Lipids in Psychiatric Disorders: Functional and Potential Diagnostic Role as Blood Biomarkers
Abstract
1. Introduction
2. Lipids and Their Role in Neuropsychiatric Disorders
3. Effect of Medications on Lipid Metabolism
3.1. Antipsychotics
3.2. Antidepressants
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AA | Arachidonic acid |
| AD | Anxiety disorder |
| Apo | Apolipoprotein |
| BPD | Bipolar disorder |
| CAR | Acylcarnitine |
| CDCA | Chenodeoxycholic acid |
| CE | Cholesteryl ester |
| Cer | Ceramide |
| CNS | Central nervous system |
| DG | Diacylglycerol |
| DHA | Docosahexaenoic acid |
| FEP | First-episode psychosis |
| GAD | General anxiety disorder |
| GLCA | Glycolithocholic acid |
| GM | Monosialotetrahexosylganglioside |
| GP | Glycerophospholipid |
| HDL | High-density lipoprotein |
| HPA | Hypothalamic–pituitary–adrenal axis |
| IP3 | Inositol triphosphate |
| LCA | Lithocholic acid |
| LDL | Low-density lipoprotein |
| LPC | Lysophosphatidylcholine |
| LPC-O | Lysoplasmanyl-phosphatidylcholine |
| LPC-P | Lysoplasmenyl-phosphatidylcholine |
| LPE | Lysophosphatidylethanolamine |
| LPI | Lysophosphatidylinositol |
| MDD | Major depressive disorder |
| MOCA | Montreal Cognitive Assessment |
| PANSS | Positive and Negative Syndrome Scale |
| PC | Phosphatidylcholine |
| PC-O | Octadecyl-phosphatidylcholine |
| PC-P | Plasmenyl-phosphatidylcholine |
| PE | Phosphatidylethanolamine |
| PE-O | Octadecyl-phosphatidylethanolamine |
| PE-P | Plasmenyl-phosphatidylethanolamine |
| PG | Prostaglandin |
| PI | Phosphatidylinositol |
| PIP | Phosphatidylinositol phosphate |
| PLA2 | Phospholipase A2 |
| PS | Phosphatidylserine |
| PUFAs | Polyunsaturated fatty acids |
| RBANS | Repeated Battery for the Assessment of Neuropsychological Status |
| SCZ | Schizophrenia |
| SFA | Saturated fatty acid |
| SM | Sphingomyelin |
| SP | Sphingolipid |
| SREBP | Sterol regulatory element-binding protein |
| TAG | Triacylglycerol |
| TC | Total cholesterol |
| TG | Triacylglycerol |
| TGH | Triacylglycerol hydrolase |
| TLCA | Taurolithocholic acid |
| UHR | Ultra-high risk |
| VLDL | Very low-density lipoprotein |
References
- WHO. Transforming Mental Health for All; WHO: Geneva, Switzerland, 2022. [Google Scholar]
- LIPID MAPS. Available online: https://www.lipidmaps.org/ (accessed on 8 November 2023).
- Mesa-Herrera, F.; Taoro-González, L.; Valdés-Baizabal, C.; Diaz, M.; Marín, R. Lipid and Lipid Raft Alteration in Aging and Neurodegenerative Diseases: A Window for the Development of New Biomarkers. Int. J. Mol. Sci. 2019, 20, 3810. [Google Scholar] [CrossRef] [PubMed]
- Yoon, J.H.; Seo, Y.; Jo, Y.S.; Lee, S.; Cho, E.; Cazenave-Gassiot, A.; Shin, Y.S.; Moon, M.H.; An, H.J.; Wenk, M.R.; et al. Brain Lipidomics: From Functional Landscape to Clinical Significance. Sci. Adv. 2022, 8, eadc9317. [Google Scholar] [CrossRef] [PubMed]
- Cooper, G.M. The Cell: A Molecular Approach, 2nd ed.; Sinauer Associates: Sunderland, MA, USA, 2000; ISBN 0-87893-106. [Google Scholar]
- Kraft, M.L. Sphingolipid Organization in the Plasma Membrane and the Mechanisms that Influence It. Front. cell Dev. Biol. 2016, 4, 154. [Google Scholar] [CrossRef] [PubMed]
- Arriaga, L.R.; Rodríguez-García, R.; Moleiro, L.H.; Prévost, S.; López-Montero, I.; Hellweg, T.; Monroy, F. Dissipative Dynamics of Fluid Lipid Membranes Enriched in Cholesterol. Adv. Colloid Interface Sci. 2017, 247, 514–520. [Google Scholar] [CrossRef] [PubMed]
- Stieger, B.; Steiger, J.; Locher, K.P. Membrane Lipids and Transporter Function. Biochim. Biophys. Acta-Mol. Basis Dis. 2021, 1867, 166079. [Google Scholar] [CrossRef]
- Itri, R.; Junqueira, H.C.; Mertins, O.; Baptista, M.S. Membrane Changes under Oxidative Stress: The Impact of Oxidized Lipids. Biophys. Rev. 2014, 6, 47–61. [Google Scholar] [CrossRef]
- Hilgemann, D.W.; Dai, G.; Collins, A.; Lariccia, V.; Magi, S.; Deisl, C.; Fine, M. Lipid Signaling to Membrane Proteins: From Second Messengers to Membrane Domains and Adapter-Free Endocytosis. J. Gen. Physiol. 2018, 150, 211–224. [Google Scholar] [CrossRef]
- Podbielska, M.; Ariga, T.; Pokryszko-Dragan, A. Sphingolipid Players in Multiple Sclerosis: Their Influence on the Initiation and Course of the Disease. Int. J. Mol. Sci. 2022, 23, 5330. [Google Scholar] [CrossRef]
- Lauwers, E.; Goodchild, R.; Verstreken, P. Membrane Lipids in Presynaptic Function and Disease. Neuron 2016, 90, 11–25. [Google Scholar] [CrossRef]
- Martín, M.G.; Dotti, C.G. Plasma Membrane and Brain Dysfunction of the Old: Do We Age from Our Membranes? Front. cell Dev. Biol. 2022, 10, 1031007. [Google Scholar] [CrossRef]
- Postila, P.A.; Róg, T. A Perspective: Active Role of Lipids in Neurotransmitter Dynamics. Mol. Neurobiol. 2020, 57, 910–925. [Google Scholar] [CrossRef] [PubMed]
- Puchkov, D.; Haucke, V. Greasing the Synaptic Vesicle Cycle by Membrane Lipids. Trends Cell Biol. 2013, 23, 493–503. [Google Scholar] [CrossRef] [PubMed]
- Manna, M.; Niemelä, M.; Tynkkynen, J.; Javanainen, M.; Kulig, W.; Müller, D.J.; Rog, T.; Vattulainen, I. Mechanism of Allosteric Regulation of Β2-Adrenergic Receptor by Cholesterol. eLife 2016, 5, e18432. [Google Scholar] [CrossRef] [PubMed]
- Zhuo, C.; Hou, W.; Tian, H.; Wang, L.; Li, R. Lipidomics of the Brain, Retina, and Biofluids: From the Biological Landscape to Potential Clinical Application in Schizophrenia. Transl. Psychiatry 2020, 10, 391. [Google Scholar] [CrossRef]
- Ji, B.; Skup, M. Roles of Palmitoylation in Structural Long-Term Synaptic Plasticity. Mol. Brain 2021, 14, 8. [Google Scholar] [CrossRef] [PubMed]
- Buszka, A.; Pytyś, A.; Colvin, D.; Włodarczyk, J.; Wójtowicz, T. S-Palmitoylation of Synaptic Proteins in Neuronal Plasticity in Normal and Pathological Brains. Cells 2023, 12, 387. [Google Scholar] [CrossRef]
- Vaughen, J.P.; Theisen, E.; Clandinin, T.R. From Seconds to Days: Neural Plasticity Viewed through a Lipid Lens. Curr. Opin. Neurobiol. 2023, 80, 102702. [Google Scholar] [CrossRef]
- Bernal-Vega, S.; García-Juárez, M.; Camacho-Morales, A. Contribution of Ceramides Metabolism in Psychiatric Disorders. J. Neurochem. 2023, 164, 708–724. [Google Scholar] [CrossRef]
- Panov, A.; Orynbayeva, Z.; Vavilin, V.; Lyakhovich, V. Fatty Acids in Energy Metabolism of the Central Nervous System. Biomed Res. Int. 2014, 2014, 472459. [Google Scholar] [CrossRef]
- Lajtha, A.; Gibson, G.E.; Dienel, G.A. Handbook of Neurochemistry and Molecular Neurobiology: Brain Energetics. Integration of Molecular and Cellular Processes; Springer: New York, NY, USA, 2007; ISBN 9780387303468. [Google Scholar]
- Gorji, A. Neuroinflammation: The Pathogenic Mechanism of Neurological Disorders. Int. J. Mol. Sci. 2022, 23, 5744. [Google Scholar] [CrossRef]
