The Role of Systemic Microvascular Dysfunction in Heart Failure with Preserved Ejection Fraction
Abstract
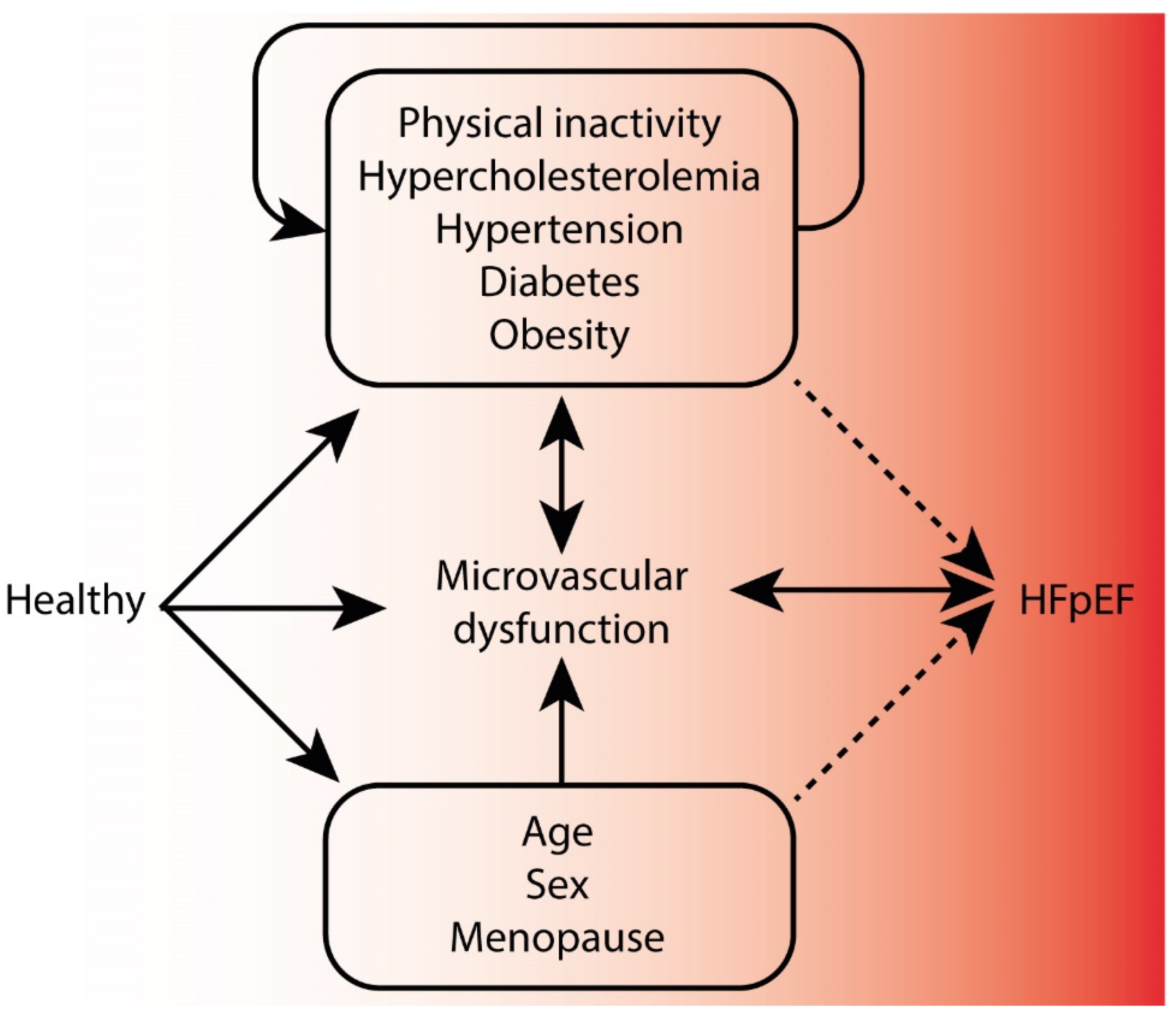
1. Introduction
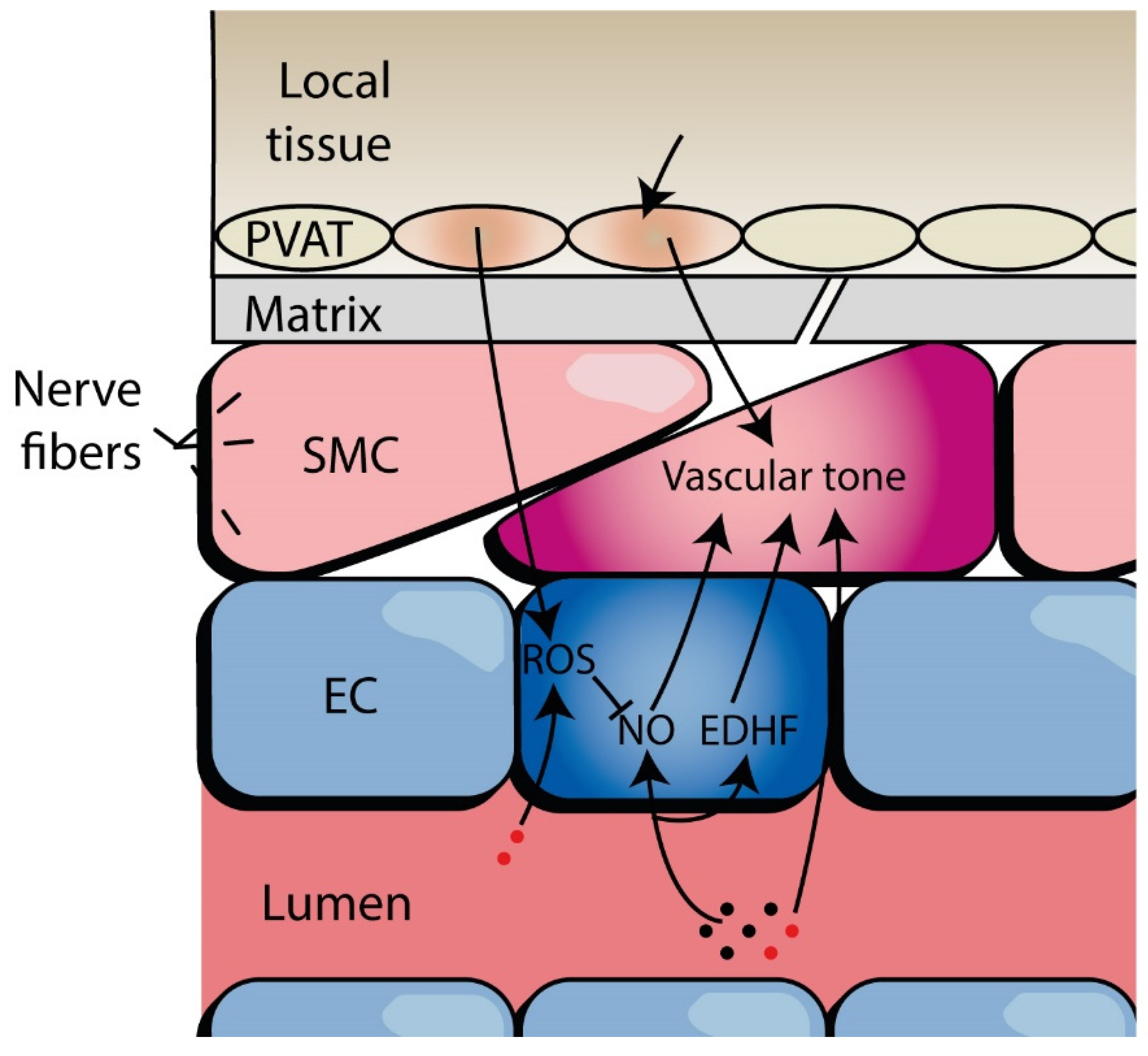
2. Defining Microvascular Function and Dysfunction
3. Evidence of Microvascular Dysfunction in HFpEF
3.1. Vasoreactivity in HFpEF
3.1.1. Endothelium-Dependent Vasodilation
3.1.2. Endothelium-Independent Vasodilation
3.2. Capillary Rarefaction in HFpEF
3.3. Microvascular Biomarkers in HFpEF
4. Other Tissue Alterations and Pathways Related to MVD in HFpEF
4.1. Adipose Tissue Changes and MVD
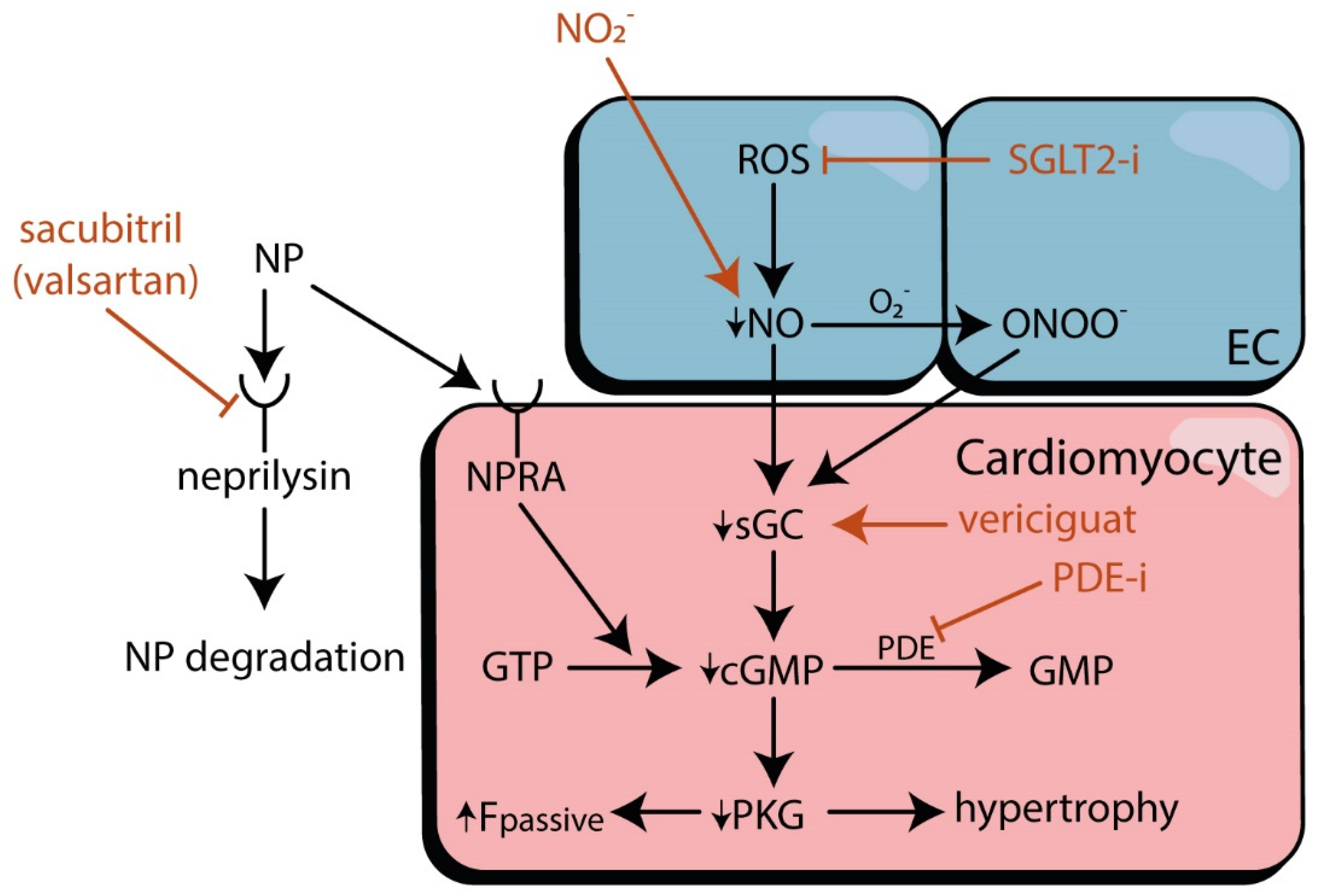
4.2. MVD Pathways and Cardiomyocyte Stiffness
5. Microvascular Interventions in HFpEF
6. Challenges
7. Future Perspectives
8. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Reddy, Y.N.; Borlaug, B.A. Heart Failure With Preserved Ejection Fraction. Curr. Probl. Cardiol. 2016, 41, 145–188. [Google Scholar] [CrossRef]
- Savarese, G.; Lund, L.H. Global Public Health Burden of Heart Failure. Card. Fail. Rev. 2017, 3, 7–11. [Google Scholar] [CrossRef]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.; Coats, A.J.; Falk, V.; Gonzalez-Juanatey, J.R.; Harjola, V.P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. J. Heart Fail. 2016, 18, 891–975. [Google Scholar] [CrossRef]
- Savji, N.; Meijers, W.C.; Bartz, T.M.; Bhambhani, V.; Cushman, M.; Nayor, M.; Kizer, J.R.; Sarma, A.; Blaha, M.J.; Gansevoort, R.T.; et al. The Association of Obesity and Cardiometabolic Traits With Incident HFpEF and HFrEF. JACC Heart Fail. 2018, 6, 701–709. [Google Scholar] [CrossRef]
- Senni, M.; Caravita, S.; Paulus, W.J. Do Existing Definitions Identify Subgroup Phenotypes or Reflect the Natural History of Heart Failure With Preserved Ejection Fraction? Circulation 2019, 140, 366–369. [Google Scholar] [CrossRef] [PubMed]
- Kalogeropoulos, A.; Georgiopoulou, V.; Psaty, B.M.; Rodondi, N.; Smith, A.L.; Harrison, D.G.; Liu, Y.; Hoffmann, U.; Bauer, D.C.; Newman, A.B.; et al. Inflammatory markers and incident heart failure risk in older adults: The Health ABC (Health, Aging, and Body Composition) study. J. Am. Coll. Cardiol. 2010, 55, 2129–2137. [Google Scholar] [CrossRef]
- Paulus, W.J.; Tschope, C. A novel paradigm for heart failure with preserved ejection fraction: Comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J. Am. Coll. Cardiol. 2013, 62, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Franssen, C.; Chen, S.; Unger, A.; Korkmaz, H.I.; De Keulenaer, G.W.; Tschope, C.; Leite-Moreira, A.F.; Musters, R.; Niessen, H.W.; Linke, W.A.; et al. Myocardial Microvascular Inflammatory Endothelial Activation in Heart Failure With Preserved Ejection Fraction. JACC Heart Fail. 2016, 4, 312–324. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.H.; Obokata, M.; Reddy, Y.N.V.; Redfield, M.M.; Lerman, A.; Borlaug, B.A. Endothelium-dependent and independent coronary microvascular dysfunction in patients with heart failure with preserved ejection fraction. Eur. J. Heart Fail. 2020, 22, 432–441. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.J.; Lam, C.S.P.; Svedlund, S.; Saraste, A.; Hage, C.; Tan, R.S.; Beussink-Nelson, L.; Ljung Faxen, U.; Fermer, M.L.; Broberg, M.A.; et al. Prevalence and correlates of coronary microvascular dysfunction in heart failure with preserved ejection fraction: PROMIS-HFpEF. Eur. Heart J. 2018, 39, 3439–3450. [Google Scholar] [CrossRef] [PubMed]
- Balmain, S.; Padmanabhan, N.; Ferrell, W.R.; Morton, J.J.; McMurray, J.J. Differences in arterial compliance, microvascular function and venous capacitance between patients with heart failure and either preserved or reduced left ventricular systolic function. Eur. J. Heart Fail. 2007, 9, 865–871. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, S.F.; Hussain, S.; Mirzoyev, S.A.; Edwards, W.D.; Maleszewski, J.J.; Redfield, M.M. Coronary microvascular rarefaction and myocardial fibrosis in heart failure with preserved ejection fraction. Circulation 2015, 131, 550–559. [Google Scholar] [CrossRef] [PubMed]
- Dryer, K.; Gajjar, M.; Narang, N.; Lee, M.; Paul, J.; Shah, A.P.; Nathan, S.; Butler, J.; Davidson, C.J.; Fearon, W.F.; et al. Coronary microvascular dysfunction in patients with heart failure with preserved ejection fraction. Am. J. Physiol. Heart Circ. Physiol. 2018, 314, H1033–H1042. [Google Scholar] [CrossRef]
- Xu, Z.; Gu, H.P.; Gu, Y.; Sun, W.; Yu, K.; Zhang, X.W.; Kong, X.Q. Increased index of microcirculatory resistance in older patients with heart failure with preserved ejection fraction. J. Geriatr. Cardiol. 2018, 15, 687–694. [Google Scholar] [CrossRef]
- Sandesara, P.B.; O’Neal, W.T.; Kelli, H.M.; Samman-Tahhan, A.; Hammadah, M.; Quyyumi, A.A.; Sperling, L.S. The Prognostic Significance of Diabetes and Microvascular Complications in Patients With Heart Failure With Preserved Ejection Fraction. Diabetes Care 2018, 41, 150. [Google Scholar] [CrossRef] [PubMed]
- Kitzman, D.W.; Nicklas, B.; Kraus, W.E.; Lyles, M.F.; Eggebeen, J.; Morgan, T.M.; Haykowsky, M. Skeletal muscle abnormalities and exercise intolerance in older patients with heart failure and preserved ejection fraction. Am. J. Physiol. Heart Circ. Physiol. 2014, 306, H1364–H1370. [Google Scholar] [CrossRef]
- Houben, A.J.H.M.; Stehouwer, C.D.A. Microvascular dysfunction: Determinants and treatment, with a focus on hyperglycemia. Endocr. Metab. Sci. 2021, 2, 100073. [Google Scholar] [CrossRef]
- Parikh, K.S.; Sharma, K.; Fiuzat, M.; Surks, H.K.; George, J.T.; Honarpour, N.; Depre, C.; Desvigne-Nickens, P.; Nkulikiyinka, R.; Lewis, G.D.; et al. Heart Failure With Preserved Ejection Fraction Expert Panel Report: Current Controversies and Implications for Clinical Trials. JACC Heart Fail. 2018, 6, 619–632. [Google Scholar] [CrossRef]
- Houben, A.; Martens, R.J.H.; Stehouwer, C.D.A. Assessing Microvascular Function in Humans from a Chronic Disease Perspective. J. Am. Soc. Nephrol. 2017, 28, 3461–3472. [Google Scholar] [CrossRef]
- Segal, S.S. Integration and Modulation of Intercellular Signaling Underlying Blood Flow Control. J. Vasc. Res. 2015, 52, 136–157. [Google Scholar] [CrossRef]
- Secomb, T.W.; Pries, A.R. The microcirculation: Physiology at the mesoscale. J. Physiol. 2011, 589, 1047–1052. [Google Scholar] [CrossRef] [PubMed]
- Aird, W.C. Phenotypic Heterogeneity of the Endothelium. Circ. Res. 2007, 100, 158–173. [Google Scholar] [CrossRef] [PubMed]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef] [PubMed]
- Akiyama, E.; Sugiyama, S.; Matsuzawa, Y.; Konishi, M.; Suzuki, H.; Nozaki, T.; Ohba, K.; Matsubara, J.; Maeda, H.; Horibata, Y.; et al. Incremental prognostic significance of peripheral endothelial dysfunction in patients with heart failure with normal left ventricular ejection fraction. J. Am. Coll. Cardiol. 2012, 60, 1778–1786. [Google Scholar] [CrossRef]
- Matsue, Y.; Suzuki, M.; Nagahori, W.; Ohno, M.; Matsumura, A.; Hashimoto, Y.; Yoshida, K.; Yoshida, M. Endothelial dysfunction measured by peripheral arterial tonometry predicts prognosis in patients with heart failure with preserved ejection fraction. Int. J. Cardiol. 2013, 168, 36–40. [Google Scholar] [CrossRef]
- Yamamoto, E.; Hirata, Y.; Tokitsu, T.; Kusaka, H.; Sakamoto, K.; Yamamuro, M.; Kaikita, K.; Watanabe, H.; Hokimoto, S.; Sugiyama, S.; et al. The pivotal role of eNOS uncoupling in vascular endothelial dysfunction in patients with heart failure with preserved ejection fraction. Int. J. Cardiol. 2015, 190, 335–337. [Google Scholar] [CrossRef] [PubMed]
- Waku, R.; Tokoi, S.; Toyoda, S.; Kitahara, K.; Naganuma, J.; Yazawa, H.; Sakuma, M.; Abe, S.; Nakajima, T.; Inoue, T. Flow-Mediated Vasodilation and Reactive Hyperemia Index in Heart Failure with Reduced or Preserved Ejection Fraction. Tohoku J. Exp. Med. 2020, 252, 85–93. [Google Scholar] [CrossRef]
- Gevaert, A.B.; Beckers, P.J.; Van Craenenbroeck, A.H.; Lemmens, K.; Van De Heyning, C.M.; Heidbuchel, H.; Vrints, C.J.; Van Craenenbroeck, E.M. Endothelial dysfunction and cellular repair in heart failure with preserved ejection fraction: Response to a single maximal exercise bout. Eur. J. Heart Fail. 2019, 21, 125–127. [Google Scholar] [CrossRef]
- Borlaug, B.A.; Olson, T.P.; Lam, C.S.; Flood, K.S.; Lerman, A.; Johnson, B.D.; Redfield, M.M. Global cardiovascular reserve dysfunction in heart failure with preserved ejection fraction. J. Am. Coll. Cardiol. 2010, 56, 845–854. [Google Scholar] [CrossRef]
- Marechaux, S.; Samson, R.; van Belle, E.; Breyne, J.; de Monte, J.; Dedrie, C.; Chebai, N.; Menet, A.; Banfi, C.; Bouabdallaoui, N.; et al. Vascular and Microvascular Endothelial Function in Heart Failure With Preserved Ejection Fraction. J. Card. Fail. 2016, 22, 3–11. [Google Scholar] [CrossRef]
