Abstract
Periodontitis is a microbially driven, host-mediated disease that leads to loss of periodontal attachment and resorption of bone. It is associated with the elevation of systemic inflammatory markers and with the presence of systemic comorbidities. Coronavirus disease 2019 (COVID-19) is a contagious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Although the majority of patients have mild symptoms, others experience important complications that can lead to death. After the spread of the COVID-19 pandemic, several investigations demonstrating the possible relationship between periodontitis and COVID-19 have been reported. In addition, both periodontal disease and COVID-19 seem to provoke and/or impair several cardiometabolic complications such as cardiovascular disease, type 2 diabetes, metabolic syndrome, dyslipidemia, insulin resistance, obesity, non-alcoholic fatty liver disease, and neurological and neuropsychiatric complications. Therefore, due to the increasing number of investigations focusing on the periodontitis-COVID-19 relationship and considering the severe complications that such an association might cause, this review aims to summarize all existing emerging evidence regarding the link between the periodontitis-COVID-19 axis and consequent cardiometabolic impairments.
1. Introduction
Periodontitis is a microbially driven host-mediated disease that leads to loss of periodontal attachment and resorption of bone [1]. During the initial stages, gingival inflammation (i.e., gingivitis) is provoked by bacterial biofilm formation. Consequently, the progression of periodontal disease to destructive periodontitis depends on: microbial dysbiosis in response to nutrients from gingival inflammatory and tissue breakdown products favoring the growth of some bacterial species; and reducing anti-bacterial mechanisms that try to contain the microbial challenge within the gingival sulcus [1]. It has now clearly emerged that periodontal inflammation is not just a local phenomenon, but is also associated with systemic conditions and diseases, such as obesity [2] and diabetes mellitus [3,4,5].
Coronavirus disease 2019 (COVID-19) is a contagious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Although in the majority of cases infected patients are asymptomatic and/or have mild symptoms, in some cases this virus can cause severe complications and can be life-threatening. Regrettably, the COVID-19 pandemic heavily hit the regular functionality of the health system worldwide, leading to a tremendous deficiency in providing primary care and leading to an extremely urgent need for new vaccines [6]. A retrospective study conducted on 860 Nepalese COVID-19 patients admitted at the Sukraraj Tropical and Infectious Disease Hospital reported that 5.8% of them died, 2.9% of them needed advanced treatment such as dialysis and mechanical ventilation, and 16% of them showed microbiological evidence of secondary infection [7]. Very interestingly, several serious COVID-19 patients showed the presence of mucormycosis (or black fungus), a severe fungal infection provoked by mucormycetes, probably due to poor oral hygiene, uncontrolled diabetes, unhygienic use of oxygen therapy, and overuse of steroids [8]. Even though the use of steroids has become controversial and confusing among physicians, a recent metanalysis has found that steroids, in particular methylprednisolone, might significantly reduce deaths among hospitalized COVID-19 patients [9]. Despite still being a controversial issue, another study observed that the use of angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers (ACEi/ARB) in COVID-19 hypertensive patients was not associated with their mortality rate [10].
Numerous recent studies highlighted that both periodontitis and COVID-19 might present a bidirectional relationship; in addition, they hypothesized that their synergic effects may lead to an important impairment in patients with other systemic diseases [11,12,13].
Thus, the objective of this review article is to describe the possible association between periodontal disease and COVID-19 with respect to the increased risk and cardiometabolic complications of both diseases.
2. Periodontitis and Chronic Non-Communicable Diseases
Chronic non-communicable diseases (NCDs) are diseases that are not directly transmissible from one person to another, as defined by the World Health Organization (WHO). They include cardiovascular diseases, cancer, chronic respiratory diseases, and diabetes, and are responsible for 61% of all deaths worldwide [14].
Periodontitis was reported to be one of the most prevalent chronic NCDs in the USA [15] and has numerous risk factors in common with other NDCs, including smoking, glycemic control, unhealthy diet, alcohol consumption, personal hygiene, stress, genetics, and socio-economic determinants [16].
Periodontal inflammation is not just a local phenomenon. Even though periodontitis has been independently associated with NDCs, the possible relationship between periodontitis and systemic conditions has been widely reported in recent years. In 2013, in the “Proceedings of a workshop jointly held by the European Federation of Periodontology and the American Academy of Periodontology”, the authors concluded that proinflammatory (infectious) events related to periodontal disease may have a systemic impact and, conversely, some systemic disorders might influence periodontal outcomes [17,18,19,20].
A 12-year cohort study in a Korean population reported that periodontally compromised patients have a significantly increased risk of NCDs, in particular obesity (OR 1.30), osteoporosis (OR 1.22), and angina pectoris (OR 1.22) [21]. A cross-sectional study in a Brazilian population of non-smokers and non-alcohol users found that periodontal patients had a higher level of triglycerides, C-reactive protein, blood glucose, lower HDL-c levels, and a higher risk of coronary heart disease [22]. Moreover, older adults had a significantly higher prevalence of dyslipidemia and subclinical atherosclerosis, whereas young adults had a significantly higher prevalence of obesity, pre-diabetes, hypertension, and metabolic syndrome [22]. Although the role of periodontal inflammation as a mediating mechanism in NDCs has not yet been thoroughly explained [23], a very recent overview on oral health and NCDs remarked on the importance of good oral care, which was defined as one of the most important lifestyle-related determinants of health, as well as physical exercise, in reducing the risk of systemic diseases [24]. A systematic review and meta-analysis concluded that periodontitis was associated with an increased risk of all-cause mortality (RR 1.46), mortality due to cardiovascular disease (RR 1.47), cancer (RR 1.38), coronary heart disease (2.58), and cerebrovascular diseases (RR 3.11); pneumonia was associated with edentulism (RR 1.72), which is the ultimate sequela of periodontal disease [25].
Within the aims of the present review, a potential role of periodontitis in the development of respiratory diseases such as asthma, chronic obstructive pulmonary disease (COPD), and pneumonia is investigated [26]. Pneumonia can be classified as community-acquired, developed in non-institutionalized people, nosocomial (hospital-acquired), and/or aspiration pneumonia [27,28]. In particular, nosocomial pneumonia is an infection of the inferior respiratory tract, acquired by patients in a hospital setting at least 48 h after hospitalization [29] due to the aspiration of saliva containing gram-negative anaerobic bacteria (including Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae, Pseudomonas aeruginosa, Acinetobacter spp., Enterobacter spp.) [30], leading to severe anaerobic pulmonary infections [31]. Therefore, patients with periodontitis may have a significantly increased risk of having pneumonia [32], as confirmed by Awano et al. in a study on a Japanese population of 80-year-olds, which found that aspiration pneumonia caused a mortality 3.9 times higher in subjects with 10 or more teeth with periodontal pockets > 4 mm deep compared with periodontally healthy individuals [33]. Although firm conclusions were not drawn due to different limitations in study design, several systematic reviews have reported that periodontitis might be associated with nosocomial/aspiration pneumonia [34,35], in particular in patients admitted in intensive care units (ICU) and those admitted for a long period (OR 2.55) [36]. Very interestingly, a study on 787 healthy patients (whose data were recollected from the ORIGINS project database) revealed that the log-ratio of Treponema to Corynebacterium bacteria might be a novel microbial indicator of periodontitis (MIP) that correlates with poor periodontal health and cardiometabolic markers early in disease pathogenesis in both the subgingival plaque and saliva [37].
3. COVID-19 and Associated Factors
Coronavirus disease 2019 (COVID-19) is a contagious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) derived from the Coronaviridae family (WHO).
COVID-19 may infect people mainly via respiratory droplets and aerosols (e.g., from coughing, sneezing, shouting) during close face-to--to-face contact, even though contaminated surfaces might also be contagious [38]. Originally identified in the city of Wuhan in China [39,40,41], COVID-19 provoked a tremendous pandemic with more than 600 million positive cases and more than 6.5 million deaths, as of 9 October 2022 (https://coronavirus.jhu.edu/map.html).
In terms of pathogenicity, SARS-CoV-2 presents a protein spike (S) on its surface that binds to the angiotensin-converting enzyme 2 (ACE2) receptor [42]. Another important role is played by the type 2 transmembrane serine protease (TMPRSS2), which is located in the host cell and leads to viral penetration by cleaving ACE2 and activating the SARS-CoV-2 S protein [42]. ACE2 and TMPRS22 are expressed in host target cells such as alveolar epithelial type II cells [43]. The average incubation period, that is, the time from exposure to symptom onset, is around 5 (2–7) days, and about 97% of subjects who develop any symptoms do so within 11.5 days of infection [44]. However, those features/timings may change depending on the different newer COVID-19 variants that have evolved over time. Patients infected by COVID-19 may be asymptomatic or may either present mild symptoms including anosmia and/or dysgeusia or severe complications that can lead to death [45]. A Chinese study reported an occurrence of mild manifestations in 81% of patients, severe manifestations in 14% of patients, and critical manifestations (e.g., respiratory failure, septic shock, and multiple organ dysfunction [41]) in 5% of the patients [46]. The most common symptoms in hospitalized patients are fever (up to 90% of patients), dry cough (60–86%), shortness of breath (53–80%), fatigue (38%), nausea/vomiting or diarrhea (15–39%), and myalgia (15–44%). Approximately 17%–35% of hospitalized patients with COVID-19 are treated in the ICU, most commonly due to hypoxemic respiratory failure (pneumonia observed in 75% of cases and acute respiratory distress syndrome (ARDS) in 15% of cases) [38,47].
