Gas Chromatography–Mass Spectrometry Reveals Stage-Specific Metabolic Signatures of Ankylosing Spondylitis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Sample Preparation and Metabolomics Analysis
2.3. Statistical Analysis
3. Results
3.1. Characterization of the Subjects
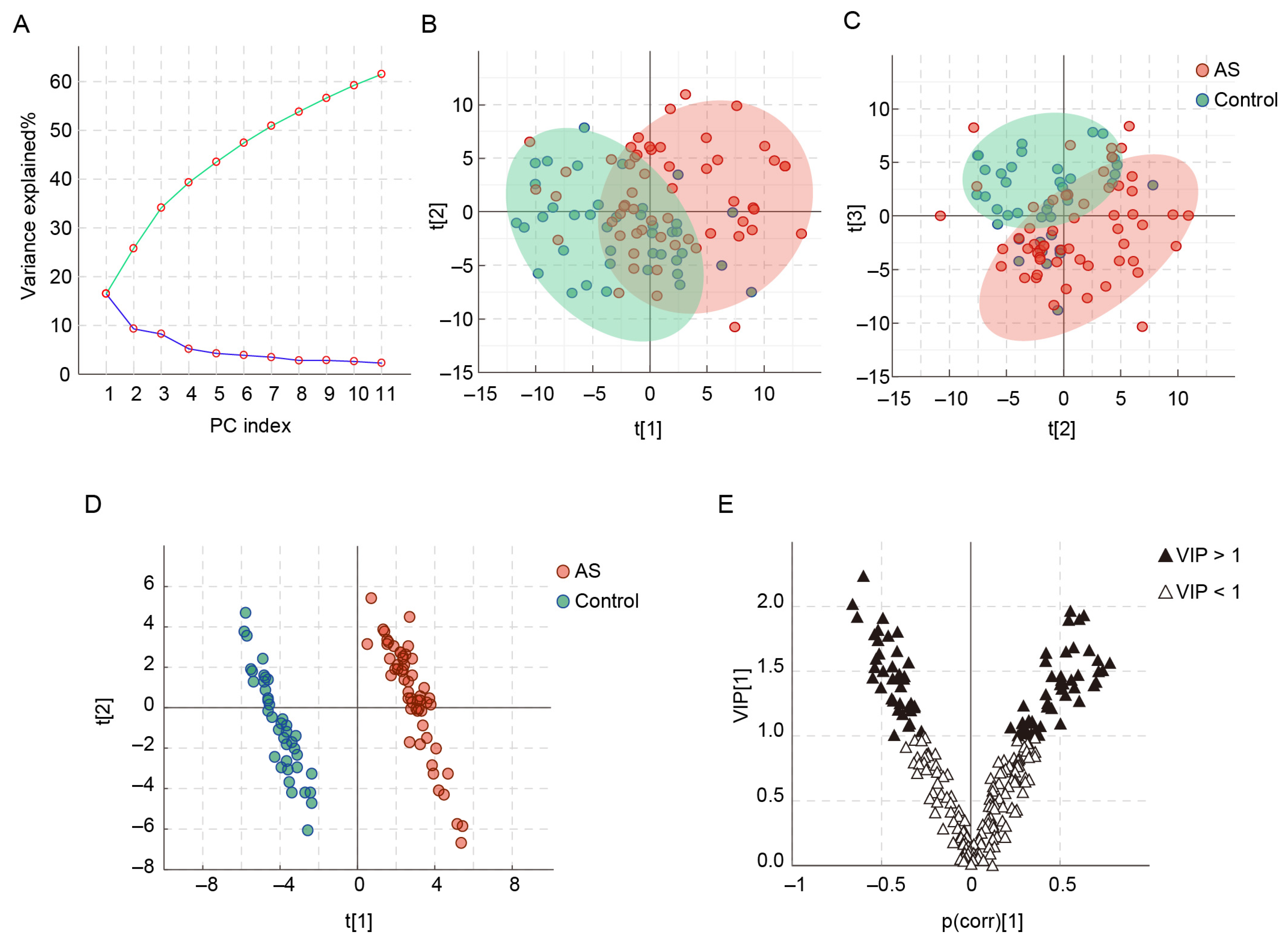
3.2. Characteristics of the Serum Metabolomics Analysis
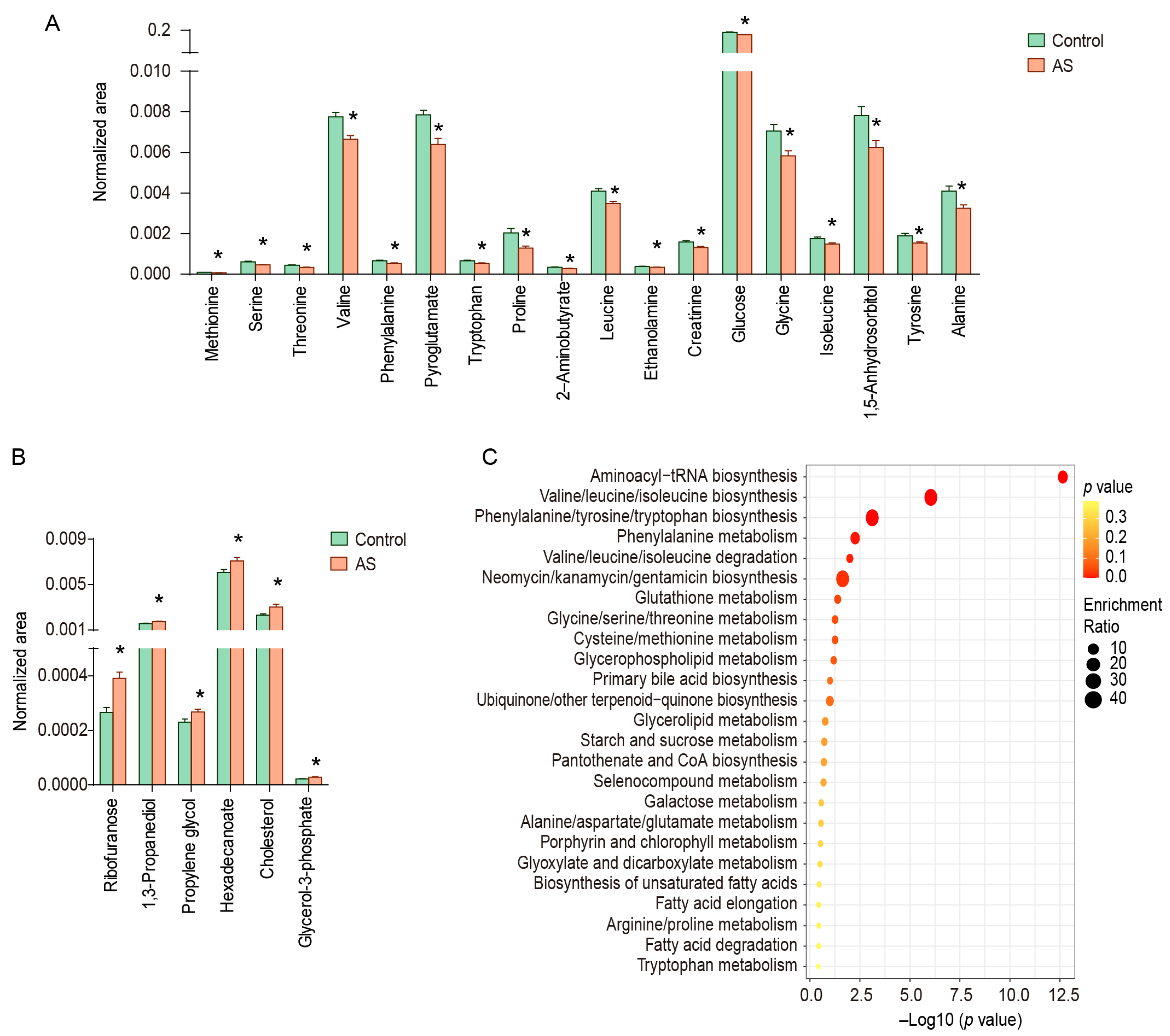
3.3. Serum Metabolic Differences between AS Patients and Controls
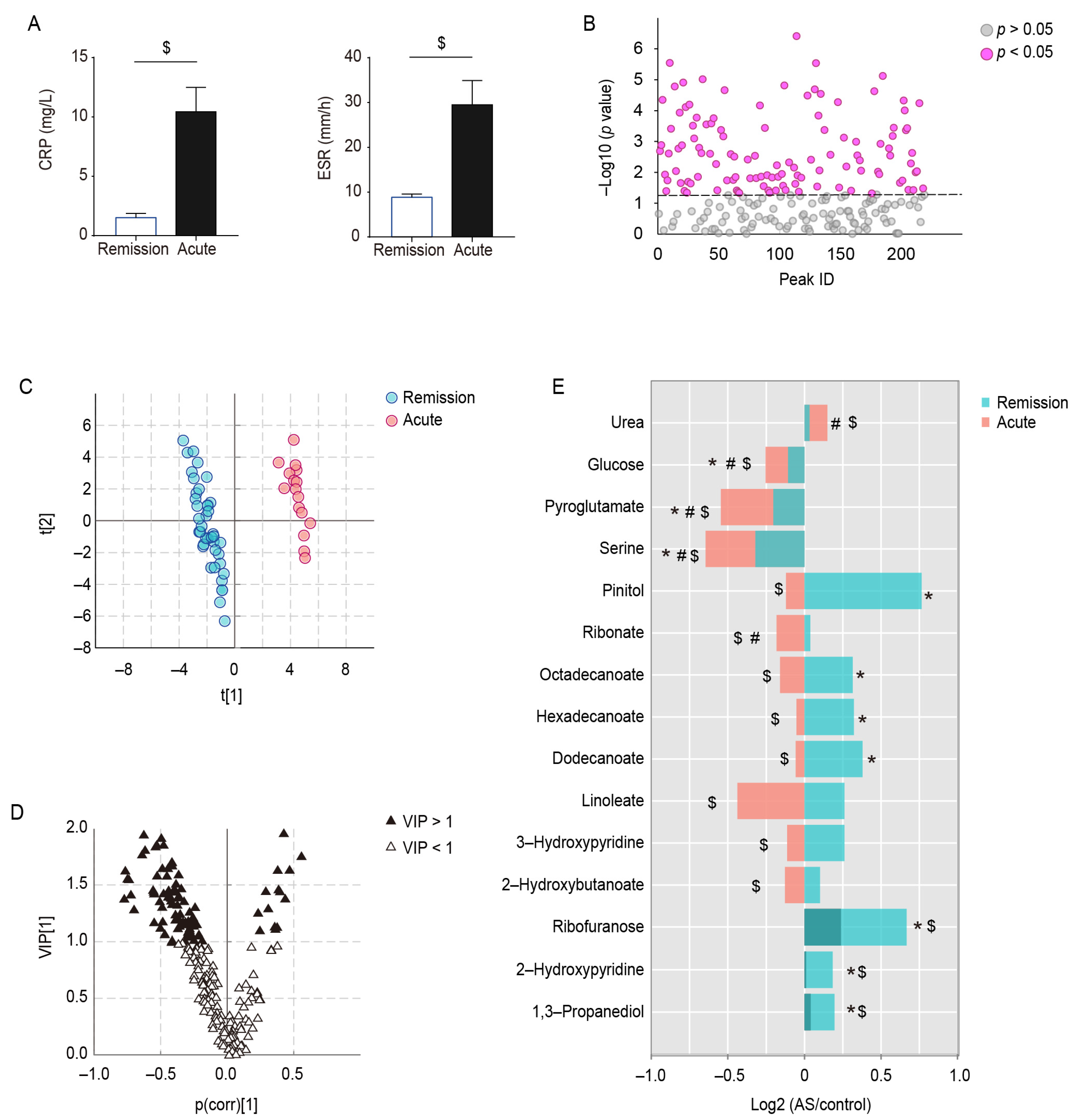
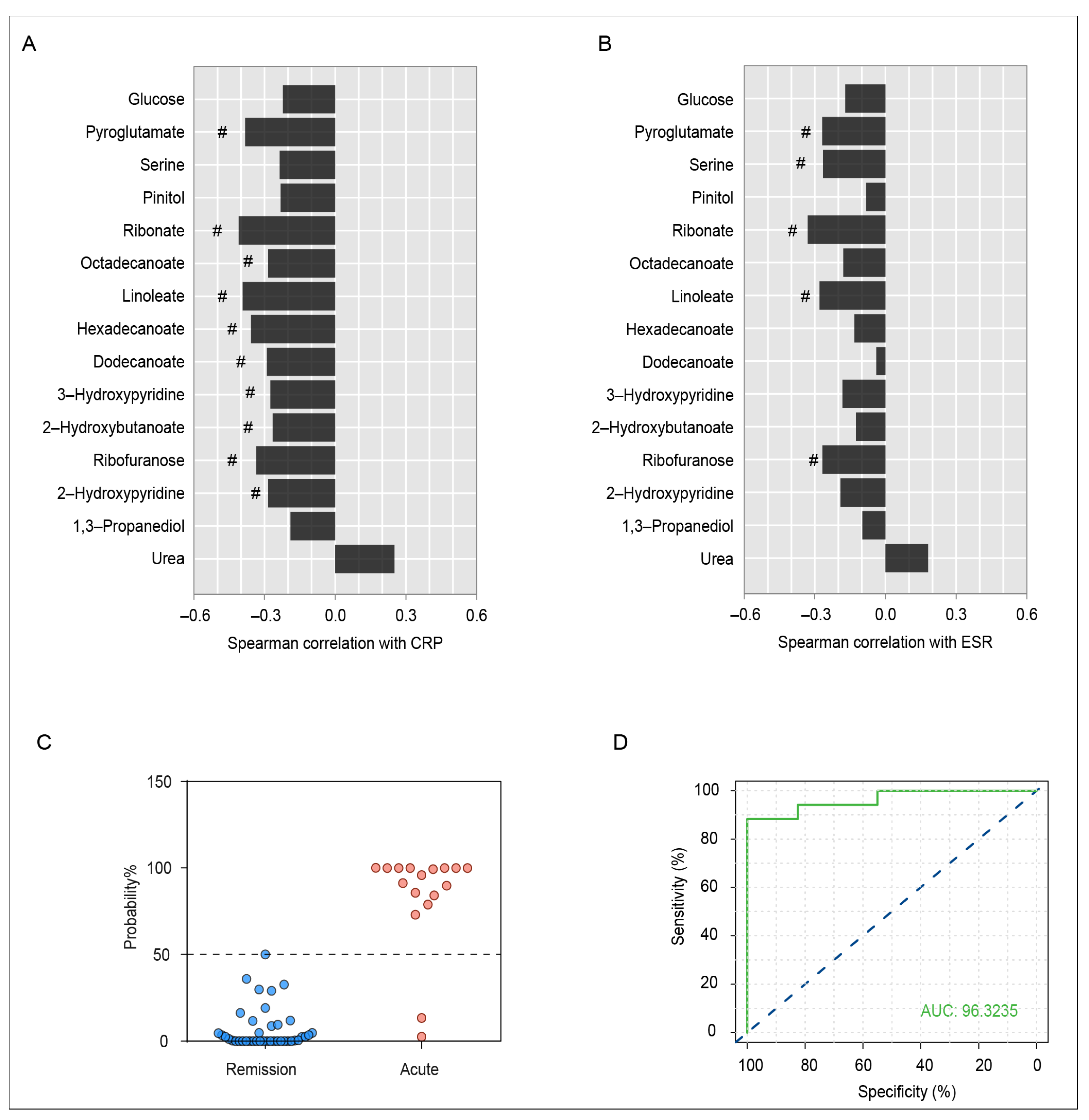
3.4. Serum Metabolic Differences between Acute and Remission Stages of AS Patients
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Liu, L.; Yuan, Y.; Zhang, S.; Xu, J.; Zou, J. Osteoimmunological insights into the pathogenesis of ankylosing spondylitis. J. Cell. Physiol. 2021, 236, 6090–6100. [Google Scholar] [CrossRef]
- Smith, J.A. Update on ankylosing spondylitis: Current concepts in pathogenesis. Curr. Allergy Asthma Rep. 2015, 15, 489. [Google Scholar] [CrossRef]
- Watad, A.; Bridgewood, C.; Russell, T.; Marzo-Ortega, H.; Cuthbert, R.; McGonagle, D. The Early Phases of Ankylosing Spondylitis: Emerging Insights From Clinical and Basic Science. Front. Immunol. 2018, 9, 2668. [Google Scholar] [CrossRef]
- Costantino, F.; Talpin, A.; Said-Nahal, R.; Goldberg, M.; Henny, J.; Chiocchia, G.; Garchon, H.J.; Zins, M.; Breban, M. Prevalence of spondyloarthritis in reference to HLA-B27 in the French population: Results of the GAZEL cohort. Ann. Rheum. Dis. 2015, 74, 689–693. [Google Scholar] [CrossRef]
- Zochling, J.; Braun, J. Assessments in ankylosing spondylitis. Best Pract. Res. Clin. Rheumatol. 2007, 21, 699–712. [Google Scholar] [CrossRef]
- Braun, J.; Sieper, J. Ankylosing spondylitis. Lancet 2007, 369, 1379–1390. [Google Scholar] [CrossRef]
