Injectable Biostimulator in Adipose Tissue: An Update and Literature Review
Abstract
1. Introduction
2. Summary of Evidence
| Study | Agents/Methods | Findings | Limitations | Level |
|---|---|---|---|---|
| Turkevych et al. [30] | PCL | Enhanced ADSC differentiation, collagen synthesis, improved dermal thickness, and elasticity. | Lacks large-scale trials and longitudinal data. | IIb |
| Bota et al. [1] | PLLA, PCL, CaHA | Induced collagen production and adipogenesis; improved dermal remodeling. | Lacks meta-analysis, relies on heterogeneous studies. | IIa |
| Radke et al. [31] | PLLA | Promoted fibroblast stimulation, collagen deposition, and adipocyte metabolic activity. | Lacks quantitative data, anecdotal evidence. | IIIb |
| De Paula Barbosa et al. [32] | PLLA | Improved dermal thickness and skin elasticity; high patient satisfaction. | Small sample size, no control group. | IIb |
| Jin et al. [33] | PLLA | Lactate enhances adipocyte metabolism; reduced adipose tissue volume, improved dermal quality. | Lacks large-scale trials. | IIb |
| Melfa et al. [27] | SEFFI and CaHA | Improved skin elasticity and volume; supported adipogenesis and tissue repair. | Retrospective design, lacks control group. | IIIb |
| Zubair et al. [29] | PLLA | Significant increases in dermal thickness and patient satisfaction; enhanced adipocyte activity. | Focused on one area, potential for bias. | Ib |
| Lee et al. [34] | Poly-D, L-lactic acid (PDLLA) | Stimulated fibroblasts/adipocytes, enhanced collagen production, and adipogenesis. | Lacks systematic methodology, no quantitative synthesis. | IIa |
| Ablon et al. [35] | PRP, exosomes, stem cells | Enhanced adipocyte proliferation and differentiation; improved tissue regeneration. | Lacks standardized protocols, anecdotal evidence. | IIIb |
| Barbosa et al. [36] | PLLA, CaHA | Improved dermal quality and volume through adipocyte stimulation. | Lacks clinical data to support claims. | IIIc |
| Bezpalko et al. [37] | Hyaluronic acid fillers | Increased adipose tissue volume, improved skin hydration and elasticity. | Non-randomized design, small sample size. | IIb |
| Nogueira et al. [38] | PLLA | Protocol outlined for improving skin flaccidity and adipocyte activity; biostimulatory effects noted. | Lacks clinical trial data. | IIIb |
| Dhillon et al. [39] | PLLA, CaHA | Enhanced adipocyte activity and collagen production; tailored treatment plans for cellulite. | Lacks systematic approach, relies on non-randomized evidence. | IIa |
| Surowiecka et al. [18] | ADSCs | Promoted adipogenesis and collagen production, improved skin elasticity and thickness. | Most evidence from small-scale trials. | IIb |
| Mazzuco et al. [40] | PLLA, CaHA | Improved dermal thickness and collagen density; PLLA showed superior adipocyte stimulation. | Small sample size, lacks control group. | Ib |
| Silveira et al. [41] | Hyperdiluted CaHA | Significant improvements in volume and skin texture, attributed to CaHA’s effects. | Small sample size, lacks control group. | IIIc |
| O’Daniel et al. [42] | PLLA | Enhanced volume retention post-facelift; high patient satisfaction. | Observational design, lacks control group. | IIIb |
| Sparavigna et al. [43] | Hybrid hyaluronan complexes | Improved dermal thickness and elasticity; supports adipocyte activity. | Non-randomized design, limited generalizability. | IIb |
| Munia et al. [44] | PLLA | Improved facial volume and contour using vector technique; enhanced adipocyte stimulation. | Small sample size, lacks control group. | IIIc |
| Nikolis et al. [45] | PLLA | Demonstrated enhanced adipocyte activity and dermal thickness with extended injection technique. | Limited study scope; generalizability may be affected. | Ib |
| Sarlos et al. [46] | PLLA, hyaluronic acid | Improved facial contour and dermal elasticity; high patient satisfaction. | Observational nature, small sample size. | IIIb |
| Thomas et al. [47] | PLLA, CaHA | Overview of techniques and effects on adipocytes; practical guidance for clinicians. | Lacks supporting clinical data; relies on expert opinion. | V |
| Kim et al. [48] | PRP | Enhances adipocyte activity and dermal volume; promising results from case studies. | Lacks large-scale evidence; based on anecdotal evidence. | IV |
| Xiao et al. [49] | PRP | Enhanced adipocyte activity and dermal remodeling; observed improvements across studies. | Significant heterogeneity in study design; limited conclusions. | IIa |
| Mazzuco et al. [50] | PLLA, CaHA | Discusses mechanisms for cellulite treatment; highlights gradual stimulation effects. | Lacks supporting clinical studies; based on expert opinion. | V |
