Abstract
Neurological symptoms are increasingly recognized in SARS-CoV-2 infected individuals. However, the neuropathogenesis remains unclear and it is not possible to define a specific damage pattern due to brain virus infection. In the present study, 33 cases of brain autopsies performed during the first (February–April 2020) and the second/third (November 2020–April 2021) pandemic waves are described. In all the cases, SARS-CoV-2 RNA was searched. Pathological findings are described and compared with those presently published.
1. Introduction
The coronavirus disease 2019 (COVID-19) is caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) and it was declared pandemic by the World Health Organization (WHO) in March 2020 [1], after its outbreak in Wuhan, China.
In Italy, as of April 2021, more than 15 million persons have been diagnosed with COVID-19 and 160,000 of them have died [2].
Most patients with COVID-19 are asymptomatic or have mild respiratory symptoms (fever, cold, cough) but about 20% develop a moderate to severe illness characterized by interstitial pneumonia, acute hypoxemic respiratory failure and, rarely, multiple organ dysfunction syndrome (MODS) [3].
It is now well understood that severe COVID-19 is not limited to the respiratory tract, but complications involving blood homeostasis [4] and other organs (such as heart, liver, kidney, skin) have been described [5,6,7,8].
Retrospective series focused on hospitalized patients have also reported several types of neurological manifestations in COVID-19, ranging from headache, myalgia, smell and taste disturbances (without significant nasal obstruction) to Guillain–Barre syndrome, encephalopathy, myelopathy, encephalitis and acute cerebro-vascular events [9].
In a recent study [10] we investigated the neuroinvasive potential of SARS-CoV-2, searching for morphological and microbiological features of viral involvement of the central nervous system (CNS) in individuals who died of COVID-19 related respiratory failure during the first pandemic wave (February–April 2020).
SARS-CoV-2 RNA was retrieved from the olfactory bulbs and tracts and from the brain tissue in 1 out of 11 patients only, while most of the brain damage was related to thrombosis.
During the second and the third pandemic waves (November 2020–April 2021), a further 22 brain autopsies were performed. SARS-CoV-2 RNA was searched in all cases and transmission electron microscopy (TEM) was also added to detect the viral particles on positive specimens.
Aim of the present paper is to report the pathological findings observed in the brain autopsies in the first, second and third pandemic waves.
2. Materials and Methods
2.1. Study Setting and Data Collection
Complete postmortem examinations were performed according to standard procedures on all 33 deceased patients with diagnosis of SARS-CoV-2 related pneumonia (comprising 10 patients previously reported, 30). The diagnosis of SARS-CoV-2 infection was performed by RT-PCR on pre mortem oropharyngeal swabs and confirmed on post mortem lung tissues in 33 patients. In one case SARS-CoV-2 pneumonia was diagnosed after autopsy (case 29). Autopsies were performed on patients with an atypical clinical course in order to identify relevant pathological features and to provide clinicians with an appropriate feedback. Autopsies were performed in Bologna, Italy, at Bellaria Hospital (Unit of Pathological Anatomy, “M. Malpighi”) and at St. Orsola-Malpighi Polyclinic (Unit of Pathological Anatomy).
2.2. Brain Cutting and Gross Examination
Neuropathological gross evaluation was performed, as previously described [10]. Briefly, samples from a standard set of brain regions were obtained as follows: the whole brain stem, basal ganglia, thalamus hippocampus, pre-rolandic and post-rolandic gyrus, frontal (parasaggital), temporal (T2) and occipital lobes (calcarine sulcus). In addition, the olfactory bulbs and tracts up to the lateral olfactory stria were removed. Formalin fixed blocks were paraffin embedded according to routine procedures (FFPE).
2.3. Histopathological Examinations
Sections (5 μm thick) were prepared from formalin fixed paraffin embedded blocks (FFPE) and were stained with hematoxylin and eosin (H&E) and Luxol fast blue (LFB). Immunohistochemistry was performed in an automated stainer (Ventana, Tucson, AZ, USA, using Ventana purchased pre-diluted antibodies): NeuN (as neuronal marker), NF (neurofilaments, as axonal marker), GFAP (glialfibrillary acid protein, as glial marker), CD68/CD45 (as microglial markers), CD45/CD20/CD3/CD4/ CD8 (lymphoid markers).
2.4. Microbiological Analysis
SARS-CoV-2 RNA was searched in all the cases on sections from olfactory bulb and tract, postrolandic cortex and rostral medulla as previously described (10). FFPE 10 micron sections were pre-treated using 160 µL Deparaffinization Solution (Qiagen, Hilden, Germany) with 180 μL of tissue lysis buffer (ATL buffer, Qiagen) and 20 μL of protease (Proteinase K solution, Qiagen, Germany). Tissues were incubated overnight at 56 °C and one-hour at 90 °C. Then extraction and amplification of nucleic acids were performed using ELITeInGenius® instrument with ELITeInGenius SP 200 and SARS-CoV-2 ELITe MGB Kit (ELITechGroup, Milano, Italy). The tissue viral load was reported as number of copies/microgram RNA. Quantification of RNA was performed using Qubit Assay (Invitrogen by ThermoFisher). Positive results below the lower limit of quantification (2 copies/reaction) were reported as <15 copies/microgram RNA. The identification of key mutations in SARS-CoV-2 Spike Protein gene (E484K, N501Y, HV69-70 del, L452R, K417T, K417N, W152C) was performed with Allplex SARS-CoV-2 Variants I and II Assay, Seegene.
