915-MHz Continuous-Wave Doppler Radar Sensor for Detection of Vital Signs
Abstract
:1. Introduction
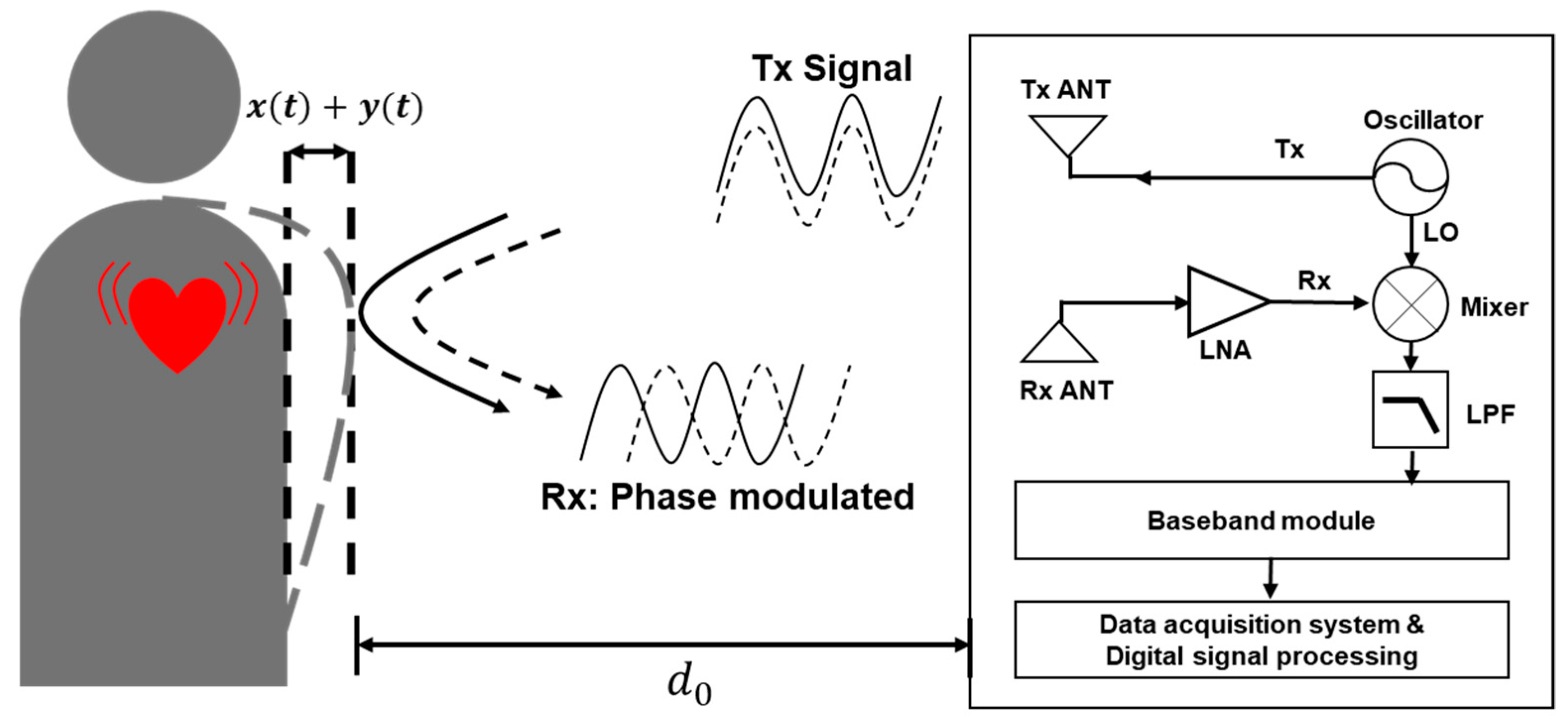
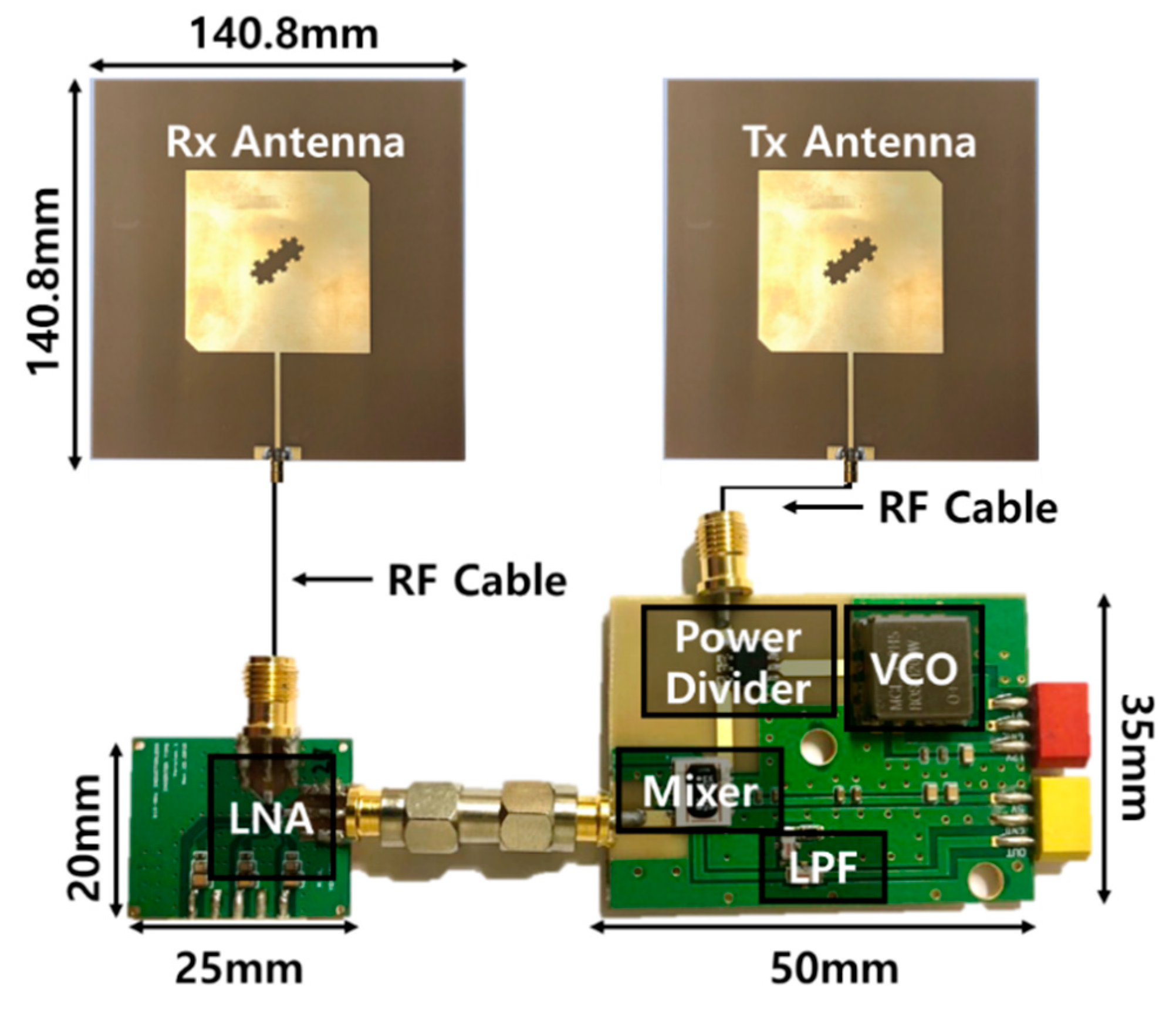
2. 915 MHz CW Doppler Radar Sensor
2.1. Radar Architecture
2.2. Path-Loss Calculation
3. Implementation of Radar Sensor
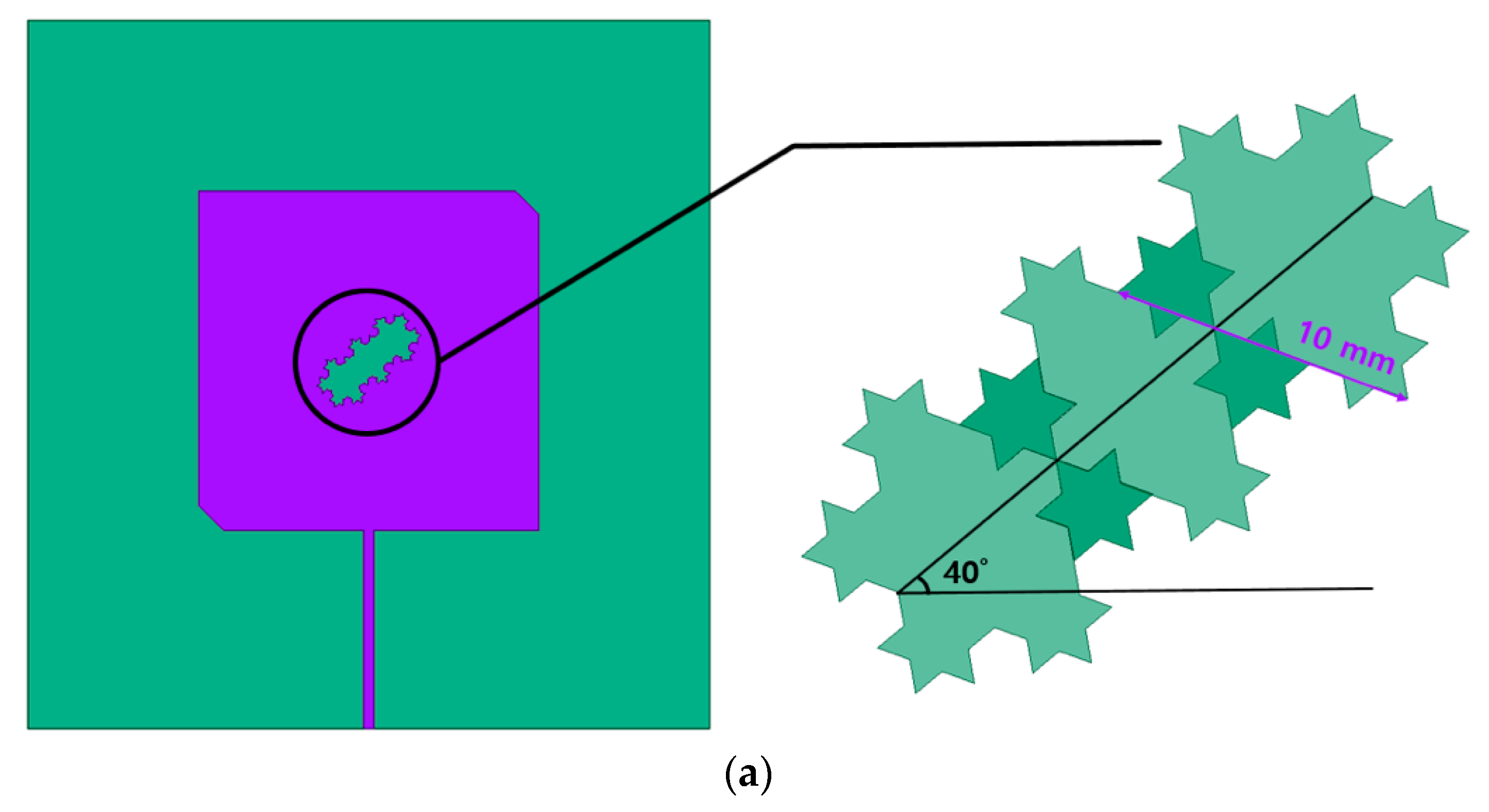
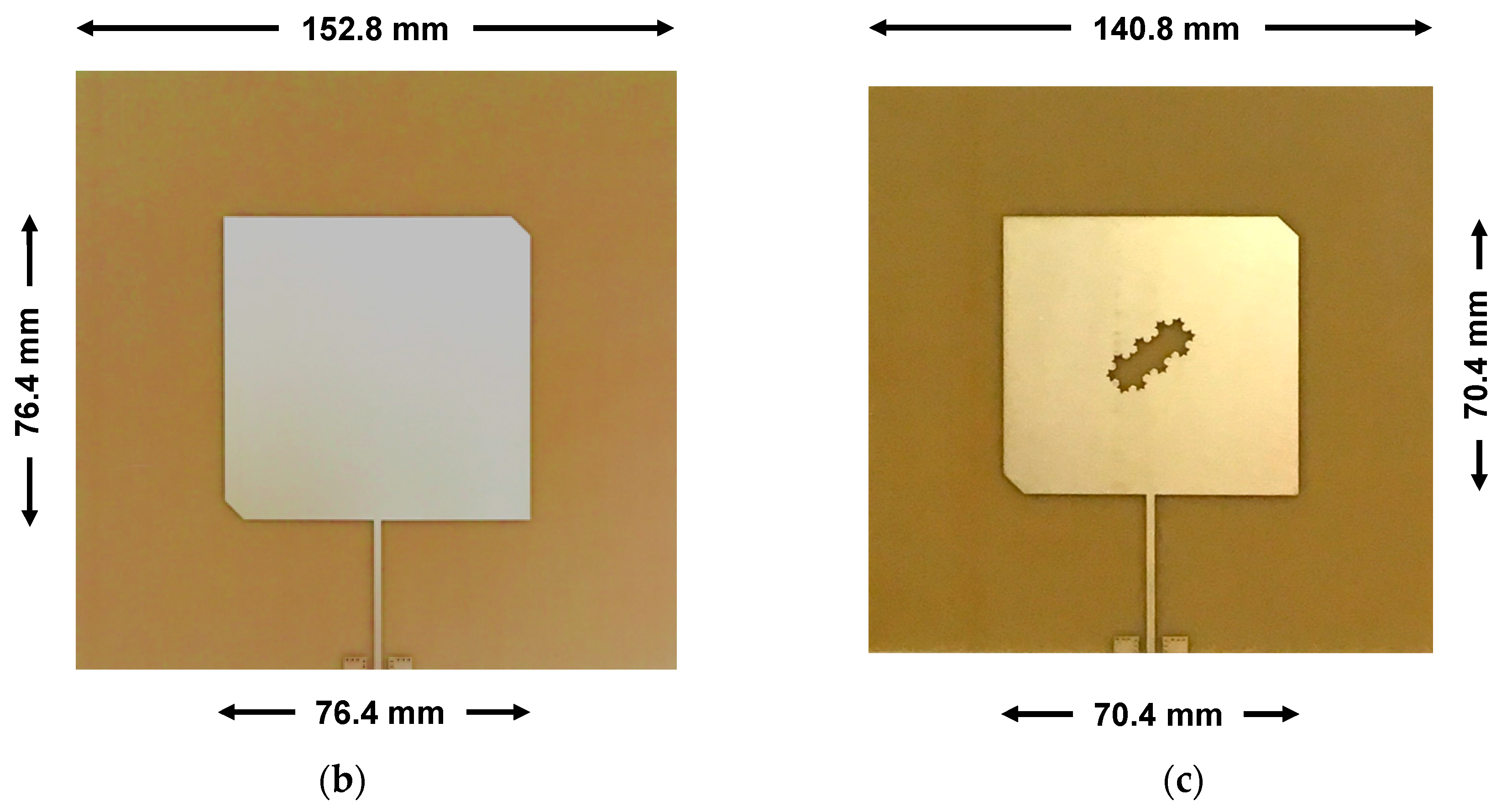
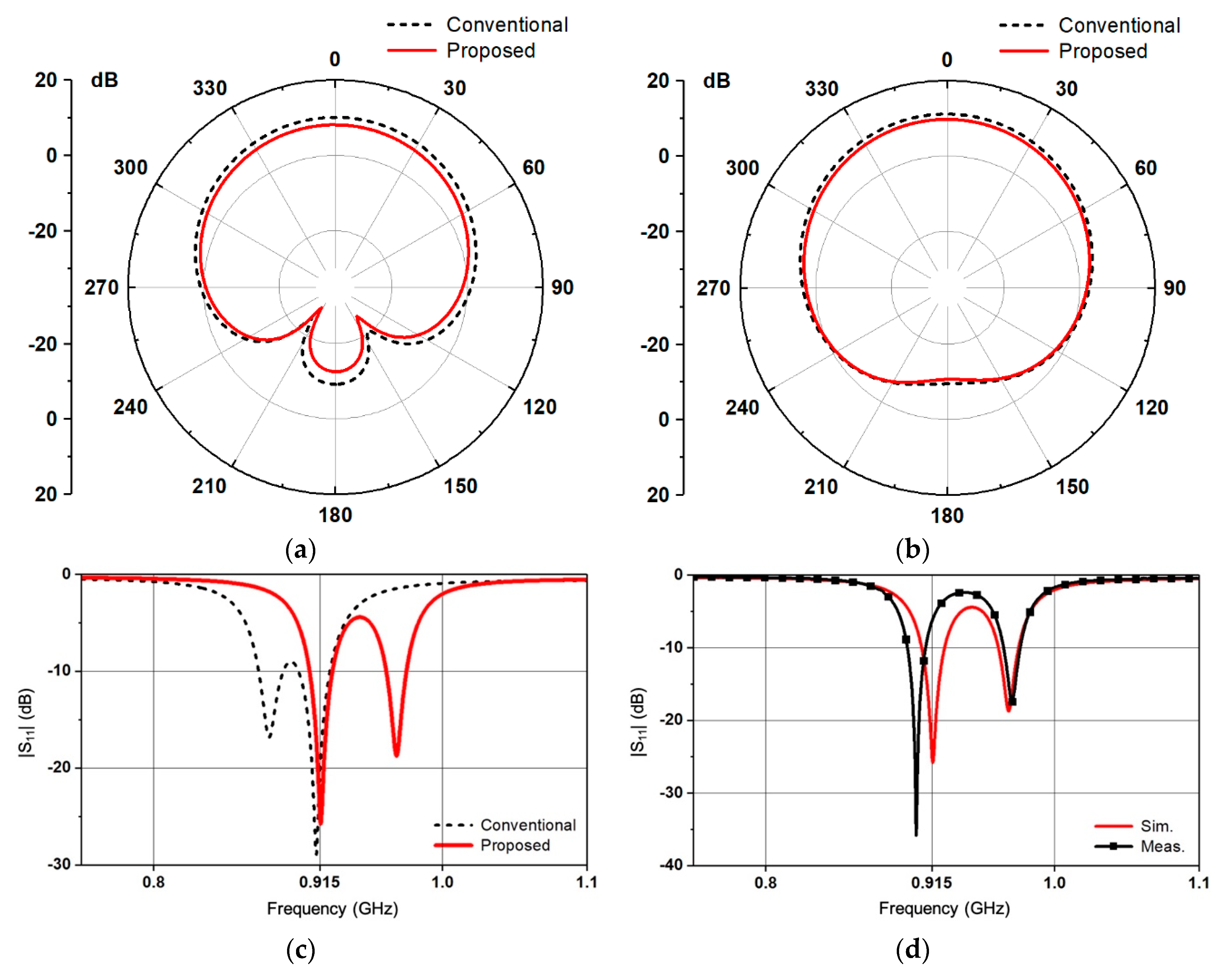
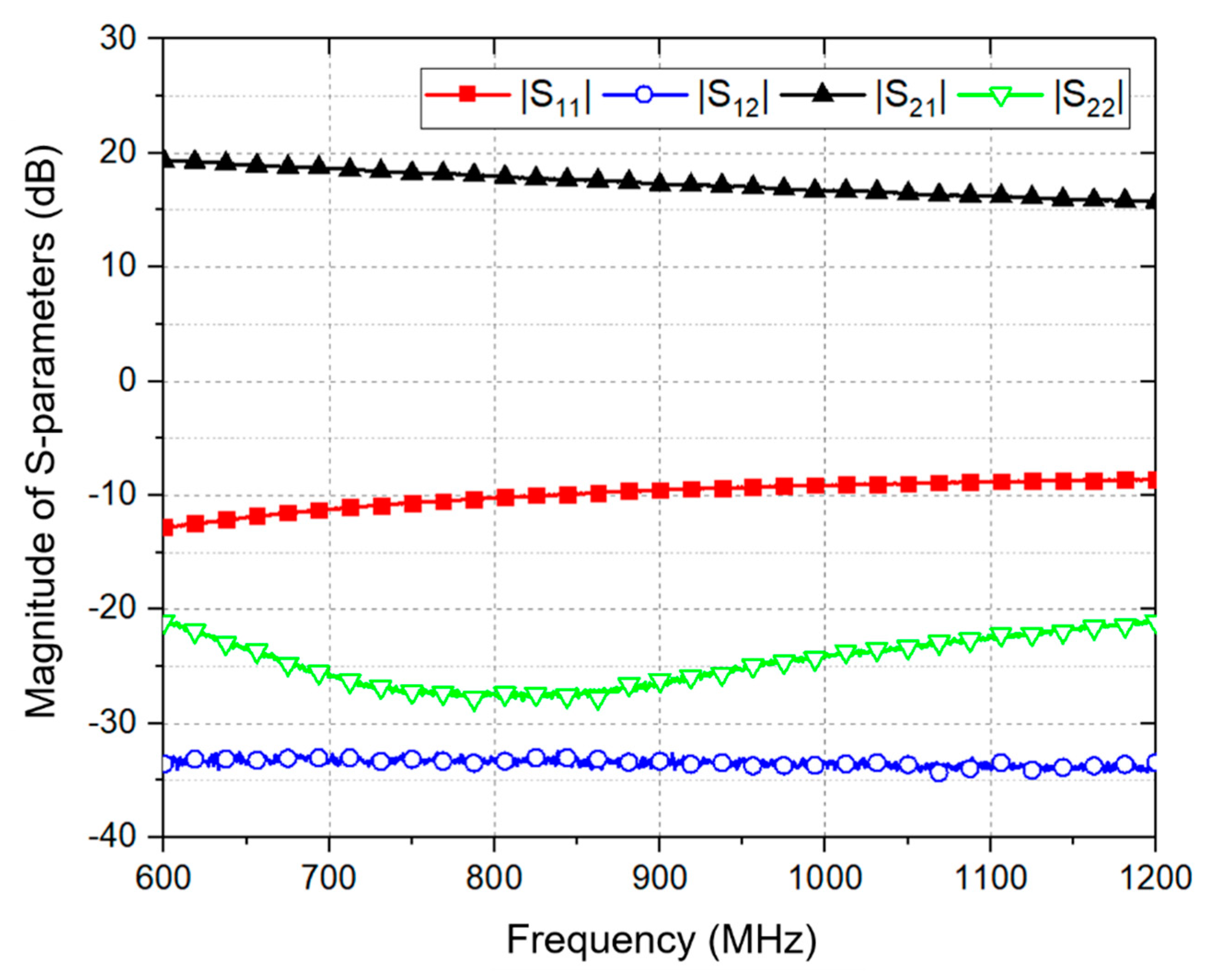
3.1. Fractal-Slot Patch Antenna
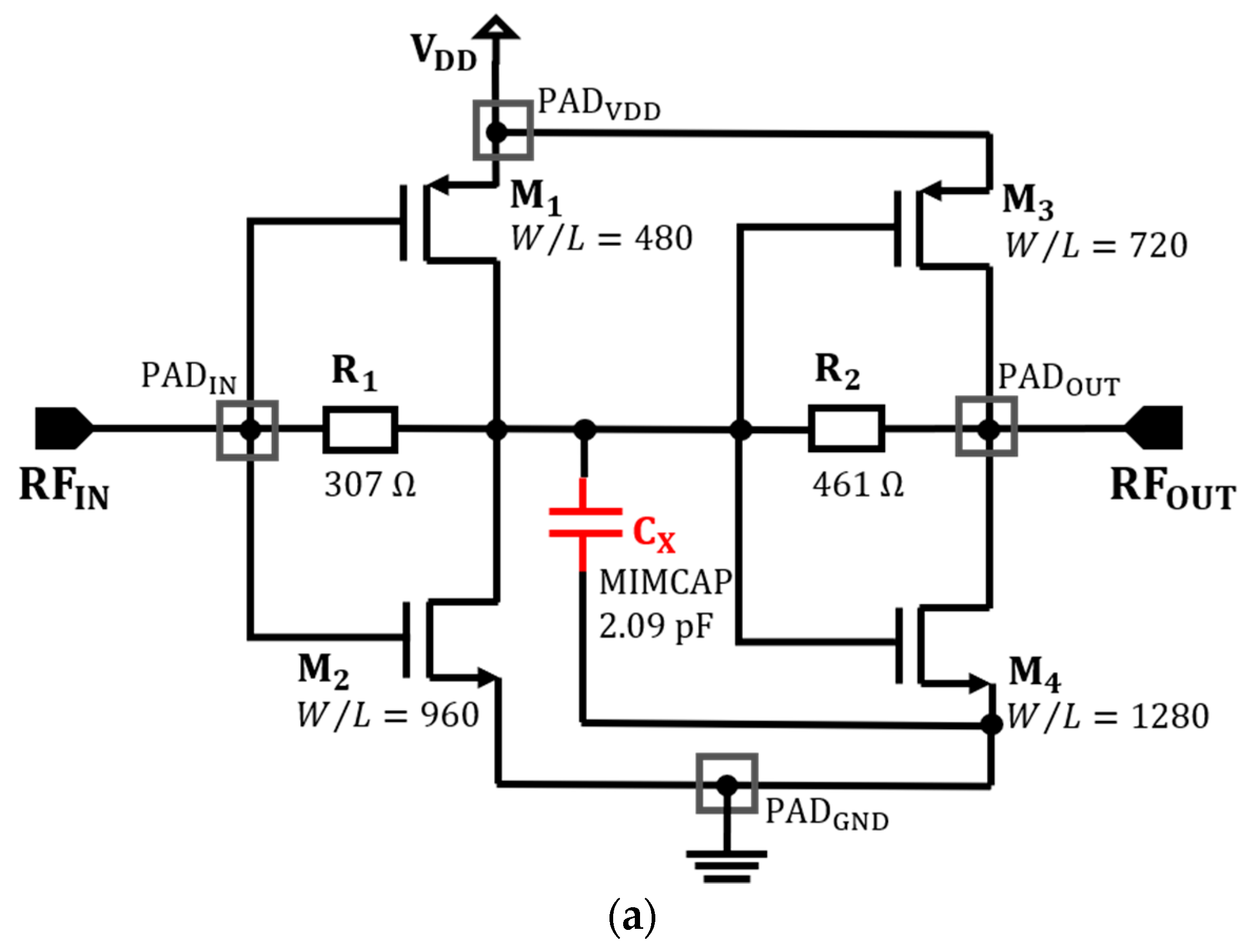
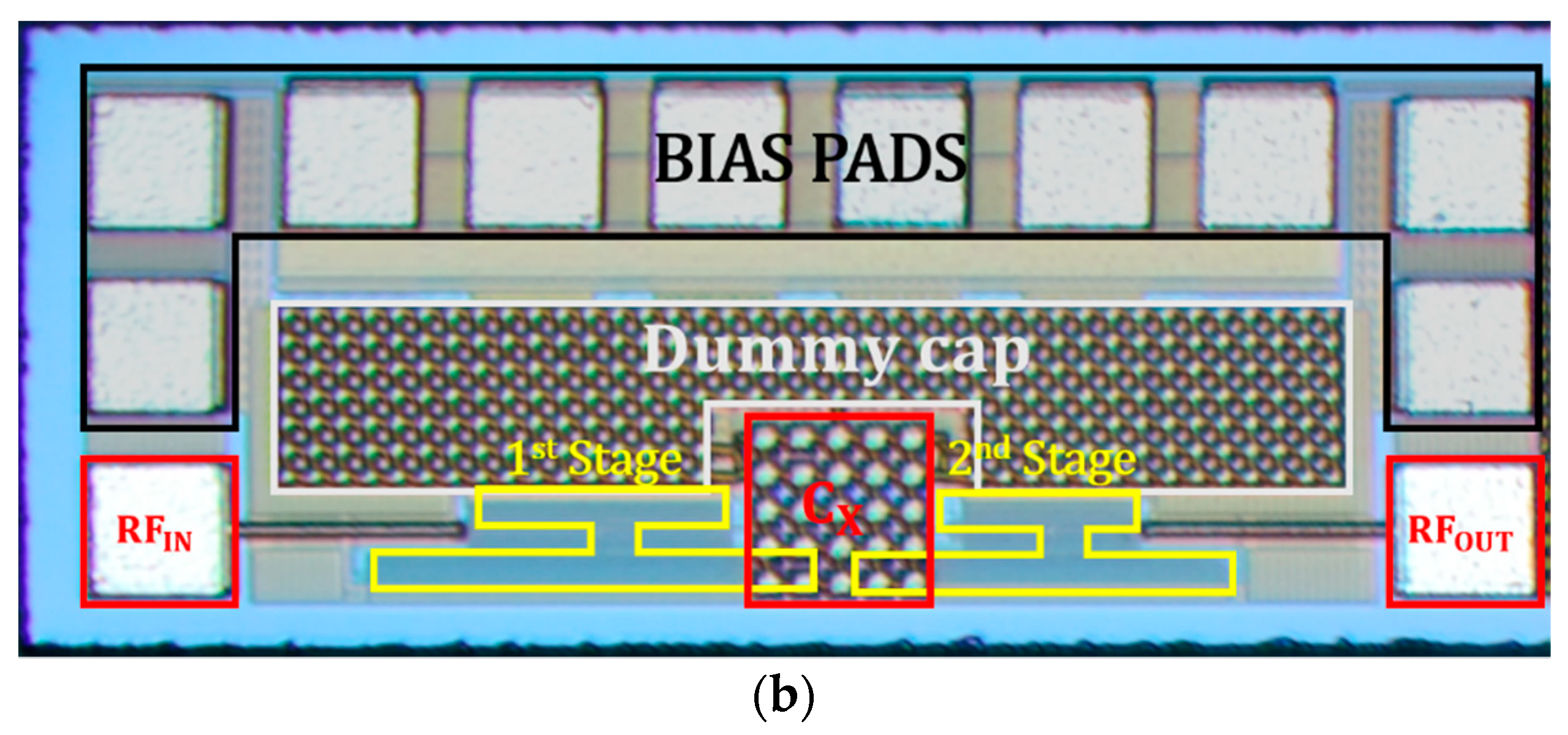
3.2. Two-Stage LNA
3.3. 915 MHz Radar Sensor Module
4. Measurements and Discussion
