Abstract
Background: Traditional and evidence-based medicines, as seen depicted throughout human history, reportedly first begin with the application of medicinal plants, animal products, or inorganic minerals as a basic framework towards effectively engineering the prototypes generally aligned to pharmaceuticals and medical nutrition. The growing global trend of complementary treatments for glaucoma can be explained by the intraocular pressure (IOP)-independent mechanisms of the disease and its interpretation as a progressive neurodegenerative disorder. Unfortunately, the categorical positions of the major fields of applied popular complementary therapies and their relation to glaucoma are consistently neglected. Methods: In consideration of bibliographic resources, the most well-known online scientific databases were searched. Conclusion: The rising popularity and the trends of products coming onto the market cannot escape the attention of pharmacists and ophthalmologists, as their patients suffering from eye diseases are also increasingly looking for such medicinal products. Most of them still lack knowledge of the appropriate evidence and side effect profiles. Our proposed systematic charts demonstrate the position of each mainstream complementary therapy throughout the applied medical sciences and are distinctively unique; we could not find any similar relevant illustration or resource among the published international literature.
1. Introduction
It is estimated by the World Health Organization (WHO) that 60–80% of the population, especially in the developing world [1,2], are dependent upon complementary medical practices to relieve symptoms or to treat their health conditions, and 85% of these individuals rely on the use of herbs or herb-based products. These therapies represent a holistic approach to the human organism and its function [2]. Human history, in reference to traditional medicine, reportedly first began with the application of medicinal plants, animal products, or inorganic minerals as a basic framework to engineer prototypes regarding pharmaceuticals and medical nutrition. Classic examples characteristic of natural substances are salicylates (Salix spp.), digitalis glycosides (Digitalis lanata Ehrh. and D. purpurea L.), pilocarpine (Pilocarpus jaborandi Holmes), quinine (Cinchona officinalis L.), etc. [3,4]. The evolution of medicine is based upon empirical experience and prescientific observations leading to the construction of systematic therapy methods and practices. Recently, developing and ongoing evidence-based medical research and studies have yielded far more complex standardized therapies for the treatment of disease. Today, our world has far greater access to contemporary pharmacotherapy; however, developing countries, especially their rural areas, are indeed lacking in adequate healthcare and are confronted with unsatisfactory sanitation. Therefore, the only option is traditional medicine, which is sometimes either harmful or scientifically not yet fully substantiated. However, a growing tendency witnessed among developed nations is a return to classic ethnomedicinal practices, in particular, herb-based preparations [5]. The regular use of complementary therapies among mainstream European countries hovers at 49% in France, 46% in Germany, 35% in the United Kingdom, 31% in Belgium, and 25% throughout Northern Europe. In the majority of the countries, these naturopathic medical methods have not been officially recognized; however, an increasing demand emanating from both patients and healthcare professionals is reported [6]. The role of the classical medical substances can be factually demonstrated; statistically, 56% of prescribed pharmaceuticals are synthetic, of which 24% are herbal derivatives, 6% are directly extracted from plants, and 5% are of animal origin [3].
2. Challenges in Glaucoma
The heterogenous disease group of glaucoma is a progressive optic neuropathy causing vision loss; in 2022, it was the second leading cause of vision loss after cataracts [4]. The degeneration of retinal ganglion cells accelerates in the retinal nerve fiber layer, and its effect influences the visual pathway up to the visual cortex, causing visual field deficits. Early detection and proper treatment can decelerate the progression and preserve long-term visual function. Lowering the intraocular pressure (IOP), as the only modifiable risk factor, is the primary evidence-based therapeutic strategy, including topical medications, selective laser trabeculoplasty, and filtration surgeries. The growing global trend of complementary treatments for glaucoma can be further explained by the IOP-independent mechanisms, focusing on herbal remedies and diet. These molecular mechanisms create a cascade, rather than discrete events, and include the withdrawal of neurotrophic factors, oxidative stress, mitochondrial dysfunction, glutamate excitotoxicity, autophagy, protein misfolding, ischemia, and hypoxia [4,7].
Complementary medical practices consist in the application of several traditional and well-established herbal, mineral, or animal-related substances, mostly taught throughout pharmaceutical education. Moreover, these products can mostly be found in pharmacies in the form of dietary supplements, herb-based medications, foods (filtered teas), and cosmetics (essential oils, etc.) [8]. The number of herbal preparations used in ophthalmology, especially in the treatment of glaucoma, is currently low, but their increase can be predicted [9]. In a survey, 13.6% of glaucoma patients stated that they use complementary medicine in addition to their antiglaucoma eye drops, while 62.5% did not inform their treating ophthalmologist. Among their applied methods, 34.5% consisted of herbal therapy, 22.7% of diet, and 18.8% of dietary supplements [7,10]. An interesting result obtained from this study is that the use of complementary therapies was related to younger age, the severity of glaucoma disease, earlier diagnosis, greater use of topical therapy, previous anti-glaucoma surgery, higher education, and, finally, the effect of glaucoma on quality of life. At the same time, almost the same proportion of participants (40.5%) were satisfied with their complementary treatment as those who were not pleased (40.2%). Another interesting result is that only 16.7% of the patients were able to obtain information from their treating ophthalmologist about the complementary remedies used in glaucoma, while the role of the media (37.1%) was more representative [7,10]. Although North America was the primary site of the mentioned study, the growing trend of complementary treatments for glaucoma can be interpreted for the rest of the world. The rising popularity and the trend of even more products coming onto the market cannot escape the attention of ophthalmologists, as their patients suffering from cataracts, glaucoma, age-related macular degeneration (AMD), and diabetic retinopathy are also increasingly looking for such medicinal products [10,11,12]. As a recent example, in 2021, 22–67% of Middle Eastern patients applied complementary medicine, especially for their ophthalmic disease [13]. Most patients still lack knowledge of the appropriate evidence and side effect profiles [12].
In this article, we propose a novel classification system including appropriate definitions to demonstrate the complementary pharmacy-related medical sciences and their relation to glaucoma therapy. The categorical position regarding these complementary therapies in the major field of applied human medicines is, unfortunately, consistently neglected. We suggest a new type of classification specifically intended for phytomedicine-related applied complementary medical methods and well-founded evidence-based definitions, to effectively aid future healthcare professionals and medical researchers.
3. Materials and Methods
In consideration of the bibliographic resources, a thorough search was implemented in the most frequently applied online scientific databases, including PubMed.org, ScienceDirect.com, and Researchgate.net, using the following keywords: “Phytotherapy”, “Aromatherapy”, “Aromachology”, “Aromatology”, “Hydrosols”, “Apitherapy”, “Mycotherapy”, “Gemmotherapy”, “Hirudotherapy”, “Schüssler salts”, “Bach Flower Therapy”, “definition”, “classification”, “limitation”, “chart”, and various combinations.
4. Phytotherapy
4.1. Definitions and Description
Phytotherapy (or herbalism) is a major branch of medicine treating medical conditions, promoting health, and preventing diseases using plant-based substances. The origin of the term is Ancient Greek—“φυτόν” (plant) and “θεραπεία” (service, medical treatment)—and was first used in 1913 by Henri Leclerc, who described medicinal plants and their empirical therapeutic use in clinical trials [14]. Originally, it was representative of applied medicine and pharmacy; however, as of recently, it is now classified into complementary medicine. Practically, it does not differ from evidence-based pharmaceutical drug usage, yet in complementary medical practice, several plants may have non-official, non-evidence-based, or off-label applications. Phytotherapy generally uses the chemical composition and pharmacological activity of the source plant (either the entire herb, or a processed portion, e.g., buds, leaves, sprouts, flowers, fruits, seeds, bark, and/or roots) for therapeutic purposes [6,15]. According to Bürgi’s law, plant-derived remedies have combined synergistic effects, rather than just one useful molecule, so they cannot be simplified to a single pharmacologic mechanism [4]. Herb-based therapies are widely applied in all existing medical traditions, including anthroposophic medicine, Traditional Chinese Medicine (TCM), Ayurvedic medicine, Tibetan–Mongolian medicine, etc., including evidence-based medicine (EBM). Physicians and non-medical health practitioners may use either single-herb monotherapies or synergistic polytherapy believed to have adjuvant effects. Such therapies are often supported by non-herbal supplements, such as minerals, vitamins, or animal products [6,15].