2.5. Transmission Electron Microscopy (TEM)
From paraffin blocks of brain section with known SARS-CoV-2 RNA positivity, 5 mm3 areas were selected for TEM examination. Tissues were dewaxed in xylene, subsequently washed in a graded series of ethanol (100%, 95%, 70%), rehydrated rapidly in distilled water and then rinsed in cacodylate buffer 0.15 M overnight. Rehydrated tissue samples were postfixed in 1% OsO4 in cacodylate buffer, dehydrated in graded ethanol, and embedded in Araldite. Ultrathin sections, stained with uranyl acetate and lead citrate, were examined with Philips TEM CM100 Transmission Electron Microscope.
3. Results
3.1. Clinical Data
The present series included 11 patients who died during the first pandemic wave (from February 2020 to April 2020), 9 after the second pandemic wave (from November 2020 to December 2020) and 13 after the third wave (January 2021 to April 2021).
Cases include 25 men and 8 women, ranging in age from 44 to 90 years old (median age: 61).
Twenty-eight patients died after mechanical ventilation support in the intensive care unit or non-intensive care ward; patient 29 died of a sudden cardiac arrest.
The average length of symptoms duration before death was 20 days (ranging from 5 to 51 days).
On anamnesis the following conditions were present: hypertension (20 cases), obesity (17 cases), previous cerebrovascular incident (2 cases), diabetes (9 cases), dyslipidemia (8 cases), kidney failure (5 cases), ischemic heart disease (3 cases), previous cancer (3 case), chronic obstructive bronchitis (3 cases), idiopathic pulmonary fibrosis (1 case), Crohn’s disease (1 case) and distal arteriopathy (1 case). The most common symptoms at onset were dyspnea and fever (13 cases). Patients 9 and 19 came to the hospital for urinary retention, fever, syncope and may have acquired SARS-CoV2-pneumonia during hospitalization; patient 10 complained of progressive muscular weakness in addition to fever; patient 20 was hospitalized for an isolated syncope. Symptoms related to intracranial hypertension were reported in 4 cases (cases 6, 9, 10, 29); meningitis was clinically suspected in patient 20. No other acute neurological symptoms were clinically evident before death.
Clinical data are summarized in Supplementary Files—Table S1.
3.2. Brain Cutting
In all cases, the brain surface was edematous with widened gyri, flattened surface, narrowed sulci and leptomeningeal vessels congestion. Brain weight ranged from 1270 to 1870 gr. (mean 1445 gr.). In 4 cases uncal herniation was identified (cases 5, 6, 13, 29). Areas of cerebral infarction were noticed in 6 cases (case 1 left frontal, case 2 right parietal, 3 right frontal, 9 right parietal, 19 right pre-rolandic and 21 pre-rolandic and frontal). Intraparenchymal acute hemorrhage areas were seen in basal ganglia, cortex and pons in case 23 (Figure 1). Meninges were grossly congested: purulent accumulation on the leptomeningeal vault (case 8 and case 11) and focal subarachnoid hemorrhage (case 9, case 23) were observed.
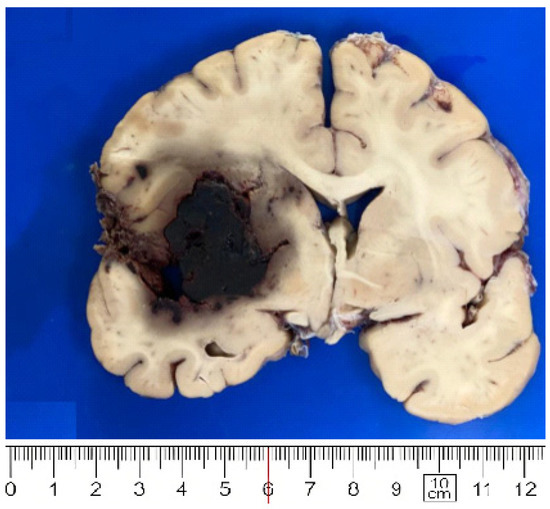
Figure 1.
Large hemorrhage in basal ganglia (case 23).
All details are sumarized in Supplementary Files—Table S2.
3.3. PCR Results
RT-PCR detected SARS-CoV-2 RNA in the brain tissues, in 2 cases only (cases 1 and 20). Case 1 was positive in the olfactory tract, in the hyppocampus and in the medulla oblongata. The viral load was 252 copies/microgram RNA. No key mutations in SARS-CoV-2 Spike Protein gene were detected suggesting the presence of original Wuhan-Hu-1 strain of SARS-CoV-2 (wild-type strain). Case 20 revealed positivity in olfactory tract only, with a viral load below the lower limit of quantification (<15 copies/microgram RNA). The low viral load did not allow the identification of key mutations. Patient 1, a 51-year-old man, with a history of drug abuse, had experienced a previous brain infarct, involving the left side motor area, therefore suffering of right hemiplegia. The same patient was in dialysis for chronic renal failure. He had the shortest COVID-19 duration, as he died 6 days after the symptoms’ onset. In addition, in the same case, SARS-CoV-2 RNA was isolated from multiple organs (lungs, liver, kidney and heart). Patient 20 was an 86-year-old man, with a history of chronic renal failure, ischemic cardiomyopathy, diabetes and distal arterial occlusive disease (DAOD). He died 11 days after the symptoms’ onset.
