Exploring Potential Determinants of Mosquito Net Ownership and Use in Somalia: A Cross-Sectional Study
Abstract
1. Introduction
2. Methods
2.1. Study Context
2.2. Data Source
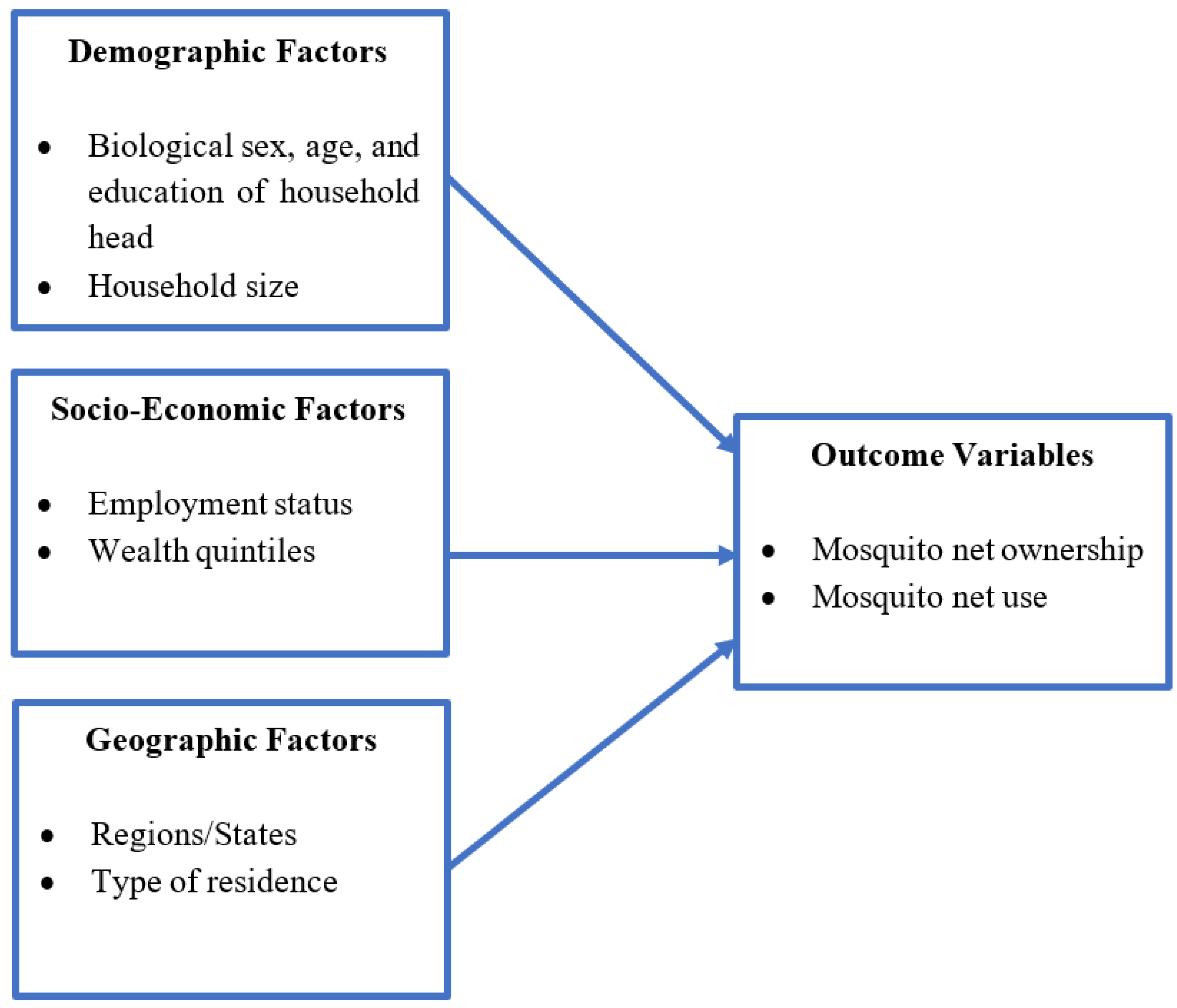
2.3. Variables
2.4. Data Analysis
2.5. Ethical Approval
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cox, F.E. History of the discovery of the malaria parasites and their vectors. Parasites Vectors 2010, 3, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Tuteja, R. Malaria—An overview. FEBS J. 2007, 274, 4670–4679. [Google Scholar] [CrossRef] [PubMed]
- Murray, C.J.L.; Rosenfeld, L.C.; Lim, S.S.; Andrews, K.G.; Foreman, K.J.; Haring, D.; Fullman, N.; Naghavi, M.; Lozano, R.; Lopez, A.D. Global malaria mortality between 1980 and 2010: A systematic analysis. Lancet 2012, 379, 413–431. [Google Scholar] [CrossRef]
- Cibulskis, R.E.; Alonso, P.; Aponte, J.; Aregawi, M.; Barrette, A.; Bergeron, L.; Fergus, C.A.; Knox, T.; Lynch, M.; Patouillard, E.; et al. Malaria: Global progress 2000–2015 and future challenges. Infect. Dis. Poverty 2016, 5, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Weiss, D.J.; Lucas, T.C.; Nguyen, M.; Nandi, A.K.; Bisanzio, D.; Battle, K.E.; Cameron, E.; Twohig, K.A.; Pfeffer, D.A.; Rozier, J.A.; et al. Mapping the global prevalence, incidence, and mortality of Plasmodium falciparum, 2000–2017: A spatial and temporal modelling study. Lancet 2019, 394, 322–331. [Google Scholar] [CrossRef]
- Institute for Health Metrics and Evaluation (IHME). GBD Compare. Seattle, WA: IHME, University of Washington. 2015. Available online: http://vizhub.healthdata.org/gbd-compare (accessed on 18 February 2022).
- World Health Organization. World Malaria Report 2021; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Wangdi, K.; Furuya-Kanamori, L.; Clark, J.; Barendregt, J.J.; Gatton, M.L.; Banwell, C.; Kelly, G.C.; Doi, S.A.; Clements, A.C. Comparative effectiveness of malaria prevention measures: A systematic review and network meta-analysis. Parasites Vectors 2018, 11, 1–13. [Google Scholar] [CrossRef] [PubMed]