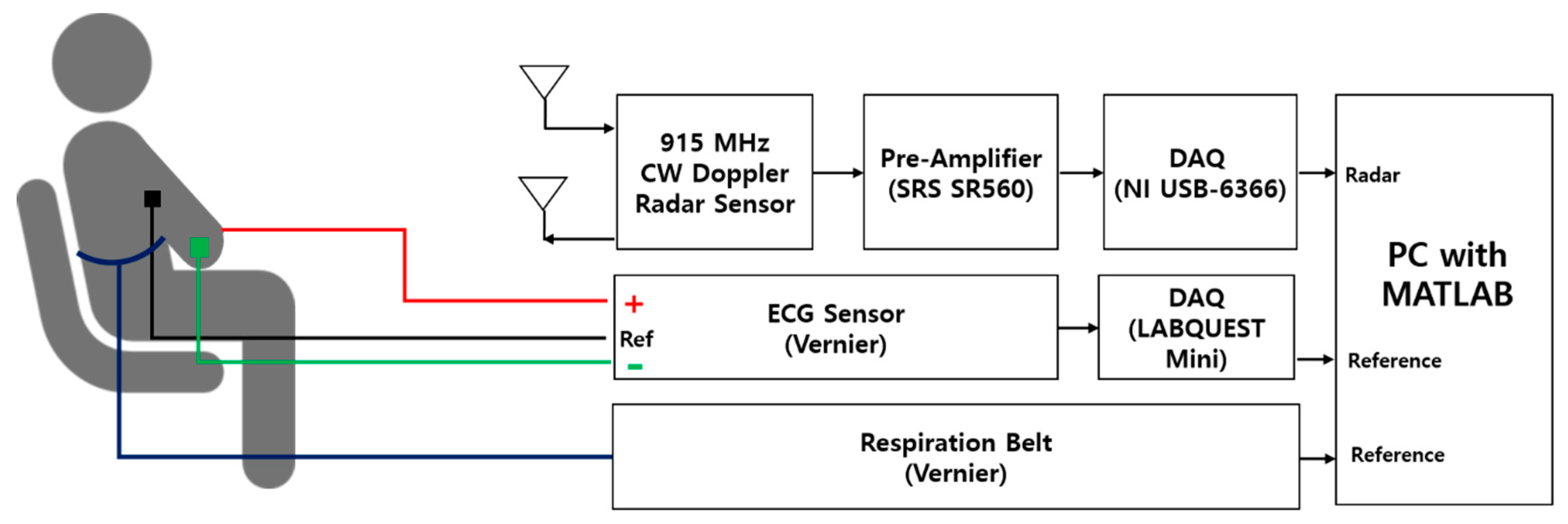
4.1. Experiment Setup
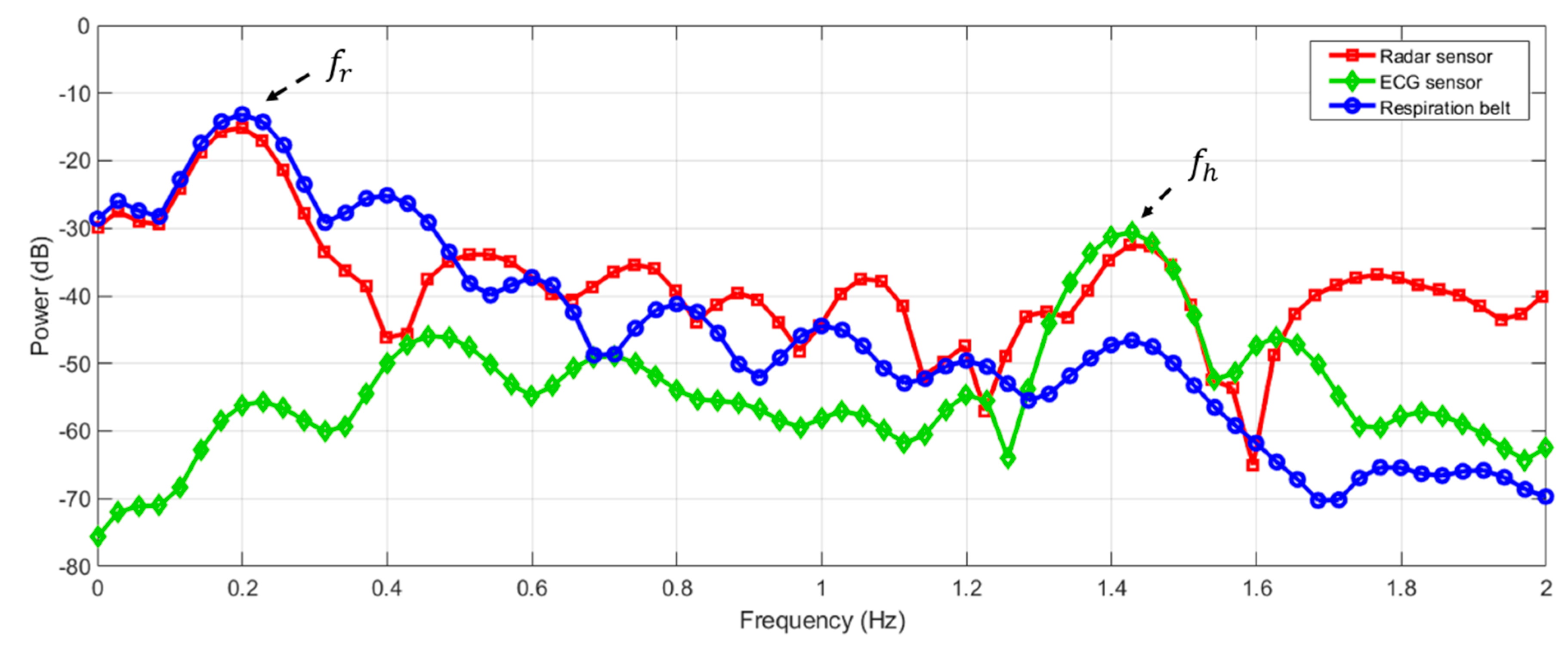
4.2. Measurement Results and Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Chen, K.M.; Huang, Y.; Zhang, J. Microwave life-detection systems for searching human subjects under earthquake rubble or behind barier. IEEE Trans. Biomed. Eng. 2000, 47, 105–114. [Google Scholar] [CrossRef] [PubMed]
- Lin, F.; Zhuang, Y.; Li, C. Sleep sense: A noncontact and cost-effective sleep monitoring system. IEEE Trans. Biomed. Circuits Syst. 2016, 11, 189–202. [Google Scholar] [CrossRef] [PubMed]