- Yang, D.; Wang, X.; Zhang, L.; Fang, Y.; Zheng, Q.; Liu, X.; Yu, W.; Chen, S.; Ying, J.; Hua, F. Lipid Metabolism and Storage in Neuroglia: Role in Brain Development and Neurodegenerative Diseases. Cell Biosci. 2022, 12, 106. [Google Scholar] [CrossRef] [PubMed]
- Muzio, L.; Viotti, A.; Martino, G. Microglia in Neuroinflammation and Neurodegeneration: From Understanding to Therapy. Front. Neurosci. 2021, 15, 742065. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Liu, C.C.; Zheng, H.; Kanekiyo, T.; Atagi, Y.; Jia, L.; Wang, D.; N’songo, A.; Can, D.; Xu, H.; et al. LRP1 Modulates the Microglial Immune Response via Regulation of JNK and NF-ΚB Signaling Pathways. J. Neuroinflammation 2016, 13, 304. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Wu, L.; Chen, J.; Dong, L.; Chen, C.; Wen, Z.; Hu, J.; Fleming, I.; Wang, D.W. Metabolism Pathways of Arachidonic Acids: Mechanisms and Potential Therapeutic Targets. Signal Transduct. Target. Ther. 2021, 6, 94. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.Y.; Jin, H.K.; Bae, J.S. Sphingolipids in Neuroinflammation: A Potential Target for Diagnosis and Therapy. BMB Rep. 2020, 53, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Schneider, M.; Levant, B.; Reichel, M.; Gulbins, E.; Kornhuber, J.; Müller, C.P. Lipids in Psychiatric Disorders and Preventive Medicine. Neurosci. Biobehav. Rev. 2017, 76, 336–362. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Gao, Y.; Wang, D.; Hu, X.; Jiang, J.; Qing, Y.; Yang, X.; Cui, G.; Wang, P.; Zhang, J.; et al. Impaired Membrane Lipid Homeostasis in Schizophrenia. Schizophr. Bull. 2022, 48, 1125–1135. [Google Scholar] [CrossRef]
- Yao, J.K.; Dougherty, G.G.; Gautier, C.H.; Haas, G.L.; Condray, R.; Kasckow, J.W.; Kisslinger, B.L.; Gurklis, J.A.; Messamore, E. Prevalence and Specificity of the Abnormal Niacin Response: A Potential Endophenotype Marker in Schizophrenia. Schizophr. Bull. 2016, 42, 369–376. [Google Scholar] [CrossRef]
- Ong, W.-Y.; Farooqui, T.; Farooqui, A.A. Involvement of Cytosolic Phospholipase A(2), Calcium Independent Phospholipase A(2) and Plasmalogen Selective Phospholipase A(2) in Neurodegenerative and Neuropsychiatric Conditions. Curr. Med. Chem. 2010, 17, 2746–2763. [Google Scholar] [CrossRef]
- Wang, F.; Guo, L.; Zhang, T.; Cui, Z.; Wang, J.; Zhang, C.; Xue, F.; Zhou, C.; Li, B.; Tan, Q.; et al. Alterations in Plasma Lipidomic Profiles in Adult Patients with Schizophrenia and Major Depressive Disorder. Medicina 2022, 58, 1509. [Google Scholar] [CrossRef]
- Walther, A.; Cannistraci, C.V.; Simons, K.; Durán, C.; Gerl, M.J.; Wehrli, S.; Kirschbaum, C. Lipidomics in Major Depressive Disorder. Front. Psychiatry 2018, 9, 459. [Google Scholar] [CrossRef] [PubMed]
- Chan, P.; Suridjan, I.; Mohammad, D.; Herrmann, N.; Mazereeuw, G.; Hillyer, L.M.; Ma, D.W.L.; Oh, P.I.; Lanctôt, K.L. Novel Phospholipid Signature of Depressive Symptoms in Patients with Coronary Artery Disease. J. Am. Heart Assoc. 2018, 7, e008278. [Google Scholar] [CrossRef] [PubMed]
- Healy-Stoffel, M.; Levant, B. N-3 (Omega-3) Fatty Acids: Effects on Brain Dopamine Systems and Potential Role in the Etiology and Treatment of Neuropsychiatric Disorders. CNS Neurol. Disord.-Drug Targets 2018, 17, 216–232. [Google Scholar] [CrossRef]
- Hussain, G.; Anwar, H.; Rasul, A.; Imran, A.; Qasim, M.; Zafar, S.; Imran, M.; Kamran, S.K.S.; Aziz, N.; Razzaq, A.; et al. Lipids as Biomarkers of Brain Disorders. Crit. Rev. Food Sci. Nutr. 2020, 60, 351–374. [Google Scholar] [CrossRef] [PubMed]
- Riddle, E.L.; Rau, K.S.; Topham, M.K.; Hanson, G.R.; Fleckenstein, A.E. Ceramide-Induced Alterations in Dopamine Transporter Function. Eur. J. Pharmacol. 2003, 458, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Song, X.; Liu, X.; Pu, J.; Gui, S.; Xu, S.; Tian, L.; Zhong, X.; Zhao, L.; Wang, H.; et al. Alteration of Lipids and Amino Acids in Plasma Distinguish Schizophrenia Patients from Controls: A Targeted Metabolomics Study. Psychiatry Clin. Neurosci. 2021, 75, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Tkachev, A.; Stekolshchikova, E.; Anikanov, N.; Zozulya, S.; Barkhatova, A.; Klyushnik, T.; Petrova, D. Shorter Chain Triglycerides Are Negatively Associated with Symptom Improvement in Schizophrenia. Biomolecules 2021, 11, 720. [Google Scholar] [CrossRef]
- Yan, L.; Zhou, J.; Wang, D.; Si, D.; Liu, Y.; Zhong, L.; Yin, Y. Unbiased Lipidomic Profiling Reveals Metabolomic Changes during the Onset and Antipsychotics Treatment of Schizophrenia Disease. Metabolomics 2018, 14, 80. [Google Scholar] [CrossRef]
- Orešič, M.; Seppänen-Laakso, T.; Sun, D.; Tang, J.; Therman, S.; Viehman, R.; Mustonen, U.; van Erp, T.G.; Hyötyläinen, T.; Thompson, P.; et al. Phospholipids and Insulin Resistance in Psychosis: A Lipidomics Study of Twin Pairs Discordant for Schizophrenia. Genome Med. 2012, 4, 1. [Google Scholar] [CrossRef]
- Costa, A.C.; Riça, L.B.; van de Bilt, M.; Zandonadi, F.S.; Gattaz, W.F.; Talib, L.L.; Sussulini, A. Application of Lipidomics in Psychiatry: Plasma-Based Potential Biomarkers in Schizophrenia and Bipolar Disorder. Metabolites 2023, 13, 600. [Google Scholar] [CrossRef]
- Wang, D.; Sun, X.; Maziade, M.; Mao, W.; Zhang, C.; Wang, J.; Cao, B. Characterising Phospholipids and Free Fatty Acids in Patients with Schizophrenia: A Case-Control Study. World J. Biol. Psychiatry 2021, 22, 161–174. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Cheng, S.L.; Fei, Q.; Gu, H.; Raftery, D.; Cao, B.; Sun, X.; Yan, J.; Zhang, C.; Wang, J. Metabolic Profiling Identifies Phospholipids as Potential Serum Biomarkers for Schizophrenia. Psychiatry Res. 2019, 272, 18–29. [Google Scholar] [CrossRef] [PubMed]
- Frajerman, A.; Chaumette, B.; Farabos, D.; Despres, G.; Simonard, C.; Lamazière, A.; Krebs, M.O.; Kebir, O. Membrane Lipids in Ultra-High-Risk Patients: Potential Predictive Biomarkers of Conversion to Psychosis. Nutrients 2023, 15, 2215. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Yang, P.; Tang, M.; Liu, Y.; Guo, W.; Lang, B.; Wang, J.; Wu, H.; Tang, H.; Yu, Y.; et al. Reduced Erythrocyte Membrane Polyunsaturated Fatty Acid Levels Indicate Diminished Treatment Response in Patients with Multi- versus First-Episode Schizophrenia. Schizophrenia 2022, 8, 7. [Google Scholar] [CrossRef] [PubMed]
- Goh, X.X.; Tang, P.Y.; Tee, S.F. Blood-Based Oxidation Markers in Medicated and Unmedicated Schizophrenia Patients: A Meta-Analysis. Asian J. Psychiatr. 2022, 67, 102932. [Google Scholar] [CrossRef] [PubMed]
- Song, M.; Liu, Y.; Zhou, J.; Shi, H.; Su, X.; Shao, M.; Yang, Y.; Wang, X.; Zhao, J.; Guo, D.; et al. Potential Plasma Biomarker Panels Identification for the Diagnosis of First-Episode Schizophrenia and Monitoring Antipsychotic Monotherapy with the Use of Metabolomics Analyses. Psychiatry Res. 2023, 321, 115070. [Google Scholar] [CrossRef] [PubMed]
