Wearable Sensors to Characterize the Autonomic Nervous System Correlates of Food-Like Odors Perception: A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Signal Acquisition
- Baseline (3’): Basal measurement. Here, the volunteer was asked to sit comfortably on a chair and relax;
- Task (8’): The subject was presented with 12 odors for 10 s each, followed by an inter-stimulus lag of 30 s;
- Recovery (3’): Post-task rest measurement. The volunteer was asked to sit comfortably on a chair and relax, analogously to the Baseline.
2.3. Olfactory Stimulation
2.4. Questionnaires
- A smell self-rating questionnaire, related to the subjective perception of their own olfactory function ability, was administered prior to the registration. Here, the volunteer was asked to answer the question, “How good do you judge your sense of smell?” on a seven-item Likert-like scale ranging 1 (very poor) to 7 (very good), as already used in literature [40];
- At the same time, volunteers were asked to complete two questionnaires, one for assessing odor pleasantness and one investigating odor familiarity. The odor pleasantness questionnaire required the volunteer to answer the question, “How pleasant do you judge this odor?” on a nine-item Likert-like scale ranging from –4 (extremely unpleasant) to +4 (extremely pleasant) for each perceived odor [11]. On the other hand, odor familiarity was administered by asking the volunteer, “How familiar is this odor for you?” allowing them to answer on a seven-item Likert-like scale ranging 1 (completely unknown) to 7 (completely familiar), in a similar fashion to existing literature;
- After the completion of physiological recording and olfactory testing, two validated, well-grounded questionnaires were presented for the assessment of food and general neophobia. The first one was the Food Neophobia Scale (FNS), consisting of 10 questions (items), such as, “I am constantly sampling new and different foods”, or “I don’t trust new foods”, each producing a score ranging from 1 to 7 [21]. The second one, General Neophobia Scale (GNS), consisted of eight questions, each one similarly defined by scores ranging 1 to 7 [21]. Such questions were, for example: “I feel uncomfortable when I find myself in novel situations”, or “Whenever I’m away, I want to get home to my familiar surroundings”, therefore more related to general sensations of phobia and not devoted to feeding situations, which were specifically investigated by the FNS.
2.5. Signal Analysis
2.5.1. ECG
- -
- In the time domain:
- Heart rate (HR): the number of contractions of the heart occurring per time unit, expressed in bpm;
- Standard deviation of normal to normal RR intervals (SDNN): measure of heart rate variability (HRV), expressed in ms;
- Changes in successive normal sinus (NN) intervals exceeding 50 ms (pNN50), expressed as a percentage;
- -
- In the frequency domain:
- Normalized component of the power spectral density of the ECG signal at low frequency (0.04–0.15 Hz) (nLF);
- Normalized component of the power spectral density of the ECG spectrum at high frequency (0.15–0.4 Hz) (nHF);
- Low versus high Frequency components of the power spectral density of the ECG spectrum (LF/HF Ratio).
2.5.2. GSR
2.6. Statistical Analysis
3. Results
3.1. ECG
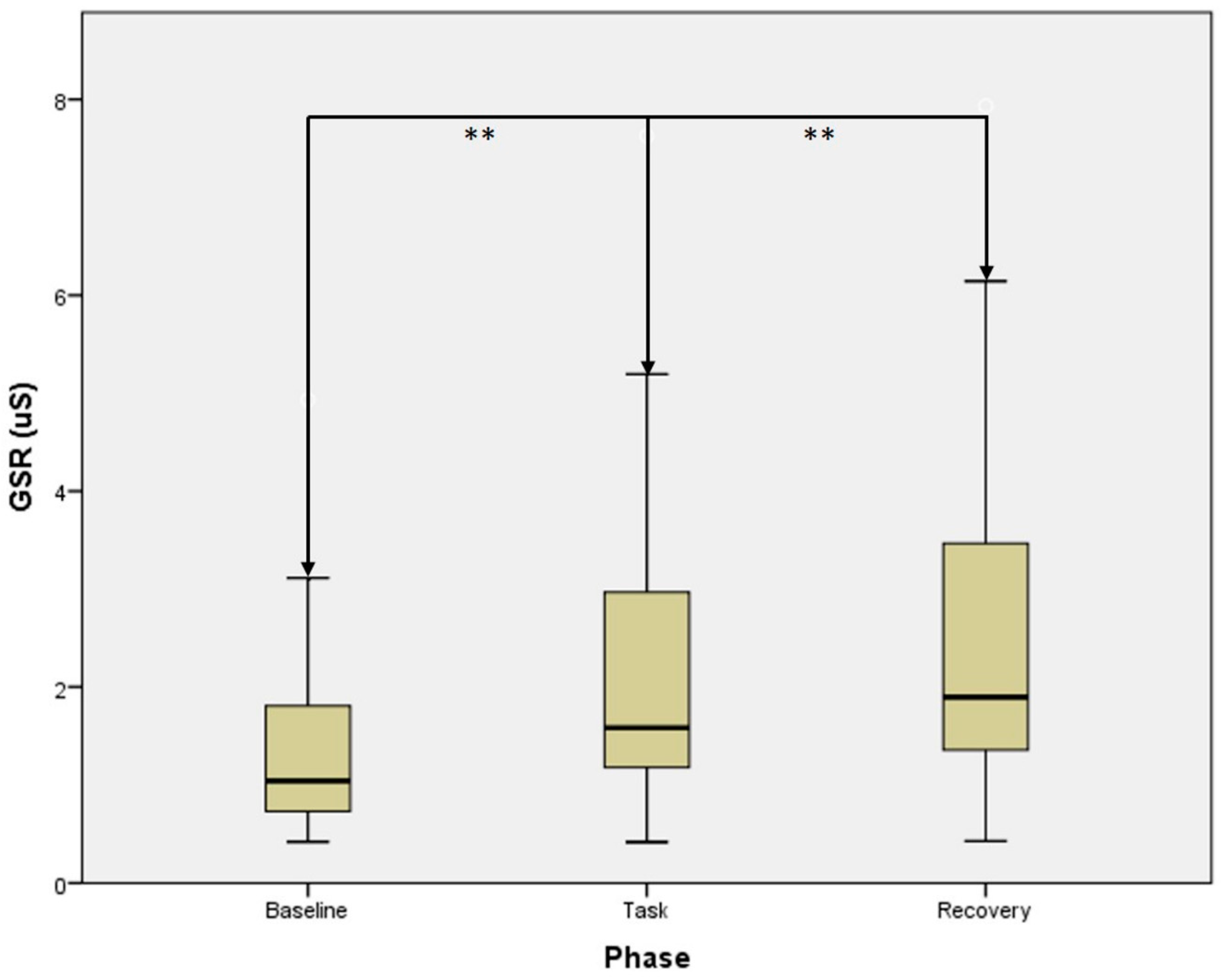
3.2. GSR
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Hoover, K.C. Smell with inspiration. The evolutionary significance of olfaction. Am. J. Phys. Anthropol. 2010, 53, 63–74. [Google Scholar] [CrossRef] [PubMed]
- Klajner, F.; Herman, C.P.; Polivy, J.; Chhabra, R. Human obesity, dieting, and anticipatory salivation to food. Physiol. Behav. 1981, 27, 195–198. [Google Scholar] [CrossRef]
- Legoff, D.B.; Spigelman, M.N. Salivary response to olfactory food stimuli as a function of dietary restraint and body-weight. Appetite 1987, 8, 29–35. [Google Scholar] [CrossRef]
- Rogers, P.J.; Hill, A.J. Breakdown of dietary restraint following mere exposure to food stimuli. Interrelationships between restraint, hunger, salivation, and food intake. Addict. Behav. 1989, 14, 387–397. [Google Scholar] [CrossRef]
- Bensafi, M.; Rouby, C.; Farget, V.; Bertrand, B.; Vigouroux, M.; Holley, A. Psychophysiological correlates of affects in human olfaction. Neurophysiol. Clin. 2002, 32, 326–332. [Google Scholar] [CrossRef]
- Jacquier, C.; Bonthoux, F.; Baciu, M.; Ruffieux, B. Improving the effectiveness of nutritional information policies. Assessment of unconscious pleasure mechanisms involved in food-choice decisions. Nutr. Rev. 2012, 70, 118–131. [Google Scholar] [CrossRef]
- Rodgers, R.F.; Paxton, S.J.; McLean, S.A.; Campbell, K.J.; Wertheim, E.H.; Skouteris, H.; Gibbons, K. Maternal negative affect is associated with emotional feeding practices and emotional eating in young children. Appetite 2014, 80, 242–247. [Google Scholar] [CrossRef]
- Stevenson, R.J.; Mahmut, M. Using response consistency to probe olfactory knowledge. Chem. Senses 2013, 38, 237–249. [Google Scholar] [CrossRef]
- Trellakis, S.; Tagay, S.; Fischer, C.; Rydleuskaya, A.; Scherag, A.; Bruderek, K.; Schlegl, S.; Greve, J.; Canbay, A.E.; Lang, S.; et al. Ghrelin, leptin and adiponectin as possible predictors of the hedonic value of odors. Regul. Pept. 2011, 167, 112–117. [Google Scholar] [CrossRef]
- Knaapila, A.; Tuorila, H.; Silventoinen, K.; Wright, M.J.; Kyvik, K.O.; Keskitalo, K.; Hansen, J.; Kaprio, J.; Perola, M. Environmental effects exceed genetic effects on perceived intensity and pleasantness of several odors: A three-population twin study. Behav. Genet. 2008, 38, 484–492. [Google Scholar] [CrossRef]
- Knaapila, A.; Laaksonen, O.; Virtanen, M.; Yang, B.; Lagström, H.; Sandell, M. Pleasantness, familiarity, and identification of spice odors are interrelated and enhanced by consumption of herbs and food neophilia. Appetite 2017, 109, 190–200. [Google Scholar] [CrossRef]