- Agca, R.; Heslinga, S.C.; Rollefstad, S.; Heslinga, M.; McInnes, I.B.; Peters, M.J.; Kvien, T.K.; Dougados, M.; Radner, H.; Atzeni, F.; et al. EULAR recommendations for cardiovascular disease risk management in patients with rheumatoid arthritis and other forms of inflammatory joint disorders: 2015/2016 update. Ann. Rheum. Dis. 2017, 76, 17–28. [Google Scholar] [CrossRef]
- Tan, S.; Yao, J.; Ward, M.M.; Yao, L.; Summers, R.M. Computer aided evaluation of ankylosing spondylitis using high-resolution CT. IEEE Trans. Med. Imaging 2008, 27, 1252–1267. [Google Scholar] [CrossRef]
- Van der Heijde, D.; Landewe, R. Imaging in spondylitis. Curr. Opin. Rheumatol. 2005, 17, 413–417. [Google Scholar] [CrossRef]
- De Vlam, K. Soluble and tissue biomarkers in ankylosing spondylitis. Best Pract. Res. Clin. Rheumatol. 2010, 24, 671–682. [Google Scholar] [CrossRef]
- Dunn, W.B.; Broadhurst, D.; Begley, P.; Zelena, E.; Francis-McIntyre, S.; Anderson, N.; Brown, M.; Knowles, J.D.; Halsall, A.; Haselden, J.N.; et al. Procedures for large-scale metabolic profiling of serum and plasma using gas chromatography and liquid chromatography coupled to mass spectrometry. Nat. Protoc. 2011, 6, 1060–1083. [Google Scholar] [CrossRef]
- Johnson, C.H.; Ivanisevic, J.; Siuzdak, G. Metabolomics: Beyond biomarkers and towards mechanisms. Nat. Rev. Mol. Cell Biol. 2016, 17, 451–459. [Google Scholar] [CrossRef] [PubMed]
- Rinschen, M.M.; Ivanisevic, J.; Giera, M.; Siuzdak, G. Identification of bioactive metabolites using activity metabolomics. Nat. Rev. Mol. Cell Biol. 2019, 20, 353–367. [Google Scholar] [CrossRef] [PubMed]
- Bujak, R.; Struck-Lewicka, W.; Markuszewski, M.J.; Kaliszan, R. Metabolomics for laboratory diagnostics. J. Pharm. Biomed. Anal. 2015, 113, 108–120. [Google Scholar] [CrossRef] [PubMed]
- Rutowski, J.; Zhong, F.; Xu, M.; Zhu, J. Metabolic shift of Staphylococcus aureus under sublethal dose of methicillin in the presence of glucose. J. Pharm. Biomed. Anal. 2019, 167, 140–148. [Google Scholar] [CrossRef] [PubMed]
