Curcumin and Vitamin C Attenuate Gentamicin-Induced Nephrotoxicity by Modulating Distinctive Reactive Species
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Experimental Protocol
2.3. Renal Function Evaluation
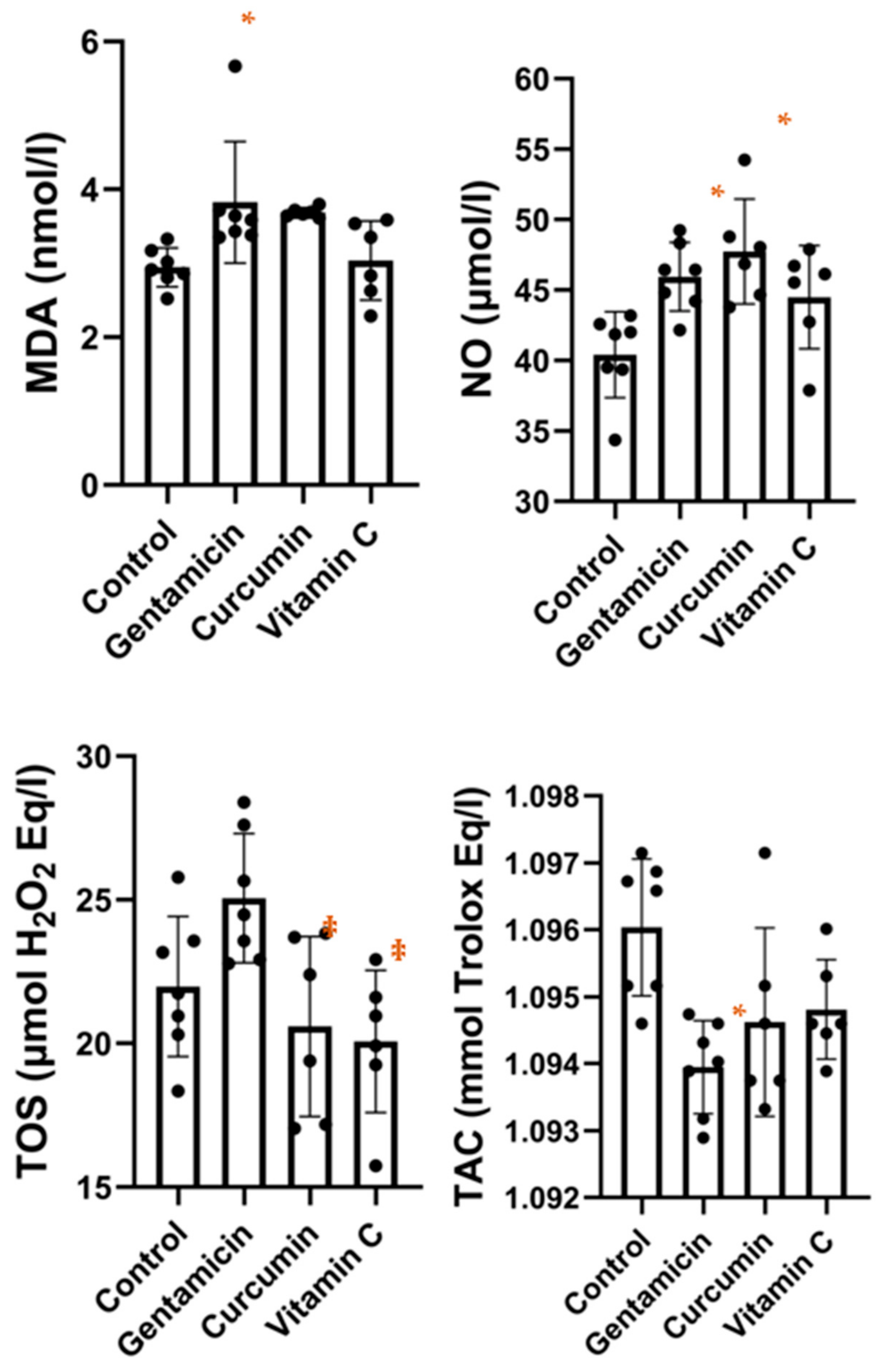
2.4. Oxidative Stress Analysis
2.5. Antioxidant and Anti-Inflammatory Analysis
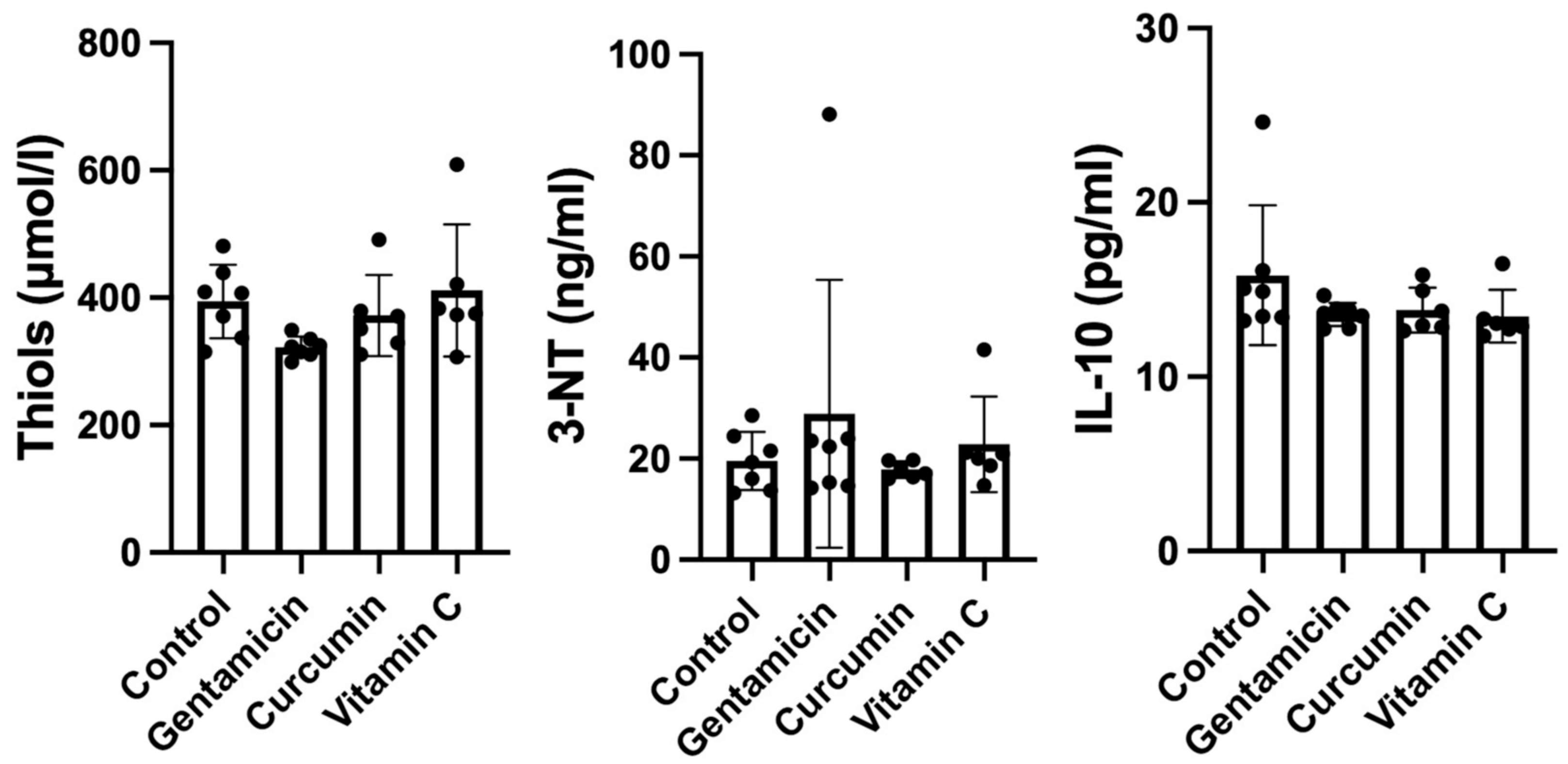
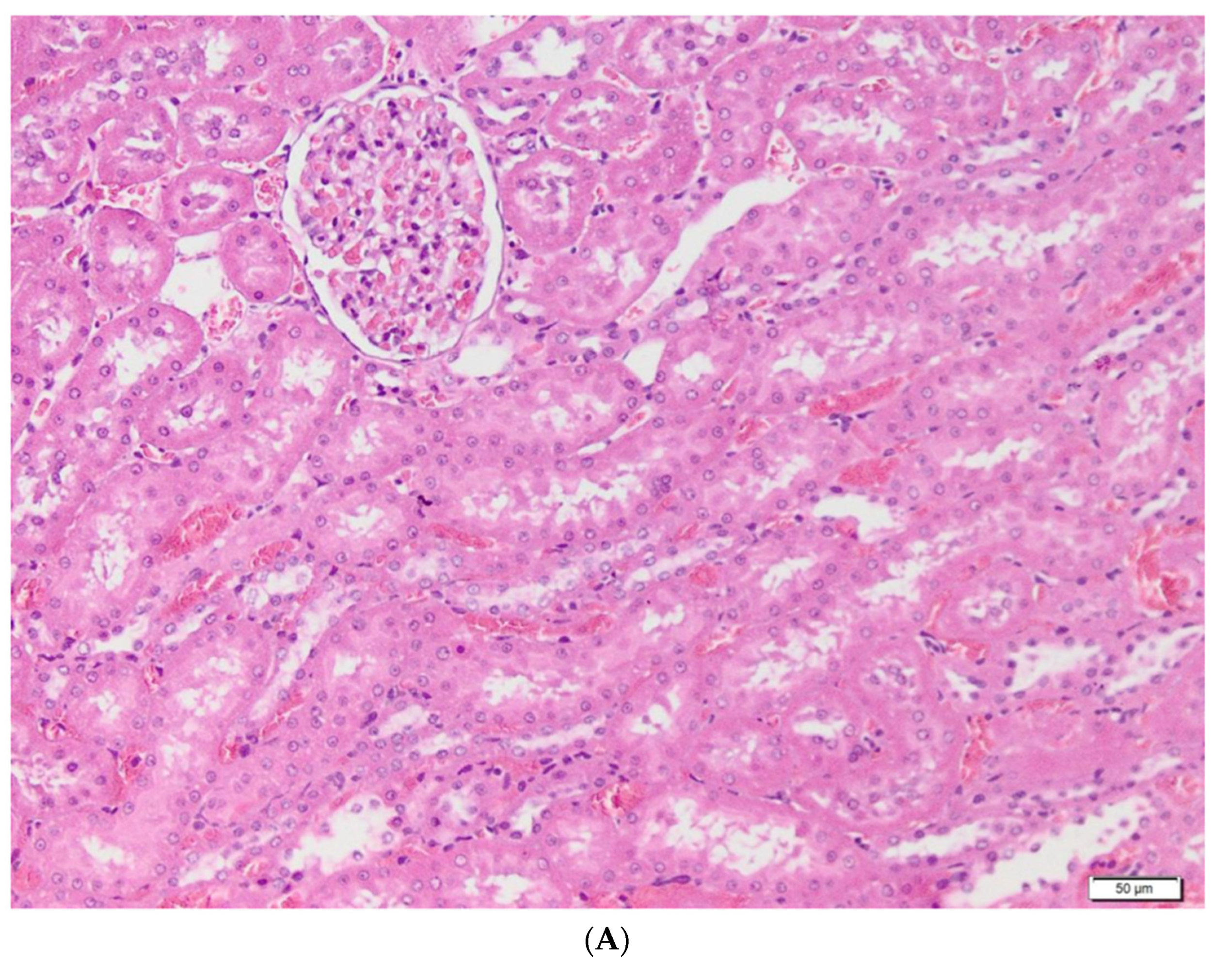
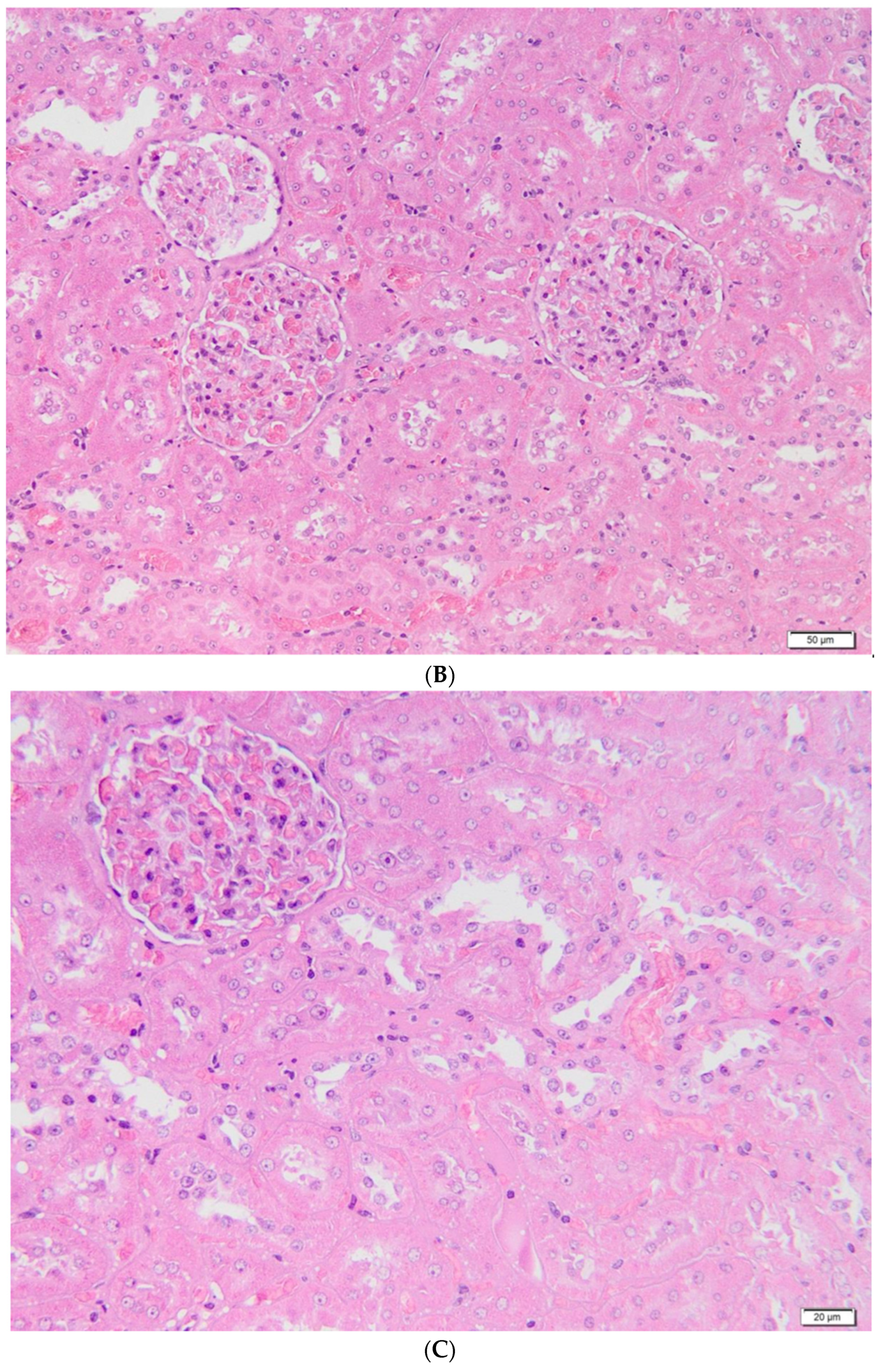
2.6. Histological Analysis
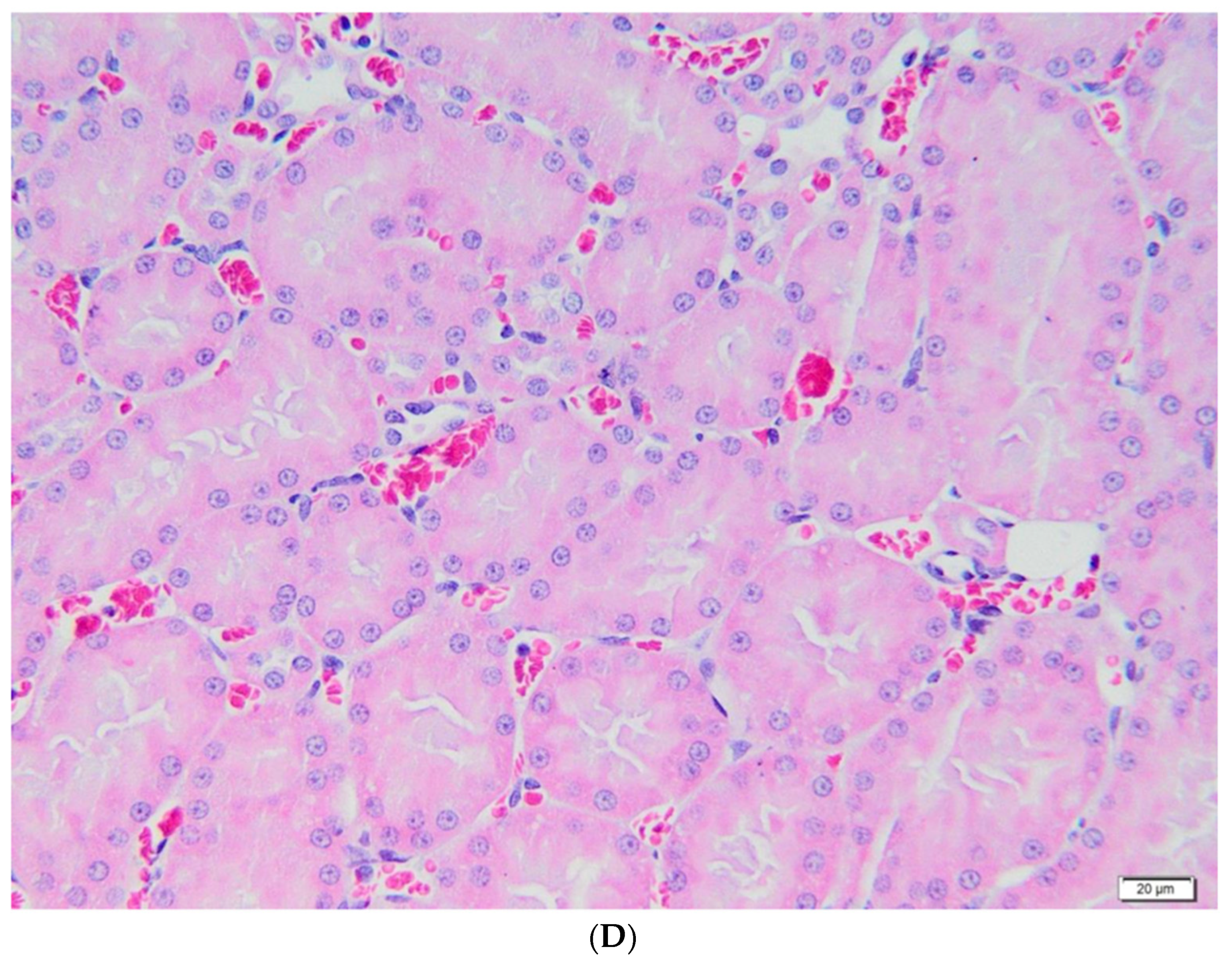
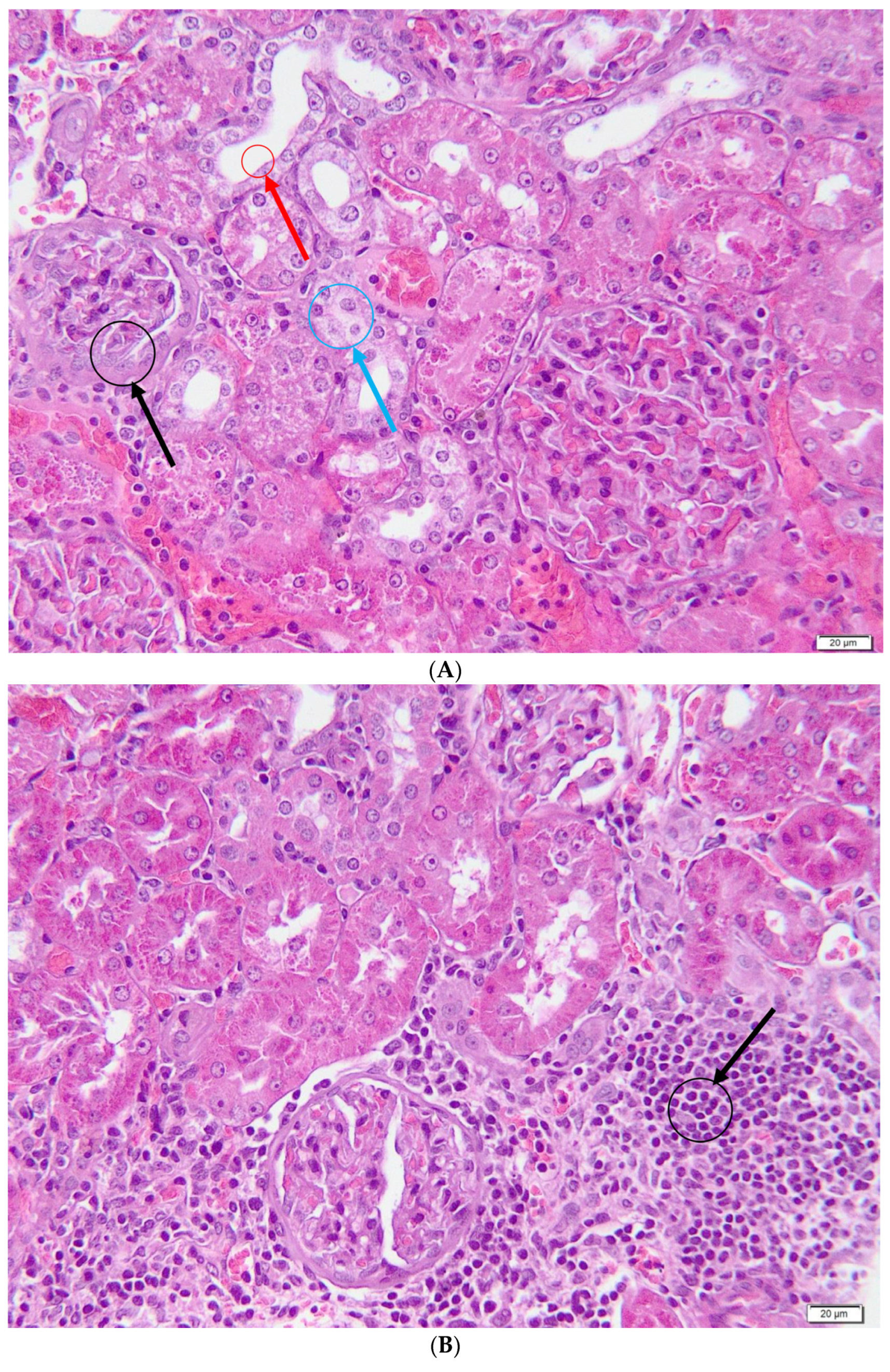
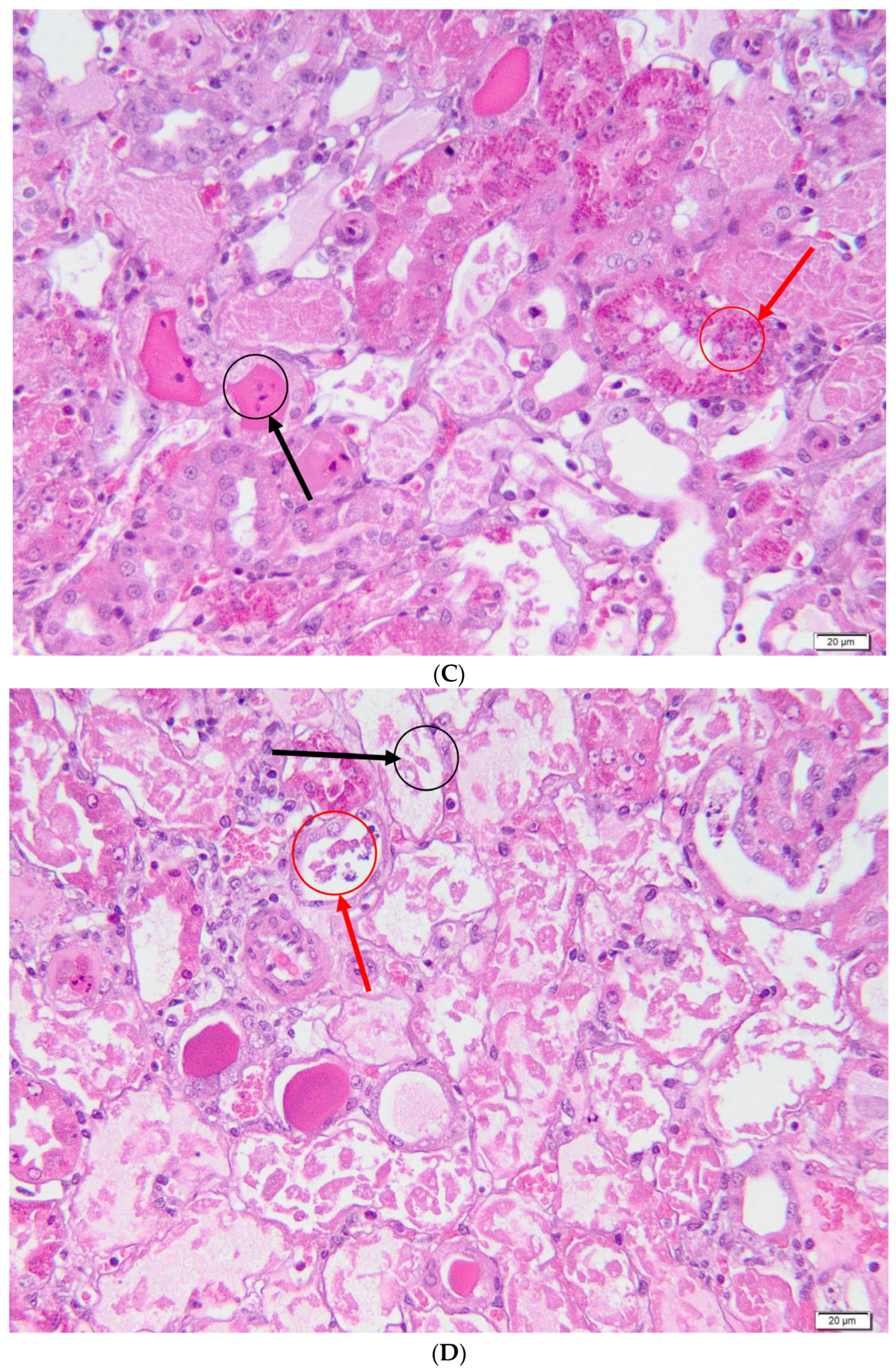
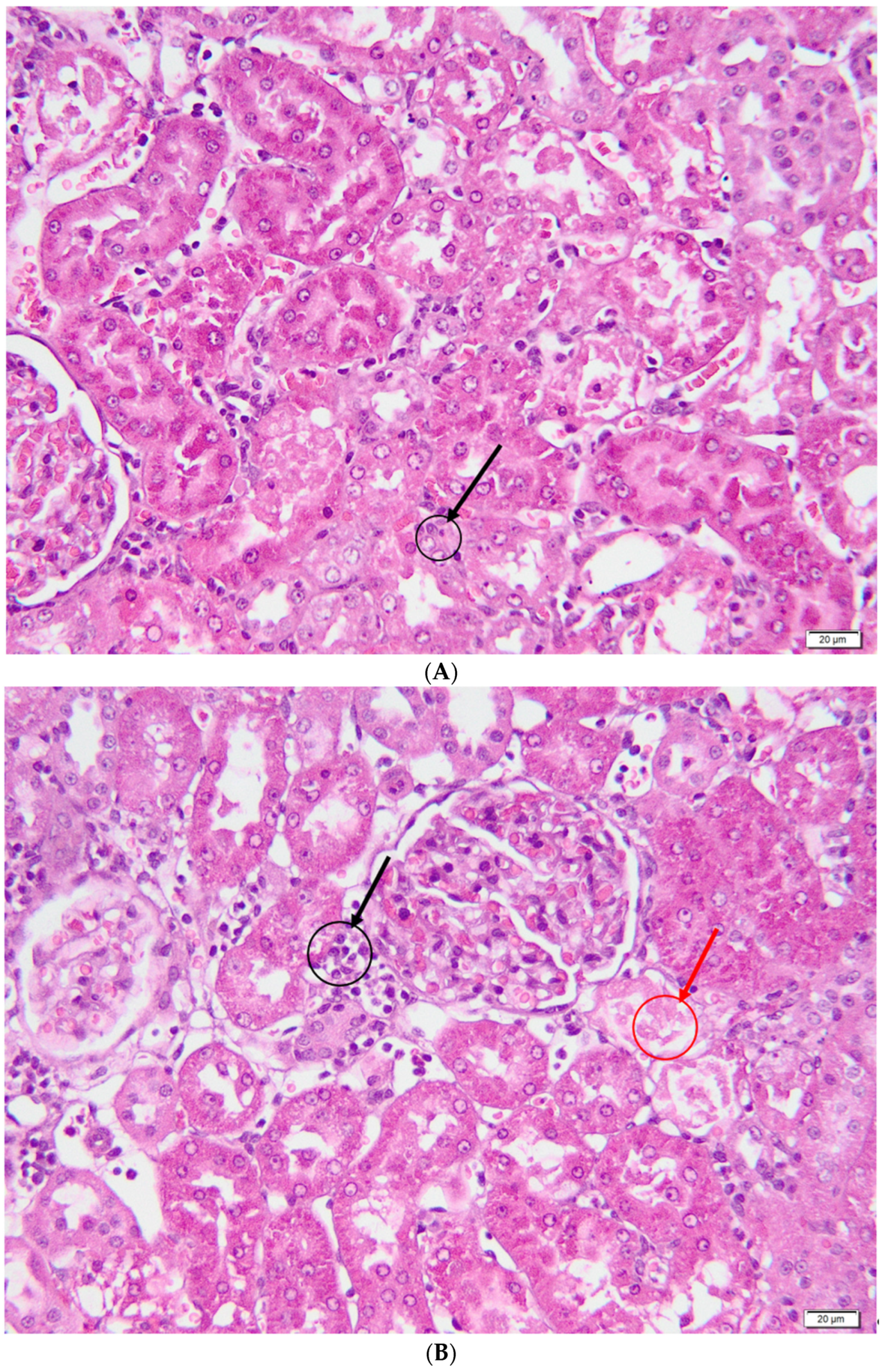
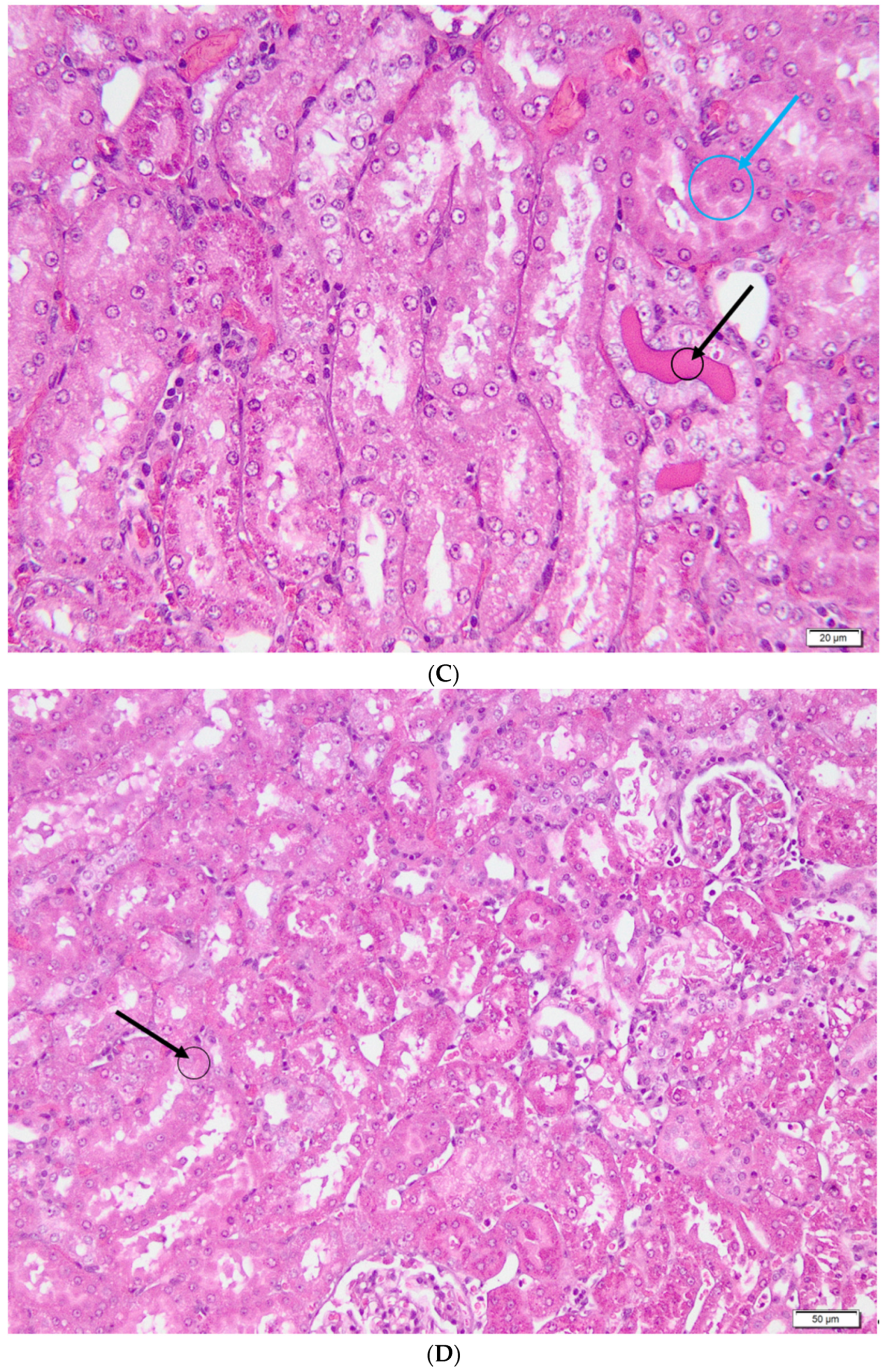
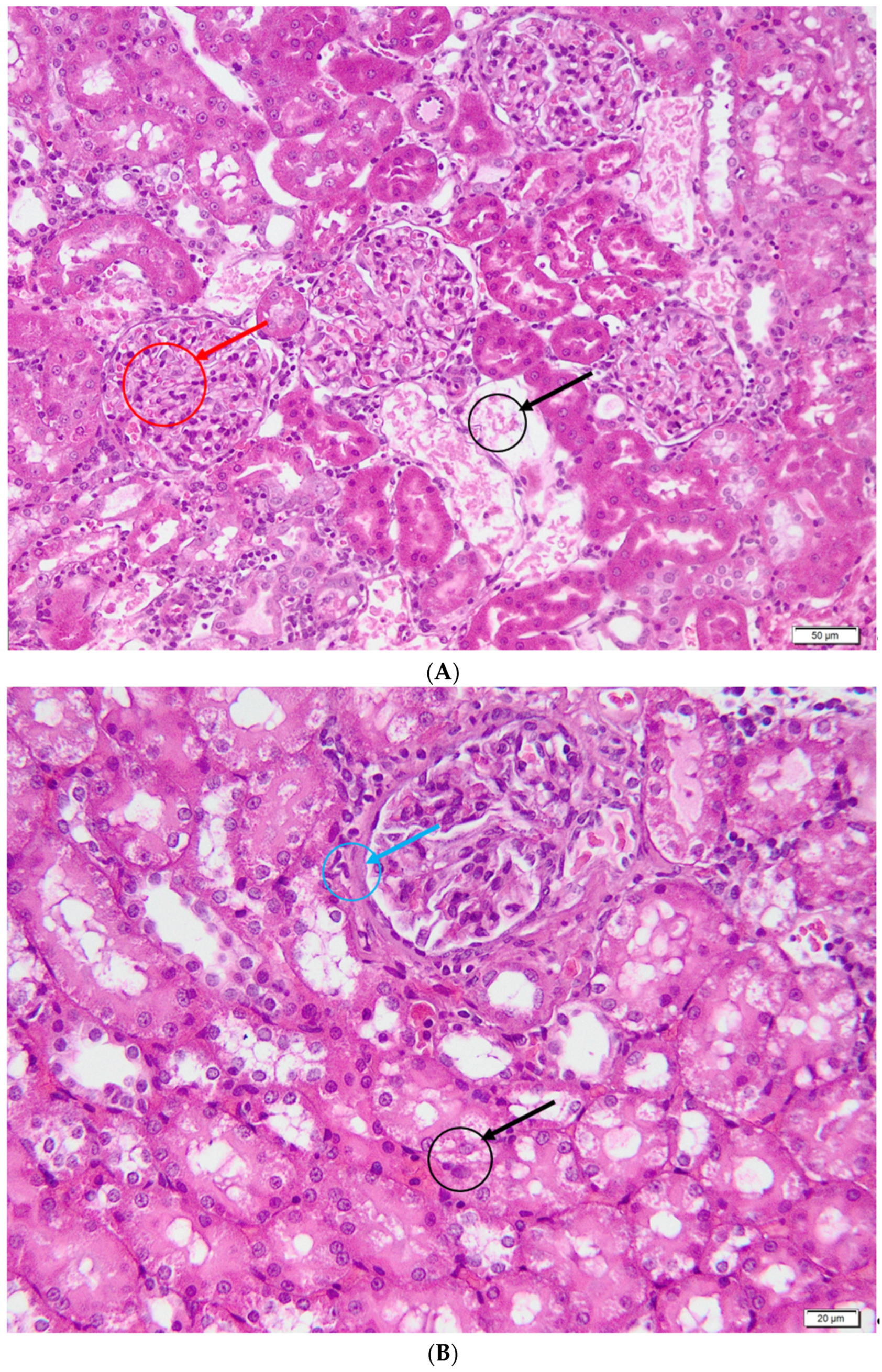
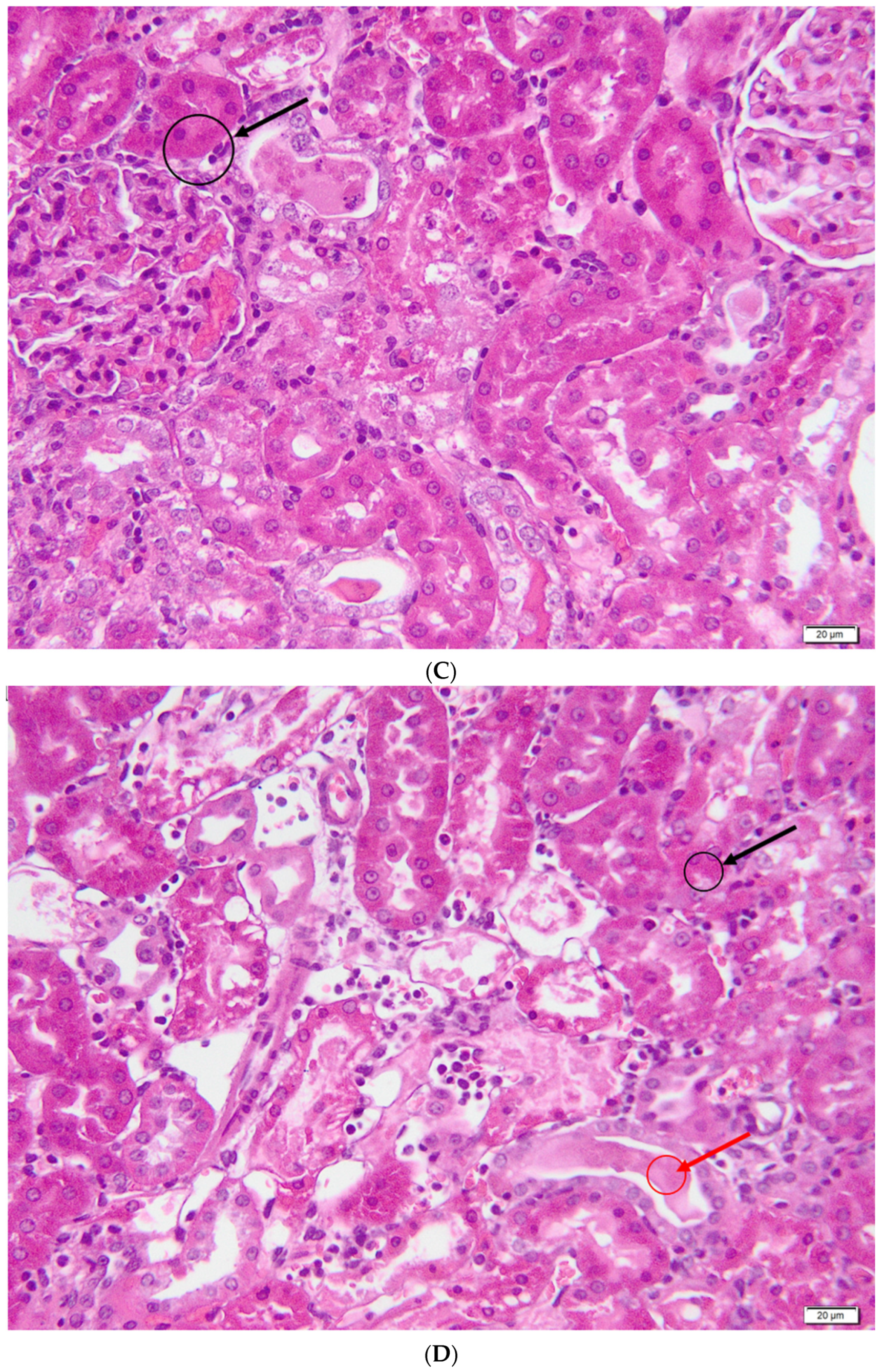
- Overall damage to the parenchyma—0: unaffected parenchyma; 1: ≤10% of the affected parenchyma; 2: 11–25% of the affected parenchyma; 3: 26–45% of the affected parenchyma; 4: 46–75% of the affected parenchyma; 5: >75% of the affected parenchyma;
- Glomerular lesions—0: absence of lesions; 1: ≤10% glomeruli with non-specific lesions; 2: 11–25% glomeruli with non-specific lesions; 3: 26–45% glomeruli with non-specific lesions; 4: 46–75% glomeruli with non-specific lesions; 5: >75% glomeruli with non-specific lesions;
- Acute tubular necrosis—0: absent tubular necrosis; 1: ≤10% of the affected tubes; 2: 11–25% of the affected tubes; 3: 26–45% of the affected tubes; 4: 46–75% of the affected tubes; 5: >75% of the affected tubes;
- Tubulo-intestinal inflammatory infiltrate—0: lack of inflammatory infiltrate; 1: discrete inflammatory infiltrate at the interstitial level; 2: severe inflammatory infiltrate both at the interstitium and at the tubular level.
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- National Institute of Diabetes and Digestive and Kidney Diseases. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]; Gentamicin. [Updated 2019 Apr 12]; National Institute of Diabetes and Digestive and Kidney Diseases: Bethesda, MD, USA, 2012. Available online: https://www.ncbi.nlm.nih.gov/books/NBK548706/ (accessed on 7 January 2022).