- Boyes, N.G.; Eckstein, J.; Pylypchuk, S.; Marciniuk, D.D.; Butcher, S.J.; Lahti, D.S.; Dewa, D.M.K.; Haykowsky, M.J.; Wells, C.R.; Tomczak, C.R. Effects of heavy-intensity priming exercise on pulmonary oxygen uptake kinetics and muscle oxygenation in heart failure with preserved ejection fraction. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2019, 316, R199–R209. [Google Scholar] [CrossRef]
- Ahmad, A.; Corban, M.T.; Toya, T.; Verbrugge, F.H.; Sara, J.D.; Lerman, L.O.; Borlaug, B.A.; Lerman, A. Coronary microvascular dysfunction is associated with exertional haemodynamic abnormalities in patients with heart failure with preserved ejection fraction. Eur. J. Heart Fail. 2021, 23, 765–772. [Google Scholar] [CrossRef]
- Rush, C.J.; Berry, C.; Oldroyd, K.G.; Rocchiccioli, J.P.; Lindsay, M.M.; Touyz, R.M.; Murphy, C.L.; Ford, T.J.; Sidik, N.; McEntegart, M.B.; et al. Prevalence of Coronary Artery Disease.e and Coronary Microvascular Dysfunction in Patients With Heart Failure With Preserved Ejection Fraction. JAMA Cardiol. 2021, 6, 1130–1143. [Google Scholar] [CrossRef] [PubMed]
- Sucato, V.; Evola, S.; Novo, G.; Sansone, A.; Quagliana, A.; Andolina, G.; Assennato, P.; Novo, S. Angiographic Evaluation of Coronary Microvascular Dysfunction in Patients with Heart Failure and Preserved Ejection Fraction. Microcirculation 2015, 22, 528–533. [Google Scholar] [CrossRef] [PubMed]
- AbouEzzeddine, O.F.; Kemp, B.J.; Borlaug, B.A.; Mullan, B.P.; Behfar, A.; Pislaru, S.V.; Fudim, M.; Redfield, M.M.; Chareonthaitawee, P. Myocardial Energetics in Heart Failure With Preserved Ejection Fraction. Circ. Heart Fail. 2019, 12, e006240. [Google Scholar] [CrossRef] [PubMed]
- Srivaratharajah, K.; Coutinho, T.; deKemp, R.; Liu, P.; Haddad, H.; Stadnick, E.; Davies, R.A.; Chih, S.; Dwivedi, G.; Guo, A.; et al. Reduced Myocardial Flow in Heart Failure Patients With Preserved Ejection Fraction. Circ. Heart Fail. 2016, 9, e002562. [Google Scholar] [CrossRef]
- Taqueti, V.R.; Solomon, S.D.; Shah, A.M.; Desai, A.S.; Groarke, J.D.; Osborne, M.T.; Hainer, J.; Bibbo, C.F.; Dorbala, S.; Blankstein, R.; et al. Coronary microvascular dysfunction and future risk of heart failure with preserved ejection fraction. Eur. Heart J. 2018, 39, 840–849. [Google Scholar] [CrossRef]
- Kato, S.; Saito, N.; Kirigaya, H.; Gyotoku, D.; Iinuma, N.; Kusakawa, Y.; Iguchi, K.; Nakachi, T.; Fukui, K.; Futaki, M.; et al. Impairment of Coronary Flow Reserve Evaluated by Phase Contrast Cine-Magnetic Resonance Imaging in Patients With Heart Failure With Preserved Ejection Fraction. J. Am. Heart Assoc. 2016, 5. [Google Scholar] [CrossRef]
- Kato, S.; Fukui, K.; Kodama, S.; Azuma, M.; Nakayama, N.; Iwasawa, T.; Kimura, K.; Tamura, K.; Utsunomiya, D. Cardiovascular magnetic resonance assessment of coronary flow reserve improves risk stratification in heart failure with preserved ejection fraction. J. Cardiovasc. Magn. Reson. 2021, 23, 112. [Google Scholar] [CrossRef]
- Masci, P.G.; Pavon, A.G.; Berchier, G.; Schwitter, J. Probing the intravascular and interstitial compartments of remodeled myocardium in heart failure patients with preserved and reduced ejection fraction: A CMR study. BMC Med. Imaging 2019, 19, 1. [Google Scholar] [CrossRef]
- Mahfouz, R.A.; Gouda, M.; Abdelhamid, M. Relation of microvascular dysfunction and exercise tolerance in patients with heart failure with preserved ejection fraction. Echocardiography 2020, 37, 1192–1198. [Google Scholar] [CrossRef] [PubMed]
- Bivalacqua, T.J.; Champion, H.C.; Lambert, D.G.; Kadowitz, P.J. Vasodilator responses to adenosine and hyperemia are mediated by A1 and A2 receptors in the cat vascular bed. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2002, 282, R1696–R1709. [Google Scholar] [CrossRef] [PubMed]
- Adapala, R.K.; Talasila, P.K.; Bratz, I.N.; Zhang, D.X.; Suzuki, M.; Meszaros, J.G.; Thodeti, C.K. PKCα mediates acetylcholine-induced activation of TRPV4-dependent calcium influx in endothelial cells. Am. J. Physiol. Heart Circ. Physiol. 2011, 301, H757–H765. [Google Scholar] [CrossRef] [PubMed]
- Thodeti, C.K.; Matthews, B.; Ravi, A.; Mammoto, A.; Ghosh, K.; Bracha, A.L.; Ingber, D.E. TRPV4 Channels Mediate Cyclic Strain–Induced Endothelial Cell Reorientation Through Integrin-to-Integrin Signaling. Circ. Res. 2009, 104, 1123–1130. [Google Scholar] [CrossRef] [PubMed]
- Wilson, R.F.; Wyche, K.; Christensen, B.V.; Zimmer, S.; Laxson, D.D. Effects of adenosine on human coronary arterial circulation. Circulation 1990, 82, 1595–1606. [Google Scholar] [CrossRef] [PubMed]
- Duncker, D.J.; Bache, R.J. Regulation of Coronary Blood Flow During Exercise. Physiol. Rev. 2008, 88, 1009–1086. [Google Scholar] [CrossRef]
- Tadamura, E.; Iida, H.; Matsumoto, K.; Mamede, M.; Kubo, S.; Toyoda, H.; Shiozaki, T.; Mukai, T.; Magata, Y.; Konishi, J. Comparison of myocardial blood flow during dobutamine-atropine infusion with that after dipyridamole administration in normal men. J. Am. Coll. Cardiol. 2001, 37, 130–136. [Google Scholar] [CrossRef]
- Prior, J.O.; Quiñones, M.J.; Hernandez-Pampaloni, M.; Facta, A.D.; Schindler, T.H.; Sayre, J.W.; Hsueh, W.A.; Schelbert, H.R. Coronary Circulatory Dysfunction in Insulin Resistance, Impaired Glucose Tolerance, and Type 2 Diabetes Mellitus. Circulation 2005, 111, 2291–2298. [Google Scholar] [CrossRef]
- Cheng, D.; Talib, J.; Stanley, C.P.; Rashid, I.; Michaëlsson, E.; Lindstedt, E.-L.; Croft, K.D.; Kettle, A.J.; Maghzal, G.J.; Stocker, R. Inhibition of MPO (Myeloperoxidase) Attenuates Endothelial Dysfunction in Mouse Models of Vascular Inflammation and Atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2019, 39, 1448–1457. [Google Scholar] [CrossRef]
- Hage, C.; Michaëlsson, E.; Kull, B.; Miliotis, T.; Svedlund, S.; Linde, C.; Donal, E.; Daubert, J.-C.; Gan, L.-M.; Lund, L.H. Myeloperoxidase and related biomarkers are suggestive footprints of endothelial microvascular inflammation in HFpEF patients. ESC Heart Fail. 2020, 7, 1534–1546. [Google Scholar] [CrossRef]
- Nagele, M.P.; Barthelmes, J.; Ludovici, V.; Cantatore, S.; von Eckardstein, A.; Enseleit, F.; Luscher, T.F.; Ruschitzka, F.; Sudano, I.; Flammer, A.J. Retinal microvascular dysfunction in heart failure. Eur. Heart J. 2018, 39, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Mimoun, L.; Massin, P.; Steg, G. Retinal microvascularisation abnormalities and cardiovascular risk. Arch. Cardiovasc. Dis. 2009, 102, 449–456. [Google Scholar] [CrossRef] [PubMed]
- Cheung, N.; Bluemke, D.A.; Klein, R.; Sharrett, A.R.; Islam, F.M.; Cotch, M.F.; Klein, B.E.; Criqui, M.H.; Wong, T.Y. Retinal arteriolar narrowing and left ventricular remodeling: The multi-ethnic study of atherosclerosis. J. Am. Coll. Cardiol. 2007, 50, 48–55. [Google Scholar] [CrossRef]
- Chandra, A.; Seidelmann, S.B.; Claggett, B.L.; Klein, B.E.; Klein, R.; Shah, A.M.; Solomon, S.D. The association of retinal vessel calibres with heart failure and long-term alterations in cardiac structure and function: The Atherosclerosis Risk in Communities (ARIC) Study. Eur. J. Heart Fail. 2019, 21, 1207–1215. [Google Scholar] [CrossRef]
- Wong, T.Y.; Rosamond, W.; Chang, P.P.; Couper, D.J.; Sharrett, A.R.; Hubbard, L.D.; Folsom, A.R.; Klein, R. Retinopathy and risk of congestive heart failure. JAMA 2005, 293, 63–69. [Google Scholar] [CrossRef]
- Tromp, J.; Lim, S.L.; Tay, W.T.; Teng, T.-H.K.; Chandramouli, C.; Ouwerkerk, W.; Wander, G.S.; Sawhney, J.P.S.; Yap, J.; MacDonald, M.R.; et al. Microvascular Disease in Patients With Diabetes With Heart Failure and Reduced Ejection Versus Preserved Ejection Fraction. Diabetes Care 2019, 42, 1792. [Google Scholar] [CrossRef] [PubMed]
- Mordi, I.R.; Tee, A.; Palmer, C.N.; McCrimmon, R.J.; Doney, A.S.F.; Lang, C.C. Microvascular disease and heart failure with reduced and preserved ejection fraction in type 2 diabetes. ESC Heart Fail. 2020, 7, 1168–1177. [Google Scholar] [CrossRef] [PubMed]
- Wong, T.Y.; Islam, F.M.A.; Klein, R.; Klein, B.E.K.; Cotch, M.F.; Castro, C.; Sharrett, A.R.; Shahar, E. Retinal Vascular Caliber, Cardiovascular Risk Factors, and Inflammation: The Multi-Ethnic Study of Atherosclerosis (MESA). Investig. Ophthalmol. Vis. Sci. 2006, 47, 2341–2350. [Google Scholar] [CrossRef]
- Gutterman, D.D.; Chabowski, D.S.; Kadlec, A.O.; Durand, M.J.; Freed, J.K.; Ait-Aissa, K.; Beyer, A.M. The Human Microcirculation: Regulation of Flow and Beyond. Circ. Res. 2016, 118, 157–172. [Google Scholar] [CrossRef]
- Aird, W.C. Phenotypic heterogeneity of the endothelium: II. Representative vascular beds. Circ. Res. 2007, 100, 174–190. [Google Scholar] [CrossRef]
- Giannitsi, S.; Bougiakli, M.; Bechlioulis, A.; Naka, K. Endothelial dysfunction and heart failure: A review of the existing bibliography with emphasis on flow mediated dilation. JRSM Cardiovasc. Dis. 2019, 8, 2048004019843047. [Google Scholar] [CrossRef]