| Lin et al. [51] | PDLLA | Improved dermal elasticity and volume restoration; significant follow-up outcomes. | Limited by small number of cases; lacks control group. | IV |
| Rovatti et al. [52] | Hyperdiluted CaHA | Significant improvements in facial rejuvenation; high patient satisfaction. | Small sample size; lacks control group. | IIb |
| Othman et al. [53] | PLLA, CaHA | Comprehensive overview of biostimulatory effects; highlights effectiveness for temporal augmentation. | Lacks uniformity among studies; no meta-analysis performed. | IIa |
| Gil-del Valle et al. [54] | PRP with ozone | Improved dermal volume and quality of life in HIV patients; promotes adipocyte activity. | Small sample size; specific patient population limits generalizability. | IIb |
| de Albuquerque et al. [55] | PLLA, CaHA | Discusses body rejuvenation techniques; highlights gradual and immediate effects of injectables. | Lacks supporting clinical data; relies on expert opinion. | V |
| da Cunha et al. [56] | CaHA | Significant improvements in facial aging; high patient satisfaction. | Lack of control group; small sample size. | IIb |
| Davis et al. [57] | PLLA, CaHA | Highlights combination treatments for cellulite; emphasizes treatment customization. | Lacks systematic methodology; based on expert opinion. | IV |
| Palermo et al. [58] | PLLA, CaHA | Introduces a three-dimensional approach to rejuvenation; discusses individualized treatment plans. | Lacks supporting clinical trial data; relies on expert opinion. | V |
| Zarei et al. [59] | ADSCs | Promotes adipogenesis and dermal remodeling; shows promise in facial rejuvenation. | Variability in protocols; lacks long-term safety data. | IIa |
| Antonio et al. [60] | ADSCs, PRP | Highlights regenerative potential; improves skin elasticity and volume. | Relies on theoretical concepts; small-scale studies limit evidence strength. | IIIc |
| Aunna Pourang et al. [61] | PRP | Enhances adipocyte activity; promising case studies reported. | Lacks standardized protocols; relies on anecdotal evidence. | IV |
| Jáñez et al. [62] | PRP | Delivers growth factors that enhance adipocyte activity; minimal adverse effects noted. | Based on small-scale trials; lacks large-scale studies. | V |
| Alessandrini et al. [63] | Hyaluronic acid | Improved skin hydration and volume; potential for adipocyte stimulation. | Small sample size; short follow-up period. | IIb |
3. Discussion
3.1. Mechanisms of Action
3.2. Clinical Efficacy
3.3. Safety Considerations
3.4. Standardized Protocols
3.5. Emerging Applications and Combination Therapies
3.6. Limitations and Future Directions
- (1)
- Protocol standardization: Define agent-specific preparation (dilution, particle size/activation), injection planes, volumes, and session spacing to reduce heterogeneity and enable pooling.To improve cross-study comparability, future reports should also specify a minimum reporting set, including: (i) product preparation (brand, particle size, dilution), (ii) plane and instrument (cannula vs. needle; gauge), (iii) device parameters when applicable (energy type, fluence, pulse width, passes), (iv) session spacing and sequence (matrix-first vs. immediate agents), (v) objective endpoints (ultrasound thickness, elastography, histology) with pre-specified timepoints (e.g., 3/6/12 months), and (vi) AE capture windows (early/delayed). Establishing such a dataset will enhance reproducibility and enable a meaningful comparison across combination protocols.
- (2)
- Head-to-head randomized trials: Compare PLLA, PCL, and CaHA (±HA/PRP) with prespecified objective endpoints (ultrasound dermal thickness, elastography, histology), blinded assessments, and ≥12–24 month follow-up.
- (3)
- Mechanistic readouts: Integrate imaging and tissue biomarkers (collagen type I/III ratios, ECM organization) to link dose, kinetics (onset vs. durability), and clinical effect.
- (4)
- Safety surveillance: Establish prospective registries to quantify delayed nodules/granulomas, vascular events, and mitigation strategies (e.g., massage, cannula use, reversal/management algorithms).
- (5)
- Patient stratification and indications: Identify responders by phenotype (age, skin laxity, weight-loss status) and optimize combination algorithms (e.g., SEFFI + CaHA, PLLA with energy-based devices) by anatomical site.
- (6)
- Methodological rigor: Standardize core outcome sets, incorporate allocation concealment/blinding, and report attrition/selective reporting to minimize bias.
- (7)
- Health economics and QoL: Include cost-effectiveness and validated patient-reported outcomes alongside objective measures.