- Srisung, W.; Teerakanok, J.; Tantrachoti, P.; Karukote, A.; Nugent, K. Surgical prophylaxis with gentamicin and acute kidney injury: A systematic review and meta-analysis. Ann. Transl. Med. 2017, 5, 100. [Google Scholar] [CrossRef] [PubMed]
- Balakumar, P.; Rohilla, A.; Thangathirupathi, A. Gentamicin-induced nephrotoxicity: Do we have a promising therapeutic approach to blunt it? Pharmacol. Res. 2010, 62, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Tomsa, A.M.; Alexa, A.L.; Junie, M.L.; Rachisan, A.L.; Ciumarnean, L. Oxidative stress as a potential target in acute kidney injury. PeerJ 2019, 7, e8046. [Google Scholar] [CrossRef] [PubMed]
- Tomşa, A.M.; Picoş, A.; Picoş, A.M.; Răchişan, A.L. Mitochondrial nanotargeting in malignancies (Review). Exp. Ther. Med. 2020, 20, 3444–3451. [Google Scholar] [CrossRef] [PubMed]
- Zorov, D.B. Amelioration of aminoglycoside nephrotoxicity requires protection of renal mitochondria. Kidney Int. 2010, 77, 841–843. [Google Scholar] [CrossRef]
- Randjelovic, P.; Veljkovic, S.; Stojiljkovic, N.; Sokolovic, D.; Ilic, I. Gentamicin nephrotoxicity in animals: Current knowledge and future perspectives. EXCLI J. 2017, 16, 388–399. [Google Scholar] [CrossRef]
- Arulselvan, P.; Fard, M.T.; Tan, W.S.; Gothai, S.; Fakurazi, S.; Norhaizan, M.E.; Kumar, S.S. Role of Antioxidants and Natural Products in Inflammation. Oxid. Med. Cell. Longev. 2016, 2016, 5276130. [Google Scholar] [CrossRef]
- Pfingstgraf, I.O.; Taulescu, M.; Pop, R.M.; Orăsan, R.; Vlase, L.; Uifalean, A.; Todea, D.; Alexescu, T.; Toma, C.; Pârvu, A.E. Protective Effects of Taraxacum officinale L. (Dandelion) Root Extract in Experimental Acute on Chronic Liver Failure. Antioxidants 2021, 10, 504. [Google Scholar] [CrossRef]
- Hassanzadeh, K.; Buccarello, L.; Dragotto, J.; Mohammadi, A.; Corbo, M.; Feligioni, M. Obstacles against the Marketing of Curcumin as a Drug. Int. J. Mol. Sci. 2020, 21, 6619. [Google Scholar] [CrossRef]
- Trujillo, J.; Chirino, Y.I.; Molina-Jijón, E.; Andérica-Romero, A.C.; Tapia, E.; Pedraza-Chaverrí, J. Renoprotective effect of the antioxidant curcumin: Recent findings. Redox Biol. 2013, 1, 448–456. [Google Scholar] [CrossRef]