- Wei, Y.; Wang, T.; Li, G.; Feng, J.; Deng, L.; Xu, H.; Yin, L.; Ma, J.; Chen, D.; Chen, J. Investigation of Systemic Immune-Inflammation Index, Neutrophil/High-Density Lipoprotein Ratio, Lymphocyte/High-Density Lipoprotein Ratio, and Monocyte/High-Density Lipoprotein Ratio as Indicators of Inflammation in Patients with Schizophrenia and Bipolar Disorder. Front. Psychiatry 2022, 13, 941728. [Google Scholar] [CrossRef]
- Nandeesha, H.; Keshri, N.; Rajappa, M.; Menon, V. Association of Hyperglycaemia and Hyperlipidaemia with Cognitive Dysfunction in Schizophrenia Spectrum Disorder. Arch. Physiol. Biochem. 2023, 129, 497–504. [Google Scholar] [CrossRef]
- McEvoy, J.; Baillie, R.A.; Zhu, H.; Buckley, P.; Keshavan, M.S.; Nasrallah, H.A.; Dougherty, G.G.; Yao, J.K.; Kaddurah-Daouk, R. Lipidomics Reveals Early Metabolic Changes in Subjects with Schizophrenia: Effects of Atypical Antipsychotics. PLoS ONE 2013, 8, e68717. [Google Scholar] [CrossRef]
- Kaddurah-Daouk, R.; McEvoy, J.; Baillie, R.; Zhu, H.K.; Yao, J.; Nimgaonkar, V.L.; Buckley, P.F.; Keshavan, M.S.; Georgiades, A.; Nasrallah, H.A. Impaired Plasmalogens in Patients with Schizophrenia. Psychiatry Res. 2012, 198, 347–352. [Google Scholar] [CrossRef]
- Guidara, W.; Messedi, M.; Naifar, M.; Maalej, M.; Khrouf, W.; Grayaa, S.; Maalej, M.; Bonnefont-Rousselot, D.; Lamari, F.; Ayadi, F. Plasma Oxysterols in Drug-Free Patients with Schizophrenia. J. Steroid Biochem. Mol. Biol. 2022, 221, 106123. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; Ye, X.; Wang, X.; Lin, Y.; Zhu, C.; Pan, J.; Yin, X.; Ye, M.; Lv, W.; Tang, W.; et al. Serum Total Cholesterol Levels Associated with Immediate Memory Performance in Patients with Chronic Schizophrenia. Schizophr. Res. 2023, 255, 256–260. [Google Scholar] [CrossRef] [PubMed]
- Pillai, R.R.; Wilson, A.B.; Premkumar, N.R.; Kattimani, S.; Sagili, H.; Rajendiran, S. Low Serum Levels of High-Density Lipoprotein Cholesterol (HDL-c) as an Indicator for the Development of Severe Postpartum Depressive Symptoms. PLoS ONE 2018, 13, e0192811. [Google Scholar] [CrossRef]
- Liu, X.; Li, J.; Zheng, P.; Zhao, X.; Zhou, C.; Hu, C.; Hou, X.; Wang, H.; Xie, P.; Xu, G. Plasma Lipidomics Reveals Potential Lipid Markers of Major Depressive Disorder. Anal. Bioanal. Chem. 2016, 408, 6497–6507. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Zheng, P.; Zhao, X.; Zhang, Y.; Hu, C.; Li, J.; Zhao, J.; Zhou, J.; Xie, P.; Xu, G. Discovery and Validation of Plasma Biomarkers for Major Depressive Disorder Classification Based on Liquid Chromatography-Mass Spectrometry. J. Proteome Res. 2015, 14, 2322–2330. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.Y.; Lee, J.W.; Lee, M.Y.; Kim, S.H.; Mok, H.J.; Ha, K.; Ahn, Y.M.; Kim, K.P. Serum Lipidomic Analysis for the Discovery of Biomarkers for Major Depressive Disorder in Drug-Free Patients. Psychiatry Res. 2018, 265, 174–182. [Google Scholar] [CrossRef]
- Zhang, T.; Guo, L.; Li, R.; Wang, F.; Yang, W.M.; Yang, J.B.; Cui, Z.Q.; Zhou, C.H.; Chen, Y.H.; Yu, H.; et al. Alterations of Plasma Lipids in Adult Women with Major Depressive Disorder and Bipolar Depression. Front. Psychiatry 2022, 13, 927817. [Google Scholar] [CrossRef]
- Kuwano, N.; Kato, T.A.; Setoyama, D.; Sato-Kasai, M.; Shimokawa, N.; Hayakawa, K.; Ohgidani, M.; Sagata, N.; Kubo, H.; Kishimoto, J.; et al. Tryptophan-Kynurenine and Lipid Related Metabolites as Blood Biomarkers for First-Episode Drug-Naïve Patients with Major Depressive Disorder: An Exploratory Pilot Case-Control Study. J. Affect. Disord. 2018, 231, 74–82. [Google Scholar] [CrossRef]
- Demirkan, A.; Isaacs, A.; Ugocsai, P.; Liebisch, G.; Struchalin, M.; Rudan, I.; Wilson, J.F.; Pramstaller, P.P.; Gyllensten, U.; Campbell, H.; et al. Plasma Phosphatidylcholine and Sphingomyelin Concentrations Are Associated with Depression and Anxiety Symptoms in a Dutch Family-Based Lipidomics Study. J. Psychiatr. Res. 2013, 47, 357–362. [Google Scholar] [CrossRef]
- Liu, Z.; Cai, Y.; Zhang, X.; Zhu, Z.; He, J. High Serum Levels of Malondialdehyde and Antioxidant Enzymes Are Associated with Post-Stroke Anxiety. Neurol. Sci. 2018, 39, 999–1007. [Google Scholar] [CrossRef]
- Dong, M.X.; Hu, L.; Wei, Y.D.; Chen, G.H. Metabolomics Profiling Reveals Altered Lipid Metabolism and Identifies a Panel of Lipid Metabolites as Biomarkers for Parkinson’s Disease Related Anxiety Disorder. Neurosci. Lett. 2021, 745, 135626. [Google Scholar] [CrossRef] [PubMed]
- Kui, H.; Su, H.; Wang, Q.; Liu, C.; Li, Y.; Tian, Y.; Kong, J.; Sun, G.; Huang, J. Serum Metabolomics Study of Anxiety Disorder Patients Based on LC-MS. Clin. Chim. Acta. 2022, 533, 131–143. [Google Scholar] [CrossRef] [PubMed]
- De Berardis, D.; Serroni, N.; Campanella, D.; Marini, S.; Rapini, G.; Valchera, A.; Iasevoli, F.; Mazza, M.; Fornaro, M.; Perna, G.; et al. Alexithymia, Suicide Ideation, C-Reactive Protein, and Serum Lipid Levels Among Outpatients with Generalized Anxiety Disorder. Arch. Suicide Res. 2017, 21, 100–112. [Google Scholar] [CrossRef] [PubMed]
- Sevincok, L.; Buyukozturk, A.; Dereboy, F. Serum Lipid Concentrations in Patients with Comorbid Generalized Anxiety Disorder and Major Depressive Disorder. Can. J. Psychiatry 2001, 46, 68–71. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Jiang, C.; Chen, L.; Wu, S.; Lin, J.; Gao, L.; Xie, B.; Zheng, D.; Yang, R.; Li, S.; et al. A Cross-Sectional Study to Investigate the Correlation between Depression Comorbid with Anxiety and Serum Lipid Levels. Compr. Psychiatry 2016, 69, 163–168. [Google Scholar] [CrossRef] [PubMed]
- Hu, M.X.; Penninx, B.W.J.H.; de Geus, E.J.C.; Lamers, F.; Kuan, D.C.H.; Wright, A.G.C.; Marsland, A.L.; Muldoon, M.F.; Manuck, S.B.; Gianaros, P.J. Associations of Immunometabolic Risk Factors with Symptoms of Depression and Anxiety: The Role of Cardiac Vagal Activity. Brain. Behav. Immun. 2018, 73, 493–503. [Google Scholar] [CrossRef] [PubMed]
- Pistorio, E.; Luca, M.; Luca, A.; Messina, V.; Calandra, C. Autonomic Nervous System and Lipid Metabolism: Findings in Anxious-Depressive Spectrum and Eating Disorders. Lipids Health Dis. 2011, 10, 192. [Google Scholar] [CrossRef]
- Thesing, C.S.; Bot, M.; Milaneschi, Y.; Giltay, E.J.; Penninx, B.W.J.H. Omega-3 and Omega-6 Fatty Acid Levels in Depressive and Anxiety Disorders. Psychoneuroendocrinology 2018, 87, 53–62. [Google Scholar] [CrossRef]
- Verly-Miguel, M.V.B.; Farias, D.R.; Pinto, T.d.J.P.; Lepsch, J.; Nardi, A.E.; Kac, G. Serum Docosahexaenoic Acid (DHA) Is Inversely Associated with Anxiety Disorders in Early Pregnancy. J. Anxiety Disord. 2015, 30, 34–40. [Google Scholar] [CrossRef]
