The Constitutive Lack of α7 Nicotinic Receptor Leads to Metabolic Disorders in Mouse
Abstract
1. Introduction
2. Experimental Procedures
2.1. Mice
2.2. Cell Culture
2.3. Intraperitoneal Glucose, Insulin and Pyruvate Tolerance Tests
2.4. In Vivo 2-Deoxyglucose Uptake Measurement
2.5. Body Composition
2.6. Food Intake and Body Weight Measurement
2.7. Plasma Insulin Levels
2.8. Pancreatic Insulin Content
2.9. Islet Isolation
2.10. Static Incubation for Insulin Test
2.11. Plasma Non-Esterified Fatty Acid Levels and Hepatic Glycogen Content
2.12. Histomorphometric Studies
2.13. RNA Extraction and Real-Time Quantitative RT-PCR
2.14. Correlation Studies in Mice Islets
2.15. Statistical Analysis
3. Results
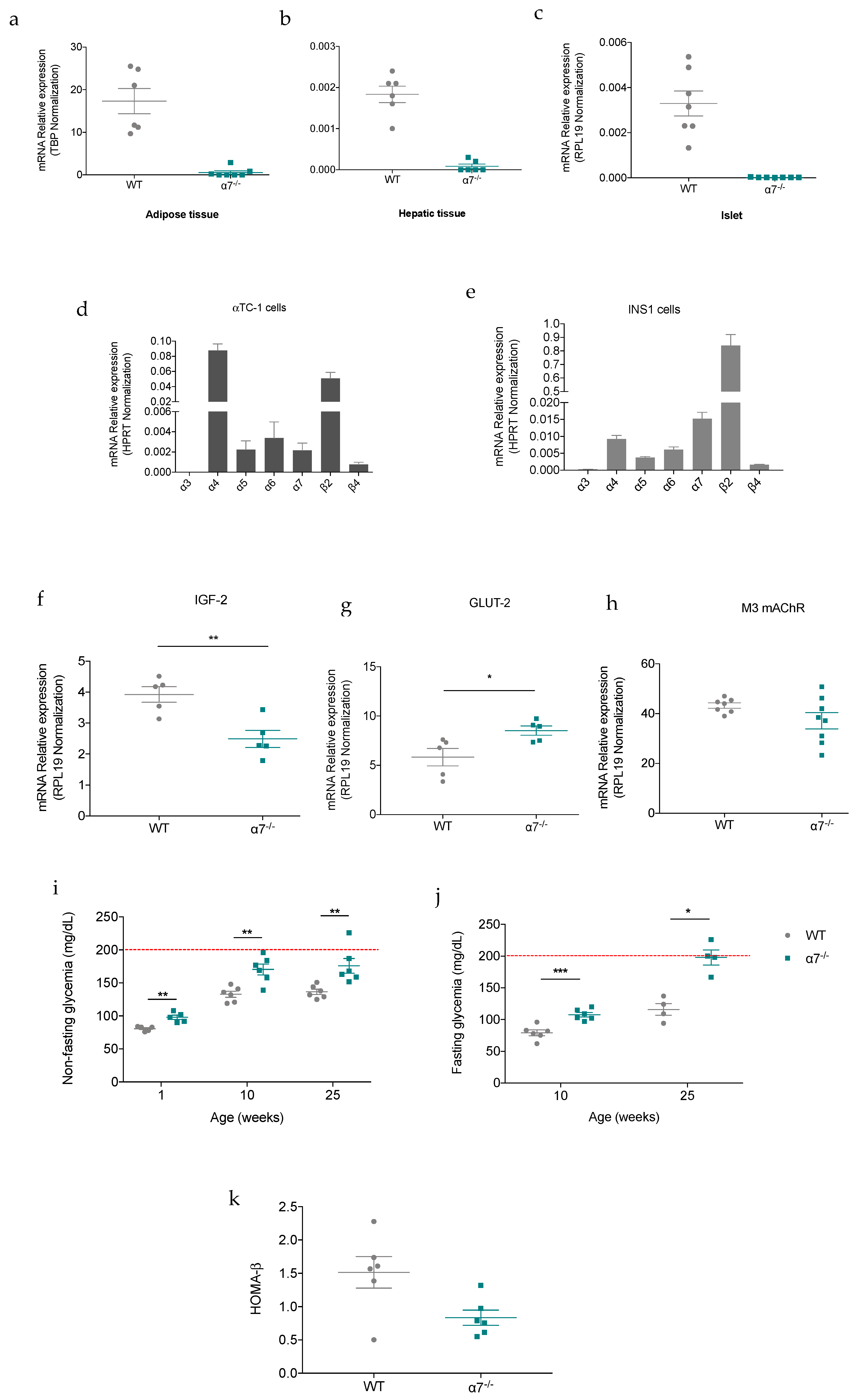
3.1. The Lack of α7 nAChR Induces a Chronic Mild High Glycemia in Mice Fed a Standard Chow Diet
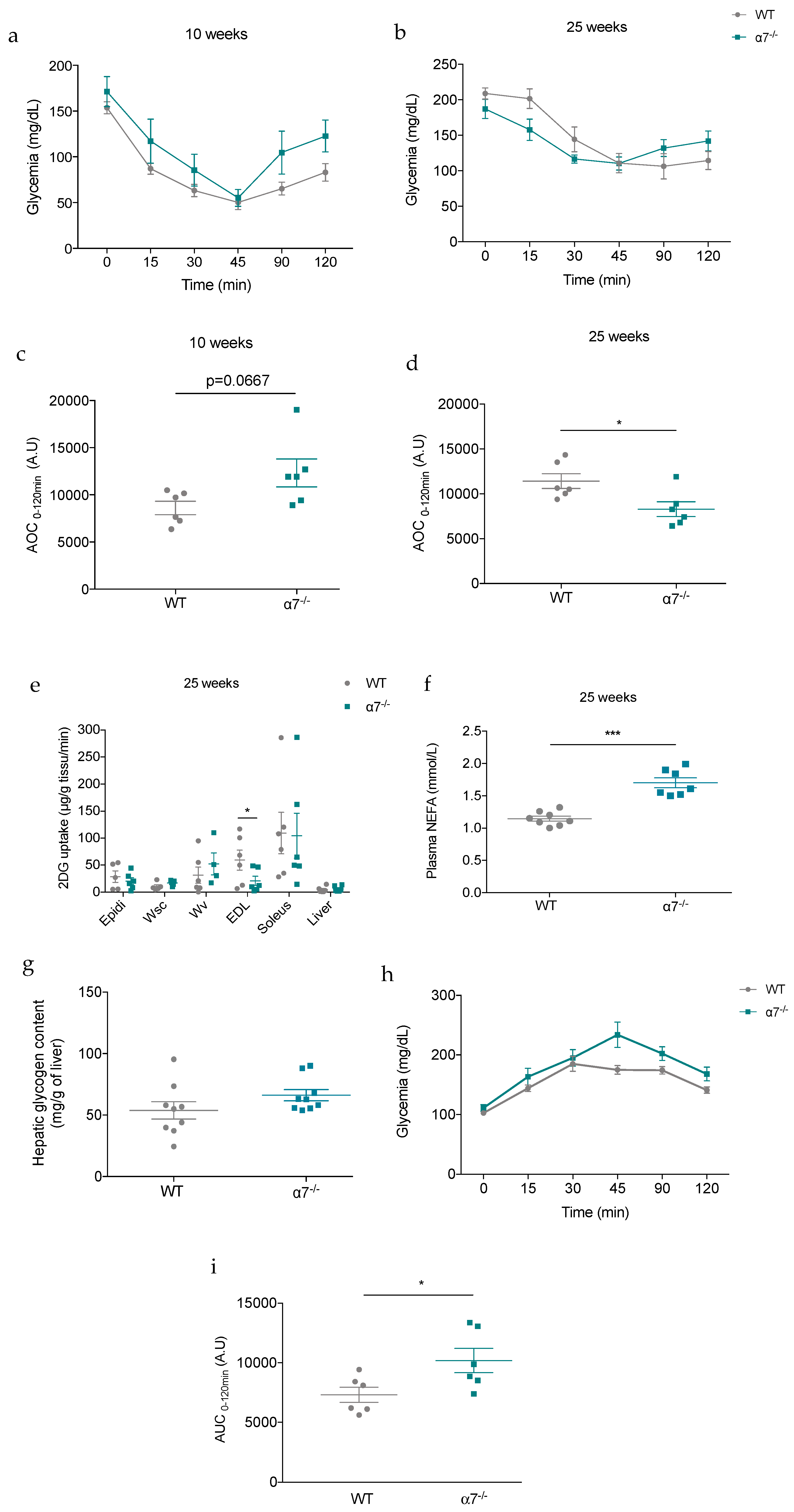
3.2. Glucose metabolism Is Altered in α7−/− mice Fed a Standard Chow Diet
3.3. 25-Week-Old α7−/− Mice Develop Insulin Resistance
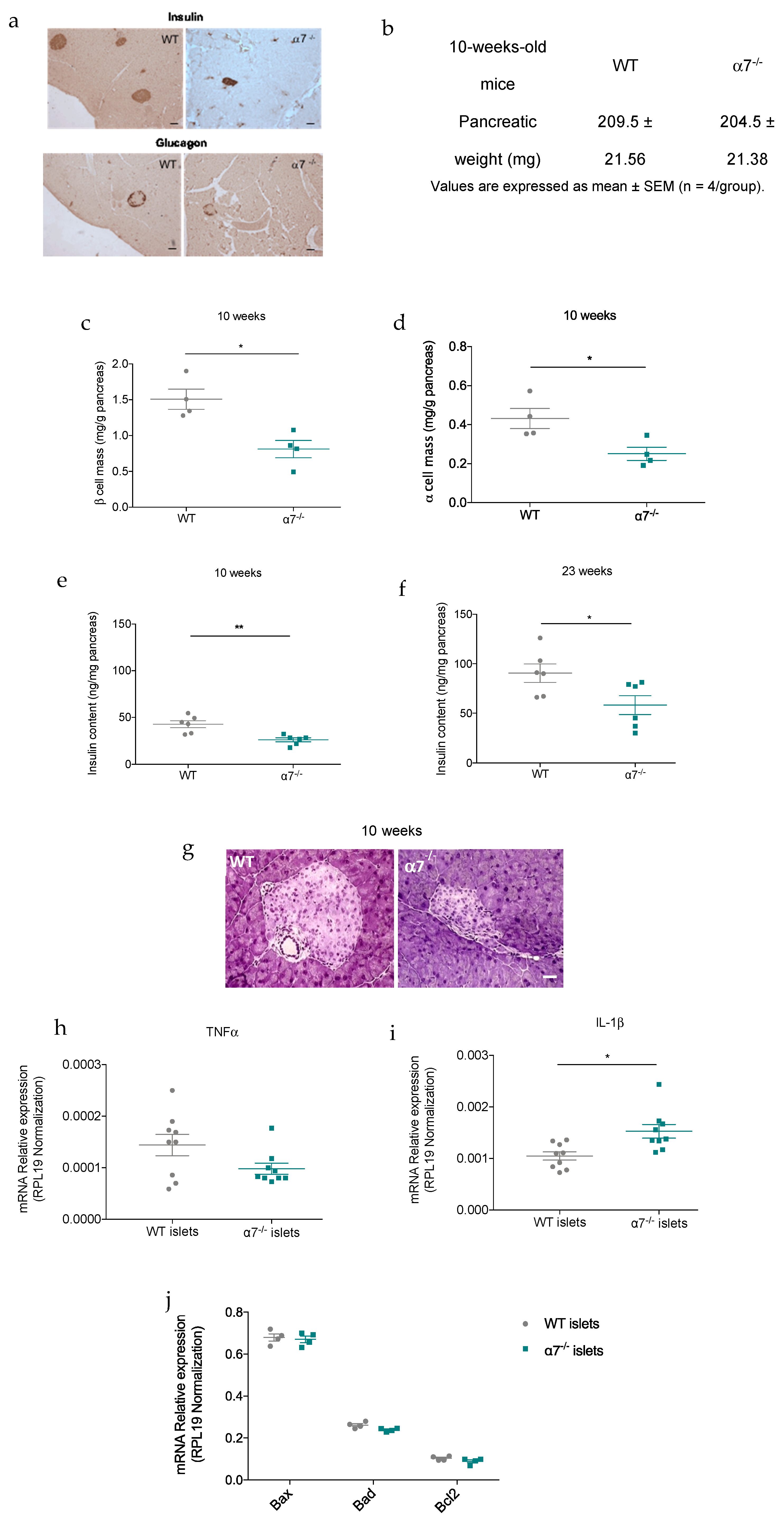
3.4. α7 nAChR Deficiency Is Associated to a Reduction in β-cell Mass in Mice
3.5. α7 nAChR Deficiency Is Associated to Embryonic Remodeling of Pancreatic Islet Mass
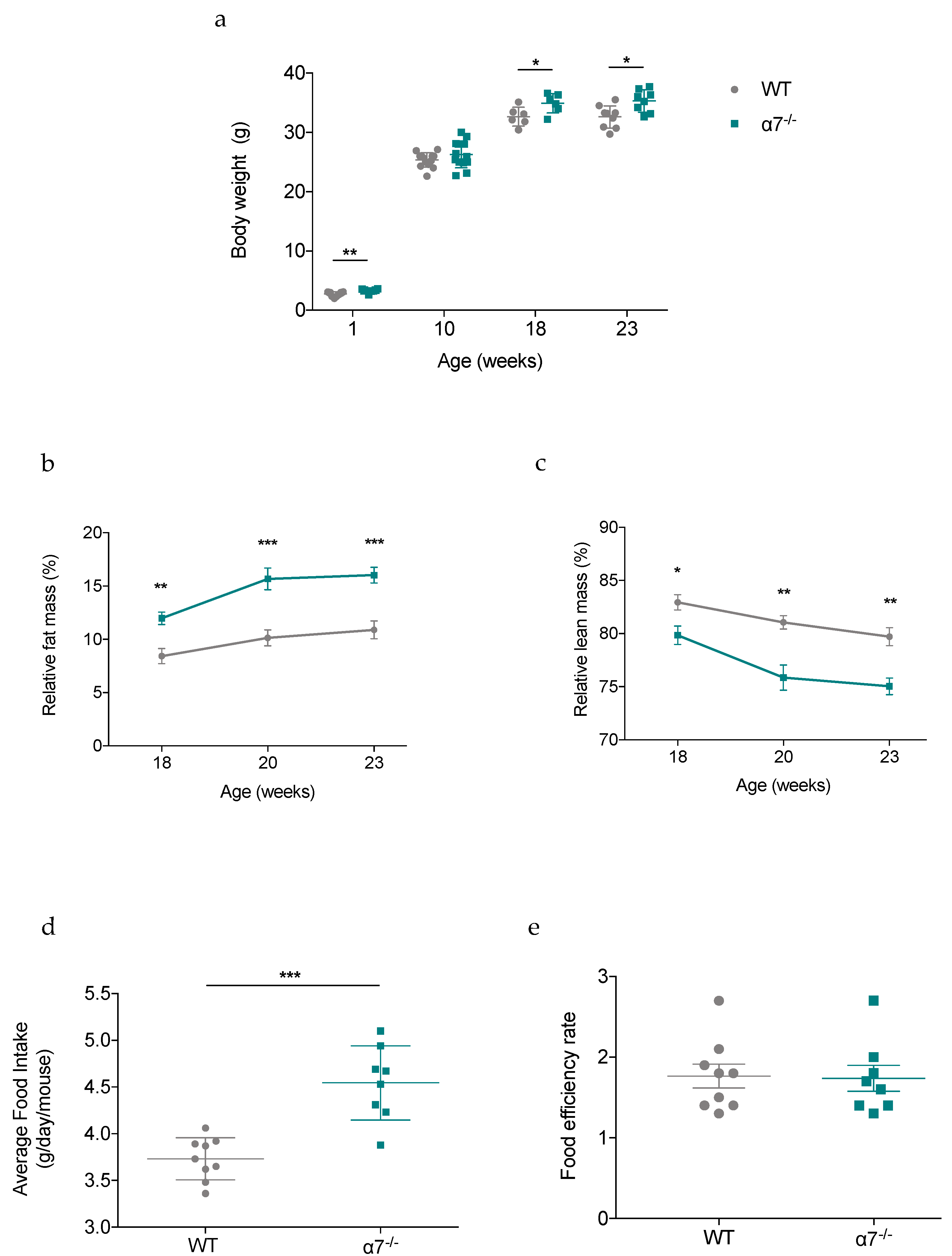
3.6. Body Weight and Food Intake Are Disturbed in α7−/− Mice Fed a standard Chow Diet
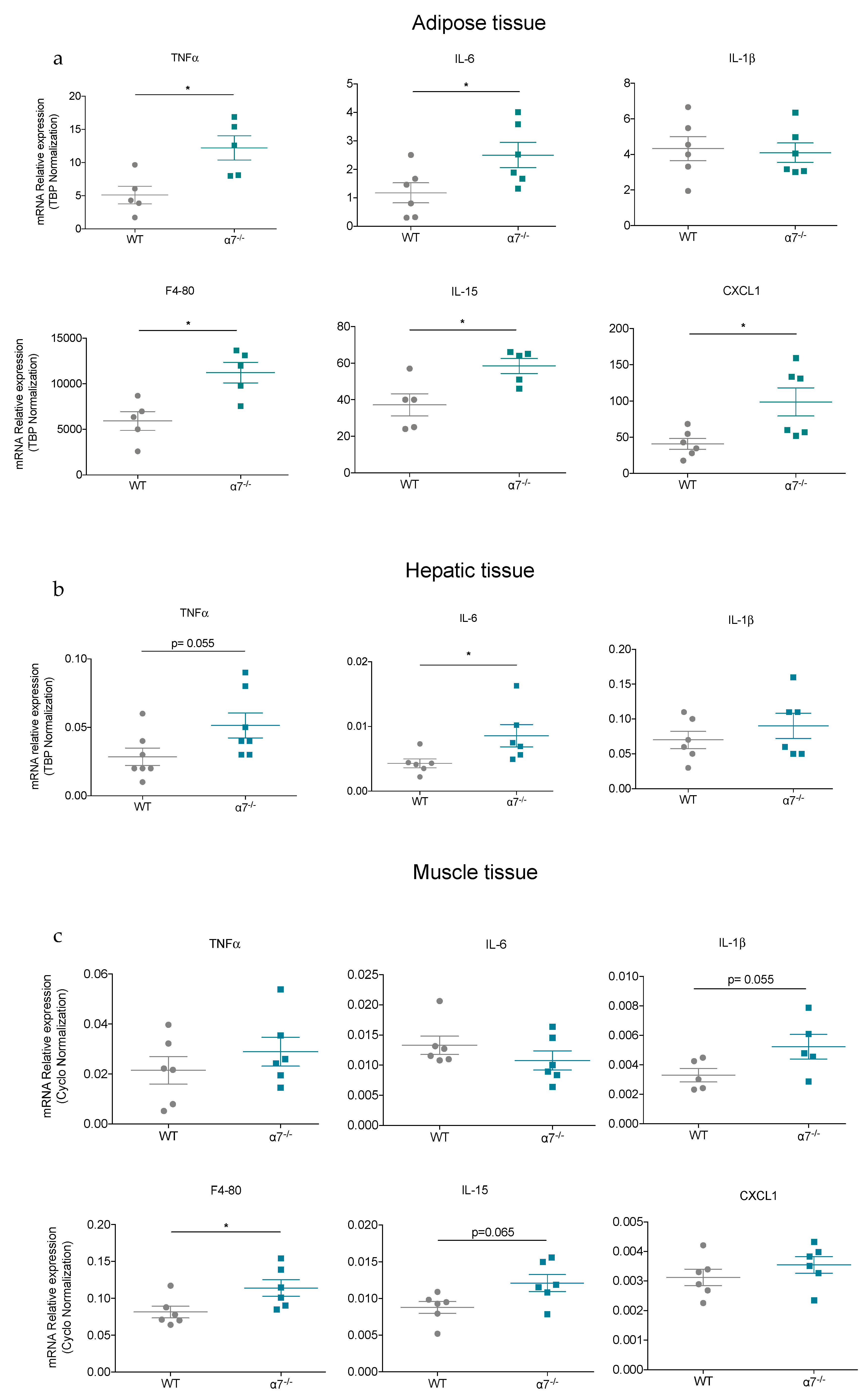
3.7. Adipose Tissue in 25-Week-Old α7−/− Mice Exhibits Higher Expression of Pro-Inflammtory Genes
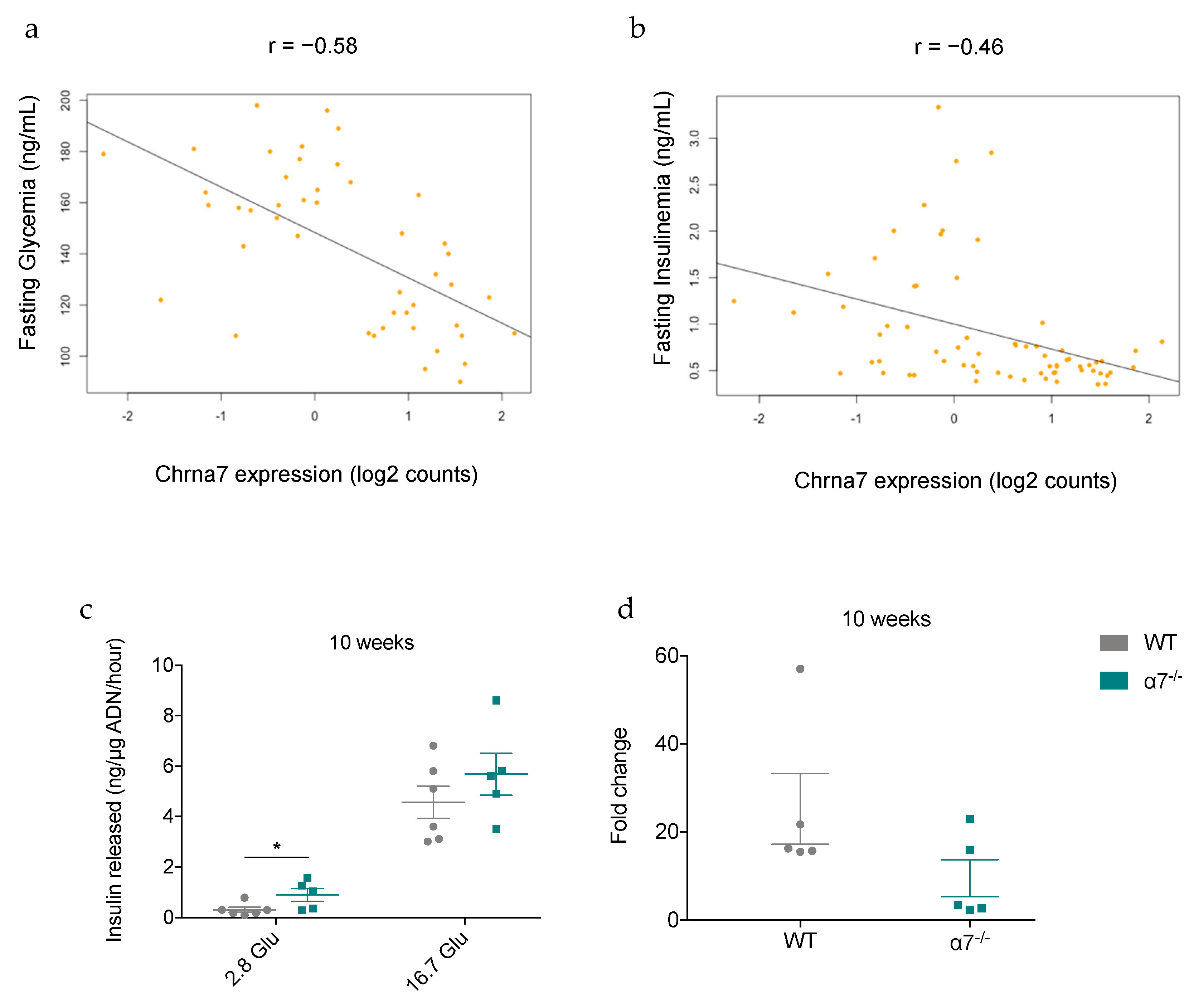
3.8. Correlation between the Expression of α7 nAChR in Mouse Islets and Fasting Glycemia and Insulinemia
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbrevation
| AOC | Area Over Curve |
| AUC | Aera Under Curve |
| Chrna7 | Cholinergic receptor nicotinic alpha7 |
| Cyclo A | Cyclophilin A |
| EDL | Extensor Digitorum Longus |
| GSIS | glucose-stimulated insulin secretion |
| GTT | Glucose tolerance test |
| HPRT | Hypoxanthine phosphoribosyl transferase |
| ITT | Insulin tolerance test |
| IGF-1 | Insulin-like growth factor-1 |
| IGF-1R | Insulin-like growth factor-1 receptor |
| IGF-2 | Insulin-like growth factor-2 |
| IRS 2 | Insulin receptor substrate 2 |
| mAChRs | muscarinic acetylcholine receptors |
| M-MLV | Moloney-murine leukemia virus |
| nAChR | nicotinic acetylcholine receptor |
| NEFAs | Non-esterified fatty acids |
| PTT | Pyruvate tolerance test |
| RPL19 | Ribosomal protein L19 |
| TBP | TATA-box binding protein |
| T1D | type 1 diabetes |
| T2D | type 2 diabetes |
| WT | Wild-Type |
References
- Guariguata, L.; Whiting, D.R.; Hambleton, I.R.; Beagley, J.; Linnenkamp, U.; Shaw, J. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res. Clin. Pract. 2014, 103, 137–149. [Google Scholar] [CrossRef] [PubMed]
- DeFronzo, R.A. Pathogenesis of type 2 diabetes mellitus. Med. Clin. N. Am. 2004, 88, 787–835. [Google Scholar] [CrossRef] [PubMed]
- Sowers, J.R.; Frohlich, E.D. Insulin and insulin resistance: Impact on blood pressure and cardiovascular disease. Med. Clin. N. Am. 2004, 88, 63–82. [Google Scholar] [CrossRef]