4. Methodology
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Boța, M.; Cristea, A.M.; Vlaia, L.L.; Vlaia, V. The impact of injectable biostimulatory substances on current trends in aesthetic medicine: Focus on poly-L-lactic acid, polycaprolactone, and calcium hydroxyapatite. Med. Evol. 2025, 31, 177–186. [Google Scholar] [CrossRef]
- Fisher, S.M.; Borab, Z.; Weir, D.; Rohrich, R.J. The emerging role of biostimulators as an adjunct in facial rejuvenation: A systematic review. J. Plast. Reconstr. Aesthetic Surg. 2024, 92, 118–129. [Google Scholar] [CrossRef] [PubMed]
- Pan, Y.; Hao, Y.; Xiao, Y.; Shi, K.; Qu, Y.; Qian, Z. Injectable soft tissue nano/micro fillers for facial reconstruction. J. Biomed. Nanotechnol. 2021, 17, 1–17. [Google Scholar] [CrossRef] [PubMed]
- da Cunha, M.G.; Engracia, M.; de Souza, L.G.; Filho, C.D.A.M. Biostimulators and their mechanisms of action. Surg. Cosmet. Dermatol. 2020, 12, 109–117. [Google Scholar]
- Wong, T.H.S. A revision and summary of injectable fillers. J. Cosmet. Med. 2020, 4, 7–11. [Google Scholar] [CrossRef]
- Haddad, S.; Galadari, H.; Patil, A.; Goldust, M.; Al Salam, S.; Guida, S. Evaluation of the biostimulatory effects and the level of neocollagenesis of dermal fillers: A review. Int. J. Dermatol. 2022, 61, 1284–1288. [Google Scholar] [CrossRef]
- Attenello, N.H.; Maas, C.S. Injectable fillers: Review of material and properties. Facial Plast. Surg. 2015, 31, 29–34. [Google Scholar] [CrossRef]
- Guo, J.; Fang, W.; Wang, F. Injectable fillers: Current status, physicochemical properties, function mechanism, and perspectives. RSC Adv. 2023, 13, 23841–23858. [Google Scholar] [CrossRef]
- Corduff, N.; Goldie, K.; Lin, F.; Lowe, S.; Siew, T.W.; Vachiramon, V.; Chao, Y.Y.; Lesthari, I.; Ong-Amoranto, B.; Lim, T.S.; et al. The evolving field of regenerative aesthetics: A review and case series. Cureus 2025, 17, e87878. [Google Scholar] [CrossRef]
- Rho, N.K.; Kim, H.S.; Kim, S.Y.; Lee, W. Injectable “skin boosters” in aging skin rejuvenation: A current overview. Arch. Plast. Surg. 2024, 51, 528–541. [Google Scholar] [CrossRef]
- Bellei, B.; Migliano, E.; Picardo, M. Therapeutic potential of adipose tissue derivatives in modern dermatology. Exp. Dermatol. 2022, 31, 1837–1852. [Google Scholar] [CrossRef]
- Gaur, M.; Dobke, M.; Lunyak, V.V. Mesenchymal stem cells from adipose tissue in clinical applications for dermatological indications and skin aging. Int. J. Mol. Sci. 2017, 18, 208. [Google Scholar] [CrossRef]
- Naderi, N.; Combellack, E.J.; Griffin, M.; Sedaghati, T.; Javed, M.; Findlay, M.W.; Wallace, C.G.; Mosahebi, A.; Butler, P.E.; Seifalian, A.M.; et al. The regenerative role of adipose-derived stem cells (ADSCs) in plastic and reconstructive surgery. Int. Wound J. 2017, 14, 112–124. [Google Scholar] [CrossRef]