- Rosenberry, R.; Trojacek, D.; Chung, S.; Cipher, D.J.; Nelson, M.D. Interindividual differences in the ischemic stimulus and other technical considerations when assessing reactive hyperemia. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2019, 317, R530–R538. [Google Scholar] [CrossRef]
- Moerland, M.; Kales, A.J.; Schrier, L.; van Dongen, M.G.J.; Bradnock, D.; Burggraaf, J. Evaluation of the EndoPAT as a Tool to Assess Endothelial Function. Int. J. Vasc. Med. 2012, 2012, 904141. [Google Scholar] [CrossRef]
- Jakubowski, M.; Turek-Jakubowska, A.; Szahidewicz-Krupska, E.; Gawrys, K.; Gawrys, J.; Doroszko, A. Profiling the endothelial function using both peripheral artery tonometry (EndoPAT) and Laser Doppler Flowmetry (LD) - Complementary studies or waste of time? Microvasc. Res. 2020, 130, 104008. [Google Scholar] [CrossRef]
- Fukumoto, K.; Takemoto, Y.; Norioka, N.; Takahashi, K.; Namikawa, H.; Tochino, Y.; Shintani, A.; Yoshiyama, M.; Shuto, T. Predictors of the effects of smoking cessation on the endothelial function of conduit and digital vessels. Hypertens. Res. 2021, 44, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Bo’, C.D.; Campolo, J.; Porrini, M.; Fracassetti, D.; Parolini, M.; Klimis-Zacas, D.; Riso, P. Acute cigarette smoking impairs microvascular function in young moderate smokers: A potential model for studying vasoactive properties of food bioactives. PharmaNutrition 2014, 2, 1–7. [Google Scholar] [CrossRef][Green Version]
- Kiowski, W.; Linder, L.; Stoschitzky, K.; Pfisterer, M.; Burckhardt, D.; Burkart, F.; Bühler, F.R. Diminished vascular response to inhibition of endothelium-derived nitric oxide and enhanced.d vasoconstriction to exogenously administered endothelin-1 in clinically healthy smokers. Circulation 1994, 90, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Deanfield, J.E.; Halcox, J.P.; Rabelink, T.J. Endothelial function and dysfunction: Testing and clinical relevance. Circulation 2007, 115, 1285–1295. [Google Scholar] [CrossRef]
- Hamburg, N.M.; Keyes, M.J.; Larson, M.G.; Vasan, R.S.; Schnabel, R.; Pryde, M.M.; Mitchell, G.F.; Sheffy, J.; Vita, J.A.; Benjamin, E.J. Cross-sectional relations of digital vascular function to cardiovascular risk factors in the Framingham Heart Study. Circulation 2008, 117, 2467–2474. [Google Scholar] [CrossRef]
- Muris, D.M.; Houben, A.J.; Kroon, A.A.; Henry, R.M.; van der Kallen, C.J.; Sep, S.J.; Koster, A.; Dagnelie, P.C.; Schram, M.T.; Stehouwer, C.D. Age, waist circumference, and blood pressure are associated with skin microvascular flow motion: The Maastricht Study. J. Hypertens. 2014, 32, 2439–2449. [Google Scholar] [CrossRef]
- Quyyumi, A.A.; Dakak, N.; Andrews, N.P.; Gilligan, D.M.; Panza, J.A.; Cannon, R.O., 3rd. Contribution of nitric oxide to metabolic coronary vasodilation in the human heart. Circulation 1995, 92, 320–326. [Google Scholar] [CrossRef]
- Mombouli, J.V.; Vanhoutte, P.M. Endothelial dysfunction: From physiology to therapy. J. Mol. Cell Cardiol. 1999, 31, 61–74. [Google Scholar] [CrossRef]
- van Sloten, T.T.; Czernichow, S.; Houben, A.J.; Protogerou, A.D.; Henry, R.M.; Muris, D.M.; Schram, M.T.; Sep, S.J.; Dagnelie, P.C.; van der Kallen, C.J.; et al. Association Between Arterial Stiffness and Skin Microvascular Function: The SUVIMAX2 Study and The Maastricht Study. Am. J. Hypertens. 2015, 28, 868–876. [Google Scholar] [CrossRef] [PubMed]
- Haykowsky, M.J.; Kouba, E.J.; Brubaker, P.H.; Nicklas, B.J.; Eggebeen, J.; Kitzman, D.W. Skeletal muscle composition and its relation to exercise intolerance in older patients with heart failure and preserved ejection fraction. Am. J. Cardiol. 2014, 113, 1211–1216. [Google Scholar] [CrossRef] [PubMed]
- Myers, C.E.; Klein, R.; Knudtson, M.D.; Lee, K.E.; Gangnon, R.; Wong, T.Y.; Klein, B.E. Determinants of retinal venular diameter: The Beaver Dam Eye Study. Ophthalmology 2012, 119, 2563–2571. [Google Scholar] [CrossRef] [PubMed]
- Arnal, J.F.; Fontaine, C.; Billon-Gales, A.; Favre, J.; Laurell, H.; Lenfant, F.; Gourdy, P. Estrogen receptors and endothelium. Arterioscler. Thromb. Vasc. Biol. 2010, 30, 1506–1512. [Google Scholar] [CrossRef]
- Maturana, M.A.; Irigoyen, M.C.; Spritzer, P.M. Menopause, estrogens, and endothelial dysfunction: Current concepts. Clinics 2007, 62, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Sickinghe, A.A.; Korporaal, S.J.A.; den Ruijter, H.M.; Kessler, E.L. Estrogen Contributions to Microvascular Dysfunction Evolving to Heart Failure With Preserved Ejection Fraction. Front. Endocrinol. 2019, 10, 442. [Google Scholar] [CrossRef] [PubMed]
- Pepine, C.J.; Anderson, R.D.; Sharaf, B.L.; Reis, S.E.; Smith, K.M.; Handberg, E.M.; Johnson, B.D.; Sopko, G.; Bairey Merz, C.N. Coronary microvascular reactivity to adenosine predicts adverse outcome in women evaluated for suspected ischemia results from the National Heart, Lung and Blood Institute WISE (Women’s Ischemia Syndrome Evaluation) study. J. Am. Coll. Cardiol. 2010, 55, 2825–2832. [Google Scholar] [CrossRef]
- Nagele, M.P.; Barthelmes, J.; Ludovici, V.; Cantatore, S.; Frank, M.; Ruschitzka, F.; Flammer, A.J.; Sudano, I. Retinal microvascular dysfunction in hypercholesterolemia. J. Clin. Lipidol. 2018, 12, 1523–1531.e2. [Google Scholar] [CrossRef]
- Zeiher, A.M.; Drexler, H.; Wollschläger, H.; Just, H. Modulation of coronary vasomotor tone in humans. Progressive endothelial dysfunction with different early stages of coronary atherosclerosis. Circulation 1991, 83, 391–401. [Google Scholar] [CrossRef]
- Sorensen, B.M.; Houben, A.; Berendschot, T.; Schouten, J.; Kroon, A.A.; van der Kallen, C.J.H.; Henry, R.M.A.; Koster, A.; Reesink, K.D.; Dagnelie, P.C.; et al. Hyperglycemia Is the Main Mediator of Prediabetes- and Type 2 Diabetes-Associated Impairment of Microvascular Function: The Maastricht Study. Diabetes Care 2017, 40, e103–e105. [Google Scholar] [CrossRef]
- Fujimoto, K.; Hozumi, T.; Watanabe, H.; Tokai, K.; Shimada, K.; Yoshiyama, M.; Homma, S.; Yoshikawa, J. Acute hyperglycemia induced by oral glucose loading suppresses coronary microcirculation on transthoracic Doppler echocardiography in healthy young adults. Echocardiography 2006, 23, 829–834. [Google Scholar] [CrossRef] [PubMed]
- Papanek, P.E.; Rieder, M.J.; Lombard, J.H.; Greene, A.S. Gender-specific protection from microvessel rarefaction in female hypertensive rats. Am. J. Hypertens. 1998, 11, 998–1005. [Google Scholar] [CrossRef][Green Version]
- Noon, J.P.; Walker, B.R.; Webb, D.J.; Shore, A.C.; Holton, D.W.; Edwards, H.V.; Watt, G.C. Impaired microvascular dilatation and capillary rarefaction in young adults with a predisposition to high blood pressure. J. Clin. Investig. 1997, 99, 1873–1879. [Google Scholar] [CrossRef]
- Melik, Z.; Princi, T.; Grill, V.; Cankar, K. The effect of caffeine on cutaneous postocclusive reactive hyperaemia. PLoS ONE 2019, 14, e0214919. [Google Scholar] [CrossRef] [PubMed]
- van Haare, J.; Kooi, M.E.; Vink, H.; Post, M.J.; van Teeffelen, J.J.W.; Slenter, J.; Munts, C.; Cobelens, H.; Strijkers, G.J.; Koehn, D.; et al. Early impairment of coronary microvascular perfusion capacity in rats on a high fat diet. Cardiovasc. Diabetol. 2015, 14, 150. [Google Scholar] [CrossRef]
- Maranhao, P.A.; de Souza, M.; Panazzolo, D.G.; Nogueira Neto, J.F.; Bouskela, E.; Kraemer-Aguiar, L.G. Metabolic Changes Induced by High-Fat Meal Evoke Different Microvascular Responses in Accordance with Adiposity Status. Biomed. Res. Int. 2018, 2018, 5046508. [Google Scholar] [CrossRef] [PubMed]
- Demiot, C.; Dignat-George, F.; Fortrat, J.O.; Sabatier, F.; Gharib, C.; Larina, I.; Gauquelin-Koch, G.; Hughson, R.; Custaud, M.A. WISE 2005: Chronic bed rest impairs microcirculatory endothelium in women. Am. J. Physiol. Heart Circ. Physiol. 2007, 293, H3159–H3164. [Google Scholar] [CrossRef]
- Lanting, S.M.; Johnson, N.A.; Baker, M.K.; Caterson, I.D.; Chuter, V.H. The effect of exercise training on cutaneous microvascular reactivity: A systematic review and meta-analysis. J. Sci. Med. Sport 2017, 20, 170–177. [Google Scholar] [CrossRef]
- Streese, L.; Khan, A.W.; Deiseroth, A.; Hussain, S.; Suades, R.; Tiaden, A.; Kyburz, D.; Cosentino, F.; Hanssen, H. High-intensity interval training modulates retinal microvascular phenotype and DNA methylation of p66Shc gene: A randomized controlled trial (EXAMIN AGE). Eur. Heart J. 2020, 41, 1514–1519. [Google Scholar] [CrossRef] [PubMed]
- Shankar, A.; Sabanayagam, C.; Klein, B.E.K.; Klein, R. Retinal Microvascular Changes and the Risk of Developing Obesity: Population-Based Cohort Study. Microcirculation 2011, 18, 655–662. [Google Scholar] [CrossRef] [PubMed]
- Joris, P.J.; Plat, J.; Kusters, Y.H.; Houben, A.J.; Stehouwer, C.C.D.; Schalkwijk, C.G.; Mensink, R.P. Diet-induced weight loss improves not only cardiometabolic risk markers but also markers of vascular function: A randomized controlled trial in abdominally obese men. Am. J. Clin. Nutr. 2017, 105, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Huxley, V.H.; Kemp, S.S. Sex-Specific Characteristics of the Microcirculation. Adv. Exp. Med. Biol. 2018, 1065, 307–328. [Google Scholar] [CrossRef]