- Sandur, S.K.; Pandey, M.K.; Sung, B.; Ahn, K.S.; Murakami, A.; Sethi, G.; Limtrakul, P.; Badmaev, V.; Aggarwal, B.B. Curcumin, demethoxycurcumin, bisdemethoxycurcumin, tetrahydrocurcumin and turmerones differentially regulate anti-inflammatory and anti-proliferative responses through a ROS-independent mechanism. Carcinogenesis 2007, 28, 1765–1773. [Google Scholar] [CrossRef] [PubMed]
- Carr, A.C.; Maggini, S. Vitamin C and Immune Function. Nutrients 2017, 9, 1211. [Google Scholar] [CrossRef] [PubMed]
- Abraham, P. Vitamin C may be beneficial in the prevention of paracetamol-induced renal damage. Clin. Exp. Nephrol. 2005, 9, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Fischer, H.; Schwarzer, C.; Illek, B. Vitamin C controls the cystic fibrosis transmembrane conductance regulator chloride channel. Proc. Natl. Acad. Sci. USA 2004, 101, 3691–3696. [Google Scholar] [CrossRef] [PubMed]
- Cárcamo, J.M.; Pedraza, A.; Bórquez-Ojeda, O.; Zhang, B.; Sanchez, R.; Golde, D.W. Vitamin C is a kinase inhibitor: Dehydroascorbic acid inhibits IkappaBalpha kinase beta. Mol. Cell Biol. 2004, 24, 6645–6652. [Google Scholar] [CrossRef]
- Hemilä, H.; Chalker, E. Vitamin C for preventing and treating the common cold. Cochrane Database Syst. Rev. 2013, 2013, CD000980. [Google Scholar] [CrossRef]
- Kuhn, S.O.; Meissner, K.; Mayes, L.M.; Bartels, K. Vitamin C in sepsis. Curr. Opin. Anaesthesiol. 2018, 31, 55–60. [Google Scholar] [CrossRef]
- Ngo, B.; Van Riper, J.M.; Cantley, L.C.; Yun, J. Targeting cancer vulnerabilities with high-dose vitamin C. Nat. Rev. Cancer 2019, 19, 271–282. [Google Scholar] [CrossRef]
- Mitev, D.; Gradeva, H.; Stoyanova, Z.; Petrova, N.; Karova, N.; Dimov, D.; Iliev, V.; Koychev, A.; Prakova, G.; Vlaykova, T. Evaluation of thiol compounds and lipid peroxidative products in plasma of patients with COPD. Trakia J. Sci. 2010, 8, 306–314. [Google Scholar]
- Miranda, M.K.; Espey, G.M.; Wink, A.D. A rapid, Simple Spectrophotometric Method for Simultaneous Detection of Nitrate and Nitrite. Nitric. Oxide. Biol. Chem. 2001, 5, 62–71. [Google Scholar] [CrossRef]