- White, M.T.; Conteh, L.; Cibulskis, R.; Ghani, A.C. Costs and cost-effectiveness of malaria control interventions-a systematic review. Malar. J. 2011, 10, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Scates, S.S.; Finn, T.P.; Wisniewski, J.; Dadi, D.; Mandike, R.; Khamis, M.; Greer, G.; Serbantez, N.; Segbaya, S.; Owusu, P.; et al. Costs of insecticide-treated bed net distribution systems in sub-Saharan Africa. Malar. J. 2020, 19, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Tapera, O. Determinants of long-lasting insecticidal net ownership and utilization in malaria transmission regions: Evidence from Zimbabwe Demographic and Health Surveys. Malar. J. 2019, 18, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Kateera, F.; Ingabire, C.M.; Hakizimana, E.; Rulisa, A.; Karinda, P.; Grobusch, M.P.; Mutesa, L.; van Vugt, M.; Mens, P.F. Long-lasting insecticidal net source, ownership and use in the context of universal coverage: A household survey in eastern Rwanda. Malar. J. 2015, 14, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Tassew, A.; Hopkins, R.; Deressa, W. Factors influencing the ownership and utilization of long-lasting insecticidal nets for malaria prevention in Ethiopia. Malar. J. 2017, 16, 1–9. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Somalia. 2018. Available online: https://www.who.int/malaria/publications/country-profiles/profile_som_en.pdf?ua=1 (accessed on 17 March 2022).
- World Health Organization. Estimated Malaria Incidence (per 1000 Population at Risk). 2022. Available online: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/malaria-incidence-(per-1000-population-at-risk) (accessed on 17 March 2022).