- Kobayashi, Y.; Fearon, W.F.; Honda, Y.; Tanaka, S.; Pargaonkar, V.; Fitzgerald, P.J.; Lee, D.P.; Stefanick, M.; Yeung, A.C.; Tremmel, J.A. Effect of Sex Differences on Invasive Measures of Coronary Microvascular Dysfunction in Patients With Angina in the Absence of Obstructive Coronary Artery Disease. JACC Cardiovasc. Interv. 2015, 8, 1433–1441. [Google Scholar] [CrossRef]
- Rooks, C.; Faber, T.; Votaw, J.; Veledar, E.; Goldberg, J.; Raggi, P.; Quyyumi, A.A.; Bremner, J.D.; Vaccarino, V. Effects of smoking on coronary microcirculatory function: A twin study. Atherosclerosis 2011, 215, 500–506. [Google Scholar] [CrossRef]
- Espino-Gonzalez, E.; Tickle, P.G.; Benson, A.P.; Kissane, R.W.P.; Askew, G.N.; Egginton, S.; Bowen, T.S. Abnormal skeletal muscle blood flow, contractile mechanics and fibre morphology in a rat model of obese-HFpEF. J. Physiol. 2021, 599, 981–1001. [Google Scholar] [CrossRef]
- Bhella, P.S.; Prasad, A.; Heinicke, K.; Hastings, J.L.; Arbab-Zadeh, A.; Adams-Huet, B.; Pacini, E.L.; Shibata, S.; Palmer, M.D.; Newcomer, B.R.; et al. Abnormal haemodynamic response to exercise in heart failure with preserved ejection fraction. Eur. J. Heart Fail. 2011, 13, 1296–1304. [Google Scholar] [CrossRef]
- Dhakal, B.P.; Malhotra, R.; Murphy, R.M.; Pappagianopoulos, P.P.; Baggish, A.L.; Weiner, R.B.; Houstis, N.E.; Eisman, A.S.; Hough, S.S.; Lewis, G.D. Mechanisms of exercise intolerance in heart failure with preserved ejection fraction: The role of abnormal peripheral oxygen extraction. Circ. Heart Fail. 2015, 8, 286–294. [Google Scholar] [CrossRef]
- Biegus, J.; Niewinski, P.; Josiak, K.; Kulej, K.; Ponikowska, B.; Nowak, K.; Zymlinski, R.; Ponikowski, P. Pathophysiology of Advanced Heart Failure: What Knowledge Is Needed fo.......or Clinical Management? Heart Fail. Clin. 2021, 17, 519–531. [Google Scholar] [CrossRef]
- Hartupee, J.; Mann, D.L. Neurohormonal activation in heart failure with reduced ejection fraction. Nat. Rev. Cardiol. 2017, 14, 30–38. [Google Scholar] [CrossRef]
- Phan, T.T.; Abozguia, K.; Nallur Shivu, G.; Mahadevan, G.; Ahmed, I.; Williams, L.; Dwivedi, G.; Patel, K.; Steendijk, P.; Ashrafian, H.; et al. Heart failure with preserved ejection fraction is characterized by dynamic impairment of active relaxation and contraction of the left ventricle on exercise and associated with myocardial energy deficiency. J. Am. Coll. Cardiol. 2009, 54, 402–409. [Google Scholar] [CrossRef]
- Serné, E.H.; Gans, R.O.; ter Maaten, J.C.; Tangelder, G.J.; Donker, A.J.; Stehouwer, C.D. Impaired skin capillary recruitment in essential hypertension is caused by both functional and structural capillary rarefaction. Hypertension 2001, 38, 238–242. [Google Scholar] [CrossRef]
- Wolinsky, H. A proposal linking clearance of circulating lipoproteins to tissue metabolic activity as a basis for understanding atherogenesis. Circ. Res. 1980, 47, 301–311. [Google Scholar] [CrossRef] [PubMed]
- Meijers, W.C.; van der Velde, A.R.; de Boer, R.A. Biomarkers in heart failure with preserved ejection fraction. Neth. Heart J. 2016, 24, 252–258. [Google Scholar] [CrossRef]
- Carnes, J.; Gordon, G. Biomarkers in Heart Failure With Preserved Ejection Fraction: An Update on Progress and Future Challenges. Heart Lung Circ. 2020, 29, 62–68. [Google Scholar] [CrossRef]
- Mantovani, A.; Dejana, E. Endothelium. In Encyclopedia of Immunology; Delves, P.J., Ed.; Elsevier: Oxford, UK, 1998; pp. 802–806. [Google Scholar]
- Westermann, D.; Lindner, D.; Kasner, M.; Zietsch, C.; Savvatis, K.; Escher, F.; von Schlippenbach, J.; Skurk, C.; Steendijk, P.; Riad, A.; et al. Cardiac inflammation contributes to changes in the extracellular matrix in patients with heart failure and normal ejection fraction. Circ. Heart Fail. 2011, 4, 44–52. [Google Scholar] [CrossRef]
- Patel, R.B.; Colangelo, L.A.; Reiner, A.P.; Gross, M.D.; Jacobs, D.R., Jr.; Launer, L.J.; Lima, J.A.C.; Lloyd-Jones, D.M.; Shah, S.J. Cellular Adhesion Molecules in Young Adulthood and Cardiac Function in Later Life. J. Am. Coll. Cardiol. 2020, 75, 2156–2165. [Google Scholar] [CrossRef] [PubMed]
- Patel, R.B.; Colangelo, L.A.; Bielinski, S.J.; Larson, N.B.; Ding, J.; Allen, N.B.; Michos, E.D.; Shah, S.J.; Lloyd-Jones, D.M. Circulating Vascular Cell Adhesion Molecule-1 and Incident Heart Failure: The Multi-Ethnic Study of Atherosclerosis (MESA). J. Am. Heart Assoc. 2020, 9, e019390. [Google Scholar] [CrossRef]
- Kleber, M.E.; Koller, L.; Goliasch, G.; Sulzgruber, P.; Scharnagl, H.; Silbernagel, G.; Grammer, T.B.; Delgado, G.; Tomaschitz, A.; Pilz, S.; et al. Von Willebrand factor improves risk prediction in addition to N-terminal pro-B-type natriuretic peptide in patients referred to coronary angiography and signs and symptoms of heart failure and preserved ejection fraction. Circ. Heart Fail. 2015, 8, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Rack, K.; Huck, V.; Hoore, M.; Fedosov, D.A.; Schneider, S.W.; Gompper, G. Margination and stretching of von Willebrand factor in the blood stream enable adhesion. Sci. Rep. 2017, 7, 14278. [Google Scholar] [CrossRef]
- Creemers, E.E.; Tijsen, A.J.; Pinto, Y.M. Circulating microRNAs: Novel biomarkers and extracellular communicators in cardiovascular disease? Circ. Res. 2012, 110, 483–495. [Google Scholar] [CrossRef] [PubMed]
- Eissa, S.; Matboli, M.; Bekhet, M.M. Clinical verification of a novel urinary microRNA panal: 133b, -342 and -30 as biomarkers for diabetic nephropathy identified by bioinformatics analysis. Biomed. Pharmacother. 2016, 83, 92–99. [Google Scholar] [CrossRef]
- Mazzeo, A.; Lopatina, T.; Gai, C.; Trento, M.; Porta, M.; Beltramo, E. Functional analysis of miR-21-3p, miR-30b-5p and miR-150-5p shuttled by extracellular vesicles from diabetic subjects reveals their association with diabetic retinopathy. Exp. Eye Res. 2019, 184, 56–63. [Google Scholar] [CrossRef]
- Juni, R.P.; Al-Shama, R.; Kuster, D.W.D.; van der Velden, J.; Hamer, H.M.; Vervloet, M.G.; Eringa, E.C.; Koolwijk, P.; van Hinsbergh, V.W.M. Empagliflozin restores chronic kidney disease–induced impairment of endothelial regulation of cardiomyocyte relaxation and contraction. Kidney. Int. 2021, 99, 1088–1101. [Google Scholar] [CrossRef]
- Schmitter, D.; Voors, A.A.; van der Harst, P. HFpEF vs. HFrEF: Can microRNAs advance the diagnosis? Eur. J. Heart Fail. 2015, 17, 351–354. [Google Scholar] [CrossRef] [PubMed]
- Florijn, B.W.; Valstar, G.B.; Duijs, J.M.G.J.; Menken, R.; Cramer, M.J.; Teske, A.J.; Ghossein-Doha, C.; Rutten, F.H.; Spaanderman, M.E.A.; den Ruijter, H.M.; et al. Sex-specific microRNAs in women with diabetes and left ventricular diastolic dysfunction or HFpEF associate with microvascular injury. Sci. Rep. 2020, 10, 13945. [Google Scholar] [CrossRef] [PubMed]
- Florijn, B.W.; Bijkerk, R.; van der Veer, E.P.; van Zonneveld, A.J. Gender and cardiovascular disease: Are sex-biased microRNA networks a driving force behind heart failure with preserved ejection fraction in women? Cardiovasc. Res. 2018, 114, 210–225. [Google Scholar] [CrossRef]
- Wei, J.; Nelson, M.D.; Szczepaniak, E.W.; Smith, L.; Mehta, P.K.; Thomson, L.E.; Berman, D.S.; Li, D.; Bairey Merz, C.N.; Szczepaniak, L.S. Myocardial steatosis as a possible mechanistic link between diastolic dysfunction and coronary microvascular dysfunction in women. Am. J. Physiol. Heart Circ. Physiol. 2016, 310, H14–H19. [Google Scholar] [CrossRef]
- Mahmod, M.; Pal, N.; Holloway, C.; Ferreira, V.M.; Dass, S.; Francis, J.M.; Rider, O.; Karamitsos, T.D.; Ashrafian, H.; Neubauer, S. Cardiac steatosis and left ventricular remodeling in heart failure with reduced and preserved ejection fraction. J. Cardiovasc. Magn. Reson. 2015, 17, P309. [Google Scholar] [CrossRef]
- Packer, M. Epicardial Adipose Tissue May Mediate Deleterious Effects of Obesity and Inflammation on the Myocardium. J. Am. Coll. Cardiol. 2018, 71, 2360–2372. [Google Scholar] [CrossRef]
- Mahmod, M.; Pal, N.; Rayner, J.; Holloway, C.; Raman, B.; Dass, S.; Levelt, E.; Ariga, R.; Ferreira, V.; Banerjee, R.; et al. The interplay between metabolic alterations, diastolic strain rate and exercise capacity in mild heart failure with preserved ejection fraction: A cardiovascular magnetic resonance study. J. Cardiovasc. Magn. Reson. 2018, 20, 88. [Google Scholar] [CrossRef]
- Valero-Munoz, M.; Li, S.; Wilson, R.M.; Hulsmans, M.; Aprahamian, T.; Fuster, J.J.; Nahrendorf, M.; Scherer, P.E.; Sam, F. Heart Failure With Preserved Ejection Fraction Induces Beiging in Adipose Tissue. Circ. Heart Fail. 2016, 9, e002724. [Google Scholar] [CrossRef]
- Koepp, K.E.; Obokata, M.; Reddy, Y.N.V.; Olson, T.P.; Borlaug, B.A. Hemodynamic and Functional Impact of Epicardial Adipose Tissue in Heart Failure With Preserved Ejection Fraction. Heart Fail. 2020, 8, 657–666. [Google Scholar] [CrossRef]