- Halban, P.A.; Polonsky, K.S.; Bowden, N.W.; Hawkins, M.A.; Ling, C.; Mather, K.J.; Powers, A.C.; Rhodes, C.J.; Sussel, L.; Weir, G.C. β-Cell Failure in Type 2 Diabetes: Postulated Mechanisms and Prospects for Prevention and Treatment. J. Clin. Endocrinol. Metab. 2014, 99, 1983–1992. [Google Scholar] [CrossRef]
- Ahrén, B. Autonomic regulation of islet hormone secretion—Implications for health and disease. Diabetologia 2000, 43, 393–410. [Google Scholar] [CrossRef]
- Lausier, J.; Diaz, W.C.; Roskens, V.; LaRock, K.; Herzer, K.; Fong, C.G.; Latour, M.G.; Peshavaria, M.; Jetton, T.L. Vagal control of pancreatic ß-cell proliferation. Am. J. Physiol. Metab. 2010, 299, E786–E793. [Google Scholar] [CrossRef]
- Guo, Y.; Traurig, M.; Ma, L.; Kobes, S.; Harper, I.; Infante, A.M.; Bogardus, C.; Baier, L.J.; Prochazka, M. CHRM3 Gene Variation Is Associated With Decreased Acute Insulin Secretion and Increased Risk for Early-Onset Type 2 Diabetes in Pima Indians. Diabetes 2006, 55, 3625–3629. [Google Scholar] [CrossRef]
- Gilon, P. Mechanisms and Physiological Significance of the Cholinergic Control of Pancreatic -Cell Function. Endocr. Rev. 2001, 22, 565–604. [Google Scholar] [CrossRef]
- Ejiri, K.; Taniguchi, H.; Ishihara, K.; Hara, Y.; Baba, S. Possible involvement of cholinergic nicotinic receptor in insulin release from isolated rat islets. Diabetes Res. Clin. Pract. 1990, 8, 193–199. [Google Scholar] [CrossRef]
- Yoshikawa, H.; Hellström-Lindahl, E.; Grill, V. Evidence for functional nicotinic receptors on pancreatic β cells. Metabolism 2005, 54, 247–254. [Google Scholar] [CrossRef]
- Ohtani, M.; Oka, T.; Badyuk, M.; Xiao, Y.; Kellar, K.J.; Daly, J.W. Mouse β-TC6 Insulinoma Cells: High Expression of Functional α3β4 Nicotinic Receptors Mediating Membrane Potential, Intracellular Calcium, and Insulin Release. Mol. Pharmacol. 2005, 69, 899–907. [Google Scholar] [CrossRef] [PubMed]
- Maddatu, J.; Anderson-Baucum, E.; Evans-Molina, C. Smoking and the risk of type 2 diabetes. Transl. Res. 2017, 184, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Ganic, E.; Singh, T.; Luan, C.; Fadista, J.; Johansson, J.K.; Cyphert, H.A.; Bennet, H.; Storm, P.; Prost, G.; Ahlenius, H.; et al. MafA-Controlled Nicotinic Receptor Expression Is Essential for Insulin Secretion and Is Impaired in Patients with Type 2 Diabetes. Cell Rep. 2016, 14, 1991–2002. [Google Scholar] [CrossRef] [PubMed]
- Changeux, J.-P. The Nicotinic Acetylcholine Receptor: The Founding Father of the Pentameric Ligand-gated Ion Channel Superfamily. J. Biol. Chem. 2012, 287, 40207–40215. [Google Scholar] [CrossRef] [PubMed]
- Steinbach, J.H. Mechanism of Action of the Nicotinic Acetylcholine Receptor. Ciba Found. Symp. Bilharz. 2007, 53–67. [Google Scholar] [CrossRef]
- Séguéla, P.; Wadiche, J.; Dineley-Miller, K.; Dani, J.; Patrick, J. Molecular cloning, functional properties, and distribution of rat brain alpha 7: A nicotinic cation channel highly permeable to calcium. J. Neurosci. 1993, 13, 596–604. [Google Scholar] [CrossRef]
- Maouche, K.; Polette, M.; Jolly, T.; Medjber, K.; Cloëz-Tayarani, I.; Changeux, J.-P.; Burlet, H.; Terryn, C.; Coraux, C.; Zahm, J.-M.; et al. α7 Nicotinic Acetylcholine Receptor Regulates Airway Epithelium Differentiation by Controlling Basal Cell Proliferation. Am. J. Pathol. 2009, 175, 1868–1882. [Google Scholar] [CrossRef]
