Optimal Cut-Off Values for Body Mass Index and Fat Mass Index Based on Age in Physically Active Males Using Receiver Operating Characteristic Curve
Abstract
:1. Introduction
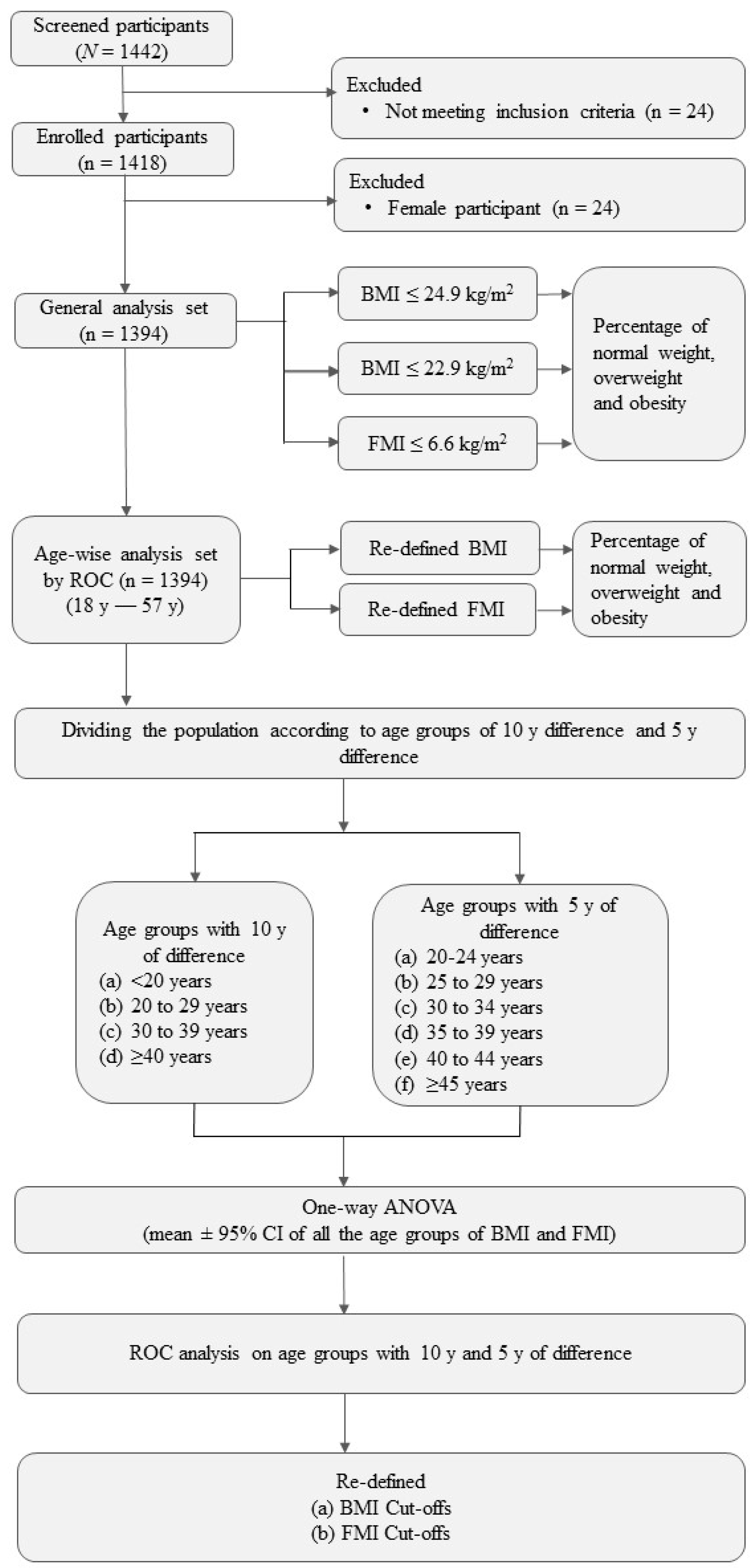
2. Materials and Methods
2.1. Participants
2.2. Categorization of the Participants
2.3. Assessment of Body Composition
2.3.1. Anthropometric and Body Composition Measurements
2.3.2. Bioelectric Impedance Analyzer (BIA)
2.3.3. Physical Activity Level (PAL) Value Assessment
2.4. Statistical Analysis
3. Results
3.1. Prevalence of Overweight and Obesity in the Study Population
3.1.1. Body Mass Index (BMI)
