Comparing Levels of Metabolic Predictors of Coronary Heart Disease between Healthy Lean and Overweight Females
Abstract
1. Introduction
2. Results
2.1. General Characteristics of Participants
2.2. Classical CHD Traits Associated with Overweight
2.3. CHD Metabolites Associated with Being Overweight
2.4. Validation of the Identified CHD Biomarkers Differentiating BMI Groups in an Independent Cohort
2.5. Classical Risk Factors Associated with CHD Metabolites Differentiating Lean from Overweight Females
3. Discussion
4. Materials and Methods
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lozano, R.; Naghavi, M.; Foreman, K.; Lim, S.; Shibuya, K.; Aboyans, V.; Abraham, J.; Adair, T.; Aggarwal, R.; Ahn, S.Y.; et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2095–2128. [Google Scholar] [CrossRef]
- Abdelaal, M.; le Roux, C.W.; Docherty, N.G. Morbidity and mortality associated with obesity. Ann. Transl. Med. 2017, 5, 161. [Google Scholar] [CrossRef] [PubMed]
- Cercato, C.; Fonseca, F.A. Cardiovascular risk and obesity. Diabetol. Metab. Syndr. 2019, 11, 74. [Google Scholar] [CrossRef]
- Khan, S.S.; Ning, H.; Wilkins, J.T.; Allen, N.; Carnethon, M.; Berry, J.D.; Sweis, R.N.; Lloyd-Jones, D.M. Association of Body Mass Index With Lifetime Risk of Cardiovascular Disease and Compression of Morbidity. JAMA Cardiol. 2018, 3, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Wilson, P.W.; D’Agostino, R.B.; Sullivan, L.; Parise, H.; Kannel, W.B. Overweight and obesity as determinants of cardiovascular risk: The Framingham experience. Arch. Intern. Med. 2002, 162, 1867–1872. [Google Scholar] [CrossRef]
- Folsom, A.R. Classical and novel biomarkers for cardiovascular risk prediction in the United States. J. Epidemiol. 2013, 23, 158–162. [Google Scholar] [CrossRef]
- Yu, L.; Li, K.; Zhang, X. Next-generation metabolomics in lung cancer diagnosis, treatment and precision medicine: Mini review. Oncotarget 2017, 8. [Google Scholar] [CrossRef]
- Rasmiena, A.A.; Theodore, W.N.; Meikle, P.J. Metabolomics and ischaemic heart disease. Clin. Sci. 2013, 124, 289–306. [Google Scholar] [CrossRef]
- Al-Sulaiti, H.; Diboun, I.; Banu, S.; Al-Emadi, M.; Amani, P.; Harvey, T.M.; Domling, A.S.; Latiff, A.; Elrayess, M.A. Triglyceride profiling in adipose tissues from obese insulin sensitive, insulin resistant and type 2 diabetes mellitus individuals. J. Transl. Med. 2018, 16, 175. [Google Scholar] [CrossRef]
