Impact of the Level of Adherence to the DASH Diet on Blood Pressure: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Methods
2.1. Protocol
2.2. Search Strategy
2.3. Eligibility Criteria
2.4. Outcomes
2.5. Data Extraction
2.6. Quality Appraisal
2.7. Statistical Analysis
2.8. Quality of the Evidence
3. Results
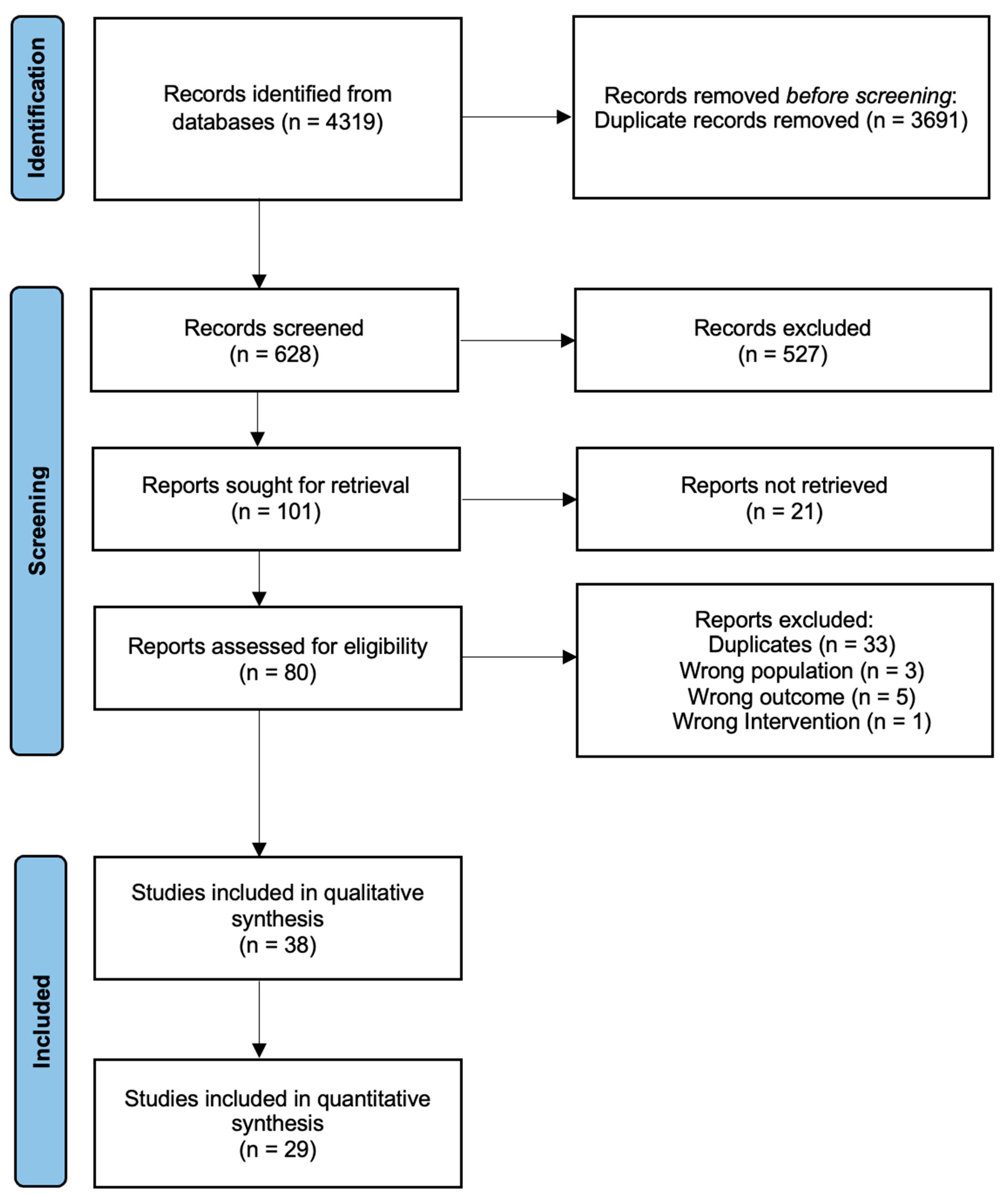
3.1. Study Selection
3.2. Study and Patient Characteristics
3.3. SBP and DBP Levels
3.4. Subgroup Analysis
3.5. Sensitivity Analysis
3.6. Risk of Bias Assessment
3.7. Publication Bias
3.8. Certainty of Findings
4. Discussion
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Collaborators, G.R.F. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar] [CrossRef]
- Mills, K.T.; Stefanescu, A.; He, J. The global epidemiology of hypertension. Nat. Rev. Nephrol. 2020, 16, 223–237. [Google Scholar] [CrossRef] [PubMed]
- Law, M.R.; Morris, J.K.; Wald, N.J. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: Meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ (Clin. Res. Ed.) 2009, 338, b1665. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef]
- Appel, L.J.; Moore, T.J.; Obarzanek, E.; Vollmer, W.M.; Svetkey, L.P.; Sacks, F.M.; Bray, G.A.; Vogt, T.M.; Cutler, J.A.; Windhauser, M.M.; et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N. Engl. J. Med. 1997, 336, 1117–1124. [Google Scholar] [CrossRef]
- Blumenthal, J.A.; Babyak, M.A.; Hinderliter, A.; Watkins, L.L.; Craighead, L.; Lin, P.H.; Caccia, C.; Johnson, J.; Waugh, R.; Sherwood, A. Effects of the DASH diet alone and in combination with exercise and weight loss on blood pressure and cardiovascular biomarkers in men and women with high blood pressure: The ENCORE study. Arch. Intern. Med. 2010, 170, 126–135. [Google Scholar] [CrossRef]
- De Geest, S.; Sabaté, E. Adherence to long-term therapies: Evidence for action. Eur. J. Cardiovasc. Nurs. 2003, 2, 323. [Google Scholar] [CrossRef]
- Sacks, F.M.; Svetkey, L.P.; Vollmer, W.M.; Appel, L.J.; Bray, G.A.; Harsha, D.; Obarzanek, E.; Conlin, P.R.; Miller, E.R., 3rd; Simons-Morton, D.G.; et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N. Engl. J. Med. 2001, 344, 3–10. [Google Scholar] [CrossRef]
- Feng, Q.; Fan, S.; Wu, Y.; Zhou, D.; Zhao, R.; Liu, M.; Song, Y. Adherence to the dietary approaches to stop hypertension diet and risk of stroke: A meta-analysis of prospective studies. Medicine 2018, 97, e12450. [Google Scholar] [CrossRef]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef]
- Brooke, B.S.; Schwartz, T.A.; Pawlik, T.M. MOOSE Reporting Guidelines for Meta-analyses of Observational Studies. JAMA Surg. 2021, 156, 787–788. [Google Scholar] [CrossRef]
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 2014, 14, 135. [Google Scholar] [CrossRef]
- Higgins, J.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions Version 6.3; Cochrane: London, UK, 2022. [Google Scholar]
- Banerjee, T.; Crews, D.C.; Tuot, D.S.; Pavkov, M.E.; Burrows, N.R.; Stack, A.G.; Saran, R.; Bragg-Gresham, J.; Powe, N.R. Poor accordance to a DASH dietary pattern is associated with higher risk of ESRD among adults with moderate chronic kidney disease and hypertension. Kidney Int. 2019, 95, 1433–1442. [Google Scholar] [CrossRef]
- Bendinelli, B.; Masala, G.; Bruno, R.M.; Caini, S.; Saieva, C.; Boninsegni, A.; Ungar, A.; Ghiadoni, L.; Palli, D. A priori dietary patterns and blood pressure in the EPIC Florence cohort: A cross-sectional study. Eur. J. Nutr. 2019, 58, 455–466. [Google Scholar] [CrossRef]
- Bonaccio, M.; Di Castelnuovo, A.; Costanzo, S.; De Curtis, A.; Persichillo, M.; Cerletti, C.; Donati, M.B.; de Gaetano, G.; Iacoviello, L. Association of a traditional Mediterranean diet and non-Mediterranean dietary scores with all-cause and cause-specific mortality: Prospective findings from the Moli-sani Study. Eur. J. Nutr. 2021, 60, 729–746. [Google Scholar] [CrossRef] [PubMed]
- Chan, Q.; Wren, G.M.; Lau, C.E.; Ebbels, T.M.D.; Gibson, R.; Loo, R.L.; Aljuraiban, G.S.; Posma, J.M.; Dyer, A.R.; Steffen, L.M.; et al. Blood pressure interactions with the DASH dietary pattern, sodium, and potassium: The International Study of Macro-/Micronutrients and Blood Pressure (INTERMAP). Am. J. Clin. Nutr. 2022, 116, 216–229. [Google Scholar] [CrossRef]
- Critselis, E.; Kontogianni, M.D.; Georgousopoulou, E.; Chrysohoou, C.; Tousoulis, D.; Pitsavos, C.; Panagiotakos, D.B. Comparison of the Mediterranean diet and the Dietary Approach Stop Hypertension in reducing the risk of 10-year fatal and non-fatal CVD events in healthy adults: The ATTICA Study (2002–2012). Public Health Nutr. 2021, 24, 2746–2757. [Google Scholar] [CrossRef]
- Dai, S.; Xiao, X.; Xu, C.; Jiao, Y.; Qin, Z.; Meng, J.; Zuo, H.; Zeng, P.; Tang, D.; Wu, X.; et al. Association of Dietary Approaches to Stop Hypertension diet and Mediterranean diet with blood pressure in less-developed ethnic minority regions. Public Health Nutr. 2022, 25, 1–29. [Google Scholar] [CrossRef]
- Daniel, G.D.; Chen, H.; Bertoni, A.G.; Rapp, S.R.; Fitzpatrick, A.L.; Luchsinger, J.A.; Wood, A.C.; Hughes, T.M.; Burke, G.L.; Hayden, K.M. DASH diet adherence and cognitive function: Multi-ethnic study of atherosclerosis. Clin. Nutr. ESPEN 2021, 46, 223–231. [Google Scholar] [CrossRef] [PubMed]