In addition, as described by two review articles, COVID-19 was associated with several oral manifestations, including oral lesions (in both keratinized and non-keratinized mucosa), taste dysfunction (dysgeusia), and xerostomia [48,49]. Dysgeusia was the first recognized oral symptom of COVID-19, whereas aphthous-like lesions, herpetiform lesions, candidiasis, and oral lesions of Kawasaki-like disease were the most common oral manifestations. The most common sites involved were the tongue (38%), labial mucosa (26%), palate (22%), gingiva (8%), buccal mucosa (5%), oropharynx (4%), and tonsil (1%), with those lesions being symptomatic (pain, pruritus, burning sensations) in 68% of cases, equal in both sexes, and more wide-spread and severe in older people with a higher severity of COVID-19 [48]. Lack of oral hygiene, opportunistic infections, stress, immunosuppression, vasculitis, and hyper-inflammatory response were identified as the most important predisposing factors for the onset of oral lesions in COVID-19 patients [48].
4. Periodontitis and COVID-19: Association Studies and Outcomes
Over the past two years, several studies with the purpose of demonstrating a connection between periodontitis and COVID-19 have been published.
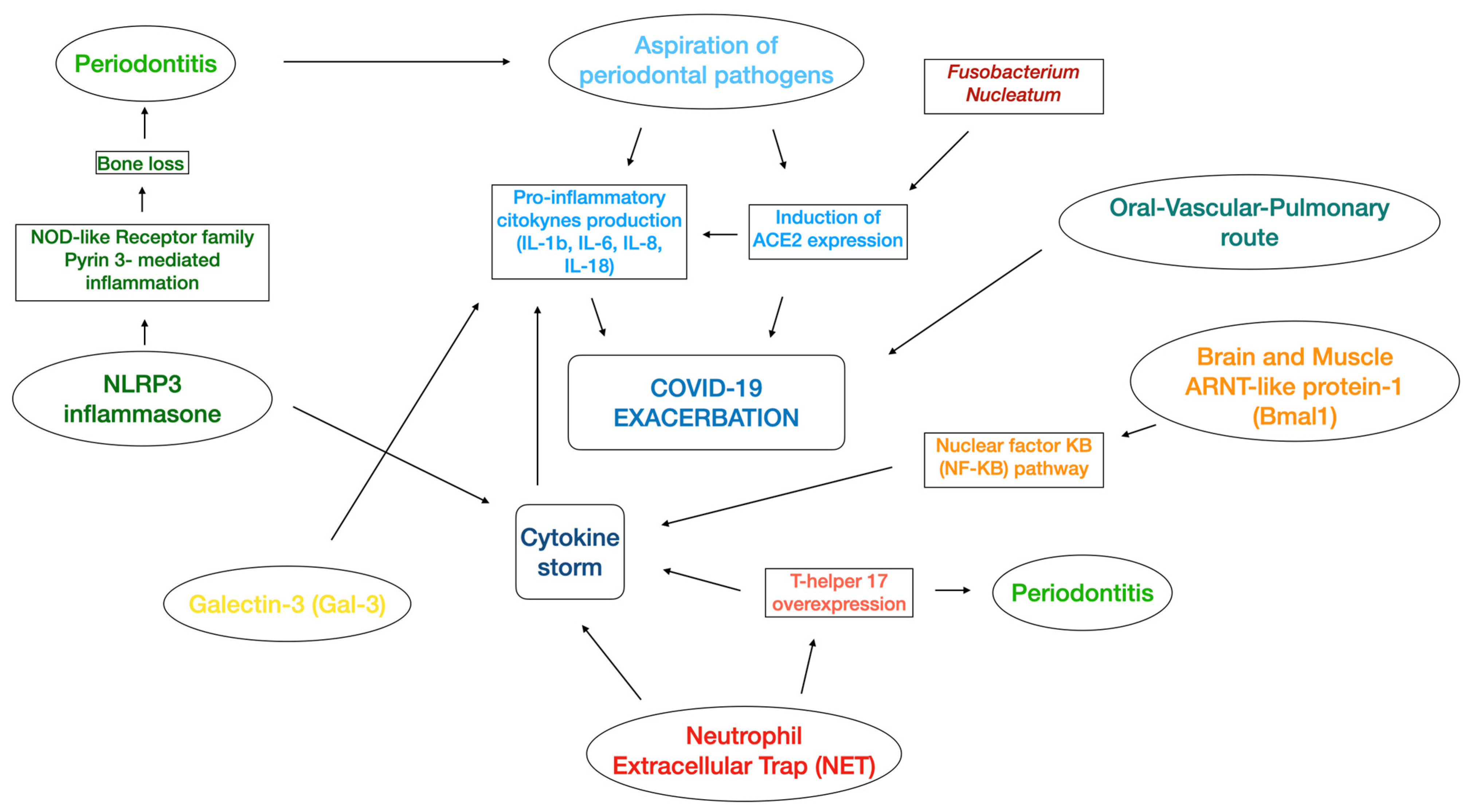
In line with the periodontitis–nosocomial pneumonia association discussed above, the aspiration of periodontopathic bacteria induces the expression of angiotensin-converting enzyme 2 (ACE2), a receptor for SARS-CoV-2, and after cleaving the S protein (essential for the development of SARS-CoV-2) by producing proteases [50], may link periodontitis with COVID-19 (Figure 1). In addition, periodontopathic bacteria increase the production of inflammatory cytokines in the lower respiratory tract [50]. An in vitro study confirmed that the culture supernatant of Fusobacterium nucleatum (CSF) upregulated the expression of ACE2 in human alveolar epithelial cells and the production of IL-6 and IL-8 in human respiratory epithelial cells [51].
Figure 1.
Illustration of the several mechanisms related to the association between periodontitis and COVID-19. NLRP3 inflammasone: nucleotide-binding domain, leucine-rich repeat pyrin domain containing 3 inflammasone; ARNT-like protein 1: aryl hydrocarbon receptor nuclear translocator-like protein 1; IL: Interleukin; NOD-like receptor: nucleotide-binding and oligomineralization domain-like receptor.
Regarding the role of the mouth, numerous investigations have reported that the oral cavity might be an important viral reservoir [52,53,54,55,56]. Specifically, the virus might be present in the epithelial lining/mucosa wall and periodontal fibroblast of the deep pockets [52]; a high expression of ACE2 was mainly found in the tongue mucosa [55,57] and was higher in the minor salivary glands than in the lungs [58]. Furthermore, other studies have reported that the SARS-CoV-2 viral load was consistently high in saliva (more than in the oropharynx) [59] and was harbored in the dental biofilm [60] and gingival crevicular fluid (GCF) of COVID-19 subjects [61]. Very interestingly, in a postmortem study, video-endoscope minimally invasive biopsies were performed in seven subjects, and the authors found that the periodontal tissues of five patients contained the presence of SARS-CoV-2, indicating that the virus could be stored in the mouth for a long period of time [62].
Another plausible mechanism considers the role of the NLRP3 inflammasome, which are components of the innate immune system and play an important role in the activation of inflammatory responses and maturation and secretion of proinflammatory cytokines, including IL-18 and IL-1β. Several studies have reported that the NOD-like receptor family pyrin 3- (NLRP3-) mediated inflammation was effective in alveolar bone loss [63,64,65]. COVID-19 infection may activate the NLRP3 inflammasome with consequent intensive cytokine expression (cytokine storm) [66] which, in turn, might determine the severity of periodontitis [67,68].
Some authors hypothesized that both diseases might share the production of neutrophil extracellular traps (NET), which resides in an alternative form of cell death (causing damage either directly or via the activation of autoimmune mechanisms), leading to the creation of neutrophil extracellular traps to contain and eliminate insults [69]. The same authors proposed that both diseases may have a connection related to cytokines. In detail, the aforementioned “cytokine storm” (elevated serum level of IL-1b, IL-2, IL-7, IL-8, IL-9 IL-10, IL-17, GM-CSF, G-CSF, INF-gamma, INF alpha, MIP1A, MIP1B, MCP1, and IP1) was present in COVID-19 together with an elevated T-helper 17 (Th17) pathway response [70,71,72]. Interestingly, in advanced periodontal disease, the strong Th17 response might exacerbate the cytokine storm in COVID-19, leading to major complications such as ICU admission, tissue damage in lung infections, and pulmonary oedema [73]. Another possible link might be related to interleukin-6 (IL-6), which was described to be important in the pathogenesis of both periodontitis and the cytokine storm [74,75]. Consistently, a systematic review and meta-analysis reported that, in patients with complicated COVID-19, the mean IL-6 levels were 2.9-fold higher compared with patients presenting non-complicated disease [76].