- Al-Khelaifi, F.; Donati, F.; Botre, F.; Latiff, A.; Abraham, D.; Hingorani, A.; Georgakopoulos, C.; Suhre, K.; Yousri, N.A.; Elrayess, M.A. Metabolic profiling of elite athletes with different cardiovascular demand. Scand. J. Med. Sci. Sports 2019, 29, 933–943. [Google Scholar] [CrossRef]
- Al-Sulaiti, H.; Diboun, I.; Agha, M.V.; Mohamed, F.F.S.; Atkin, S.; Domling, A.S.; Elrayess, M.A.; Mazloum, N.A. Metabolic signature of obesity-associated insulin resistance and type 2 diabetes. J. Transl. Med. 2019, 17, 348. [Google Scholar] [CrossRef] [PubMed]
- Diboun, I.; Al-Mansoori, L.; Al-Jaber, H.; Albagha, O.; Elrayess, M.A. Metabolomics of lean/overweight insulin resistant females reveals alterations in steroids and fatty acids. J. Clin. Endocrinol. Metab. 2020, 106, e638–e649. [Google Scholar] [CrossRef]
- Deidda, M.; Piras, C.; Dessalvi, C.C.; Congia, D.; Locci, E.; Ascedu, F.; De Candia, G.; Cadeddu, M.; Lai, G.; Pirisi, R.; et al. Blood metabolomic fingerprint is distinct in healthy coronary and in stenosing or microvascular ischemic heart disease. J. Transl. Med. 2017, 15, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Ussher, J.R.; Elmariah, S.; Gerszten, R.E.; Dyck, J.R.B. The Emerging Role of Metabolomics in the Diagnosis and Prognosis of Cardiovascular Disease. J. Am. Coll. Cardiol. (JACC) 2016, 68, 2850–2870. [Google Scholar] [CrossRef]
- Wang, Z.; Zhu, C.; Nambi, V.; Morrison, A.C.; Folsom, A.R.; Ballantyne, C.M.; Boerwinkle, E.; Yu, B. Metabolomic Pattern Predicts Incident Coronary Heart Disease. Arter. Thromb. Vasc. Biol. 2019, 39, 1475–1482. [Google Scholar] [CrossRef] [PubMed]
- Al-Khelaifi, F.; Diboun, I.; Donati, F.; Botre, F.; Alsayrafi, M.; Georgakopoulos, C.; Suhre, K.; Yousri, N.A.; Elrayess, M.A. A pilot study comparing the metabolic profiles of elite-level athletes from different sporting disciplines. Sports Med. Open 2018, 4, 2. [Google Scholar] [CrossRef]
- Evans, A.M.; Bridgewater, B.R.; Liu, Q.; Mitchell, M.W.; Robinson, R.J.; Dai, H.; Stewart, S.J.; DeHaven, C.D.; Miller, L.A.D. High Resolution Mass Spectrometry Improves Data Quantity and Quality as Compared to Unit Mass Resolution Mass Spectrometry in High- Throughput Profiling Metabolomics. Metabolomics 2014, 4. [Google Scholar] [CrossRef]
- Drake, K.J.; Sidorov, V.Y.; McGuinness, O.P.; Wasserman, D.H.; Wikswo, J.P. Amino acids as metabolic substrates during cardiac ischemia. Exp. Biol. Med. 2012, 237, 1369–1378. [Google Scholar] [CrossRef] [PubMed]