- Tilg, H.; Moschen, A.R. Adipocytokines: Mediators linking adipose tissue, inflammation and immunity. Nat. Rev. Immunol. 2006, 6, 772–783. [Google Scholar] [CrossRef] [PubMed]
- Antonopoulos, A.S.; Sanna, F.; Sabharwal, N.; Thomas, S.; Oikonomou, E.K.; Herdman, L.; Margaritis, M.; Shirodaria, C.; Kampoli, A.M.; Akoumianakis, I.; et al. Detecting human coronary inflammation by imaging perivascular fat. Sci. Transl. Med. 2017, 9. [Google Scholar] [CrossRef]
- Greenstein, A.S.; Khavandi, K.; Withers, S.B.; Sonoyama, K.; Clancy, O.; Jeziorska, M.; Laing, I.; Yates, A.P.; Pemberton, P.W.; Malik, R.A.; et al. Local Inflammation and Hypoxia Abolish the Protective Anticontractile Properties of Perivascular Fat in Obese Patients. Circulation 2009, 119, 1661–1670. [Google Scholar] [CrossRef]
- Meijer, R.I.; Bakker, W.; Alta, C.L.; Sipkema, P.; Yudkin, J.S.; Viollet, B.; Richter, E.A.; Smulders, Y.M.; van Hinsbergh, V.W.; Serné, E.H.; et al. Perivascular adipose tissue control of insulin-induced vasoreactivity in muscle is impaired in db/db mice. Diabetes 2013, 62, 590–598. [Google Scholar] [CrossRef] [PubMed]
- Withers, S.B.; Forman, R.; Meza-Perez, S.; Sorobetea, D.; Sitnik, K.; Hopwood, T.; Lawrence, C.B.; Agace, W.W.; Else, K.J.; Heagerty, A.M.; et al. Eosinophils are key regulators of perivascular adipose tissue and vascular functionality. Sci. Rep. 2017, 7, 44571. [Google Scholar] [CrossRef] [PubMed]
- Withers, S.B.; Agabiti-Rosei, C.; Livingstone, D.M.; Little, M.C.; Aslam, R.; Malik, R.A.; Heagerty, A.M. Macrophage activation is responsible for loss of anticontractile function in inflamed perivascular fat. Arterioscler. Thromb. Vasc. Biol. 2011, 31, 908–913. [Google Scholar] [CrossRef] [PubMed]
- Meijer, R.I.; Hoevenaars, F.P.M.; Serné, E.H.; Yudkin, J.S.; Kokhuis, T.J.A.; Weijers, E.M.; van Hinsbergh, V.W.M.; Smulders, Y.M.; Eringa, E.C. JNK2 in myeloid cells impairs insulin’s vasodilator effects in muscle during early obesity development through perivascular adipose tissue dysfunction. Am. J. Physiol. Heart Circ. Physiol. 2019, 317, H364–H374. [Google Scholar] [CrossRef] [PubMed]
- Turaihi, A.H.; Serné, E.H.; Molthoff, C.F.M.; Koning, J.J.; Knnol, J.; Niessen, H.W.; Goumans, M.J.T.H.; van Poelgeest, E.M.; Yudkin, J.S.; Smulders, Y.M.; et al. Perivascular Adipose Tissue Controls Insulin-Stimulated Perfusion, Mitochondrial Protein Expression, and Glucose Uptake in Muscle Through Adipomuscular Arterioles. Diabetes 2020, 69, 603. [Google Scholar] [CrossRef] [PubMed]
- Ayton, S.L.; Gulsin, G.S.; McCann, G.P.; Moss, A.J. Epicardial adipose tissue in obesity-related cardiac dysfunction. Heart 2021. [Google Scholar] [CrossRef]
- Pugliese, N.R.; Paneni, F.; Mazzola, M.; De Biase, N.; Del Punta, L.; Gargani, L.; Mengozzi, A.; Virdis, A.; Nesti, L.; Taddei, S.; et al. Impact of epicardial adipose tissue on cardiovascular haemodynamics, metabolic profile, and prognosis in heart failure. Eur. J. Heart Fail. 2021, 23, 1858–1871. [Google Scholar] [CrossRef] [PubMed]
- Ying, W.; Sharma, K.; Yanek, L.R.; Vaidya, D.; Schär, M.; Markl, M.; Subramanya, V.; Soleimani, S.; Ouyang, P.; Michos, E.D.; et al. Visceral adiposity, muscle composition, and exercise tolerance in heart failure with preserved ejection fraction. ESC Heart Fail. 2021, 8, 2535–2545. [Google Scholar] [CrossRef]
- van Woerden, G.; van Veldhuisen, D.J.; Gorter, T.M.; van Empel, V.P.M.; Hemels, M.E.W.; Hazebroek, E.J.; van Veldhuisen, S.L.; Willems, T.P.; Rienstra, M.; Westenbrink, B.D. Importance of epicardial adipose tissue localization using cardiac magnetic resonance imaging in patients with heart failure with mid-range and preserved ejection fraction. Clin. Cardiol. 2021, 44, 987–993. [Google Scholar] [CrossRef]
- Sorimachi, H.; Obokata, M.; Takahashi, N.; Reddy, Y.N.V.; Jain, C.C.; Verbrugge, F.H.; Koepp, K.E.; Khosla, S.; Jensen, M.D.; Borlaug, B.A. Pathophysiologic importance of visceral adipose tissue in women with heart failure and preserved ejection fraction. Eur. Heart J. 2021, 42, 1595–1605. [Google Scholar] [CrossRef]
- Packer, M.; Lam, C.S.P.; Lund, L.H.; Maurer, M.S.; Borlaug, B.A. Characterization of the inflammatory-metabolic phenotype of heart failure with a preserved ejection fraction: A hypothesis to explain influence of sex on the evolution and potential treatment of the disease. Eur. J. Heart Fail. 2020, 22, 1551–1567. [Google Scholar] [CrossRef]
- White, U.A.; Tchoukalova, Y.D. Sex dimorphism and depot differences in adipose tissue function. Biochim. Biophys. Acta. Mol. Basis Dis. 2014, 1842, 377–392. [Google Scholar] [CrossRef]
- Lyle, M.A.; Alabdaljabar, M.S.; Han, Y.S.; Brozovich, F.V. The. vasculature in HFpEF vs HFrEF: Differences in contractile protein expression produce distinct phenotypes. Heliyon 2020, 6, e03129. [Google Scholar] [CrossRef]
- Hahn, V.S.; Yanek, L.R.; Vaishnav, J.; Ying, W.; Vaidya, D.; Lee, Y.Z.J.; Riley, S.J.; Subramanya, V.; Brown, E.E.; Hopkins, C.D.; et al. Endomyocardial Biopsy Characterization of Heart Failure With Preserved Ejection Fraction and Prevalence of Cardiac Amyloidosis. JACC Heart Fail. 2020, 8, 712–724. [Google Scholar] [CrossRef]
- Conceicao, G.; Heinonen, I.; Lourenco, A.P.; Duncker, D.J.; Falcao-Pires, I. Animal models of heart failure with preserved ejection fraction. Neth. Heart J. 2016, 24, 275–286. [Google Scholar] [CrossRef] [PubMed]
- Gevaert, A.B.; Shakeri, H.; Leloup, A.J.; Van Hove, C.E.; De Meyer, G.R.Y.; Vrints, C.J.; Lemmens, K.; Van Craenenbroeck, E.M. Endothelial Senescence Contributes to Heart Failure With Preserved Ejection Fraction in an Aging Mouse Model. Circ. Heart Fail. 2017, 10, e003806. [Google Scholar] [CrossRef] [PubMed]
- Kolijn, D.; Pabel, S.; Tian, Y.; Lódi, M.; Herwig, M.; Carrizzo, A.; Zhazykbayeva, S.; Kovács, Á.; Fülöp, G.Á.; Falcão-Pires, I.; et al. Empagliflozin improves endothelial and cardiomyocyte function in human heart failure with preserved ejection fraction via reduced pro-inflammatory-oxidative pathways and protein kinase Gα oxidation. Cardiovasc. Res. 2021, 117, 495–507. [Google Scholar] [CrossRef]
- Juni, R.P.; Kuster, D.W.D.; Goebel, M.; Helmes, M.; Musters, R.J.P.; van der Velden, J.; Koolwijk, P.; Paulus, W.J.; van Hinsbergh, V.W.M. Cardiac Microvascular Endothelial Enhancement of Cardiomyocyte Function Is Impaired by Inflammation and Restored by Empagliflozin. JACC Basic Transl. Sci. 2019, 4, 575–591. [Google Scholar] [CrossRef] [PubMed]
- Verloop, W.L.; Beeftink, M.M.; Santema, B.T.; Bots, M.L.; Blankestijn, P.J.; Cramer, M.J.; Doevendans, P.A.; Voskuil, M. A systematic review concerning the relation between the sympathetic nervous system and heart failure with preserved left ventricular ejection fraction. PLoS ONE 2015, 10, e0117332. [Google Scholar] [CrossRef] [PubMed]
- Mancia, G.; Grassi, G. The autonomic nervous system and hypertension. Circ. Res. 2014, 114, 1804–1814. [Google Scholar] [CrossRef]
- Kristensen, S.L.; Jhund, P.S.; Lee, M.M.Y.; Kober, L.; Solomon, S.D.; Granger, C.B.; Yusuf, S.; Pfeffer, M.A.; Swedberg, K.; McMurray, J.J.V.; et al. Prevalence of Prediabetes and Undiagnosed Diabetes in Patients with HFpEF and HFrEF and Associated Clinical Outcomes. Cardiovasc. Drugs Ther. 2017, 31, 545–549. [Google Scholar] [CrossRef]
- Waddingham, M.T.; Sonobe, T.; Tsuchimochi, H.; Edgley, A.J.; Sukumaran, V.; Chen, Y.C.; Hansra, S.S.; Schwenke, D.O.; Umetani, K.; Aoyama, K.; et al. Diastolic dysfunction is initiated by cardiomyocyte impairment ahead of endothelial dysfunction due to increased oxidative stress and inflammation in an experimental prediabetes model. J. Mol. Cell Cardiol. 2019, 137, 119–131. [Google Scholar] [CrossRef] [PubMed]
- Otto, M.; Brabenec, L.; Müller, M.; Kintrup, S.; Hellenthal, K.E.M.; Holtmeier, R.; Steinbuch, S.C.; Karsten, O.S.; Pryvalov, H.; Rossaint, J.; et al. Development of heart failure with preserved ejection fraction in type 2 diabetic mice is ameliorated by preserving vascular function. Life Sci. 2021, 284, 119925. [Google Scholar] [CrossRef] [PubMed]
- Schiattarella, G.G.; Altamirano, F.; Tong, D.; French, K.M.; Villalobos, E.; Kim, S.Y.; Luo, X.; Jiang, N.; May, H.I.; Wang, Z.V.; et al. Nitrosative stress drives heart failure with preserved ejection fraction. Nature 2019, 568, 351–356. [Google Scholar] [CrossRef] [PubMed]
- Pieske, B.; Maggioni, A.P.; Lam, C.S.P.; Pieske-Kraigher, E.; Filippatos, G.; Butler, J.; Ponikowski, P.; Shah, S.J.; Solomon, S.D.; Scalise, A.V.; et al. Vericiguat in patients with worsening chronic heart failure and preserved ejection fraction: Results of the SOluble guanylate Cyclase stimulatoR in heArT failurE patientS with PRESERVED EF (SOCRATES-PRESERVED) study. Eur. Heart J. 2017, 38, 1119–1127. [Google Scholar] [CrossRef] [PubMed]