- Bensafi, M.; Pierson, A.; Rouby, C. Modulation of visual event-related potentials by emotional olfactory stimuli. Clin. Neurophysiol. 2002, 32, 335–342. [Google Scholar] [CrossRef]
- Masago, R.; Shimomura, Y.; Iwanaga, K.; Katsuura, T. The effects of hedonic properties of odors and attentional modulation on the olfactory eventrelated potentials. J. Physiol. Anthropol. Appl. Hum. Sci. 2001, 20, 7–13. [Google Scholar] [CrossRef]
- Anderson, A.K.; Christoff, K.; Stappen, I.; Panitz, D.; Ghahremani, D.G.; Glover, G.; Gabrieli, J.D.; Sobel, N. Dissociated neural representations of intensity and valence in human olfaction. Nat. Neurosci. 2003, 6, 196–202. [Google Scholar] [CrossRef]
- Grabenhorst, F.; Rolls, E.T.; Margot, C.; da Silva, M.A.; Velazco, M.I. How pleasant and unpleasant stimuli combine in different brain regions: Odor mixtures. J. Neurosci. 2007, 27, 13532–13540. [Google Scholar] [CrossRef]
- Delplanque, S.; Grandjean, D.; Chrea, C.; Aymard, L.; Cayeux, I.; Le Calve, B.; Velazco, M.I.; Scherer, K.R.; Sander, D. Emotional processing of odors: Evidence for a nonlinear relation between pleasantness and familiarity evaluations. Chem. Senses 2008, 33, 469–479. [Google Scholar] [CrossRef]
- Ferdenzi, C.; Roberts, S.C.; Schirmer, A.; Delplanque, S.; Cekic, S.; Porcherot, C.; Cayeux, I.; Sander, D.; Grandjean, D. Variability of affective responses to odors: Culture, gender, and olfactory knowledge. Chem. Senses 2013, 38, 175–186. [Google Scholar] [CrossRef]
- Schloss, K.B.; Goldberger, C.S.; Palmer, S.E.; Levitan, C.A. What’s that smell? An ecological approach to understanding preferences for familiar odors. Perception 2015, 44, 23–38. [Google Scholar] [CrossRef]
- Boesveldt, S.; Frasnelli, J.; Gordon, A.R.; Lundström, J.N. The fish is bad: Negative food odors elicit faster and more accurate reactions than other odors. Biol. Psychol. 2010, 84, 313–317. [Google Scholar] [CrossRef]
- Demattè, M.L.; Endrizzi, I.; Biasioli, F.; Corollaro, M.L.; Pojer, N.; Zampini, M.; Aprea, E.; Gasperi, F. Food neophobia and its relation with olfactory ability in common odour identification. Appetite 2013, 68, 112–117. [Google Scholar] [CrossRef]
- Pliner, P.; Hobden, K. Development of a scale to measure the trait of food neophobia in humans. Appetite 1992, 19, 105–120. [Google Scholar] [CrossRef]
- Wildes, J.E.; Zucker, N.L.; Marcus, M.D. Picky eating in adults: Results of a web-based survey. Int. J. Eat. Disord. 2012, 45, 575–582. [Google Scholar] [CrossRef]
- Frank, R.A.; van der Klaauw, N.J. The contribution of chemosensory factors to individual differences in reported food preferences. Appetite 1994, 22, 101–123. [Google Scholar] [CrossRef]
- Wansink, B. Environmental factors that increase the food intake and consumption volume of unknowing consumers. Annu. Rev. Nutr. 2004, 24, 455–479. [Google Scholar] [CrossRef] [PubMed]