3.1.2. Fat Mass Index (FMI)
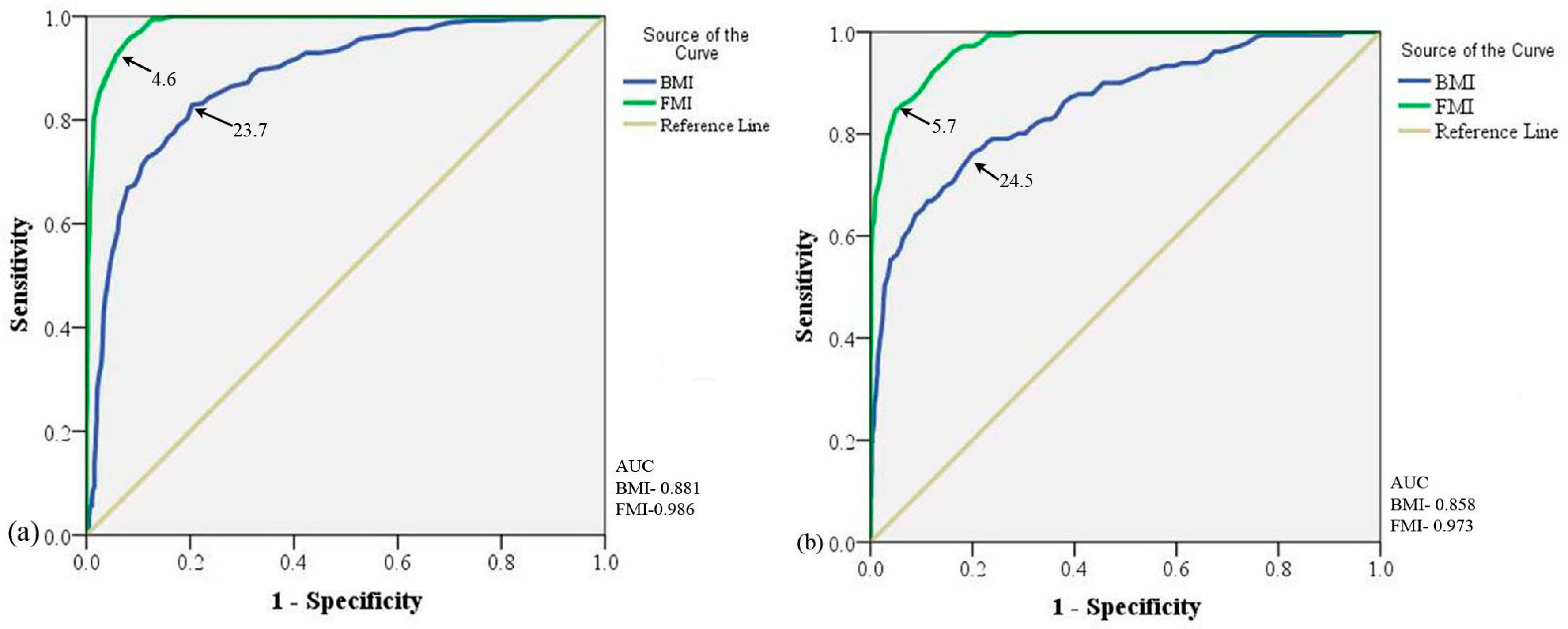
3.2. Evaluating the Study Population Based on BMI and FMI Cut-Off by ROC Curve
3.3. Defining Cut-Offs Based on Different Age Groups
3.3.1. Age Group with 10 Years of Difference
3.3.2. Age Group with 5 Years of Difference
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Grier, T.; Canham-Chervak, M.; Sharp, M.; Jones, B.H. Does body mass index misclassify physically active young men. Prev. Med. Rep. 2015, 2, 483–487. [Google Scholar] [CrossRef] [PubMed]
- WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004, 363, 157–163.
