Hepatitis C Virus Infection Increases Fatigue in Health Care Workers
Abstract
1. Introduction
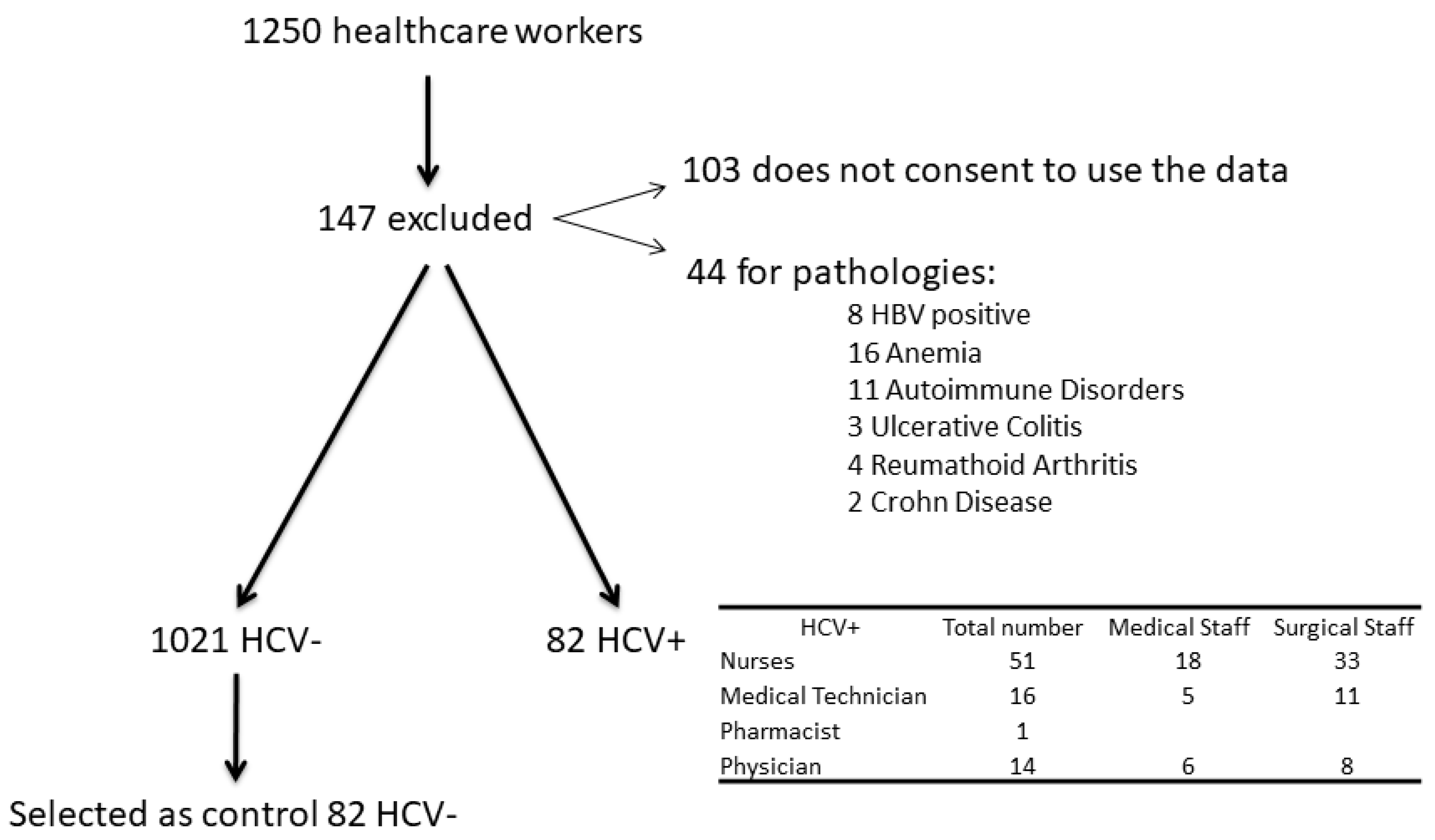
2. Patients and Methods
2.1. Serum Analysis
2.2. Questionnaire Evaluating Fatigue
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- WHO. Who Global Hepatitis Report; WHO: Geneva, Switzerland, 2017; ISBN 9789241565455. [Google Scholar]
- Petruzziello, A.; Marigliano, S.; Loquercio, G.; Cozzolino, A.; Cacciapuoti, C. Global epidemiology of hepatitis C virus infection: An up-date of the distribution and circulation of hepatitis C virus genotypes. World J. Gastroenterol. 2016, 22, 7824–7840. [Google Scholar] [CrossRef] [PubMed]
- Lavanchy, D. Evolving epidemiology of hepatitis C virus. Clin. Microbiol. Infect. 2011, 17, 107–115. [Google Scholar] [CrossRef]
- Hanafiah, K.M.; Groeger, J.; Flaxman, A.D.; Wiersma, S.T. Global epidemiology of hepatitis C virus infection: New estimates of age-specific antibody to HCV seroprevalence. Hepatology 2013, 57, 1333–1342. [Google Scholar] [CrossRef] [PubMed]
- Rogers, B.; Goodno, L. Evaluation of interventions to prevent needlestick injuries in health care occupations. Am. J. Prev. Med. 2000, 18, 90–98. [Google Scholar] [CrossRef]
- King, K.C.; Strony, R. Needlestick; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Sharpe, M. The report of the Chief Medical Officer’s CFS/ME working group: What does it say and will it help? Clin. Med. 2002, 2, 427–429. [Google Scholar] [CrossRef] [PubMed]
- Reichard, A.A.; Marsh, S.M.; Moore, P.H. Fatal and Nonfatal Injuries Among Emergency Medical Technicians and Paramedics. Prehosp. Emerg. Care 2011, 15, 511–517. [Google Scholar] [CrossRef] [PubMed]
- Roberts, M.H.; Sim, M.R.; Black, O.; Smith, P. Occupational injury risk among ambulance officers and paramedics compared with other healthcare workers in Victoria, Australia: Analysis of workers’ compensation claims from 2003 to 2012. Occup. Environ. Med. 2015, 72, 489–495. [Google Scholar] [CrossRef]
- Maguire, B.J.; O’Meara, P.; Brightwell, R.F.; O’Neill, B.J.; Fitzgerald, G. Occupational injury risk among Australian paramedics: An analysis of national data. Med. J. Aust. 2014, 200, 477–480. [Google Scholar] [CrossRef]
- Webster, D.P.; Klenerman, P.; Dusheiko, G.M. Hepatitis C. Lancet 2015, 385, 1124–1135. [Google Scholar] [CrossRef]
- Schuurmans, J.; Lutgens, S.; Groen, L.; Schneeberger, P. Do safety engineered devices reduce needlestick injuries? J. Hosp. Infect. 2018, 100, 99–104. [Google Scholar] [CrossRef]
