A Company Is Only as Healthy as Its Workers: A 6-Month Metabolic Health Management Pilot Program Improves Employee Health and Contributes to Cost Savings
Abstract
:1. Introduction
2. Materials and Methods
2.1. Establishment of an Employee Metabolic Health Management Program
2.2. Patient Enrollment, Consent, and Completion
2.3. In-Clinic Baseline and Quarterly Assessments
2.4. At-Home Monitoring
2.5. Team-Based, Patient-Centered, Asynchronous, Community-Orientated Medicine
2.6. Statistics
3. Results
3.1. Baseline Characteristics
3.2. Main Results
3.3. Deprescription and Estimated Cost Savings
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Glossary
| ACC | American College of Cardiology |
| AHA | American Heart Association |
| CGM | Continuous glucose monitor |
| CRP | C-reactive protein |
| HbA1c | glycated hemoglobin |
| HDL-C | HDL cholesterol |
| HOMA-IR | homeostatic model of insulin resistance |
| LDL-C | LDL cholesterol |
References
- Type 2 Diabetes. 2021. Available online: https://www.cdc.gov/diabetes/basics/type2.html (accessed on 1 July 2022).
- Cost-Effectiveness of Diabetes Interventions. 2022. Available online: https://www.cdc.gov/chronicdisease/programs-impact/pop/diabetes.htm (accessed on 5 July 2022).
- American Diabetes Association. Economic Costs of Diabetes in the U.S. in 2017. Diabetes Care 2018, 41, 917–928.
- Tremmel, M.; Gerdtham, U.-G.; Nilsson, P.M.; Saha, S. Economic Burden of Obesity: A Systematic Literature Review. Int. J. Environ. Res. Public Health 2017, 14, 435. [Google Scholar] [CrossRef]
- Finkelstein, E.; Fiebelkorn, I.C.; Wang, G. The costs of obesity among full-time employees. Am. J. Health Promot. 2005, 20, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Okunogbe, A.; Nugent, R.; Spencer, G.; Ralston, J.; Wilding, J. Economic impacts of overweight and obesity: Current and future estimates for eight countries. BMJ Glob. Health 2021, 6, e006351. [Google Scholar] [CrossRef] [PubMed]
- Indrajeet, P. Visualizations with statistical details: The ‘ggstatsplot’ approach. J. Open Source Softw. 2021, 6, 3167. [Google Scholar]
- Goff, D.C., Jr.; Lloyd-Jones, D.M.; Bennett, G.; Coady, S.; D’agostino, R.B.; Gibbons, R.; Greenland, P.; Lackland, D.T.; Levy, D.; O’donnell, C.J.; et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2014, 63, 2935–2959. [Google Scholar] [CrossRef]