- Gurunathan, U.; Myles, P.S. Limitations of body mass index as an obesity measure of perioperative risk. Br. J. Anaesth. 2016, 116, 319–321. [Google Scholar] [CrossRef] [PubMed]
- Jackson, A.S.; Stanforth, P.R.; Gagnon, J.; Rankinen, T.; Leon, A.S.; Rao, D.C.; Skinner, J.S.; Bouchard, C.; Wilmore, J.H. The effect of sex, age and race on estimating percentage body fat from body mass index: The Heritage Family Study. Int. J. Obes. Relat. Metab. Disord. 2002, 26, 789–796. [Google Scholar] [CrossRef] [PubMed]
- Rao, K.M.; Arlappa, N.; Radhika, M.S.; Balakrishna, N.; Laxmaiah, A.; Brahmam, G.N. Correlation of Fat Mass Index and Fat-Free Mass Index with percentage body fat and their association with hypertension among urban South Indian adult men and women. Ann. Hum. Biol. 2012, 39, 54–58. [Google Scholar] [CrossRef] [PubMed]
- Ramirez-Velez, R.; Correa-Bautista, J.E.; Sanders-Tordecilla, A.; Ojeda-Pardo, M.L.; Cobo-Mejia, E.A.; Castellanos-Vega, R.D.P.; Garcia-Hermoso, A.; Gonzalez-Jimenez, E.; Schmidt-RioValle, J.; Gonzalez-Ruiz, K. Percentage of Body Fat and Fat Mass Index as a Screening Tool for Metabolic Syndrome Prediction in Colombian University Students. Nutrients 2017, 9, 1009. [Google Scholar] [CrossRef] [PubMed]
- Provencher, M.T.; Chahla, J.; Sanchez, G.; Cinque, M.E.; Kennedy, N.I.; Whalen, J.; Price, M.D.; Moatshe, G.; LaPrade, R.F. Body Mass Index Versus Body Fat Percentage in Prospective National Football League Athletes: Overestimation of Obesity Rate in Athletes at the National Football League Scouting Combine. J. Strength Cond. Res. 2018, 32, 1013–1019. [Google Scholar] [CrossRef] [PubMed]
- Weir, C.B.; Jan, A. BMI Classification Percentile and Cut Off Points. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Porto, L.G.; Nogueira, R.M.; Nogueira, E.C.; Molina, G.E.; Farioli, A.; Junqueira, L.F., Jr.; Kales, S.N. Agreement between BMI and body fat obesity definitions in a physically active population. Arch. Endocrinol. Metab. 2016, 60, 515–525. [Google Scholar] [CrossRef]
- Kruschitz, R.; Wallner-Liebmann, S.J.; Hamlin, M.J.; Moser, M.; Ludvik, B.; Schnedl, W.J.; Tafeit, E. Detecting body fat-A weighty problem BMI versus subcutaneous fat patterns in athletes and non-athletes. PLoS ONE 2013, 8, e72002. [Google Scholar] [CrossRef]
- Domaradzki, J.; Kozlenia, D. The performance of body mass component indices in detecting risk of musculoskeletal injuries in physically active young men and women. PeerJ 2022, 10, e12745. [Google Scholar] [CrossRef]
- Scheit, L.; End, B.; Schroder, J.; Hoffmann, M.A.; Reer, R. BMI Alterations and Prevalence of Overweight and Obesity Related to Service Duration at the German Armed Forces. Healthcare 2023, 11, 225. [Google Scholar] [CrossRef]
- Ghosh, J.R.; Bandyopadhyay, A.R. Receiver operating characteristic curve analysis of BMI in assessing obesity among adult Bengalee males in India. Coll. Antropol. 2007, 31, 705–708. [Google Scholar] [PubMed]
- Kesavachandran, C.N.; Bihari, V.; Mathur, N. The normal range of body mass index with high body fat percentage among male residents of Lucknow city in north India. Indian J. Med. Res. 2012, 135, 72–77. [Google Scholar] [PubMed]