- Mazini, L.; Rochette, L.; Amine, M.; Malka, G. Regenerative capacity of adipose-derived stem cells (ADSCs) compared with mesenchymal stem cells (MSCs). Int. J. Mol. Sci. 2019, 20, 2523. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Lu, F.; Feng, J. Aging and homeostasis of the hypodermis in the age-related deterioration of skin function. Cell Death Dis. 2024, 15, 443. [Google Scholar] [CrossRef] [PubMed]
- Bonté, F.; Girard, D.; Archambault, J.C.; Desmoulière, A. Skin changes during ageing. In Biochemistry and Cell Biology of Ageing: Part II Clinical Science; Springer: Berlin/Heidelberg, Germany, 2019; pp. 249–280. [Google Scholar]
- Wollina, U.; Wetzker, R.; Abdel-Naser, M.B.; Kruglikov, I.L. Role of adipose tissue in facial aging. Clin. Interv. Aging 2017, 12, 2069–2076. [Google Scholar] [CrossRef] [PubMed]
- Surowiecka, A.; Strużyna, J. Adipose-derived stem cells for facial rejuvenation. J. Pers. Med. 2022, 12, 117. [Google Scholar] [CrossRef]
- Corduff, N. Introducing aesthetic regenerative scaffolds: An immunological perspective. J. Cosmet. Dermatol. 2023, 22, 8–14. [Google Scholar] [CrossRef]
- Christen, M.O. Collagen stimulators in body applications: A review focused on poly-L-lactic acid (PLLA). Clin. Cosmet. Investig. Dermatol. 2022, 15, 997–1019. [Google Scholar] [CrossRef]
- Oh, S.; Shin, N.; Lee, S.J.; Son, K.H.; Byun, K. Poly-L-lactic acid filler increases adipogenesis and adiponectin in aged subcutaneous tissue. Polymers 2025, 17, 1826. [Google Scholar] [CrossRef]
- Kim, J.S. Changes in dermal thickness in biopsy study of histologic findings after a single injection of polycaprolactone-based filler into the dermis. Aesthetic Surg. J. 2019, 39, NP484–NP494. [Google Scholar] [CrossRef]
- Christen, M.O.; Vercesi, F. Polycaprolactone: How a well-known and futuristic polymer has become an innovative collagen stimulator in esthetics. Clin. Cosmet. Investig. Dermatol. 2020, 13, 31–48. [Google Scholar] [CrossRef] [PubMed]
- Amiri, M.; Meçani, R.; Niehot, C.D.; Phillips, T.; Kolb, J.; Daughtry, H.; Muka, T. Skin regeneration-related mechanisms of calcium hydroxyapatite (CaHA): A systematic review. Front. Med. 2023, 10, 1195934. [Google Scholar] [CrossRef] [PubMed]
- Turkevych, A.; Turkevych, D. Influence of calcium hydroxyapatite on soft tissues—A critical viewpoint. J. Appl. Cosmetol. 2022, 40, 19. [Google Scholar]
- De Almeida, A.T.; Figueredo, V.; da Cunha, A.L.G.; Casabona, G.; de Faria, J.R.C.; Alves, E.V.; Sato, M.; Branco, A.; Guarnieri, C.; Palermo, E. Consensus recommendations for the use of hyperdiluted calcium hydroxyapatite (Radiesse) as a face and body biostimulatory agent. Plast. Reconstr. Surg.–Glob. Open 2019, 7, e2160. [Google Scholar] [CrossRef]
- Melfa, F.; McCarthy, A.; Aguilera, S.B.; van Loghem, J.; Gennai, A. Guided SEFFI and CaHA: A retrospective observational study of an innovative protocol for regenerative aesthetics. J. Clin. Med. 2024, 13, 4381. [Google Scholar] [CrossRef]