Other authors proposed the “Oral-Vascular-Pulmonary Route”, which consists of a direct viral delivery from the oral cavity (gingival capillaries) via the venous drainage of the mouth, neck (jugular veins), and chest (superior vena cava) through the right side of the heart and then to the pulmonary vessels, causing pulmonary vasoconstriction and immunothrombosis [77]. Poor oral hygiene and periodontal disease (with the consequent presence of periodontal wounds due to ulcerations in the pocket’s epithelium) may thus increase the probability of having severe COVID-19 complications [77].
Another studied mechanism involves the role of galectin-3 (Gal-3), a member of the beta-galactoside binding protein family with proinflammatory properties and involved in T-cell-mediated inflammation that is expressed in immune cells, epithelial cells, endothelial cells, and sensory neurons [78]. A study demonstrated that a consistent area in the spike protein (essential for virus entrance into the host cells) of COVID-19 is almost the same as the morphology of Gal-3 [79], whereas other authors reported that there is a positive correlation between increased levels of Gal-3 and the severity of periodontitis (data not published) [78]. Therefore, the authors hypothesized that Gal-3-mediated increased immune response and increased viral attachment might reinforce the relationship between periodontitis and COVID-19 [78].
A further link may derive from the circadian system [80]. In fact, a circadian gene named brain and muscle ARNT-like protein-1 (Bmal1), which decreases when the sleep-wake cycle is disrupted, may induce the cytokine storm (common for both COVID-19 and periodontitis) via the nuclear factor kB (NF-kB) pathway [80].
Figure 1 illustrates the described perio-COVID-19 mechanisms, and Table 1 summarizes all of the possible molecules that are involved.

Table 1.
Summary of some of the several molecules that are involved in the mechanisms behind the COVID-19 and the periodontitis relationship.
A case-control study on 568 Qatarian patients with COVID-19 reported that, after adjusting for important confounders including smoking, age, and sex, periodontitis was associated with important COVID-19 complications (overall OR 3.67, 95% CI 1.46–9.27) such as intensive care unit (ICU) admissions (OR 3.54, 95% CI 1.39–9.05), need for assisted ventilation (OR 4.57, 95% CI 1.19–17.4), and death (OR 8.81, 95% CI 1.00–77.7). Moreover, C-Reactive Protein, white blood cells (WBC), and HbA1c levels were significantly higher in COVID-19 patients with periodontitis [81]. Another case-control study in India observed that, after adjusting for frequency of self-oral hygiene and age, COVID-19 was significantly associated with mean plaque score ≥ 1 (OR 7.01, 95% CI 1.83–26.94), gingivitis (OR 17.65, 95% CI 5.95–52.37), mean clinical attachment level (CAL) ≥ 2 mm (OR 8.46, 95% CI 3.47–20.63) and severe periodontitis (OR 11.75, 95% CI 3.89–35.49); additionally, gingival bleeding and plaque accumulation were more frequently present in COVID-19 patients [82]. A further case-control study in an Indian cohort showed that patients with bleeding on probing presented a greater risk of a need for assisted ventilation (OR 4.14, 95% CI 1.51–11.34, in particular among patients with periodontitis Stage III-IV), presence of COVID-19 pneumonia (OR 3.63), and hospital admission (OR 3.18, 95% CI 1.24–8.15) [83]. A higher severity of periodontitis was correlated with the need of assisted ventilation (OR 7.45), COVID-19 pneumonia (OR 4.42), death (OR 14.58), and hospital admission (OR 36.52). Furthermore, 10% of deceased patients had severe periodontal disease [83]. However, it must be highlighted that significant confounders such as socioeconomic status, obesity, and smoking were not considered.
A retrospective study based on examination records and panoramic X-rays showed that patients with a higher dental damage stage (DD Stg) (a new score that takes into account periodontal condition, caries, root canal treatment, and missing teeth) presented an increased hospitalization and mortality rate of COVID-19 [84]. Nevertheless, no confounding variables from other factors were taken into account in the analysis. Two more retrospective studies reported that patients with COVID-19 and periodontitis presented a significantly higher mortality (OR 1.71, 95% CI: 1.05–2.72) compared with periodontally health patients after adjusting for age, sex, ethnicity, average total household income, BMI, systolic and diastolic blood pressure, history of smoking, and history of previous systemic conditions [85]; additionally, patients with periodontal diseases were 4.7 times more likely to develop COVID-19 compared with non-periodontal patients after adjusting for smoking [86]. A Mendelian randomization (MR) study suggested that genetically proxied periodontal disease was significantly associated with a major risk of susceptibility and hospitalization of COVID-19, even though it did not seem to have a causal effect on COVID-19 severe respiratory complications [87].
Different reviews have indicated a series of possible shared risk factors such as aging, male sex, diabetes [3,4,50], hypertension and cardiovascular disease, coronary artery disease, atherosclerotic diseases, obesity [2], pregnancy, chronic obstructive pulmonary disease (COPD), smoking, asthma, HIV, cancer, oral dysbiosis, liver diseases, dementia, chronic kidney disease, Down syndrome, type A blood group, specific ethnic groups, physical disability/learning difficulty, and rheumatoid arthritis [77,88,89]. A very recent meta-analysis of epidemiological studies found that periodontal patients with COVID-19 have a four times higher risk of hospitalization, a six times higher risk of need for assisting ventilation, and seven times higher risk of death due to COVID-19 complications [90].
Oral hygiene has been hypothesized to be crucial in preventing post-COVID-19 complications [91]. Metagenomic analysis of COVID-19 patients showed the presence of high reads for periodontal bacteria such as Fusobacterium, Prevotella, and Staphylococcus [92]. Authors recommend that self-oral hygiene should be improved to reduce the bacterial load and the risk of bacterial superinfection [91]. A cross-sectional study on an Egyptian population, with the aid of questionnaires, found that poor oral status significantly impacted the severity of COVID-19 and, additionally, was correlated with increased values of C-reactive protein (CRP) and delayed recovery period [93]. Curiously, an online survey in a Turkish population showed an association between COVID-19 fear and oral health status [94]. Patients that started to pay more attention to their hygiene habits and rate/quality of food consumption were the ones with the higher fear of COVID-19; moreover, although those patients had increased complaints and dental problems, they hesitated to go to the dentist as they believed that the dental setting might increase the risks of COVID-19 contamination [94].
Conversely, other authors focused on the plausible negative effect that COVID-19 might have on periodontal health and hypothesized that COVID-19 might predispose to necrotizing periodontal disease (NPD) [95]. In fact, bacteria that are usually present in NPD lesions such as Prevotella intermedia, Fusobacterium, and Treponema were found in metagenomic analyses of infected subjects with severe COVID-19 disease [95].
Table 2 summarizes the existing studies focused on the plausible periodontitis–COVID-19 relationship.

Table 2.
Summary of existing studies investigating the possible association between COVID-19 and periodontitis.