- MahmoudianDehkordi, S.; Bhattacharyya, S.; Brydges, C.R.; Jia, W.; Fiehn, O.; Rush, A.J.; Dunlop, B.W.; Kaddurah-Daouk, R. Gut Microbiome-Linked Metabolites in the Pathobiology of Major Depression with or without Anxiety—A Role for Bile Acids. Front. Neurosci. 2022, 16, 937906. [Google Scholar] [CrossRef]
- Xing, Y.; Tang, Y.; Zhao, L.; Wang, Q.; Qin, W.; Ji, X.; Zhang, J.; Jia, J. Associations between Plasma Ceramides and Cognitive and Neuropsychiatric Manifestations in Parkinson’s Disease Dementia. J. Neurol. Sci. 2016, 370, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.Y.; Arnold, D.; Qiu, C.F.; Miller, R.S.; Williams, M.A.; Enquobahrie, D.A. Association of Serum Vitamin D with Symptoms of Depression and Anxiety in Early Pregnancy. J. Women’s Heal. 2014, 23, 588. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Zhu, H.; Harshfield, G.A.; Treiber, F.A.; Pollock, J.S.; Pollock, D.; Okereke, O.I.; Su, S.; Dong, Y. Serum 25-Hydroxyvitamin D Concentrations Are Associated with Mental Health and Psychosocial Stress in Young Adults. Nutrients 2020, 12, 1938. [Google Scholar] [CrossRef] [PubMed]
- Casseb, G.A.S.; Ambrósio, G.; Rodrigues, A.L.S.; Kaster, M.P. Levels of 25-Hydroxyvitamin D3, Biochemical Parameters and Symptoms of Depression and Anxiety in Healthy Individuals. Metab. Brain Dis. 2019, 34, 527–535. [Google Scholar] [CrossRef] [PubMed]
- Tao, S.; Zhang, Y.; Wang, Q.; Qiao, C.; Deng, W.; Liang, S.; Wei, J.; Wei, W.; Yu, H.; Li, X.; et al. Identifying Transdiagnostic Biological Subtypes across Schizophrenia, Bipolar Disorder, and Major Depressive Disorder Based on Lipidomics Profiles. Front. cell Dev. Biol. 2022, 10, 969575. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Sun, L.; Zhao, A.; Hu, X.; Qing, Y.; Jiang, J.; Yang, C.; Xu, T.; Wang, P.; Liu, J.; et al. Serum Fatty Acid Patterns in Patients with Schizophrenia: A Targeted Metabonomics Study. Transl. Psychiatry 2017, 7, e1176. [Google Scholar] [CrossRef]
- Zhou, X.; Long, T.; Haas, G.L.; Cai, H.L.; Yao, J.K. Reduced Levels and Disrupted Biosynthesis Pathways of Plasma Free Fatty Acids in First-Episode Antipsychotic-Naïve Schizophrenia Patients. Front. Neurosci. 2020, 14, 784. [Google Scholar] [CrossRef]
- Zhou, X.; Liu, L.; Lan, X.; Cohen, D.; Zhang, Y.; Ravindran, A.V.; Yuan, S.; Zheng, P.; Coghill, D.; Yang, L.; et al. Polyunsaturated Fatty Acids Metabolism, Purine Metabolism and Inosine as Potential Independent Diagnostic Biomarkers for Major Depressive Disorder in Children and Adolescents. Mol. Psychiatry 2019, 24, 1478–1488. [Google Scholar] [CrossRef]
- Assies, J.; Pouwer, F.; Lok, A.; Mocking, R.J.T.; Bockting, C.L.H.; Visser, I.; Abeling, N.G.G.M.; Duran, M.; Schene, A.H. Plasma and Erythrocyte Fatty Acid Patterns in Patients with Recurrent Depression: A Matched Case-Control Study. PLoS ONE 2010, 5, e10635. [Google Scholar] [CrossRef]
- Scola, G.; Versace, A.; Metherel, A.H.; Monsalve-Castro, L.A.; Phillips, M.L.; Bazinet, R.P.; Andreazza, A.C. Alterations in Peripheral Fatty Acid Composition in Bipolar and Unipolar Depression. J. Affect. Disord. 2018, 233, 86–91. [Google Scholar] [CrossRef]
- Pomponi, M.; Janiri, L.; La Torre, G.; Di Stasio, E.; Di Nicola, M.; Mazza, M.; Martinotti, G.; Bria, P.; Lippa, S.; Natili, R.; et al. Plasma Levels of N-3 Fatty Acids in Bipolar Patients: Deficit Restricted to DHA. J. Psychiatr. Res. 2013, 47, 337–342. [Google Scholar] [CrossRef]
- Sobczak, S.; Honig, A.; Christophe, M.; Maes, M.; Helsdingen, R.W.C.; De Vriese, S.; Reidel, W.J. Lower High-Density Lipoprotein Cholesterol and Increased Omega-6 Polyunsaturated Fatty Acids in First-Degree Relatives of Bipolar Patients. Psychol. Med. 2004, 34, 103–112. [Google Scholar] [CrossRef]
- McNamara, R.K.; Jandacek, R.; Tso, P.; Blom, T.J.; Welge, J.A.; Strawn, J.R.; Adler, C.M.; DelBello, M.P.; Strakowski, S.M. First-Episode Bipolar Disorder Is Associated with Erythrocyte Membrane Docosahexaenoic Acid Deficits: Dissociation from Clinical Response to Lithium or Quetiapine. Psychiatry Res. 2015, 230, 447–453. [Google Scholar] [CrossRef][Green Version]
- Igarashi, M.; Ma, K.; Gao, F.; Kim, H.W.; Greenstein, D.; Rapoport, S.I.; Rao, J.S. Brain Lipid Concentrations in Bipolar Disorder. J. Psychiatr. Res. 2010, 44, 177–182. [Google Scholar] [CrossRef]
- Saunders, E.F.H.; Reider, A.; Singh, G.; Gelenberg, A.J.; Rapoport, S.I. Low Unesterified: Esterified Eicosapentaenoic Acid (EPA) Plasma Concentration Ratio Is Associated with Bipolar Disorder Episodes, and Omega-3 Plasma Concentrations Are Altered by Treatment. Bipolar Disord. 2015, 17, 729–742. [Google Scholar] [CrossRef]
- Mongan, D.; Healy, C.; Jones, H.J.; Zammit, S.; Cannon, M.; Cotter, D.R. Plasma Polyunsaturated Fatty Acids and Mental Disorders in Adolescence and Early Adulthood: Cross-Sectional and Longitudinal Associations in a General Population Cohort. Transl. Psychiatry 2021, 11, 321. [Google Scholar] [CrossRef]
- Li, X.; Yuan, X.; Pang, L.; Zhang, S.; Li, Y.; Huang, X.; Fan, X.; Song, X. The Effect of Serum Lipids and Short-Chain Fatty Acids on Cognitive Functioning in Drug-Naïve, First Episode Schizophrenia Patients. Psychiatry Res. 2022, 313, 114582. [Google Scholar] [CrossRef]
- Cao, B.; Wang, D.; Pan, Z.; McIntyre, R.S.; Brietzke, E.; Subramanieapillai, M.; Nozari, Y.; Wang, J. Metabolic Profiling for Water-Soluble Metabolites in Patients with Schizophrenia and Healthy Controls in a Chinese Population: A Case-Control Study. World J. Biol. Psychiatry 2020, 21, 357–367. [Google Scholar] [CrossRef]
- Jadoon, A.; Chiu, C.C.; McDermott, L.; Cunningham, P.; Frangou, S.; Chang, C.J.; Sun, I.W.; Liu, S.I.; Lu, M.L.; Su, K.P.; et al. Associations of Polyunsaturated Fatty Acids with Residual Depression or Anxiety in Older People with Major Depression. J. Affect. Disord. 2012, 136, 918–925. [Google Scholar] [CrossRef] [PubMed]
- Kriisa, K.; Leppik, L.; Balõtšev, R.; Ottas, A.; Soomets, U.; Koido, K.; Volke, V.; Innos, J.; Haring, L.; Vasar, E.; et al. Profiling of Acylcarnitines in First Episode Psychosis before and after Antipsychotic Treatment. J. Proteome Res. 2017, 16, 3558–3566. [Google Scholar] [CrossRef] [PubMed]
- Cao, B.; Wang, D.; Pan, Z.; Brietzke, E.; McIntyre, R.S.; Musial, N.; Mansur, R.B.; Subramanieapillai, M.; Zeng, J.; Huang, N.; et al. Characterizing Acyl-Carnitine Biosignatures for Schizophrenia: A Longitudinal Pre- and Post-Treatment Study. Transl. Psychiatry 2019, 9, 19. [Google Scholar] [CrossRef] [PubMed]