- Greenwald, A. Supplemental material for understanding and using the implicit association test: III. Meta-analysis of predictive validity. J. Personal. Soc. Psychol. 2009, 97, 17–41. [Google Scholar] [CrossRef] [PubMed]
- Billman, G.E. Heart rate variability—A historical perspective. Front. Physiol. 2011, 2, 86. [Google Scholar] [CrossRef]
- Kuroda, K.; Inoue, N.; Ito, Y.; Kubota, K.; Sugimoto, A.; Kakuda, T.; Fushiki, T. Sedative effects of the jasmine tea odor and (R)-(−)-linalool, one of its major odor components, on autonomic nerve activity and mood states. Eur. J. Appl. Physiol. 2005, 95, 107–114. [Google Scholar] [CrossRef]
- Robin, O.; Alaoui-Ismaïli, O.; Dittmar, A.; Vernet-Maury, E. Emotional responses evoked by dental odors: An evaluation from autonomic parameters. J. Dent. Res. 1998, 77, 1638–1646. [Google Scholar] [CrossRef]
- Robin, O.; Alaoui-Ismaïli, O.; Dittmar, A.; Vernet-Maury, E. Basic emotions evoked by eugenol odor differ according to the dental experience. A neurovegetative analysis. Chem. Senses 1999, 24, 327–335. [Google Scholar] [CrossRef]
- Crawford, C. Marketing research and the new product failure rate. J. Market. 1977, 41, 55–61. [Google Scholar] [CrossRef]
- Riera, C.E.; Tsaousidou, E.; Halloran, J.; Follett, P.; Hahn, O.; Pereira, M.M.; Ruud, L.E.; Alber, J.; Tharp, K.; Anderson, C.M.; et al. The Sense of Smell Impacts Metabolic Health and Obesity. Cell Metab. 2017, 26, 198–211. [Google Scholar] [CrossRef] [PubMed]
- Bonfils, P.; Avan, P.; Faulcon, P.; Malinvaud, D. Distorted odorant perception: Analysis of a series of 56 patients with parosmia. Arch. Otolaryngol. Head Neck Surg. 2005, 131, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Bensafi, M.; Rouby, C.; Farget, V.; Bertrand, B.; Vigouroux, M.; Holley, A. Autonomic nervous system responses to odours: The role of pleasantness and arousal. Chem. Senses 2002, 27, 703–709. [Google Scholar] [CrossRef] [PubMed]
- Raudenbush, B.; Capiola, A. Physiological responses of food neophobics and food neophilics to food and non-food stimuli. Appetite 2012, 58, 1106–1108. [Google Scholar] [CrossRef] [PubMed]
- He, W.; Boesveldt, S.; de Graaf, C.; de Wijk, R.A. Dynamics of autonomic nervous system responses and facial expressions to odors. Front. Psychol. 2014, 5, 110. [Google Scholar] [CrossRef] [PubMed]
- He, W.; de Wijk, R.A.; de Graaf, C.; Boesveldt, S. Implicit and Explicit Measurements of Affective Responses to Food Odors. Chem. Senses 2016, 41, 661–668. [Google Scholar] [CrossRef]
- Tonacci, A.; Baldus, G.; Corda, D.; Piccaluga, E.; Andreassi, M.; Cremonesi, A.; Guagliumi, G.; Picano, E. Olfactory non-cancer effects of exposure to ionizing radiation in staff working in the cardiac catheterization laboratory. Int. J. Cardiol. 2014, 171, 461–463. [Google Scholar] [CrossRef]