3.4. Histology
On histology (all features are sumarized in Supplementary Files—Table S3), the SARS CoV-2 positive olfactory bulbs, tracts and brain tissues did not differ from the negative ones: they lacked features suggestive of direct viral damage as lymphocytic infiltration, and neuronophagia.
Neuropathological examination revealed several features that can be grouped as follows: microthrombi with recent ischemic damage, acute hemorrhages, global hypoxic-ischemic injury and old ischemic damage.
Microthrombi with acute and subacute ischemic damage: all 11 cases (100%) of the first pandemic wave showed a variable number of microthrombi located in the lumen of small intraparenchymal blood vessels (Figure 2A). Focal microscopic (usually 1–2 mm in size) cortical or deep-seated (located in the basal ganglia and through the brainstem) recent infarcts were identified: they consisted of ill-defined pale areas with ischemic red neurons and scattered macrophages, sometimes clearly related to small vessel occlusion by microthrombi. Case 10 showed a larger ischemic damage of the para-hippocampal region whereas cases 2 and 9 were characterized by well-defined lesion with macrophages infiltration, hypertrophy and hyperplasia of capillary vascular cells, plump astrocytes. In the second and third waves small infarcts caused by microthrombi were less frequent (8 out of 22 cases, 38%). In all 33 cases (100%) small blood vessels ectasia, variable perivascular edema, perivascular micro-hemorrhages and scattered hemosiderin-laden macrophages (Figure 2B) were noticed. Necrotic blood vessels or intense perivascular inflammation were not identified. Immunohistochemical analysis (CD20, CD3, CD4, CD8 and CD68) highlighted mild lymphocytic or histiocytic accumulation around occasional vessels (Figure 2C). LFB and NF demonstrated only a slight perivascular myelin reduction with no clear evidence of axonal injury. Activation of microglia and astrocytes was noticed mainly in the brainstem (Figure 2D): transformation from cells with delicate processes to elements with thicker cell projections was detected by immunohistochemistry (CD68 and GFAP). No evidence of neuronophagia was present.
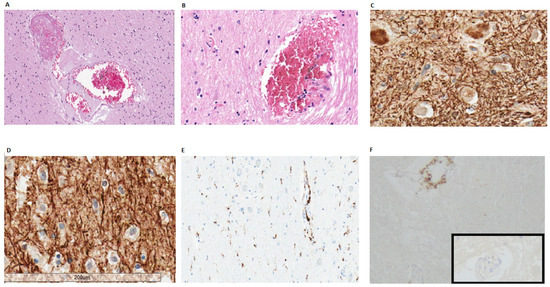
Figure 2.
(A) Micro-thrombi in small intra-parenchymal vessels (case 28, frontal cortex); (B) Micro-hemorrhages surrounding small intraparenchymal of the brain stem (case 13); (C,D) Neurofilament staining showed no clear axonal damage in the medulla oblongata (C) and in the olfactory tract (D) of SARS-CoV-2 positive specimens; (E) Microglial activation and perivascular histiocytes were evidenced by CD68 (case 1). (F) Immunostaining for CD4 highlighted sparse perivascular lymphocytes CD4+ (case 4, medulla oblongata). Inset: normal brain parenchymal vessel without inflammation (immunostaining for CD4).
Acute hemorrhage was observed in 2 cases (one in each first and second pandemic waves). Case 23 showed multiple acute hemorrhages (ranging from 6 cm to 0.5 cm) through infratentorial leptomeninges, basal ganglia, pons and cortex. No amyloid deposition or septic emboli could be noticed. In this brain microthrombi and subacute infarction were also present. In case 9 supratentorial hemorrhagic areas were seen.
Global hypoxic-ischemic injury was observed in all brains (in the first, second and third pandemic waves). Ischemic red neurons were present through all the brain stem, the hippocampal CA1 region and the cerebellar Purkinje cells, consistent with global ischemic injury.
Old ischemic damage (consistent with anamnestic data) was observed in 2 cases. Case 1 showed a 2 cm cystic lesion involving the internal capsule and atrophy of the pyramidal tract, consistent with the history of remote brain infarct. Case 3 presented an area of astrogliosis in the right insula, consistent with an ischemic damage diagnosed 2 years prior death.
Cases 9, 19, 21, 23, 29 and 30 showed atherosclerosis involving bilaterally the internal carotids and the basilar artery.
Internal carotid artery aneurysm was evidenced in case 18.
In addition, 16 out of 33 cases (48%) showed leptomeningeal mild chronic inflammation.
Leptomeningeal inflammation was noticed especially in specimens from the third wave (9 out of 13, 69%).
The most evident features of bacterial superinfection were observed in cases 8, 9 and 11, all observed during the first pandemic wave. Cases 8 and 11 showed macroscopically evident purulent leptomeningeal accumulation and revealed, on histology, endovascular thrombi composed of dense fibrin with neutrophils and necrotic debris, as seen in suppurative leptomeningitis. In case 9 histological evidence of initial infection was detected, characterized by endoluminal leukocytes accumulation and fibrin deposits with blood extravasation. In those patients (cases 8, 9 and 11) Pseudomonas aeruginosa, Candida albicans, Staphylococcus capitis, Staphylococcus aureus, Methicillin-resistant Staphylococcus aureus (MRSA) and Enterococcus faecium were isolated from blood cultures.
Differences between the main three pandemic waves are summarized in Table 1, according to clinical, gross and microscopic features.

Table 1.
Summary of findings in the three pandemic waves.