- Mamalakis, G.; Jansen, E.; Cremers, H.; Kiriakakis, M.; Tsibinos, G.; Kafatos, A. Depression and Adipose and Serum Cholesteryl Ester Polyunsaturated Fatty Acids in the Survivors of the Seven Countries Study Population of Crete. Eur. J. Clin. Nutr. 2006, 60, 1016–1023. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Beydoun, M.A.; Beydoun, H.A.; Dore, G.A.; Fanelli-Kuczmarski, M.T.; Evans, M.K.; Zonderman, A.B. Total Serum Cholesterol, Atherogenic Indices and Their Longitudinal Association with Depressive Symptoms among US Adults. Transl. Psychiatry 2015, 5, e518. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, H.C.; Klassen, A.; Pedrini, M.; Carvalho, M.S.; Rizzo, L.B.; Noto, M.N.; Zeni-Graiff, M.; Sethi, S.; Fonseca, F.A.H.; Tasic, L.; et al. A Preliminary Study of Bipolar Disorder Type I by Mass Spectrometry-Based Serum Lipidomics. Psychiatry Res. 2017, 258, 268–273. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.J.; Tsai, S.Y.; Chung, K.H.; Chen, P.H.; Huang, S.H.; Kuo, C.J. State-Dependent Alterations of Lipid Profiles in Patients with Bipolar Disorder. Int. J. Psychiatry Med. 2018, 53, 273–281. [Google Scholar] [CrossRef] [PubMed]
- Peter, H.; Hand, I.; Hohagen, F.; Koenig, A.; Mindermann, O.; Oeder, F.; Wittich, M. Serum Cholesterol Level Comparison: Control Subjects, Anxiety Disorder Patients, and Obsessive-Compulsive Disorder Patients. Can. J. Psychiatry 2002, 47, 557–561. [Google Scholar] [CrossRef] [PubMed]
- De Lacerda, A.L.T.; Caetano, D.; Caetano, S.C. Cholesterol Levels in Panic Disorder, Generalized Anxiety Disorder and Major Depression. Arq. Neuropsiquiatr. 2000, 58, 408–411. [Google Scholar] [CrossRef][Green Version]
- Cenik, B.; Cenik, C.; Snyder, M.P.; Brown, E.S. Plasma Sterols and Depressive Symptom Severity in a Population-Based Cohort. PLoS ONE 2017, 12, e0184382. [Google Scholar] [CrossRef]
- Sun, N.; Zhang, J.; Wang, J.; Liu, Z.; Wang, X.; Kang, P.; Yang, C.; Liu, P.; Zhang, K. Abnormal Gut Microbiota and Bile Acids in Patients with First-Episode Major Depressive Disorder and Correlation Analysis. Psychiatry Clin. Neurosci. 2022, 76, 321–328. [Google Scholar] [CrossRef]
- Köhnke, C.; Herrmann, M.; Berger, K. Associations of Major Depressive Disorder and Related Clinical Characteristics with 25-Hydroxyvitamin D Levels in Middle-Aged Adults. Nutr. Neurosci. 2022, 25, 1209–1218. [Google Scholar] [CrossRef]
- Boerman, R.; Cohen, D.; Schulte, P.F.J.; Nugter, A. Prevalence of Vitamin D Deficiency in Adult Outpatients With Bipolar Disorder or Schizophrenia. J. Clin. Psychopharmacol. 2016, 36, 588–592. [Google Scholar] [CrossRef] [PubMed]
- Wood, P.L.; Unfried, G.; Whitehead, W.; Phillipps, A.; Wood, J.A. Dysfunctional Plasmalogen Dynamics in the Plasma and Platelets of Patients with Schizophrenia. Schizophr. Res. 2015, 161, 506–510. [Google Scholar] [CrossRef] [PubMed]
- Leppik, L.; Parksepp, M.; Janno, S.; Koido, K.; Haring, L.; Vasar, E.; Zilmer, M. Profiling of Lipidomics before and after Antipsychotic Treatment in First-Episode Psychosis. Eur. Arch. Psychiatry Clin. Neurosci. 2020, 270, 59–70. [Google Scholar] [CrossRef]
- He, Y.; Yu, Z.; Giegling, I.; Xie, L.; Hartmann, A.M.; Prehn, C.; Adamski, J.; Kahn, R.; Li, Y.; Illig, T.; et al. Schizophrenia Shows a Unique Metabolomics Signature in Plasma. Transl. Psychiatry 2012, 2, e149. [Google Scholar] [CrossRef] [PubMed]
- Stirton, H.; Meek, B.P.; Edel, A.L.; Solati, Z.; Surendran, A.; Aukema, H.; Modirrousta, M.; Ravandi, A. Oxolipidomics Profile in Major Depressive Disorder: Comparing Remitters and Non-Remitters to Repetitive Transcranial Magnetic Stimulation Treatment. PLoS ONE 2021, 16, e0246592. [Google Scholar] [CrossRef] [PubMed]
- Costa, A.C.; Joaquim, H.P.G.; Talib, L.L.; Serpa, M.H.; Zanetti, M.V.; Gattaz, W.F. Plasma Metabolites in First Episode Psychoses. Schizophr. Res. 2019, 206, 468–470. [Google Scholar] [CrossRef]
- Cai, H.L.; Cao, T.; Li, N.N.; Fang, P.F.; Xu, P.; Wu, X.X.; Zhang, B.K.; Xiang, D.X. Quantitative Monitoring of a Panel of Stress-Induced Biomarkers in Human Plasma by Liquid Chromatography–Tandem Mass Spectrometry: An Application in a Comparative Study between Depressive Patients and Healthy Subjects. Anal. Bioanal. Chem. 2019, 411, 5765–5777. [Google Scholar] [CrossRef]
- Tkachev, A.I.; Stekolshchikova, E.A.; Morozova, A.Y.; Anikanov, N.A.; Zorkina, Y.A.; Alekseyeva, P.N.; Khobta, E.B.; Andreyuk, D.S.; Zozulya, S.A.; Barkhatova, A.N.; et al. Ceramides: Shared Lipid Biomarkers of Cardiovascular Disease and Schizophrenia. Consort. Psychiatr. 2021, 2, 35–43. [Google Scholar] [CrossRef]
- Gracia-Garcia, P.; Rao, V.; Haughey, N.J.; Banduru, V.V.R.; Smith, G.; Rosenberg, P.B.; Lobo, A.; Lyketsos, C.G.; Mielke, M.M. Elevated Plasma Ceramides in Depression. J. Neuropsychiatry Clin. Neurosci. 2011, 23, 215–218. [Google Scholar] [CrossRef]
- Brunkhorst-Kanaan, N.; Klatt-Schreiner, K.; Hackel, J.; Schröter, K.; Trautmann, S.; Hahnefeld, L.; Wicker, S.; Reif, A.; Thomas, D.; Geisslinger, G.; et al. Targeted Lipidomics Reveal Derangement of Ceramides in Major Depression and Bipolar Disorder. Metabolism 2019, 95, 65–76. [Google Scholar] [CrossRef]
- Brunkhorst-Kanaan, N.; Trautmann, S.; Schreiber, Y.; Thomas, D.; Kittel-Schneider, S.; Gurke, R.; Geisslinger, G.; Reif, A.; Tegeder, I. Sphingolipid and Endocannabinoid Profiles in Adult Attention Deficit Hyperactivity Disorder. Biomedicines 2021, 9, 1173. [Google Scholar] [CrossRef] [PubMed]
- Solberg, D.K.; Bentsen, H.; Refsum, H.; Andreassen, O.A. Lipid Profiles in Schizophrenia Associated with Clinical Traits: A Five Year Follow-up Study. BMC Psychiatry 2016, 16, 299. [Google Scholar] [CrossRef] [PubMed]
- Maes, M.; Mihaylova, I.; Kubera, M.; Uytterhoeven, M.; Vrydags, N.; Bosmans, E. Lower Plasma Coenzyme Q10 in Depression: A Marker for Treatment Resistance and Chronic Fatigue in Depression and a Risk Factor to Cardiovascular Disorder in That Illness. Neuro-Endocrinol. Lett. 2009, 30, 462–469. [Google Scholar] [PubMed]
- Hurşitoğlu, O.; Orhan, F.Ö.; Kurutaş, E.B.; Doğaner, A.; Durmuş, H.T.; Kopar, H. Diagnostic Performance of Increased Malondialdehyde Level and Oxidative Stress in Patients with Schizophrenia. Noro Psikiyatr. Ars. 2021, 58, 184–188. [Google Scholar] [CrossRef] [PubMed]
- Günes, M.; Camkurt, M.A.; Bulut, M.; Demir, S.; Ibiloglu, A.O.; Kaya, M.C.; Atli, A.; Kaplan, I.; Sir, A. Evaluation of Paraoxonase, Arylesterase and Malondialdehyde Levels in Schizophrenia Patients Taking Typical, Atypical and Combined Antipsychotic Treatment. Clin. Psychopharmacol. Neurosci. 2016, 14, 345–350. [Google Scholar] [CrossRef]
- Uddin, S.M.N.; Sultana, F.; Uddin, M.G.; Dewan, S.M.R.; Hossain, M.K.; Islam, M.S. Effect of Antioxidant, Malondialdehyde, Macro-Mineral, and Trace Element Serum Concentrations in Bangladeshi Patients with Schizophrenia: A Case-Control Study. Health Sci. Rep. 2021, 4, e291. [Google Scholar] [CrossRef]