- Svingen, G.F.; Ueland, P.M.; Pedersen, E.K.; Schartum-Hansen, H.; Seifert, R.; Ebbing, M.; Loland, K.H.; Tell, G.S.; Nygard, O. Plasma dimethylglycine and risk of incident acute myocardial infarction in patients with stable angina pectoris. Arter. Thromb. Vasc. Biol. 2013, 33, 2041–2048. [Google Scholar] [CrossRef]
- Zhang, J.; Fan, J.; Venneti, S.; Cross, J.R.; Takagi, T.; Bhinder, B.; Djaballah, H.; Kanai, M.; Cheng, E.H.; Judkins, A.R.; et al. Asparagine plays a critical role in regulating cellular adaptation to glutamine depletion. Mol. Cell 2014, 56, 205–218. [Google Scholar] [CrossRef]
- Graber, C.D.; Goust, J.M.; Glassman, A.D.; Kendall, R.; Loadholt, C.B. Immunomodulating properties of dimethylglycine in humans. J. Infect. Dis. 1981, 143, 101–105. [Google Scholar] [CrossRef] [PubMed]
- McCann, A.; Giil, L.M.; Ulvik, A.; Seifert, R.; Rebnord, E.W.; Pedersen, E.R.; Tveitevåg Svingen, G.F.; Meyer, K.; Strand, E.; Dankel, S.; et al. Plasma Amino Acids and Incident Type 2 Diabetes in Patients With Coronary Artery Disease. Diabetes Care 2019, 42, 1225–1233. [Google Scholar] [CrossRef]
- Lever, M.; George, P.M.; Elmslie, J.L.; Atkinson, W.; Slow, S.; Molyneux, S.L.; Troughton, R.W.; Richards, A.M.; Frampton, C.M.; Chambers, S.T. Betaine and Secondary Events in an Acute Coronary Syndrome Cohort. PLoS ONE 2012, 7, e37883. [Google Scholar] [CrossRef]
- Sokola-Wysoczanska, E.; Wysoczanski, T.; Wagner, J.; Czyz, K.; Bodkowski, R.; Lochynski, S.; Patkowska-Sokola, B. Polyunsaturated Fatty Acids and Their Potential Therapeutic Role in Cardiovascular System Disorders-A Review. Nutrients 2018, 10, 1561. [Google Scholar] [CrossRef]
- Toledo, E.; Wang, D.D.; Ruiz-Canela, M.; Clish, C.B.; Razquin, C.; Zheng, Y.; Guasch-Ferre, M.; Hruby, A.; Corella, D.; Gomez-Gracia, E.; et al. Plasma lipidomic profiles and cardiovascular events in a randomized intervention trial with the Mediterranean diet. Am. J. Clin. Nutr 2017, 106, 973–983. [Google Scholar] [CrossRef] [PubMed]
- Stegemann, C.; Pechlaner, R.; Willeit, P.; Langley, S.R.; Mangino, M.; Mayr, U.; Menni, C.; Moayyeri, A.; Santer, P.; Rungger, G.; et al. Lipidomics profiling and risk of cardiovascular disease in the prospective population-based Bruneck study. Circulation 2014, 129, 1821–1831. [Google Scholar] [CrossRef]
- Kosek, A.B.; Durbin, D.; Jonas, A. Binding affinity and reactivity of lecithin cholesterol acyltransferase with native lipoproteins. Biochem. Biophys. Res. Commun. 1999, 258, 548–551. [Google Scholar] [CrossRef] [PubMed]