- Federal Ministry of Health; Ministry of Health [Somaliland]; Ministry of Health [Puntland]; UNICEF. BrandPro, GroundWork, 2020. Somalia Micronutrient Survey 2019. Available online: https://www.unicef.org/somalia/media/1681/file/Somalia-Micronutient-Survey-2019.pdf (accessed on 17 March 2022).
- Donkor, W.E.; Mbai, J.; Sesay, F.; Ali, S.I.; Woodruff, B.A.; Hussein, S.M.; Mohamud, K.M.; Muse, A.; Mohamed, W.S.; Mohamoud, A.M.; et al. Risk factors of stunting and wasting in Somali pre-school age children: Results from the 2019 Somalia micronutrient survey. BMC Public Health 2022, 22, 1–11. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Vector-Borne Diseases. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/vector-borne-diseases (accessed on 30 October 2022).
- Ernst, K.C.; Hayden, M.H.; Olsen, H.; Cavanaugh, J.L.; Ruberto, I.; Agawo, M.; Munga, S. Comparing ownership and use of bed nets at two sites with differential malaria transmission in western Kenya. Malar. J. 2016, 15, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Perkins, J.M.; Krezanoski, P.; Takada, S.; Kakuhikire, B.; Batwala, V.; Tsai, A.C.; Christakis, N.A.; Bangsberg, D.R. Social norms, misperceptions, and mosquito net use: A population-based, cross-sectional study in rural Uganda. Malar. J. 2019, 18, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Pulford, J.; Hetzel, M.W.; Bryant, M.; Siba, P.M.; Mueller, I. Reported reasons for not using a mosquito net when one is available: A review of the published literature. Malar. J. 2011, 10, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Federal Ministry of Health. National Health Data Warehouse. 2022. Available online: https://hmissomalia.net/dhis-web-commons/security/login.action (accessed on 25 March 2022).
- Krumpal, I. Determinants of social desirability bias in sensitive surveys: A literature review. Qual. Quant. 2013, 47, 2025–2047. [Google Scholar] [CrossRef]
| Variables | n | Weighted % |
|---|---|---|
| Sex of Household Head | ||
| Male | 262 | 12.87 |
| Female | 1910 | 87.13 |
| Age of Household Head | ||
| 25 or younger | 491 | 22.01 |
| 26–35 | 627 | 28.37 |
| 36–45 | 399 | 18.83 |
| 46 or higher | 655 | 30.79 |
| Education of Household Head | ||
| None or preschool | 1569 | 75.49 |
| Koranic | 257 | 10.53 |
| Primary or higher | 334 | 13.98 |
| Household Size | ||
| Small (1–3 people) | 1034 | 49.96 |
| Medium (4–7) | 883 | 38.25 |
| Large (8 or more) | 255 | 11.78 |
| Any Employed Household Member | ||
| Yes | 792 | 32.99 |
| No | 1373 | 67.01 |
| Wealth Quintile | ||
| Poorest | 286 | 20.25 |
| Poorer | 336 | 19.75 |
| Middle | 485 | 20.01 |
| Richer | 573 | 20.03 |
| Richest | 492 | 19.95 |
| Regions/States | ||
| Banadir | 458 | 14.88 |
| Somaliland | 455 | 26.44 |
| Puntland | 343 | 9.37 |
| Hirshabelle | 163 | 4.51 |
| Galmudug | 249 | 7.47 |
| Southwest | 217 | 15.97 |