3.5. Transmission Electron Microscopy (TEM)
In positive brain samples of case 1, neurons showed perinuclear cytoplasmic vacuoles ranging in size from 180 to 211 nm and surrounded by a double membrane (Figure 3A). Occasional small vesicles bulging into the vacuole lumen were seen. In addition, cytoplasmic ribosome aggregates and nuclear bodies were seen, suggestive of unspecific viral infection (Figure 3B). No true spike-delimited virions were detected. The vascular structures showed severe artifactual alterations likely due to suboptimal formalin fixation of autoptic specimens. No specific signs of viral infections were detectable and mitochondria appeared swollen with fragmented cristae (Figure 3C).
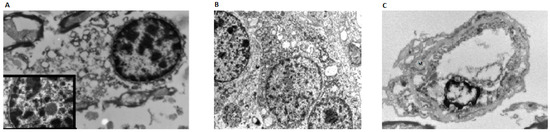
Figure 3.
(A) TEM analysis in SARS-CoV-2 positive medulla oblongata showed cytoplasmatic vacuoles sized 180 to 211 nm. A nuclear body can be detectable (inset); (B) Neuronal cell with two synaptic structures (left) in the setting of a ganglioglioma for comparison; (C) a capillary shows severe artifactual alterations without viral-related structures: mitochondria (M) are swollen with fragmented cristae.
4. Discussion
Several neurological symptoms have been described in SARS-CoV-2 infected patients, while the exact tissue damage mechanism is still under debate. The main question is to determine if SARS-CoV-2 virus can directly infect the brain parenchyma.
In the present series, SARS-CoV-2 RNA was present in olfactory nerve and in the brain tissue of 2 (out of 33 tested, 6%) patients, but on histology, the PCR positive olfactory tract and brain tissues did not show any specific histological change suggestive of direct viral damage.
TEM analysis showed some feature indicative but non-specific of viral infection.
The small percentage of SARS-CoV-2 infected brains in the present series could be consequent of the method of virus detection, performed on FFPE and not on freshly frozen tissues. Mukerji and Salomon reviewed the COVID-19 brain autopsies published [10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30] exploring all the ancillary tests used to detect SARS-CoV-2 in CNS specimens: immunohistochemistry (IHC) identified the viral nucleocapsid (N) or spike (S) proteins in 21% of cases tested (n = 16/74); TEM reported virus-like particles in only one case [29]; in situ hybridization (ISH) for viral RNA was negative in the single case tested [27]; RT-PCR identified SARS-CoV-2 RNA in 41% of formalin-fixed paraffin-embedded brain tissue (n = 34/84) and in 25% of olfactory bulb/tract specimens (n = 9/36) but cannot specifically identify the localization of virus.
Due to the different methods used it is difficult to exactly assess the rate of SARS-CoV-2 brain infection, nevertheless, all the data published confirm that the SARS-CoV-2virus can infect the brain tissue.
Most probably SARS-CoV-2 invade the brain through the Angiotensin-Converting Enzyme 2 (ACE2) receptor of the olfactory epithelium [31] or through endothelial cells of the blood–brain barrier (BBB) with the ACE2 receptor-mediated pathway [31]. In spite of SARS-CoV-2’s ability to invade the brain tissue, most of the brain damage observed is related to intraparenchymal thrombosis and ischemic damage.
The present data are consistent with those found previously published [29,30].
Accordingly, microglial activation and astrogliosis in the brainstem (n = 73), acute hypoxic injury from mild to severe (n = 59), infarcts/ischemic necrosis (n = 22), focal microhemorrhages (n = 23), intravascular microthrombi (n =12) and neutrophilic plugs (n = 3) constituted the most frequently detected brain alterations. T-cell predominant lymphocytic infiltrates can be identified, but without clear evidence of vasculitis or meningoencephalitis [29,30]. In the present series, microthrombi and microscopic infarcts were less frequently detected (8/21, 38%) in cases from the second and the third pandemic waves (November 2020 to April 2021) than in cases of the first pandemic wave (11/11, 100%). This difference can be explained by the more extensive application of anticoagulant therapy in critical patients recently adopted.
From a clinical point of view, different central acute neurological manifestations in patients with COVID-19 have been reported. Ischemic stroke, sinus venous thrombosis and cerebral hemorrhage have been described [32,33,34] and have been related to the inflammation, hypoxia, immobilization or diffuse intravascular coagulation [32]. Our findings and the other neuropathological data in the literature seem to confirm this hypothesis. Dizziness, impaired consciousness, confusion, headache, syncope and seizures have also been reported in SARS-CoV-2 infected patients [35]: they are extremely non-specific and could be the manifestation of an ischemic event, such as global cerebral hypoxia, inflammatory status or electrolyte imbalances rather than a direct viral damage of circumscribed cerebral areas.
All these histological data indicate that CNS is probably “a victim more than a target” in SARS-CoV-2 [36]: intravascular microthrombi and microinfarcts are in keeping with the hypercoagulable state of severe SARS-CoV-2 infected patients whereas the hypoxic-ischemic general condition, related to the respiratory failure, may indeed be worsened by the consequent brainstem damage appearing as a final event.
Clinical and radiological data suggest that SARS-CoV2 can cause meningitis and encephalitis.