4.2. Limitations
Most of the herbal formulas are not well established in human clinical research since the majority of them have been tried and justified only in animal experimental models or in vitro pilot studies. However, a few of them have become evidence based or been clinically trialed, while the rest of them were translated to possible human applications. Due to inevitable environmental factors, some herbal formulae may even contain some heavy metal contamination, and the effective molecular content cannot always be clearly identified. Further, according to Bürgi’s law of herbal synergism, one extracted useful molecule cannot always to be reduced to the same pharmacological effect that it has in synergism with other plant substances. Therefore, it is more difficult to produce evidence-based standardized herbal pharmacotherapy [4]. However, the rapid growth of the herbal product industry and the lack of corresponding regulations and legislation have caused the WHO and other regulatory bodies to be increasingly concerned with the safety and efficacy of herbal medicines. Phytotherapy is the most studied complementary medical field, as highlighted by the clinical and pharmacological results, but comprehensive evidence-based guidelines are still missing. Laymen and non-medical therapists often rely on rural ethnomedicinal oral or documented practices lacking scientific evidence, resulting in unintentional adverse side effects. Furthermore, patients are often exposed to internet fraud or the illegal market of herb-based products. The quality and quantity of over-the-counter herbal supplements and medications are questionable due to the unsatisfactory manufacturing regulations. Herbal monographs (such as those by the European Medicines Agency (EMA) and European Scientific Cooperative on Phytotherapy (ESCOP), etc.) comprise all scientifically proven botanical, pharmacological, and medical information, providing a clinical and evidence-based application “guideline” in support of phytotherapists [6].
4.3. Application in Glaucoma
In their review, Kovács-Valasek et al. enumerated at least 16 herbs and herbal compositions with possible pharmacologic roles in complementary glaucoma therapy. These herbal compounds act on different molecular pathways that affect IOP change, inflammation, apoptosis, neurodegeneration, ocular ischemia, and neovascularization [4]. Early pharmacological treatments of glaucoma relied on herbal remedies and diet. Pilocarpine, a parasympathomimetic alkaloid still used for primary angle closure glaucoma (PACG) management, is extracted from Pilocarpus jaborandi Holmes and causes ciliary muscle contraction, facilitating aqueous humor outflow through the trabecular meshwork [4]. Herbal remedies are not always safe for glaucomatous patients, as Edington et al. reported that Hypericum perforatum L. may affect IOP control. It interacts with several drugs, including β-blockers, as it induces the cytochrome P450 system and causes faster drug metabolism in the ciliary body, iris, and retinal pigment epithelium (RPE) in human eyes. The resulting suboptimal IOP control can be improved on discontinuation of the herb [4].
5. Aromatherapy
5.1. Definitions and Description
Aromatherapy is the art and clinical science utilizing naturally extracted lipophilic essential and vegetal oils, including hydrophilic herbal essences, in medical curative processes while promoting mental–physical wellness [16,17]. The term was created by Dr. René Maurice Gattefossé, in 1937 [18,19], and originates from Ancient Greek—“ἄρωμα” (scent, fragranced oil or plant, and spices) and “θεραπεία” (service and medical treatment). The essential products characteristic of aromatherapy include essential oils; their scientific pharmaceutical Latin name appears as aetheroleum, which has Greek roots (“αἰθήρ”—heaven, upper purer air, and/or ether). Essential oils are mostly pleasant-scented complex mixtures of mono- and sesquiterpenes and phenylpropane derivatives. According to some surveys, aromatherapy is the second most popular complementary medical practice in the U.K. [20] and has become a worldwide, fast-growing holistic treatment practice.
Aromachology describes the effects of essential oil scents on human cognitive functions, behavior, emotional status, and, comprehensively, psychological interrelationships. The aromatic scent characteristic of essential oils stimulates the cerebral olfactory pathways, particularly the anatomical parts of the limbic system. The results are based on the subjective emotional status and well-being [21]. Aromatology assesses the physicochemical features and biological–pharmacological activity of essential oils. Furthermore, internal (per os) application is connected to aromatology, characterizing the continental (French) medical aromatherapy practices (excluding the English aromatherapy school) [21]. The clinical practice is divided by its geographical origin: the popular and esoteric English aromatherapy is based mostly on Ayurvedic medicine and aromachology, practiced in Great Britain; the medical-associated French aromatherapy, on the contrary, is characterized by the scientific chemistry based on aromatology [21]. A relatively new field is hydrosol aromatherapy, anecdotally referred to as “the homoeopathic aqueous extracts of plants and essential oils” (Figure 1.). Hydro-distillation is the most well-known technology applied to obtain the main products used in aromatherapy. The distilled aqueous phase, in the form of hydrosol, is a by-product, yet it possesses hydrophilic or partially hydrophobic aromatic components with appropriate pharmacological bioactivities. Hydrosol aromatherapy applies hydrosols with the same indications as those of essential oils as affordable and safer alternatives [22,23,24]. Aromatherapists practice their field of profession in several ways. Ali et al. (2015) classified aromatherapy in their review into five fields of application: massage, medical, psycho-, cosmetical, and olfactory aromatherapy [25].
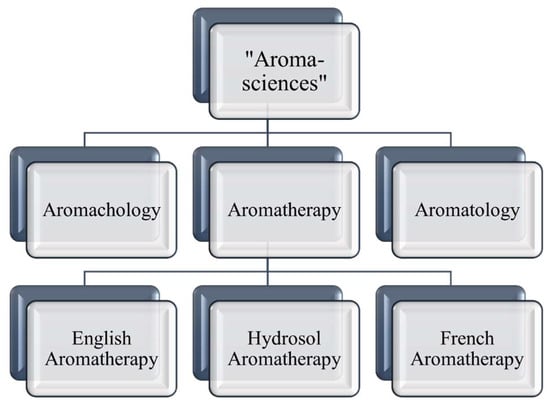
Figure 1.
Summarized chart representing the “Aroma-sciences”. The recent scientific literature and databases lack an official description regarding “Aroma-sciences”; therefore, for this purpose, we summarize them in a self-made chart.
5.2. Limitations
Essential oils are complex products comprising lipophilic herbal agents in a very concentrated means; therefore, the oral application of these oils is considerably limited. Although essential oil demand is emerging in the global market, its “omnipotent” marketing often leads to illegal plant harvesting and essential oil counterfeiting. In addition to the ecological hazard, counterfeited essential oils have no pharmacological effect and are often toxic. Essential oils also have adverse side effects when applied either internally (nausea, vomiting, liver, kidney damage, etc.) or externally (epilepsy, allergy, glaucoma, migraine, burns, dermatitis, etc.). The most common effects are skin irritation and contact dermatitis [20]. To prevent these harmful events and quackery, herbal monographs (EMA, ESCOP, etc.) and the scientific aromatherapy literature also contain various medical descriptions and applications of essential oils.
5.3. Application in Glaucoma
Aromatherapy may be an effective intervention for alleviating blindness-associated anxiety (13–30%), depression (11–25%), and sleep disturbances in glaucomatous patients (Flammer syndrome) [26,27,28]; however, to date, the effects remain inconclusive. Sabel et al. (2018) summarized the psychological impact in glaucomatous patients, finding that 80% experienced negative emotional reactions after their glaucoma diagnosis, and one-third were afraid of going blind [27]. Higher levels of anxiety and depressive symptoms were associated with faster progression of perimetric visual field loss in more patients with PACG than in those with primary open-angle glaucoma (POAG) [27]. In normotension glaucoma (NTG), stress was previously clearly identified as a major risk factor causing vascular dysregulation of the optic nerve head and retina [27,28]. Logically, aromatherapy may have a potential role in normalizing blood pressure or ameliorating the sleep pattern and coping with stress [26], although we do not know of any current aromatherapy-related clinical study treating glaucoma, proving the effect of the aforementioned risk factors.