- Hu, C.; Zhang, J.; Hong, S.; Li, H.; Lu, L.; Xie, G.; Luo, W.; Du, Y.; Xie, Z.; Han, X.; et al. Oxidative stress-induced aberrant lipid metabolism is an important causal factor for dysfunction of immunocytes from patients with systemic lupus erythematosus. Free. Radic. Biol. Med. 2021, 163, 210–219. [Google Scholar] [CrossRef]
- Arneth, B.; Arneth, R.; Shams, M. Metabolomics of Type 1 and Type 2 Diabetes. Int. J. Mol. Sci. 2019, 20, 2467. [Google Scholar] [CrossRef]
- Ferrarini, A.; Di Poto, C.; He, S.; Tu, C.; Varghese, R.S.; Kara Balla, A.; Jayatilake, M.; Li, Z.; Ghaffari, K.; Fan, Z.; et al. Metabolomic Analysis of Liver Tissues for Characterization of Hepatocellular Carcinoma. J. Proteome Res. 2019, 18, 3067–3076. [Google Scholar] [CrossRef]
- Guma, M.; Dadpey, B.; Coras, R.; Mikuls, T.R.; Hamilton, B.; Quehenberger, O.; Thorisdottir, H.; Bittleman, D.; Lauro, K.; Reilly, S.M.; et al. Xanthine oxidase inhibitor urate-lowering therapy titration to target decreases serum free fatty acids in gout and suppresses lipolysis by adipocytes. Arthritis Res. Ther. 2022, 24, 175. [Google Scholar] [CrossRef]
- Rizzo, C.; Camarda, F.; Donzella, D.; La Barbera, L.; Guggino, G. Metabolomics: An Emerging Approach to Understand Pathogenesis and to Assess Diagnosis and Response to Treatment in Spondyloarthritis. Cells 2022, 11, 549. [Google Scholar] [CrossRef]
- Fischer, R.; Trudgian, D.C.; Wright, C.; Thomas, G.; Bradbury, L.A.; Brown, M.A.; Bowness, P.; Kessler, B.M. Discovery of candidate serum proteomic and metabolomic biomarkers in ankylosing spondylitis. Mol. Cell Proteomics 2012, 11, M111.013904. [Google Scholar] [CrossRef]