- Brüster, C.; Antink, C.H.; Wartzek, T. Ambient and unobtrusive cardiorespiratory monitoring techniques. IEEE Rev. Biomed. Eng. 2015, 8, 30–43. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.-K.; Horng, T.-S.; Peng, K.-C.; Jau, J.-K.; Li, J.-Y.; Chen, C.-C. Single-antenna Doppler radars using self and mutual injection locking for vital sign detection with random body movement cancellation. IEEE Trans. Microwave Theory Tech. 2011, 59, 3577–3587. [Google Scholar] [CrossRef]
- Xiao, Y.; Lin, J.; Boric-Lubecke, O.; Lubecke, M. Frequency-tuning technique for remote detection of heartbeat and respiration using low-power double-sideband transmission in the ka-band. IEEE Trans. Microwave Theory Tech. 2006, 54, 2023–2032. [Google Scholar] [CrossRef]
- Lee, J.-H.; Park, S.-O. A 14 GHz non-contact radar system for long range heart rate detection. In Proceedings of the International Symposium on Antennas and Propagation, Nanjing, China, 23–25 October 2013. [Google Scholar]
- Lubecke, O.B.; Lukecke, V.M.; Droitcour, A.D.; Park, B.K.; Singh, A. Doppler Radar Physiological Sensing; Wiley: Hoboken, NJ, USA, 2016. [Google Scholar]
- Gabriel, C. Compilation of the Dielectric Properties of Body Tissues at RF and Microwave Frequency; Brooks AFB: San Antonio, Tx, USA, 1996. [Google Scholar]