An interesting question is the “citral” problem in glaucomatous eyes. Leach and Lloyd, in 1955, found that orange oil, prepared from orange peel, and a hydrochloride extract were both strongly active in raising the IOP in rabbits and monkeys. They identified the active substance as citral, and its additive oral ingestion might be an important factor causing secondary glaucoma. Citral is a monoterpene aldehyde covering two geometric isomers, geranial (trans(E)-citral or citral A) and neral (cis(Z)-citral or citral B). Aromatherapist guidelines discourage patients with glaucoma from applying high-citral-containing essential oils, e.g., Backhousia citriodora F.Muell. (90–98%), Litsea cubeba (Lour.) Pers. (90%), Cymbopogon schoenanthus Spreng. and Cymbopogon citratus (DC.) Stapf (65–85%), Leptospermum petersonii F.M.Bailey (70–80%), Ocimum gratissimum L. (66.5%), Corymbia citriodora (Hook.) K.D. Hill & L.A.S.Johnson (65%), Citrus × aurantium L. (36%), Aloysia citriodora Paláu (30–35%), Eucalyptus staigeriana F.Muell. ex F.M.Bailey (26%), Melissa officinalis L. (11%), Citrus × aurantiifolia (Christm.) Swingle (6–9%), and Citrus × limon (L.) Osbeck (2–5%). Later, Rodger and Saiduzzafar et al. repeated the experiments, but they could not reproduce the same effect conclusively [29,30,31,32]. With the lack of a proven IOP-increasing effect, aromatherapists must not discourage the usage of citral-containing essential oils in glaucomatous patients, but regular ophthalmic examinations are recommended.
6. Gemmotherapy
6.1. Definitions and Description
Gemmotherapy is a recently developed therapeutic technique based on the application of extracts obtained by the ethanolic or glycerolic maceration of fresh meristematic plant tissues, primarily buds (gemma in Latin) and sprouts, on the basis of the plant’s medical properties [6]. These principles originate from the experiments of the Ukrainian researcher Professor Filatov (Odessa University); however, the evolution of gemmotherapy as a therapeutic method is credited to the Belgian physician Dr. Paul Henry, from Brussels, who announced his results in 1954. These bud preparations reportedly contain a vital source of energy (high levels of vitamins and terpenic and phenolic compounds) and consist of herbs with much more potential agents than in the classic phytotherapeutic use of adult plants. The active substances are characterized by the presence of growth factors, such as gibberellins and auxins. In comparison with adult herb preparations, buds contain pharmacologically more active compounds, which are considerably more suitable in effectively treating definitive human diseases and/or promoting health. As a raw material, they are applied in both the herbal and cosmetic industries [6,33].
6.2. Limitations
Bud derivatives are a novelty in complementary medicine, yet they are still poorly studied. Regarding gemmotherapeutic preparations, therapists encounter several difficulties: Fresh buds must be harvested, generally from spontaneously grown plants, in a very limited period (late winter and/or early spring) corresponding to the annual germination of the chosen medical plant. During this time, the plant may not present its distinctive characteristics; hence, the attribution of the species may prove difficult for the collector. From another perspective, the manufacturing process and the extraction protocols are not strictly defined, regulations are rarely enforced, and results are deficient [6].
6.3. Application in Glaucoma
Vaccinium myrtillus L. is used to cure retinal vascular fragility, glaucoma, and AMD, but its bud preparation has not been properly researched. Among the four major anthocyanins discovered in the buds of Ribes nigrum L., delphinidin-3-O-rutinoside was the most prevalent, followed by cyanidin-3-O-rutinoside. In healthy humans, the administration of blackcurrant anthocyanins for 2 weeks significantly decreased the IOP. The effect on visual function was also studied on glaucoma patients: 24 months of administration decreased the IOP, delayed visual field loss, and elevated ocular blood flow. The exact mechanisms have not been thoroughly studied, but one proposed hypothesis mentioned plasma endothelin-1 (ET-1), serving as a potent vasoconstrictor, which has been suggested to play a role in the local autoregulation of blood flow in glaucomatous patients, especially in NTG [4,27,34].
7. Bach Flower Therapy
7.1. Definitions and Description
Bach Flower Remedies (BFRs) or Bach Flower Therapies are alcoholic fresh flower tinctures, highly diluted and similar to homoeopathy in principle. These remedies are manufactured using two steps: first, obtain the “mother tincture” by placing a fresh flower into rock water with plenty of sunshine; second, add the first solution to brandy (alcoholic component). The products are based on a definite thirty-eight remedies (thirty-seven plants and rock water), which do not contain pharmacologically relevant active agents; however, they are scientifically unproven and believed to possess subtle forms of self-healing energy [35,36]. The remedies and the theory regarding this therapy were invented by the British physician Dr. Edward Bach in the 1930s, and they were recognized by the WHO in 1974 [2,36]. According to Bach’s principles, BFRs can be used on any kind of medical condition; however, they are widely used in civilization-associated psychological problems, such as for treating stress and anxiety [36,37]. Dr. Bach distinguished seven emotional or personality groups, across which the thirty-eight flower essences are categorized, as depicted in Table 1 [36,38].

Table 1.
Basic materials of Bach Flower Remedies classified by Dr. Edward Bach according to the seven emotions. (Self-edited table based on the studies of Dr. Bach and other reviews [36,38].) The table demonstrates the numeric ordinal, traditional English and scientific names, and indications of Bach flowers.
BFRs are also available in the following application forms in clinical practice: tinctures, skin creams, pastilles, chewing gums, dissolvable capsules, lozenges, effervescent tablets, and liquid sprays. Dr. Bach created a special combination remedy, the Rescue Remedy, for emergency cases (combating fear, panic, shock, and fear of losing control), which consists of Prunus cerasifera Ehrh., Clematis vitalba L., Impatiens glandulifera Royle, Helianthemum nummularium (L.) Mill., and Ornithogalum umbellatum L. [36,39].
7.2. Limitations
More studies suggest that Bach Flower Therapy has a lower rate of evidence, and while its therapeutic use is limited and uncertain, it is likely safe [36]. Although BFRs have demonstrated potential roles in pain management and minor psychiatric disorders, there is no specific evidence beyond the placebo effect. BFRs’ mode of action is dependent not on molecular or pharmacological mechanisms but on the subtle forms of “energy”. The application of flower remedies may likely become hazardous when treating severe forms of disease. Professional BFR organizations set up the following indications: anxiety/stress, depression, general mental stress, lack of confidence, etc., associated with emotional and physical traumas; however, various studies report successful results treating other diseases (e.g., temporal–mandibular joint dysfunction, teething difficulties, low back pain, eczema, hypertension, migraines, attention-deficit hyperactivity disorder, drug and alcohol addictions, motion sickness, allergies, asthma, insomnia, nocturnal enuresis, etc.). Conclusions from the available clinical trials have failed to demonstrate convincing evidence differentiating from the use of a placebo [35,39].
7.3. Application in Glaucoma
There is no mention of BFRs in evidence-based literature, even in nonscientific texts associated with glaucoma. BFRs are produced to relieve psychosocial and mental symptoms; therefore, glaucomatous patients can take them regardless of their ocular disease. However, psychosocial distresses, depression, fear of blindness, and other mental disorders are quite frequent in glaucomatous patients, and there is no evident relationship between BRFs and glaucoma progression [4,27,36].