5. Cardiometabolic Connections in the Perio-COVID-19 Axis
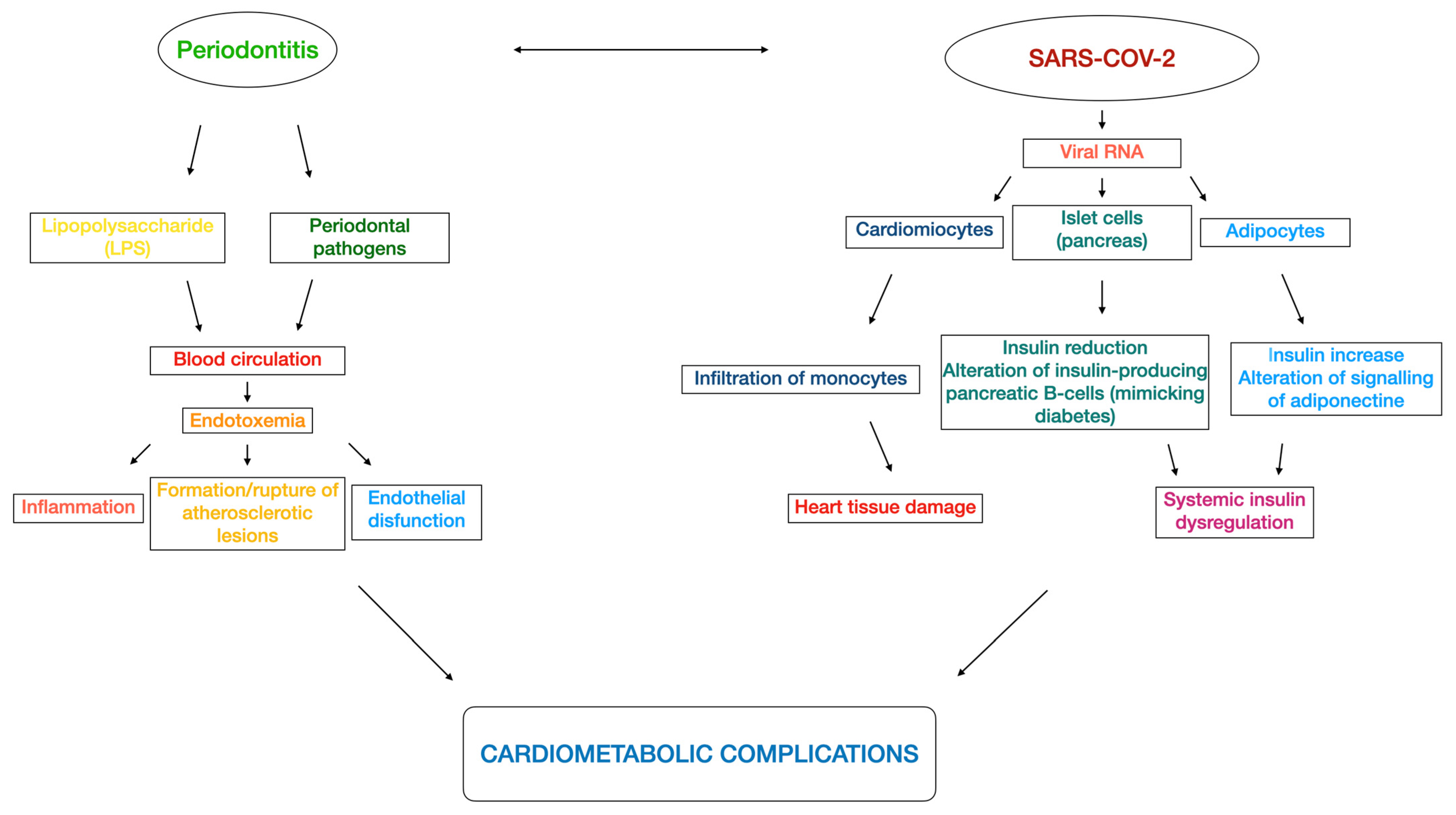
As extensively reported in the literature, periodontitis and cardiometabolic diseases (including cardiovascular disease, type 2 diabetes, metabolic syndrome, dyslipidemia, insulin resistance, obesity, and non-alcoholic fatty liver disease [96]) might present a bidirectional relationship [97,98,99]. The dysbiosis of periodontal microbiota might cause endotoxemia as well, as it occurs due to the entrance of bacterial lipopolysaccharide (LPS) into the blood circulation [100]. Consequently, those bacteria in the blood stream may provoke inflammation [101], formation and/or rupture of atherosclerotic lesions [102], and may affect the vessel walls (i.e., endothelial dysfunction, [103]), leading to a major risk of cardiometabolic complications [100]. A retrospective cohort study based on a UK population found that subjects with gingivitis and/or periodontitis had an increased likelihood of having a diagnosis of cardiometabolic diseases (aOR: 1.16; 95% CI 1.13 to 1.19) and an increased risk of developing cardiometabolic diseases (HR 1.07; 95% CI 1.03 to 1.10) compared with periodontally healthy patients [104].
Similarly, as suggested by the American College of Cardiology Foundation, COVID-19 showed epidemiological and mechanistic relationships with cardiometabolic links [105,106] such as abnormal adiposity, dysglycemia [107,108,109,110,111], dyslipidemia, and hypertension [112]. In fact, COVID-19 caused an inflammatory response that might affect the cardiometabolic status. More specifically, as reported by a study using a hamster model, SARS-CoV-2 infected cardiomyocytes and provoked a mechanism of immune cell infiltration and histopathology that might result in heart tissue damage in COVID-19 patients [113]. Moreover, evidence suggests that altered insulin signaling with consequent insulin dysregulation was caused by the presence of viral RNA in pancreatic cells and adipocytes [114,115]. A Swedish nationwide case-control study of COVID-19 patients requiring invasive mechanical ventilation reported that diabetes, hypertension, and obesity were independently associated with severe COVID-19; additionally, the younger population (<57 years) had a stronger association than the older one [116]. Interestingly, an investigation based on data from the UK Biobank found that increased adiposity (adipose volume), assessed as body mass index (BMI), waist:hip ratio (WHR), and body fat, was associated with higher risks of COVID-19-related mortality [117]. In addition, some COVID-19 patients unfortunately presented the so called “long-COVID” (also named “long-haul COVID”, “post-COVID syndrome”, or “post-COVID conditions”), characterized by protracted symptoms for a period that may remain from more than 4 weeks to more than 3 months [118,119]. In detail, those patients showed malaise, fatigue, dyspnea, neuropsychiatric syndromes, and defect in memory and concentration [120]. A UK cohort study with 12-month follow-up reported that diabetes incidence was elevated for at least 12 weeks following COVID-19 before decreasing, whereas cardiovascular disease incidence such as pulmonary embolism, atrial arrhythmias, and venous thromboses was high for the first 4 weeks, then decreased from 5 to 12 weeks, and, lastly, consistently dropped from 13 to 52 weeks [121]. Figure 2 illustrates the plausible perio-COVID pathways that might impair the cardiometabolic complications.
Figure 2.
Flowchart of the several perio-COVID pathways that might lead to cardiometabolic impairments.
6. Clinical Relevance and Take-Home Message
Due to the aforementioned concrete risks of developing severe complications, a syndemic approach involving biological, social, economic, and environmental factors has been proposed by the Cardiometabolic Panel of International experts on Syndemic COVID-19 (CAPISCO) [122]. Furthermore, physicians should follow a holistic approach when treating COVID-19 patients, also taking into account the observed increased neurological and neuropsychiatric complications such as memory loss, sleep disorders, impaired concentration, major depression, and delirium [123,124].
Moreover, efforts should be taken to prevent periodontal disease and, for patients that already have periodontitis, an immediate intervention should be provided to improve their gingival health. In particular, physicians should remark the importance of having a proper oral hygiene, and they should ideally suggest to their patients to have regular dental visits in order to prevent or detect any form of periodontal disease, above all during the current pandemic period, keeping in mind the potential associations between periodontitis and cardiometabolic complications [125,126,127].
7. Conclusions and Recommendations for Future Studies
Within the limitations of the included studies, the following conclusions can be drawn:
- Periodontitis and COVID-19 have in common a hyper-inflammatory state. Despite some consistent associations in cross-sectional studies, definitive conclusions regarding their link cannot be drawn.
- Nevertheless, in light of a possible bidirectional relationship, the importance of maintaining or achieving periodontal health to prevent or contain COVID-19 complications must be highlighted.
- The importance of having proper oral hygiene to reduce any possible viral source proceeding from the mouth must be considered and, in particular, periodontally compromised patients should receive adequate periodontal management, including oral hygiene instructions.
- A multi-professional therapeutic plan from physicians and dentists must be agreed upon to identify and adequately manage each COVID-19 patient while doing so in a tailored manner.
In terms of future research, long-term clinical trials investigating the magnitude of the association between periodontitis and COVID-19 and their mechanisms are needed.