- Misra, A.; Pandey, R.M.; Sinha, S.; Guleria, R.; Sridhar, V.; Dudeja, V. Receiver operating characteristics curve analysis of body fat & body mass index in dyslipidaemic Asian Indians. Indian J. Med. Res. 2003, 117, 170–179. [Google Scholar] [PubMed]
- Silveira, E.A.; Pagotto, V.; Barbosa, L.S.; Oliveira, C.; Pena, G.D.G.; Velasquez-Melendez, G. Accuracy of BMI and waist circumference cut-off points to predict obesity in older adults. Cienc. Saude Colet. 2020, 25, 1073–1082. [Google Scholar] [CrossRef] [PubMed]
- Mungreiphy, N.K.; Kapoor, S.; Sinha, R. Association between BMI, Blood Pressure, and Age: Study among Tangkhul Naga Tribal Males of Northeast India. J. Anthropol. 2011, 2011, 748147. [Google Scholar] [CrossRef]
- Indian Council of Medical Research. Dietary Guidelines for Indians—A Manual, 2nd ed.; National Institute of Nutrition: Hyderabad, India, 2011. [Google Scholar]
- Moshfegh, A.J.; Rhodes, D.G.; Baer, D.J.; Murayi, T.; Clemens, J.C.; Rumpler, W.V.; Paul, D.R.; Sebastian, R.S.; Kuczynski, K.J.; Ingwersen, L.A.; et al. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am. J. Clin. Nutr. 2008, 88, 324–332. [Google Scholar] [CrossRef] [PubMed]
- Conway, J.M.; Ingwersen, L.A.; Vinyard, B.T.; Moshfegh, A.J. Effectiveness of the U.S. Department of Agriculture 5-step multiple-pass method in assessing food intake in obese and nonobese women. Am. J. Clin. Nutr. 2003, 77, 1171–1178. [Google Scholar] [CrossRef]
- Rakhra, G.; Masih, D.; Vats, A.; Verma, S.K.; Singh, V.K.; Rana, R.T.; Kirar, V.; Singh, S.N. Effect of physical activity and age on plasma copper, zinc, iron, and magnesium concentration in physically active healthy males. Nutrition 2017, 43–44, 75–82. [Google Scholar] [CrossRef]
- Kadam, P.; Bhalerao, S. Sample size calculation. Int. J. Ayurveda Res. 2010, 1, 55–57. [Google Scholar]
- Masih, D.; Rakhra, G.; Vats, A.; Verma, S.K.; Sharma, Y.K.; Singh, S.N. Assessing body composition by bioelectric impedance analysis and dual- energy X- ray absorptiometry in physically active normal and overweight Indian males. Natl. J. Physiol. Pharm. Pharmacol. 2018, 8, 755–761. [Google Scholar] [CrossRef]
- WHO. Energy and Protein Requirements: Report of a Joint FAO/WHO/UNU Expert Consultation; WHO: Geneva, Switzerland, 1985; Volume 724, 206p. [Google Scholar]
- Singh, S.N.; Vats, P.; Shukla, V. A comparison of free living energy expenditure determinations of physically active Indians using different methods and the validation against doubly labeled water. In Non-Nuclear Applications of Heavy Water and Deuterium; Bhaskaran, M., Ed.; Macmillan Publisher Indian Ltd.: Delhi, India, 2010; pp. 194–204. [Google Scholar]
- Hajian-Tilaki, K. Receiver Operating Characteristic (ROC) Curve Analysis for Medical Diagnostic Test Evaluation. Casp. J. Intern. Med. 2013, 4, 627–635. [Google Scholar]
- Masih, D.; Tripathi, J.K.; Rakhra, G.; Vats, A.; Verma, S.K.; Jha, P.K.; Sharma, M.; Ashraf, M.Z.; Singh, S.N. Deciphering Biochemical and Molecular Signatures Associated with Obesity in Context of Metabolic Health. Genes 2021, 12, 290. [Google Scholar] [CrossRef]
- Release of NFHS-5 (2019-21)—Compendium of Factsheets. India and Phase-II States & UTs. Available online: https://main.mohfw.gov.in/basicpage-14 (accessed on 15 July 2022).