8. Mycotherapy
8.1. Definitions and Description
Culinary and medicinal mushrooms and their extracts (such as Pleurotus giganteus (Berk.) Karun. & K.D.Hyde, Ganoderma lucidum Karst, Hericium erinaceus (Bull.) Persoon, Lentinula edodes (Berk.) Pegler, etc.) are commonly produced and applied worldwide as dietary supplements, nutraceutical foods, and pharmaceutical drugs. The important health benefits demonstrated comprise a broad spectrum of pharmacological bioactivities, including anti-inflammatory, antioxidative, immunomodulating, and neuroprotective effects [40,41,42,43]. The most popular indication of these natural mushroom compounds has been linked primarily to the modulation of the immune system and specific molecular targets of cell functions, including cell proliferation, cell survival, and angiogenesis, by branched polysaccharides (glucans), sesquiterpenes, glycoproteins, or peptide/protein-bound polysaccharides. They also have a large number of bioactive compounds, such as alkaloids, antibiotics, and metal-chelating agents, making them useful pharmaceutic ingredients. Medicinal mushrooms are a rich source of carbohydrates, proteins, fibers, minerals, and vitamins (e.g., thiamin, riboflavin, ascorbic acid, and vitamin D) and are low in calories and fat, contributing to overall health benefits. Recently, they have become popular throughout Europe, although they have been applied in Asian traditional medicine and cuisine for thousands of years [40,41,42,43].
8.2. Limitations
The growing interest in mycotherapy requires a strong commitment towards expanding scientific clinical trials. Most of the data originate from in vitro and in vivo experimental models. The small number of studies unfortunately limits the evidence-based application of mycotherapy in everyday practice [42].
8.3. Application in Glaucoma
Bioactive metabolites from fungal endophytes are important sources for mycotherapy. The Ganoderma genus produces many biologically active triterpenoids, and 35 compounds from Ganoderma lucidum were screened by Amen et al. for their Rho-kinase inhibitory activity. Their results suggest that the traditional uses of G. lucidum, with its lanostane triterpenes, might be in part due to its ROCK-I and ROCK-II inhibitory potential. Synthetic Rho-kinase inhibitors have emerged as potential therapeutic agents to treat disorders such as glaucoma, so these findings would be helpful for the design of natural Rho-kinase inhibitors [44,45]. The Xylariaceae family comprises mostly small ascomycetous fungi, and their metabolites have shown antioxidant and anti-inflammatory activities. Lin et al. examined the retinoprotective compound Theissenolactone C (LC53), which is a fungal derivate extracted from Theissenia cinerea Y.M. Ju, J.D. Rogers & H.M. Hsieh (Xylariaceae). According to their results, the application exerted a retinal protective effect through NF-κB inhibition and was highly potent against MMP-9 activities after high-IOP-induced retinal injury. This suggests a promising drug possibility for glaucoma or ocular-related medical conditions attributed to retinal ischemia [45]. The results of both above-mentioned studies need to be examined in human glaucomatous patients in clinical trials to obtain evidence-based information about the possible potential in glaucoma complementary therapy.
9. Apitherapy
9.1. Definitions and Descriptions
Apitherapy is the application of honeybee (Apis mellifera L.) and beehive-related products such as honey, pollen, propolis, royal jelly, bee bread, bee venom (apitoxin), beeswax, apilarnil, and beehive air in disease prevention, health promotion, and curative treatment [8,46,47,48] (Figure 2). Globally, this is a well-known aspect of traditional medicine that was popularly used in the past much as it is today. According to the oldest human historical findings, honey collecting dates back some 9000 years. In written sources, its use stretches back to ancient Egypt, and it is also used in Traditional Chinese and Tibetan Medicine. Hippocrates, the great ancient Greek physician, described the biological properties of honey and pollen applied to sores and wounds [8,46,49].
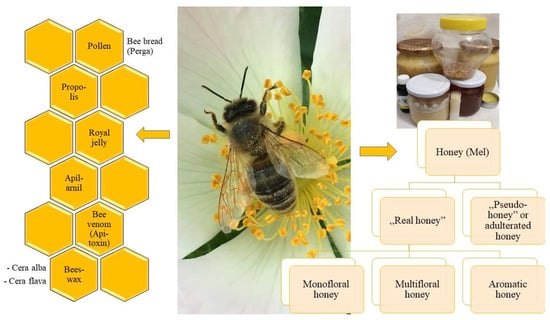
Figure 2.
Classification and illustration of products used in apitherapy. (Self-edited and photographed image. The central image is of Apis mellifera L., courtesy of the photographer, Dr. Gina Vágó, Bőszénfa, Hungary, 2020.).
Honey (mel in Latin) is a supersaturated aqueous, slightly acidic (pH 3.2 to 4.5) solution with high nutritional value collected and processed by various Apis spp. through repeated digestion and regurgitation of the nectar of plants. The chemical structure of this pure and functional food is dependent upon geographical and botanical diversity, containing 70–80% carbohydrates (glucose and fructose), a-tocopherol, ascorbic acid, phenolics, amino acids, minerals, vitamins, trace elements, and enzymes such as glucose oxidase, catalase, and peroxidase [50,51]. Honey can be classified into four clusters based on its origin: Pure, monofloral honey is derived from a single herb and has a higher market value when compared with multifloral honey, which contains more bioactive compounds from a variety of herbs. Aromatic honey is a natural and not-human-made product using essential oils or herbal parts to add bioactive components into the base honey. Adulterated honey (or “pseudo-honey”) is a totally or partially human-made product using fructose or other plant-based carbohydrates [52,53,54] (Figure 2).
Propolis is a resinous material collected and produced by Apis spp. from the buds and exudates of plants, mixed with bee enzymes, pollen, and beeswax. The term originates from Ancient Greek—“πρό” (before) and “πόλις” (city). This antiseptic–antimicrobial material defends the structure and the colony of the beehive [55].
Pollen is a natural product in the anthers of spermatophytes and has an essential role in the reproduction of entomophilous (insect-pollinated) plant species. It is collected by Apis spp. and utilized as a valuable nutrient, rich in proteins, vitamins, and minerals. Bee bread (perga) is a special mixture of pollen in the form of granules which is fermented and agglutinated by nectar and enzymes (e.g., amylase and catalase) secreted by honeybee salivary glands [48,56].
Royal jelly (some resources reference it as bee milk) is a white and viscous jelly-like “super-food” and is defined as a form of hypopharyngeal and mandibular gland secretion from the worker bees, consumed by the queen bee and larvae. Royalactin is the main compound in royal jelly, which allows the morphological change of a larva into the queen bee. It is widely used as a dietary supplement with various pharmacological uses [57].
Apilarnil is a bee-related product rich in androgenic substances, obtained from drone bee larvae, containing dry matter (25–35%), proteins (9–12%), carbohydrates (6–10%), lipids (5–8%), ash (2%), and 3% other materials. Its bioactivity is mostly aphrodisiac and neuroprotective [58,59].
Beeswax (Cera flava, “yellow wax”) is naturally produced by the wax glands of Apis mellifera L. using honey sugars (fructose, glucose, and sucrose) as raw materials. Purified or bleached beeswax is referred to as Cera alba (“white wax”) [60].
Notably, bee venom (or apitoxin) is essentially a very complex mixture of natural secondary metabolites extracted from Apis mellifera L. containing more than sixty identifiable bioactive components such as peptides, enzymes, biologically active amines, and non-peptides. There are several documented health conditions in which bee venom has been used therapeutically, such as treating arthritis or neurodegenerative disorders. Introducing bee venom into the human body by manual injection or by direct living bee stings is referred to as apipuncture. Bee venom also can be used in topical skin ointments [49,61,62].
9.2. Limitations
The potential benefit of bee-related products is supported by the positive experiences of a large group of beekeepers and apitherapists, who use these products to treat a wide range of medical conditions without substantiated scientific evidence. An important factor associated with apitherapeutic medicines is human safety. Additionally, reasons of contraindications and lack of compliance regarding an allergic history or intolerance against even smaller amounts of honey, or disliking the taste of pollen and royal jelly, obscure the issue regarding the actual benefits [8,46,47,56,63]. Furthermore, apipuncture treatments lead to pain and subsequent local or general edema, and in some cases, allergic reactions have been reported from areas such as South Korea, in which bee venom apitherapy is traditionally used. Apitherapy practitioners should be trained in managing anaphylactic reactions in patients until they can be admitted to an intensive care unit [56,62,63]. Finally, the potential risks regarding the consumption of organic bee pollen, honey, etc., include contamination by fungal mycotoxins, pesticides, or toxic metals. Due to the presence of Botulinum toxin, the consumption of honey by toddlers under 1–2 years old must be avoided. Lastly, the limited amounts of genuine honey samples result in the potential degradation of herbal proteins and bioactive compounds during the conversion of nectar into honey. On the other hand, honey contains several other compounds that were not originally present in the nectar. Therefore, the pharmacological properties of the original herbs and honey are not consistently equivocal [8,46,47,56,63,64].