- Epstein, D.E.; Sherwood, A.; Smith, P.J.; Craighead, L.; Caccia, C.; Lin, P.H.; Babyak, M.A.; Johnson, J.J.; Hinderliter, A.; Blumenthal, J.A. Determinants and consequences of adherence to the dietary approaches to stop hypertension diet in African-American and white adults with high blood pressure: Results from the ENCORE trial. J. Acad. Nutr. Diet. 2012, 112, 1763–1773. [Google Scholar] [CrossRef] [PubMed]
- Francisco, S.C.; Araújo, L.F.; Griep, R.H.; Chor, D.; Molina, M.; Mil, J.G.; Bensenor, I.M.; Matos, S.M.A.; Barreto, S.M.; Giatti, L. Adherence to the Dietary Approaches to Stop Hypertension (DASH) and hypertension risk: Results of the Longitudinal Study of Adult Health (ELSA-Brasil). Br. J. Nutr. 2020, 123, 1068–1077. [Google Scholar] [CrossRef]
- Gao, X.; Tian, Z.; Zhao, D.; Li, K.; Zhao, Y.; Xu, L.; Wang, X.; Fan, D.; Ma, X.; Ling, W.; et al. Associations between Adherence to Four A Priori Dietary Indexes and Cardiometabolic Risk Factors among Hyperlipidemic Patients. Nutrients 2021, 13, 2179. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Cui, L.F.; Sun, Y.Y.; Yang, W.H.; Wang, J.R.; Wu, S.L.; Gao, X. Adherence to the Dietary Approaches to Stop Hypertension Diet and Hyperuricemia: A Cross-Sectional Study. Arthritis Care Res. 2020, 73, 603–611. [Google Scholar] [CrossRef] [PubMed]
- Ghorabi, S.; Salari-Moghaddam, A.; Daneshzad, E.; Sadeghi, O.; Azadbakht, L.; Djafarian, K. Association between the DASH diet and metabolic syndrome components in Iranian adults. Diabetes Metab. Syndr. 2019, 13, 1699–1704. [Google Scholar] [CrossRef] [PubMed]
- Glenn, A.J.; Hernández-Alonso, P.; Kendall, C.W.C.; Martínez-González, M.Á.; Corella, D.; Fitó, M.; Martínez, J.A.; Alonso-Gómez, Á.M.; Wärnberg, J.; Vioque, J.; et al. Longitudinal changes in adherence to the portfolio and DASH dietary patterns and cardiometabolic risk factors in the PREDIMED-Plus study. Clin. Nutr. 2021, 40, 2825–2836. [Google Scholar] [CrossRef]
- Goyal, P.; Balkan, L.; Ringel, J.B.; Hummel, S.L.; Sterling, M.R.; Kim, S.; Arora, P.; Jackson, E.A.; Brown, T.M.; Shikany, J.M.; et al. The Dietary Approaches to Stop Hypertension (DASH) Diet Pattern and Incident Heart Failure. J. Card. Fail. 2021, 27, 512–521. [Google Scholar] [CrossRef]
- Harrington, J.M.; Fitzgerald, A.P.; Kearney, P.M.; McCarthy, V.J.; Madden, J.; Browne, G.; Dolan, E.; Perry, I.J. DASH diet score and distribution of blood pressure in middle-aged men and women. Am. J. Hypertens. 2013, 26, 1311–1320. [Google Scholar] [CrossRef]
- Hu, E.A.; Coresh, J.; Anderson, C.A.M.; Appel, L.J.; Grams, M.E.; Crews, D.C.; Mills, K.T.; He, J.; Scialla, J.; Rahman, M.; et al. Adherence to Healthy Dietary Patterns and Risk of CKD Progression and All-Cause Mortality: Findings From the CRIC (Chronic Renal Insufficiency Cohort) Study. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 2021, 77, 235–244. [Google Scholar] [CrossRef]
- Ishikawa, Y.; Laing, E.M.; Anderson, A.K.; Zhang, D.; Kindler, J.M.; Trivedi-Kapoor, R.; Sattler, E.L.P. Adherence to the Dietary Approaches to Stop Hypertension (DASH) diet is associated with low levels of insulin resistance among heart failure patients. Nutr. Metab. Cardiovasc. Dis. NMCD 2022, 32, 1841–1850. [Google Scholar] [CrossRef]
- Jalilpiran, Y.; Darooghegi Mofrad, M.; Mozaffari, H.; Bellissimo, N.; Azadbakht, L. Adherence to dietary approaches to stop hypertension (DASH) and Mediterranean dietary patterns in relation to cardiovascular risk factors in older adults. Clin. Nutr. ESPEN 2020, 39, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Jayedi, A.; Mirzaei, K.; Rashidy-Pour, A.; Yekaninejad, M.S.; Zargar, M.S.; Akbari Eidgahi, M.R. Dietary approaches to stop hypertension, mediterranean dietary pattern, and diabetic nephropathy in women with type 2 diabetes: A case-control study. Clin. Nutr. ESPEN 2019, 33, 164–170. [Google Scholar] [CrossRef]
- Jones, N.R.V.; Forouhi, N.G.; Khaw, K.T.; Wareham, N.J.; Monsivais, P. Accordance to the Dietary Approaches to Stop Hypertension diet pattern and cardiovascular disease in a British, population-based cohort. Eur. J. Epidemiol. 2018, 33, 235–244. [Google Scholar] [CrossRef]
- Kang, S.H.; Cho, K.H.; Do, J.Y. Association between the Modified Dietary Approaches to Stop Hypertension and Metabolic Syndrome in Postmenopausal Women without Diabetes. Metab. Syndr. Relat. Disord. 2018, 16, 282–289. [Google Scholar] [CrossRef]
- Khodarahmi, M.; Nikniaz, L.; Abbasalizad Farhangi, M. The Interaction between Fatty Acid Desaturase-2 (FADS2) rs174583 Genetic Variant and Dietary Quality Indices (DASH and MDS) Constructs Different Metabolic Phenotypes Among Obese Individuals. Front. Nutr. 2021, 8, 669207. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Huan, T.; Joehanes, R.; McKeown, N.M.; Horvath, S.; Levy, D.; Ma, J. Higher diet quality relates to decelerated epigenetic aging. Am. J. Clin. Nutr. 2022, 115, 163–170. [Google Scholar] [CrossRef]
- Köroğlu, Ö.; Tel Adıgüzel, K. Cardiometabolic risk parameters of individuals with lower extremity amputation: What is the effect of adherence to DASH diet and Mediterranean diet? Turk. J. Phys. Med. Rehabil. 2020, 66, 291–298. [Google Scholar] [CrossRef]