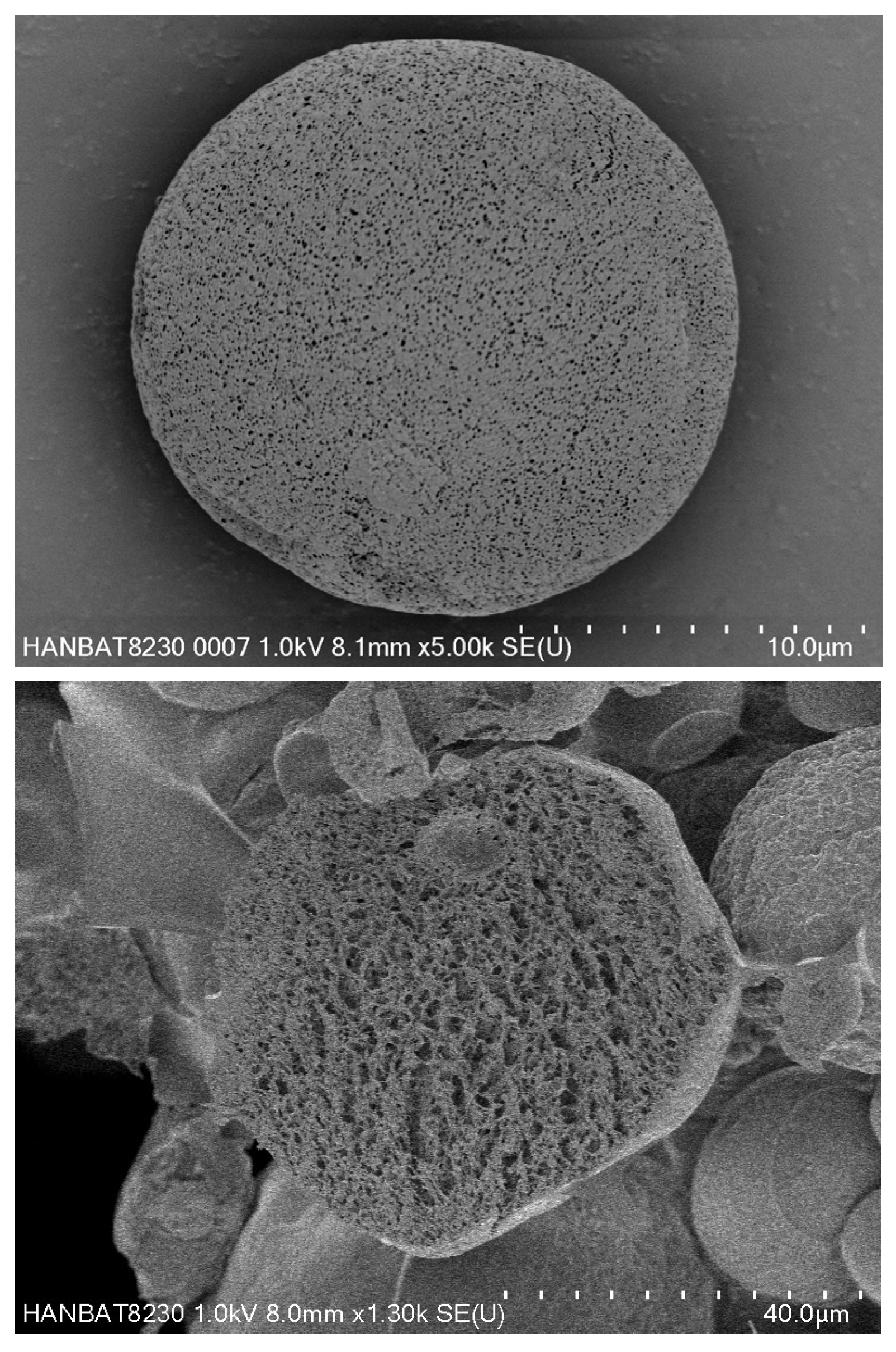
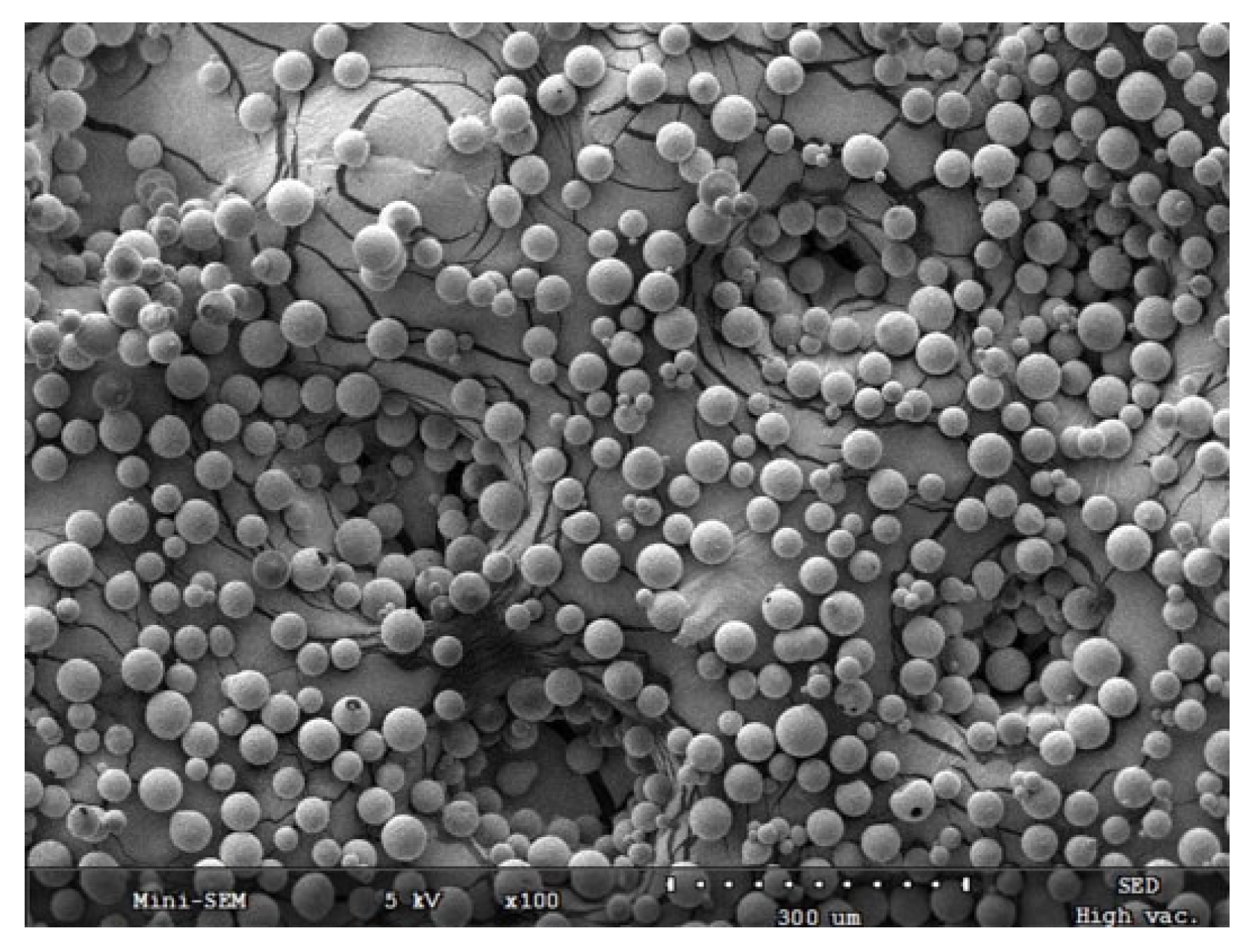
- Melfa, F.; Gennai, A.; Carfagna, G.; Bovani, B.; Piccolo, D.; Colli, M.; Baldessin, M.; Siragusa, D. Characterization of adipose-derived mesenchymal stem cells from tissue harvested with the guided SEFFI technique and co-cultured with calcium hydroxyapatite. J. Appl. Cosmetol. 2023, 41, 4–19. [Google Scholar] [CrossRef]
- Zubair, R.; Ishii, L.; Loyal, J.; Hartman, N.; Fabi, S.G. SPLASH: Split-body randomized clinical trial of poly-L-lactic acid for adipogenesis and volumization of the hip dell. Dermatol. Surg. 2024, 50, 1155–1162. [Google Scholar] [CrossRef]
- Turkevych, O.; Turkevych, D. Polycaprolactone (PCL) as an adipose-derived stem cell (ADSC) stimulator—The experimental trial. J. Appl. Cosmetol. 2025, 43, 40–52. [Google Scholar] [CrossRef]
- Radke, F.; Wüst, S. PLLA as a biostimulator: What do we know and what should patients be informed about? Cosmet. Med. Aesthetic Surg. 2025, 1, 51. [Google Scholar]
- De Paula Barbosa, A.; Ferreira, A.C.M.; Duarte, A.C.; da Silva, R.V. Novel therapeutic approaches with poly-L-lactic acid for treating gluteal skin laxity in male patients. Chin. J. Plast. Reconstr. Surg. 2025, 7, 23–29. [Google Scholar] [CrossRef]
- Jin, W.; Chen, G.; Chen, W.; Qiao, G.; Deng, Y.; Li, K.; Cai, W. Poly-L-lactic acid reduces the volume of dermal adipose tissue through its metabolite lactate. Aesthetic Plast. Surg. 2024, 48, 5136–5146. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.W.A.; Chan, L.K.W.; Lee, A.W.K.; Lee, C.H.; Wong, S.T.H.; Yi, K.H. Poly-D,L-lactic acid (PDLLA) application in dermatology: A literature review. Polymers 2024, 16, 2583. [Google Scholar] [CrossRef] [PubMed]
- Ablon, G.; Smith, Z.I.; Munavalli, G. Applications of plasma-rich plasma, exosomes, and stem cells in aesthetics: A narrative review. Dermatol. Rev. 2024, 5, e250. [Google Scholar] [CrossRef]
- Barbosa, A.D.P.; Espasandin, I.; Pinheiro de Lima, L.; de Souza Ribeiro, C.; Raquel Silva, L.; Faria Quintal, T.; Nascimento Lima, E.; Catarina Duarte Vieira, L.; Soares, T.R.; Autran Colaço, A.R. Body harmonization: The definition of a new concept. Clin. Cosmet. Investig. Dermatol. 2023, 16, 3753–3766. [Google Scholar] [CrossRef]
- Bezpalko, L.; Filipskiy, A. Clinical and ultrasound evaluation of skin quality after subdermal injection of two non-crosslinked hyaluronic acid-based fillers. Clin. Cosmet. Investig. Dermatol. 2023, 16, 2175–2183. [Google Scholar] [CrossRef]
- Nogueira, P.L.; de Morais Teodoro, M.R.F. Protocol for the use of poly-L-lactic acid (Elleva and Elleva X) for skin flaccidity in body areas. J. Clin. Exp. Dermatol. Res. 2023, 14, 629. [Google Scholar]