9.3. Application in Glaucoma
Even Aristotle (350 BC) mentioned that honey is a good medicine for eye diseases. The application of honey in glaucoma therapy, according to the medical literature, is mainly based on the principles of Ayurvedic medicine. Therefore, to reduce the IOP and improve the flow of aqueous humor, it is recommended to use a solution of honey with Camphora officinarum Nees, Zingiber officinale Roscoe, and Citrus × limon (L.) Osbeck in the form of drops for patients with glaucoma. The formula needs further scientific proof due to a lack of clinical evidence. Okuda et al. experimentally placed honeycombs with honey in rabbits as an adhesive barrier during glaucoma filtration procedures. The honeycombs were placed inside the subconjunctival pocket. Lower IOP values and a lower percentage of inflammatory postoperative complications were observed compared to the other group of rabbits treated with mitomycin C in trabeculectomy [54]. In TCM, dense honey-based solutions are given to glaucomatous patients to drink in case of elevated IOP. The honey is not equivalent to glycerol or mannitol, but osmotically active substances have been applied since ancient times to reduce the IOP [65].
10. Hirudotherapy
10.1. Definitions and Description
Hirudotherapy (or Medicinal Leech Therapy) is the application of farm-cultured medicinal leeches (Hirudo spp.) to a human host’s skin, which is used to treat several disorders and has been in existence for thousands of years, throughout the history of human ethnomedicine and in every culture spanning the globe. Hirudotherapy reached its therapeutic peak of popularity on the European continent in the 17th century, and it has since been revived in the last decade among complementary human and veterinary forms of medicine. Today, more than 300 prescriptions containing Hirudo spp. exist in the clinical practice of Traditional Chinese Medicine, a practice lasting some 2000 years, referred to as Shuǐzhì or Mǎhuáng. Hirudo medicinalis L. saliva has more than twenty reported bioactive compounds (the most relevant include the following ingredients: hirudin, bdellin, apyrase, eglin, destabilase, hyaluronidase, lipase, esterase, anti-elastase, and calin) as vasodilative, anti-inflammatory, analgesic, antimicrobial, and anticoagulant agents [66,67,68,69,70,71,72]. The application of the bioactive components of Hirudo medicinalis L. in dermal ointments is used to alleviate the symptoms of crural varices or skin hematomas and is also a form of hirudotherapy.
10.2. Limitations
The complications of hirudotherapy, according to various studies, are classified into five clusters—infection (51%), allergy (21%), prolonged bleeding (15%), migration to different body parts (8%), and other (5%). Bacterial infection is inevitable without the use of prophylactic antibiotics (ciprofloxacin, sulfamethoxazole/trimethoprim, and second- and third-generation cephalosporins). The most common allergic reactions are skin erythema, edema, and the formation of a central black eschar on the skin, for instance. Prolonged bleeding is defined as bleeding continuously for more than two hours despite compression, which can cause severe anemia and hemorrhagic shock. A hirudotherapist should be aware of contraindications—hemophilia, leukemia, arterial insufficiency, hypotension, septic disorders, cachexia, hepatobiliary diseases, HIV infection, and the use of anticoagulants and immunosuppressants—while avoiding the treatment of pregnant or lactating individuals and children under sixteen years of age. The skin surfaces of the epigastric, liver, spleen, and gluteal regions must be avoided. Daily clinical assessment is necessary [66,72,73].
10.3. Application in Glaucoma
Currently, in some countries of Eastern Europe, Russia, and South Asia (Indian peninsula, Sri Lanka), hirudotherapy is officially recognized as a classic alternative therapy for diseases and symptoms such as glaucoma. In South Asia, hirudotherapy (Irsal-e-Alaq), as a part of Unani medicine (which has its roots in Ancient Greco-Roman medicine), can offer a complementary approach for all forms of glaucoma (maa-e-aksa). The hirudotherapists place 2–4 leeches on the lower temporal and supraorbital regions. An important reduction in the IOP is usually observed in about 3 h. A significant reduction in the IOP and improvements in visual acuity and ocular hydro- and hemodynamics were observed by Belezkaya et al. after a course of hirudotherapy (2–6 leeches daily for 2 weeks). They recommend it in the terminal stages of glaucoma, when almost all therapeutic and surgical methods of treatment are unsuccessful. However, while hirudotherapy was able to prevent complete blindness in some studies, it lacks scientific evidence for validation. Therefore, hirudotherapy is generally not recommended as a complementary cure for glaucoma [72,73].
11. Systematic Overview and Future Prospects
Medicine is a continuously developing universal system comprising all the holistic approaches regarding human pathology–pathophysiology and various therapeutic methods. The most recently officially recognized medicine is referred to as EBM. Those countries in which parallel medical systems exist are characterized as “Western Medicine” or “Allopathic Medicine” to EBM. It is universally described that every medical system possesses its own pharmaceutical practice based on plants, fungi, animal products, and minerals. Phytomedicinals are the most ancient materials used in disease prevention, health promotion, and curative treatment; therefore, phytotherapy (or herbalism) is a major element in pharmacy. In countries in which phytotherapy is an officially recognized therapeutic process with a state-accredited examination, including certification, phytotherapic practice consists of subspecializations including aromatherapy, mycotherapy, and apitherapy. In the authors’ professional opinion, gemmotherapy, as a new entity, is also a branch of phytotherapy according to its products. BFRs, sold mostly in pharmacies, are plant-based alcoholic tinctures; however, the pharmacologic agents and the philosophy of the therapy have a homoeopathic basis. Therefore, we suggest Bach Flower Therapy as a frontier field including both homoeopathy and phytotherapy. Fungi also possess pharmacologically active components applied in human and veterinarian medicine; therefore, mycotherapy is also growing in importance. Schüssler Cell/Tissue Salts contain homeopathically potentized doses of essential minerals [74] and are not plant-based inorganic products; however, their manufacturing process is homoeopathic-based. Additional characteristics are not available, due to the lack of clinical trials and scientific evidence associated with the Schüssler Salts, which can be considered as a limitation. Distinctly, Figure 3 demonstrates the systematic position of each complementary medical science.
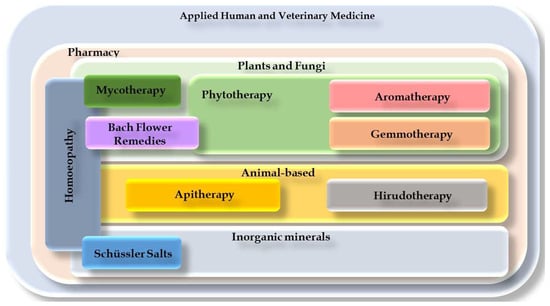
Figure 3.
Positions of plant-based therapy systems and their frontier areas in contemporary medicine—self-edited chart. Applied human and veterinary medicine systems holistically consist of the subdivisions “Western” or “Allopathic” EBM and complementary medicinal systems (TCM, Ayurvedic medicine, Tibetan–Mongolian medicine, anthroposophic medicine, etc.).
