histochemistry | Good | GSDMD was negatively related to the histopathologic grade, the tumor size, the clinical stage, the possibility of lymph node metastasis, and the risk of death | [105] |
| Diseases | Expression | Sample Source | Sample Size | Technique | Results | Refs | |
|---|---|---|---|---|---|---|---|
| Nervous system | Alzheimer’s disease | 3.19 ± 0.55 ng/mL | Human cerebrospinal fluid | 60 | ELISA | GSDMD was differentially expressed in AD and VD | [8] |
| Vascular dementia | 1.35 ± 0.34 ng/mL | Human fluid | 60 | ELISA | GSDMD was differentially expressed in AD and VD | [8] | |
| Neonatal hypoxic–ischemic encephalopathy | ↑ | Human peripheral blood | 9 | qRT-PCR and Western blotting | The NLRP-3/caspase-1/GSDMD axis is required for microglia pyroptosis and activation | [120,125] | |
| Anti-NMDAR encephalitis | 7.21 ± 3.53 ng/mL | Mice peripheral blood | - | qRT-PCR and Western blotting | GSDMD-mediated pyroptosis exacerbates the inflammatory response and liver damage and is regulated by CD38 | [126] | |
| Respiratory system | Chronic obstructive pulmonary disease | ↑ | In vitro | - | Western blotting and qPCR | Nicotine exposure increased the expression levels of GSDMD in an epithelial cell line, which may be associated with the progression of COPD | [127] |
| Severe acute respiratory syndrome coronavirus 2 | ↑ | Human blood monocytes | 60 | Immunoblot and ELISA | GSDMD was significantly elevated in COVID-19 patient plasma | [128] | |
| Acute respiratory distress syndrome | ↑ | Human blood monocytes | 40 | ELISA | The expression of GSDMD-N protein in PBMC was significantly increased and negatively correlated with PaO2/FiO2 in ARDS patients | [129] | |
| Digestive system | Intestinal Behçet’s syndrome | 16.6% ± 1.9%, 9.8% ± 1.3%, ↑ | Human intestinal tissues | 30 | Immunohistochemistry and qRT-PCR | GSDMD was significantly increased in the intestinal tissues of patients with IBS | [130] |
| Inflammatory bowel disease | ↑ | Human intestinal mucosal tissue | 15 | Immunofluorescence | The function of GSDMD depends on its subcellular location: cytoplasmic GSDMD improves prognosis while GSDMD of the nucleus promotes tumor invasion and metastasis | [131] | |
| Liver fibrosis | ↓ | Rat hepatic stellate cells | - | qPCR and Western blotting | GSDMD was decreased in hepatic stellate cells | [27] | |
| Urinary system | Diabetic kidney disease | ↑ | Human kidney tissues | 43 | Immunohistochemistry and Western blotting | GSDMD is closely related to tubular injury | [132,133,134] |
| Lupus nephritis | ↑ | Tumor tissues | 43 | Immunohistochemistry and Western blotting | GSDMD was strongly induced and cleaved | [135] | |
| Reproductive system | Ovarian cancer | ↑ | Human ovarian tissue | 578 | Data analysis | GSDMD is differently expressed among several histotypes of epithelial ovarian cancer | [136] |
| Preeclampsia | ↑ | Serum and placenta tissue | 10 | Immunofluorescence | GSDMD and its signaling pathway proteins are significant pathophysiologies | [40,42] | |
| Recurrent spontaneous abortion | ↑ | Decidual tissue | 105 | Immunohistochemistry, Western blotting, immunofluorescence, and ELISA | GSDMD was upregulated in the decidual tissues of URSA patients | [137] | |
| Myocardial infarction | ↑ | Rats’ myocardial tissues and mice’s cardiomyocytes | 41 | ELISA | GSDMD was significantly elevated in chronic MI patients | [138,139,140] | |
| Muscle tissue | Myocardial reperfusion injury | ↑ | Mice’s heart tissue | - | Immunofluorescence and immunohistochemistry | I/R caused gasdermin D expression increase in vivo and in vitro | [141] |
| Atherosclerotic | ↑ | In vitro | 100 | Immunofluorescence, Western blotting, and RT-PCR | Ox-LDL was found to promote the expression of GSDMD-N | [142] | |
| Diabetic cardiomyopathy | ↑ | Rats’ cardiac tissue | 60 | Western blotting, histology staining, and fluorescent staining | AIM2-siRNA alleviated GSDMD-N-related pyroptosis in H9c2 cardiomyoblasts | [143] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wan, N.; Shi, J.; Xu, J.; Huang, J.; Gan, D.; Tang, M.; Li, X.; Huang, Y.; Li, P. Gasdermin D: A Potential New Auxiliary Pan-Biomarker for the Detection and Diagnosis of Diseases. Biomolecules 2023, 13, 1664. https://doi.org/10.3390/biom13111664
Wan N, Shi J, Xu J, Huang J, Gan D, Tang M, Li X, Huang Y, Li P. Gasdermin D: A Potential New Auxiliary Pan-Biomarker for the Detection and Diagnosis of Diseases. Biomolecules. 2023; 13(11):1664. https://doi.org/10.3390/biom13111664
Chicago/Turabian StyleWan, Ningyi, Jing Shi, Jianguo Xu, Juan Huang, Delu Gan, Min Tang, Xiaohan Li, Ying Huang, and Pu Li. 2023. "Gasdermin D: A Potential New Auxiliary Pan-Biomarker for the Detection and Diagnosis of Diseases" Biomolecules 13, no. 11: 1664. https://doi.org/10.3390/biom13111664
APA StyleWan, N., Shi, J., Xu, J., Huang, J., Gan, D., Tang, M., Li, X., Huang, Y., & Li, P. (2023). Gasdermin D: A Potential New Auxiliary Pan-Biomarker for the Detection and Diagnosis of Diseases. Biomolecules, 13(11), 1664. https://doi.org/10.3390/biom13111664