- Dhillon, R.K.; Dayan, S.H.; Hexsel, D.; Shridharani, S.; Chilukuri, S.; LaTowsky, B.; Fabi, S.G. Update: Cellulite therapies and optimizing treatment combinations. Aesthetic Surg. J. 2023, 43, 1508–1520. [Google Scholar] [CrossRef]
- Mazzuco, R.; Evangelista, C.; Gobbato, D.O.; de Almeida, L.M. Clinical and histological comparative outcomes after injections of poly-L-lactic acid and calcium hydroxyapatite in arms: A split-side study. J. Cosmet. Dermatol. 2022, 21, 6727–6733. [Google Scholar] [CrossRef]
- Silveira, I.; Martinez, B. Bilateral gluteal augmentation with hyperdilute calcium hydroxyapatite microspheres performed using the Bella Vida Instant Brazilian Butt Lift (BBL)TM. Cureus 2022, 14, e26834. [Google Scholar]
- O’Daniel, T.G.; Kachare, M.D. The utilization of poly-L-lactic acid as a safe and reliable method for volume maintenance after facelift surgery with fat grafting. Aesthetic Surg. J. Open Forum 2022, 4, ojac014. [Google Scholar] [CrossRef] [PubMed]
- Sparavigna, A.; Bombelli, L.; Giori, A.M.; Bellia, G. Efficacy and tolerability of hybrid complexes of high- and low-molecular-weight hyaluronan intradermal injections for the treatment of skin roughness and laxity of the neck. Sci. World J. 2022, 2022, 4497176. [Google Scholar] [CrossRef] [PubMed]
- Munia, C.; Parada, M.; de Alvarenga Morais, M.H. Changes in facial morphology using poly-L-lactic acid application according to vector technique: A case series. J. Clin. Aesthetic Dermatol. 2022, 15, 38–42. [Google Scholar]
- Nikolis, A.; Rosengaus, F.; Blackburn, G.; Safran, T.; Enright, K.M. A randomized controlled trial evaluating traditional versus extended techniques of poly-L-lactic acid injection for the aesthetic improvement of the temporal fossae. Dermatol. Surg. 2022, 51, 702–709. [Google Scholar] [CrossRef]
- Sarlos, P.; Haddad, A.; Avelar, L.E.; Saito, F.L. Facial remodeling addressing fat loss and skin sagging with poly-L-lactic acid SCA and hyaluronic acid filler after semaglutide-associated prescriptive weight loss. Dermatol. Surg. 2022, 51, 1002–1005. [Google Scholar] [CrossRef]
- Thomas, M.; Dsilva, J. Newer approaches in non-surgical facial rejuvenation. In Integrated Procedures in Facial Cosmetic Surgery; Springer International Publishing: Cham, Switzerland, 2021; pp. 451–467. [Google Scholar]
- Kim, H.J.; González, N.E. Platelet-rich plasma for dermal augmentation of the face and body. In Platelet-Rich Plasma in Dermatologic Practice; Springer International Publishing: Cham, Switzerland, 2021; pp. 93–101. [Google Scholar]
- Xiao, H.; Xu, D.; Mao, R.; Xiao, M.; Fang, Y.; Liu, Y. Platelet-rich plasma in facial rejuvenation: A systematic appraisal of the available clinical evidence. Clin. Cosmet. Investig. Dermatol. 2021, 14, 1697–1724. [Google Scholar] [CrossRef]