- Erel, O. A new automated colorimetric method for measuring total oxidant status. Clin. Biochem. 2005, 38, 1103–1111. [Google Scholar] [CrossRef] [PubMed]
- Hu, M.L. Measurement of protein thiol groups and glutathione in plasma. In Methods in Enzymology; Academic Press, Inc.: Cambridge, MA, USA, 1994; Volume 233, pp. 380–384. [Google Scholar]
- Erel, O. A novel automated direct measurement method for total antioxidant capacity using a new generation, more stable ABTS radical cation. Clin. Biochem. 2004, 37, 277–285. [Google Scholar] [CrossRef] [PubMed]
- Al-Shabanah, O.A.; Aleisa, A.M.; Al-Yahya, A.A.; Al-Rejaie, S.S.; Bakheet, S.A.; Fatani, A.G.; Sayed-Ahmed, M.M. Increased urinary losses of carnitine and decreased intramitochondrial coenzyme A in gentamicin-induced acute renal failure in rats. Nephrol. Dial. Transpl. 2010, 25, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Melnikov, V.Y.; Faubel, S.; Siegmund, B.; Lucia, M.S.; Ljubanovic, D.; Edelstein, C.L. Neutrophil-independent mechanisms of caspase-1–and IL-18–mediated ischemic acute tubular necrosis in mice. J. Clin. Investig. 2002, 110, 1083–1091. [Google Scholar] [CrossRef] [PubMed]
- Hayward, R.S.; Harding, J.; Molloy, R.; Land, L.; Longcroft-Neal, K.; Moore, D.; Ross, J.D. Adverse effects of a single dose of gentamicin in adults: A systematic review. Br. J. Clin. Pharmacol. 2018, 84, 223–238. [Google Scholar] [CrossRef] [PubMed]
- Smit, C.; van Schip, A.M.; van Dongen, E.P.A.; Brüggemann, R.J.M.; Becker, M.L.; Knibbe, C.A.J. Dose recommendations for gentamicin in the real-world obese population with varying body weight and renal (dys)function. J. Antimicrob. Chemother. 2020, 75, 3286–3292. [Google Scholar] [CrossRef]
- Lee, M.C.; Cheng, K.J.; Chen, S.M.; Li, Y.C.; Imai, K.; Lee, C.M.; Lee, J.A. A novel preventive mechanism of gentamicin-induced nephrotoxicity by atorvastatin. Biomed. Chromatogr. 2019, 33, e4639. [Google Scholar] [CrossRef]