- Tonacci, A.; Mrakic-Sposta, S.; Ujka, K.; Sansone, F.; Ferrisi, A.; Giardini, G.; Conte, R.; Pratali, L. Neurosensory and Cognitive Modifications in Europe’s Toughest RandoRaid Competition: The Transpyrénéa Extreme Study. Front. Physiol. 2017, 8, 201. [Google Scholar] [CrossRef]
- Lötsch, J.; Lange, C.; Hummel, T. A simple and reliable method for clinical assessment of odor thresholds. Chem. Senses 2004, 29, 311–317. [Google Scholar] [CrossRef]
- Knaapila, A.; Tuorila, H.; Kyvik, K.O.; Wright, M.J.; Keskitalo, K.; Hansen, J.; Kaprio, J.; Perola, M.; Silventoinen, K. Self-ratings of olfactory function reflect odor annoyance rather than olfactory acuity. Laryngoscope 2008, 118, 2212–2217. [Google Scholar] [CrossRef]
- Hummel, T.; Kobal, G.; Gudziol, H.; Mackay-Sim, A. Normative data for the “Sniffin’ Sticks” including tests of odor identification, odor discrimination, and olfactory thresholds: An upgrade based on a group of more than 3000 subjects. Eur. Arch. Otorhinolaryngol. 2007, 264, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Sorokowska, A.; Albrecht, E.; Haehner, A.; Hummel, T. Extended version of the “Sniffin’ Sticks” identification test: Test-retest reliability and validity. J. Neurosci. Methods 2015, 243, 111–114. [Google Scholar] [CrossRef] [PubMed]
- Pan, J.; Tompkins, W.J. A real-time QRS detection algorithm. IEEE Trans. Biomed. Eng. 1985, 32, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Billeci, L.; Tartarisco, G.; Brunori, E.; Crifaci, G.; Scardigli, S.; Balocchi, R.; Pioggia, G.; Maestro, S.; Morales, M.A. The role of wearable sensors and wireless technologies for the assessment of heart rate variability in anorexia nervosa. Eat. Weight Disord. 2015, 20, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Di Palma, S.; Tonacci, A.; Narzisi, A.; Domenici, C.; Pioggia, G.; Muratori, F.; Billeci, L.; MICHELANGELO Study Group. Monitoring of autonomic response to sociocognitive tasks during treatment in children with Autism Spectrum Disorders by wearable technologies: A feasibility study. Comput. Biol. Med. 2017, 85, 143–152. [Google Scholar] [CrossRef]
- Billeci, L.; Tonacci, A.; Narzisi, A.; Manigrasso, Z.; Varanini, M.; Fulceri, F.; Lattarulo, C.; Calderoni, S.; Muratori, F. Heart Rate Variability during a Joint Attention Task in Toddlers with Autism Spectrum Disorders. Front. Physiol. 2018, 9, 467. [Google Scholar] [CrossRef]
- Tonacci, A.; Billeci, L.; Sansone, F.; Masci, A.; Pala, A.P.; Domenici, C.; Conte, R. An Innovative, Unobtrusive Approach to Investigate Smartphone Interaction in Nonaddicted Subjects Based on Wearable Sensors: A Pilot Study. Medicina 2019, 55, 37. [Google Scholar] [CrossRef]
- Welch, P.D. The use of Fast Fourier Transform for the estimation of power spectra: A method based on time averaging over short, modified periodograms. IEEE Trans. Audio Electroacoust. 1967, 15, 70–73. [Google Scholar] [CrossRef]
- Benedek, M.; Kaernbach, C. A continuous measure of phasic electrodermal activity. J. Neurosci. Methods 2010, 190, 80–91. [Google Scholar] [CrossRef]