- Little, M.; Humphries, S.; Patel, K.; Dewey, C. Factors associated with BMI, underweight, overweight, and obesity among adults in a population of rural south India: A cross-sectional study. BMC Obes. 2016, 3, 12. [Google Scholar] [CrossRef]
- Luhar, S.; Mallinson, P.A.C.; Clarke, L.; Kinra, S. Trends in the socioeconomic patterning of overweight/obesity in India: A repeated cross-sectional study using nationally representative data. BMJ Open 2018, 8, e023935. [Google Scholar] [CrossRef]
- Luhar, S.; Timæus, I.M.; Jones, R.; Cunningham, S.; Patel, S.A.; Kinra, S.; Clarke, L.; Houben, R. Forecasting the prevalence of overweight and obesity in India to 2040. PLoS ONE 2020, 15, e0229438. [Google Scholar] [CrossRef]
- Misra, A.; Khurana, L. Obesity and the metabolic syndrome in developing countries. J. Clin. Endocrinol. Metab. 2008, 93 (Suppl. 1), S9–S30. [Google Scholar] [CrossRef]
- Mohan, I.; Gupta, R.; Misra, A.; Sharma, K.K.; Agrawal, A.; Vikram, N.K.; Sharma, V.; Shrivastava, U.; Pandey, R.M. Disparities in Prevalence of Cardiometablic Risk Factors in Rural, Urban-Poor, and Urban-Middle Class Women in India. PLoS ONE 2016, 11, e0149437. [Google Scholar] [CrossRef]
- Misra, A.; Vikram, N.K. Clinical and pathophysiological consequences of abdominal adiposity and abdominal adipose tissue depots. Nutrition 2003, 19, 457–466. [Google Scholar] [CrossRef]
- Deurenberg-Yap, M.; Schmidt, G.; van Staveren, W.A.; Deurenberg, P. The paradox of low body mass index and high body fat percentage among Chinese, Malays and Indians in Singapore. Int. J. Obes. Relat. Metab. Disord. 2000, 24, 1011–1017. [Google Scholar] [CrossRef]
- Gallagher, D.; Heymsfield, S.B.; Heo, M.; Jebb, S.A.; Murgatroyd, P.R.; Sakamoto, Y. Healthy percentage body fat ranges: An approach for developing guidelines based on body mass index. Am. J. Clin. Nutr. 2000, 72, 694–701. [Google Scholar] [CrossRef] [PubMed]
- Kagawa, M.; Uenishi, K.; Kuroiwa, C.; Mori, M.; Binns, C.W. Is the BMI cut-off level for Japanese females for obesity set too high? A consideration from a body composition perspective. Asia Pac. J. Clin. Nutr. 2006, 15, 502–507. [Google Scholar] [PubMed]
- Piers, L.S.; Rowley, K.G.; Soares, M.J.; O’Dea, K. Relation of adiposity and body fat distribution to body mass index in Australians of Aboriginal and European ancestry. Eur. J. Clin. Nutr. 2003, 57, 956–963. [Google Scholar] [CrossRef] [PubMed]
- Luke, A.; Durazo-Arvizu, R.; Rotimi, C.; Prewitt, T.E.; Forrester, T.; Wilks, R.; Ogunbiyi, O.J.; Schoeller, D.A.; McGee, D.; Cooper, R.S. Relation between body mass index and body fat in black population samples from Nigeria, Jamaica, and the United States. Am. J. Epidemiol. 1997, 145, 620–628. [Google Scholar] [CrossRef] [PubMed]