- Elfaky, M.A.; Thabit, A.K.; Sirwi, A.; Fahmy, U.A.; Bahabri, R.M.; Al-Awad, E.A.; Basaeed, L.F. Development of a Novel Pharmaceutical Formula of Nanoparticle Lipid Carriers of Gentamicin/α-Tocopherol and In Vivo Assessment of the Antioxidant Protective Effect of α-Tocopherol in Gentamicin-Induced Nephrotoxicity. Antibiotics 2019, 8, 234. [Google Scholar] [CrossRef]
- Mahmoud, Y.I. Kiwi fruit (Actinidia deliciosa) ameliorates gentamicin-induced nephrotoxicity in albino mice via the activation of Nrf2 and the inhibition of NF-κB (Kiwi & gentamicin-induced nephrotoxicity). Biomed. Pharmacother. 2017, 94, 206–218. [Google Scholar] [CrossRef]
- Negrette-Guzmán, M.; García-Niño, W.R.; Tapia, E.; Zazueta, C.; Huerta-Yepez, S.; León-Contreras, J.C.; Hernández-Pando, R.; Aparicio-Trejo, O.E.; Madero, M.; Pedraza-Chaverri, J. Curcumin Attenuates Gentamicin-Induced Kidney Mitochondrial Alterations: Possible Role of a Mitochondrial Biogenesis Mechanism. Evid. Based Complement Alternat. Med. 2015, 2015, 917435. [Google Scholar] [CrossRef]
- Luft, F.C. Biomarkers and predicting acute kidney injury. Acta Physiol. 2021, 231, e13479. [Google Scholar] [CrossRef] [PubMed]
- Askenazi, D.J.; Ambalavanan, N.; Goldstein, S.L. Acute kidney injury in critically ill newborns: What do we know? What do we need to learn? Pediatr. Nephrol. 2009, 24, 265–274. [Google Scholar] [CrossRef] [PubMed]
- Schmid, M.; Dalela, D.; Tahbaz, R.; Langetepe, J.; Randazzo, M.; Dahlem, R.; Fisch, M.; Trinh, Q.D.; Chun, F.K. Novel biomarkers of acute kidney injury: Evaluation and evidence in urologic surgery. World J. Nephrol. 2015, 4, 160–168. [Google Scholar] [CrossRef] [PubMed]
- Tomşa, A.M.; Răchişan, A.L.; Pandrea, S.L.; Benea, A.; Uifălean, A.; Parvu, A.E.; Junie, L.M. Accelerated lipid peroxidation in a rat model of gentamicin nephrotoxicity. Exp. Ther. Med. 2021, 22, 1218. [Google Scholar] [CrossRef] [PubMed]
- Al-Kuraishy, H.M.; Al-Gareeb, A.I.; Al-Nami, M.S. Irbesartan Attenuates Gentamicin-induced Ne-phrotoxicity in Rats through Modulation of Oxidative Stress and Endogenous Antioxidant Capacity. Int. J. Prev. Med. 2020, 11, 16. [Google Scholar] [CrossRef]