- Gao, P.; Lu, C.; Zhang, F.; Sang, P.; Yang, D.; Li, X.; Kong, H.; Yin, P.; Tian, J.; Lu, X.; et al. Integrated GC-MS and LC-MS plasma metabonomics analysis of ankylosing spondylitis. Analyst 2008, 133, 1214–1220. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Yang, G.J.; Zhang, J.; Chen, C.; Jia, Z.Y.; Li, J.; Xu, W.D. Plasma, urine and ligament tissue metabolite profiling reveals potential biomarkers of ankylosing spondylitis using NMR-based metabolic profiles. Arthritis Res. Ther. 2016, 18, 244. [Google Scholar] [CrossRef]
- Doğan, H.O.; Şenol, O.; Karadağ, A.; Yıldız, S.N. Metabolomic profiling in ankylosing spondylitis using time-of-flight mass spectrometry. Clin. Nutr. ESPEN 2022, 50, 124–132. [Google Scholar] [CrossRef]
- Berlinberg, A.J.; Regner, E.H.; Stahly, A.; Brar, A.; Reisz, J.A.; Gerich, M.E.; Fennimore, B.P.; Scott, F.I.; Freeman, A.E.; Kuhn, K.A. Multi ‘Omics Analysis of Intestinal Tissue in Ankylosing Spondylitis Identifies Alterations in the Tryptophan Metabolism Pathway. Front. Immunol. 2021, 12, 587119. [Google Scholar] [CrossRef] [PubMed]
- Sundstrom, B.; Johansson, G.; Kokkonen, H.; Cederholm, T.; Wallberg-Jonsson, S. Plasma phospholipid fatty acid content is related to disease activity in ankylosing spondylitis. J. Rheumatol. 2012, 39, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Eryavuz Onmaz, D.; Sivrikaya, A.; Isik, K.; Abusoglu, S.; Albayrak Gezer, I.; Humeyra Yerlikaya, F.; Abusoglu, G.; Unlu, A.; Tezcan, D. Altered kynurenine pathway metabolism in patients with ankylosing spondylitis. Int. Immunopharmacol. 2021, 99, 108018. [Google Scholar] [CrossRef] [PubMed]
- Chong, J.; Soufan, O.; Li, C.; Caraus, I.; Li, S.; Bourque, G.; Wishart, D.S.; Xia, J. MetaboAnalyst 4.0: Towards more transparent and integrative metabolomics analysis. Nucleic Acids Res. 2018, 46, W486–W494. [Google Scholar] [CrossRef]
- Mauro, D.; Thomas, R.; Guggino, G.; Lories, R.; Brown, M.A.; Ciccia, F. Ankylosing spondylitis: An autoimmune or autoinflammatory disease? Nat. Rev. Rheumatol. 2021, 17, 387–404. [Google Scholar] [CrossRef]