- Wieser, M.J.; Pauli, P.; Alpers, G.W.; Mühlberger, A. Is eye to eye contact really threatening and avoided in social anxiety?—An eye-tracking and psychophysiology study. J. Anxiety Disord. 2009, 23, 93–103. [Google Scholar] [CrossRef]
- Shapiro, S.S.; Wilk, M.B. An analysis of variance test for normality (complete samples). Biometrika 1965, 52, 591–611. [Google Scholar] [CrossRef]
- Tonacci, A.; Sansone, F.; Pala, A.P.; Centrone, A.; Napoli, F.; Domenici, C.; Conte, R. Effect of Feeding on Neurovegetative Response to Olfactory Stimuli. In Proceedings of the 2017 E-Health and Bioengineering Conference, EHB 2017, Sinaia, Romania, 21–24 June 2017; pp. 9–12. [Google Scholar]
- Shaffer, F.; Ginsberg, J.P. An Overview of Heart Rate Variability Metrics and Norms. Front. Public Health 2017, 5, 258. [Google Scholar] [CrossRef] [PubMed]
- Jung, D.J.; Cha, J.Y.; Kim, S.E.; Ko, I.G.; Jee, Y.S. Effects of Ylang-Ylang aroma on blood pressure and heart rate in healthy men. J. Exerc. Rehabil. 2013, 9, 250–255. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, T.; Kimura, T.; Hayashi, T. Aromatic effects of a Japanese citrus fruit-yuzu (Citrus junos Sieb. ex Tanaka)-on psychoemotional states and autonomic nervous system activity during the menstrual cycle: A single-blind randomized controlled crossover study. Biopsychosoc. Med. 2016, 10, 11. [Google Scholar] [CrossRef]
- Kolbeneva, M.G.; Alexandrov, Y.I. Mental Reactivation and Pleasantness Judgment of Experience Related to Vision, Hearing, Skin Sensations, Taste and Olfaction. PLoS ONE 2016, 11, e0159036. [Google Scholar] [CrossRef]
- Uryvaev, Y.V.; Golubeva, N.K.; Nechaev, A.M. Differences in human involuntary reactions to perceptible and imperceptible odors. Dokl. Akad. Nauk SSSR 1986, 290, 501–504. [Google Scholar]
- Sorokowska, A.; Schriever, V.A.; Gudziol, V.; Hummel, C.; Hähner, A.; Iannilli, E.; Sinding, C.; Aziz, M.; Seo, H.S.; Negoias, S.; et al. Changes of olfactory abilities in relation to age: Odor identification in more than 1400 people aged 4 to 80 years. Eur. Arch. Otorhinolaryngol. 2015, 272, 1937–1944. [Google Scholar] [CrossRef]
- Fjaeldstad, A.; Sundbøll, J.; Niklassen, A.; Ovesen, T. Odor Familiarity and Identification Abilities in Adolescents. Chem. Senses 2017, 42, 239–246. [Google Scholar] [CrossRef]
- Bahar-Fuchs, A.; Moss, S.; Rowe, C.; Savage, G. Awareness of olfactory deficits in healthy aging, amnestic mild cognitive impairment and Alzheimer’s disease. Int. Psychogeriatr. 2011, 23, 1097–1106. [Google Scholar] [CrossRef]
- Kawasaki, I.; Baba, T.; Takeda, A.; Mori, E. Loss of awareness of hyposmia is associated with mild cognitive impairment in Parkinson’s disease. Parkinsonism Relat. Disord. 2016, 22, 74–79. [Google Scholar] [CrossRef]