The first case of meningoencephalitis was reported in a 24-year-old male with fever and seizures: SARS-CoV-2 RNA was found in the cerebrospinal fluid (CSF) but not in the naso-pharyngeal swab [37]. Duong et al. reported meningoencephalitis in a 41-year-old female who presented with fever and stiff neck [38]: she was tested positive for COVID-19 but the presence of virus RNA in the CSF was not confirmed. Lewis et al. in a recent review highlighted that detection of SARS-CoV-2 in CSF via PCR or evaluation for intrathecal antibody synthesis appears to be rare: of 58 patients whose CSF was tested for SARS-CoV-2 antibody, 7 (12%) had positive antibodies; of 132 patients who had oligoclonal, only 3 (2%) had evidence of intrathecal antibody synthesis; of 77 patients tested for autoimmune antibodies in the CSF, 4 (5%) had positive findings [39].
In our series we did not find signs of viral meningitis but purulent leptomeningitis was seen in 2 cases and bacteria (Pseudomonas aeruginosa, Candida albicans, Staphylococcus capitis, Staphlococcus aureusand Methicillinresistant Staphylococcus aureus, Enterococcus faecium) were isolated, suggesting hematogenous bacterial spread leading to acute bacterial meningitis or encephalitis.
Neuropathological evidence is still not available for Guillain–Barre syndrome [40], Miller–Fisher syndrome [41] or polyneuritis cranialis [42] in SARS-CoV-2 infected patients.
Even more complicated is the debate about subsequent development of chronic neurological disease in COVID-19 patients. This hypothesis is based on experimental models for SARS-CoV and MERSCoV (that already demonstrated the presence of these viruses inside the nerve cells, with degeneration and neuronal death) [43].
Specifically, the evidence from murine lung injury models by coronaviruses emphasizes the correlation between the NLRP3 inflammasome-mediated and the pathological accumulation of neurodegeneration-associated peptides such as fibrillar amyloid-β [44], leading to Alzheimer’s disease.
Much remains also to be learned about the effects of central nervous system chronic inflammation and microenvironment changes after COVID-19 [45].
SARS-CoV-2 infection might elicit the proinflammatory microglia phenotype, which can present in a patient as a neurodegenerative disorder [46].
The presence of reactive pro-inflammatory microglia can also increase the expression of genes that cause neuroinflammation [47].
In the cases here studied, inflammation was minimal to mild: rare T-lymphocytes and macrophages are detected mainly by immunohistochemistry around intraparenchymal vessels or leptomeninges.
In addition, inflammation could have been reduced by long immunosuppressive therapy (steroid). Astrogliosis and microglia activation (sometimes with microglial nodules) are instead prominent.
The present study has some limitations, including the small sample size and the absence of pre-mortem specific neurologic symptoms. Prospective studies are needed to investigate potential correlations between acute, sub-acute, chronic COVID-19 infections and long-term neurological complications.
5. Conclusions
The data here shown are consistent with data presently published and features indicate that:
SARS-CoV-2 can directly infect the CNS even if it is not clear which is the direct type of brain tissue damage.
Morphological features indicate that SARS-CoV-2 related coagulation disorders are the main cause of the brain tissue damage. The immediate use of anticoagulant therapy in critical patients reduced thromboembolic complications.
Bacterial superinfection can be the cause of acute leptomeningitis during SARS-CoV-2 infection.
Brain damage can be present even in absence of specific neurological symptoms. Therefore, it is possible that brain involvement could be an underestimated feature in SARS-CoV-2 infected patients [48].
Astrogliosis, microglial activation and chronic inflammation could play a role for the development of chronic neurological disorders.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/biom12050629/s1: Table S1: clinical data, Table S2: Summary of gross neuropathological findings, Table S3: summary of histological findings.
Author Contributions
All authors contributed to the study conception and design. Specifically: Conceptualization, V.P.F., M.R., A.D. and M.P.F.; methodology, V.P.F., M.R., A.D. and M.P.F.; formal analysis, V.P.F., M.R., T.L., L.G., C.G., G.C., C.T.; investigation, V.P.F., M.R., A.D. and M.P.F.; data curation V.P.F., M.R., T.L., L.G., R.A., G.F., R.L. (Rocco Liguori), R.L. (Raffaele Lodi); writing—original draft preparation V.P.F., M.R., M.P.F.; writing—review and editing, V.P.F., M.R., T.L., L.G., G.C., R.A., R.L. (Rocco Liguori); supervision, R.L. (Rocco Liguori), R.L. (Raffaele Lodi), A.D. and M.P.F. All authors commented on previous versions of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
No funds were obtained for the present paper.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Area Vasta Emilia Centrale, AVEC (protocol code 863/2020/Oss/AOUBo).
Data Availability Statement
All the data that have been cited in this paper are openly available in PubMed® at https://pubmed.ncbi.nlm.nih.gov/ (accessed on 1 April 2022). All the data supporting the findings of this study are available from the corresponding author on request.
Acknowledgments
Acknowledgment is due to all the technical staff for technical help. Specifically, Rocco Ierinò, Monia Venturoli and Rosanna Amato.
Conflicts of Interest
MPF received grants from Roche, Devicor Mammotome, MSD and Biocartis. All the remaining authors declare no conflict of interest regarding the present paper.
References
- Cucinotta, D.; Vanelli, M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [CrossRef]
- Italian Ministry of Health, Coronavirus Resource Center. Available online: http://www.salute.gov.it (accessed on 1 April 2022).