- Hirsch-Reinshagen, V.; Donkin, J.; Stukas, S.; Chan, J.; Wilkinson, A.; Fan, J.; Parks, J.S.; Kuivenhoven, J.A.; Lutjohann, D.; Pritchard, H.; et al. LCAT synthesized by primary astrocytes esterifies cholesterol on glia-derived lipoproteins. J. Lipid Res. 2009, 50, 885–893. [Google Scholar] [CrossRef]
- Zordoky, B.N.; Sung, M.M.; Ezekowitz, J.; Mandal, R.; Han, B.; Bjorndahl, T.C.; Bouatra, S.; Anderson, T.; Oudit, G.Y.; Wishart, D.S.; et al. Metabolomic fingerprint of heart failure with preserved ejection fraction. PLoS ONE 2015, 10, e0124844. [Google Scholar] [CrossRef]
- Feng, Q.; Liu, Z.; Zhong, S.; Li, R.; Xia, H.; Jie, Z.; Wen, B.; Chen, X.; Yan, W.; Fan, Y.; et al. Integrated metabolomics and metagenomics analysis of plasma and urine identified microbial metabolites associated with coronary heart disease. Sci. Rep. 2016, 6, 22525. [Google Scholar] [CrossRef]
- Mardinoglu, A.; Stancakova, A.; Lotta, L.A.; Kuusisto, J.; Boren, J.; Bluher, M.; Wareham, N.J.; Ferrannini, E.; Groop, P.H.; Laakso, M.; et al. Plasma Mannose Levels Are Associated with Incident Type 2 Diabetes and Cardiovascular Disease. Cell Metab. 2017, 26, 281–283. [Google Scholar] [CrossRef]
- Yu, D.; Moore, S.C.; Matthews, C.E.; Xiang, Y.-B.; Zhang, X.; Gao, Y.-T.; Zheng, W.; Shu, X.-O. Plasma metabolomic profiles in association with type 2 diabetes risk and prevalence in Chinese adults. Metabolomics 2016, 12, 3. [Google Scholar] [CrossRef]
- Koseler, A.; Arslan, I.; Sabirli, R.; Zeytunluoglu, A.; Kılıç, O.; Kilic, I.D. Molecular and Biochemical Parameters Related to Plasma Mannose Levels in Coronary Artery Disease Among Nondiabetic Patients. Genet. Test. Mol. Biomark. 2020, 24, 562–568. [Google Scholar] [CrossRef]
- Ottosson, F.; Smith, E.; Melander, O.; Fernandez, C. Altered Asparagine and Glutamate Homeostasis Precede Coronary Artery Disease and Type 2 Diabetes. J. Clin. Endocrinol. Metab. 2018, 103, 3060–3069. [Google Scholar] [CrossRef]
- Zhao, D.; Guallar, E.; Ouyang, P.; Subramanya, V.; Vaidya, D.; Ndumele, C.E.; Lima, J.A.; Allison, M.A.; Shah, S.J.; Bertoni, A.G.; et al. Endogenous Sex Hormones and Incident Cardiovascular Disease in Post-Menopausal Women. J. Am. Coll. Cardiol. 2018, 71, 2555–2566. [Google Scholar] [CrossRef]
- Reinecke, H.; Bogdanski, J.; Woltering, A.; Breithardt, G.; Assmann, G.; Kerber, S.; von Eckardstein, A. Relation of serum levels of sex hormone binding globulin to coronary heart disease in postmenopausal women. Am. J. Cardiol. 2002, 90, 364–368. [Google Scholar] [CrossRef]