- Lin, J.; Fung, T.T.; Hu, F.B.; Curhan, G.C. Association of dietary patterns with albuminuria and kidney function decline in older white women: A subgroup analysis from the Nurses’ Health Study. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 2011, 57, 245–254. [Google Scholar] [CrossRef]
- Liu, Y.; Kuczmarski, M.F.; Miller, E.R., 3rd; Nava, M.B.; Zonderman, A.B.; Evans, M.K.; Powe, N.R.; Crews, D.C. Dietary Habits and Risk of Kidney Function Decline in an Urban Population. J. Ren. Nutr. Off. J. Counc. Ren. Nutr. Natl. Kidney Found. 2017, 27, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Mackenbach, J.D.; Lakerveld, J.; Generaal, E.; Gibson-Smith, D.; Penninx, B.; Beulens, J.W.J. Local fast-food environment, diet and blood pressure: The moderating role of mastery. Eur. J. Nutr. 2019, 58, 3129–3134. [Google Scholar] [CrossRef] [PubMed]
- Mattei, J.; Sotos-Prieto, M.; Bigornia, S.J.; Noel, S.E.; Tucker, K.L. The Mediterranean Diet Score Is More Strongly Associated with Favorable Cardiometabolic Risk Factors over 2 Years than Other Diet Quality Indexes in Puerto Rican Adults. J. Nutr. 2017, 147, 661–669. [Google Scholar] [CrossRef]
- Mertens, E.; Markey, O.; Geleijnse, J.M.; Lovegrove, J.A.; Givens, D.I. Adherence to a healthy diet in relation to cardiovascular incidence and risk markers: Evidence from the Caerphilly Prospective Study. Eur. J. Nutr. 2018, 57, 1245–1258. [Google Scholar] [CrossRef] [PubMed]
- Missikpode, C.; Ricardo, A.C.; Durazo-Arvizu, R.A.; Manoharan, A.; Mattei, J.; Isasi, C.R.; Mossavar-Rahmani, Y.; Talavera, G.A.; Sotres-Alvarez, D.; Daviglus, M.L.; et al. Association of Diet Quality Indices with Longitudinal Changes in Kidney Function in U.S. Hispanics/Latinos: Findings from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Kidney360 2021, 2, 50–62. [Google Scholar] [CrossRef] [PubMed]
- Mousavi, S.N.; Hassani, F.; Namadian, M. Dietary Patterns and the Intake of Trace Elements in People with Hypertension: A Cross-Sectional Study. J. Adv. Med. Biomed. Res. 2020, 28, 1–10. [Google Scholar] [CrossRef]
- Navarro-Prado, S.; Schmidt-RioValle, J.; Montero-Alonso, M.A.; Fernández-Aparicio, Á.; González-Jiménez, E. Stricter Adherence to Dietary Approaches to Stop Hypertension (DASH) and its Association with Lower Blood Pressure, Visceral Fat, and Waist Circumference in University Students. Nutrients 2020, 12, 740. [Google Scholar] [CrossRef]
- Nilsson, A.; Halvardsson, P.; Kadi, F. Adherence to DASH-Style Dietary Pattern Impacts on Adiponectin and Clustered Metabolic Risk in Older Women. Nutrients 2019, 11, 805. [Google Scholar] [CrossRef] [PubMed]
- Ramezankhani, A.; Hosseini-Esfahani, F.; Mirmiran, P.; Azizi, F.; Hadaegh, F. The association of priori and posteriori dietary patterns with the risk of incident hypertension: Tehran Lipid and Glucose Study. J. Transl. Med. 2021, 19, 44. [Google Scholar] [CrossRef] [PubMed]
- Rebholz, C.M.; Crews, D.C.; Grams, M.E.; Steffen, L.M.; Levey, A.S.; Miller, E.R., 3rd; Appel, L.J.; Coresh, J. DASH (Dietary Approaches to Stop Hypertension) Diet and Risk of Subsequent Kidney Disease. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 2016, 68, 853–861. [Google Scholar] [CrossRef]
- Santiago-Torres, M.; Shi, Z.; Tinker, L.F.; Lampe, J.W.; Allison, M.A.; Barrington, W.; Crane, T.E.; Garcia, D.O.; Hayden, K.M.; Isasi, C.R.; et al. Diet quality indices and risk of metabolic syndrome among postmenopausal women of Mexican ethnic descent in the Women’s Health Initiative Observational Study. Nutr. Healthy Aging 2020, 5, 261–272. [Google Scholar] [CrossRef]
- Tangney, C.; Sarkar, D.; Staffileno, B.A. Comparison of three DASH scoring paradigms and prevalent hypertension among older Hispanics. J. Hum. Hypertens. 2016, 30, 210–215. [Google Scholar] [CrossRef]
- Fung, T.T.; Chiuve, S.E.; McCullough, M.L.; Rexrode, K.M.; Logroscino, G.; Hu, F.B. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch. Intern. Med. 2008, 168, 713–720. [Google Scholar] [CrossRef]
- Mellen, P.B.; Gao, S.K.; Vitolins, M.Z.; Goff, D.C., Jr. Deteriorating Dietary Habits Among Adults with Hypertension: DASH Dietary Accordance, NHANES 1988–1994 and 1999–2004. Arch. Intern. Med. 2008, 168, 308–314. [Google Scholar] [CrossRef] [PubMed]
- Valipour, G.; Esmaillzadeh, A.; Azadbakht, L.; Afshar, H.; Hassanzadeh, A.; Adibi, P. Adherence to the DASH diet in relation to psychological profile of Iranian adults. Eur. J. Nutr. 2017, 56, 309–320. [Google Scholar] [CrossRef]
- Lee, H.S.; Lee, K.B.; Hyun, Y.Y.; Chang, Y.; Ryu, S.; Choi, Y. DASH dietary pattern and chronic kidney disease in elderly Korean adults. Eur. J. Clin. Nutr. 2017, 71, 755–761. [Google Scholar] [CrossRef]
- Folsom, A.R.; Parker, E.D.; Harnack, L.J. Degree of concordance with DASH diet guidelines and incidence of hypertension and fatal cardiovascular disease. Am. J. Hypertens. 2007, 20, 225–232. [Google Scholar] [CrossRef]
- Fransen, H.P.; May, A.M.; Stricker, M.D.; Boer, J.M.; Hennig, C.; Rosseel, Y.; Ocké, M.C.; Peeters, P.H.; Beulens, J.W. A posteriori dietary patterns: How many patterns to retain? J. Nutr. 2014, 144, 1274–1282. [Google Scholar] [CrossRef]
- National Heart, Lung, and Blood Institute. Your Guide to Lowering Your Blood Pressure with DASH; National Heart, Lung, and Blood Institute: Bethesda, MD, USA, 2006.