Author Contributions
Conceptualization, G.M., L.N., M.I. and M.R.; methodology, G.M., L.N., M.I. and M.R.; data curation, G.M.; writing—original draft preparation, G.M., L.N., M.I. and M.R.; writing—review and editing, W.A.M., K.A.-R., K.A.-A., M.B., Y.B., A.C., M.C., F.C., A.F., M.G., S.-Y.G., A.J., S.K., N.K., P.K., N.L., P.L., N.P., A.A.R., A.S., R.D.S., A.P.S., P.P.T. and V.V.; supervision, L.N., M.I. and M.R.; project administration, M.R.; funding acquisition, M.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Tonetti, M.S.; Greenwell, H.; Kornman, K.S. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J. Periodontol. 2018, 89 (Suppl. S1), S159–S172. [Google Scholar] [CrossRef] [PubMed]
- Čolak, D.; Cmok Kučič, A.; Pintar, T.; Gašpirc, B.; Gašperšič, R. Periodontal and systemic health of morbidly obese patients eligible for bariatric surgery: A cross-sectional study. BMC Oral Health 2022, 22, 174. [Google Scholar] [CrossRef] [PubMed]
- Preshaw, P.M.; Bissett, S.M. Periodontitis and diabetes. Br. Dent. J. 2019, 227, 577–584. [Google Scholar] [CrossRef] [PubMed]
- Stöhr, J.; Barbaresko, J.; Neuenschwander, M.; Schlesinger, S. Bidirectional association between periodontal disease and diabetes mellitus: A systematic review and meta-analysis of cohort studies. Sci. Rep. 2021, 11, 13686. [Google Scholar] [CrossRef]
- Nibali, L.; Gkranias, N.; Mainas, G.; Di Pino, A. Periodontitis and implant complications in diabetes. Periodontol 2000 2022, 90, 88–105. [Google Scholar] [CrossRef]
- Leggat, P.A.; Frean, J.; Blumberg, L. COVID-19: Current Challenges and Future Perspectives. Trop. Med. Infect. Dis. 2022, 7, 16. [Google Scholar] [CrossRef]
- Bastola, A.; Shrestha, S.; Nepal, R.; Maharjan, K.; Shrestha, B.; Chalise, B.S.; Thapa, P.; Balla, P.; Sapkota, A.; Shah, P. Clinical Mortality Review of COVID-19 Patients at Sukraraj Tropical and Infectious Disease Hospital, Nepal; A Retrospective Study. Trop. Med. Infect. Dis. 2021, 6, 137. [Google Scholar] [CrossRef]
- Kumar, A. Mucormycosis in COVID-19 recovered patients. J. Med. Virol. 2022, 94, 1272–1273. [Google Scholar] [CrossRef]
- Thakur, M.; Datusalia, A.K.; Kumar, A. Use of steroids in COVID-19 patients: A meta-analysis. Eur. J. Pharmacol. 2022, 914, 174579. [Google Scholar] [CrossRef]
- Azad, G.N.; Kumar, A. ACEi/ ARB and Deaths of COVID-19 Patients. Curr. Hypertens. Rev. 2022, 18, 158–162. [Google Scholar] [CrossRef]
- Kapoor, N.; Kalra, S.; Al Mahmeed, W.; Al-Rasadi, K.; Al-Alawi, K.; Banach, M.; Banerjee, Y.; Ceriello, A.; Cesur, M.; Cosentino, F.; et al. The Dual Pandemics of COVID-19 and Obesity: Bidirectional Impact. Diabetes Ther. 2022, 13, 1723–1736. [Google Scholar] [CrossRef] [PubMed]
- Rizvi, A.A.; Kathuria, A.; Al Mahmeed, W.; Al-Rasadi, K.; Al-Alawi, K.; Banach, M.; Banerjee, Y.; Ceriello, A.; Cesur, M.; Cosentino, F.; et al. Post-COVID syndrome, inflammation, and diabetes. J. Diabetes Complicat. 2022, 36, 108336. [Google Scholar] [CrossRef] [PubMed]
- Lo Presti, E.; Nuzzo, D.; Al Mahmeed, W.; Al-Rasadi, K.; Al-Alawi, K.; Banach, M.; Banerjee, Y.; Ceriello, A.; Cesur, M.; Cosentino, F.; et al. Molecular and pro-inflammatory aspects of COVID-19: The impact on cardiometabolic health. Biochim. Biophys. Acta Mol. Basis Dis. 2022, 1868, 166559. [Google Scholar] [CrossRef] [PubMed]
- GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar] [CrossRef]
- Eke, P.I.; Dye, B.A.; Wei, L.; Slade, G.D.; Thornton-Evans, G.O.; Borgnakke, W.S.; Taylor, G.W.; Page, R.C.; Beck, J.D.; Genco, R.J. Update on Prevalence of Periodontitis in Adults in the United States: NHANES 2009 to 2012. J. Periodontol. 2015, 86, 611–622. [Google Scholar] [CrossRef] [PubMed]
- Petersen, P.E.; Ogawa, H. The global burden of periodontal disease: Towards integration with chronic disease prevention and control. Periodontol 2000 2012, 60, 15–39. [Google Scholar] [CrossRef]
- Linden, G.J.; Herzberg, M.C. Periodontitis and systemic diseases: A record of discussions of working group 4 of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. J. Clin. Periodontol. 2013, 40 (Suppl. S14), S20–S23. [Google Scholar] [CrossRef]
- Borgnakke, W.S.; Ylöstalo, P.V.; Taylor, G.W.; Genco, R.J. Effect of periodontal disease on diabetes: Systematic review of epidemiologic observational evidence. J. Periodontol. 2013, 84, S135–S152. [Google Scholar] [CrossRef]
- Dietrich, T.; Sharma, P.; Walter, C.; Weston, P.; Beck, J. The epidemiological evidence behind the association between periodontitis and incident atherosclerotic cardiovascular disease. J. Periodontol. 2013, 84, S70–S84. [Google Scholar] [CrossRef]
- Ide, M.; Papapanou, P.N. Epidemiology of association between maternal periodontal disease and adverse pregnancy outcomes--systematic review. J. Periodontol. 2013, 84, S181–S194. [Google Scholar] [CrossRef]
- Lee, J.H.; Oh, J.Y.; Youk, T.M.; Jeong, S.N.; Kim, Y.T.; Choi, S.H. Association between periodontal disease and non-communicable diseases: A 12-year longitudinal health-examinee cohort study in South Korea. Medicine 2017, 96, e7398. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, F.C.F.; Marin-Leon, L.; Gomes, E.P.; PedrÃo, A.M.N.; Pereira, A.D.C.; Francisco, P. Relationship between periodontitis and subclinical risk indicators for chronic non-communicable diseases. Braz. Oral Res. 2020, 34, e058. [Google Scholar] [CrossRef] [PubMed]
- Dörfer, C.; Benz, C.; Aida, J.; Campard, G. The relationship of oral health with general health and NCDs: A brief review. Int. Dent. J. 2017, 67 (Suppl. S2), 14–18. [Google Scholar] [CrossRef] [PubMed]
- Wolf, T.G.; Cagetti, M.G.; Fisher, J.M.; Seeberger, G.K.; Campus, G. Non-communicable Diseases and Oral Health: An Overview. Front. Oral Health 2021, 2, 725460. [Google Scholar] [CrossRef]
- Romandini, M.; Baima, G.; Antonoglou, G.; Bueno, J.; Figuero, E.; Sanz, M. Periodontitis, Edentulism, and Risk of Mortality: A Systematic Review with Meta-analyses. J. Dent. Res. 2021, 100, 37–49. [Google Scholar] [CrossRef]
- Gomes-Filho, I.S.; Cruz, S.S.D.; Trindade, S.C.; Passos-Soares, J.S.; Carvalho-Filho, P.C.; Figueiredo, A.; Lyrio, A.O.; Hintz, A.M.; Pereira, M.G.; Scannapieco, F. Periodontitis and respiratory diseases: A systematic review with meta-analysis. Oral Dis. 2020, 26, 439–446. [Google Scholar] [CrossRef]
- Raghavendran, K.; Mylotte, J.M.; Scannapieco, F.A. Nursing home-associated pneumonia, hospital-acquired pneumonia and ventilator-associated pneumonia: The contribution of dental biofilms and periodontal inflammation. Periodontol 2000 2007, 44, 164–177. [Google Scholar] [CrossRef]
- Scannapieco, F.A.; Giuliano, K.K.; Baker, D. Oral health status and the etiology and prevention of nonventilator hospital-associated pneumonia. Periodontol 2000 2022, 89, 51–58. [Google Scholar] [CrossRef]
- Craven, D.E.; Chroneou, A.; Zias, N.; Hjalmarson, K.I. Ventilator-associated tracheobronchitis: The impact of targeted antibiotic therapy on patient outcomes. Chest 2009, 135, 521–528. [Google Scholar] [CrossRef]
- Joseph, N.M.; Sistla, S.; Dutta, T.K.; Badhe, A.S.; Parija, S.C. Ventilator-associated pneumonia: Role of colonizers and value of routine endotracheal aspirate cultures. Int. J. Infect. Dis. 2010, 14, e723–e729. [Google Scholar] [CrossRef]