- Jang, B.J.; Wi, S.H.; Yook, J.G.; Lee, M.Q.; Lee, K.J. Wireless bio-radar sensor for heartbeat and respiration detection. Prog. Electromagnet. Res. C 2008, 5, 149–168. [Google Scholar]
- Droitcour, A. Non-contact Measurement of Heart and Respiration Rates with A Single-Chip Microwave Doppler Radar. Ph.D. Thesis, Stanford University, Stanford, CA, USA, June 2006. [Google Scholar]
- Yilmaz, T.; Foster, R.; Hao, Y. Detecting vital signs with wearable wireless sensors. Sensors 2010, 10, 10837–10862. [Google Scholar] [CrossRef] [PubMed]
- Andersen, N.; Granhaug, K. A 188-mW pulse-based radar SoC in 55-nm CMOS for non-contact human vital signs detection. IEEE J. Solid-State Circuits 2017, 52, 3421–3433. [Google Scholar] [CrossRef]
- Alomainy, A.; Hao, Y.; Hu, X.; Parini, C.; Hall, P. UWB on-body radio propagation and system modelling for wireless body-centric networks. IEE Proc. Commun. 2006, 153, 107–114. [Google Scholar] [CrossRef]
- Zhadobov, M.; Chahar, N.; Sauleau, R.; Le Quement, C.; Le Drean, Y. Millimeter-wave interactions with the human body: state of knowledge and recent advances. Int. J. Microwave Wireless Technolog. 2011, 3, 237–247. [Google Scholar] [CrossRef]
- EMF Guidelines, International Commission on Non-Ionizing Radiation Protection (ICNIRP). Available online: https://www.icnirp.org/en/frequencies/high-frequency/index.html (accessed on 12 April 2019).