- Piva, S.; Filippini, M.; Turla, F.; Cattaneo, S.; Margola, A.; De Fulviis, S.; Nardiello, I.; Beretta, A.; Ferrari, L.; Trotta, R.; et al. Clinical presentation and initial management critically ill patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in Brescia, Italy. J. Crit. Care 2020, 58, 29–33. [Google Scholar] [CrossRef] [PubMed]
- Levi, M.; Thachil, J.; Iba, T.; Levy, J.H. Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol. 2020, 7, e438–e440. [Google Scholar] [CrossRef]
- Basso, C.; Leone, O.; Rizzo, S.; De Gaspari, M.; Van Der Wal, A.C.; Aubry, M.-C.; Bois, M.C.; Lin, P.T.; Maleszewski, J.J.; Stone, J.R. Pathological features of COVID-19-associated myocardial injury: A multicentre cardiovascular pathology study. Eur. Heart J. 2020, 41, 3827–3835. [Google Scholar] [CrossRef]
- Sun, J.; Aghemo, A.; Forner, A.; Valenti, L. COVID-19 and liver disease. Liver Int. 2020, 40, 1278–1281. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ronco, C.; Reis, T. Kidney involvement in COVID-19 and rationale for extracorporeal therapies. Nat. Rev. Nephrol. 2020, 16, 308–310. [Google Scholar] [CrossRef] [Green Version]
- Marzano, A.; Cassano, N.; Genovese, G.; Moltrasio, C.; Vena, G. Cutaneous manifestations in patients with COVID-19: A preliminary review of an emerging issue. Br. J. Dermatol. 2020, 183, 431–442. [Google Scholar] [CrossRef] [PubMed]
- Ellul, M.A.; Benjamin, L.; Singh, B.; Lant, S.; Michael, B.D.; Easton, A.; Kneen, R.; Defres, S.; Sejvar, J.; Solomon, T. Neurological associations of COVID-19. Lancet Neurol. 2020, 19, 767–783. [Google Scholar] [CrossRef]
- Fabbri, V.P.; Foschini, M.P.; Lazzarotto, T.; Gabrielli, L.; Cenacchi, G.; Gallo, C.; Aspide, R.; Frascaroli, G.; Cortelli, P.; Riefolo, M.; et al. Brain ischemic injury in COVID-19-infected patients: A series of 10 post-mortem cases. Brain Pathol. 2021, 31, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Matschke, J.; Lütgehetmann, M.; Hagel, C.; Sperhake, J.P.; Schröder, A.S.; Edler, C.; Mushumba, H.; Fitzek, A.; Allweiss, L.; Dandri, M.; et al. Neuropathology of patients with COVID-19 in Germany: A post-mortem case series. Lancet Neurol. 2020, 19, 919–929. [Google Scholar] [CrossRef]
- Solomon, I.H.; Normandin, E.; Bhattacharyya, S.; Mukerji, S.S.; Keller, K.; Ali, A.S.; Adams, G.; Hornick, J.L.; Padera, R.F., Jr.; Sabeti, P. Neuropathological Features of Covid-19. N. Engl. J. Med. 2020, 383, 989–992. [Google Scholar] [CrossRef] [PubMed]
- Remmelink, M.; De Mendonça, R.; D’Haene, N.; De Clercq, S.; Verocq, C.; Lebrun, L.; Lavis, P.; Racu, M.-L.; Trépant, A.-L.; Maris, C.; et al. Unspecific post-mortem findings despite multiorgan viral spread in COVID-19 patients. Crit. Care 2020, 24, 495. [Google Scholar] [CrossRef]
- Schurink, B.; Roos, E.; Radonic, T.; Barbe, E.; Bouman, C.S.C.; de Boer, H.H.; de Bree, G.J.; Bulle, E.B.; Aronica, E.M.; Florquin, S.; et al. Viral presence and immunopathology in patients with lethal COVID-19: A prospective autopsy cohort study. Lancet Microbe 2020, 1, e290–e299. [Google Scholar] [CrossRef]
- Schaller, T.; Hirschbühl, K.; Burkhardt, K.; Braun, G.; Trepel, M.; Märkl, B.; Claus, R. Postmortem Examination of Patients with COVID-19. JAMA 2020, 323, 2518–2520. [Google Scholar] [CrossRef] [PubMed]
- Hanley, B.; Naresh, K.; Roufosse, C.; Nicholson, A.G.; Weir, J.; Cooke, G.S.; Thursz, M.; Manousou, P.; Corbett, R.; Goldin, R.; et al. Histopathological findings and viral tropism in UK patients with severe fatal COVID-19: A post-mortem study. Lancet Microbe 2020, 1, e245–e253. [Google Scholar] [CrossRef]
- Deigendesch, N.; Sironi, L.; Kutza, M.; Wischnewski, S.; Fuchs, V.; Hench, J.; Frank, A.; Nienhold, R.; Mertz, K.D.; Cathomas, G.; et al. Correlates of critical illness-related encephalopathy predominate postmortem COVID-19 neuropathology. Acta Neuropathol. 2020, 140, 583–586. [Google Scholar] [CrossRef] [PubMed]
- Bussani, R.; Schneider, E.; Zentilin, L.; Collesi, C.; Ali, H.; Braga, L.; Volpe, M.C.; Colliva, A.; Zanconati, F.; Berlot, G.; et al. Persistence of viral RNA, pneumocyte syncytia and thrombosis are hallmarks of advanced COVID-19 pathology. EBioMedicine 2020, 61, 103104. [Google Scholar] [CrossRef]