- Islam, M.R.; Islam, M.R.; Ahmed, I.; Moktadir, A.A.; Nahar, Z.; Islam, M.S.; Shahid, S.F.B.; Islam, S.N.; Islam, M.S.; Hasnat, A. Elevated Serum Levels of Malondialdehyde and Cortisol Are Associated with Major Depressive Disorder: A Case-Control Study. SAGE Open Med. 2018, 6, 2050312118773953. [Google Scholar] [CrossRef]
- Alvarez-Mon, M.A.; Ortega, M.A.; García-Montero, C.; Fraile-Martinez, O.; Lahera, G.; Monserrat, J.; Gomez-Lahoz, A.M.; Molero, P.; Gutierrez-Rojas, L.; Rodriguez-Jimenez, R.; et al. Differential Malondialdehyde (MDA) Detection in Plasma Samples of Patients with Major Depressive Disorder (MDD): A Potential Biomarker. J. Int. Med. Res. 2022, 50, 3000605221094995. [Google Scholar] [CrossRef]
- Aydemir, Ö.; Çubukçuoğlu, Z.; Erdin, S.; Taş, C.; Onur, E.; Berk, M. Oxidative Stress Markers, Cognitive Functions, and Psychosocial Functioning in Bipolar Disorder: An Empirical Cross-Sectional Study. Rev. Bras. Psiquiatr. 2014, 36, 293–297. [Google Scholar] [CrossRef]
- Islam, M.R.; Ahmed, M.U.; Islam, M.S.; Sayeed, M.S.B.; Sadia, F.; Chowdhury, Z.S.; Nahar, Z.; Hasnat, A. Comparative Analysis of Serum Malondialdehyde, Antioxidant Vitamins and Immunoglobulin Levels in Patients Suffering from Generalized Anxiety Disorder. Drug Res. 2014, 64, 406–411. [Google Scholar] [CrossRef]
- Uyar, B.; Budak, E.A. Effects of Major Depressive Disorder on Monocytes, High-Density Lipoprotein (HDL) and Monocyte to HDL Ratio: A Case-Control Study. Psychiatr. Danub. 2022, 34, 687–694. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, H.R.; Kellogg, M.D.; Kramer, F.M.; Bathalon, G.P.; Lesher, L.L. Lipid and Other Plasma Markers Are Associated with Anxiety, Depression, and Fatigue. Health Psychol. 2012, 31, 210–216. [Google Scholar] [CrossRef] [PubMed]
- Veen, G.; Giltay, E.J.; DeRijk, R.H.; van Vliet, I.M.; van Pelt, J.; Zitman, F.G. Salivary Cortisol, Serum Lipids, and Adiposity in Patients with Depressive and Anxiety Disorders. Metabolism 2009, 58, 821–827. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.L.; Wu, S.C.; Chiang, Y.S.; Chen, J.F. Correlation between Serum Lipid, Lipoprotein Concentrations and Anxious State, Depressive State or Major Depressive Disorder. Psychiatry Res. 2003, 118, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Skrede, S.; Steen, V.M.; Fernø, J. Antipsychotic-Induced Increase in Lipid Biosynthesis: Activation through Inhibition? J. Lipid Res. 2013, 54, 307–309. [Google Scholar] [CrossRef] [PubMed]
- Kaddurah-Daouk, R.; McEvoy, J.; Baillie, R.A.; Lee, D.; Yao, J.K.; Doraiswamy, P.M.; Krishnan, K.R.R. Metabolomic Mapping of Atypical Antipsychotic Effects in Schizophrenia. Mol. Psychiatry 2007, 12, 934–945. [Google Scholar] [CrossRef]
- Pillinger, T.; McCutcheon, R.A.; Vano, L.; Mizuno, Y.; Arumuham, A.; Hindley, G.; Beck, K.; Natesan, S.; Efthimiou, O.; Cipriani, A.; et al. Comparative Effects of 18 Antipsychotics on Metabolic Function in Patients with Schizophrenia, Predictors of Metabolic Dysregulation, and Association with Psychopathology: A Systematic Review and Network Meta-Analysis. Lancet Psychiatry 2020, 7, 64–77. [Google Scholar] [CrossRef]
- Huang, J.; Xiao, J.; Peng, Z.; Shao, P.; Sun, M.; Long, Y.; Wang, X.; Shen, M.; Kang, D.; Yang, Y.; et al. PCSK9 Mediates Dyslipidemia Induced by Olanzapine Treatment in Schizophrenia Patients. Psychopharmacology 2022, 239, 83–91. [Google Scholar] [CrossRef]
- Chaggar, P.S.; Shaw, S.M.; Williams, S.G. Effect of Antipsychotic Medications on Glucose and Lipid Levels. J. Clin. Pharmacol. 2011, 51, 631–638. [Google Scholar] [CrossRef]
- Canfrań-Duque, A.; Casado, M.E.; Pastor, Ó.; Sánchez-Wandelmer, J.; De La Penã, G.; Lerma, M.; Mariscal, P.; Bracher, F.; Lasunción, M.A.; Busto, R. Atypical Antipsychotics Alter Cholesterol and Fatty Acid Metabolism in Vitro. J. Lipid Res. 2013, 54, 310–324. [Google Scholar] [CrossRef]
- Sánchez-Wandelmer, J.; Dávalos, A.; de la Peña, G.; Cano, S.; Giera, M.; Canfrán-Duque, A.; Bracher, F.; Martín-Hidalgo, A.; Fernández-Hernando, C.; Lasunción, M.A.; et al. Haloperidol Disrupts Lipid Rafts and Impairs Insulin Signaling in SH-SY5Y Cells. Neuroscience 2010, 167, 143–153. [Google Scholar] [CrossRef] [PubMed]
- Canfrán-Duque, A.; Pastor, Ó.; García-Seisdedos, D.; Molina, Y.L.; Babiy, B.; Lerma, M.; Sánchez-Castellano, C.; Martínez-Botas, J.; Gómez-Coronado, D.; Lasunción, M.A.; et al. The Antipsychotic Risperidone Alters Dihydroceramide and Ceramide Composition and Plasma Membrane Function in Leukocytes In Vitro and In Vivo. Int. J. Mol. Sci. 2021, 22, 3919. [Google Scholar] [CrossRef] [PubMed]
- Cai, H.L.; Tan, Q.Y.; Jiang, P.; Dang, R.L.; Xue, Y.; Tang, M.M.; Xu, P.; Deng, Y.; Li, H.D.; Yao, J.K. A Potential Mechanism Underlying Atypical Antipsychotics-Induced Lipid Disturbances. Transl. Psychiatry 2015, 5, e661. [Google Scholar] [CrossRef] [PubMed]
- Alves, I.; Staneva, G.; Tessier, C.; Salgado, G.F.; Nuss, P. The Interaction of Antipsychotic Drugs with Lipids and Subsequent Lipid Reorganization Investigated Using Biophysical Methods. Biochim. Biophys. Acta 2011, 1808, 2009–2018. [Google Scholar] [CrossRef]
- Smesny, S.; Langbein, K.; Rzanny, R.; Gussew, A.; Burmeister, H.P.; Reichenbach, J.R.; Sauer, H. Antipsychotic Drug Effects on Left Prefrontal Phospholipid Metabolism: A Follow-up 31P-2D-CSI Study of Haloperidol and Risperidone in Acutely Ill Chronic Schizophrenia Patients. Schizophr. Res. 2012, 138, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Dietrich-Muszalska, A.; Kolińska-Łukaszuk, J. Comparative Effects of Aripiprazole and Selected Antipsychotic Drugs on Lipid Peroxidation in Plasma. Psychiatry Clin. Neurosci. 2018, 72, 329–336. [Google Scholar] [CrossRef] [PubMed]
- de Almeida, V.; Alexandrino, G.L.; Aquino, A.; Gomes, A.F.; Murgu, M.; Dobrowolny, H.; Guest, P.C.; Steiner, J.; Martins-de-Souza, D. Changes in the Blood Plasma Lipidome Associated with Effective or Poor Response to Atypical Antipsychotic Treatments in Schizophrenia Patients. Prog. Neuropsychopharmacol. Biol. Psychiatry 2020, 101, 109945. [Google Scholar] [CrossRef]
- Gabriel, A. Changes in Plasma Cholesterol in Mood Disorder Patients: Does Treatment Make a Difference? J. Affect. Disord. 2007, 99, 273–278. [Google Scholar] [CrossRef]
- Pan, S.J.; Tan, Y.L.; Yao, S.W.; Xin, Y.; Yang, X.; Liu, J.; Xiong, J. Fluoxetine Induces Lipid Metabolism Abnormalities by Acting on the Liver in Patients and Mice with Depression. Acta Pharmacol. Sin. 2018, 39, 1463–1472. [Google Scholar] [CrossRef]
- McIntyre, R.S.; Soczynka, J.K.; Konarski, J.Z.; Kennedy, S.H. The Effect of Antidepressants on Lipid Homeostasis: A Cardiac Safety Concern? Expert Opin. Drug Saf. 2006, 5, 523–537. [Google Scholar] [CrossRef]
- Nicholas, L.M.; Ford, A.L.; Esposito, S.M.; Ekstrom, R.D.; Golden, R.N. The Effects of Mirtazapine on Plasma Lipid Profiles in Healthy Subjects. J. Clin. Psychiatry 2003, 64, 883–889. [Google Scholar] [CrossRef] [PubMed]