The rate of regular use of complementary therapies among the main European countries hovers between 25% and 49% [6]. In the majority of these countries, naturopathic medical methods have not been officially recognized, yet an increasing demand by both patients and healthcare professionals is distinctly observed [6]. Complementary medical practices consist in the application of several traditional and well-established herbal, mineral, or animal-related substances, mostly taught throughout pharmaceutical education. Moreover, these products are found mostly in pharmacies in the form of dietary supplements, herb-based medications, foods (filtered teas), and cosmetics (essential oils, etc.) [8]. In the future, more and more bioactive compounds of plant and animal origin may become official medicines. However, identifying the right formulation, the purity of the active ingredients, and the possibility of illegal additives and synthetic counterfeiting that prioritize profit could be a serious problem. Supervision of natural medicines is important to ensure that they remain safe for patients. Reliable pharmacobotanic analytical techniques (such as high-performance liquid chromatography (HPLC), high-performance thin-layer chromatography (HPTLC), liquid chromatography–tandem mass spectrometry (LC-MS/MS), nuclear magnetic resonance (NMR) analysis, capillary electrophoresis (CE), thin-layered chromatography combined with surface-enhanced Raman spectroscopy (TLC-SERS), and densitometry) [75] are already at our service and will play an increasingly prominent role in the future.
12. Conclusions
The rising popularity and the trends of medicinal products coming onto the market cannot escape the attention of ophthalmologists, as their patients suffering from eye diseases are increasingly looking for such products. According to surveys, a significant number of glaucoma patients are applying complementary medication without disclosing it to their treating ophthalmologist or pharmacist. Most of them still lack knowledge of the appropriate evidence and side effect profiles. In this article, we proposed a novel classification system highlighting appropriate definitions to demonstrate the complementary pharmacy-related medical sciences. The proposed systematic charts demonstrating the position of each mainstream complementary therapy in the applied medical sciences are distinctly unique, since there is no trace of any similar relevant illustration or resource throughout the published international literature. Healthcare professionals should be prepared for the popular pharmacy-related complementary sciences to serve the needs of their patients, while alerting them to the limitations, hazards, and contraindications of these products and interventions.
Author Contributions
T.R.: Conceptualization, Methodology, Investigation, Resources, Writing, Visualization. A.C.: Professional review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Acknowledgments
The authors express their gratitude to Gina Vágó for the photographed image used for Figure 2.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
| AMD | Age-Related Macular Degeneration |
| BFRs | Bach Flower Remedies |
| EBM | Evidence-Based Medicine |
| EMA | European Medicines Agency |
| ESCOP | European Scientific Cooperative on Phytotherapy |
| ET-1 | Endothelin-1 |
| IOP | Intraocular Pressure |
| MMP-9 | Matrix Metalloproteinase-9 |
| NF-κB | Nuclear Factor Kappa B |
| NTG | Normotension Glaucoma |
| PACG | Primary Angle Closure Glaucoma |
| POAG | Primary Open-Angle Glaucoma |
| RPE | Retinal Pigment Epithelium |
| TCM | Traditional Chinese Medicine |
| WHO | World Health Organization |
References
- WHO. WHO Global Report on Traditional and Complementary Medicine; World Health Organization: Geneva, Switzerland, 2019; ISBN 978-92-4-151543-6. [Google Scholar]
- de Carvalho Resende, M.M.; de Carvalho Costa, F.E.; Gardona, R.G.B.; Araújo, R.G.; Mundim, F.G.L.; de Carvalho Costa, M.J. Preventive Use of Bach Flower Rescue Remedy in the Control of Risk Factors for Cardiovascular Disease in Rats. Complement. Ther. Med. 2014, 22, 719–723. [Google Scholar] [CrossRef] [PubMed]
- Sen, T.; Samanta, S.K. Medicinal Plants, Human Health and Biodiversity: A Broad Review. Adv. Biochem. Eng. Biotechnol. 2014, 147, 59–110. [Google Scholar] [CrossRef]
- Kovács-Valasek, A.; Rák, T.; Pöstyéni, E.; Csutak, A.; Gábriel, R. Three Major Causes of Metabolic Retinal Degenerations and Three Ways to Avoid Them. Int. J. Mol. Sci. 2023, 24, 8728. [Google Scholar] [CrossRef] [PubMed]
- Colalto, C. What Phytotherapy Needs: Evidence-Based Guidelines for Better Clinical Practice. Phyther. Res. 2018, 32, 413–425. [Google Scholar] [CrossRef] [PubMed]
- Donno, D.; Mellano, M.G.; Cerutti, A.K.; Beccaro, G.L. Biomolecules and Natural Medicine Preparations: Analysis of New Sources of Bioactive Compounds from Ribes and Rubus spp. Buds. Pharmaceuticals 2016, 9, 7. [Google Scholar] [CrossRef] [PubMed]
- Wan, M.J.; Daniel, S.; Kassam, F.; Mutti, G.; Butty, Z.; Kasner, O.; Trope, G.E.; Buys, Y.M. Survey of Complementary and Alternative Medicine Use in Glaucoma Patients. J. Glaucoma 2010, 21, 79–82. [Google Scholar] [CrossRef] [PubMed]
- Trumbeckaite, S.; Dauksiene, J.; Bernatoniene, J.; Janulis, V. Knowledge, Attitudes, and Usage of Apitherapy for Disease Prevention and Treatment among Undergraduate Pharmacy Students in Lithuania. Evid. Based. Complement. Alternat. Med. 2015, 2015, 172502. [Google Scholar] [CrossRef]
- Ige, M.; Liu, J. Focus: Plant-Based Medicine and Pharmacology: Herbal Medicines in Glaucoma Treatment. Yale J. Biol. Med. 2020, 93, 347. [Google Scholar]
- Rák, T.; Kovács-Valasek, A.; Pöstyéni, E.; Csutak, A.; Gábriel, R. Complementary Approaches to Retinal Health Focusing on Diabetic Retinopathy. Cells 2023, 12, 2699. [Google Scholar] [CrossRef]
- Hassen, G.; Belete, G.; Carrera, K.G.; Iriowen, R.O.; Araya, H.; Alemu, T.; Solomon, N.; Bam, D.S.; Nicola, S.M.; Araya, M.E.; et al. Clinical Implications of Herbal Supplements in Conventional Medical Practice: A US Perspective. Cureus 2022, 14, e26893. [Google Scholar] [CrossRef]
- West, A.L.; Oren, G.A.; Moroi, S.E. Evidence for the Use of Nutritional Supplements and Herbal Medicines in Common Eye Diseases. Am. J. Ophthalmol. 2006, 141, 157–166. [Google Scholar] [CrossRef]
- Sim, R.H.; Sirasanagandla, S.R.; Das, S.; Teoh, S.L. Treatment of Glaucoma with Natural Products and Their Mechanism of Action: An Update. Nutrients 2022, 14, 534. [Google Scholar] [CrossRef] [PubMed]