- Kiriazi, J.E.; Boric-Lubecke, O.; Lubecke, V.M. Dual-Frequency Technique for Assessment of Cardiopulmonary Effective RCS and Displacement. IEEE Sensor J. 2012, 12, 574–582. [Google Scholar] [CrossRef]
- Balanis, C.A. Antenna Theory: Analysis and Design, 3rd edition; John Wiley & Sons: Hoboken, NJ, USA, 2005; p. 34. [Google Scholar]
- Droitcour, A.D.; Boric-Lubecke, O.; Lubecke, V.M.; Lin, J.; Kovacs, G.T.A. Range correlation and I/Q performance benefits in single-chip silicon Doppler radars for noncontact cardiopulmonary monitoring. IEEE Trans. Microwave Theory Tech. 2004, 52, 838–848. [Google Scholar] [CrossRef]
- Park, B.-K.; Yamada, S.; Lubecke, V.M.; Boric-Lubecke, O. Single channel receiver limitations in Doppler radar measurements of periodic motion. In Proceedings of the 2006 IEEE Radio Wireless Symposium, San Diego, CA, USA, 17–19 January 2006. [Google Scholar]
- Park, B.-K.; Boric-Lubecke, O.; Lubecke, V.M. Arctangent demodulation with DC offset compensation in quadrature Doppler radar receiver systems. IEEE Trans. Microwave Theory Tech. 2007, 55, 1073–1079. [Google Scholar] [CrossRef]
- Andreuccetti, R.D.; Petrucchi, C. An internet resource for the calculation of the dielectric properties of body tissues in the frequency range 10 Hz–100 GHz. Available online: http://niremf.ifac.cnr.it/tissprop (accessed on 3 April 2019).
- Staderini, E.M. UWB radars in medicine. IEEE Aerosp. Electron. Syst. Mag. 2002, 17, 13–18. [Google Scholar] [CrossRef]
- The visible human project. Available online: https://www.nlm.nih.gov/research/visible/visible_ human.html (accessed on 12 April 2019).
- Lee, J.H. Non-Invasive Detection of Respiration and Heart Rate Using High Sensitivity Radar. Ph.D. Thesis, Korea Advanced Institute of Science and Technology, Daejeon, Korea, 2014. [Google Scholar]
- Oloumi, D.; Ebadi, S.; Kordzadeh, A.; Semnani, A.; Mousavi, P.; Gong, Z. Miniaturized reflectarray unit cell using fractal-shaped patch-slot configuration. IEEE Antennas Wirel. Propag. Lett. 2012, 11, 10–13. [Google Scholar] [CrossRef]
- Chew, D.K.C.; Saunders, S.R. Meander line technique for size reduction of quadrifilar helix antenna. IEEE Antennas Wirel. Propag. Lett. 2002, 1, 109–111. [Google Scholar] [CrossRef]
- Aguilar, S.M.; Al-Joumayly, M.A.; Burfeindt, M.J.; Behdad, N.; Hagness, S.C. Multiband miniaturized patch antennas for a compact, shielded microwave breast imaging array. IEEE Trans. Antennas Propag. 2014, 62, 1221–1231. [Google Scholar] [CrossRef] [PubMed]
- Oraizi, H.; Hedayati, S. Circularly polarized multiband microstrip antenna using the square and Giuseppe Peano fractals. IEEE IEEE Trans. Antennas Propag. 2012, 60, 3466–3470. [Google Scholar] [CrossRef]
- Park, J.-Y.; Lee, J.-Y.; Yeo, C.-K.; Yun, T.-Y. Analysis and optimization of a resistive-feedback inverter LNA. Microwave Opt. Technol. Lett. 2018, 60, 1143–1151. [Google Scholar] [CrossRef]
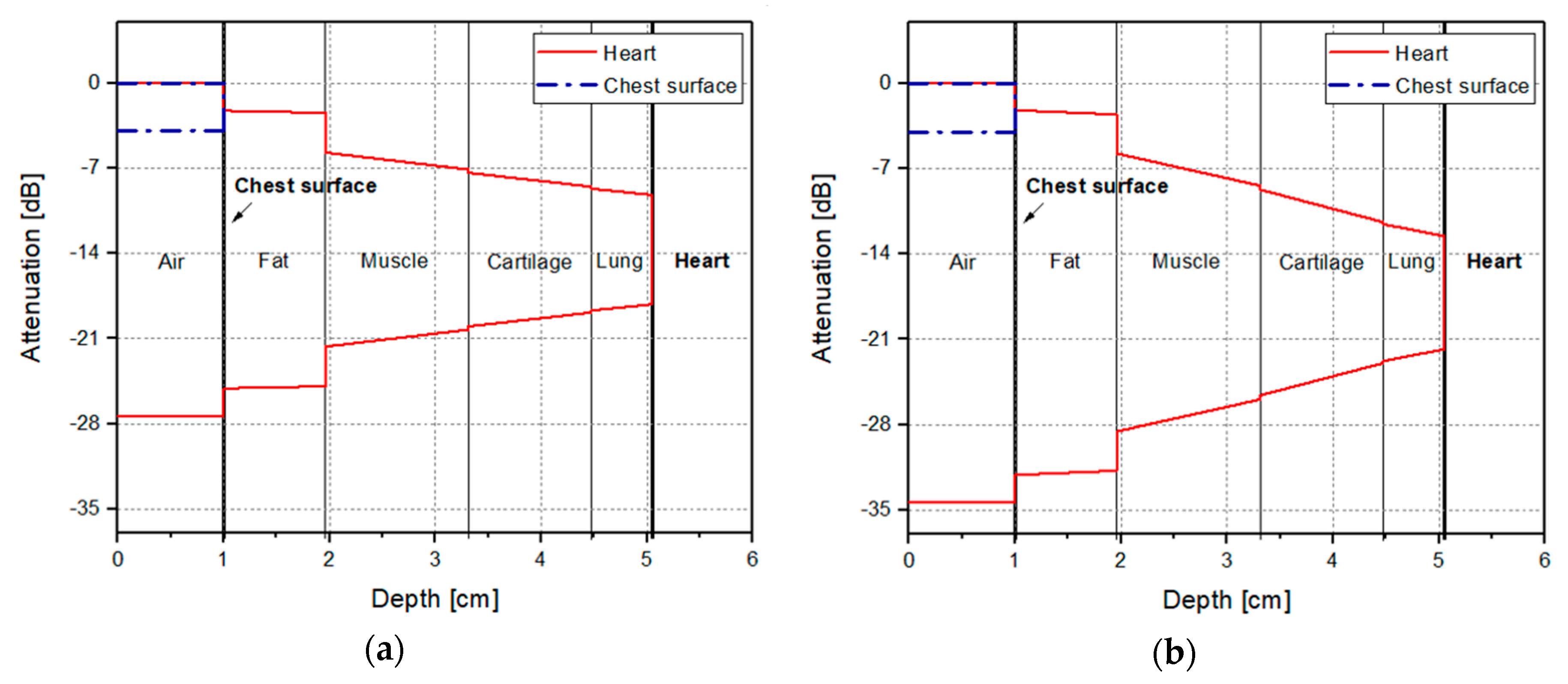

| Type of Tissue | Conductivity (S/m) | Relative Permittivity | Impedance (Ω) | Speed (m/s) | Attenuation (m−1) | Thickness (cm) |
|---|---|---|---|---|---|---|
| Air | 0 | 1 | 376.87 | 3 × 108 | 0 | 1 |
| Fat | 0.05 | 5.46 | 159.27 + 14.61i | 1.28 × 108 | 4.13 | 0.96 |