- Catassi, A.; Servent, D.; Paleari, L.; Cesario, A.; Russo, P. Multiple roles of nicotine on cell proliferation and inhibition of apoptosis: Implications on lung carcinogenesis. Mutat. Res. Mutat. Res. 2008, 659, 221–231. [Google Scholar] [CrossRef]
- Wang, H.; Yu, M.; Ochani, M.; Amella, C.A.; Tanovic, M.; Susarla, S.; Li, J.H.; Wang, H.; Yang, H.; Ulloa, L.; et al. Nicotinic acetylcholine receptor α7 subunit is an essential regulator of inflammation. Nature 2002, 421, 384–388. [Google Scholar] [CrossRef]
- Cancello, R.; Zulian, A.; Maestrini, S.; Mencarelli, M.; Della Barba, A.; Invitti, C.; Liuzzi, A.; Di Blasio, A.M. The nicotinic acetylcholine receptor α7 in subcutaneous mature adipocytes: Downregulation in human obesity and modulation by diet-induced weight loss. Int. J. Obes. 2012, 36, 1552–1557. [Google Scholar] [CrossRef]
- Marrero, M.B.; Lucas, R.; Salet, C.; Hauser, T.A.; Mazurov, A.; Lippiello, P.M.; Bencherif, M. An α7 Nicotinic Acetylcholine Receptor-Selective Agonist Reduces Weight Gain and Metabolic Changes in a Mouse Model of Diabetes. J. Pharmacol. Exp. Ther. 2009, 332, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Yang, Z.; Xue, B.; Shi, H. Activation of the cholinergic antiinflammatory pathway ameliorates obesity-induced inflammation and insulin resistance. Endocrinology 2011, 152, 836–846. [Google Scholar] [CrossRef] [PubMed]
- Xu, T.-Y.; Guo, L.-L.; Wang, P.; Song, J.; Le, Y.; Viollet, B.; Miao, C.-Y. Chronic Exposure to Nicotine Enhances Insulin Sensitivity through α7 Nicotinic Acetylcholine Receptor-STAT3 Pathway. PLoS ONE 2012, 7, e51217. [Google Scholar] [CrossRef]
- Somm, E.; Guérardel, A.; Maouche, K.; Toulotte, A.; Veyrat-Durebex, C.; Rohner-Jeanrenaud, F.; Maskos, U.; Hüppi, P.S.; Schwitzgebel, V.M. Concomitant alpha7 and beta2 nicotinic AChR subunit deficiency leads to impaired energy homeostasis and increased physical activity in mice. Mol. Genet. Metab. 2014, 112, 64–72. [Google Scholar] [CrossRef]
- Lerat, H.; Imache, M.R.; Polyte, J.; Gaudin, A.; Mercey, M.; Donati, F.; Baudesson, C.; Higgs, M.R.; Picard, A.; Magnan, C.; et al. Hepatitis C virus induces a prediabetic state by directly impairing hepatic glucose metabolism in mice. J. Biol. Chem. 2017, 292, 12860–12873. [Google Scholar] [CrossRef]
- Movassat, J.; Saulnier, C.; Serradas, P.; Portha, B. Impaired development of pancreatic beta-cell mass is a primary event during the progression to diabetes in the GK rat. Diabetologia 1997, 40, 916–925. [Google Scholar] [CrossRef]
- Figeac, F.; Ilias, A.; Bailbé, D.; Portha, B.; Movassat, J. Local In Vivo GSK3β Knockdown Promotes Pancreatic β Cell and Acinar Cell Regeneration in 90% Pancreatectomized Rat. Mol. Ther. 2012, 20, 1944–1952. [Google Scholar] [CrossRef] [PubMed]
- Cruciani-Guglielmacci, C.; Bellini, L.; Denom, J.; Oshima, M.; Fernandez, N.; Normandie-Levi, P.; Berney, X.P.; Kassis, N.; Rouch, C.; Dairou, J.; et al. Molecular phenotyping of multiple mouse strains under metabolic challenge uncovers a role for Elovl2 in glucose-induced insulin secretion. Mol. Metab. 2017, 6, 340–351. [Google Scholar] [CrossRef]