- Ejiri, K.; Miyoshi, T.; Kihara, H.; Hata, Y.; Nagano, T.; Takaishi, A.; Toda, H.; Nanba, S.; Nakamura, Y.; Akagi, S.; et al. Effect of Luseogliflozin on Heart Failure With Preserved Ejection Fraction in Patients With Diabetes Mellitus. J. Am. Heart Assoc. 2020, 9, e015103. [Google Scholar] [CrossRef] [PubMed]
- Solomon, S.D.; Zile, M.; Pieske, B.; Voors, A.; Shah, A.; Kraigher-Krainer, E.; Shi, V.; Bransford, T.; Takeuchi, M.; Gong, J.; et al. The angiotensin receptor neprilysin inhibitor LCZ696 in heart failure with preserved ejection fraction: A phase 2 double-blind randomised controlled trial. Lancet 2012, 380, 1387–1395. [Google Scholar] [CrossRef]
- Redfield, M.M.; Chen, H.H.; Borlaug, B.A.; Semigran, M.J.; Lee, K.L.; Lewis, G.; LeWinter, M.M.; Rouleau, J.L.; Bull, D.A.; Mann, D.L.; et al. Effect of phosphodiesterase-5 inhibition on exercise capacity and clinical status in heart failure with preserved ejection fraction: A randomized clinical trial. JAMA 2013, 309, 1268–1277. [Google Scholar] [CrossRef]
- Redfield, M.M.; Anstrom, K.J.; Levine, J.A.; Koepp, G.A.; Borlaug, B.A.; Chen, H.H.; LeWinter, M.M.; Joseph, S.M.; Shah, S.J.; Semigran, M.J.; et al. Isosorbide Mononitrate in Heart Failure with Preserved Ejection Fraction. N. Engl. J. Med. 2015, 373, 2314–2324. [Google Scholar] [CrossRef]
- Patel, R.B.; Shah, S.J. Drug Targets for Heart Failure with Preserved Ejection Fraction: A Mechanistic Approach and Review of Contemporary Clinical Trials. Annu. Rev. Pharmacol. Toxicol. 2019, 59, 41–63. [Google Scholar] [CrossRef]
- Sorensen, B.M.; Houben, A.J.; Berendschot, T.T.; Schouten, J.S.; Kroon, A.A.; van der Kallen, C.J.; Henry, R.M.; Koster, A.; Sep, S.J.; Dagnelie, P.C.; et al. Prediabetes and Type 2 Diabetes Are Associated With Generalized Microvascular Dysfunction: The Maastricht Study. Circulation 2016, 134, 1339–1352. [Google Scholar] [CrossRef]
- Stehouwer, C.D.A. Microvascular Dysfunction and Hyperglycemia: A Vicious Cycle With Widespread Consequences. Diabetes 2018, 67, 1729. [Google Scholar] [CrossRef]
- Adingupu, D.D.; Gopel, S.O.; Gronros, J.; Behrendt, M.; Sotak, M.; Miliotis, T.; Dahlqvist, U.; Gan, L.M.; Jonsson-Rylander, A.C. SGLT2 inhibition with empagliflozin improves coronary microvascular function and cardiac contractility in prediabetic ob/ob(-/-) mice. Cardiovasc. Diabetol. 2019, 18, 16. [Google Scholar] [CrossRef]
- Zinman, B.; Wanner, C.; Lachin, J.M.; Fitchett, D.; Bluhmki, E.; Hantel, S.; Mattheus, M.; Devins, T.; Johansen, O.E.; Woerle, H.J.; et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N. Engl. J. Med. 2015, 373, 2117–2128. [Google Scholar] [CrossRef] [PubMed]
- Anker, S.D.; Butler, J.; Filippatos, G.; Ferreira, J.P.; Bocchi, E.; Böhm, M.; Brunner–La Rocca, H.-P.; Choi, D.-J.; Chopra, V.; Chuquiure-Valenzuela, E.; et al. Empagliflozin in Heart Failure with a Preserved Ejection Fraction. N. Engl. J. Med. 2021, 385, 1451–1461. [Google Scholar] [CrossRef] [PubMed]
- Xue, M.; Li, T.; Wang, Y.; Chang, Y.; Cheng, Y.; Lu, Y.; Liu, X.; Xu, L.; Li, X.; Yu, X.; et al. Empagliflozin prevents cardiomyopathy via sGC-cGMP-PKG pathway in type 2 diabetes mice. Clin. Sci 2019, 133, 1705–1720. [Google Scholar] [CrossRef] [PubMed]
- Solomon, S.D.; McMurray, J.J.V.; Anand, I.S.; Ge, J.; Lam, C.S.P.; Maggioni, A.P.; Martinez, F.; Packer, M.; Pfeffer, M.A.; Pieske, B.; et al. Angiotensin-Neprilysin Inhibition in Heart Failure with Preserved Ejection Fraction. N. Engl. J. Med. 2019, 381, 1609–1620. [Google Scholar] [CrossRef]
- Mátyás, C.; Németh, B.T.; Oláh, A.; Török, M.; Ruppert, M.; Kellermayer, D.; Barta, B.A.; Szabó, G.; Kökény, G.; Horváth, E.M.; et al. Prevention of the development of heart failure with preserved ejection fraction by the phosphodiesterase-5A inhibitor vardenafil in rats with type 2 diabetes. Eur. J. Heart Fail. 2017, 19, 326–336. [Google Scholar] [CrossRef]
- D’Amario, D.; Migliaro, S.; Borovac, J.A.; Restivo, A.; Vergallo, R.; Galli, M.; Leone, A.M.; Montone, R.A.; Niccoli, G.; Aspromonte, N.; et al. Microvascular Dysfunction in Heart Failure With Preserved Ejection Fraction. Front. Physiol. 2019, 10, 1347. [Google Scholar] [CrossRef]
- Borlaug, B.A.; Lewis, G.D.; McNulty, S.E.; Semigran, M.J.; LeWinter, M.; Chen, H.; Lin, G.; Deswal, A.; Margulies, K.B.; Redfield, M.M. Effects of sildenafil on ventricular and vascular function in heart failure with preserved ejection fraction. Circ. Heart Fail. 2015, 8, 533–541. [Google Scholar] [CrossRef]
- Debevec, T.; Millet, G.P.; Pialoux, V. Hypoxia-Induced Oxidative Stress Modulation with Physical Activity. Front. Physiol. 2017, 8, 84. [Google Scholar] [CrossRef]
- Zamani, P.; Rawat, D.; Shiva-Kumar, P.; Geraci, S.; Bhuva, R.; Konda, P.; Doulias, P.T.; Ischiropoulos, H.; Townsend, R.R.; Margulies, K.B.; et al. Effect of inorganic nitrate on exercise capacity in heart failure with preserved ejection fraction. Circulation 2015, 131, 371–380. [Google Scholar] [CrossRef]
- Maher, A.R.; Milsom, A.B.; Gunaruwan, P.; Abozguia, K.; Ahmed, I.; Weaver, R.A.; Thomas, P.; Ashrafian, H.; Born, G.V.; James, P.E.; et al. Hypoxic modulation of exogenous nitrite-induced vasodilation in humans. Circulation 2008, 117, 670–677. [Google Scholar] [CrossRef]
- Borlaug, B.A.; Koepp, K.E.; Melenovsky, V. Sodium Nitrite Improves Exercise Hemodynamics and Ventricular Performance in Heart Failure With Preserved Ejection Fraction. J. Am. Coll. Cardiol. 2015, 66, 1672–1682. [Google Scholar] [CrossRef]
- Borlaug, B.A.; Anstrom, K.J.; Lewis, G.D.; Shah, S.J.; Levine, J.A.; Koepp, G.A.; Givertz, M.M.; Felker, G.M.; LeWinter, M.M.; Mann, D.L.; et al. Effect of Inorganic Nitrite vs Placebo on Exercise Capacity Among Patients With Heart Failure With Preserved Ejection Fraction: The INDIE-HFpEF Randomized Clinical Trial. JAMA 2018, 320, 1764–1773. [Google Scholar] [CrossRef]
- Schwartzenberg, S.; Redfield, M.M.; From, A.M.; Sorajja, P.; Nishimura, R.A.; Borlaug, B.A. Effects of Vasodilation in Heart Failure With Preserved or Reduced Ejection Fraction: Implications of Distinct Pathophysiologies on Response to Therapy. J. Am. Coll. Cardiol. 2012, 59, 442–451. [Google Scholar] [CrossRef] [PubMed]
- Fukuta, H. Effects of Exercise Training on Cardiac Function in Heart Failure with Preserved Ejection Fraction. Card. Fail. Rev. 2020, 6, e27. [Google Scholar] [CrossRef] [PubMed]
- Tucker, W.J.; Angadi, S.S.; Haykowsky, M.J.; Nelson, M.D.; Sarma, S.; Tomczak, C.R. Pathophysiology of Exercise Intolerance and Its Treatment With Exercise-Based Cardiac Rehabilitation in Heart Failure With Preserved Ejection Fraction. J. Cardiopulm. Rehabil. Prev. 2020, 40, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Fu, T.C.; Yang, N.I.; Wang, C.H.; Cherng, W.J.; Chou, S.L.; Pan, T.L.; Wang, J.S. Aerobic Interval Training Elicits Different Hemodynamic Adaptations Between Heart Failure Patients with Preserved and Reduced Ejection Fraction. Am. J. Phys. Med. Rehabil. 2016, 95, 15–27. [Google Scholar] [CrossRef]
- Shear, F.E. Novel paradigms in the therapeutic management of heart failure with preserved ejection fraction: Clinical perspectives. Am. J. Cardiovasc. Dis. 2019, 9, 91–108. [Google Scholar] [PubMed]
- De Keulenaer, G.W.; Segers, V.F.M.; Zannad, F.; Brutsaert, D.L. The future of pleiotropic therapy in heart failure. Lessons from the benefits of exercise training on endothelial function. Eur. J. Heart Fail. 2017, 19, 603–614. [Google Scholar] [CrossRef]
- Withaar, C.; Lam, C.S.P.; Schiattarella, G.G.; de Boer, R.A.; Meems, L.M.G. Heart failure with preserved ejection fraction in humans and mice: Embracing clinical complexity in mouse models. Eur. Heart J. 2021, 42, 4420–4430. [Google Scholar] [CrossRef]
- Johnson, P.C. Introduction. In Comprehensive Physiology; Pollock, D.M., Ed.; American Physiological Society: Rockville, MD, USA, 2011. [Google Scholar] [CrossRef]
- Clapauch, R.; Mecenas, A.S.; Maranhao, P.A.; Bouskela, E. Microcirculatory function in postmenopausal women: Role of aging, hormonal exposure and metabolic syndrome. Microvasc. Res. 2009, 78, 405–412. [Google Scholar] [CrossRef]
- Miller, V.M. Gender and vascular reactivity. Lupus 1999, 8, 409–415. [Google Scholar] [CrossRef]
- Scotland, R.S.; Madhani, M.; Chauhan, S.; Moncada, S.; Andresen, J.; Nilsson, H.; Hobbs, A.J.; Ahluwalia, A. Investigation of vascular responses in endothelial nitric oxide synthase/cyclooxygenase-1 double-knockout mice: Key role for endothelium-derived hyperpolarizing factor in the regulation of blood pressure in vivo. Circulation 2005, 111, 796–803. [Google Scholar] [CrossRef]
- Jonk, A.M.; Houben, A.J.; Schaper, N.C.; de Leeuw, P.W.; Serne, E.H.; Smulders, Y.M.; Stehouwer, C.D. Meal-related increases in microvascular vasomotion are impaired in obese individuals: A potential mechanism in the pathogenesis of obesity-related insulin resistance. Diabetes Care 2011, 34 Suppl 2, S342–S348. [Google Scholar] [CrossRef]