- White, T.L.; Sadikot, A.F.; Djordjevic, J. Metacognitive knowledge of olfactory dysfunction in Parkinson’s disease. Brain Cognit. 2016, 104, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Delplanque, S.; Coppin, G.; Bloesch, L.; Cayeux, I.; Sander, D. The mere exposure effect depends on an odor’s initial pleasantness. Front. Psychol. 2015, 6, 911. [Google Scholar] [CrossRef] [PubMed]
- Tonacci, A.; Billeci, L.; Tartarisco, G.; Ruta, L.; Muratori, F.; Pioggia, G.; Gangemi, S. Olfaction in autism spectrum disorders: A systematic review. Child Neuropsychol. 2017, 23, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Muratori, F.; Tonacci, A.; Billeci, L.; Catalucci, T.; Igliozzi, R.; Calderoni, S.; Narzisi, A. Olfactory processing in male children with autism: Atypical odor threshold and Identification. J. Autism Dev. Disord. 2017, 47, 3243–3251. [Google Scholar] [CrossRef]
- Tonacci, A.; Calderoni, S.; Billeci, L.; Maestro, S.; Fantozzi, P.; Ciuccoli, F.; Morales, M.A.; Narzisi, A.; Muratori, F. Autistic traits impact on olfactory processing in adolescent girls with Anorexia Nervosa restricting type. Psychiatry Res. 2019, 274, 20–26. [Google Scholar] [CrossRef]
- Okruszek, L.; Dolan, K.; Lawrence, M.; Cella, M. The beat of social cognition: Exploring the role of Heart Rate Variability as marker of mentalizing abilities. Soc. Neurosci. 2017, 12, 489–493. [Google Scholar] [CrossRef]
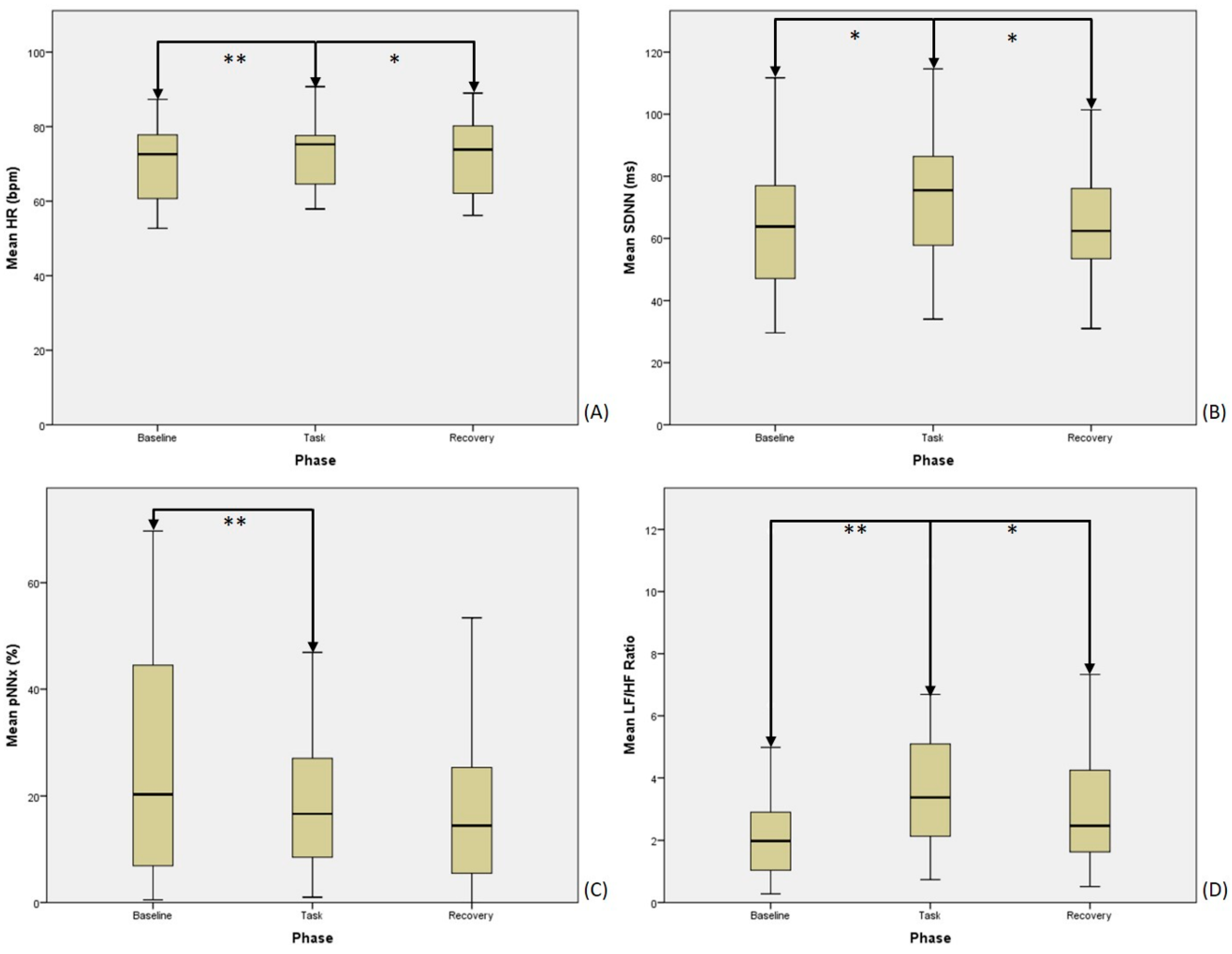
| Feature (Mean ± SD) | Baseline | Task | Recovery | p-Value |
|---|---|---|---|---|
| HR (bpm) | 70.1 ± 2.2 | 73.6 ± 2.0 | 72.0 ± 2.2 | <0.001 ** |
| SDNN (ms) | 62.6 ± 4.6 | 71.9 ± 4.4 | 64.3 ± 4.2 | 0.003 ** |
| pNNx (%) | 24.1 ± 4.7 | 17.4 ± 2.9 | 18.2 ± 3.6 | 0.002 ** |
| nLF (n.u.) | 0.64 ± 0.04 | 0.75 ± 0.03 | 0.70 ± 0.03 | 0.001 ** |
| nHF (n.u.) | 0.36 ± 0.04 | 0.25 ± 0.03 | 0.30 ± 0.03 | 0.001 ** |
| LF/HF (Ratio) | 2.76 ± 0.58 | 3.87 ± 0.50 | 3.18 ± 0.43 | 0.102 |
| Feature | Baseline versus Task | Task versus Recovery | ||
|---|---|---|---|---|
| Z | p-Value | Z | p-Value | |
| HR | −3.372 | 0.001 ** | 2.030 | 0.042 * |
| SDNN | −2.581 | 0.010 * | 2.451 | 0.014 * |
| pNNx | 2.711 | 0.007 ** | 0.191 | 0.848 |
| nLF | −3.180 | 0.001 ** | 2.273 | 0.023 * |
| nHF | 3.180 | 0.001 ** | -2.273 | 0.023 * |
| LF/HF Ratio | −2.659 | 0.008 ** | 2.094 | 0.036 * |
| Odor Nr. (Compound), CAS Nr. | GSR Response (µS, Mean ± SD) |
|---|---|
| 1 (Orange), 112-14-1 | 0.068 ± 0.112 |
| 2 (Banana), 132-92-2 | 0.000 ± 0.081 |
| 3 (Lemon), 203-376-6 | −0.009 ± 0.102 |
| 4 (Apple), 2173-56-0 | 0.016 ± 0.153 |
| 5 (Pineapple), 105-54-4 | 0.040 ± 0.110 |
| 6 (Pear), 3025-30-7 | 0.047 ± 0.186 |
| 7 (Grapefruit), 8016-20-4 | 0.053 ± 0.190 |
| 8 (Raspberry), 5471-51-2 | 0.005 ± 0.076 |
| 9 (Coconut), 104-61-0 | 0.061 ± 0.158 |
| 10 (Lavender), 8000-28-0 | 0.042 ± 0.128 |
| 11 (Melon), 111-79-5 | 0.025 ± 0.205 |
| 12 (Peach), 95962-14-4 | −0.007 ± 0.127 |
| OI | OP | OF | SSR | FNS | GNS | |
| HR | r = 0.304 p = 0.169 | r = −0.595* p = 0.004 | r = −0.369 p = 0.091 | r = −0.027 p = 0.904 | r = −0.145 p = 0.541 | r = 0.470 p = 0.037 |