| Jubaland | 287 | 21.36 |
| Type of Residence | ||
| Rural | 700 | 34.82 |
| Urban | 1129 | 49.48 |
| IDP | 343 | 15.70 |
| Own At Least One Mosquito Net | ||
| Yes | 1290 | 57.26 |
| No | 818 | 42.74 |
| All Mosquito Nets Used | ||
| Yes | 1186 | 92.3 |
| No | 104 | 7.7 |
| Ownership * | All Nets Used * | |||
|---|---|---|---|---|
| Study Variables | F | p-value | F | p-value |
| Sex of Household Head | 1.51 | 0.222 | 0.22 | 0.637 |
| Age of Household Head | 10.58 | <0.001 | 1.79 | 0.153 |
| Education of Household Head | 10.74 | <0.001 | 5.60 | 0.005 |
| Household Size | 3.14 | 0.046 | 1.15 | 0.320 |
| Any Household Member with Employment | 28.96 | <0.001 | 6.67 | 0.011 |
| Wealth Quintiles | 18.85 | <0.001 | 1.26 | 0.290 |
| States | 5.13 | <0.001 | 3.02 | 0.009 |
| Type of Residence | 11.59 | <0.001 | 0.54 | 0.582 |
| Odds Ratio | Std. Err. | t | p-Value | 95% CIs | ||
|---|---|---|---|---|---|---|
| Sex of Household Head (Ref: Male) | ||||||
| Female | 0.924 | 0.163 | −0.45 | 0.657 | 0.652 | 1.310 |
| Age of Household Head (Ref: 25 or younger) | ||||||
| 26–35 | 2.247 | 0.368 | 4.94 | <0.001 | 1.625 | 3.105 |
| 36–45 | 2.087 | 0.432 | 3.55 | 0.001 | 1.386 | 3.143 |
| 46 or older | 1.312 | 0.213 | 1.67 | 0.097 | 0.952 | 1.810 |
| Education of Household Head (Ref: None or preschool) | ||||||
| Koranic | 0.664 | 0.119 | −2.28 | 0.024 | 0.466 | 0.947 |
| Primary or Higher | 0.923 | 0.143 | −0.52 | 0.603 | 0.680 | 1.252 |
| Household Size (Ref: Small) | ||||||
| Medium | 0.835 | 0.122 | −1.23 | 0.219 | 0.625 | 1.115 |
| Large | 0.611 | 0.141 | −2.13 | 0.035 | 0.387 | 0.965 |
| Any household member with employment (Ref: No) | ||||||
| Yes | 1.480 | 0.246 | 2.36 | 0.020 | 1.065 | 2.057 |
| Wealth quintiles (Ref: Poorest) | ||||||
| Poorer | 2.264 | 0.582 | 3.18 | 0.002 | 1.362 | 3.763 |
| Middle | 4.776 | 1.503 | 4.97 | <0.001 | 2.564 | 8.897 |
| Richer | 9.919 | 3.583 | 6.35 | <0.001 | 4.857 | 20.256 |
| Richest | 12.822 | 4.721 | 6.93 | <0.001 | 6.193 | 26.547 |
| Regions/States (Ref: Banadir) | ||||||
| Somaliland | 2.388 | 0.643 | 3.23 | 0.002 | 1.402 | 4.066 |
| Puntland | 2.132 | 0.536 | 3.01 | 0.003 | 1.297 | 3.506 |
| Hirshabelle | 3.930 | 1.213 | 4.44 | <0.001 | 2.135 | 7.233 |
| Galmudug | 11.376 | 5.617 | 4.92 | <0.001 | 4.287 | 30.190 |
| Southwest | 3.580 | 1.119 | 4.08 | <0.001 | 1.930 | 6.641 |
| Jubaland | 4.303 | 1.715 | 3.66 | <0.001 | 1.957 | 9.460 |
| Type of Residence (Ref: Rural) | ||||||
| Urban | 1.925 | 0.500 | 2.52 | 0.013 | 1.152 | 3.217 |
| IDP | 1.170 | 0.366 | 0.50 | 0.616 | 0.631 | 2.170 |
| Constant | 0.061 | 0.027 | −6.24 | <0.001 | 0.025 | 0.148 |
| F-statistic (degrees of freedom) | 6.49 (21, 123) | |||||
| Odds Ratio | Std. Err. | t | p-Value | 95% CIs | ||
|---|---|---|---|---|---|---|
| Sex of Household Head (Ref: Male) | ||||||
| Female | 1.089 | 0.454 | 0.21 | 0.837 | 0.478 | 2.482 |