- WHO. Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation on Obesity; WHO: Geneva, Switzerland, 1998. [Google Scholar]
- Kagawa, M.; Kerr, D.; Uchida, H.; Binns, C.W. Differences in the relationship between BMI and percentage body fat between Japanese and Australian-Caucasian young men. Br. J. Nutr. 2006, 95, 1002–1007. [Google Scholar] [CrossRef] [PubMed]
- Deurenberg, P.; Deurenberg-Yap, M.; Guricci, S. Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship. Obes. Rev. 2002, 3, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Luke, A. Ethnicity and the BMI-body fat relationship. Br. J. Nutr. 2009, 102, 485–487. [Google Scholar] [CrossRef] [PubMed]
- Dulloo, A.G.; Jacquet, J.; Solinas, G.; Montani, J.P.; Schutz, Y. Body composition phenotypes in pathways to obesity and the metabolic syndrome. Int. J. Obes. 2010, 34 (Suppl. 2), S4–S17. [Google Scholar] [CrossRef]
- Blundell, J.E.; Dulloo, A.G.; Salvador, J.; Fruhbeck, G. Beyond BMI—Phenotyping the obesities. Obes. Facts 2014, 7, 322–328. [Google Scholar] [CrossRef]
- Singh, S.P.; Sikri, G.; Garg, M.K. Body Mass Index and Obesity: Tailoring “cut-off” for an Asian Indian Male Population. Med. J. Armed Forces India 2008, 64, 350–353. [Google Scholar] [CrossRef]
- Peltz, G.; Aguirre, M.T.; Sanderson, M.; Fadden, M.K. The role of fat mass index in determining obesity. Am. J. Hum. Biol. 2010, 22, 639–647. [Google Scholar] [CrossRef]
- Samadi, M.; Sadrzade-Yeganeh, H.; Azadbakht, L.; Jafarian, K.; Rahimi, A.; Sotoudeh, G. Sensitivity and specificity of body mass index in determining obesity in children. J. Res. Med. Sci. 2013, 18, 537–542. [Google Scholar]



| S. No. | Characteristics | Mean | SD | Min–Max | IQR (Q1–Q3) |
|---|---|---|---|---|---|
| 1. | N | 1394 | - | - | - |
| 2. | Sex | Male | - | - | - |
| 3. | Age (y) | 29 | 8.7 | 18–57 | 14 (21–35) |
| 4. | Height (cm) | 171.4 | 5.0 | 154–187.1 | 6.9 (168–174) |
| 5. | Weight (kg) | 66.8 | 8.9 | 44.5–100.8 | 13 (60–73) |
| 6. | BMI (kg/m2) | 22.7 | 2.8 | 15.9–35.7 | 4.0 (20.7–24.7) |
| 7. | FMI (kg/m2) | 4.3 | 1.7 | 1.0–12.3 | 2.6 (2.9–5.5) |
| 8. | FM (kg) | 12.7 | 4.9 | 3.1–34.7 | 7.6 (8.5–16.1) |
| 9. | FM % | 18.5 | 5.3 | 5.3–35.1 | 8.7(13.9–22.6) |
| 10. | FFM (kg) | 54.5 | 14.8 | 30.1–568.5 | 7.2 (50.5–57.7) |
| 11. | Muscle mass (kg) | 53.6 | 4.7 | 39.1–73.4 | 5.5 (50.5–56.0) |
| 12. | Total body water (kg) | 38.6 | 4.2 | 27.6–56.3 | 5.4 (35.6–41.0) |
| 13. | Degree of obesity | 9.7 | 11.7 | −20.0–62.3 | 15.1 (2.0–17.1) |
| 14. | BMR (kcal/day) | 1600 | 143 | 1249–2263 | 163.3 (1513–1677) |
| Health Status | Previous Cut-Off BMI ≥ 24.9 kg/m2 | New Cut-Off BMI ≥ 22.9 kg/m2 | ROC Curve Produced Cut-Off BMI ≥ 23.7 kg/m2 | FMI ≥ 6.6 kg/m2 | ROC Curve Produced Cut-Off FMI ≥ 4.6 kg/m2 |