- Markovic-Denic, L.; Maksimović, N.; Marusic, V.; Vucicevic, J.; Ostric, I.; Đurić, D. Occupational exposure to blood and body fluids among health-care workers in Serbia. Med. Princ. Pract. 2015, 24, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Cooke, C.E.; Stephens, J.M. Clinical, economic, and humanistic burden of needlestick injuries in healthcare workers. Med. Devices Evid. Res. 2017, 10, 225–235. [Google Scholar] [CrossRef] [PubMed]
- Pennisi, M.; Malaguarnera, G.; Di Bartolo, G.; Lanza, G.; Bella, R.; Chisari, E.M.; Cauli, O.; Vicari, E.; Malaguarnera, M. Decrease in Serum Vitamin D Level of Older Patients with Fatigue. Nutrients 2019, 11, 2531. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, W.; Watson, J.; Round, A. Rational testing: Investigating fatigue in primary care. BMJ 2010, 341, 502–504. [Google Scholar] [CrossRef]
- Larun, L.; Brurberg, K.G.; Odgaard-Jensen, J.; Price, J.R. Exercise therapy for chronic fatigue syndrome. Cochrane Database Syst. Rev. 2019, 4, CD003200. [Google Scholar] [CrossRef]
- Gates, M.; Wingert, A.; Featherstone, R.; Samuels, C.; Simon, C.; Dyson, M.P. Impact of fatigue and insufficient sleep on physician and patient outcomes: A systematic review. BMJ Open 2018, 8, e021967. [Google Scholar] [CrossRef]
- Reyes, M.; Nisenbaum, R.; Hoaglin, D.C.; Unger, E.R.; Emmons, C.; Randall, B.; Stewart, J.A.; Abbey, S.; Jones, J.F.; Gantz, N.; et al. Prevalence and Incidence of Chronic Fatigue Syndrome in Wichita, Kansas. Arch. Intern. Med. 2003, 163, 1530–1536. [Google Scholar] [CrossRef]
- Reeves, W.C.; Jones, J.F.; Maloney, E.; Heim, C.; Hoaglin, D.C.; Boneva, R.S.; Morrissey, M.; Devlin, R. Prevalence of chronic fatigue syndrome in metropolitan, urban, and rural Georgia. Popul. Health Metr. 2007, 5, 5. [Google Scholar] [CrossRef]
- Alavi, N.M.; Madani, M.; Sadat, Z.; Kashani, H.H.; Sharif, M.R. Fatigue and Vitamin D Status in Iranian Female Nurses. Glob. J. Health Sci. 2015, 8, 196–202. [Google Scholar] [CrossRef]
- Taylor, J.L.; Amann, M.; Duchateau, J.; Meeusen, R.; Rice, C.L. Neural contributions to muscle fatigue: From the brain to the muscle and back again. Med. Sci. Sports Exerc. 2016, 48, 2294–2306. [Google Scholar] [CrossRef]
- Gandevia, S.C.; Allen, G.M.; Neering, I.R.; Middleton, J.; Jones, R. Strength, voluntary drive, and endurance during isometric contractions in prior polio subjects. Ann. N. Y. Acad. Sci. 1995, 753, 408–409. [Google Scholar] [PubMed]