- Mazzuco, R.; Dini, T.D.F. Using fillers to treat cellulite. In Illustrated Manual of Injectable Fillers; CRC Press: Boca Raton, FL, USA, 2020; pp. 133–141. [Google Scholar]
- Lin, J.Y.; Lin, C.Y. Injectable poly-D,L-lactic acid in facial rejuvenation: Three case reports. Cosmetol. J. 2020, 4, 000120. [Google Scholar]
- Rovatti, P.P.; Pellacani, G.; Guida, S. Hyperdiluted calcium hydroxyapatite 1:2 for mid and lower facial skin rejuvenation: Efficacy and safety. Dermatol. Surg. 2020, 46, e112–e117. [Google Scholar] [CrossRef]
- Othman, S.; Cohn, J.E.; Burdett, J.; Daggumati, S.; Bloom, J.D. Temporal augmentation: A systematic review. Facial Plast. Surg. 2020, 36, 217–225. [Google Scholar] [CrossRef]
- Gil-del Valle, L.; Suarez, M.A.A.; Rabeiro-Martinez, C.L.; Gravier-Hernández, R.; González-Abreu, M.C.H.; Bermúdez-Alfonso, Y.; Rosa-Font, M.; Campos-Díaz, J.; Hernández-Requejo, D.; Martínez-Sánchez, G.; et al. Facial biostimulation with PRP activated with ozone resounds on cellular redox balance, improves lipoatrophy and quality of life in HIV patients. J. Pharm. Pharmacogn. Res. 2019, 7, 273–287. [Google Scholar] [CrossRef]
- de Albuquerque, G.C. Fillers and collagen stimulator for body rejuvenation and cellulitis. In Botulinum Toxins, Fillers and Related Substances; Springer International Publishing: Cham, Switzerland, 2019; pp. 1–7. [Google Scholar]
- da Cunha, M.G.; da Cunha, A.L.G.; Gonzaga, M.; da Veiga, G.L.; Alves, B.D.C.A.; Fonseca, F.L.A.; Machado Filho, C.A. Treatment of facial aging with calcium hydroxyapatite–Filling and lifting concept. Eur. J. Biol. Res. 2019, 9, 267–275. [Google Scholar]
- Davis, D.S.; Boen, M.; Fabi, S.G. Cellulite: Patient selection and combination treatments for optimal results—A review and our experience. Dermatol. Surg. 2019, 45, 1171–1184. [Google Scholar] [CrossRef]
- Palermo, E.C.; Anzai, A.; Jacomo, A.L. Three-dimensional approach of cosmetic patient: Aging gracefully. In Botulinum Toxins, Fillers and Related Substances; Springer International Publishing: Cham, Switzerland, 2019; pp. 199–220. [Google Scholar]
- Zarei, F.; Abbaszadeh, A. Application of cell therapy for anti-aging facial skin. Curr. Stem Cell Res. Ther. 2019, 14, 244–248. [Google Scholar] [CrossRef]
- Antonio, C.R.; Trídico, L.A. Cells biomodulation: The future of dermatology. Surg. Cosmet. Dermatol. 2019, 11, 11. [Google Scholar] [CrossRef]
- Aunna Pourang, M.; Rockwell, H.; Karimi, K. Rejuvenation, including stem cells and autologous. Facial Plast. Surg. Clin. N. Am. 2019, 28, 101–117. [Google Scholar] [CrossRef]
- Jáñez, L.; Tejero, P.; Battistella, M. Platelet-rich plasma applications, outcomes and security. In Regenerative Medicine Procedures for Aesthetic Physicians; Springer: Berlin/Heidelberg, Germany, 2019; Volume 8, pp. 139–150. [Google Scholar]