- Shay, K. Infectious complications of dental and periodontal diseases in the elderly population. Clin. Infect. Dis. 2002, 34, 1215–1223. [Google Scholar] [CrossRef] [PubMed]
- Scannapieco, F.A. Role of oral bacteria in respiratory infection. J. Periodontol. 1999, 70, 793–802. [Google Scholar] [CrossRef] [PubMed]
- Awano, S.; Ansai, T.; Takata, Y.; Soh, I.; Akifusa, S.; Hamasaki, T.; Yoshida, A.; Sonoki, K.; Fujisawa, K.; Takehara, T. Oral health and mortality risk from pneumonia in the elderly. J. Dent. Res. 2008, 87, 334–339. [Google Scholar] [CrossRef] [PubMed]
- Scannapieco, F.A.; Bush, R.B.; Paju, S. Associations between periodontal disease and risk for nosocomial bacterial pneumonia and chronic obstructive pulmonary disease. A systematic review. Ann. Periodontol. 2003, 8, 54–69. [Google Scholar] [CrossRef] [PubMed]
- Cagnani, A.; Barros, A.M.D.S.; Sousa, L.L.A.d.; Zanin, L.; Bergamaschi, C.d.C.; Peruzzo, D.C.; Flório, F.M. Periodontal disease as a risk factor for aspiration pneumonia: A systematic review. Biosci. J. (Online) 2016, 32, 813–821. [Google Scholar] [CrossRef]
- Jerônimo, L.S.; Abreu, L.G.; Cunha, F.A.; Esteves Lima, R.P. Association Between Periodontitis and Nosocomial Pneumonia: A Systematic Review and Meta-analysis of Observational Studies. Oral Health Prev. Dent. 2020, 18, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Marotz, C.; Molinsky, R.; Martino, C.; Bohn, B.; Roy, S.; Rosenbaum, M.; Desvarieux, M.; Yuzefpolskaya, M.; Paster, B.J.; Jacobs, D.R.; et al. Early microbial markers of periodontal and cardiometabolic diseases in ORIGINS. NPJ Biofilms Microbiomes 2022, 8, 30. [Google Scholar] [CrossRef] [PubMed]
- Wiersinga, W.J.; Rhodes, A.; Cheng, A.C.; Peacock, S.J.; Prescott, H.C. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. Jama 2020, 324, 782–793. [Google Scholar] [CrossRef]
- Ruan, Q.; Yang, K.; Wang, W.; Jiang, L.; Song, J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020, 46, 846–848. [Google Scholar] [CrossRef]
- Cheng, V.C.; Wong, S.C.; Chuang, V.W.; So, S.Y.; Chen, J.H.; Sridhar, S.; To, K.K.; Chan, J.F.; Hung, I.F.; Ho, P.L.; et al. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. J. Infect. 2020, 81, 107–114. [Google Scholar] [CrossRef]
- Yang, X.; Yu, Y.; Xu, J.; Shu, H.; Xia, J.; Liu, H.; Wu, Y.; Zhang, L.; Yu, Z.; Fang, M.; et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir. Med. 2020, 8, 475–481. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Krüger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.H.; Nitsche, A.; et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020, 181, 271–280.e8. [Google Scholar] [CrossRef]
- Sungnak, W.; Huang, N.; Bécavin, C.; Berg, M.; Queen, R.; Litvinukova, M.; Talavera-López, C.; Maatz, H.; Reichart, D.; Sampaziotis, F.; et al. SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat. Med. 2020, 26, 681–687. [Google Scholar] [CrossRef]
- Lauer, S.A.; Grantz, K.H.; Bi, Q.; Jones, F.K.; Zheng, Q.; Meredith, H.R.; Azman, A.S.; Reich, N.G.; Lessler, J. The Incubation Period of Coronavirus Disease 2019 (COVID-19) From Publicly Reported Confirmed Cases: Estimation and Application. Ann. Intern. Med. 2020, 172, 577–582. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [PubMed]
- The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19)—China, 2020. China CDC Wkly 2020, 2, 113–122. [Google Scholar] [CrossRef]
- Mehta, P.; McAuley, D.F.; Brown, M.; Sanchez, E.; Tattersall, R.S.; Manson, J.J. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet 2020, 395, 1033–1034. [Google Scholar] [CrossRef] [PubMed]
- Iranmanesh, B.; Khalili, M.; Amiri, R.; Zartab, H.; Aflatoonian, M. Oral manifestations of COVID-19 disease: A review article. Dermatol. Ther. 2021, 34, e14578. [Google Scholar] [CrossRef] [PubMed]
- Darestani, M.N.; Akbari, A.; Yaghobee, S.; Taheri, M.; Akbari, S. COVID-19 Pandemic and Periodontal Practice: The Immunological, Clinical, and Economic Points of View. Biomed. Res. Int. 2022, 2022, 3918980. [Google Scholar] [CrossRef]
- Takahashi, Y.; Watanabe, N.; Kamio, N.; Kobayashi, R.; Iinuma, T.; Imai, K. Aspiration of periodontopathic bacteria due to poor oral hygiene potentially contributes to the aggravation of COVID-19. J. Oral Sci. 2020, 63, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, Y.; Watanabe, N.; Kamio, N.; Yokoe, S.; Suzuki, R.; Sato, S.; Iinuma, T.; Imai, K. Expression of the SARS-CoV-2 Receptor ACE2 and Proinflammatory Cytokines Induced by the Periodontopathic Bacterium Fusobacterium nucleatum in Human Respiratory Epithelial Cells. Int. J. Mol. Sci. 2021, 22, 1352. [Google Scholar] [CrossRef] [PubMed]
- Badran, Z.; Gaudin, A.; Struillou, X.; Amador, G.; Soueidan, A. Periodontal pockets: A potential reservoir for SARS-CoV-2? Med. Hypotheses 2020, 143, 109907. [Google Scholar] [CrossRef] [PubMed]
- Bao, L.; Zhang, C.; Dong, J.; Zhao, L.; Li, Y.; Sun, J. Oral Microbiome and SARS-CoV-2: Beware of Lung Co-infection. Front. Microbiol. 2020, 11, 1840. [Google Scholar] [CrossRef] [PubMed]
- Botros, N.; Iyer, P.; Ojcius, D.M. Is there an association between oral health and severity of COVID-19 complications? Biomed. J. 2020, 43, 325–327. [Google Scholar] [CrossRef]
- Herrera, D.; Serrano, J.; Roldán, S.; Sanz, M. Is the oral cavity relevant in SARS-CoV-2 pandemic? Clin. Oral Investig. 2020, 24, 2925–2930. [Google Scholar] [CrossRef]
- Huang, N.; Pérez, P.; Kato, T.; Mikami, Y.; Okuda, K.; Gilmore, R.C.; Conde, C.D.; Gasmi, B.; Stein, S.; Beach, M.; et al. SARS-CoV-2 infection of the oral cavity and saliva. Nat. Med. 2021, 27, 892–903. [Google Scholar] [CrossRef]
- Xu, H.; Zhong, L.; Deng, J.; Peng, J.; Dan, H.; Zeng, X.; Li, T.; Chen, Q. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int. J. Oral Sci. 2020, 12, 8. [Google Scholar] [CrossRef]
- Xu, J.; Li, Y.; Gan, F.; Du, Y.; Yao, Y. Salivary Glands: Potential Reservoirs for COVID-19 Asymptomatic Infection. J. Dent. Res. 2020, 99, 989. [Google Scholar] [CrossRef]
- Yoon, J.G.; Yoon, J.; Song, J.Y.; Yoon, S.Y.; Lim, C.S.; Seong, H.; Noh, J.Y.; Cheong, H.J.; Kim, W.J. Clinical Significance of a High SARS-CoV-2 Viral Load in the Saliva. J. Korean Med. Sci. 2020, 35, e195. [Google Scholar] [CrossRef]
- Gomes, S.C.; Fachin, S.; da Fonseca, J.G.; Angst, P.D.M.; Lamers, M.L.; da Silva, I.S.B.; Nunes, L.N. Dental biofilm of symptomatic COVID-19 patients harbours SARS-CoV-2. J. Clin. Periodontol. 2021, 48, 880–885. [Google Scholar] [CrossRef]
- Gupta, S.; Mohindra, R.; Chauhan, P.K.; Singla, V.; Goyal, K.; Sahni, V.; Gaur, R.; Verma, D.K.; Ghosh, A.; Soni, R.K.; et al. SARS-CoV-2 Detection in Gingival Crevicular Fluid. J. Dent. Res. 2021, 100, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Fernandes Matuck, B.; Dolhnikoff, M.; Maia, G.V.A.; Isaac Sendyk, D.; Zarpellon, A.; Costa Gomes, S.; Duarte-Neto, A.N.; Rebello Pinho, J.R.; Gomes-Gouvêa, M.S.; Sousa, S.; et al. Periodontal tissues are targets for SARS-CoV-2: A post-mortem study. J. Oral Microbiol. 2020, 13, 1848135. [Google Scholar] [CrossRef] [PubMed]
- Ramseier, C.A.; Anerud, A.; Dulac, M.; Lulic, M.; Cullinan, M.P.; Seymour, G.J.; Faddy, M.J.; Bürgin, W.; Schätzle, M.; Lang, N.P. Natural history of periodontitis: Disease progression and tooth loss over 40 years. J. Clin. Periodontol. 2017, 44, 1182–1191. [Google Scholar] [CrossRef] [PubMed]