- Ostrander, L.D., Jr.; Lamphiear, D.E.; Carman, W.J.; Williams, G.W. Blood glucose and risk of coronary heart disease. Arteriosclerosis 1981, 1, 33–37. [Google Scholar] [CrossRef] [PubMed]
- Kunutsor, S.K.; Bakker, S.J.; Gansevoort, R.T.; Chowdhury, R.; Dullaart, R.P. Circulating total bilirubin and risk of incident cardiovascular disease in the general population. Arter. Thromb. Vasc. Biol. 2015, 35, 716–724. [Google Scholar] [CrossRef] [PubMed]
- Kunutsor, S.K.; Bakker, S.J.; Kootstra-Ros, J.E.; Gansevoort, R.T.; Gregson, J.; Dullaart, R.P. Serum Alkaline Phosphatase and Risk of Incident Cardiovascular Disease: Interrelationship with High Sensitivity C-Reactive Protein. PLoS ONE 2015, 10, e0132822. [Google Scholar] [CrossRef]
- Ling, Y.; Jiang, J.; Gui, M.; Liu, L.; Aleteng, Q.; Wu, B.; Wang, S.; Liu, X.; Gao, X. Thyroid Function, Prevalent Coronary Heart Disease, and Severity of Coronary Atherosclerosis in Patients Undergoing Coronary Angiography. Int. J. Endocrinol. 2015, 2015, 708272. [Google Scholar] [CrossRef] [PubMed]
- Cabrera de Leon, A.; Oliva Garcia, J.G.; Marcelino Rodriguez, I.; Almeida Gonzalez, D.; Aleman Sanchez, J.J.; Brito Diaz, B.; Dominguez Coello, S.; Bertomeu Martinez, V.; Aguirre Jaime, A.; Rodriguez Perez Mdel, C. C-peptide as a risk factor of coronary artery disease in the general population. Diab. Vasc. Dis. Res. 2015, 12, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Fretts, A.M.; Mozaffarian, D.; Siscovick, D.S.; Sitlani, C.; Psaty, B.M.; Rimm, E.B.; Song, X.; McKnight, B.; Spiegelman, D.; King, I.B.; et al. Plasma phospholipid and dietary alpha-linolenic acid, mortality, CHD and stroke: The Cardiovascular Health Study. Br. J. Nutr. 2014, 112, 1206–1213. [Google Scholar] [CrossRef] [PubMed]

| Measurement | Variables | Total | Lean | Overweight | p-Value |
|---|---|---|---|---|---|
| (N = 200) | (N = 108) | (N = 92) | |||
| Vital signs | Age (years) | 29.1 (5.4) | 28 (5.5) | 30.4 (5.1) | 0.073 |
| BMI (kg/m2) | 24.7 (2.8) | 22.5 (1.4) | 27.3 (1.4) | 0.000 | |
| WHR | 0.74 (0.1) | 0.73 (0.1) | 0.75 (0.1) | 0.026 | |
| SBP (mmHg) | 101.1 (9.4) | 99.9 (8) | 102.5 (10.7) | 0.047 | |
| DBP (mmHg) | 65.9 (8.1) | 65.9 (6.9) | 65.9 (9.3) | 0.987 | |
| Pulse (pulse per minute) | 72.3 (9.3) | 72.7 (9.6) | 71.9 (8.9) | 0.541 | |
| Lipid profile | Cholesterol total (mmol/L) | 4.7 (0.7) | 4.5 (0.7) | 4.9 (0.8) | 0.000 |