- Petkova, V.; Hadzhieva, B.; Nedialkov, P. Phytotherapeutic Approaches to Treatment and Prophylaxis in Pediatric Practice. Pharmacia 2019, 66, 115–119. [Google Scholar] [CrossRef]
- Falzon, C.C.; Balabanova, A. Phytotherapy: An Introduction to Herbal Medicine. Prim. Care-Clin. Off. Pract. 2017, 44, 217–227. [Google Scholar] [CrossRef] [PubMed]
- Reis, D.; Jones, T. Aromatherapy: Using Essential Oils as a Supportive Therapy. Clin. J. Oncol. Nurs. 2017, 21, 16–19. [Google Scholar] [CrossRef] [PubMed]
- Fazlollahpour-Rokni, F.; Shorofi, S.A.; Mousavinasab, N.; Ghafari, R.; Esmaeili, R. The Effect of Inhalation Aromatherapy with Rose Essential Oil on the Anxiety of Patients Undergoing Coronary Artery Bypass Graft Surgery. Complement. Ther. Clin. Pract. 2019, 34, 201–207. [Google Scholar] [CrossRef]
- Boehm, K.; Büssing, A.; Ostermann, T. Aromatherapy as an Adjuvant Treatment in Cancer Care—A Descriptive Systematic Review. Afr. J. Tradit. Complement. Altern. Med. 2012, 9, 503–518. [Google Scholar] [CrossRef] [PubMed]
- Farrar, A.J.; Farrar, F.C. Clinical Aromatherapy. Nurs. Clin. N. Am. 2020, 55, 489–504. [Google Scholar] [CrossRef] [PubMed]
- Posadzki, P.; Alotaibi, A.; Ernst, E. Adverse Effects of Aromatherapy: A Systematic Review of Case Reports and Case Series. Int. J. Risk Saf. Med. 2012, 24, 147–161. [Google Scholar] [CrossRef]
- Wang, C.X.; Chen, S.L. Aromachology and Its Application in the Textile Field. Fibres Text. East. Eur. 2005, 13, 41–44. [Google Scholar]
- Georgiev, V.; Ananga, A.; Dincheva, I.; Badjakov, I.; Gochev, V.; Tsolova, V. Chemical Composition, in Vitro Antioxidant Potential, and Antimicrobial Activities of Essential Oils and Hydrosols from Native American Muscadine Grapes. Molecules 2019, 24, 3355. [Google Scholar] [CrossRef]
- Edris, A.E. Identification and Absolute Quantification of the Major Water-Soluble Aroma Components Isolated from the Hydrosols of Some Aromatic Plants. J. Essent. Oil-Bearing Plants 2009, 12, 155–161. [Google Scholar] [CrossRef]
- Santarsiero, A.; Onzo, A.; Pascale, R.; Acquavia, M.A.; Coviello, M.; Convertini, P.; Todisco, S.; Marsico, M.; Pifano, C.; Iannece, P.; et al. Pistacia Lentiscus Hydrosol: Untargeted Metabolomic Analysis and Anti-Inflammatory Activity Mediated by NF- κ B and the Citrate Pathway. Oxid. Med. Cell. Longev. 2020, 2020, 4264815. [Google Scholar] [CrossRef] [PubMed]
- Ali, B.; Al-Wabel, N.A.; Shams, S.; Ahamad, A.; Khan, S.A.; Anwar, F. Essential Oils Used in Aromatherapy: A Systemic Review. Asian Pac. J. Trop. Biomed. 2015, 5, 601–611. [Google Scholar] [CrossRef]
- Liu, J.; Cao, L.; Yang, G.; Zhou, R. Effects of Non-Pharmacological Interventions on Anxiety, Depression, and Sleep Quality in Patients with Postoperative Glaucoma: A Protocol for Systematic Review and Network Meta-Analysis. Medicine 2021, 100, E27090. [Google Scholar] [CrossRef] [PubMed]
- Sabel, B.A.; Wang, J.; Cárdenas-Morales, L.; Faiq, M.; Heim, C. Mental Stress as Consequence and Cause of Vision Loss: The Dawn of Psychosomatic Ophthalmology for Preventive and Personalized Medicine. EPMA J. 2018, 9, 133. [Google Scholar] [CrossRef]
- Shin, D.Y.; Jung, K.I.; Park, H.Y.L.; Park, C.K. The Effect of Anxiety and Depression on Progression of Glaucoma. Sci. Rep. 2021, 11, 1769. [Google Scholar] [CrossRef]
- Southwell, I. Backhousia Citriodora F. Muell. (Lemon Myrtle), an Unrivalled Source of Citral. Foods 2021, 10, 1596. [Google Scholar] [CrossRef]
- Lis-Balchin, M. The Safety Issue in Aromatherapy. Aromather. Sci. Guid. Healthc. Prof. 2005, 17, 86–87. [Google Scholar]
- Rodger, F.C.; Grover, A.D.; Saiduzzafar, H. The Effect of Citral on Intraocular Dynamics in Monkeys. AMA. Arch. Ophthalmol. 1960, 63, 77–83. [Google Scholar] [CrossRef]
- Saiduzzafar, H. The Effect of Citral on Variations in the Aqueous Outflow Facility of Rabbits. Indian J. Ophthalmol. 1959, 7, 39. [Google Scholar]
- Sarkova, A.; Sarek, M. EAV and Gemmotherapy—Medicine for the next Millennium? (Technique as a Means to Link Eastern and Western Medicine). In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology, Shanghai, China, 17–18 January 2006; Volume 7, pp. 4943–4946. [Google Scholar]
- Cao, L.; Park, Y.; Lee, S.; Kim, D.O. Extraction, Identification, and Health Benefits of Anthocyanins in Blackcurrants (Ribes nigrum L.). Appl. Sci. 2021, 11, 1863. [Google Scholar] [CrossRef]
- Ernst, E. Bach Flower Remedies: A Systematic Review of Randomised Clinical Trials. Swiss Med. Wkly. 2010, 140, 29–31. [Google Scholar] [CrossRef]
- Thaler, K.; Kaminski, A.; Chapman, A.; Langley, T.; Gartlehner, G. Bach Flower Remedies for Psychological Problems and Pain: A Systematic Review. BMC Complement. Altern. Med. 2009, 9, 16. [Google Scholar] [CrossRef]
- Rivas-Suárez, S.R.; Águila-Vázquez, J.; Suárez-Rodríguez, B.; Vázquez-León, L.; Casanova-Giral, M.; Morales-Morales, R.; Rodríguez-Martín, B.C. Exploring the Effectiveness of External Use of Bach Flower Remedies on Carpal Tunnel Syndrome: A Pilot Study. J. Evid.-Based Complement. Altern. Med. 2017, 22, 18–24. [Google Scholar] [CrossRef]
- Howard, J. Do Bach Flower Remedies Have a Role to Play in Pain Control? A Critical Analysis Investigating Therapeutic Value beyond the Placebo Effect, and the Potential of Bach Flower Remedies as a Psychological Method of Pain Relief. Complement. Ther. Clin. Pract. 2007, 13, 174–183. [Google Scholar] [CrossRef]
- de Oliveira, F.N.; Okuyama, C.E.; de Souza Marquez, A.; Fernandes, K.B.; Dalaqua, P.V.; do Carmo, A.C.; Branco-Barreiro, F.C. Use of Bach Flower Remedies in Children and Adolescents with Attention Deficit Hyperactivity Disorder: Systematic Review and Meta-Analysis. Adv. Integr. Med. 2023, 10, 93–100. [Google Scholar] [CrossRef]
- Yadav, S.K.; Ir, R.; Jeewon, R.; Doble, M.; Hyde, K.D.; Kaliappan, I.; Jeyaraman, R.; Reddi, R.N.; Krishnan, J.; Li, M.; et al. A Mechanistic Review on Medicinal Mushrooms-Derived Bioactive Compounds: Potential Mycotherapy Candidates for Alleviating Neurological Disorders. Planta Med. 2020, 86, 1161–1175. [Google Scholar] [CrossRef]
- Zmitrovich, I.V.; Belova, N.V.; Balandaykin, M.E.; Bondartseva, M.A.; Wasser, S.P. Cancer without Pharmacological Illusions and a Niche for Mycotherapy (Review). Int. J. Med. Mushrooms 2019, 21, 105–119. [Google Scholar] [CrossRef] [PubMed]
- Rossi, P.; Difrancia, R.; Quagliariello, V.; Savino, E.; Tralongo, P.; Randazzo, C.L.; Berretta, M. B-Glucans from Grifola Frondosa and Ganoderma Lucidum in Breast Cancer: An Example of Complementary and Integrative Medicine. Oncotarget 2018, 9, 24837–24856. [Google Scholar] [CrossRef] [PubMed]