- Zalai, D.; Sherman, M.; McShane, K.; Shapiro, C.M.; Carney, C.E. The importance of fatigue cognitions in chronic hepatitis C infection. J. Psychosom. Res. 2015, 78, 193–198. [Google Scholar] [CrossRef]
- Malaguarnera, G.; Pennisi, M.; Gagliano, C.; Vacante, M.; Malaguarnera, M.; Salomone, S.; Drago, F.; Bertino, G.; Caraci, F.; Nunnari, G.; et al. Acetyl-L-Carnitine Supplementation during HCV Therapy with Pegylated Interferon-α2b Plus Ribavirin: Effect on Work Performance; A Randomized Clinical Trial. Hepat. Mon. 2014, 14, e11608. [Google Scholar] [CrossRef]
- Komaroff, A.L. Variability in medical practice: An investigative opportunity for general medicine. J. Gen. Intern. Med. 1986, 1, 31–34. [Google Scholar]
- Rassouli, M.; Zandiye, S.; Noorian, M.; Zayeri, F. Fatigue and Its Related Factors in Pediatric and Adult Oncology Nurses. Iran. J. Nurs. 2011, 24, 37–47. [Google Scholar]
- Nobile, C.G.A.; Montuori, P.; Diaco, E.; Villari, P. Healthcare personnel and hand decontamination in intensive care units: Knowledge, attitudes, and behaviour in Italy. J. Hosp. Infect. 2002, 51, 226–232. [Google Scholar] [CrossRef] [PubMed]
- Knodell, R.G.; Ishak, K.G.; Black, W.C.; Chen, T.S.; Craig, R.; Kaplowitz, N.; Kiernan, T.W.; Wollman, J. Formulation and application of a numerical scoring system for assessing histological activity in asymptomatic chronic active hepatitis. Hepatology 1981, 1, 431–435. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Steer, R.A.; Carbin, M.G. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin. Psychol. Rev. 1988, 8, 77–100. [Google Scholar] [CrossRef]
- Krupp, L.B.; Larocca, N.G.; Muir Nash, J.; Steinberg, A.D. The fatigue severity scale: Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch. Neurol. 1989, 46, 1121–1123. [Google Scholar] [CrossRef]
- Wessely, S.; Powell, R. Fatigue syndromes: A comparison of chronic “postviral” fatigue with neuromuscular and affective disorders. J. Neurol. Neurosurg. Psychiatry 1989, 52, 940–948. [Google Scholar] [CrossRef]
- Chalder, T.; Berelowitz, G.; Pawlikowska, T.; Watts, L.; Wessely, S.; Wright, D.; Wallace, E.P. Development of a fatigue scale. J. Psychosom. Res. 1993, 37, 147–153. [Google Scholar] [CrossRef]
- Pistone, G.; Marino, A.D.; Leotta, C.; Dell’Arte, S.; Finocchiaro, G.; Malaguarnera, M. Levocarnitine administration in elderly subjects with rapid muscle fatigue: Effect on body composition, lipid profile and fatigue. Drugs Aging 2003, 20, 761–767. [Google Scholar] [CrossRef] [PubMed]