- Bansal, N. Prediabetes diagnosis and treatment: A review. World J. Diabetes 2015, 6, 296–303. [Google Scholar] [CrossRef]
- Kergoat, M.; Guerre-Millo, M.; Lauva, M.; Portha, B. Increased insulin action in rats with mild insulin deficiency induced by neonatal streptozotocin. Am. J. Physiol. Metab. 1991, 260, E561–E567. [Google Scholar] [CrossRef]
- Randle, P.J. Regulatory interactions between lipids and carbohydrates: The glucose fatty acid cycle after 35 years. Diabetes Metab. Rev. 1998, 14, 263–283. [Google Scholar] [CrossRef]
- Nuutila, P.; Koivisto, V.A.; Knuuti, J.; Ruotsalainen, U.; Teräs, M.; Haaparanta, M.; Bergman, J.; Solin, O.; Voipio-Pulkki, L.M.; Wegelius, U. Glucose-free fatty acid cycle operates in human heart and skeletal muscle in vivo. J. Clin. Investig. 1992, 89, 1767–1774. [Google Scholar] [CrossRef] [PubMed]
- Lam, T.K.T.; Van De Werve, G.; Giacca, A. Free fatty acids increase basal hepatic glucose production and induce hepatic insulin resistance at different sites. Am. J. Physiol. Metab. 2003, 284, E281–E290. [Google Scholar] [CrossRef] [PubMed]
- Stingl, H.; Krššák, M.; Krebs, M.; Bischof, M.G.; Nowotny, P.; Fürnsinn, C.; Shulman, G.I.; Waldhäusl, W.; Roden, M. Lipid-dependent control of hepatic glycogen stores in healthy humans. Diabetologia 2001, 44, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Perseghin, G.; Petersen, K.; Shulman, G.I. Cellular mechanism of insulin resistance: Potential links with inflammation. Int. J. Obes. 2003, 27, S6–S11. [Google Scholar] [CrossRef]
- Portha, B.; Chavey, A.; Movassat, J. Early-Life Origins of Type 2 Diabetes: Fetal Programming of the Beta-Cell Mass. Exp. Diabetes Res. 2011, 2011, 1–16. [Google Scholar] [CrossRef]
- Lumeng, C.N.; Saltiel, A.R. Inflammatory links between obesity and metabolic disease. J. Clin. Investig. 2011, 121, 2111–2117. [Google Scholar] [CrossRef]
- Hotamisligil, G.S. Inflammation and metabolic disorders. Nature 2006, 444, 860–867. [Google Scholar] [CrossRef]
- Ramanathan, S.; Lacraz, G.; Donates, Y.C.; Mayhue, M.; Langois, M.F.; Pleszczynski, M.R.; Ilangumaran, S. Interleukin-15 in the Regulation of Obesity and Fatty Liver Disease. J. Clin. Exp. Hepatol. 2014, 4, S32. [Google Scholar] [CrossRef]
- Nunemaker, C.S.; Chung, H.G.; Verrilli, G.M.; Corbin, K.L.; Upadhye, A.; Sharma, P.R. Increased serum CXCL1 and CXCL5 are linked to obesity, hyperglycemia, and impaired islet function. J. Endocrinol. 2014, 222, 267–276. [Google Scholar] [CrossRef]
- Wajchenberg, B.L. β-Cell Failure in Diabetes and Preservation by Clinical Treatment. Endocr. Rev. 2007, 28, 187–218. [Google Scholar] [CrossRef] [PubMed]
- Pick, A.; Clark, J.; Kubstrup, C.; Levisetti, M.; Pugh, W.; Bonner-Weir, S.; Polonsky, K.S. Role of apoptosis in failure of beta-cell mass compensation for insulin resistance and beta-cell defects in the male Zucker diabetic fatty rat. Diabetes 1998, 47, 358–364. [Google Scholar] [CrossRef] [PubMed]
- Woods, S.C.; Porte, D. Neural control of the endocrine pancreas. Physiol. Rev. 1974, 54, 596–619. [Google Scholar] [CrossRef] [PubMed]