- Zang, Y.; Song, J.H.; Oh, S.H.; Kim, J.W.; Lee, M.N.; Piao, X.; Yang, J.W.; Kim, O.S.; Kim, T.S.; Kim, S.H.; et al. Targeting NLRP3 Inflammasome Reduces Age-Related Experimental Alveolar Bone Loss. J. Dent. Res. 2020, 99, 1287–1295. [Google Scholar] [CrossRef] [PubMed]
- Isola, G.; Polizzi, A.; Santonocito, S.; Alibrandi, A.; Williams, R.C. Periodontitis activates the NLRP3 inflammasome in serum and saliva. J. Periodontol. 2022, 93, 135–145. [Google Scholar] [CrossRef]
- Toldo, S.; Bussani, R.; Nuzzi, V.; Bonaventura, A.; Mauro, A.G.; Cannatà, A.; Pillappa, R.; Sinagra, G.; Nana-Sinkam, P.; Sime, P.; et al. Inflammasome formation in the lungs of patients with fatal COVID-19. Inflamm. Res. 2021, 70, 7–10. [Google Scholar] [CrossRef]
- van den Berg, D.F.; Te Velde, A.A. Severe COVID-19: NLRP3 Inflammasome Dysregulated. Front. Immunol. 2020, 11, 1580. [Google Scholar] [CrossRef]
- Zhao, Z.; Wei, Y.; Tao, C. An enlightening role for cytokine storm in coronavirus infection. Clin. Immunol. 2021, 222, 108615. [Google Scholar] [CrossRef]
- Gupta, S.; Sahni, V. The intriguing commonality of NETosis between COVID-19 & Periodontal disease. Med. Hypotheses 2020, 144, 109968. [Google Scholar] [CrossRef]
- Bhaskar, S.; Sinha, A.; Banach, M.; Mittoo, S.; Weissert, R.; Kass, J.S.; Rajagopal, S.; Pai, A.R.; Kutty, S. Cytokine Storm in COVID-19-Immunopathological Mechanisms, Clinical Considerations, and Therapeutic Approaches: The REPROGRAM Consortium Position Paper. Front. Immunol. 2020, 11, 1648. [Google Scholar] [CrossRef]
- Elisetti, N. Periodontal pocket and COVID-19: Could there be a possible link? Med. Hypotheses 2021, 146, 110355. [Google Scholar] [CrossRef] [PubMed]
- Mulchandani, R.; Lyngdoh, T.; Kakkar, A.K. Deciphering the COVID-19 cytokine storm: Systematic review and meta-analysis. Eur. J. Clin. Investig. 2021, 51, e13429. [Google Scholar] [CrossRef] [PubMed]
- Sahni, V.; Gupta, S. COVID-19 & Periodontitis: The cytokine connection. Med. Hypotheses 2020, 144, 109908. [Google Scholar] [CrossRef] [PubMed]
- Magán-Fernández, A.; O’Valle, F.; Abadía-Molina, F.; Muñoz, R.; Puga-Guil, P.; Mesa, F. Characterization and comparison of neutrophil extracellular traps in gingival samples of periodontitis and gingivitis: A pilot study. J. Periodontal Res. 2019, 54, 218–224. [Google Scholar] [CrossRef]
- Magán-Fernández, A.; Rasheed Al-Bakri, S.M.; O’Valle, F.; Benavides-Reyes, C.; Abadía-Molina, F.; Mesa, F. Neutrophil Extracellular Traps in Periodontitis. Cells 2020, 9, 1494. [Google Scholar] [CrossRef]
- Coomes, E.A.; Haghbayan, H. Interleukin-6 in COVID-19: A systematic review and meta-analysis. Rev. Med. Virol. 2020, 30, 1–9. [Google Scholar] [CrossRef]
- Lloyd-Jones, G.; Molayem, S.; Pontes, C.C.; Chapple, I. The COVID-19 pathway: A proposed oral-vascular-pulmonary route of SARS-CoV-2 infection and the importance of oral healthcare measures. J. Oral Med. Dent. Res. 2021, 2, 1–25. [Google Scholar] [CrossRef]
- Kara, C.; Çelen, K.; Dede, F.; Gökmenoğlu, C.; Kara, N.B. Is periodontal disease a risk factor for developing severe COVID-19 infection? The potential role of Galectin-3. Exp. Biol. Med. 2020, 245, 1425–1427. [Google Scholar] [CrossRef]
- Caniglia, J.L.; Guda, M.R.; Asuthkar, S.; Tsung, A.J.; Velpula, K.K. A potential role for Galectin-3 inhibitors in the treatment of COVID-19. PeerJ 2020, 8, e9392. [Google Scholar] [CrossRef]
- Sehirli, A.; Chukwunyere, U.; Aksoy, U.; Sayiner, S.; Abacioglu, N. The circadian clock gene Bmal1: Role in COVID-19 and periodontitis. Chronobiol. Int. 2021, 38, 779–784. [Google Scholar] [CrossRef]
- Marouf, N.; Cai, W.; Said, K.N.; Daas, H.; Diab, H.; Chinta, V.R.; Hssain, A.A.; Nicolau, B.; Sanz, M.; Tamimi, F. Association between periodontitis and severity of COVID-19 infection: A case-control study. J. Clin. Periodontol. 2021, 48, 483–491. [Google Scholar] [CrossRef]
- Anand, P.S.; Jadhav, P.; Kamath, K.P.; Kumar, S.R.; Vijayalaxmi, S.; Anil, S. A case-control study on the association between periodontitis and coronavirus disease (COVID-19). J. Periodontol. 2022, 93, 584–590. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Mohindra, R.; Singla, M.; Khera, S.; Sahni, V.; Kanta, P.; Soni, R.K.; Kumar, A.; Gauba, K.; Goyal, K.; et al. The clinical association between Periodontitis and COVID-19. Clin. Oral Investig. 2022, 26, 1361–1374. [Google Scholar] [CrossRef] [PubMed]
- Sirin, D.A.; Ozcelik, F. The relationship between COVID-19 and the dental damage stage determined by radiological examination. Oral Radiol. 2021, 37, 600–609. [Google Scholar] [CrossRef] [PubMed]
- Larvin, H.; Wilmott, S.; Wu, J.; Kang, J. The Impact of Periodontal Disease on Hospital Admission and Mortality During COVID-19 Pandemic. Front. Med. 2020, 7, 604980. [Google Scholar] [CrossRef]
- Katz, J.; Yue, S.; Xue, W. Dental diseases are associated with increased odds ratio for coronavirus disease 19. Oral Dis. 2022, 28, 991–993. [Google Scholar] [CrossRef]
- Wang, Y.; Deng, H.; Pan, Y.; Jin, L.; Hu, R.; Lu, Y.; Deng, W.; Sun, W.; Chen, C.; Shen, X.; et al. Periodontal disease increases the host susceptibility to COVID-19 and its severity: A Mendelian randomization study. J. Transl. Med. 2021, 19, 528. [Google Scholar] [CrossRef] [PubMed]
- Pitones-Rubio, V.; Chávez-Cortez, E.G.; Hurtado-Camarena, A.; González-Rascón, A.; Serafín-Higuera, N. Is periodontal disease a risk factor for severe COVID-19 illness? Med. Hypotheses 2020, 144, 109969. [Google Scholar] [CrossRef]
- Tamimi, F.; Altigani, S.; Sanz, M. Periodontitis and coronavirus disease 2019. Periodontol 2000 2022, 89, 207–214. [Google Scholar] [CrossRef]
- Baima, G.; Marruganti, C.; Sanz, M.; Aimetti, M.; Romandini, M. Periodontitis and COVID-19: Biological Mechanisms and Meta-analyses of Epidemiological Evidence. J. Dent. Res. 2022, 101, 1430–1440. [Google Scholar] [CrossRef]
- Sampson, V.; Kamona, N.; Sampson, A. Could there be a link between oral hygiene and the severity of SARS-CoV-2 infections? Br. Dent. J. 2020, 228, 971–975. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, I.; Maity, P. COVID-19 outbreak: Migration, effects on society, global environment and prevention. Sci. Total Environ. 2020, 728, 138882. [Google Scholar] [CrossRef] [PubMed]
- Kamel, A.H.M.; Basuoni, A.; Salem, Z.A.; AbuBakr, N. The impact of oral health status on COVID-19 severity, recovery period and C-reactive protein values. Br. Dent. J. 2021, 1–7. [Google Scholar] [CrossRef]
- Sari, A.; Bilmez, Z.Y. Effects of Coronavirus (COVID-19) Fear on Oral Health Status. Oral Health Prev. Dent 2021, 19, 411–423. [Google Scholar] [CrossRef]
- Patel, J.; Woolley, J. Necrotizing periodontal disease: Oral manifestation of COVID-19. Oral Dis. 2021, 27 (Suppl. S3), 768–769. [Google Scholar] [CrossRef]
- Castro, J.P.; El-Atat, F.A.; McFarlane, S.I.; Aneja, A.; Sowers, J.R. Cardiometabolic syndrome: Pathophysiology and treatment. Curr. Hypertens. Rep. 2003, 5, 393–401. [Google Scholar] [CrossRef]
- Rizzo, M.; Cappello, F.; Marfil, R.; Nibali, L.; Marino Gammazza, A.; Rappa, F.; Bonaventura, G.; Galindo-Moreno, P.; O’Valle, F.; Zummo, G.; et al. Heat-shock protein 60 kDa and atherogenic dyslipidemia in patients with untreated mild periodontitis: A pilot study. Cell Stress Chaperones 2012, 17, 399–407. [Google Scholar] [CrossRef] [PubMed]
- Hajishengallis, G.; Chavakis, T. Local and systemic mechanisms linking periodontal disease and inflammatory comorbidities. Nat. Rev. Immunol. 2021, 21, 426–440. [Google Scholar] [CrossRef]