- Kopf, D.; Westphal, S.; Luley, C.W.; Ritter, S.; Gilles, M.; Weber-Hamann, B.; Lederbogen, F.; Lehnert, H.; Henn, F.A.; Heuser, I.; et al. Lipid Metabolism and Insulin Resistance in Depressed Patients: Significance of Weight, Hypercortisolism, and Antidepressant Treatment. J. Clin. Psychopharmacol. 2004, 24, 527–531. [Google Scholar] [CrossRef]
- Yosmaoǧlu, A.; Fistikci, N.; Keyvan, A.; Hacioǧlu, M.; Erten, E.; Saatçioǧlu, Ö.; Kora, K. Correlation of Selective Serotonin Re-Uptake Inhibitor Use with Weight Gain and Metabolic Parameters. Anatol. J. Psychiatry 2013, 14, 245–251. [Google Scholar] [CrossRef]
- Beyazyüz, M.; Albayrak, Y.; Eğilmez, O.B.; Albayrak, N.; Beyazyüz, E. Relationship between SSRIs and Metabolic Syndrome Abnormalities in Patients with Generalized Anxiety Disorder: A Prospective Study. Psychiatry Investig. 2013, 10, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Olguner Eker, Ö.; Özsoy, S.; Eker, B.; Doğan, H. Metabolic Effects of Antidepressant Treatment. Noro Psikiyatr. Ars. 2017, 54, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Deisenhammer, E.A.; Kramer-Reinstadler, K.; Liensberger, D.; Kemmler, G.; Hinterhuber, H.; Fleischhacker, W.W. No Evidence for an Association between Serum Cholesterol and the Course of Depression and Suicidality. Psychiatry Res. 2004, 121, 253–261. [Google Scholar] [CrossRef]
- Xiong, J.; Yang, H.; Wu, L.; Shang, W.; Shan, E.; Liu, W.; Hu, G.; Xi, T.; Yang, J. Fluoxetine Suppresses AMP-Activated Protein Kinase Signaling Pathway to Promote Hepatic Lipid Accumulation in Primary Mouse Hepatocytes. Int. J. Biochem. Cell Biol. 2014, 54, 236–244. [Google Scholar] [CrossRef]
- Hsiao, C.C. Difference in Pre- and Post-Treatment Plasma DHEA Levels Were Significantly and Positively Correlated with Difference in Pre- and Post-Treatment Hamilton Depression Scores Following Successful Therapy for Major Depression. Psychoneuroendocrinology 2006, 31, 839–846. [Google Scholar] [CrossRef]
- Mocking, R.J.T.; Nap, T.S.; Westerink, A.M.; Assies, J.; Vaz, F.M.; Koeter, M.W.J.; Ruhé, H.G.; Schene, A.H. Biological Profiling of Prospective Antidepressant Response in Major Depressive Disorder: Associations with (Neuro)Inflammation, Fatty Acid Metabolism, and Amygdala-Reactivity. Psychoneuroendocrinology 2017, 79, 84–92. [Google Scholar] [CrossRef]
- Hummel, J.; Westphal, S.; Weber-Hamann, B.; Gilles, M.; Lederbogen, F.; Angermeier, T.; Luley, C.; Deuschle, M.; Kopf, D. Serum Lipoproteins Improve after Successful Pharmacologic Antidepressant Treatment: A Randomized Open-Label Prospective Trial. J. Clin. Psychiatry 2011, 72, 885–891. [Google Scholar] [CrossRef]
- Sonawalla, S.B.; Papakostas, G.I.; Petersen, T.J.; Yeung, A.S.; Smith, M.M.; Sickinger, A.H.; Gordon, J.; Israel, J.A.; Tedlow, J.R.; Lamon-Fava, S.; et al. Elevated Cholesterol Levels Associated with Nonresponse to Fluoxetine Treatment in Major Depressive Disorder. Psychosomatics 2002, 43, 310–316. [Google Scholar] [CrossRef]
- Noordam, R.; Aarts, N.; De Keyser, C.E.; Hofman, A.; Stricker, B.H.; Visser, L.E. Antidepressants with a High Serotonin Reuptake Transporter Affinity and Serum Lipid Levels in a Population-Based Study in Older Adults. J. Psychopharmacol. 2015, 29, 1112–1118. [Google Scholar] [CrossRef]
- Homorogan, C.; Nitusca, D.; Enatescu, V.; Schubart, P.; Moraru, C.; Socaciu, C.; Marian, C. Untargeted Plasma Metabolomic Profiling in Patients with Major Depressive Disorder Using Ultra-High Performance Liquid Chromatography Coupled with Mass Spectrometry. Metabolites 2021, 11, 466. [Google Scholar] [CrossRef]
- Pinto, B.; Conde, T.; Domingues, I.; Domingues, M.R. Adaptation of Lipid Profiling in Depression Disease and Treatment: A Critical Review. Int. J. Mol. Sci. 2022, 23, 2032. [Google Scholar] [CrossRef]
- MahmoudianDehkordi, S.; Ahmed, A.T.; Bhattacharyya, S.; Han, X.; Baillie, R.A.; Arnold, M.; Skime, M.K.; John-Williams, L.S.; Moseley, M.A.; Thompson, J.W.; et al. Alterations in Acylcarnitines, Amines, and Lipids Inform about the Mechanism of Action of Citalopram/Escitalopram in Major Depression. Transl. Psychiatry 2021, 11, 153. [Google Scholar] [CrossRef]


| FATTY ACYLS | ||||
| Type of Lipid | Disorder | |||
| SCZ | MDD | BPD | AD | |
| PUFAs | ↑ 8 types [45], ↑ monounsaturated fatty acids and ω-6 PUFAs [80], and ↓ 5 types [40] ↓ 6 types [81] | ↓ including eicosapentaenoic acid and arachidonic acid [82], ↑ in plasma, mostly ↓ membrane fatty acids, exp octadectetraenoic, gamma-linolenic acid, and docosadienoic acid [83]. ↑ AA: eicosapentaenoic acid (EPA) ratio [84]. | ↑ omega-6 PUFA, AA: EPA and AA: EPA+ docosahexaenoic acid (DHA) [84]. ↑ linoleic acid, AA, α-linolenic acid, EPA [85], ↑ ratio of omega-6/omega-3 [86] ↓ DHA 22:6n-3 decreased in membrane [87], and ↓ DHA (22:6n-3) and AA (20:4n-6) [88] ↓ EPA acid [89]. ↓ DHA [85]. | ↑ n-6:n-3 ratio [90] ↓ N-3 PUFA and ↓ N3:FA ratio in patients with comorbid depressive and anxiety disorder [72]. ↓ DHA in pregnant women [73]. ↓ 3 types of PUFAs in patients with comorbid Parkinson’s disease and AD [65]. |
| SFA | ↑ [91], ↑ 4 types [45], ↑ linoleic acid [47], ↓ stearic acid, behenic acid, α-dimorphecolic [50], ↓ lithocholic acid [40], and ↓ 16:0 [92]. Higher levels of total SCFAs, acetic acid, acetic acid/ propionic acid ratio SCZ compared to CTL. The lipid levels were positively associated with acetic acid/propionic acid ratio | ↑ azelaic acid, ↓ palmitic acid, dodecanoic acid, and capric acid [82]. ↑ plasma, mostly ↓ membrane exp. palmitic acid [83]. | No information. | ↓ hexacosanoic acid and 10-oxo-nonadecanoic acid in patients with comorbid Parkinson’s disease and AD [65]. ↑ 3-Hydroxysebacic acid and ↓ 2-Hydroxy-3-methylpentanoic acid [66]. ↑ erythrocyte membrane linoleic acid in patients with anxiety symptoms comorbid to MDD [93]. |
| Carnitine | ↑ long chain in FEP [94], ↑ CAR 10:2 [44], ↑ 3 types of carnitine [95], ↓ [34], ↓ 3 types of carnitine [40], ↓ medium and high chain [95], ↓ short-chain CAR in FEP [94], and ↓ 18:2 in FEP [42]. | ↓ 5 types [59]. ↓ AcCAR [61]. | ↓ [61]. | ↓ propionylcarnitine [66]. |
| Transdiagnostic between SCZ, MDD, BPD, and AD: ↓ 10-nitro-9Z,12Z-octadecadienoic acid decreased; ↑ 9,12-octadecadienal, cyclopentaneoctanoic acid, hexadecandioic acid, 12-tridecynoic acid, and caprylic acid [79]. | ||||
| SACCHAROLIPIDS | ||||
| Type of lipid | Disorder | |||
| SCZ | MDD | BPD | AD | |
| MGDG | No information. | ↓ [61]. | ↓ [61]. | No information. |
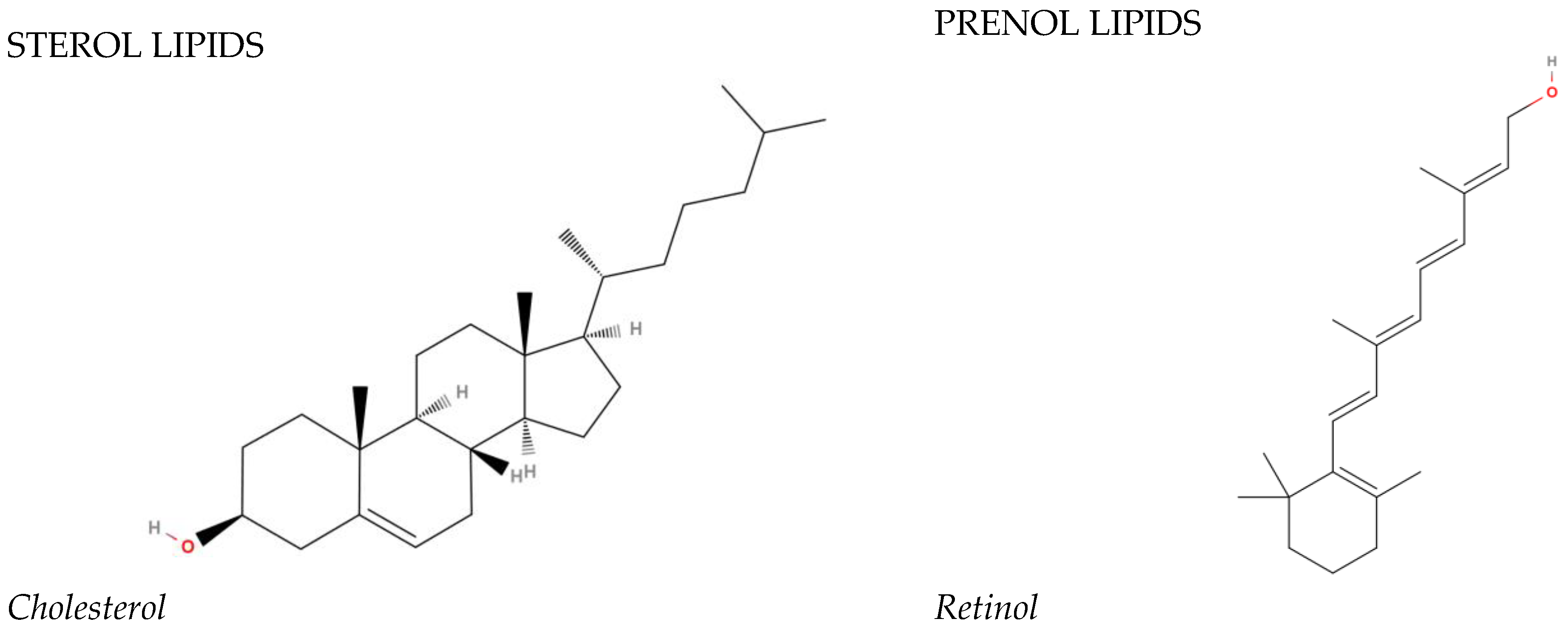
| STEROL LIPIDS | ||||
| Type of lipid | Disorder | |||
| SCZ | MDD | BPD | AD | |