- Edvell, A.; Lindström, P. Vagotomy in young obese hyperglycemic mice: Effects on syndrome development and islet proliferation. Am. J. Physiol. Content 1998, 274, E1034–E1039. [Google Scholar] [CrossRef]
- Yamamoto, J.; Imai, J.; Izumi, T.; Takahashi, H.; Kawana, Y.; Takahashi, K.; Kodama, S.; Kaneko, K.; Gao, J.; Uno, K.; et al. Neuronal signals regulate obesity induced β-cell proliferation by FoxM1 dependent mechanism. Nat. Commun. 2017, 8, 1930. [Google Scholar] [CrossRef]
- Gupta, D.; Lacayo, A.A.; Greene, S.M.; Leahy, J.L.; Jetton, T.L. β-Cell mass restoration by α7 nicotinic acetylcholine receptor activation. J. Biol. Chem. 2018, 293, 20295–20306. [Google Scholar] [CrossRef]
- Fujimoto, K.; Polonsky, K.S. Pdx1 and other factors that regulate pancreatic beta-cell survival. Diabetes Obes. Metab. 2009, 11, 30–37. [Google Scholar] [CrossRef]
- Duttaroy, A.; Zimliki, C.L.; Gautam, D.; Cui, Y.; Mears, D.; Wess, J. Muscarinic stimulation of pancreatic insulin and glucagon release is abolished in m3 muscarinic acetylcholine receptor-deficient mice. Diabetes 2004, 53, 1714–1720. [Google Scholar] [CrossRef]
- Gautam, D.; Han, S.-J.; Hamdan, F.F.; Jeon, J.; Li, B.; Li, J.H.; Cui, Y.; Mears, D.; Lu, H.; Deng, C.; et al. A critical role for β cell M3 muscarinic acetylcholine receptors in regulating insulin release and blood glucose homeostasis in vivo. Cell Metab. 2006, 3, 449–461. [Google Scholar] [CrossRef]
- Devedjian, J.-C.; George, M.; Casellas, A.; Pujol, A.; Visa, J.; Pelegrin, M.; Gros, L.; Bosch, F. Transgenic mice overexpressing insulin-like growth factor-II in β cells develop type 2 diabetes. J. Clin. Investig. 2000, 105, 731–740. [Google Scholar] [CrossRef] [PubMed]
- Petrik, J.; Reusens, B.; Arany, E.; Remacle, C.; Coelho, C.; Hoet, J.J.; Hill, D.J. A Low Protein Diet Alters the Balance of Islet Cell Replication and Apoptosis in the Fetal and Neonatal Rat and Is Associated with a Reduced Pancreatic Expression of Insulin-Like Growth Factor-II1. Endocrinology 1999, 140, 4861–4873. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, C. Contrasted Impact of Maternal Rat Food Restriction on the Fetal Endocrine Pancreas. Endocrinology 1997, 138, 2267–2273. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, E.; Martín, M.A.; Fajardo, S.; Escrivá, F.; Alvarez, C. Increased IRS-2 content and activation of IGF-I pathway contribute to enhance β-cell mass in fetuses from undernourished pregnant rats. Am. J. Physiol. Metab. 2007, 292, E187–E195. [Google Scholar] [CrossRef][Green Version]
- Martín, M.A.; Serradas, P.; Ramos, S.; Fernandez, E.; Goya, L.; Gangnerau, M.N.; Lacorne, M.; Pascual-Leone, A.M.; Escrivá, F.; Portha, B.; et al. Protein-Caloric Food Restriction Affects Insulin-Like Growth Factor System in Fetal Wistar Rat. Endocrinology 2005, 146, 1364–1371. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Thorel, F.; Nepote, V.; Avril, I.; Kohno, K.; Desgraz, R.; Chera, S.; Herrera, P.L. Conversion of adult pancreatic α-cells to β-cells after extreme β-cell loss. Nature 2010, 464, 1149–1154. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.-P.; Thorel, F.; Boyer, D.F.; Herrera, P.L.; Wright, C.V.E. Context-specific α-to-β-cell reprogramming by forced Pdx1 expression. Genes Dev. 2011, 25, 1680–1685. [Google Scholar] [CrossRef]