- Chen, R.; Han, S.; Dong, D.M.; Wang, Y.S.; Liu, Q.P.; Xie, W.; Li, M.; Yao, M. Serum fatty acid profiles and potential biomarkers of ankylosing spondylitis determined by gas chromatography-mass spectrometry and multivariate statistical analysis. Biomed. Chromatogr. 2015, 29, 604–611. [Google Scholar] [CrossRef]
- Wagner, C.; Visvanathan, S.; Braun, J.; van der Heijde, D.; Deodhar, A.; Hsu, B.; Mack, M.; Elashoff, M.; Inman, R.D. Serum markers associated with clinical improvement in patients with ankylosing spondylitis treated with golimumab. Ann. Rheum. Dis. 2012, 71, 674–680. [Google Scholar] [CrossRef] [PubMed]
- Boden, G.; She, P.; Mozzoli, M.; Cheung, P.; Gumireddy, K.; Reddy, P.; Xiang, X.; Luo, Z.; Ruderman, N. Free fatty acids produce insulin resistance and activate the proinflammatory nuclear factor-kappaB pathway in rat liver. Diabetes 2005, 54, 3458–3465. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, M.T.; Yudell, B.E.; Loor, J.J. Regulation of energy metabolism by long-chain fatty acids. Prog. Lipid Res. 2014, 53, 124–144. [Google Scholar] [CrossRef] [PubMed]
- He, Q.; Chen, Y.; Wang, Z.; He, H.; Yu, P. Cellular Uptake, Metabolism and Sensing of Long-Chain Fatty Acids. Front. Biosci. Landmark 2023, 28, 10. [Google Scholar] [CrossRef] [PubMed]
- Mulukutla, B.C.; Yongky, A.; Le, T.; Mashek, D.G.; Hu, W.S. Regulation of Glucose Metabolism—A Perspective From Cell Bioprocessing. Trends Biotechnol. 2016, 34, 638–651. [Google Scholar] [CrossRef]
- Possik, E.; Al-Mass, A.; Peyot, M.L.; Ahmad, R.; Al-Mulla, F.; Madiraju, S.R.M.; Prentki, M. New Mammalian Glycerol-3-Phosphate Phosphatase: Role in beta-Cell, Liver and Adipocyte Metabolism. Front. Endocrinol. 2021, 12, 706607. [Google Scholar] [CrossRef]
- Sousa, A.P.; Cunha, D.M.; Franco, C.; Teixeira, C.; Gojon, F.; Baylina, P.; Fernandes, R. Which Role Plays 2-Hydroxybutyric Acid on Insulin Resistance? Metabolites 2021, 11, 835. [Google Scholar] [CrossRef]