- Moraes, D.L.; Colucci, W.S.; Givertz, M.M. Secondary Pulmonary Hypertension in Chronic Heart Failure. Circulation 2000, 102, 1718–1723. [Google Scholar] [CrossRef] [PubMed]
- Bauman, A.E.; Sallis, J.F.; Dzewaltowski, D.A.; Owen, N. Toward a better understanding of the influences on physical activity: The role of determinants, correlates, causal variables, mediators, moderators, and confounders. Am. J. Prev. Med. 2002, 23, 5–14. [Google Scholar] [CrossRef]
- Ference, B.A.; Ginsberg, H.N.; Graham, I.; Ray, K.K.; Packard, C.J.; Bruckert, E.; Hegele, R.A.; Krauss, R.M.; Raal, F.J.; Schunkert, H.; et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur. Heart J. 2017, 38, 2459–2472. [Google Scholar] [CrossRef] [PubMed]
- Taher, R.; Sara, J.D.; Toya, T.; Borlaug, B.A.; Lerman, L.O.; Lerman, A. Peripheral endothelial dysfunction is a novel risk factor for systolic dysfunction and heart failure progression. Int. J. Cardiol. Heart Vasc. 2020, 30, 100584. [Google Scholar] [CrossRef]
- Li, W.; Schram, M.T.; Sörensen, B.M.; van Agtmaal, M.J.M.; Berendschot, T.T.J.M.; Webers, C.A.B.; Jansen, J.F.A.; Backes, W.H.; Gronenschild, E.H.B.M.; Schalkwijk, C.G.; et al. Microvascular Phenotyping in the Maastricht Study: Design and Main Findings, 2010–2018. Am. J. Epidemiol. 2020, 189, 873–884. [Google Scholar] [CrossRef]
- Paulus, W.J.; Tschöpe, C.; Sanderson, J.E.; Rusconi, C.; Flachskampf, F.A.; Rademakers, F.E.; Brutsaert, D.L. How to diagnose diastolic heart failure: A consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur. Heart J. 2007, 28, 2539–2550. [Google Scholar] [CrossRef] [PubMed]
- McKee, P.A.; Castelli, W.P.; McNamara, P.M.; Kannel, W.B. The Natural History of Congestive Heart Failure: The Framingham Study. N. Engl. J. Med. 1971, 285, 1441–1446. [Google Scholar] [CrossRef] [PubMed]
- Authors/Task Force Members; McMurray, J.J.; Adamopoulos, S.; Anker, S.D.; Auricchio, A.; Böhm, M.; Ponikowski, P. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2012, 33, 1787–1847. [Google Scholar]
- Armstrong, P.W.; Lam, C.S.; Anstrom, K.J.; Ezekowitz, J.; Hernandez, A.F.; O’Connor, C.M.; VITALITY-HFpEF Study Group. Effect of Vericiguat vs Placebo on Quality of Life in Patients With Heart Failure and Preserved Ejection Fraction: The VITALITY-HFpEF Randomized Clinical Trial. JAMA 2020, 324, 1512–1521. [Google Scholar] [CrossRef] [PubMed]
- Udelson, J.E.; Lewis, G.D.; Shah, S.J.; Zile, M.R.; Redfield, M.M.; Burnett, J.; Konstam, M.A. Effect of Praliciguat on Peak Rate of Oxygen Consumption in Patients With Heart Failure With Preserved Ejection Fraction: The CAPACITY HFpEF Randomized Clinical Trial. Jama 2020, 2020 324, 1522–1531. [Google Scholar] [CrossRef]
- Ueda, T.; Kasama, S.; Yamamoto, M.; Nakano, T.; Ueshima, K.; Morikawa, Y.; Kawata, H.; Yoshihisa, A.; Nakayama, M.; Komatsu, S.; et al. Effect of the Sodium-Glucose Cotransporter 2 Inhibitor Canagliflozin for Heart Failure With Preserved Ejection Fraction in Patients With Type 2 Diabetes. Circ. Rep. 2021, 3, 440–448. [Google Scholar] [CrossRef] [PubMed]
- Nassif, M.E.; Windsor, S.L.; Borlaug, B.A.; Kitzman, D.W.; Shah, S.J.; Tang, F.; Khariton, Y.; Malik, A.O.; Khumri, T.; Umpierrez, G.; et al. The SGLT2 inhibitor dapagliflozin in heart failure with preserved ejection fraction: A multicenter randomized trial. Nat. Med. 2021, 27, 1954–1960. [Google Scholar] [CrossRef] [PubMed]
- Abraham, W.T.; Lindenfeld, J.; Ponikowski, P.; Agostoni, P.; Butler, J.; Desai, A.S.; Filippatos, G.; Gniot, J.; Fu, M.; Gullestad, L.; et al. Effect of empagliflozin on exercise ability and symptoms in heart failure patients with reduced and preserved ejection fraction, with and without type 2 diabetes. Eur. Hear. J. 2021, 42, 700–710. [Google Scholar] [CrossRef] [PubMed]
- Butler, J.; Filippatos, G.; Siddiqi, T.J.; Brueckmann, M.; Böhm, M.; Chopra, V.K.; Ferreira, J.P.; Januzzi, J.L.; Kaul, S.; Piña, I.L.; et al. Empagliflozin, Health Status, and Quality of Life in Patients With Heart Failure and Preserved Ejection Fraction: The EMPEROR-Preserved Trial. Circulation 2022, 145, 184–193. [Google Scholar] [CrossRef] [PubMed]
- Pieske, B.; Wachter, R.; Shah, S.J.; Baldridge, A.; Szeczoedy, P.; Ibram, G.; Killat, H. Effect of Sacubitril/Valsartan vs Standard Medical Therapies on Plasma NT-proBNP Concentration and Submaximal Exercise Capacity in Patients With Heart Failure and Preserved Ejection Fraction: The PARALLAX Randomized Clinical Trial. JAMA 2021, 2021 326, 1919–1929. [Google Scholar] [CrossRef]
- Nanayakkara, S.; Byrne, M.; Mak, V.; Carter, K.; Dean, E.; Kaye, D.M. Extended-Release Oral Milrinone for the Treatment of Heart Failure With Preserved Ejection Fraction. J. Am. Hear. Assoc. 2020, 9, e015026. [Google Scholar] [CrossRef]
- Zamani, P.; Akers, S.; Soto-Calderon, H.; Beraun, M.; Koppula, M.R.; Varakantam, S.; Rawat, D.; Shiva-Kumar, P.; Haines, P.G.; Chittams, J.; et al. Isosorbide Dinitrate, With or Without Hydralazine, Does Not Reduce Wave Reflections, Left Ventricular Hypertrophy, or Myocardial Fibrosis in Patients With Heart Failure With Preserved Ejection Fraction. J. Am. Hear. Assoc. 2017, 6. [Google Scholar] [CrossRef]

| Study Design | HFpEF Population | Control Population | Method (Measurement) | Stimulus | Microvascular Function Assessed | Outcome (SD/IQR) |
|---|---|---|---|---|---|---|
| Skin-finger | ||||||
| Prospective [24] | n = 321 | Controls without HF, matched for age, sex, HT, and DM (n = 173) | Peripheral arterial tonometry (endoPAT): (RHI) | Ischemia | Hyperaemia | Log RHI: 0.53 ± 0.20 vs. 0.64 ± 0.20, p < 0.001 |
| Prospective [10] | n = 202 | No controls | endoPAT (RHI) | Ischemia | Hyperaemia | Log RHI: no absolute values reported. Correlation with CFR of R 0.21, p = 0.004 |
| Retrospective [25] | n = 159 | No controls | endoPAT (RHI) | Ischemia | Hyperaemia | Log RHI: 0.50 ± 0.09. Event free 0.52 ± 0.09 vs. Events 0.46 ± 0.08, p < 0.001 |
| Prospective (cross-sectional) [26] | n = 62 | Controls matched for age, sex, HT, DM, dyslipidaemia and CAD (n = 64) | endoPAT (RHI) | Ischemia | Hyperaemia | RHI: 2.01 [1.64–2.42] vs. 1.70 [1.55–1.88], p < 0.001 |
| Prospective [27] | n = 42 | HFrEF (n = 46) | endoPAT (RHI) | Ischemia | Hyperaemia | RHI: 1.77 [1.67–2.16] vs. 1.53 [1.42–1.94], p = 0.014. |
| Prospective [28] | n = 26 | Healthy controls, matched for age and sex (n = 26) | endoPAT (RHI) | Ischemia | Hyperaemia | RHI interpretation from boxplots: 1.9 [1.6–2.9] vs. 1.8 [2.0–3.3], p = 0.036. No effect of exercise |
| Prospective [29] | n = 21 | HT controls without HF (n = 19) Healthy controls (n = 10) | endoPAT (RHI) | Ischemia | Hyperaemia | Log RHI: 0.85 ± 0.42 vs. 0.92 ± 0.38 vs. 1.33 ± 0.34, p = n.s. between HFpEF and HT controls |
| Skin-arm | ||||||
| Prospective [30] | n = 45 | HT controls, matched for age, sex and diabetic status (n = 45) | Laser Doppler flowmetry (LDF), power spectral density (PSD) of the LDF signal | None, ischemia | Vasomotion, hyperaemia | LDF PSD: lower in HFpEF, no absolute numbers reported, p < 0.05. Peak blood flow (PU): 135 [104–206] vs. 177 [139–216], p = 0.03 |
| Prospective [11] | HFpEF with CAD n = 12 | HFrEF with CAD (n = 12) CAD without HF (n = 12) | Laser Doppler imaging (LDI) coupled with transcutaneous iontophoresis of vasodilators | acetylcholine, sodium nitroprusside | Hyperaemia | Vasodilation due to Acth: No absolute values reported. p = 0.00099 (HF vs. controls). Vasodilation due to nitroprusside: p = 0.006 (HF vs. controls) |
| Muscle-leg | ||||||
| Prospective [16] | n = 22 | Healthy controls, age-matched (n = 43). | Histology (skeletal muscle biopsy of thigh) | Capillary density | Capillary-to-fibre ratio: 1.35 ± 0.32 vs. 2.53 ± 1.37, p = 0.006 | |
| Prospective [31] | n = 7 | No controls. | Near-infrared spectroscopy: index for skeletal muscle haemoglobin oxygenation of thigh | Diffusion | Muscle deoxygenation overshoot was decreased after priming exercise, p = 0.041 | |
| Study Design | Study Population | Method (Measurement) | Stimulus | Microvascular Function Assessed | Outcome (SD/IQR) | Outcome Adjusted for Confounders |
|---|---|---|---|---|---|---|
| Heart-autopsy | ||||||
| Retrospective [12] | Deceased: HFpEF (n = 124); Controls (no HF) (n = 104) | Histology: microvessels/mm2 (microvascular density) | Rarefaction | Microvascular density: 961 (800–1370) vs. 1316 (1148–1467), p < 0.0001 | Not performed, unmatched population | |
| Invasive coronary function assessment | ||||||
| Retrospective [14] | CAG after positive stress test: HFpEF > 65 (n = 32); HFpEF < 65 (n = 24); Controls (n = 31) | Invasive CFR and IMR | Adenosine | Hyperaemia | CFR: 1.94 ± 0.28 vs. 1.83 ± 0.32 vs. 3.24 ± 1.11, p ≤ 0.04 IMR: 39.2 ± 6.8 vs. 27.2 ± 6.4 vs. 18.3 ± 4.4, p ≤ 0.03 | Age, sex, HT, DM, CKD, AF, BMI, LVMI. Unmatched controls |