- Weir, G.C.; Bonner-Weir, S. Five of stages of evolving β-cell dysfunction during progression to diabetes. Diabetes 2004, 53 (Suppl. 3), S16–S21. [Google Scholar] [CrossRef]
- King, A.J.F. The use of animal models in diabetes research. Br. J. Pharmacol. 2012, 166, 877–894. [Google Scholar] [CrossRef]
- Bonner-Weir, S.; Trent, D.F.; Honey, R.N.; Weir, G.C. Responses of neonatal rat islets to streptozotocin: Limited B-cell regeneration and hyperglycemia. Diabetes 1981, 30, 64–69. [Google Scholar] [CrossRef]
- Leahy, J.L.; Cooper, H.E.; Weir, G.C. Impaired Insulin Secretion Associated With Near Normoglycemia: Study in Normal Rats With 96-h In Vivo Glucose Infusions. Diabetes 1987, 36, 459–464. [Google Scholar] [CrossRef]
- Laury, M.C.; Takao, F.; Bailbé, D.; Penicaud, L.; Portha, B.; Picon, L.; Ktorza, G.A. Differential Effects of Prolonged Hyperglycemia on in Vivo and in Vitro Insulin Secretion in Rats. Endocrinology 1991, 128, 2526–2533. [Google Scholar] [CrossRef]
- Chen, M.; Porte, D. The Effect of Rate and Dose of Glucose Infusion on the Acute Insulin Response in Man. J. Clin. Endocrinol. Metab. 1976, 42, 1168–1175. [Google Scholar] [CrossRef]
- Thiebaud, D.; Jacot, E.; DeFronzo, R.A.; Maeder, E.; Jequier, E.; Felber, J.-P. The Effect of Graded Doses of Insulin on Total Glucose Uptake, Glucose Oxidation, and Glucose Storage in Man. Diabetes 1982, 31, 957–963. [Google Scholar] [CrossRef]
- Lillioja, S.; Mott, D.M.; Spraul, M.; Ferraro, R.; Foley, J.E.; Ravussin, E.; Knowler, W.C.; Bennett, P.H.; Bogardus, C. Insulin Resistance and Insulin Secretory Dysfunction as Precursors of Non-Insulin-Dependent Diabetes Mellitus: Prospective Studies of Pima Indians. N. Engl. J. Med. 1993, 329, 1988–1992. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.; Kurose, T.; Matsukura, S. Oral nicotine administration decreases tumor necrosis factor-alpha expression in fat tissues in obese rats. Metabolism 2001, 50, 79–85. [Google Scholar] [CrossRef]
- Hotamisligil, G.; Shargill, N.; Spiegelman, B. Adipose expression of tumor necrosis factor-alpha: Direct role in obesity-linked insulin resistance. Science 1993, 259, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Uysal, K.T.; Wiesbrock, S.M.; Hotamisligil, G.S. Functional Analysis of Tumor Necrosis Factor (TNF) Receptors in TNF-α-Mediated Insulin Resistance in Genetic Obesity. Endocrinology 1998, 139, 4832–4838. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, M.W.; Woods, S.C.; Porte, D.; Seeley, R.J.; Baskin, D.G. Central nervous system control of food intake. Nature 2000, 404, 661–671. [Google Scholar] [CrossRef] [PubMed]
- McFadden, K.L.; Cornier, M.-A.; Tregellas, J.R. The role of alpha-7 nicotinic receptors in food intake behaviors. Front. Psychol. 2014, 5. [Google Scholar] [CrossRef] [PubMed]
- Jo, Y.-H.; Talmage, D.; Role, L.W. Nicotinic receptor-mediated effects on appetite and food intake. J. Neurobiol. 2002, 53, 618–632. [Google Scholar] [CrossRef] [PubMed]