| Age of Household Head (Ref: 25 or younger) | ||||||
| 26–35 | 0.445 | 0.161 | −2.23 | 0.027 | 0.217 | 0.912 |
| 36–45 | 0.450 | 0.175 | −2.06 | 0.042 | 0.209 | 0.970 |
| 46 or older | 0.366 | 0.132 | −2.79 | 0.006 | 0.180 | 0.747 |
| Education of Household Head (Ref: None or preschool) | ||||||
| Koranic | 0.650 | 0.271 | −1.03 | 0.303 | 0.286 | 1.481 |
| Primary or Higher | 1.075 | 0.465 | 0.17 | 0.867 | 0.457 | 2.528 |
| Household Size (Ref: Small) | ||||||
| Medium | 1.003 | 0.275 | 0.01 | 0.992 | 0.583 | 1.724 |
| Large | 0.672 | 0.282 | −0.95 | 0.345 | 0.293 | 1.541 |
| Any household member with employment (Ref: No) | ||||||
| Yes | 0.677 | 0.242 | −1.09 | 0.277 | 0.334 | 1.372 |
| Wealth quintiles (Ref: Poorest) | ||||||
| Poorer | 2.706 | 1.590 | 1.69 | 0.092 | 0.847 | 8.647 |
| Middle | 0.746 | 0.437 | −0.50 | 0.618 | 0.234 | 2.377 |
| Richer | 0.648 | 0.411 | −0.68 | 0.495 | 0.185 | 2.270 |
| Richest | 0.309 | 0.201 | −1.81 | 0.073 | 0.086 | 1.116 |
| Regions/States (Ref: Banadir) | ||||||
| Somaliland | 1.849 | 0.782 | 1.45 | 0.148 | 0.801 | 4.266 |
| Puntland | 1.307 | 0.724 | 0.48 | 0.630 | 0.437 | 3.907 |
| Hirshabelle | 1.043 | 0.605 | 0.07 | 0.942 | 0.331 | 3.287 |
| Galmudug | 0.303 | 0.113 | −3.20 | 0.002 | 0.145 | 0.634 |
| Southwest | 0.213 | 0.105 | −3.14 | 0.002 | 0.081 | 0.565 |
| Jubaland | 0.728 | 0.425 | −0.54 | 0.588 | 0.230 | 2.310 |
| Type of Residence (Ref: Rural) | ||||||
| Urban | 0.991 | 0.347 | −0.03 | 0.980 | 0.496 | 1.982 |
| IDP | 0.646 | 0.292 | −0.97 | 0.335 | 0.265 | 1.578 |
| Constant | 74.558 | 57.093 | 5.63 | <0.001 | 16.399 | 338.965 |
| F-statistic (degrees of freedom) | 4.47 (21, 116) | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hirai, M.; Umar, U.; Darikwa, P.; Osman, A.A.; Mohamed, A.; Jama, A.M.; Masheti, C.; Kader, M. Exploring Potential Determinants of Mosquito Net Ownership and Use in Somalia: A Cross-Sectional Study. Diseases 2022, 10, 109. https://doi.org/10.3390/diseases10040109
Hirai M, Umar U, Darikwa P, Osman AA, Mohamed A, Jama AM, Masheti C, Kader M. Exploring Potential Determinants of Mosquito Net Ownership and Use in Somalia: A Cross-Sectional Study. Diseases. 2022; 10(4):109. https://doi.org/10.3390/diseases10040109
Chicago/Turabian StyleHirai, Mitsuaki, Usman Umar, Patricia Darikwa, Ali Abdirahman Osman, Abdirahman Mohamed, Ahmed Mohamed Jama, Carolyn Masheti, and Millhia Kader. 2022. "Exploring Potential Determinants of Mosquito Net Ownership and Use in Somalia: A Cross-Sectional Study" Diseases 10, no. 4: 109. https://doi.org/10.3390/diseases10040109
APA StyleHirai, M., Umar, U., Darikwa, P., Osman, A. A., Mohamed, A., Jama, A. M., Masheti, C., & Kader, M. (2022). Exploring Potential Determinants of Mosquito Net Ownership and Use in Somalia: A Cross-Sectional Study. Diseases, 10(4), 109. https://doi.org/10.3390/diseases10040109