| Retrospective [9] | HFpEF (n = 162) | Invasive CFR and coronary blood flow (CBF) | Adenosine, acetylcholine | Hyperaemia | No absolute values reported. Mortality is increased in coronary MVD (HR 2.8–3.5). | Age, sex, BMI, DM, HT, hyperlipidaemia, smoking, Hb, creatinine, uric acid |
| Retrospective [32] | HFpEF (n = 22); no HFpEF (n = 29) | Invasive CFR and CBF | Adenosine, acetylcholine | Hyperaemia | CFR: 2.5 ± 0.6 vs. 3.2 ± 0.7, p = 0.0003 Median CBF % increase: 1 (−35;34) vs. 64 (−4;133), p = 0.002 | Age, sex |
| Prospective [33] | HFpEF with obstructive epicardial CAD (n = 38); HFpEF without epicardial CAD (n = 37) | CAG (CFR, coronary reactivity, IMR) and MRI | Adenosine, acetylcholine | Hyperaemia | CFR: 2.0(1.2–2.4) vs. 2.4(1.5–3.1), p = 0.06. IMR: 18(12–26) vs. 27(19–43), p = 0.02. 24% microvascular spasm due to Acth. | Clinical characteristics are compared between groups based on coronary results. |
| Prospective (cross-sectional) [13] | Clinical indication for CAG: HFpEF (n = 30); Controls (n = 14) | Invasive CFR and IMR | Adenosine | Hyperaemia | CFR: 2.55 ± 1.60 vs. 3.84 ± 1.89, p = 0.024 IMR: 26.7 ± 10.3 vs. 19.7 ± 9.7, p = 0.037 | Exploratory analysis on age, BMI, GFR, BNP, echocardiographic data, hemodynamic data. Unmatched controls |
| Retrospective [34] | Patients with angina presented to the ER: HFpEF (n = 155); Controls (n = 135) | Total myocardial blush grade score (TMBGS) | None, nitroglycerin | Blood flow | TMBGS: 5.6 ± 1.22 vs. 6.1 ± 1.26, p = 0.02 | Not performed, unmatched population |
| Non-invasive coronary assessment | ||||||
| Prospective [35] | HFpEF (n = 19); Matched healthy controls (n = 19) | PET (C-acetate-11): myocardial blood flow (MBF) and myocardial oxygen consumption (MVO2) | Dobutamine | Blood flow, hyperaemia, diffusion | MBF increase: 78% vs. 151%, p = 0.0480 MVO2 increase: 59% vs. 86%, p = 0.0079 Absolute values during stress test not significantly different. | LVH, Hb. Healthy controls were matched for age and sex. |
| Retrospective [36] | Indication for cardiac PET: HFpEF (n = 78); HT without HF (n = 112); No HF no HT (n = 186) | PET (Rb-82): global myocardial flow reserve (MFR) | Dipyridamole | Hyperaemia | MFR: 2.16 ± 0.69 vs. 2.54 ± 0.80 vs. 2.89 ± 0.70, p ≤ 0.001 | Age, sex, BMI, smoking, DM, HT, hyperlipidaemia, HT, AF, statin use. Controls matched for HT. |
| Retrospective [37] | Suspected CAD: Cohort without HF (n = 201) | PET (Rb-82): (CFR) | Regadenoson or dipyridamole | Hyperaemia | 18% of the patients had a HFpEF event during follow-up. Independent HR with CFR <2.0 of 2.47 (1.09–5.62) | In entire cohort: AF, CKD, troponin, LVEF, CFR, E/e’ septal |
| Prospective [38] | HFpEF (n = 25); LVH (n = 13); Controls (n = 18) | MRI (CFR) | Adenosine | Hyperaemia | CFR: 2.21 ± 0.55 vs. 3.05 ± 0.74 vs. 3.83 ± 0.73, p ≤ 0.002 | BNP, LVEF, E/e’, LA dimension |
| Retrospective [39] | HFpEF without events (n = 137), with events (n = 26) | MRI (CFR) | Adenosine | Hyperaemia | CFR: 2.67 ± 0.64 vs. 1.93 ± 0.38 | Not performed |
| Prospective [40] | HFpEF (n = 6); Post MI (n = 6); Healthy controls (n = 20) | MRI: intravascular volume of basal septum (IVV) | Gadofosveset | Permeability | IVV: 0.155 ± 0.033 vs. 0.146 ± 0.038 vs. 0.135 ± 0.018, p = 0.413 | Not performed, unmatched controls |
| Prospective [10] | HFpEF (n = 202) | Echocardiography (CFR) | Adenosine | Hyperaemia | CFR: 2.13 ± 0.51 | Age, sex, BMI, AF, DM, CAD, smoking, LV mass, 6MWT, KCCQ, urinary albumin-creatinine ratio. No controls. |
| Prospective [41] | HFpEF (n = 77); Healthy controls (n = 30) | Echocardiography (CFR) | Adenosine | Hyperaemia | CFR: 1.7 ± 0.2 (with MVD) vs. 3.1 ± 0.4 (no MVD) vs. 3.4 ± 0.3 (control) | Age, LAVI, LVMI, LVEF, E/e’, 6MWT distance |
| Clinical Factor | Measurement Method | Microvascular Bed Assessed | Effect on Microvascular Function |
|---|---|---|---|
| Age [36,70,73,74,75] | Skin, eye, skeletal muscle, heart | Function decreases by increasing age | |
| Hormonal status [76,77,78,79] | Oestrogen levels, together with oestrogen receptor activity, are most accurate. Menopausal status and oral contraceptive therapy use are alternative surrogate markers. | Skin, skeletal muscle, heart | Function decreases with lower oestrogen activity |
| Hypercholesterolemia [71,80,81] | Serum cholesterol panel | Skin, eye, heart | Function decreases with higher serum low-density lipoprotein cholesterol levels |
| Hyperglycaemia [82,83] | Glucose tolerance test, fasting glucose, HbA1c | Skin, eye, heart | Function decreases with higher plasma glucose levels |
| Hypertension [36,38,70,84,85] | 24-h systolic blood pressure shows the highest correlation | Skin, eye, skeletal muscle, heart | Function decreases with higher systolic blood pressure and by duration of hypertension |
| Dietary intake [86] | Caffeine | Skin | Function is temporarily increased |
| Dietary intake [87,88] | High-fat diet | Skin, heart | Function is temporarily decreased |
| Physical inactivity [31,89,90,91] | 24-h accelerometer, physical activity questionnaire | Skin, eye, skeletal muscle | Function decreases with more physical inactivity. |
| Obesity [8,70,92,93] | Waist circumference is more correlated than BMI or BSA. | Skin, eye, skeletal muscle, heart | Function decreases with increasing level of obesity |
| Sex [94,95] | Skin, eye, skeletal muscle, heart | Effect on function depends on other confounders. | |
| Smoking [75,96] | Self-reported use | Skin, eye, heart | Function decreases with smoking and more pack years. |
| Limitation | HFpEF is a heterogeneous syndrome and has a variety of diagnostic criteria. This leads to different study populations with different disease stages and clinical phenotypes [5]. |
| Studies mainly focused on a general pathophysiology for an entire HFpEF population rather than selected phenotypes. | |
| The microvascular function is a continuum, and there is no clear cut-off value to define microvascular dysfunction in human biology. Nevertheless, studies are often focused on finding cut-off values that can have direct clinical implications. Both quantitative and categorical approaches are needed to improve current knowledge of MVD in HFpEF and could help in evaluating the likelihood of biological causality. | |
| No gold standard exists to assess MVD. Studies often overgeneralize specific microvascular alterations, which limits study designs and comparability within and between studies. | |
| MVD is not exclusive to HFpEF. Important drivers and clinical correlates of both (Table 3) need to be accounted for when interpreting study results. This requires larger study populations, which are not available in most of the current literature. | |
| Intervention studies with a direct or indirect effect on MVD have not selected patients based on those MVD aspects that are targeted with the intervention, limiting causal inference. | |
| Knowledge Gap | Knowledge on causality and underlying mechanisms of MVD and HFpEF is mostly derived from animal models, but their agreement with corresponding human phenotypes needs more research [180]. |
| Comparable longitudinal data of microvascular function are lacking in healthy individuals, HFpEF development, and adverse disease progression due to heterogeneity in microvascular assessments and HFpEF definitions. | |
| The role of MVD in specific HFpEF phenotypes remains to be elucidated. | |
| The similarity and underlying mechanisms of peripheral and coronary MVD in HFpEF deserve more investigation, as similar impairments with the same underlying mechanism could guide future targeted therapies. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Weerts, J.; Mourmans, S.G.J.; Barandiarán Aizpurua, A.; Schroen, B.L.M.; Knackstedt, C.; Eringa, E.; Houben, A.J.H.M.; van Empel, V.P.M. The Role of Systemic Microvascular Dysfunction in Heart Failure with Preserved Ejection Fraction. Biomolecules 2022, 12, 278. https://doi.org/10.3390/biom12020278
Weerts J, Mourmans SGJ, Barandiarán Aizpurua A, Schroen BLM, Knackstedt C, Eringa E, Houben AJHM, van Empel VPM. The Role of Systemic Microvascular Dysfunction in Heart Failure with Preserved Ejection Fraction. Biomolecules. 2022; 12(2):278. https://doi.org/10.3390/biom12020278
Chicago/Turabian StyleWeerts, Jerremy, Sanne G. J. Mourmans, Arantxa Barandiarán Aizpurua, Blanche L. M. Schroen, Christian Knackstedt, Etto Eringa, Alfons J. H. M. Houben, and Vanessa P. M. van Empel. 2022. "The Role of Systemic Microvascular Dysfunction in Heart Failure with Preserved Ejection Fraction" Biomolecules 12, no. 2: 278. https://doi.org/10.3390/biom12020278
APA StyleWeerts, J., Mourmans, S. G. J., Barandiarán Aizpurua, A., Schroen, B. L. M., Knackstedt, C., Eringa, E., Houben, A. J. H. M., & van Empel, V. P. M. (2022). The Role of Systemic Microvascular Dysfunction in Heart Failure with Preserved Ejection Fraction. Biomolecules, 12(2), 278. https://doi.org/10.3390/biom12020278