| HDL-cholesterol (mmol/L) | 1.6 (0.3) | 1.6 (0.3) | 1.6 (0.3) | 0.970 | |
| LDL-cholesterol (mmol/L) | 2.6 (0.7) | 2.4 (0.6) | 2.9 (0.6) | 0.000 | |
| Triglyceride (mmol/L) | 1 (0.4) | 0.9 (0.4) | 1 (0.5) | 0.042 | |
| Blood sugar | Fasting blood glucose (mmol/L) | 4.8 (0.4) | 4.7 (0.4) | 4.8 (0.4) | 0.030 |
| Insulin (μU/mL) | 11.1 (8.3) | 9.3 (6.5) | 13.1 (9.7) | 0.001 | |
| HbA 1C (%) | 5.2 (0.3) | 5.1 (0.3) | 5.2 (0.3) | 0.055 | |
| C-Peptide (ng/mL) | 2.3 (1.1) | 2 (1) | 2.5 (1.3) | 0.005 | |
| HOMA-IR | 2.4 (1.9) | 2 (1.4) | 2.9 (2.2) | 0.001 | |
| Hormones | Thyroid stimulating hormone (mIU/L) | 1.8 (1.4) | 1.7 (1.2) | 1.8 (1.6) | 0.751 |
| Testosterone total (nmol/L) | µ1.2 (0.6) | 1.2 (0.7) | 1.2 (0.5) | 0.942 | |
| Estradiol (pmol/L) | 518.8 (137.2) | 608.7 (1821.9) | 413.9 (451) | 0.324 | |
| Sex hormone-binding globulin (nmol/L) | 92.7 (74.4) | 13.6 (1.9) | 13.4 (2.4) | 0.195 | |
| Free thyroxine (T4) (pmol/L) | 13.5 (2.1) | 13.6 (1.9) | 13.4 (2.4) | 0.620 | |
| Free triiodothyronine (T3) (pmol/L) | 4.5 (0.8) | 4.4 (0.7) | 4.4 (0.7) | 0.335 | |
| Liver function | Bilirubin total (μmol/L) | 6.2 (2.9) | 6.1 (2.7) | 6.2 (3.3) | 0.829 |
| Albumin (g/L) | 45.2 (2.3) | 45.8 (2.5) | 44.5 (1.9) | 0.000 | |
| Alkaline phosphatase (IU/L) | 62.6 (20.5) | 60.9 (15.7) | 64.6 (24.9) | 0.208 | |
| ALT ( GPT ) (IU/L) | 15 (10) | 13.2 (6.8) | 17 (12.5) | 0.006 | |
| AST (GOT) (IU/L) | 16.8 (5.6) | 16.1 (3.6) | 17.6 (7.1) | 0.055 | |
| Kidney function tests | Sodium (mmol/L) | 139.8 (1.9) | 139.8 (2) | 139.7 (1.9) | 0.775 |
| Potassium (mmol/L) | 4.3 (0.3) | 4.3 (0.4) | 4.2 (0.3) | 0.055 | |
| Chloride (mmol/L) | 101.5 (1.9) | 101.6 (1.9) | 101.5 (1.9) | 0.698 | |
| Bicarbonate (mmol/L) | 25.7 (1.9) | 25.7 (1.9) | 25.7 (1.9) | 0.992 | |
| Urea (mmol/L) | 3.9 (1.0) | 3.9 (1) | 3.9 (1) | 0.929 | |
| Creatinine (μmol/L) | 55.6 (8.5 | 7.6 (54.3) | 57.1 (9.2) | 0.018 | |
| Calcium (mmol/L) | 2.37 (0.08) | 2.38 (0.08) | 2.36 (0.08) | 0.047 | |
| Calcium corrected (mmol/L) | 2.3 (0.1) | 2.3 (0.1) | 2.3 (0.1) | 0.990 | |
| Phosphorus (mmol/L) | 1.2 (0.2) | 1.2 (0.2) | 1.2 (0.2) | 0.857 | |
| Uric Acid (umol/L) | 232 (50.8) | 221 (44.1) | 244.8 (55.2) | 0.001 | |
| Magnesium (mg/dL) | 0.8 (0.1) | 0.8 (0.1) | 0.8 (0.1) | 0.647 | |
| Total protein (g/L) | 73.5 (3.9) | 64.2 (9.6) | 65.5 (10.8) | 0.105 | |
| Homocysteine (μmol/L) | 7.8 (2.6) | 7.6 (2.6) | 7.9 (2.7) | 0.459 | |
| Ion profile | Iron (μmol/L) | 13.3 (7.2) | 14.1 (8.5) | 12.3 (5.2) | 0.079 |