- Bradley, B.T.; Maioli, H.; Johnston, R.; Chaudhry, I.; Fink, S.L.; Xu, H.; Najafian, B.; Deutsch, G.; Lacy, J.M.; Williams, T.; et al. Histopathology and ultrastructural findings of fatal COVID-19 infections in Washington State: A case series. Lancet 2020, 396, 320–332, Erratum in Lancet 2020, 396, 312. [Google Scholar] [CrossRef]
- Kantonen, J.; Mahzabin, S.; Mäyränpää, M.I.; Tynninen, O.; Paetau, A.; Andersson, N.; Sajantila, A.; Vapalahti, O.; Carpén, O.; Kekäläinen, E.; et al. Neuropathologic features of four autopsied COVID-19 patients. Brain Pathol. 2020, 30, 1012–1016. [Google Scholar] [CrossRef]
- Barton, L.M.; Duval, E.J.; Stroberg, E.; Ghosh, S.; Mukhopadhyay, S. COVID-19 Autopsies, Oklahoma, USA. Am. J. Clin. Pathol. 2020, 153, 725–733, Erratum in Am. J. Clin. Pathol. 2020, 153, 852. [Google Scholar] [CrossRef] [Green Version]
- Kirschenbaum, D.; Imbach, L.L.; Ulrich, S.; Rushing, E.J.; Keller, E.; Reimann, R.R.; Frauenknecht, K.; Lichtblau, M.; Witt, M.; Hummel, T.; et al. Inflammatory olfactory neuropathy in two patients with COVID-19. Lancet 2020, 396, 166. [Google Scholar] [CrossRef]
- Jaunmuktane, Z.; Mahadeva, U.; Green, A.; Sekhawat, V.; Barrett, N.A.; Childs, L.; Shankar-Hari, M.; Thom, M.; Jäger, H.R.; Brandner, S. Microvascular injury and hypoxic damage: Emerging neuropathological signatures in COVID-19. Acta Neuropathol. 2020, 140, 397–400. [Google Scholar] [CrossRef] [PubMed]
- Lax, S.F.; Skok, K.; Zechner, P.; Kessler, H.H.; Kaufmann, N.; Koelblinger, C.; Vander, K.; Bargfrieder, U.; Trauner, M. Pulmonary Arterial Thrombosis in COVID-19 with Fatal Outcome: Results From a Prospec-tive, Single-Center, Clinicopathologic Case Series. Ann. Intern. Med. 2020, 173, 350–361. [Google Scholar] [CrossRef] [PubMed]
- Dolhnikoff, M.; Ferranti, J.F.; de Almeida Monteiro, R.A.; Duarte-Neto, A.N.; Gomes-Gouvêa, M.S.; Degaspare, N.V.; Delgado, A.F.; Fiorita, C.M.; Leal, G.N.; Rodrigues, R.M.; et al. SARS-CoV-2 in cardiac tissue of a child with COVID-19-related multisystem inflammatory syndrome. Lancet Child Adolesc. Health 2020, 4, 790–794, Erratum in Lancet Child Adolesc. Health 2020, 4, e39. [Google Scholar] [CrossRef]
- Craver, R.; Huber, S.; Sandomirsky, M.; McKenna, D.; Schieffelin, J.; Finger, L. Fatal Eosinophilic Myocarditis in a Healthy 17-Year-Old Male with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2c). Fetal Pediatr. Pathol. 2020, 39, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Al-Dalahmah, O.; Thakur, K.T.; Nordvig, A.S.; Prust, M.L.; Roth, W.; Lignelli, A.; Uhlemann, A.-C.; Miller, E.H.; Kunnath-Velayudhan, S.; Del Portillo, A.; et al. Neuronophagia and microglial nodules in a SARS-CoV-2 patient with cerebellar hemorrhage. Acta Neuropathol. Commun. 2020, 8, 147. [Google Scholar] [CrossRef]
- Reichard, R.R.; Kashani, K.B.; Boire, N.A.; Constantopoulos, E.; Guo, Y.; Lucchinetti, C.F. Neuropathology of COVID-19: A spectrum of vascular and acute disseminated encephalomyelitis (ADEM)-like pathology. Acta Neuropathol. 2020, 140, 1–6. [Google Scholar] [CrossRef]
- Paniz-Mondolfi, A.; Bryce, C.; Grimes, Z.; Gordon, R.E.; Reidy, J.; Lednicky, J.; Sordillo, E.M.; Fowkes, M. Central nervous system involvement by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). J. Med. Virol. 2020, 92, 699–702. [Google Scholar] [CrossRef] [Green Version]
- Mukerji, S.S.; Solomon, I.H. What can we learn from brain autopsies in COVID-19? Neurosci. Lett. 2020, 742, 135528. [Google Scholar] [CrossRef]
- Bilińska, K.; Jakubowska, P.; Von Bartheld, C.S.; Butowt, R. Expression of the SARS-CoV-2 Entry Proteins, ACE2 and TMPRSS2, in Cells of the Olfactory Epithelium: Identification of Cell Types and Trends with Age. ACS Chem. Neurosci. 2020, 11, 1555–1562. [Google Scholar] [CrossRef]
- Ackermann, M.; Verleden, S.E.; Kuehnel, M.; Haverich, A.; Welte, T.; Laenger, F.; Vanstapel, A.; Werlein, C.; Stark, H.; Tzankov, A.; et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19. N. Engl. J. Med. 2020, 383, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Oxley, T.J.; Mocco, J.; Majidi, S.; Kellner, C.P.; Shoirah, H.; Singh, I.P.; De Leacy, R.A.; Shigematsu, T.; Ladner, T.R.; Yaeger, K.A.; et al. Large-Vessel Stroke as a Presenting Feature of COVID-19 in the Young. N. Engl. J. Med. 2020, 382, e60. [Google Scholar] [CrossRef] [PubMed]