- Yamini, D.; Basseri, B.; Chee, G.M.; Arakelyan, A.; Enayati, P.; Tran, T.T.; Poordad, F. Tobacco and other factors have a negative impact on quality of life in hepatitis C patients. J. Viral Hepat. 2011, 18, 714–720. [Google Scholar] [CrossRef] [PubMed]
- Bower, J.E. Cancer-related fatigue-mechanisms, risk factors, and treatments. Nat. Rev. Clin. Oncol. 2014, 11, 597–609. [Google Scholar] [CrossRef] [PubMed]
- Steege, L.M.; Pinekenstein, B.J.; Rainbow, J.G.; Arsenault Knudsen, É. Addressing Occupational Fatigue in Nurses: Current State of Fatigue Risk Management in Hospitals, Part 2. J. Nurs. Adm. 2017, 47, 484–490. [Google Scholar] [CrossRef]
- Arimura, M.; Imai, M.; Okawa, M.; Fujimura, T.; Yamada, N. Sleep, mental health status, and medical errors among hospital nurses in Japan. Ind. Health 2010, 48, 811–817. [Google Scholar] [CrossRef]
- Neri, S.; Pistone, G.; Saraceno, B.; Pennisi, G.; Luca, S.; Malaguarnera, M. L-carnitine decreases severity and type of fatigue induced by interferon-α in the treatment of patients with hepatitis C. Neuropsychobiology 2003, 47, 94–97. [Google Scholar] [CrossRef]
- Malaguarnera, G.; Bertino, G.; Chisari, G.; Motta, M.; Vecchio, M.; Vacante, M.; Caraci, F.; Greco, C.; Drago, F.; Nunnari, G.; et al. Silybin supplementation during HCV therapy with pegylated interferon-α plus ribavirin reduces depression and anxiety and increases work ability. BMC Psychiatry 2016, 16, 398. [Google Scholar] [CrossRef]
- Barreira, D.P.; Marinho, R.T.; Bicho, M.; Fialho, R.; Ouakinin, S.R.S. Psychosocial and Neurocognitive Factors Associated With Hepatitis C—Implications for Future Health and Wellbeing. Front. Psychol. 2019, 9, 9. [Google Scholar] [CrossRef]
- Modabbernia, A.; Poustchi, H.; Emalekzadeh, R. Neuropsychiatric and Psychosocial Issues of Patients with Hepatitis C Infection: A Selective Literature Review. Hepat. Mon. 2013, 13, 13. [Google Scholar] [CrossRef]
- Dantzer, R.; Connor, J.C.; Freund, G.G.; Johnson, R.W.; Kelley, K.W. From inflammation to sickness and depression: When the immune system subjugates the brain. Nat. Rev. Neurosci. 2008, 9, 46–56. [Google Scholar] [CrossRef]
- Haroon, E.; Raison, C.L.; Miller, A.H. Psychoneuroimmunology Meets Neuropsychopharmacology: Translational Implications of the Impact of Inflammation on Behavior. Neuropsychopharmacology 2012, 37, 137–162. [Google Scholar] [CrossRef]
- Bürgel, B.; Friesland, M.; Koch, A.; Manns, M.P.; Wedemeyer, H.; Weissenborn, K.; Schulz-Schaeffer, W.J.; Pietschmann, T.; Steinmann, J.; Ciesek, S. Hepatitis C virus enters human peripheral neuroblastoma cells—evidence for extra-hepatic cells sustaining hepatitis C virus penetration. J. Viral Hepat. 2010, 18, 562–570. [Google Scholar] [CrossRef]