- Raeeszadeh, M.; Rezaee, M.; Akbari, A.; Khademi, N. The comparison of the effect of Origanum vulgare L. extract and vitamin C on the gentamycin-induced nephrotoxicity in rats. Drug Chem. Toxicol. 2021, 45, 1–8. [Google Scholar] [CrossRef]
- El-Zawahry, B.H.; Abu El Kheir, E.M. The protective effect of curcumin against gentamicin-induced renal dysfunction and oxidative stress in male Albino rats. Egyptian J. Hosp. Med. 2007, 29, 546–556. [Google Scholar] [CrossRef]
- Mantzarlis, K.; Tsolaki, V.; Zakynthinos, E. Role of Oxidative Stress and Mitochondrial Dysfunction in Sepsis and Potential Therapies. Oxid. Med. Cell. Longev. 2017, 2017, 5985209. [Google Scholar] [CrossRef]
- Laorodphun, P.; Cherngwelling, R.; Panya, A.; Arjinajarn, P. Curcumin protects rats against gentamicin-induced nephrotoxicity by amelioration of oxidative stress, endoplasmic reticulum stress and apoptosis. Pharm. Biol. 2022, 60, 491–500. [Google Scholar] [CrossRef]
- Yarijani, Z.M.; Najafi, H.; Shackebaei, D.; Madani, S.H.; Modarresi, M.; Jassemi, S.V. Amelioration of renal and hepatic function, oxidative stress, inflammation and histo-pathologic damages by Malva sylvestris extract in Gentamicin induced renaltoxicity. Biomed. Pharm. 2019, 112, 108635. [Google Scholar] [CrossRef]
- Atteya, M.; Ahmed, A.M.; AlRabiah, A.; Al-Matrafi, T.A.; Arafah, M.M.; Al-Saggaf, S.; Shereef, S.H.; Ahmed, A.A.; Alqahtani, H.M.; Mohammad, R.A.T. Thymoquinone and Curcumin modify inducible nitric oxide synthase, caspase 3, and thioredoxin immuno-histochemical expression in acetaminophen hepatotoxicity. Folia Morphol. 2019, 78, 773–788. [Google Scholar] [CrossRef] [PubMed]
- Qian, J.; You, H.; Zhu, Q.; Ma, S.; Zhou, Y.; Zheng, Y.; Liu, J.; Kuang, D.; Gu, Y.; Hao, C.; et al. Nitrotyrosine level was associated with mortality in patients with acute kidney injury. PLoS ONE 2013, 8, e79962. [Google Scholar] [CrossRef]
- Gheith, I.; El-Mahmoudy, A. Novel and classical renal biomarkers as evidence for the nephroprotective effect of Carica papaya leaf extract. Biosci. Rep. 2018, 38, BSR20181187. [Google Scholar] [CrossRef] [PubMed]