- Siervo, M.; Lara, J.; Chowdhury, S.; Ashor, A.; Oggioni, C.; Mathers, J.C. Effects of the Dietary Approach to Stop Hypertension (DASH) diet on cardiovascular risk factors: A systematic review and meta-analysis. Br. J. Nutr. 2015, 113, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Saneei, P.; Salehi-Abargouei, A.; Esmaillzadeh, A.; Azadbakht, L. Influence of Dietary Approaches to Stop Hypertension (DASH) diet on blood pressure: A systematic review and meta-analysis on randomized controlled trials. Nutr. Metab. Cardiovasc. Dis. NMCD 2014, 24, 1253–1261. [Google Scholar] [CrossRef]
- Guo, R.; Li, N.; Yang, R.; Liao, X.Y.; Zhang, Y.; Zhu, B.F.; Zhao, Q.; Chen, L.; Zhang, Y.G.; Lei, Y. Effects of the Modified DASH Diet on Adults with Elevated Blood Pressure or Hypertension: A Systematic Review and Meta-Analysis. Front. Nutr. 2021, 8, 725020. [Google Scholar] [CrossRef] [PubMed]
- Chiavaroli, L.; Viguiliouk, E.; Nishi, S.K.; Blanco Mejia, S.; Rahelić, D.; Kahleová, H.; Salas-Salvadó, J.; Kendall, C.W.; Sievenpiper, J.L. DASH Dietary Pattern and Cardiometabolic Outcomes: An Umbrella Review of Systematic Reviews and Meta-Analyses. Nutrients 2019, 11, 338. [Google Scholar] [CrossRef] [PubMed]
- Al-Salmi, N.; Cook, P.; D’Souza, M.S. Diet Adherence among Adults with Type 2 Diabetes Mellitus: A Concept Analysis. Oman Med. J. 2022, 37, e361. [Google Scholar] [CrossRef]
- Jannasch, F.; Kröger, J.; Schulze, M.B. Dietary Patterns and Type 2 Diabetes: A Systematic Literature Review and Meta-Analysis of Prospective Studies. J. Nutr. 2017, 147, 1174–1182. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Hoffmann, G. Diet quality as assessed by the Healthy Eating Index, the Alternate Healthy Eating Index, the Dietary Approaches to Stop Hypertension score, and health outcomes: A systematic review and meta-analysis of cohort studies. J. Acad. Nutr. Diet. 2015, 115, 780–800.e785. [Google Scholar] [CrossRef] [PubMed]
- Salehi-Abargouei, A.; Maghsoudi, Z.; Shirani, F.; Azadbakht, L. Effects of Dietary Approaches to Stop Hypertension (DASH)-style diet on fatal or nonfatal cardiovascular diseases–incidence: A systematic review and meta-analysis on observational prospective studies. Nutrition 2013, 29, 611–618. [Google Scholar] [CrossRef]
- Theodoridis, X.; Triantafyllou, A.; Gkaliagkousi, E.; Mastrogiannis, K. Adherence to DASH Diet and Hypertension Risk: A Systematic Review and Meta-Analysis. Nutrients 2023, 15, 3261. [Google Scholar] [CrossRef] [PubMed]


| Study ID | Country | Study Design | Population | No. of Participants (Low/High) | Mean Age (SD) | Exclusion Criteria | DASH Assessment Tool | Use of Anti-Hypertensive Medication |
|---|---|---|---|---|---|---|---|---|
| Benerjee et al., 2019 [14] | U.S. | Prospective observational study | Adults with hypertension and CKD enrolled in the National Health and Nutrition Examination Survey (NHANES) III | 321/197 Total: 1110 | 70.2 ± 12.9 | Missing data on dietary intake, eGFR < 30 or >59 mL/min, pregnancy | DASH Score by Mellen et al. (2008) | ACEI, ARB |
| Bendinellii et al., 2019 [15] | Italy | Cross-sectional observational study | Residents of Florence and Prato | 843/1959 Total: 10,163 | 50.4 ± 7.7 | Diagnosis of hypertension or anti-hypertensive drugs at any time in the past | DASH Score by Fung et al. (2008) | No |
| Bonaccio et al., 2020 [16] | Italy | Prospective observational study | Men and women from the general population of Moli-sami Study | 6368/6013 Total: 12,381 | 55.0 ± 12.0 | EI < 800 kcal/day in men and <500 kcal/day in women or >4000 kcal/day in men and >3500 kcal/day in women, unreliable medical dietary questionnaires, lost to follow-up, missing data on outcome exposure, missing information on the main covariates of interest | DASH Score by Fung et al. (2008) | No |
| Chan et al., 2022 [17] | China, Japan, U.K., U.S. | Cross-sectional observational study | Adults | 410/420 Total: 2164 | 28.9 ± 5.9 | Incomplete dietary data | DASH Score by Fung et al. (2008) | Yes |
| Critselis et al., 2019 [18] | Greece | Prospective observational study | Greek male adults, free of CVD | 965/1054 Total: 2019 | 45.2 ± 14.0 | CVD at baseline | DASH Score by Fung et al. (2008) | No |
| Dai et al., 2022 [19] | China | Prospective observational study | Adults from Tibetan, Yi, Miao, Bai, Bouyei and Dong ethnic groups | No info Total: 81,433 | 50.5 ± 11.2 | <30 y or >79 y, missing information on diet-related variables, missing information on outcome-related data, implausible BMI values (BMI < 14 or >45 kg/m2), unusual daily EI (<600 or >3500 kcal/d for females, <800 or >4200 kcal/d for males), self-reported physician-diagnosed hypertension and use of anti-hypertensive medication | DASH Score by Fung et al. (2008) | No |
| Daniel et al., 2021 [20] | U.S. | Prospective observational study | Chinese, Hispanic, non-Hispanic Black or non-Hispanic white | 4169 Total: 1760 | 60.4 ± 9.5 | Extreme EI of < 500 kcal or >5000 kcal, without FFQ, no cognitive data, using Alzheimer’s medications | DASH Score by Fung et al. (2008) | Yes |
| Epstein et al., 2012 [21] | U.S. | RCT | Healthy, overweight or obese men and women with above-normal BP | 40/26 Total: 144 | 51.3 ± 9.0 | Medication, other comorbidities, too high/low BMI and BP, dietary reasons | DASH Score by Folsom et al. (2007) | No |