| Total iron-binding capacity (mmol/L) | 64.8 (10.2) | 64.2 (9.6) | 65.5 (10.8) | 0.401 | |
| Unsaturated iron-binding capacity (µmol/L) | 51.6 (12.8) | 50.2 (12.7) | 53.1 (12.8) | 0.111 | |
| Ferritin (μg/L) | 21.7 (23.3) | 19.7 (17.6) | 24 (28.5) | 0.193 | |
| Vitamins | Folate (nmol/L) | 24.7 (8) | 25.3 (7.8) | 24.1 (8.3) | 0.294 |
| Vitamin B12 (nmol/L) | 271 (108.7) | 283.4 (119.2) | 256.8 (94) | 0.089 | |
| Dihydroxyvitamin D Total (ng/mL) | 17.1 (10.1) | 16.2 (10.2) | 18.1 (9.9) | 0.198 |
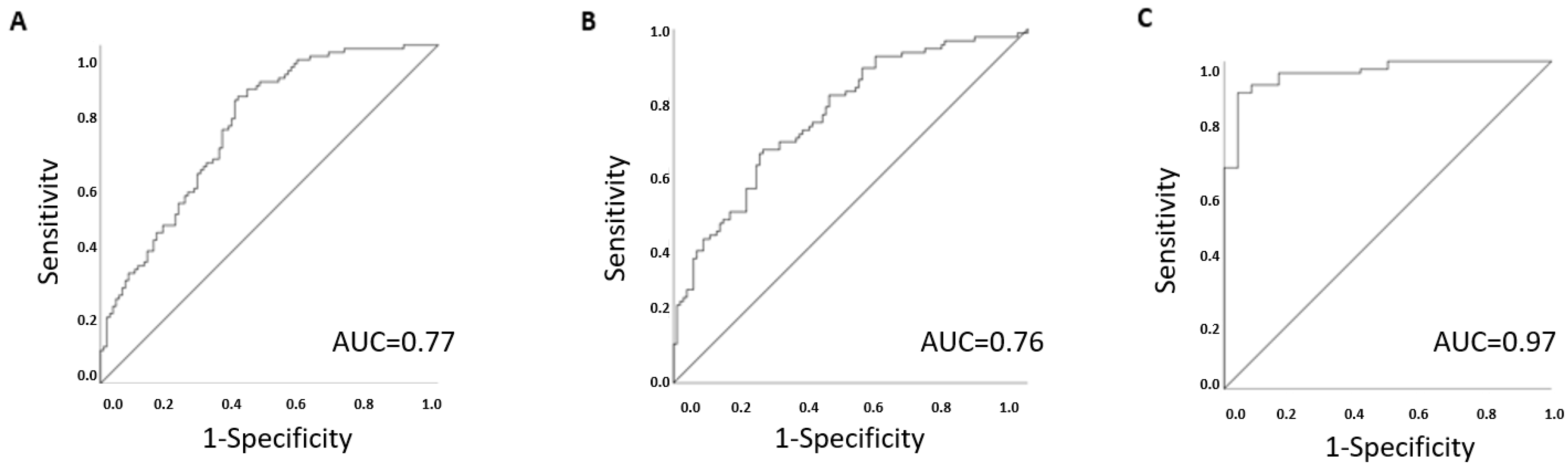
| Model | Variables | Beta | S.E. | p Value | OD (95% CI) | AUC (95% CI) |
|---|---|---|---|---|---|---|
| Classical risk factors | Glucose | 0.8 | 0.4 | 0.035 | 2.1 (1.1−4.3) | 0.77 (0.6−0.8) |
| Creatinine | 0.1 | 0.0 | 0.004 | 1.1 (1−1.1) | ||
| Albumin | −0.3 | 0.1 | 0.001 | 0.8 (0.7−0.9) | ||
| Discovery cohort | 1-Arachidonoyl-GPC (20:4n6) | 2.1 | 0.6 | 0.001 | 8.1 (2.5−26.7) | 0.76 (0.7−0.8) |
| Asparagine | −2.4 | 0.8 | 0.002 | 0.1 (0−0.4) | ||
| Mannose | 1.6 | 0.6 | 0.004 | 5.1 (1.7−15.5) | ||
| Linolenate (alpha or gamma; (18:3n3 or 6)) | −0.7 | 0.2 | 0.002 | 0.5 (0.3−0.8) | ||
| Dimethylglycine | 1.9 | 0.6 | 0.004 | 6.4 (1.8–22.4) | ||
| Replication cohort | Asparagine | –1.6 | 0.7 | 0.019 | 0.2 (0.1–0.8) | 0.97 (0.9–1) |
| Mannose | 1.7 | 0.7 | 0.017 | 5.3 (1.3–20.7) | ||
| Linolenate (alpha or gamma; (18:3n3 or 6)) | –2.2 | 0.7 | 0.002 | 9.3 (2.3–37.6) | ||
| Dimethylglycine | –0.3 | 0.5 | 0.549 | 0.7 (0.3–2) |
| Variables | Total | Lean | Overweight | p-Value |
|---|---|---|---|---|
| (N = 200) | (N = 108) | (N = 92) | ||
| 1-Arachidonoyl-GPC (20:4n6) * | 0.94 (0.3) | 0.89 (0.26) | 1.01 (0.34) | 0.001 |
| Asparagine | 1.06 (0.23) | 1.09 (0.23) | 1.03 (0.23) | 0.005 |
| Mannose | 0.93 (0.29) | 0.89 (0.29) | 0.99 (0.28) | 0.010 |
| Linolenate (alpha or gamma; (18:3n3 or 6)) | 1.25 (0.82) | 1.32 (0.81) | 1.18 (0.83) | 0.002 |
| Dimethylglycine | 0.93 (0.34) | 0.89 (0.24) | 0.99 (0.42) | 0.006 |
| Uridine | 0.91 (0.27) | 0.89 (0.27) | 0.92 (0.27) | 0.521 |
| N-acetylalanine | 0.95 (0.18) | 0.92 (0.18) | 0.98 (0.18) | 0.043 |
| 13-HODE + 9-HODE | 1.16 (0.53) | 1.24 (0.52) | 1.08 (0.53) | 0.024 |
| O-sulfo-L-tyrosine | 0.94 (0.24) | 0.91 (0.24) | 0.97 (0.25) | 0.377 |
| 4-Vinylphenol sulfate | 1.14 (2) | 1.14 (2.04) | 1.13 (1.97) | 0.376 |
| N-acetylthreonine | 0.98 (0.27) | 0.96 (0.26) | 1.01 (0.27) | 0.192 |
| N-acetyl-3-methylhistidine * | 0.86 (0.42) | 0.82 (0.29) | 0.91 (0.51) | 0.656 |