- Nie, C.; He, T.; Zhang, W.; Zhang, G.; Ma, X. Branched Chain Amino Acids: Beyond Nutrition Metabolism. Int. J. Mol. Sci. 2018, 19, 954. [Google Scholar] [CrossRef]
- Dimou, A.; Tsimihodimos, V.; Bairaktari, E. The Critical Role of the Branched Chain Amino Acids (BCAAs) Catabolism-Regulating Enzymes, Branched-Chain Aminotransferase (BCAT) and Branched-Chain alpha-Keto Acid Dehydrogenase (BCKD), in Human Pathophysiology. Int. J. Mol. Sci. 2022, 23, 4022. [Google Scholar] [CrossRef]
- Mattick, J.S.A.; Kamisoglu, K.; Ierapetritou, M.G.; Androulakis, I.P.; Berthiaume, F. Branched-chain amino acid supplementation: Impact on signaling and relevance to critical illness. Wiley Interdiscip. Rev. Syst. Biol. Med. 2013, 5, 449–460. [Google Scholar] [CrossRef]
- Mero, A. Leucine supplementation and intensive training. Sports Med. 1999, 27, 347–358. [Google Scholar] [CrossRef] [PubMed]
- Liang, T.; Chen, J.; Xu, G.; Zhang, Z.; Xue, J.; Zeng, H.; Jiang, J.; Chen, T.; Qin, Z.; Li, H.; et al. Platelet-to-Lymphocyte Ratio as an Independent Factor Was Associated With the Severity of Ankylosing Spondylitis. Front. Immunol. 2021, 12, 760214. [Google Scholar] [CrossRef] [PubMed]
- Miyajima, M. Amino acids: Key sources for immunometabolites and immunotransmitters. Int. Immunol. 2020, 32, 435–446. [Google Scholar] [CrossRef] [PubMed]
- Pakula, M.M.; Maier, T.J.; Vorup-Jensen, T. Insight on the impacts of free amino acids and their metabolites on the immune system from a perspective of inborn errors of amino acid metabolism. Expert. Opin. Ther. Targets 2017, 21, 611–626. [Google Scholar] [CrossRef] [PubMed]
- Li, P.; Yin, Y.L.; Li, D.; Kim, S.W.; Wu, G. Amino acids and immune function. Br. J. Nutr. 2007, 98, 237–252. [Google Scholar] [CrossRef]