| Fransisco et al., 2020 [22] | Brazil | Prospective observational study | Active or retired civil servants of higher education and research institutions | 4987/645 Total: 5632 | 49.9 ± 8.3 | Fulfilled the criteria for hypertension, anti-hypertensive drugs, reported CVD, missing information on BP values, dietary reasons, urinary Na, race/skin color | DASH Score developed based on guidelines by the National Institutes of Health and National Heart Lung and Blood Institute (2018) | No |
| Gao et al., 2021 [23] | China | RCT | Chinese adults with hyperilipidemia | No info Total: 269 | 58.0 ± 8.0 | Known chronic diseases, acute and chronic infectious diseases, trauma or surgery, use of hormonal therapies, use of medications known to influence lipid metabolism within the past six months, use of anti-inflammatory or antibiotic drugs within the past three months, use of vasomotor function drugs within the past three months, taking phytochemicals or other dietary supplements within the past two months and pregnant or lactating women | DASH Score by Fung et al. (2008) | No |
| Gao et al., 2020 [24] | China | Prospective observational study | Adults from Tangshan City | 18,024/19,503 Total: 71,893 | 51.4 ± 0.1 | Previously diagnosed as having gout, reported an implausible EI (<800 kcal/day or >4000 kcal/day for men, and <500 kcal/day or >3500 kcal/day for women), poor results on food frequency questionnaires, incomplete information on demographic data | DASH Score by Fung et al. (2008) | No |
| Ghorabi et al., 2019 [25] | Iran | Cross-sectional observational study | Iranian adults | 136/129 Total: 396 | 38.2 ± 9.5 | Pregnancy, post-menopausal status, lactation, any kind of cancers, medication for modifying fat, blood sugar and BP, ischemic heart disease, use of sedative or hypnotic drug, use of anti-histamine, use of immune system inhibitors, following any special diet for any reasons under the supervision of a diet therapist, being a professional athlete, use of weight loss drug | DASH Score by Valipour et al. (2017) | No |
| Glenn et al., 2021 [26] | Spain | RCT | Older men and women with BMI 27–40 kg/m2 and fulfilled at least three criteria of the MetS | 2026/1636 Total: 6874 | 65.0 | Implausible EI (<500 or >3500 kcal/d for women and <800 or >4000 kcal/d for men) or missing information on FFQ at baseline | DASH Score by Fung et al. (2008) | Yes |
| Goyal et al., 2021 [27] | U.S. | Prospective observational study | African-American and white adults | 4203/5764 Total: 18,856 | 64.0 ± 9.2 | Missing or incomplete FFQ (≤85%), implausible EI (men <3347 kJ/d or >20,920 kJ/d, and women <2093 kJ/d or >18,841) | DASH Score by Fung et al. (2008) | No |
| Harrington et al., 2013 [28] | Ireland | Cross-sectional observational study | Men and women based in a primary care setting in the North Cork Region of the Republic of Ireland | No info Total: 2047 | 60.7 | Duplicates, deaths and ineligibles, mortality, lost to follow-up, too unwell to participate | DASH Score by Fung et al. (2008) | No |
| Hu et al., 2021 [29] | U.S. | Prospective observational study | Men and women with an estimated eGFR 20–70 mL/min/1.73 m2 | 912/795 Total: 2403 | 57.3 ± 11.3 | Unfilled FFQ, extreme self-reported EI (women: <500 or >3500 kcal/d; men: <700 or >4500 kcal/d), not sufficient data to calculate all dietary pattern scores, missing covariates of interest | DASH Score by Fung et al. (2008) | ACEI, ARB |
| Ishikawa et al., 2022 [30] | U.S. | Cross-sectional observational study | Adults with self-reported diagnosis of HF | 76/81 Total: 348 | 65.3 ± 0.9 | Did not attend the mobile examination center morning session, incomplete data on fasting plasma glucose and insulin to calculate the HOMA-IR, physician diagnosis of DM or used diabetes medications, pregnancy, implausible EI (gender-specific <1st and >99th percentiles of EI per day) | DASH Score by Fung et al. (2008) | ACEIs, ARBs, beta-blockers, loop diuretics |
| Jalilpiran et al., 2020 [31] | Iran | Cross-sectional observational study | Older adult men living in southern Tehran | 203/154 Total: 357 | 64.9 ± 6.5 | Malignant diseases (e.g., cancer), under- or over-reported total EI (<800 kcal/day and >4200 kcal/day), under- and over-reporting of total EI | DASH Score by Fung et al. (2008) | No info |
| Jayedi et al., 2019 [32] | Iran | Case–control study | Women with type 2 DM and diabetic nephropathy at Kowsar Diabetes Clinic in Semnan | No info Total: 210 | 55.3 ± 7.0 | GDM, type 1 DM, medication treatment, previous history of cancer, myocardial infarction, hepatic disease, autoimmune disorders, stroke and coronary angiography | DASH Score by Fung et al. (2008) | beta-blockers, ACEIs, ARBs |
| Jones et al., 2018 [33] | U.K. | Prospective observational study | Men and women participating in general practices in Norfolk | 5744/4181 Total: 23,655 | 59.1 | Missing FFQ data, missing baseline CVD data, missing covariate data, incorrect date of death | DASH Score by Fung et al. (2008) | Yes |
| Kang et al., 2018 [34] | Korea | Cross-sectional observational study | Post-menopausal women from South Korean population | 1606/1623 Total: 6826 | 58.5 ± 6.3 | Missing clinical data, DM, extremely low or high EI (<500 kcal or 5000 kcal) | DASH Score by Lee et al. (2017) | No |
| Khodarahmi et al., 2021 [35] | Iran | Cross-sectional observational study | Healthy obese adults in the city of Tabriz | No info Total: 347 | 38.0 ± 7.4 | Pregnancy, lactation, menopausal women, medical history of chronic diseases (CVD, hypertension, hyperlipidemia, DM, renal diseases, hepatic disorders and cancer), recent surgery such as bariatric surgery, any medications and supplements which had effects on weight and variables studied such as loop diuretics, corticosteroids, antidepressants, statins and anti-hypertensive agents, EI outside of the range of 800–4200 kcal/day | DASH Score by Fung et al. (2008) | No |