| Theophylline | 1.04 (0.75) | 1.04 (0.84) | 1.04 (0.64) | 0.585 |
| Erythritol | 0.84 (0.59) | 0.85 (0.75) | 0.82 (0.3) | 0.611 |
| 2-Methylbutyrylcarnitine (C5) | 0.73 (0.37) | 0.72 (0.4) | 0.74 (0.34) | 0.769 |
| Indolelactate | 0.81 (0.27) | 0.8 (0.25) | 0.82 (0.29) | 0.246 |
| p-Cresol sulfate | 1.27 (0.83) | 1.25 (0.76) | 1.29 (0.91) | 0.130 |
| Metabolite | Predictors | Beta | p Value (Metabolite) | Adjusted R-Squared | p Value (Model) |
|---|---|---|---|---|---|
| Asparagine | Total cholesterol | −0.3 | <0.001 | 0.15 | 0.00006 |
| Sex hormone-binding globulin | 0.22 | 0.005 | |||
| Calcium | 0.22 | 0.006 | |||
| Total testosterone | −0.2 | 0.022 | |||
| Mannose | Sex hormone-binding globulin | 0.31 | <0.001 | 0.15 | 0.00002 |
| Glucose | 0.2 | 0.009 | |||
| BMI | 0.19 | 0.014 | |||
| Total bilirubin | 0.15 | 0.047 | |||
| 1-Arachidonoyl-GPC (20:4n6) | Total cholesterol | 0.85 | <0.001 | 0.37 | 1.6 × 10−12 |
| Alkaline phosphatase | 0.13 | 0.043 | |||
| Homocysteine | −0.2 | 0.004 | |||
| LDL-cholesterol | −0.5 | <0.001 | |||
| Total testosterone | −0.3 | <0.001 | |||
| Free thyroxine | 0.19 | 0.004 | |||
| Chloride | −0.1 | 0.045 | |||
| Linolenate (18:3n3 or 6) | C-Peptide | −0.4 | <0.001 | 0.23 | 6.5 × 10−9 |
| DBP | 0.19 | 0.008 | |||
| Free triiodothyronine | 0.18 | 0.014 | |||
| Total iron-binding capacity | 0.16 | 0.028 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abu-El-Ruz, R.; Abdel-Rahman, M.E.; Atkin, S.L.; Elrayess, M.A. Comparing Levels of Metabolic Predictors of Coronary Heart Disease between Healthy Lean and Overweight Females. Metabolites 2021, 11, 169. https://doi.org/10.3390/metabo11030169
Abu-El-Ruz R, Abdel-Rahman ME, Atkin SL, Elrayess MA. Comparing Levels of Metabolic Predictors of Coronary Heart Disease between Healthy Lean and Overweight Females. Metabolites. 2021; 11(3):169. https://doi.org/10.3390/metabo11030169
Chicago/Turabian StyleAbu-El-Ruz, Rasha, Manar E. Abdel-Rahman, Stephen L. Atkin, and Mohamed A. Elrayess. 2021. "Comparing Levels of Metabolic Predictors of Coronary Heart Disease between Healthy Lean and Overweight Females" Metabolites 11, no. 3: 169. https://doi.org/10.3390/metabo11030169
APA StyleAbu-El-Ruz, R., Abdel-Rahman, M. E., Atkin, S. L., & Elrayess, M. A. (2021). Comparing Levels of Metabolic Predictors of Coronary Heart Disease between Healthy Lean and Overweight Females. Metabolites, 11(3), 169. https://doi.org/10.3390/metabo11030169