- Hajishengallis, G. Interconnection of periodontal disease and comorbidities: Evidence, mechanisms, and implications. Periodontol 2000 2022, 89, 9–18. [Google Scholar] [CrossRef]
- Pussinen, P.J.; Kopra, E.; Pietiäinen, M.; Lehto, M.; Zaric, S.; Paju, S.; Salminen, A. Periodontitis and cardiometabolic disorders: The role of lipopolysaccharide and endotoxemia. Periodontol 2000 2022, 89, 19–40. [Google Scholar] [CrossRef]
- Liljestrand, J.M.; Paju, S.; Buhlin, K.; Persson, G.R.; Sarna, S.; Nieminen, M.S.; Sinisalo, J.; Mäntylä, P.; Pussinen, P.J. Lipopolysaccharide, a possible molecular mediator between periodontitis and coronary artery disease. J. Clin. Periodontol. 2017, 44, 784–792. [Google Scholar] [CrossRef]
- Mustapha, I.Z.; Debrey, S.; Oladubu, M.; Ugarte, R. Markers of systemic bacterial exposure in periodontal disease and cardiovascular disease risk: A systematic review and meta-analysis. J. Periodontol. 2007, 78, 2289–2302. [Google Scholar] [CrossRef] [PubMed]
- Tonetti, M.S.; D’Aiuto, F.; Nibali, L.; Donald, A.; Storry, C.; Parkar, M.; Suvan, J.; Hingorani, A.D.; Vallance, P.; Deanfield, J. Treatment of periodontitis and endothelial function. N. Engl. J. Med. 2007, 356, 911–920. [Google Scholar] [CrossRef] [PubMed]
- Zemedikun, D.T.; Chandan, J.S.; Raindi, D.; Rajgor, A.D.; Gokhale, K.M.; Thomas, T.; Falahee, M.; De Pablo, P.; Lord, J.M.; Raza, K.; et al. Burden of chronic diseases associated with periodontal diseases: A retrospective cohort study using UK primary care data. BMJ Open 2021, 11, e048296. [Google Scholar] [CrossRef] [PubMed]
- Bielecka-Dabrowa, A.; Cichocka-Radwan, A.; Lewek, J.; Pawliczak, F.; Maciejewski, M.; Banach, M. Cardiac manifestations of COVID-19. Rev. Cardiovasc. Med. 2021, 22, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Jensterle, M.; Herman, R.; Janež, A.; Mahmeed, W.A.; Al-Rasadi, K.; Al-Alawi, K.; Banach, M.; Banerjee, Y.; Ceriello, A.; Cesur, M.; et al. The Relationship between COVID-19 and Hypothalamic-Pituitary-Adrenal Axis: A Large Spectrum from Glucocorticoid Insufficiency to Excess-The CAPISCO International Expert Panel. Int. J. Mol. Sci. 2022, 23, 7326. [Google Scholar] [CrossRef]
- Ceriello, A.; Stoian, A.P.; Rizzo, M. COVID-19 and diabetes management: What should be considered? Diabetes Res. Clin. Pract. 2020, 163, 108151. [Google Scholar] [CrossRef]
- Stoian, A.P.; Banerjee, Y.; Rizvi, A.A.; Rizzo, M. Diabetes and the COVID-19 Pandemic: How Insights from Recent Experience Might Guide Future Management. Metab. Syndr. Relat. Disord. 2020, 18, 173–175. [Google Scholar] [CrossRef]
- Stoian, A.P.; Kempler, P.; Stulnig, T.; Rizvi, A.A.; Rizzo, M. Diabetes and COVID-19: What 2 Years of the Pandemic Has Taught Us. Metab. Syndr. Relat. Disord. 2022, 20, 137–140. [Google Scholar] [CrossRef]
- Rizvi, A.A.; Janez, A.; Rizzo, M. Cardiometabolic Alterations in the Interplay of COVID-19 and Diabetes: Current Knowledge and Future Avenues. Int. J. Mol. Sci. 2021, 22, 12311. [Google Scholar] [CrossRef] [PubMed]
- Rizvi, A.A.; Stoian, A.P.; Lessan, N.; Rizzo, M. Endocrinology in the Time of COVID-19: A Rapid Evolution of Knowledge and Care. Medicina 2021, 57, 805. [Google Scholar] [CrossRef] [PubMed]
- Mechanick, J.I.; Rosenson, R.S.; Pinney, S.P.; Mancini, D.M.; Narula, J.; Fuster, V. Coronavirus and Cardiometabolic Syndrome: JACC Focus Seminar. J. Am. Coll. Cardiol. 2020, 76, 2024–2035. [Google Scholar] [CrossRef]
- Yang, L.; Nilsson-Payant, B.E.; Han, Y.; Jaffré, F.; Zhu, J.; Wang, P.; Zhang, T.; Redmond, D.; Houghton, S.; Møller, R.; et al. Cardiomyocytes recruit monocytes upon SARS-CoV-2 infection by secreting CCL2. Stem Cell Rep. 2021, 16, 2274–2288. [Google Scholar] [CrossRef] [PubMed]
- Tang, X.; Uhl, S.; Zhang, T.; Xue, D.; Li, B.; Vandana, J.J.; Acklin, J.A.; Bonnycastle, L.L.; Narisu, N.; Erdos, M.R.; et al. SARS-CoV-2 infection induces beta cell transdifferentiation. Cell Metab. 2021, 33, 1577–1591.e1577. [Google Scholar] [CrossRef] [PubMed]
- Reiterer, M.; Rajan, M.; Gómez-Banoy, N.; Lau, J.D.; Gomez-Escobar, L.G.; Ma, L.; Gilani, A.; Alvarez-Mulett, S.; Sholle, E.T.; Chandar, V.; et al. Hyperglycemia in acute COVID-19 is characterized by insulin resistance and adipose tissue infectivity by SARS-CoV-2. Cell Metab. 2021, 33, 2174–2188.e2175. [Google Scholar] [CrossRef]
- Svensson, P.; Hofmann, R.; Häbel, H.; Jernberg, T.; Nordberg, P. Association between cardiometabolic disease and severe COVID-19: A nationwide case-control study of patients requiring invasive mechanical ventilation. BMJ Open 2021, 11, e044486. [Google Scholar] [CrossRef]
- Patel, K.H.K.; Li, X.; Quint, J.K.; Ware, J.S.; Peters, N.S.; Ng, F.S. Increasing adiposity and the presence of cardiometabolic morbidity is associated with increased COVID-19-related mortality: Results from the UK Biobank. BMC Endocr. Disord. 2021, 21, 144. [Google Scholar] [CrossRef]
- Nalbandian, A.; Sehgal, K.; Gupta, A.; Madhavan, M.V.; McGroder, C.; Stevens, J.S.; Cook, J.R.; Nordvig, A.S.; Shalev, D.; Sehrawat, T.S.; et al. Post-acute COVID-19 syndrome. Nat. Med. 2021, 27, 601–615. [Google Scholar] [CrossRef]
- Venkatesan, P. NICE guideline on long COVID. Lancet Respir. Med. 2021, 9, 129. [Google Scholar] [CrossRef]
- Mehandru, S.; Merad, M. Pathological sequelae of long-haul COVID. Nat. Immunol. 2022, 23, 194–202. [Google Scholar] [CrossRef]
- Rezel-Potts, E.; Douiri, A.; Sun, X.; Chowienczyk, P.J.; Shah, A.M.; Gulliford, M.C. Cardiometabolic outcomes up to 12 months after COVID-19 infection. A matched cohort study in the UK. PLoS Med. 2022, 19, e1004052. [Google Scholar] [CrossRef] [PubMed]
- Al Mahmeed, W.; Al-Rasadi, K.; Banerjee, Y.; Ceriello, A.; Cosentino, F.; Galia, M.; Goh, S.Y.; Kempler, P.; Lessan, N.; Papanas, N.; et al. Promoting a Syndemic Approach for Cardiometabolic Disease Management During COVID-19: The CAPISCO International Expert Panel. Front. Cardiovasc. Med. 2021, 8, 787761. [Google Scholar] [CrossRef]
- Nuzzo, D.; Vasto, S.; Scalisi, L.; Cottone, S.; Cambula, G.; Rizzo, M.; Giacomazza, D.; Picone, P. Post-Acute COVID-19 Neurological Syndrome: A New Medical Challenge. J. Clin. Med. 2021, 10, 1947. [Google Scholar] [CrossRef] [PubMed]
- Pantelis, C.; Jayaram, M.; Hannan, A.J.; Wesselingh, R.; Nithianantharajah, J.; Wannan, C.M.; Syeda, W.T.; Choy, K.C.; Zantomio, D.; Christopoulos, A.; et al. Neurological, neuropsychiatric and neurodevelopmental complications of COVID-19. Aust. N. Z. J. Psychiatr. 2021, 55, 750–762. [Google Scholar] [CrossRef] [PubMed]
- Nibali, L.; Tatarakis, N.; Needleman, I.; Tu, Y.K.; D’Aiuto, F.; Rizzo, M.; Donos, N. Clinical review: Association between metabolic syndrome and periodontitis: A systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 2013, 98, 913–920. [Google Scholar] [CrossRef]
- Mesa, F.; Magan-Fernandez, A.; Castellino, G.; Chianetta, R.; Nibali, L.; Rizzo, M. Periodontitis and mechanisms of cardiometabolic risk: Novel insights and future perspectives. Biochim. Biophys. Acta Mol. Basis Dis. 2019, 1865, 476–484. [Google Scholar] [CrossRef]
- Mainas, G.; Ide, M.; Rizzo, M.; Magan-Fernandez, A.; Mesa, F.; Nibali, L. Managing the Systemic Impact of Periodontitis. Medicina 2022, 58, 621. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).