- Souza, A.; Souza, C.M.; Amaral, C.L.; Lemes, S.F.; Santucci, L.F.; Milanski, M.; Torsoni, A.S.; Torsoni, M.A. Short-Term High-Fat Diet Consumption Reduces Hypothalamic Expression of the Nicotinic Acetylcholine Receptor α7 Subunit (α7nAChR) and Affects the Anti-inflammatory Response in a Mouse Model of Sepsis. Front. Immunol. 2019, 10, 565. [Google Scholar] [CrossRef] [PubMed]
- Riley, B.; Williamson, M.; Collier, D.; Wilkie, H.; Makoff, A. A 3-Mb Map of a Large Segmental Duplication Overlapping the α7-Nicotinic Acetylcholine Receptor Gene (CHRNA7) at Human 15q13–q14. Genomics 2002, 79, 197–209. [Google Scholar] [CrossRef] [PubMed]
- De Lucas-Cerrillo, A.M.; Maldifassi, M.C.; Arnalich, F.; Renart, J.; Atienza, G.; Serantes, R.; Cruces, J.; Pacheco, A.S.; Andrés-Mateos, E.; Montiel, C. Function of Partially Duplicated Human α7 Nicotinic Receptor Subunit CHRFAM7A Gene. J. Biol. Chem. 2010, 286, 594–606. [Google Scholar] [CrossRef]
- Brody, A.L.; Mandelkern, M.A.; London, E.D.; Olmstead, R.E.; Farahi, J.; Scheibal, D.; Jou, J.; Allen, V.; Tiongson, E.; Chefer, S.I.; et al. Cigarette Smoking Saturates Brain α4β2 Nicotinic Acetylcholine Receptors. Arch. Gen. Psychiatry 2006, 63, 907–915. [Google Scholar] [CrossRef]
- Corringer, P.-J.; Bertrand, S.; Bohler, S.; Edelstein, S.J.; Changeux, J.-P.; Bertrand, D. Critical Elements Determining Diversity in Agonist Binding and Desensitization of Neuronal Nicotinic Acetylcholine Receptors. J. Neurosci. 1998, 18, 648–657. [Google Scholar] [CrossRef]
- Olale, F.; Gerzanich, V.; Kuryatov, A.; Wang, F.; Lindstrom, J. Chronic nicotine exposure differentially affects the function of human α3, α4, and α7 neuronal nicotinic receptor subtypes. J. Pharmacol. Exp. Ther. 1997, 283, 675–683. [Google Scholar]
- Giniatullin, R.; Nistri, A.; Yakel, J.L. Desensitization of nicotinic ACh receptors: Shaping cholinergic signaling. Trends Neurosci. 2005, 28, 371–378. [Google Scholar] [CrossRef] [PubMed]
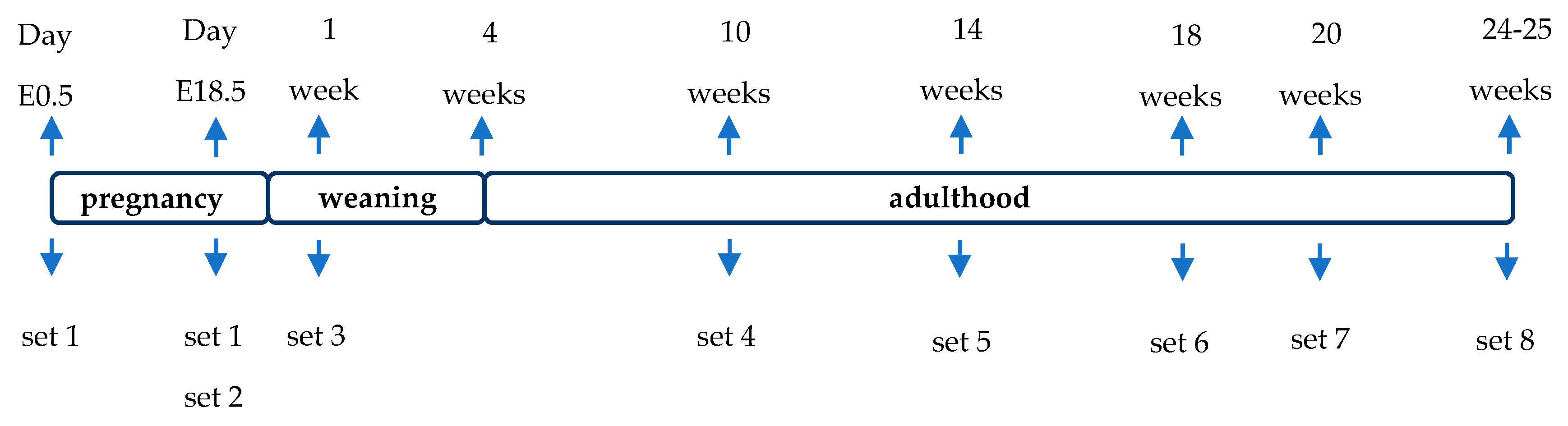


| Set 1 | Set 2 | Set 3 | Set 4 | Set 5 | Set 6 | Set 7 | Set 8 | |
|---|---|---|---|---|---|---|---|---|
| Body weight | X | X | X | X | X | |||
| Pancreas weight | X | X | X | |||||
| Non-fasting glycemia | X | X | X | X | ||||
| IPGTT, GSIS, ITT | X | X | ||||||
| IPPTT | X | |||||||
| 2DG Uptake | X | |||||||
| Food intake | X | X | X | X | ||||
| EchoMRI | X | X | X | |||||
| β- and α- cell mass | X | X | ||||||
| Insulin content | X | |||||||
| Static incubation | X | |||||||
| Hepatic glycogen content | X | |||||||
| Plasma NEFA | X | |||||||
| qPCR | X | X | X |
| Gene | Polarity | Sequence (5′ to 3′) | Genebank Number |
|---|---|---|---|
| M3 mAChR | Forward | ACCAGGCCACTCACTTACCG | 12671 |
| Reverse | CCCAAGCCAGACCAACCCTCATCACAC | ||
| α3 nicotinic subunit | Forward | ATATGAAAGCACAGAATGTAGCCA | 110,834 |
| Reverse | TGCACACCAGGATGAAAACCCA | ||
| α5 nicotinic subunit | Forward | TGATCAAGCATTCAATCTATGGGT | 110,835 |
| Reverse | CACAAAAGCCATTCCATATTGCC | ||
| α6 nicotinic subunit | Forward | CGAGAGTGTTCAATTCATAGCAGA | 11,440 |
| Reverse | GACTTTCCTGTGTTCCCAAGCA | ||
| α7 nicotinic subunit | Forward | TATCCCTGTAGCTGTCGGTC | 11,441 |
| Reverse | CCTGCCGAGTACAATGATATGCC | ||