- Hussain, T.; Gupta, R.K.; Sweet, K.; Eswaran, B.; Vijayakumar, M.; Chandana, V.R. Nephroprotective activity of Solanum xanthocarpum fruit extract against gentamicin–induced nephrotoxicity and renal dysfunction in experimental rodents. Asian Pac. J. Trop. Med. 2012, 5, 686–691. [Google Scholar] [CrossRef] [PubMed]
- Balakumar, P.; WitnessKoe, W.E.; Gan, Y.S.; JemayPuah, S.M.; Kuganesswari, S.; Prajapati, S.K.; Varatharajan, R.; Jayachristy, S.A.; Sundram, K.; Bahari, M.B. Effects of pre and post-treatments with dipyridamole in gentamicin-induced acute nephrotoxicity in the rat. Regul. Toxicol. Pharmacol. 2017, 84, 35–44. [Google Scholar] [CrossRef] [PubMed]
- Domitrović, R.; Cvijanović, O.; Pernjak-Pugel, E.; Škoda, M.; Mikelić, L.; Crnčević-Orlić, Ž. Berberine exerts nephroprotective effect against cisplatin-induced kidney damage through inhibition of oxidative/nitrosative stress, inflammation, autophagy and apoptosis. Food Chem. Toxicol. 2013, 62, 397–406. [Google Scholar] [CrossRef]
- Stojiljkovic, N.; Stoiljkovic, M.; Randjelovic, P.; Veljkovic, S.; Mihailovic, D. Cytoprotective effect of vitamin C against gentamicin-induced acute kidney injury in rats. Exp. Toxicol. Pathol. 2012, 64, 69–74. [Google Scholar] [CrossRef]
- Mahmoud, A.M.; Ahmed, O.M.; Galaly, S.R. Thymoquinone and curcumin attenuate gentamicin-induced renal oxidative stress, inflammation and apoptosis in rats. EXCLI J. 2014, 13, 98–110. [Google Scholar]

| Mean Values ± SD | Student’s t-Test | ||
|---|---|---|---|
| Control group | Initial body weight (g) | 383.57 ± 44.87 | p = 0.0347 |
| Final body weight (g) | 388.57 ± 47.60 | ||
| Gentamicin group | Initial body weight (g) | 416.57 ± 64.47 | p = 0.0011 |
| Final body weight (g) | 392.43 ± 66.76 | ||
| Curcumin group | Initial body weight (g) | 402.17 ± 23.25 | p = 0.0102 |
| Final body weight (g) | 374.33 ± 39.55 | ||
| Vitamin C group | Initial body weight (g) | 382.71 ± 16.71 | p < 0.0001 |
| Final body weight (g) | 340.57 ± 13.53 |
| Diuresis (mL/24 h) | Mean Values ± SD | ANOVA | p Value, Compared to Control |
|---|---|---|---|
| Control group | 21.500 ± 0.707 | 0.0002 | - |