- Alessandrini, A.; Tretyakova, K. The rejuvenating effect and tolerability of an auto-cross-linked hyaluronic acid on décolletage: A pilot prospective study. Aesthetic Plast. Surg. 2018, 42, 520–529. [Google Scholar] [CrossRef] [PubMed]
- Centre for Evidence-Based Medicine. Oxford Centre for Evidence-Based Medicine: Levels of Evidence (March 2009) Oxford: University of Oxford. Available online: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/oxford-centre-for-evidence-based-medicine-levels-of-evidence-march-2009 (accessed on 5 February 2023).
| Agent | Key Advantages | Key Disadvantages | Preferred Indications | Age-Stratified Notes |
|---|---|---|---|---|
| PLLA | Durable neocollagenesis; adipocyte stimulation | Delayed onset; nodule risk if dilution/massage inadequate | Midface, temple, cheek; body laxity | 35–55 and ≥55 matrix anchor; micro-dosing ≤35 for prevention |
| PCL | ADSC scaffold; long-lasting ECM remodeling | Technique-sensitive; fewer large RCTs | Global laxity; jawline, neck, arms | 35–55 and ≥55 durability focus |
| CaHA | Immediate volume + regenerative effect | Plane-specific vascular risk; variability with hyper-dilution | Neck, lower face, gluteal, arms | All ages when early effect helpful; caution in thin dermis ≥55 |
| HA | Reversible; hydration/elasticity; contour refinement | Shorter durability; limited true biostimulation | Fine lines, contouring, hydration | ≤35 for texture; all ages for finishing |
| PRP/biologics | Low morbidity; metabolic/cellular support | Protocol heterogeneity; variable endpoints | Texture improvement, recovery, hair/dermal quality | ≤35 for prevention; fragile skin ≥55 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Österreichische Pharmazeutische Gesellschaft. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, K.W.A.; Kim, H.; Song, J.K.; Sydorchuk, O.; Ka Fai, W.; Rosellini, I.; Kim, H.; Lau, K.H.; Gold, M.H.; Yi, K. Injectable Biostimulator in Adipose Tissue: An Update and Literature Review. Sci. Pharm. 2025, 93, 62. https://doi.org/10.3390/scipharm93040062
Lee KWA, Kim H, Song JK, Sydorchuk O, Ka Fai W, Rosellini I, Kim H, Lau KH, Gold MH, Yi K. Injectable Biostimulator in Adipose Tissue: An Update and Literature Review. Scientia Pharmaceutica. 2025; 93(4):62. https://doi.org/10.3390/scipharm93040062
Chicago/Turabian StyleLee, Kar Wai Alvin, Heesoo Kim, Jong Keun Song, Olena Sydorchuk, Wong Ka Fai, Isabella Rosellini, Hongseok Kim, Kian Hong Lau, Michael H. Gold, and Kyuho Yi. 2025. "Injectable Biostimulator in Adipose Tissue: An Update and Literature Review" Scientia Pharmaceutica 93, no. 4: 62. https://doi.org/10.3390/scipharm93040062
APA StyleLee, K. W. A., Kim, H., Song, J. K., Sydorchuk, O., Ka Fai, W., Rosellini, I., Kim, H., Lau, K. H., Gold, M. H., & Yi, K. (2025). Injectable Biostimulator in Adipose Tissue: An Update and Literature Review. Scientia Pharmaceutica, 93(4), 62. https://doi.org/10.3390/scipharm93040062