- Malaguarnera, G.; Vacante, M.; Drago, F.; Bertino, G.; Motta, M.; Giordano, M.; Malaguarnera, M. Endozepine-4 levels are increased in hepatic coma. World J. Gastroenterol. 2015, 21, 9103–9110. [Google Scholar] [CrossRef] [PubMed]
- Perry, W.; Hilsabeck, R.C.; Hassanein, T.I. Cognitive Dysfunction in Chronic Hepatitis C: A Review. Dig. Dis. Sci. 2008, 53, 307–321. [Google Scholar] [CrossRef] [PubMed]
- van Wijk, P.T.L.; Pelk-Jongen, M.; Wijkmans, C.; Voss, A.; Timen, A.; Schneeberger, P.M. Variation in interpretation and counselling of blood exposure incidents by different medical practitioners. Am. J. Infect. Control 2008, 36, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Bertino, G.; Ardiri, A.; Proiti, M.; Rigano, G.; Frazzetto, E.; Demma, S.; Ruggeri, M.I.; Scuderi, L.; Malaguarnera, G.; Bertino, N.; et al. Chronic hepatitis C: This and the new era of treatment. World J. Hepatol. 2016, 8, 92–106. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
| HCV N = 82 | NHCV N = 82 | HCV vs. Not HCV | |||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | 95% CI Odds Ratio | Signif. | p | |
| Gender F/M | 46/36 | 56.10 | 45/37 | 54.88 | 0.5805 to 1.905 | NS | >0.9999 |
| Smokers Y/N | 50/32 | 60.98 | 44/38 | 53.66 | 0.7421 to 2.484 | NS | 0.4300 |
| Alcohol Y/N | 5/77 | 6.10 | 7/75 | 8.54 | 0.2401 to 2.118 | NS | 0.7657 |
| MS Single Y/N | 12/70 | 14.63 | 10/72 | 12.20 | 0.5250 to 3.103 | NS | 0.8193 |
| MS Married Y/N | 60/22 | 73.17 | 56/26 | 68.29 | 0.6617 to 2.470 | NS | 0.6069 |
| MS Divorce Y/N | 6/76 | 7.32 | 10/72 | 12.20 | 0.1954 to 1.522 | NS | 0.4308 |
| MS Widow Y/N | 4/78 | 4.88 | 6/76 | 7.32 | 0.2009 to 2.567 | NS | 0.7461 |
| HCV N = 82 | Not HCV N = 82 | HCV vs. not HCV | |||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | 95% CI | Significance | p | |
| Age (years) | 46.8 | 4.1 | 44.7 | 5.8 | −3.649 to −0.5511 | ** | 0.0021 |
| Sistolic Art Press (mmHg) | 137.1 | 9.4 | 138.2 | 8.7 | −1.693 to 3.893 | NS | 0.4877 |
| Diastolic Art press (mmHg) | 81.4 | 9.1 | 80.6 | 9.2 | −3.622 to 2.022 | NS | 0.9219 |
| HR (bpm) | 70.2 | 9.6 | 72.8 | 8.7 | −0.2253 to 5.425 | NS | 0.3775 |
| BMI (Kg/m2) | 24.2 | 2.9 | 24 | 3.1 | −1.126 to 0.7257 | NS | 0.5497 |
| HCV RNA | 3.5 | 0.9 | 0 | 0 | −3.696 to −3.304 | **** | <0.0001 |
| HCV exposure (years) | 11.2 | 3.2 | / | / | |||