- Grohmann, U.; Bronte, V. Control of immune response by amino acid metabolism. Immunol. Rev. 2010, 236, 243–264. [Google Scholar] [CrossRef]
- Stone, T.W.; Williams, R.O. Modulation of T cells by tryptophan metabolites in the kynurenine pathway. Trends Pharmacol. Sci. 2023, 44, 442–456. [Google Scholar] [CrossRef]
- Zhang, H.; Chen, Y.; Li, Y.; Zhang, T.; Ying, Z.; Su, W.; Zhang, L.; Wang, T. l-Threonine improves intestinal mucin synthesis and immune function of intrauterine growth-retarded weanling piglets. Nutrition 2019, 59, 182–187. [Google Scholar] [CrossRef]
- Ye, G.; Xie, Z.; Zeng, H.; Wang, P.; Li, J.; Zheng, G.; Wang, S.; Cao, Q.; Li, M.; Liu, W.; et al. Oxidative stress-mediated mitochondrial dysfunction facilitates mesenchymal stem cell senescence in ankylosing spondylitis. Cell Death Dis. 2020, 11, 775. [Google Scholar] [CrossRef]
- Kiranatlioglu-Firat, F.; Demir, H.; Cuce, I.; Altin-Celik, P.; Eciroglu, H.; Bayram, F.; Donmez-Altuntas, H. Increased oxidative and chromosomal DNA damage in patients with ankylosing spondylitis: Its role in pathogenesis. Clin. Exp. Med. 2022, 23, 1721–1728. [Google Scholar] [CrossRef]
- Asantewaa, G.; Harris, I.S. Glutathione and its precursors in cancer. Curr. Opin. Biotechnol. 2021, 68, 292–299. [Google Scholar] [CrossRef] [PubMed]
- Petry, E.R.; Cruzat, V.F.; Heck, T.G.; Leite, J.S.; Homem de Bittencourt, P.I., Jr.; Tirapegui, J. Alanyl-glutamine and glutamine plus alanine supplements improve skeletal redox status in trained rats: Involvement of heat shock protein pathways. Life Sci. 2014, 94, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Pham, C.T. Neutrophil serine proteases: Specific regulators of inflammation. Nat. Rev. Immunol. 2006, 6, 541–550. [Google Scholar] [CrossRef] [PubMed]
- Wiedow, O.; Meyer-Hoffert, U. Neutrophil serine proteases: Potential key regulators of cell signalling during inflammation. J. Intern. Med. 2005, 257, 319–328. [Google Scholar] [CrossRef]