| Kim et al., 2022 [36] | U.S. | Prosopective observational study | Men and women of African American, Hispanic, Asian, Indian, Pacific Islander and Native American origins | 522/410 Total: 1899 | 67.0 ± 9.0 | Missing information on diets and covariates, missing mortality | DASH Score by Fung et al. (2008) | Yes |
| Köroğlu et al., 2020 [37] | Turkey | Cross-sectional observational study | Male patients with at least one year and maximum three years of amputation history | No info Total: 35 | 36.9 ± 9.3 | DM, hypertension, thyroid dysfunction, amputees due to vascular problems | DASH Score developed based on guidelines by the National Institutes of Health and National Heart Lung and Blood Institute (2018) | No |
| Lin et al., 2011 [38] | U.S. | Prospective observational study | U.S. female nurses | 780/780 Total: 3121 | 67.0 | No cumulative average dietary pattern data available, no measured plasma creatine in sample collection | DASH Score by Fung et al. (2008) | ACEI, ARB |
| Liu et al., 2017 [39] | U.S. | Prospective observational study | African American and white people from U.S. census tracts in Baltimore City, Maryland | 648/886 Total: 1534 | 48.0 | Did not undergo serum creatinine at baseline, no dietary intake data, eGFR <60 mL/min per 1.73 m2 at baseline, survived but did not undergo a follow-up serum creatinine measurement | DASH Score by Mellen et al. (2008) | No |
| Mackenbach et al., 2019 [40] | The Netherlands | Cross-sectional observational study | Adults (Netherlands Study of Depression and Anxiety) | 344/347 Total: 1543 | 52.4 ± 12.9 | Incomplete FFQ, extreme EI, missing data on their six-digit postcode, hypertensive medication | DASH Score by Fung et al. (2008) | No |
| Mattei et al., 2017 [41] | U.S. | Propsective observational study | Self-identified Puerto Ricans residing in Boston | No info Total: 1189 | Low: 55.3 ± 7.1 High: 58.8 ± 7.3 | Unable to answer questions due to serious health conditions, planned to move away from the area within two years, low MMSE score (≤10) | DASH Score by Fung et al. (2008) | Yes |
| Mertens et al., 2017 [42] | U.K. | Prospective observational study | Middle-aged men from the town of Caerphilly and adjoining villages, South Wales (U.K.) | 550/713 Total: 1867 | 56.6 ± 4.3 | Men who died, history of myocardial infarction or stroke, DM, missing dietary data | DASH Score by Fung et al. (2008) | No |
| Missikpode et al., 2021 [43] | U.S. | Prospective observational study | Adults self-identified as Hispanic/Latino | 2480/2481 Total: 9921 | 41.0 ± 0.28 | Missing information on kidney-function measures, incomplete diet data, missing data on covariates, CKD at baseline | DASH Score by Fung et al. (2008) | ACEI, ARB |
| Mousavi et al., 2020 [44] | Iran | Cross-sectional observational study | Adults with mild to moderate hypertension | 25/25 Total: 101 | 40.7 ± 4.48 | Angina pectoris, type 1 DM, renal diseases, pregnancy and lactation, special diet and intake of supplements | DASH Score derived from PCA (Fransen et al., 2014) | Yes |
| Navarro-Prado et al., 2020 [45] | Spain | Cross-sectional observational study | University students during the 2013–2014 academic year | 73/69 Total: 244 | 22.4 ± 4.76 | Accepted and signed an informed consent document, previously diagnosed with an endocrine disease, lacking anthropometric, dietary or demographic data, ≥32 years old | DASH Score by Fung et al. (2008) | No |
| Nilsson et al., 2019 [46] | Sweden | Cross-sectional observational study | Community-dwelling women | No info Total: 112 | 67.0 ± 1.6 | CHD and DM, disability with respect to mobility, using prescribed anti-inflammatory medication, smokers, incomplete data on PA, incomplete data on inflammatory and metabolic biomarkers | DASH Score by Fung et al. (2008) | Yes |
| Ramezankhani et al., [47] | Iran | Prospective observational study | Adult residents of Tehran participating in Tehran Lipid and Glucose Study (TLGS) | 1254/1279 Total: 4793 | 38.9 ± 12.7 | Under- or over-reporters of EI (<800 or ≥4200 kcal/day), hypertension at baseline, missing data on hypertension status without any follow-up data | DASH Score by Fung et al. (2008) | No |
| Rebholz et al., 2016 [48] | U.S. | Prospective observational study | Participants of Atherosclerosis Risk in Communities Study (ARIC), predominantly African American and white with baseline eGFR ≥60 mL/min/1.73 m | 5759/4840 Total: 14,882 | 54.1 ± 5.7 | Missing dietary ΕΙ data, implausibly low caloric intake (<600 kcal for men and <500 kcal for women) and implausibly high caloric EI (>4200 kcal for men and >3600 kcal for women), baseline eGFR <60 mL/min/1.73 m2 or ESRD, identified by linkage to the US Renal Data System registry, neither African American nor white, missing covariates | DASH Score by Mellen et al. (2008) | ACEI, ARB |
| Santiago-Torres et al., 2020 [49] | U.S. | Prospective observational study | Post-menopausal women of Mexican ethnic descent who participated in the Women’s Health Initiative (WHI) | 117/106 Total: 334 | 58.6 ± 6.4 | Non-Mexican, American or Chicana, metabolic syndrome, diabetes, participated in the intervention group for the Dietary Modification trial, either low or high self-reported EI from the FFQ (<500 or >4000 kcal) | DASH Score by Fung et al. (2008) | Yes |