| Gentamicin group | 11.000 ± 1.581 | p = 0.0002 | |
| Curcumin group | 14.250 ± 2.217 | p = 0.0036 | |
| Vitamin C group | 12.125 ± 1.652 | p = 0.0005 |
| Control Group | Gentamicin Group | Curcumin Group | Vitamin C Group | ||
|---|---|---|---|---|---|
| Total score | Median | 0 | 7 | 5.5 | 3 (* p < 0.0001) (^ p = 0.0131) |
| IQR | 0 | 1 | 1.75 | 1.5 | |
| Parenchymal damage score | Median | 0 | 4 | 3 | 1 |
| IQR | 0 | 0 | 0.75 | 1 (* p < 0.0001) (^ p = 0.0077) | |
| Glomeruli injury score | Median | 0 | 2 | 1.5 (* p = 0.0305) | 1 (* p = 0.0001) |
| IQR | 0 | 0 | 1 | 0 | |
| Acute tubular necrosis score | Median | 0 | 3 | 3 | 1 (* p = 0.0003) (^ p = 0.0055) |
| IQR | 0 | 1 | 0 | 1 | |
| Tubulo-interstitial infiltrate score | Median | 0 | 2 | 1 | 1 (* p = 0.0016) |
| IQR | 0 | 0.5 | 0.75 | 0.5 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tomşa, A.M.; Răchişan, A.L.; Pandrea, S.L.; Benea, A.; Uifălean, A.; Toma, C.; Popa, R.; Pârvu, A.E.; Junie, L.M. Curcumin and Vitamin C Attenuate Gentamicin-Induced Nephrotoxicity by Modulating Distinctive Reactive Species. Metabolites 2023, 13, 49. https://doi.org/10.3390/metabo13010049
Tomşa AM, Răchişan AL, Pandrea SL, Benea A, Uifălean A, Toma C, Popa R, Pârvu AE, Junie LM. Curcumin and Vitamin C Attenuate Gentamicin-Induced Nephrotoxicity by Modulating Distinctive Reactive Species. Metabolites. 2023; 13(1):49. https://doi.org/10.3390/metabo13010049
Chicago/Turabian StyleTomşa, Anamaria Magdalena, Andreea Liana Răchişan, Stanca Lucia Pandrea, Andreea Benea, Ana Uifălean, Corina Toma, Roxana Popa, Alina Elena Pârvu, and Lia Monica Junie. 2023. "Curcumin and Vitamin C Attenuate Gentamicin-Induced Nephrotoxicity by Modulating Distinctive Reactive Species" Metabolites 13, no. 1: 49. https://doi.org/10.3390/metabo13010049
APA StyleTomşa, A. M., Răchişan, A. L., Pandrea, S. L., Benea, A., Uifălean, A., Toma, C., Popa, R., Pârvu, A. E., & Junie, L. M. (2023). Curcumin and Vitamin C Attenuate Gentamicin-Induced Nephrotoxicity by Modulating Distinctive Reactive Species. Metabolites, 13(1), 49. https://doi.org/10.3390/metabo13010049