- Emmett, M. Acetaminophen toxicity and 5-oxoproline (pyroglutamic acid): A tale of two cycles, one an ATP-depleting futile cycle and the other a useful cycle. Clin. J. Am. Soc. Nephrol. 2014, 9, 191–200. [Google Scholar] [CrossRef]
- Liu, Y.; Hyde, A.S.; Simpson, M.A.; Barycki, J.J. Emerging regulatory paradigms in glutathione metabolism. Adv. Cancer Res. 2014, 122, 69–101. [Google Scholar] [CrossRef]
| Characteristics | Control (n = 40) | AS (n = 57) | p |
|---|---|---|---|
| Male/Female, | 20/20 | 28/29 | 0.932 |
| Age, y | 36.08 ± 1.53 | 39.37 ± 1.61 | 0.158 |
| BMI | 22.22 ± 0.46 | 22.68±0.53 | 0.534 |
| CRP (mg/L) | 1.90 ± 0.38 | 4.18 ± 0.85 | 0.036 |
| ESR (mm/h) | 9.32 ± 0.67 | 15.02 ± 2.08 | 0.032 |
| WBC (109/L) | 5.90 ± 0.19 | 6.66 ± 0.20 | 0.010 |
| HLA–B27 (+/−) | 2/38 | 45/12 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guo, Y.; Wei, S.; Yin, M.; Cao, D.; Li, Y.; Wen, C.; Zhou, J. Gas Chromatography–Mass Spectrometry Reveals Stage-Specific Metabolic Signatures of Ankylosing Spondylitis. Metabolites 2023, 13, 1058. https://doi.org/10.3390/metabo13101058
Guo Y, Wei S, Yin M, Cao D, Li Y, Wen C, Zhou J. Gas Chromatography–Mass Spectrometry Reveals Stage-Specific Metabolic Signatures of Ankylosing Spondylitis. Metabolites. 2023; 13(10):1058. https://doi.org/10.3390/metabo13101058
Chicago/Turabian StyleGuo, Yixuan, Shuangshuang Wei, Mengdi Yin, Dandan Cao, Yiling Li, Chengping Wen, and Jia Zhou. 2023. "Gas Chromatography–Mass Spectrometry Reveals Stage-Specific Metabolic Signatures of Ankylosing Spondylitis" Metabolites 13, no. 10: 1058. https://doi.org/10.3390/metabo13101058
APA StyleGuo, Y., Wei, S., Yin, M., Cao, D., Li, Y., Wen, C., & Zhou, J. (2023). Gas Chromatography–Mass Spectrometry Reveals Stage-Specific Metabolic Signatures of Ankylosing Spondylitis. Metabolites, 13(10), 1058. https://doi.org/10.3390/metabo13101058