| Tangney et al., 2015 [50] | U.S. | Cross sectional observational study | Older Latino adults from CAPACES (who had a score less than 14 on a 21-point Mini-Mental State Examination) | Fung: 35/28 | 66.0 ± 9.0 | Less than 50 years old, score <14 on the shortened MMSE, too young, used a walking assistive device, not Latino | DASH Score by Fung et al. (2008) | Yes |
| Study ID | Comorbidities (Low/High) * | Percentage (%) of Participants with HTN (Low/High) | BMI (Low/High) * | SBP (Low/High) * | DBP (Low/High) * | Physical Activity (Low/High) * | Smoking Status (Low/High) | Sodium Intake (mg) | Potassium Intake (mg) |
|---|---|---|---|---|---|---|---|---|---|
| Benerjee et al., 2019 [14] | CKD | No info | 26.5 ± 4.9/ 28.7 ± 6.0 | 154.1 ± 1.4/ 151.5 ± 1.6 | No info | Moderate: 96.0%/93.8% Intense: 4.0%/6.2% | Current: 22.0%/6.3% Past: 37.4%/53.4 Never: 40.6%/40.3% | 1809.9 ± 26.0/ 1597.9 ± 48.1 | 1227.7 ± 15.1/ 2249.6 ± 35.4 |
| Bendinellii et al., 2019 [15] | No | No info | Under/normal weight: 55.9%/53.9% Overweight: 33.9%/35.6% Obesity: 10.2%/10.6% | 124.6 ± 15.7/ 123.6 ± 15.7 | 80.0 ± 9.4/ 79.2 ± 9.1 | Inactive: 22.5%/16.6% Moderately inactive: 23.4%/23.9% Moderately active: 45.0%/47.7% Active: 9.1%/11.7% | Current: 34.2%/24.5% Former: 25.5%/31.3% Never smoked: 40.3%/44.3% | 2740.0 ± 9.9/2640.0 ± 11.3 | No info |
| Bonaccio et al., 2020 [16] | Obesity, DM (3.7%/5.6%), Hyperlipidemia (5.3%/10.3%) | 22.5%/31.5% | Obesity: 29.1%/29.3% | 140.0 ± 20.0/ 140.0 ± 21.0 | 82.0 ± 9.0/82.0 ± 9.0 | Leisure-time PA (MET-h/day): 42.6%/56.5% | Current: 27.2%/19.4% | No info | No info |
| Chan et al., 2022 [17] | CVD (42.2%/33.8%) | No info | 30.5 ± 6.3/ 26.9 ± 5.0 | 120.8 ± 13.6/ 114.8 ± 13.3 | 73.7 ± 9.8/ 71.5 ± 9.2 | Μoderate or heavy (hours/day): 4.0 ± 3.7/3.0 ± 2.9 | Current: 31.2%/5.5% | No info | No info |
| Critselis et al., 2019 [18] | Hypercholesterolemia (40.6%/44.5%), DM (7.4%/7.0%), MetS (18.4%/20.9%) | 29.9%/33.0% | 26.1 ± 4.4/ 26.5 ± 4.6 | 123.0 ± 18.2/ 123.0 ± 18.5 | 78.6 ± 11.2/ 79.4 ± 11.9 | 38.9%/42.7% | 42.5%/42.6% | No info | No info |
| Dai et al., 2022 [19] | Hypertension, Depression, Insomnia | 25.7%/20.4% | 24.2 ± 3.6/ 23.9 ± 3.3 | 125.8 ± 17.6/ 123.0 ± 16.5 | 79.5 ± 11.1/ 77.7 ± 10.5 | 29.1 ± 19.7/ 24.4 ± 16.7 (MET hours/day) | Never: 74.7%/76.6% Previous: 21.8%/17.7% Current: 3.5%/5.7% | No info | No info |
| Daniel et al., 2021 [20] | DM (9.3%/7.5%) | 40.3%/41.4% | 29.3 ± 5.3/ 27.4 ± 5.0 | 124.3 ± 19.7/ 125.5 ± 21.4 | 73.9 ± 10.0/ 69.9 ± 10.1 | 1456.1 ± 2631.8/ 1956.6 ± 2641.9 (MET min/week) | Current: 21.2%/4.9% | No info | No info |
| Epstein et al., 2012 [21] | Obesity | Total: 47% | No info | 129.2 ± 1.9/ 134.5 ± 2.2 | 76.6+1.1/ 80.9+1.3 | No info | No info | No info | No info |
| Fransisco et al., 2020 [22] | DM (8.1%/9.5%) | No info | 25.8 ± 4.2/ 24.9 ± 3.8 | 114.5 ± 11.5/ 114.5 ± 11.8 | 72.7 ± 8.1/ 71.4 ± 8.2 | Light: 78.6%/62.8% Μoderate: 14.1%/24.9% Vigorous: 7.3%/12.4% | Non-smoker: 58.8%/65.3% Former: 25.8%/25.4% Smokers: 15.4%/9.3% | No info | 3982.0 ± 1607.0/ 5260.0 ± 1664.0 |
| Gao et al., 2021 [23] | Central obesity (total 44.2%) | No info | Underweight (total 12%) Overweight (total 39.4%) Obesity (total 11.5%) | No info | No info | No info | No: 93.3% Yes: 6.7% | No info | No info |
| Gao et al., 2020 [24] | CHD (1.6%/2.5%) Hyperuricemia (18.3%/14.4%) | No info | 24.7 ± 0.03/ 24.8 ± 0.03 | 132.8 ± 0.1/ 131.8 ± 0.1 | 80.0 ± 0.1/ 80.8 ± 0.1 | Low: 29.4%/48.1% Μoderate: 21.1%/8.6% High: 33.0%/26.0% Unknown: 16.4%/17.2% | No: 51.5%/58.5% Yes: 48.5%/41.5% | No info | No info |
| Ghorabi et al., 2019 [25] | Components of MetS: Abdominal obesity: 30.6%/36.1%, Elevated BP: 47.3%/22.1%, High TG: 43.5%/23.2%, Reduced HDL: 27.7%/40.1%, Abnormal GL: 41.0%/32.7% | No info | 28.7 ± 4.9/ 28.5 ± 4.9 | 102.5 ± 35.8/ 68.1 ± 52.1 | 53.7 ± 33.1/ 45.8 ± 35.0 | No info | Current: 35.3%/23.5% | No info | No info |
| Glenn et al., 2021 [26] | DM (29.0%/32.0%), Hypercholesterolemia (76.0%/75.0%) | 93.0%/94.0% | 32.8 ± 3.5/ 32.1 ± 3.4 | No info | No info | 2193.0 ± 2154.0/ 2856.0 ± 2444.0 (MET min/week) | Never: 41.0%/48.0% Former: 44.0%/42.0% Current: 15.0%/32.1% | No info | No info |
| Goyal et al., 2021 [27] | Atrial fibrilation (7.3%/7.3%), DM (14.9%/17.3%) | 57.4%/53.8% | 29.0 ± 6.2/ 28.0 ± 5.7 | 128.0 ± 16.0/126.0 ± 16.0 | 77.0 ± 9.7/76.0 ± 9.1 | 4 or more times/week: 24.4%/32.0% 1 to 3 times/week: 34.7%/39.9% None: 40.9%/28.2% | Current: 26.0%/9.5% Past: 36.9%/42.1% Never: 37.2%/48.4% | No info | No info |
| Harrington et al., 2013 [28] | Hypertension | 33.6%/27.3% | No info | 131.3 ± 16.4/ 126.8 ± 16.6 | 80.9 ± 9.9/ 79.8 ± 9.6 | No info | No info | No info | No info |
| Hu et al., 2021 [29] | CKD, DM (37.0%/49.0%) | 85.0%/79.0% | 32.0 ± 8.0/ 32.0 ± 8.0 | 127.0 ± 21.0/ 125.0 ± 20.0 | 73.0 ± 13.0/ 69.0 ± 11.0 | 204.0 ± 135.0/ 198.0 ± 118.0 (METs/week) | 21.0%/5.0% | 2922.0 ± 1415.0/ 2788.0 ± 1268.0 | 2723.0 ± 1240.0/ 3311.0 ± 1313.0 |
| Ishikawa et al., 2022 [30] | No info | No info | No info | 122.4 ± 3.1/ 132.3 ± 2.8 | 70.9 ± 2.2/ 62.6 ± 1.9 | No info | 51.3%/4.3% | No info | No info |
| Jalilpiran et al., 2020 [31] | Any disease (dyslipidemia, HTN, abnormal GL levels) 60.9%/39.1% | No info | 25.7 ± 2.8/ 25.3 ± 3.4 | No info | No info | No info | 51.0%/14.8% | No info | 3710.0 ± 62.5/ 4528.8 ± 71.6 |
| Jayedi et al., 2019 [32] | Type 2 DM, Diabetic nephropathy | No info | 27.5 ± 4.6/ 28.7 ± 3.8 | 125.0 ± 15.2/ 126.3 ± 13.15 | 83.5 ± 11.9/ 79.0 ± 11.4 | Low: 28.4%/32.9% Moderate: 35.8%/36.7% High: 35.8%/30.4% | No info | No info | No info |