| β2 nicotinic subunit | Forward | TTGAAATCTACTAAGCCCCACAAC | 11,444 |
| Reverse | TTCCCTGCTTCAAAACTTTTCCC | ||
| β4 nicotinic subunit | Forward | CCTTGCCCATTAAAGTCTATGCTC | 11,438 |
| Reverse | CACACACTCCGACCCTTG | ||
| BAD | Forward | TTCCAGATCCCAGAGTTTGAGCC | 12,015 |
| Reverse | CTGTAGCACTAGCGTCTTCC | ||
| BAX | Forward | CACCAAGAAGCTGAGCGAGT | 12,028 |
| Reverse | CCCCAGTTGAAGTTGCCATCA | ||
| BCL2 | Forward | AGCGGATATACCTTTCTTACCCT | 12,043 |
| Reverse | CTTGATTCTGGTGTTTCCCCGTTG | ||
| CXCL1 | Forward | CCGAAGTCATAGCCACACTCA | 14,825 |
| Reverse | TCAGAAGCCAGCGTTCACCA | ||
| F4/80 | Forward | CCAAGCCTATTATCTATACCCTCC | 13,733 |
| Reverse | CCAAGTTTGCCATCCGGTT | ||
| GLUT 2 | Forward | TCTGTTACCTTTCCTCGGCTTC | 20,526 |
| Reverse | ACAGCTAAGAACAACTCAAGCATT | ||
| IGF 2 | Forward | ACCCAGTGTTAATATGCCTCGT | 16,002 |
| Reverse | AAGACAGTAGGGAAGAGACAAGA | ||
| IL-1β | Forward | CCTGTGTTTTCCTCCTTGCCT | 16,176 |
| Reverse | TCTCAGCTTCAATGAAAGACCTC | ||
| IL-6 | Forward | GAGACTTCCATCCAGTTGCC | 16,193 |
| Reverse | AAGTAGGGAAGGCCGTGGTT | ||
| IL-15 | Forward | CTTGCTTATTTTTAATTTATTGCT | 16,168 |
| Reverse | AAAATATCCATACAACTTTATTCCAC | ||
| TLR4 | Forward | CAGCAGGTGGAATTGTATCGC | 21,898 |
| Reverse | TGCTCAGGATTCGAGGCTTT | ||
| TNFα | Forward | AGCACAGAAAGCATGATCCG | 21,926 |
| Reverse | ACCCCGAAGTTCAGTAGACAG | ||
| Cyclophilin A | Forward | CGTGGCCAACGATAAGAAGAA | 268,373 |
| Reverse | GTCTCCACCCTGGATCATGAA | ||
| HPRT | Forward | TCCTCCTCAGACCGCTTTT | 15,452 |
| Reverse | CCTGGTTCATCATCGCTAATC | ||
| RPL19 | Forward | GGGCAGGCATATGGGCATA | 19,921 |
| Reverse | GGCGGTCAATCTTCTTGGATT | ||
| TBP | Forward | GGGGAGCTGTGATGTGAAGT | 21,374 |
| Reverse | CCAGGAAATAATTCTGGCTCA |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gausserès, B.; Liu, J.; Foppen, E.; Tourrel-Cuzin, C.; Rodriguez Sanchez-Archidona, A.; Delangre, E.; Cruciani-Guglielmacci, C.; Pons, S.; Maskos, U.; Thorens, B.; et al. The Constitutive Lack of α7 Nicotinic Receptor Leads to Metabolic Disorders in Mouse. Biomolecules 2020, 10, 1057. https://doi.org/10.3390/biom10071057
Gausserès B, Liu J, Foppen E, Tourrel-Cuzin C, Rodriguez Sanchez-Archidona A, Delangre E, Cruciani-Guglielmacci C, Pons S, Maskos U, Thorens B, et al. The Constitutive Lack of α7 Nicotinic Receptor Leads to Metabolic Disorders in Mouse. Biomolecules. 2020; 10(7):1057. https://doi.org/10.3390/biom10071057
Chicago/Turabian StyleGausserès, Blandine, Junjun Liu, Ewout Foppen, Cécile Tourrel-Cuzin, Ana Rodriguez Sanchez-Archidona, Etienne Delangre, Céline Cruciani-Guglielmacci, Stéphanie Pons, Uwe Maskos, Bernard Thorens, and et al. 2020. "The Constitutive Lack of α7 Nicotinic Receptor Leads to Metabolic Disorders in Mouse" Biomolecules 10, no. 7: 1057. https://doi.org/10.3390/biom10071057
APA StyleGausserès, B., Liu, J., Foppen, E., Tourrel-Cuzin, C., Rodriguez Sanchez-Archidona, A., Delangre, E., Cruciani-Guglielmacci, C., Pons, S., Maskos, U., Thorens, B., Magnan, C., Movassat, J., & Maouche, K. (2020). The Constitutive Lack of α7 Nicotinic Receptor Leads to Metabolic Disorders in Mouse. Biomolecules, 10(7), 1057. https://doi.org/10.3390/biom10071057