| SDNN | r = 0.007 p = 0.974 | r = 0.188 p = 0.401 | r = −0.042 p = 0.853 | r = 0.056 p = 0.806 | r = 0.034 p = 0.887 | r = 0.060 p = 0.803 |
| pNNx | r = −0.184 p = 0.412 | r = 0.406 p = 0.061 | r = −0.018 p = 0.936 | r = 0.271 p = 0.223 | r = 0.072 p = 0.762 | r = 0.040 p = 0.867 |
| nLF | r = 0.024 p = 0.915 | r = −0.596* p = 0.003 | r = −0.307 p = 0.164 | r = −0.476 p = 0.025 | r = 0.247 p = 0.294 | r = 0.034 p = 0.886 |
| nHF | r = −0.024 p = 0.915 | r = 0.596* p = 0.003 | r = 0.307 p = 0.164 | r = 0.476 p = 0.025 | r = −0.247 p = 0.294 | r = −0.034 p = 0.886 |
| LF/HF | r = 0.030 p = 0.895 | r = −0.599* p = 0.003 | r = −0.302 p = 0.172 | r = −0.479 p = 0.024 | r = 0.243 p = 0.302 | r = 0.040 p = 0.867 |
| GSR | r = 0.276 p = 0.226 | r = −0.145 p = 0.530 | r = −0.119 p = 0.608 | r = −0.010 p = 0.966 | r = −0.157 p = 0.560 | r = 0.194 p = 0.471 |
| OI | OP | OF | SSR | FNS | GNS | |
| OI | - | r = −0.125 p = 0.579 | r = 0.431 p = 0.045 | r = 0.441 p = 0.040 | r = −0.464 p = 0.061 | r = 0.071 p = 0.788 |
| OP | r = −0.125 p = 0.579 | - | r = 0.442 p = 0.040 | r = 0.385 p = 0.077 | r = −0.331 p = 0.195 | r = 0.066 p = 0.803 |
| OF | r = 0.431 p = 0.045 | r = 0.442 p = 0.040 | - | r = 0.332 p = 0.131 | r = −0.400 p = 0.112 | r = −0.069 p = 0.794 |
| SSR | r = 0.441 p = 0.040 | r = 0.385 p = 0.077 | r = 0.332 p = 0.131 | - | r = −0.599 p = 0.011 | r = 0.178 p = 0.495 |
| FNS | r = −0.464 p = 0.061 | r = −0.331 p = 0.195 | r = −0.400 p = 0.112 | r = −0.599 p = 0.011 | - | r = −0.464 p = 0.061 |
| GNS | r = 0.071 p = 0.788 | r = 0.066 p = 0.803 | r = −0.069 p = 0.794 | r = 0.178 p = 0.495 | r = −0.464 p = 0.061 | - |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tonacci, A.; Di Monte, J.; Meucci, M.B.; Sansone, F.; Pala, A.P.; Billeci, L.; Conte, R. Wearable Sensors to Characterize the Autonomic Nervous System Correlates of Food-Like Odors Perception: A Pilot Study. Electronics 2019, 8, 1481. https://doi.org/10.3390/electronics8121481
Tonacci A, Di Monte J, Meucci MB, Sansone F, Pala AP, Billeci L, Conte R. Wearable Sensors to Characterize the Autonomic Nervous System Correlates of Food-Like Odors Perception: A Pilot Study. Electronics. 2019; 8(12):1481. https://doi.org/10.3390/electronics8121481
Chicago/Turabian StyleTonacci, Alessandro, Jessica Di Monte, Maria Beatrice Meucci, Francesco Sansone, Anna Paola Pala, Lucia Billeci, and Raffaele Conte. 2019. "Wearable Sensors to Characterize the Autonomic Nervous System Correlates of Food-Like Odors Perception: A Pilot Study" Electronics 8, no. 12: 1481. https://doi.org/10.3390/electronics8121481
APA StyleTonacci, A., Di Monte, J., Meucci, M. B., Sansone, F., Pala, A. P., Billeci, L., & Conte, R. (2019). Wearable Sensors to Characterize the Autonomic Nervous System Correlates of Food-Like Odors Perception: A Pilot Study. Electronics, 8(12), 1481. https://doi.org/10.3390/electronics8121481