- Ebbeling, C.B.; Knapp, A.; Johnson, A.; Wong, J.M.W.; Greco, K.F.; Ma, C.; Mora, S.; Ludwig, D.S. Effects of a low-carbohydrate diet on insulin-resistant dyslipoproteinemia-a randomized controlled feeding trial. Am. J. Clin. Nutr. 2022, 115, 154–162. [Google Scholar] [CrossRef] [PubMed]
- Hyde, P.N.; Sapper, T.N.; Crabtree, C.D.; LaFountain, R.A.; Bowling, M.L.; Buga, A.; Fell, B.; McSwiney, F.T.; Dickerson, R.M.; Miller, V.J.; et al. Dietary carbohydrate restriction improves metabolic syndrome independent of weight loss. JCI Insight 2019, 4, e128308. [Google Scholar] [CrossRef] [PubMed]
- Jayedi, A.; Zeraattalab-Motlagh, S.; Jabbarzadeh, B.; Hosseini, Y.; Jibril, A.T.; Shahinfar, H.; Mirrafiei, A.; Hosseini, F.; Bidar, S.S. Dose-dependent effect of carbohydrate restriction for type 2 diabetes management: A systematic review and dose-response meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2022, 116, 40–56. [Google Scholar] [CrossRef] [PubMed]
- Unwin, D.; Khalid, A.A.; Unwin, J.; Crocombe, D.; Delon, C.; Martyn, K.; Golubic, R.; Ray, S. Insights from a general practice service evaluation supporting a lower carbohydrate diet in patients with type 2 diabetes mellitus and prediabetes: A secondary analysis of routine clinic data including HbA1c, weight and prescribing over 6 years. BMJ Nutr. Prev. Health 2020, 3, 285–294. [Google Scholar] [CrossRef] [PubMed]
- Athinarayanan, S.J.; Adams, R.N.; Hallberg, S.J.; McKenzie, A.L.; Bhanpuri, N.H.; Campbell, W.W.; Volek, J.S.; Phinney, S.D.; McCarter, J.P. Long-Term Effects of a Novel Continuous Remote Care Intervention Including Nutritional Ketosis for the Management of Type 2 Diabetes: A 2-Year Non-randomized Clinical Trial. Front. Endocrinol. 2019, 10, 348. [Google Scholar] [CrossRef] [PubMed]
- Nicholas, A.P.; Soto-Mota, A.; Lambert, H.; Collins, A.L. Restricting carbohydrates and calories in the treatment of type 2 diabetes: A systematic review of the effectiveness of ‘low-carbohydrate’ interventions with differing energy levels. J. Nutr. Sci. 2021, 10, e76. [Google Scholar] [CrossRef] [PubMed]