| Jones et al., 2018 [33] | DM (4.1%/4.1%) | No info | No info | 136.8/135.0 | 83.4/81.5 | Inactive: 1953/920 Active: 3791/3261 | Current: 19.0%/6.0% | No info | No info |
| Kang et al., 2018 [34] | MetS | No info | 24.3 ± 3.1/ 24.0 ± 2.9 | 123.9 ± 17.7/ 121.4 ± 17.2 | 77.5 ± 9.9/ 76.9 ± 9.8 | 47.0%/54.7% | Non-smoker: 92.3%/94.9% Ex-smoker: 1.6%/2.0% Current smoker: 6.1%/3.1% | No info | No info |
| Khodarahmi et al., 2021 [35] | Obesity, Depression, MetS | No info | No info | 120** (105.0, 130.0)/110.0** (110.0, 130.0) | 77.5 ± 12.6/70.4 ± 16.6 | Men Low: 35.3%/35.3% Moderate: 46.9%/12.5% High: 26.7%/23.3% Women Low: 33.9%/25.0% Moderate: 45.0%/30.0% High: 31.3%/18.8% | No info | No info | No info |
| Kim et al., 2022 [36] | Type 2 DM (63.0%/46.0%) | No info | 29.0 ± 6.0/ 27.0 ± 5.0 | 129.0 ± 17.0/ 128.0 ± 18.0 | No info | Score 1: 35.0 ± 6.0/ 36.0 ± 5.0 | Current: 14.0%/14.0% Former: 36.0%/32.0% | No info | No info |
| Köroğlu et al., 2020 [37] | Traumatic lower limb amputation | No info | 31.0 ± 7.7/ 24.1 ± 2.5 | 120.0 ± 17.6/112.5 ± 6.3 | 80.0 ± 11.7/ 77.5 ± 3.1 | No info | No info | No info | No info |
| Lin et al., 2011 [38] | DM (24.6%/20.3%), hypercholesterolemia (65.0%/66.4%), CVD (6.8%/5.3%) | 56.5%/48.3% | 27.3 ± 1.3/ 25.1 ± 0.9 | 130.0 ± 3.2/ 125.0 ± 3.2 | 79.5 ± 2.9/ 77.5 ± 1.6 | 8.8 ± 2.5/ 18.9 ± 3.9 (METs/week) | Current: 11.6%/2.2% Ever: 56.3%/48.4% | 2007.5 ± 67.5/ 1923.5 ± 60.4 | No info |
| Liu et al., 2017 [39] | Obesity (42.4%/41.1%), DM (15.5%/15.6%) | 42.1%/43.0% | 29.7 ± 7.6/ 29.8 ± 7.8 | 120.0 ± 19.0/ 119.0 ± 19.0 | No info | No info | Current: 52.3%/41.7% Former: 20.0%/21.4% None: 27.8%/36.9% | No info | No info |
| Mackenbach et al., 2019 [40] | Depression | 17.6%/12.6% | 26.7 ± 4.8/ 25.2 ± 4.0 | 139.9 ± 21.4/ 137.1 ± 21.7 | No info | No info | Current: 38.4%/13.0% | No info | No info |
| Mattei et al., 2017 [41] | DM (36.4%/37.4%), CVD (19.4%/25.9%), Obesity (53.4%/57.4%) | 68.2%/70.4% | 31.8 ± 6.9/ 31.7 ± 6.3 | 135.0 ± 21.0/ 136.0 ± 19.0 | 82.1 ± 11.9/ 79.4 ± 9.8 | Score 2: 31.0 ± 3.8/ 32.0 ± 4.6 | Current: 31.1%/13.8% | No info | No info |
| Mertens et al., 2017 [42] | CVD | No info | 25.5 ± 3.5/ 27.1 ± 3.4 | 145.3 ± 19.7/ 144.4 ± 19.8 | 82.6 ± 10.7/ 83.1 ± 10.1 | Active: 42.4%/44.3% | Current: 61.8%/28.9% | 2575.0 ± 596.7/ 2134.8 ± 577.3 | No info |
| Missikpode et al., 2021 [43] | DM (12.0%/19.0%), CVD (21.0%/25.0%) | 21.0%/24.0% | 29.6 ± 9.5/ 29.4 ± 8.9 | 119.6 ± 20.9/119.7 ± 26.4 | 72.4 ± 16.9/71.3 ± 16.4 | Low PA level: 44.0%/42.0% | Current: 28.0%/12.0% | No info | No info |
| Mousavi et al., 2020 [44] | Mild to moderate HTN | No info | 29.7 ± 4.3/ 29.1 ± 5.1 | 144.4 ± 10.9/ 143.0 ± 12.7 | 88.3 ± 10.5/ 88.8 ± 7.25 | 4192.5 ± 6088.1/ 4132.3 ± 5508.6 (MET/min/week) | No info | 3338.7 ± 978.7/ 2949.2 ± 320.2 | 2011.9 ± 694.5/ 2030.4 ± 915.6 |
| Navarro-Prado et al., 2020 [45] | No info | No info | 23.1 ± 4.1/ 23.1 ± 3.89 | 118.2 ± 13.3/ 111.6 ± 10.1 | 69.3 ± 12.1/65.2 ± 9.6 | PAQ-C summary score: 3.9 ± 0.8/ 4.1 ± 0.8 | No info | 2800.0 ± 940.0/2400.0 ± 1130.0 | 2400.0 ± 850.0/ 2600.0 ± 1140.0 |
| Nilsson et al., 2019 [46] | Obesity, Dyslipidemia | No info | No info | 134.0 ± 15.0/ 139.0 ± 14.0 | 79.0 ± 9.0/ 79.0 ± 7.0 | Daily time in moderate to vigorous PA (min): 23.0 ± 16.0/ 30.0 ± 24.0 | No info | No info | No info |
| Ramezankhani et al., [47] | DM (3.3%/7.7%) | No info | 26.0 ± 4.6/ 27.5 ± 4.5 | 109.0 ± 12.0/ 107.0 ± 11.7 | 72.5 ± 8.5/ 73.2 ± 8.2 | Low PAL: 75.2%/64.3% | Current: 32.5%/13.4% | No info | No info |
| Rebholz et al., 2016 [48] | DM (9.2%/13.0%) Obesity | 35.9%/32.7% | No info | 122.3 ± 19.1/ 119.6 ± 18.3 | No info | PAI: 2.3 ± 0.7/ 2.6 ± 0.8 | Current: 35.7%/17.2% | No info | No info |
| Santiago-Torres et al., 2020 [49] | MetS (42.0%/25.0%) | No info | No info | 120.0 ± 10.5/ 121.0 ± 13.4 | 70.6 ± 6.9/ 71.0 ± 8.0 | No info | No info | No info | No info |
| Tangney et al., 2015 [50] | Hypertension | Fung DASH Score: 23.0%/36.0% | Toledo DASH Score: 29.5 ± 4.4/30.7 ± 2.5 Fung DASH Score: 29.9 ± 5.7/31.0 ± 5.4 Folsom DASH Score: 30.3 ± 3.8/29.6 ± 4.5 | Fung DASH Score: 128.0 ± 18.0/132.0 ± 20.0 | Fung DASH Score: 70.0 ± 11.0/ 69.0 ± 12.0 | No info | No info | No info | No info |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Theodoridis, X.; Triantafyllou, A.; Chrysoula, L.; Mermigkas, F.; Chroni, V.; Dipla, K.; Gkaliagkousi, E.; Chourdakis, M. Impact of the Level of Adherence to the DASH Diet on Blood Pressure: A Systematic Review and Meta-Analysis. Metabolites 2023, 13, 924. https://doi.org/10.3390/metabo13080924
Theodoridis X, Triantafyllou A, Chrysoula L, Mermigkas F, Chroni V, Dipla K, Gkaliagkousi E, Chourdakis M. Impact of the Level of Adherence to the DASH Diet on Blood Pressure: A Systematic Review and Meta-Analysis. Metabolites. 2023; 13(8):924. https://doi.org/10.3390/metabo13080924
Chicago/Turabian StyleTheodoridis, Xenophon, Areti Triantafyllou, Lydia Chrysoula, Fotios Mermigkas, Violeta Chroni, Konstantina Dipla, Eugenia Gkaliagkousi, and Michail Chourdakis. 2023. "Impact of the Level of Adherence to the DASH Diet on Blood Pressure: A Systematic Review and Meta-Analysis" Metabolites 13, no. 8: 924. https://doi.org/10.3390/metabo13080924
APA StyleTheodoridis, X., Triantafyllou, A., Chrysoula, L., Mermigkas, F., Chroni, V., Dipla, K., Gkaliagkousi, E., & Chourdakis, M. (2023). Impact of the Level of Adherence to the DASH Diet on Blood Pressure: A Systematic Review and Meta-Analysis. Metabolites, 13(8), 924. https://doi.org/10.3390/metabo13080924