| Muscle | 0.95 | 55 | 48.8 + 8.04i | 3.99 × 107 | 23.76 | 1.35 |
| Cartilage | 0.79 | 42.6 | 55.12 + 9.72i | 4.52 × 107 | 22.43 | 1.16 |
| Lung | 0.66 | 36.67 | 59.54 + 10.24i | 4.88 × 107 | 20.28 | 0.58 |
| Heart | 1.24 | 59.8 | 46.03 + 9.01i | 3.8 × 107 | 29.58 | - |
| Type of Tissue | Conductivity (S/m) | Relative Permittivity | Impedance (Ω) | Speed (m/s) | Attenuation (m−1) | Thickness (cm) |
|---|---|---|---|---|---|---|
| Air | 0 | 1 | 376.87 | 3 × 108 | 0 | 1 |
| Fat | 0.1 | 5.28 | 162.73 + 11.76i | 1.3 × 108 | 8.55 | 0.96 |
| Muscle | 1.74 | 52.73 | 50.81 + 6.06i | 4.1 × 107 | 44.8 | 1.35 |
| Cartilage | 1.76 | 38.77 | 58.20 + 9.42i | 4.75 × 107 | 52.44 | 1.16 |
| Lung | 1.24 | 34.43 | 62.62 + 8.16i | 5.07 × 107 | 39.59 | 0.58 |
| Heart | 2.26 | 54.81 | 49.27 + 7.28i | 4.01 × 107 | 56.79 | - |
| @ 915 MHz | |S11| (dB) | |S21| (dB) | |S12| (dB) | |S22| (dB) | Noise Figure (dB) |
|---|---|---|---|---|---|
| Without Cx | −8.47 | 23.15 | −36.73 | −6.77 | 1.84 |
| With Cx | −11.03 | 22.45 | −37.78 | −10.53 | 1.85 |
| Radar Module | Average Heart Rate (BPM) | Measurement Error (%) | |
|---|---|---|---|
| Radar | ECG | ||
| With LNA | 78 | 77.53 | 0.6 |
| Without LNA | 70 | 81.76 | 16.8 |
| Distance (cm) | Respiration | Heart Rate | ||||
|---|---|---|---|---|---|---|
| Radar (BPM) | Reference (BPM) | Error (%) | Radar (BPM) | Reference (BPM) | Error (%) | |
| 20 | 13.67 | 13.69 | −0.13 | 75.24 | 72.00 | 4.50 |
| 40 | 13.67 | 13.69 | −0.13 | 70.08 | 70.02 | 0.09 |
| 60 | 15.38 | 15.41 | −0.16 | 66.66 | 66.84 | −0.27 |
| 80 | 13.67 | 14.06 | −2.77 | 64.98 | 65.16 | −0.28 |
| 100 | 17.09 | 17.11 | −0.09 | 64.98 | 65.16 | −0.28 |
| 120 | 17.09 | 15.48 | 10.43 | 64.98 | 66.84 | −2.78 |
| 140 | N/A | 13.69 | N/A | N/A | 66.84 | N/A |
| Subject | Respiration | Heart Rate | ||||
|---|---|---|---|---|---|---|
| Radar (BPM) | Reference (BPM) | Error (%) | Radar (BPM) | Reference (BPM) | Error (%) | |
| A | 11.96 | 11.99 | −0.25 | 85.50 | 85.68 | −0.21 |
| B | 13.67 | 13.71 | −0.26 | 76.92 | 73.68 | 4.40 |
| C | 15.38 | 15.43 | −0.27 | 88.86 | 90.84 | −2.18 |
| D | 10.25 | 10.28 | −0.29 | 71.82 | 70.26 | 2.22 |
| E | 18.80 | 18.85 | −0.25 | 70.08 | 73.68 | −4.89 |
| F | 10.25 | 10.28 | −0.29 | 86.08 | 85.68 | 0.47 |
| Mean Error Rate | - | - | 0.27 | - | - | 2.39 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, J.-H.; Jeong, Y.-J.; Lee, G.-E.; Oh, J.-T.; Yang, J.-R. 915-MHz Continuous-Wave Doppler Radar Sensor for Detection of Vital Signs. Electronics 2019, 8, 561. https://doi.org/10.3390/electronics8050561
Park J-H, Jeong Y-J, Lee G-E, Oh J-T, Yang J-R. 915-MHz Continuous-Wave Doppler Radar Sensor for Detection of Vital Signs. Electronics. 2019; 8(5):561. https://doi.org/10.3390/electronics8050561
Chicago/Turabian StylePark, Jae-Hyun, Yeo-Jin Jeong, Ga-Eun Lee, Jun-Taek Oh, and Jong-Ryul Yang. 2019. "915-MHz Continuous-Wave Doppler Radar Sensor for Detection of Vital Signs" Electronics 8, no. 5: 561. https://doi.org/10.3390/electronics8050561
APA StylePark, J.-H., Jeong, Y.-J., Lee, G.-E., Oh, J.-T., & Yang, J.-R. (2019). 915-MHz Continuous-Wave Doppler Radar Sensor for Detection of Vital Signs. Electronics, 8(5), 561. https://doi.org/10.3390/electronics8050561