- Avula, A.; Nalleballe, K.; Narula, N.; Sapozhnikov, S.; Dandu, V.; Toom, S.; Glaser, A.; Elsayegh, D. COVID-19 presenting as stroke. Brain Behav. Immun. 2020, 87, 115–119. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, I.; Rathore, F.A. Neurological manifestations and complications of COVID-19: A literature review. J. Clin. Neurosci. 2020, 77, 8–12. [Google Scholar] [CrossRef]
- Franca, R.A.; Ugga, L.; Guadagno, E.; Russo, D.; Del Basso De Caro, M. Neuroinvasive potential of SARS-CoV2 with neuroradiological and neuropathological findings: Is the brain a target or a victim? Acta Psychiatr. Scand. 2020, 129, 37–54. [Google Scholar] [CrossRef]
- Moriguchi, T.; Harii, N.; Goto, J.; Harada, D.; Sugawara, H.; Takamino, J.; Ueno, M.; Sakata, H.; Kondo, K.; Myose, N.; et al. A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. Int. J. Infect. Dis. 2020, 94, 55–58. [Google Scholar] [CrossRef]
- Duong, L.; Xu, P.; Liu, A. Meningoencephalitis without respiratory failure in a young female patient with COVID-19 infection in Downtown Los Angeles, early April 2020. Brain Behav. Immun. 2020, 87, 33. [Google Scholar] [CrossRef]
- Lewis, A.; Frontera, J.; Placantonakis, D.G.; Lighter, J.; Galetta, S.; Balcer, L.; Melmed, K. Cerebrospinal fluid in COVID-19: A systematic review of the literature. J. Neurol. Sci. 2021, 421, 117316. [Google Scholar] [CrossRef]
- Toscano, G.; Palmerini, F.; Ravaglia, S.; Ruiz, L.; Invernizzi, P.; Cuzzoni, M.G.; Franciotta, D.; Baldanti, F.; Daturi, R.; Postorino, P.; et al. Guillain–Barré Syndrome Associated with SARS-CoV-2. N. Engl. J. Med. 2020, 382, 2574–2576. [Google Scholar] [CrossRef]
- Gutiérrez-Ortiz, C.; Méndez-Guerrero, A.; Rodrigo-Rey, S.; Pedro-Murillo, E.S.; Bermejo-Guerrero, L.; Gordo-Mañas, R.; de Aragón-Gómez, F.; Benito-León, J. Miller Fisher syndrome and polyneuritis cranialis in COVID-19. Neurology 2020, 95, e601–e605. [Google Scholar] [CrossRef] [Green Version]
- Desforges, M.; Le Coupanec, A.; Dubeau, P.; Bourgouin, A.; Lajoie, L.; Dube, M.; Talbot, P.J. Human Coronaviruses and Other Respiratory Viruses: Underestimated Opportunistic Pathogens of the Central Nervous System? Viruses 2019, 12, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agrawal, A.; Garron, T.; Tao, X.; Peng, B.-H.; Wakamiya, M.; Chan, T.-S.; Couch, R.B.; Tseng, C.-T.K. Generation of a Transgenic Mouse Model of Middle East Respiratory Syndrome Coronavirus Infection and Disease. J. Virol. 2015, 89, 3659–3670. [Google Scholar] [CrossRef] [Green Version]
- Heneka, M.T.; Golenbock, D.; Latz, E.; Morgan, D.; Brown, R. Immediate and long-term consequences of COVID-19 infections for the development of neurological disease. Alzheimers Res. Ther. 2020, 12, 69. [Google Scholar] [CrossRef] [PubMed]
- Pallanti, S.; Grassi, E.; Makris, N.; Gasic, G.P.; Hollander, E. Neurocovid-19: A clinical neuroscience-based approach to reduce SARS-CoV-2 related mental health sequelae. J. Psychiatr. Res. 2020, 130, 215–217. [Google Scholar] [CrossRef] [PubMed]
- Amruta, N.; Chastain, W.H.; Paz, M.; Solch, R.J.; Murray-Brown, I.C.; Befeler, J.B.; Gressett, T.E.; Longo, M.T.; Engler-Chiurazzi, E.B.; Bix, G. SARS-CoV-2 mediated neuroinflammation and the impact of COVID-19 in neurological disorders. Cytokine Growth Factor Rev. 2021, 58, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Murta, V.; Villarreal, A.; Ramos, A.J. Severe Acute Respiratory Syndrome Coronavirus 2 Impact on the Central Nervous System: Are Astrocytes and Microglia Main Players or Merely Bystanders? ASN Neuro 2020, 12, 1759091420954960. [Google Scholar] [CrossRef] [PubMed]
- Romoli, M.; Jelčić, I.; Bernard-Valnet, R.; Azorín, D.G.; Mancinelli, L.; Akhvlediani, T.; Monaco, S.; Taba, P.; Sellner, J.; for the Infectious Disease Panel of the European Academy of Neurology. A systematic review of neurological manifestations of SARS-CoV-2 infection: The devil is hidden in the details. Eur. J. Neurol. 2020, 27, 1712–1726. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).