- Venturella, G.; Ferraro, V.; Cirlincione, F.; Gargano, M.L. Medicinal Mushrooms: Bioactive Compounds, Use, and Clinical Trials. Int. J. Mol. Sci. 2021, 22, 634. [Google Scholar] [CrossRef]
- Amen, Y.; Zhu, Q.; Tran, H.B.; Afifi, M.S.; Halim, A.F.; Ashour, A.; Shimizu, K. Partial Contribution of Rho-Kinase Inhibition to the Bioactivity of Ganoderma Lingzhi and Its Isolated Compounds: Insights on Discovery of Natural Rho-Kinase Inhibitors. J. Nat. Med. 2017, 71, 380–388. [Google Scholar] [CrossRef]
- Lin, F.L.; Cheng, Y.W.; Yu, M.; Ho, J.D.; Kuo, Y.C.; Chiou, G.C.Y.; Chang, H.M.; Lee, T.H.; Hsiao, G. The Fungus-Derived Retinoprotectant Theissenolactone C Improves Glaucoma-like Injury Mediated by MMP-9 Inhibition. Phytomedicine 2019, 56, 207–214. [Google Scholar] [CrossRef]
- Hellner, M.; Winter, D.; Von Georgi, R.; Münstedt, K. Apitherapy: Usage and Experience in German Beekeepers. Evid.-Based Complement. Altern. Med. 2008, 5, 475–479. [Google Scholar] [CrossRef]
- Münstedt, K.; Funk, D.; Riepen, T.; Berkes, E.; Hübner, J. Acceptance of Apitherapeutic Methods in Patients Consulting General Physicians or Gynaecologists. Complement. Ther. Clin. Pract. 2019, 35, 154–157. [Google Scholar] [CrossRef]
- Kavurmaci, M.; Tan, M. Determination of Knowledge and Attitudes of Nurses about Apitherapy. Complement. Ther. Clin. Pract. 2019, 36, 39–42. [Google Scholar] [CrossRef] [PubMed]
- Fratellone, P.M.; Tsimis, F.; Fratellone, G. Apitherapy Products for Medicinal Use. J. Altern. Complement. Med. 2016, 22, 1020–1022. [Google Scholar] [CrossRef] [PubMed]
- Inanc, B.B. The Quality Specialities in Turkiye’s Honies for Apitherapy. J. Pharmacopunct. 2021, 23, 194–200. [Google Scholar]
- Cornara, L.; Biagi, M.; Xiao, J.; Burlando, B. Therapeutic Properties of Bioactive Compounds from Different Honeybee Products. Front. Pharmacol. 2017, 8, 412. [Google Scholar] [CrossRef] [PubMed]
- Machado, A.M.; Miguel, M.G.; Vilas-Boas, M.; Figueiredo, A.C. Honey Volatiles as a Fingerprint for Botanical Origin—A Review on Their Occurrence on Monofloral Honeys. Molecules 2020, 25, 374. [Google Scholar] [CrossRef] [PubMed]
- Chien, H.Y.; Shih, A.T.; Yang, B.S.; Hsiao, V.K.S. Fast Honey Classification Using Infrared Spectrum and Machine Learning. Math. Biosci. Eng. 2019, 16, 6874–6891. [Google Scholar] [CrossRef]
- Nikolić-Pavljašević, S.; Redžepagić-Dervišević, E. Diseases of the eye and the therapeutic effect of honey. Hrana Zdr. Boles. Znan. časopis za Nutr. i dijetetiku 2016, 5, 27–31. [Google Scholar]
- Sforcin, J.M. Biological Properties and Therapeutic Applications of Propolis. Phyther. Res. 2016, 30, 894–905. [Google Scholar] [CrossRef]
- Denisow, B.; Denisow-Pietrzyk, M. Biological and Therapeutic Properties of Bee Pollen: A Review. J. Sci. Food Agric. 2016, 96, 4303–4309. [Google Scholar] [CrossRef] [PubMed]
- Pasupuleti, V.R.; Sammugam, L.; Ramesh, N.; Gan, S.H. Honey, Propolis, and Royal Jelly: A Comprehensive Review of Their Biological Actions and Health Benefits. Oxid. Med. Cell. Longev. 2017, 2017, 1259510. [Google Scholar] [CrossRef] [PubMed]
- Yucel, B.; Acikgoz, Z.; Bayraktar, H.; Seremet, C. The Effects of Apilarnil (Drone Bee Larvae) Administration on Growth Performance and Secondary Sex Characteristics of Male Broilers. J. Anim. Vet. Adv. 2011, 10, 2263–2266. [Google Scholar]
- Doğanyiğit, Z.; Okan, A.; Kaymak, E.; Pandır, D.; Silici, S. Investigation of Protective Effects of Apilarnil against Lipopolysaccharide Induced Liver Injury in Rats via TLR 4/HMGB-1/NF-ΚB Pathway. Biomed. Pharmacother. 2020, 125, 109967. [Google Scholar] [CrossRef] [PubMed]
- Nyman, G.S.A.; Tang, M.; Inerot, A.; Osmancevic, A.; Malmberg, P.; Hagvall, L. Contact Allergy to Beeswax and Propolis among Patients with Cheilitis or Facial Dermatitis. Contact Dermat. 2019, 81, 110–116. [Google Scholar] [CrossRef]
- Wehbe, R.; Frangieh, J.; Rima, M.; Obeid, D.; Sabatier, J.M.; Fajloun, Z. Bee Venom: Overview of Main Compounds and Bioactivities for Therapeutic Interests. Molecules 2019, 24, 2997. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Liu, Y.; Ye, Y.; Wang, X.R.; Lin, L.T.; Xiao, L.Y.; Zhou, P.; Shi, G.X.; Liu, C.Z. Bee Venom Therapy: Potential Mechanisms and Therapeutic Applications. Toxicon 2018, 148, 64–73. [Google Scholar] [CrossRef]
- Vazquez-Revuelta, P.; Madrigal-Burgaleta, R. Death Due to Live Bee Acupuncture Apitherapy. J. Investig. Allergol. Clin. Immunol. 2018, 28, 45–46. [Google Scholar] [CrossRef]
- Farkas, Á.; Molnár, R.; Morschhauser, T.; Hahn, I. Variation in Nectar Volume and Sugar Concentration of Allium ursinum L. ssp. Ucrainicum in Three Habitats. Sci. World J. 2012, 2012, 138579. [Google Scholar] [CrossRef]
- Rong, P.; Zhang, J.; Zhang, B. Applied TCM Ophthalmology [使用中医眼科学]; Zhong Guo Zhong Yi Yao Chu Ban She: Beijing, China, 2020; ISBN 9787513261678. [Google Scholar]
- Pourrahimi, M.; Abdi, M.; Ghods, R. Complications of Leech Therapy. Avicenna J. Phytomed. 2020, 10, 222–234. [Google Scholar]
- Kulbida, R.; Mathes, A.; Loeser, J. Beneficial Effects of Hirudotherapy in a Chronic Case of Complex Regional Pain Syndrome. J. Integr. Med. 2019, 17, 383–386. [Google Scholar] [CrossRef]
- Şenel, E.; Taylan Özkan, A.; Mumcuoglu, K.Y. Scientometric Analysis of Medicinal Leech Therapy. J. Ayurveda Integr. Med. 2019, 11, 534–538. [Google Scholar] [CrossRef]
- Jha, K.; Garg, A.; Narang, R.; Das, S. Hirudotherapy in Medicine and Dentistry. J. Clin. Diagn. Res. 2015, 9, ZE05. [Google Scholar] [CrossRef]
- Sobczak, N.; Kantyka, M. Hirudotherapy in Veterinary Medicine. Ann. Parasitol. 2014, 60, 89–92. [Google Scholar] [PubMed]
- Dong, H.; Ren, J.X.; Wang, J.J.; Ding, L.S.; Zhao, J.J.; Liu, S.Y.; Gao, H.M. Chinese Medicinal Leech: Ethnopharmacology, Phytochemistry, and Pharmacological Activities. Evid.-Based Complement. Altern. Med. 2016, 2016, 7895935. [Google Scholar] [CrossRef] [PubMed]
- Gileva, O.S.; Mumcuoglu, K.Y. Hirudotherapy. Biother.-Hist. Princ. Pract. 2013, 31–76. [Google Scholar] [CrossRef]
- Khan, J.A.; Parray, S.A. Irsal-e-Alaq (Leech Therapy) in Classical Literature of Unani System of Medicine: A Review. J. Blood Res. 2018, 1. [Google Scholar]
- Münstedt, K.; Riepen, T. Patients’ Decisions Regarding the Treatment of Primary Dysmenorrhoea. Complement. Ther. Med. 2019, 45, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Pratiwi, R.; Dipadharma, R.H.F.; Prayugo, I.J.; Layandro, O.A. Recent Analytical Method for Detection of Chemical Adulterants in Herbal Medicine. Molecules 2021, 26, 6606. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).