| Cholesteryl esters | ↑ in FEP [42]. ↓ CE 16:1 [44]. | Plasma tryptophan-kynurenine metabolites and CEs were significantly correlated in the MDD group, but not in the HC group [62]. No difference [96]. ↓ CE [60]. | ↓ [86] | No information. |
| Total cholesterol | ↓ [52]. | ↑ in women with depressive symptoms [97]. ↓ in postpartum depression [57]. | ↑ [98]. ↓ [51,99]. | ↑ [100]; ↑ in comorbid MDD and GAD [68]. ↓ in alexythimic patents [67], ↓ in patients with comorbid Parkinson’s disease and AD [65], ↓ in the anxious–depressive disorder group [71], and not changed compared to MDD and BPD [101]. |
| Sterols | ↑ the ratios of cholestane-3β,5α,6β-triol, 27-hydroxycholesterol, and cholestanol to tchol [55]. ↓ several types of sterol lipids [44]. | ↑ 7-dihydrocholesterol, ↓ desmosterol, and 14-desmethyl lanosterol in people with depressive symptoms [102]. | No information | ↓ 11-acetoxy-3β,6α-dihydroxy-9,11-seco-5α-cholest-7-en-9-one in patients with comorbid Parkinson’s disease and AD [67]. |
| Bile acids | ↓ [50]. ↓ lithocholic acid [40]. | ↑ 23-nordeoxycholic acid, ↓ taurolithocholic acid (TLCA), glycolithocholic acid (GLCA), and lithocholic acid (LCA) 3-sulfate ↓ [103]. ↓ chenodeoxycholic acid (CDCA) [74]. | No information. | ↓ CDCA in highly anxious participants compared to participants with less severe symptoms [74]. ↑ LCA [74]. |
| Calcifediol | ↓ [50]. | ↓ [104]; not changed depressive symptoms in healthy people [78]. | ↓ [105]. | Not changed [78]. |
| ↓ 20-oxo-22,23,24,25,26,27-hexanorvitamin D3 [79] transdiagnostic | ↓ [79] transdiagnostic. ↓ anxiety symptoms [76,77]. | |||
| GLYCEROPHOSPHOLIPIDS | ||||
| Type of lipid | Disorder | |||
| SCZ | MDD | BPD | AD | |
| PC | ↑ 32 types of PC [40], ↓ PC [50], ↓ 46:7 [44], ↓ PC (O-34:2) [40], mostly ↓ membrane PC [31], ↓ PC [45,54,106], PC-O in FEP [107], ↓ PC-P in FEP [42], ↓ PC-O [45,46], ↓ PC-O 38:6 [108], ↓ PUFA-containing PC [53], and ↓ 14 types and ↑ 11 types [34]. | ↑ [58], ↑ PC 32:1 [59], ↑ PC-O [63] ↑ PC(8:0e/6:0) [34] ↓ 3 types ↑ 5 types [82] ↑ [109] and ↓ PC-O 36:2 [59] | ↑ PC [110]. | ↓ PC O 36:4 (anxiety symptoms) [63] and ↓ LysoPC(0:0/16:0) [66]. |
| ↑ PC-O 16:0-18:1+2O [79] transdiagnostic | ||||
| PE | ↑ PE 34:2 [40], ↓ [50], ↓ 40:7 [44], ↓ PE (O-34:3), (O-36:6) [40], mostly ↓ membrane PE [31], ↓ PE-P [54,106], ↓ PE-P in FEP [42], ↓ PE-O [46], ↓ PUFA-containing PE [53], and ↓ 2 ↑ 5 [45]. | ↑ [58], ↑ PE 34:2 36:4 [59], ↓ PE-O [58], ↓ PE-O [59], ↓ PE (16:0/22:6) PE(18:0/22:6) [111], ↑ PE(18:1/0:0), and PE(18:2/0:0) [82]. | ↓ [61]. | No information. |
| LPC | ↑ LPC [40], ↑ LPC 18:1 [44], ↓ [34,43,46] ↓ in FEP [42], mostly ↓ membrane LPC [31] ↑ 4 ↓ 19 [45] | ↑ [58,59] ↑ LysoPC (16:0) and LysoPC (18:0) [111], and ↑ LPC [106], | ↑ LPC [106]. | No information. |
| Lysophosphatidylethanolamine (LPE) | ↑ [34,40] mostly ↓ membrane LPE [31] 3 ↓ 9 ↑ [45] | ↑ [58,59] | ↑ [61] | ↑ lysoPE(18:2(9Z,12Z)/0:0) [66]. |
| PS | ↑ LPS 21:0 [44], ↓ 43:2 [44], ↓ 10, ↑ 13 membrane PS [31], | ↓ [61] | ↓ [61] | No information. |
| ↑ DGTS 16:0/18:1 [79] transdiagnostic | ||||
| SPHINGOLIPIDS | ||||
| Type of lipid | Disorder | |||
| SCZ | MDD | BPD | AD | |
| Sphingomyelin | ↑ SM with PUFA (C18:1 and C24:1), ↓ 12 types [44] mostly ↓ SMs with SFA (C16:0, C20:0, and C24:0) [45], and mostly ↓ membrane SM [31] | ↑ [63], ↓ PhSM [61], and ↓SM 39:1 [58]. | ↓ SM and phSM [61]. | ↓ SPM 23:1 (anxiety symptoms) [63]. |
| Ceramide | ↑ Cer (d18: 1/16: 0), Cer (d18: 1/18: 0) и Cer (d18: 1/24: 1) [112], ↓ 44:1 [44] ↓ 22, ↑ 20 membrane Cer [31] | ↑ Cer elevated [113], ↑ Cer and HexCer [114] ↓ CerG2GNAc1(d38:4) [34], ↓ CerG2GNAc1 [61] | ↑ Cer and HexCer elevated [114] and ↑ Cer22:0 [115] | ↑ Cer 20:0 in Parkinson’s disease patients with anxiety symptoms [75]. |
| Ganglioside | No information | ↑ monosialotetrahexosylganglioside 2 (GM2) [61] | ↑ GM2 [61]. | No information. |
| Other | ↓ C16 sphinganine [50]; ↓ glycosphingolipids [44]. | ↑ total sphingolipids [68]. | ↓ N-(hexadecanoyl)-deoxysphing-4-enine-1-sulfonate in patients with comorbid Parkinson’s disease and AD [65]. | |
| GLYCEROLIPIDS | ||||
| Type of lipid | Disorders | |||
| SCZ | MDD | BPD | AD | |
| TG | ↑ 20 types [41], ↑ [43,52,116] ↑ in FEP [42], ↑ membrane TG [31], and ↓ 3 types [44]. | ↑ [58,59] and ↓ TG [60]. ↑ [34]. | ↑ [51,61,114]. ↓ TG [99]. | ↑ in alexythimic patents [67], ↑ comorbid MDD with anxiety [68,69,71], ↑ anxiety symptoms [70], and ↓ in patients with comorbid Parkinson’s disease and AD [65]. |
| DG | ↑ membrane [31]. | Not changed [60]. | ↑ [114]. | ↓ 6 types in patients with comorbid Parkinson’s disease and AD [65] |
| PRODUCTS OF LIPID METABOLISM | ||||
| Type of lipid | Disorder | |||
| SCZ | MDD | BPD | AD | |
| Coenzyme Q10 | No information. | ↓ [117]. | ↓ [61]. | No information. |
| Malondialdehyde | ↑ [49,118,119,120] | ↑ [121,122]. | ↑ [123]. | ↑ [124]; ↑ post-stroke anxiety [64]. |
| Lipoproteins | ↓ HDL [52]; ↓ HDL, LDL, and ApoE [51]. | ↑ LDL [34], ↓ HDL [125], ↓ HDL-c postpartum [57], and ↓ HDL-C [62]. | HDL ↓, LDL, and apolipoprotein E (ApoE) ↓ [51]. | ↑ LDL [67,68], ↓ LDL in patients with comorbid Parkinson’s disease and AD [65], ↓ LDL (tension-anxiety symptoms) [126], ↓ HDL [67,68,69,127,128], ↑ HDL (tension–anxiety symptoms) [126], ↑ VLDL [67], ↑ LDL/HDL [67], ↑ TC/HDL [67,128], ↑ ApoB [71], ↓ ApoB in patients with comorbid Parkinson’s disease and AD [65], and ↑ ApoA [71]. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zorkina, Y.; Ushakova, V.; Ochneva, A.; Tsurina, A.; Abramova, O.; Savenkova, V.; Goncharova, A.; Alekseenko, I.; Morozova, I.; Riabinina, D.; et al. Lipids in Psychiatric Disorders: Functional and Potential Diagnostic Role as Blood Biomarkers. Metabolites 2024, 14, 80. https://doi.org/10.3390/metabo14020080
Zorkina Y, Ushakova V, Ochneva A, Tsurina A, Abramova O, Savenkova V, Goncharova A, Alekseenko I, Morozova I, Riabinina D, et al. Lipids in Psychiatric Disorders: Functional and Potential Diagnostic Role as Blood Biomarkers. Metabolites. 2024; 14(2):80. https://doi.org/10.3390/metabo14020080
Chicago/Turabian StyleZorkina, Yana, Valeria Ushakova, Aleksandra Ochneva, Anna Tsurina, Olga Abramova, Valeria Savenkova, Anna Goncharova, Irina Alekseenko, Irina Morozova, Daria Riabinina, and et al. 2024. "Lipids in Psychiatric Disorders: Functional and Potential Diagnostic Role as Blood Biomarkers" Metabolites 14, no. 2: 80. https://doi.org/10.3390/metabo14020080
APA StyleZorkina, Y., Ushakova, V., Ochneva, A., Tsurina, A., Abramova, O., Savenkova, V., Goncharova, A., Alekseenko, I., Morozova, I., Riabinina, D., Kostyuk, G., & Morozova, A. (2024). Lipids in Psychiatric Disorders: Functional and Potential Diagnostic Role as Blood Biomarkers. Metabolites, 14(2), 80. https://doi.org/10.3390/metabo14020080