- Rubinstein, A.; Colantonio, L.; Bardach, A.; Caporale, J.; Martí, S.G.; Kopitowski, K.; Alcaraz, A.; Gibbons, L.; Augustovski, F.; Pichón-Rivière, A. Estimation of the burden of cardiovascular disease attributable to modifiable risk factors and cost-effectiveness analysis of preventative interventions to reduce this burden in Argentina. BMC Public Health 2010, 10, 627. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Baseline | 12 Weeks (Q1) | 24 Weeks | Change | |||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Age | 52.9 | 5.7 | ||||||
| BMI | 48.3 | 6.8 | 44.5 | 6.3 | 41.7 | 4.8 | −6.5 *** | 2.9 |
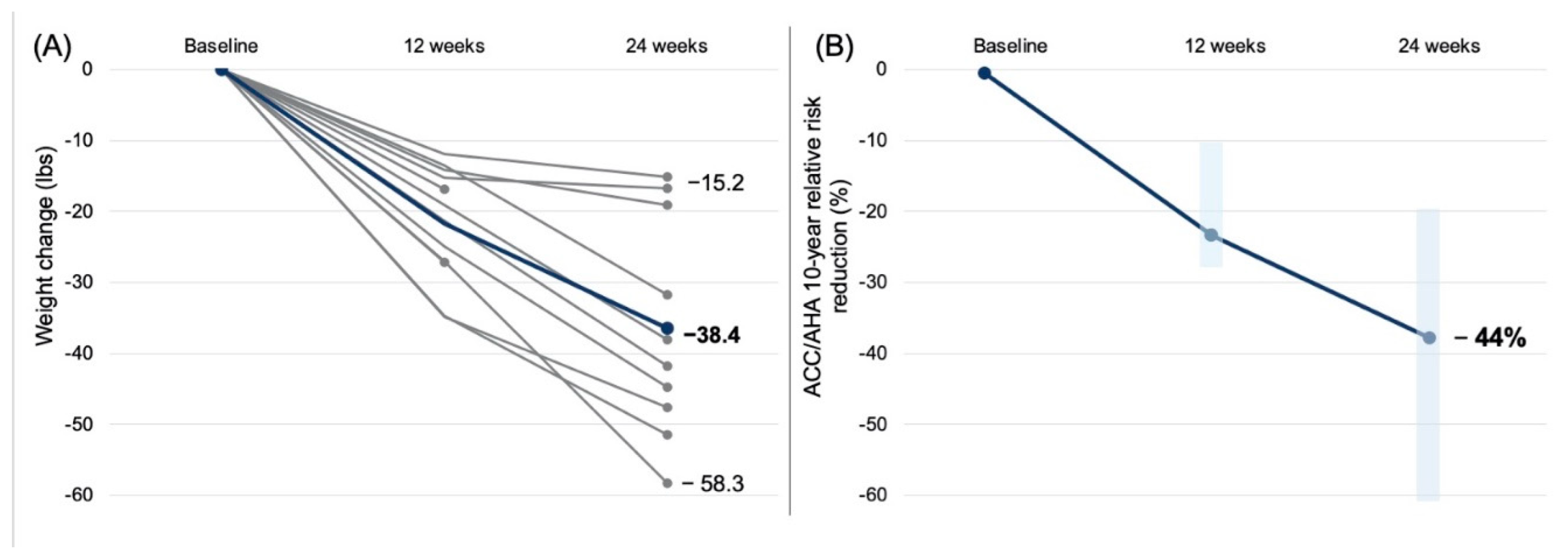
| Weight, lbs (kg) | 290.5 (131.8) | 44.9 (20.4) | 268.0 (121.6) | 44.2 (20.2) | 252.1 (114.4) | 41.1 (18.6) | −38.4 *** (−17.4) | 14.8 (6.7) |
| Fasting glucose | 145 | 45 | 119 | 19 | 110 | 21 | −35 ** | 35 |
| HbA1C | 7.1 | 1.4 | 6.4 | 0.9 | 6.0 | 0.6 | −1.1 *** | 1.4 |
| Total cholesterol | 182 | 32 | 155 | 20 | 175 | 51 | −7 | 47 |
| HDL-C | 44 | 10 | 40 | 8 | 42 | 7 | −2 | 6 |
| LDL-C | 107 | 31 | 97 | 22 | 114 | 49 | −6.3 | 43 |
| Trigs | 165 | 75 | 110 | 39 | 105 | 36 | −60 ** | 64 |
| Systolic BP | 141 | 13 | 130 | 9 | 124 | 10 | −17 * | 17 |
| Diastolic BP | 83 | 7 | 81 | 8 | 78 | 8 | −6 | 12 |
| ACC/AHA 10-year risk (absolute, %) | 9.2 | 9.7 | 7.2 | 6.9 | 5.2 | 7.3 | −4.0 * | 5.6 |
| ACC/AHA 10-year risk (relative change, %) | −44 * | 24 | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Norwitz, N.G.; Soto-Mota, A.; Kalayjian, T. A Company Is Only as Healthy as Its Workers: A 6-Month Metabolic Health Management Pilot Program Improves Employee Health and Contributes to Cost Savings. Metabolites 2022, 12, 848. https://doi.org/10.3390/metabo12090848
Norwitz NG, Soto-Mota A, Kalayjian T. A Company Is Only as Healthy as Its Workers: A 6-Month Metabolic Health Management Pilot Program Improves Employee Health and Contributes to Cost Savings. Metabolites. 2022; 12(9):848. https://doi.org/10.3390/metabo12090848
Chicago/Turabian StyleNorwitz, Nicholas G., Adrian Soto-Mota, and Tro Kalayjian. 2022. "A Company Is Only as Healthy as Its Workers: A 6-Month Metabolic Health Management Pilot Program Improves Employee Health and Contributes to Cost Savings" Metabolites 12, no. 9: 848. https://doi.org/10.3390/metabo12090848
APA StyleNorwitz, N. G., Soto-Mota, A., & Kalayjian, T. (2022). A Company Is Only as Healthy as Its Workers: A 6-Month Metabolic Health Management Pilot Program Improves Employee Health and Contributes to Cost Savings. Metabolites, 12(9), 848. https://doi.org/10.3390/metabo12090848