| Anti HCV Ab | positive | negative | |||||
| HCV genotypes | |||||||
| 1a | 10 | / | / | / | |||
| 1b | 69 | / | / | / | |||
| 2a | 1 | / | / | / | |||
| 2b | 2 | / | / | / | |||
| HCV N = 82 | Not HCV N = 82 | HCV vs. Not HCV | |||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | 95% CI | Signif. | p | |
| Urea mg/dL | 44.1 | 3.7 | 38.1 | 4.1 | 0.5829 to 5.217 | **** | <0.0001 |
| Glucose mg/dL | 74.2 | 8.7 | 77.1 | 6.1 | 0.5829 to 5.217 | * | 0.0145 |
| Total Cholesterol mg/dL | 225 | 12.8 | 220 | 13.9 | −9.121 to −0.8794 | * | 0.0177 |
| HDL Cholesterol mg/dL | 44.1 | 6.2 | 41.8 | 6.3 | −4.228 to −0.3724 | * | 0.0197 |
| Triglycerides mg/dL | 190.1 | 12.8 | 185 | 13.9 | −9.221 to −0.9794 | * | 0.0156 |
| AST IU/L | 164.2 | 22.9 | 38.2 | 3.9 | −131.1 to −120.9 | **** | <0.0001 |
| ALT IU/L | 169.8 | 32.1 | 36.1 | 3.4 | −140.7 to −126.7 | **** | <0.0001 |
| CRP mg/L | 6.25 | 1.44 | 1.67 | 0.36 | −4.904 to −4.256 | **** | <0.0001 |
| HCV N = 82 | Not HCV N = 82 | HCV vs. Not HCV | |||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | 95% CI | Signif. | p | |
| Physical fatigue | 11.4 | 2.9 | 8.2 | 3.6 | −4.208 to −2.192 | **** | <0.0001 |
| Mental Fatigue | 9.7 | 3.4 | 7.9 | 2.8 | −2.761 to −0.8395 | *** | 0.0003 |
| Fatigue Severity | 49.1 | 6.7 | 35.2 | 9.2 | −16.38 to −11.42 | **** | <0.0001 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Catania, V.E.; Malaguarnera, G.; Fiorenza, G.; Chisari, E.M.; Lipari, A.R.; Gallina, V.; Pennisi, M.; Lanza, G.; Malaguarnera, M. Hepatitis C Virus Infection Increases Fatigue in Health Care Workers. Diseases 2020, 8, 37. https://doi.org/10.3390/diseases8040037
Catania VE, Malaguarnera G, Fiorenza G, Chisari EM, Lipari AR, Gallina V, Pennisi M, Lanza G, Malaguarnera M. Hepatitis C Virus Infection Increases Fatigue in Health Care Workers. Diseases. 2020; 8(4):37. https://doi.org/10.3390/diseases8040037
Chicago/Turabian StyleCatania, Vito Emanuele, Giulia Malaguarnera, Giorgia Fiorenza, Eleonora Margherita Chisari, Anna Rita Lipari, Valentino Gallina, Manuela Pennisi, Giuseppe Lanza, and Michele Malaguarnera. 2020. "Hepatitis C Virus Infection Increases Fatigue in Health Care Workers" Diseases 8, no. 4: 37. https://doi.org/10.3390/diseases8040037
APA StyleCatania, V. E., Malaguarnera, G., Fiorenza, G., Chisari, E. M., Lipari, A. R., Gallina, V., Pennisi, M., Lanza, G., & Malaguarnera, M. (2020). Hepatitis C Virus Infection Increases Fatigue in Health Care Workers. Diseases, 8(4), 37. https://doi.org/10.3390/diseases8040037