|---|---|---|---|---|---|
| Underweight (cut-off) | 4.0% (n = 56) (<18.5 kg/m2) | 4.0% (n = 56) (<18.5 kg/m2) | 4.0% (n = 56) (<18.5 kg/m2) | - | - |
| Normal weight (cut-off) | 74.3% (n = 1037) (18.5–24.9 kg/m2) | 51.8% (n = 722) (18.5–22.9 kg/m2) | 61.3% (n = 854) (18.5–23.7 kg/m2) | 91.6% (n = 1277) (≤6.6 kg/m2) | 40.8% (n = 570) (≤4.6 kg/m2) |
| Overweight (cut-off) | 20.7% (n = 289) (25.0–29.9 kg/m2) | 22.6% (n = 315) (23.0–24.9 kg/m2) | 8.2% (n = 115) (23.8–24.5 kg/m2) | - | 20.9% (n = 292) (4.6–5.7 kg/m2) |
| Pre-obese (cut-off) | - | 20.7% (n = 289) (25.0–29.9 kg/m2) | 25.6% (n = 357) (24.6–29.9 kg/m2) | - | - |
| Obese (cut-off) | 0.9% (n = 12) | 0.9% (n = 12) (≥30.0 kg/m2) | 0.9% (n = 12) (≥30.0 kg/m2) | 8.4% (n = 117) (>6.6 kg/m2) | 19.8% (n = 277) (>5.7 kg/m2) |
| DIFFERENCE OF 10 Y AGE GROUP | |||||||
|---|---|---|---|---|---|---|---|
| BMI | |||||||
| 18–19 y | 20–29 y | 30–39 y | ≥40 y | ||||
| 18–19 y | - | *** | *** | *** | |||
| 20–29 y | *** | - | *** | *** | |||
| 30–39 y | *** | *** | - | ns | |||
| ≥40 y | *** | *** | ns | - | |||
| FMI | |||||||
| 18–19 y | 20–29 y | 30–39 y | ≥40 y | ||||
| 18–19 y | - | *** | *** | *** | |||
| 20–29 y | *** | - | *** | *** | |||
| 30–39 y | *** | *** | - | ns | |||
| ≥40 y | *** | *** | ns | - | |||
| DIFFERENCE OF 5 Y AGE GROUP | |||||||
| BMI | |||||||
| 18–19 y | 20–24 y | 25–29 y | 30–34 y | 35–39 y | 40–44 y | ≥45 y | |
| 18–19 y | -- | ** | *** | *** | *** | *** | *** |
| 20–24 y | ** | - | *** | *** | *** | *** | *** |
| 25–29 y | *** | *** | - | *** | ns | ns | *** |
| 30–34 y | *** | *** | *** | - | ns | ns | ns |
| 35–39 y | *** | *** | ns | ns | - | ns | *** |
| 40–44 y | *** | *** | ns | ns | ns | - | *** |
| ≥45 y | *** | *** | *** | ns | *** | *** | - |
| FMI | |||||||
| 18–19 y | 20–24 y | 25–29 y | 30–34 y | 35–39 y | 40–44 y | ≥45 y | |
| 18–19 y | - | *** | *** | *** | *** | *** | *** |
| 20–24 y | *** | - | *** | *** | *** | *** | *** |
| 25–29 y | *** | *** | - | *** | *** | * | *** |
| 30–34 y | *** | *** | *** | - | ns | ns | * |
| 35–39 y | *** | *** | *** | ns | - | ns | *** |
| 40–44 y | *** | *** | * | ns | ns | - | *** |
| ≥45 y | *** | *** | *** | * | *** | *** | - |
| AGE GROUPS | BMI | FMI |
|---|---|---|
| AUC (95% CI) | AUC (95% CI) | |
| 18–60 y (overweight) | 0.881 (86.1–90.2%) | 0.986 (98.1–99.1%) |
| 18–60 y(Obesity) | 0.858 (82.6–88.9%) | 0.973 (96.5–98.2%) |
| DIFFERENCE OF 10 Y AGE GROUP | ||
| 18–19 | 0.88 (83.2–92.3%) | 0.99 (98.6–100%) |
| 20–29 | 0.90 (84.7–95.1%) | 0.96 (97.4–99.6%) |
| 30–39 | 0.80 (74.3–86.4%) | 0.95 (93.1–97.7%) |
| ≥40 | 0.75 (66.3–83.4%) | 0.95 (92.2–97.7%) |
| DIFFERENCE OF 5 Y AGE GROUP | ||
| 20–24 | 0.93 (85.5–100%) | 0.99 (98.1–100%) |
| 25–29 | 0.84 (74.5–92.7%) | 0.97 (94.9–99.8%) |
| 30–34 | 0.84 (76.7–92.0%) | 0.97 (94.9–99.7%) |
| 35–39 | 0.81 (72.8–89.4%) | 0.96 (92.9–98.7%) |
| 40–44 | 0.73 (62.6–84.0%) | 0.95 (91.3–98.1%) |
| ≥45 | 0.77 (63.2–91.4%) | 0.96 (91.9–100%) |
| S. No. | Age Groups (y) | Number of Subjects | BMI Cut-Off | Obesity Prevalence (%) | FMI Cut-Off | Obesity Prevalence (%) |
|---|---|---|---|---|---|---|
| 1 | 18–19 | 205 | 22.5 (Sensitivity—100%, Specificity—87.3%) | 11.7 | 5.6 (Sensitivity—100%, Specificity—99.5%) | 1.0 |
| 2 | 20–24 | 355 | 23.3 (Sensitivity—92.3%, Specificity—86.0%) | 16.3 | 5.2 (Sensitivity—100%, Specificity—93.3%) | 9.0 |
| 3 | 25–29 | 215 | 24.3 (Sensitivity—80.8%, Specificity—75.7%) | 30.7 | 6.1 (Sensitivity—88.5%, Specificity—93.1%) | 12.6 |
| 4 | 30–34 | 238 | 26.0 (Sensitivity—75.8%, Specificity—82.4%) | 24.8 | 6.1 (Sensitivity—97.0%, Specificity—86.8%) | 20.2 |
| 5 | 35–39 | 171 | 24.7 (Sensitivity—75.5%, Specificity—80.3%) | 33.9 | 6.1 (Sensitivity—85.7%, Specificity—95.1%) | 26.3 |
| 6 | 40–44 | 147 | 26.2 (Sensitivity—52.6%, Specificity—95.4%) | 17.0 | 5.6 (Sensitivity—89.5%, Specificity—79.8%) | 38.1 |
| 7 | ≥45 | 63 | 26.6 (Sensitivity—47.4%, Specificity—97.2%) | 23.8 | 6.2 (Sensitivity—68.4%, Specificity—96.3%) | 31.7 |
| 8 | 18–57 (Entire study sample) | 1394 | 24.5 (Sensitivity—76.2%, Specificity—80.0%) | 26.5 | 5.7 (Sensitivity—92.3%, Specificity—87.7%) | 19.9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Masih, D.; Rakhra, G.; Vats, A.; Verma, S.K.; Singh, V.K.; Kirar, V.; Tripathi, J.K.; Singh, S.N. Optimal Cut-Off Values for Body Mass Index and Fat Mass Index Based on Age in Physically Active Males Using Receiver Operating Characteristic Curve. Diseases 2023, 11, 137. https://doi.org/10.3390/diseases11040137
Masih D, Rakhra G, Vats A, Verma SK, Singh VK, Kirar V, Tripathi JK, Singh SN. Optimal Cut-Off Values for Body Mass Index and Fat Mass Index Based on Age in Physically Active Males Using Receiver Operating Characteristic Curve. Diseases. 2023; 11(4):137. https://doi.org/10.3390/diseases11040137
Chicago/Turabian StyleMasih, Daisy, Gurseen Rakhra, Annu Vats, Saroj Kumar Verma, Vijay Kumar Singh, Vandana Kirar, Jitendra Kumar Tripathi, and Som Nath Singh. 2023. "Optimal Cut-Off Values for Body Mass Index and Fat Mass Index Based on Age in Physically Active Males Using Receiver Operating Characteristic Curve" Diseases 11, no. 4: 137. https://doi.org/10.3390/diseases11040137
APA StyleMasih, D., Rakhra, G., Vats, A., Verma, S. K., Singh, V. K., Kirar, V., Tripathi, J. K., & Singh, S. N. (2023). Optimal Cut-Off Values for Body Mass Index and Fat Mass Index Based on Age in Physically Active Males Using Receiver Operating Characteristic Curve. Diseases, 11(4), 137. https://doi.org/10.3390/diseases11040137








