Application Status, Challenges, and Development Prospects of Smart Technologies in Home-Based Elder Care
Abstract
:1. Introduction
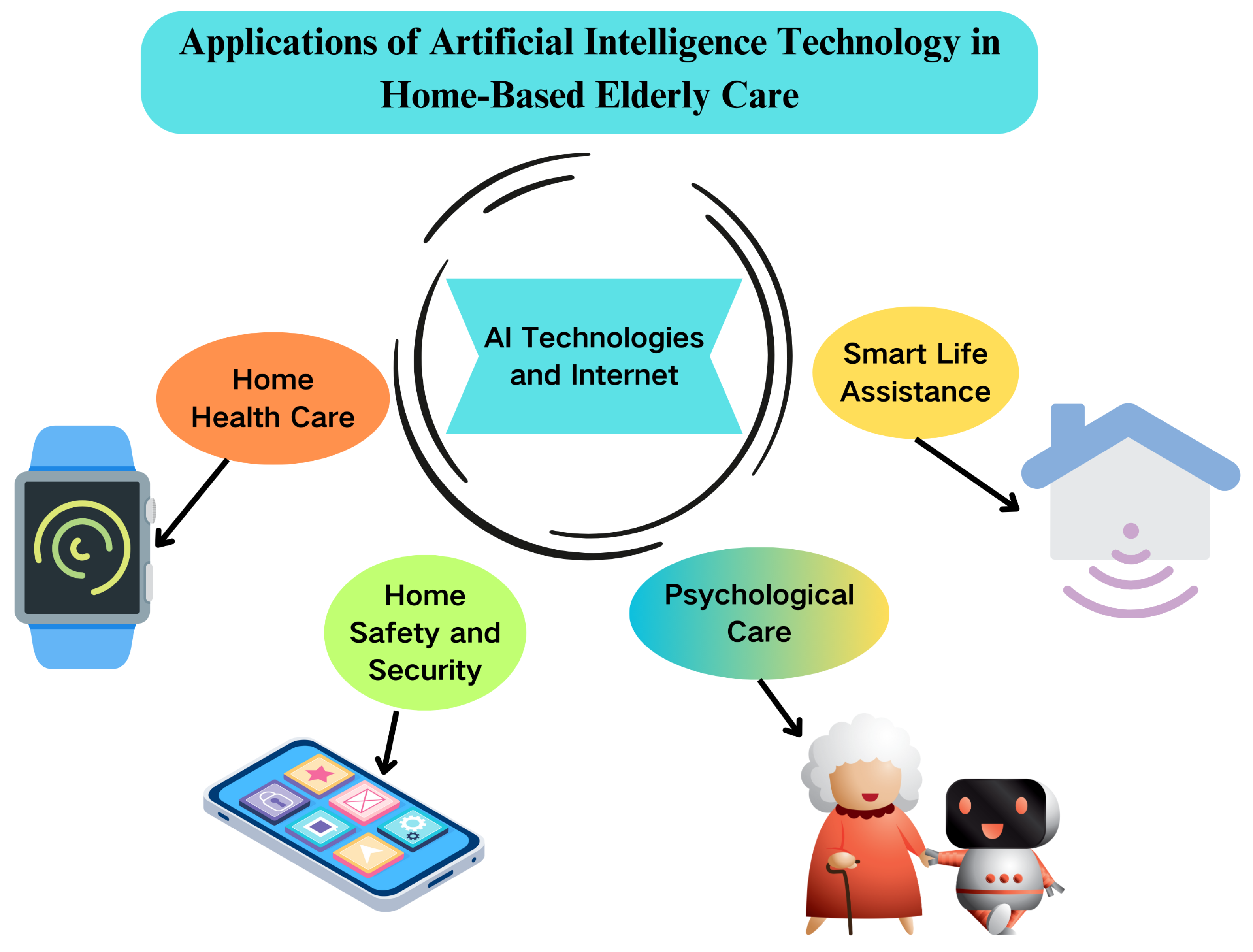
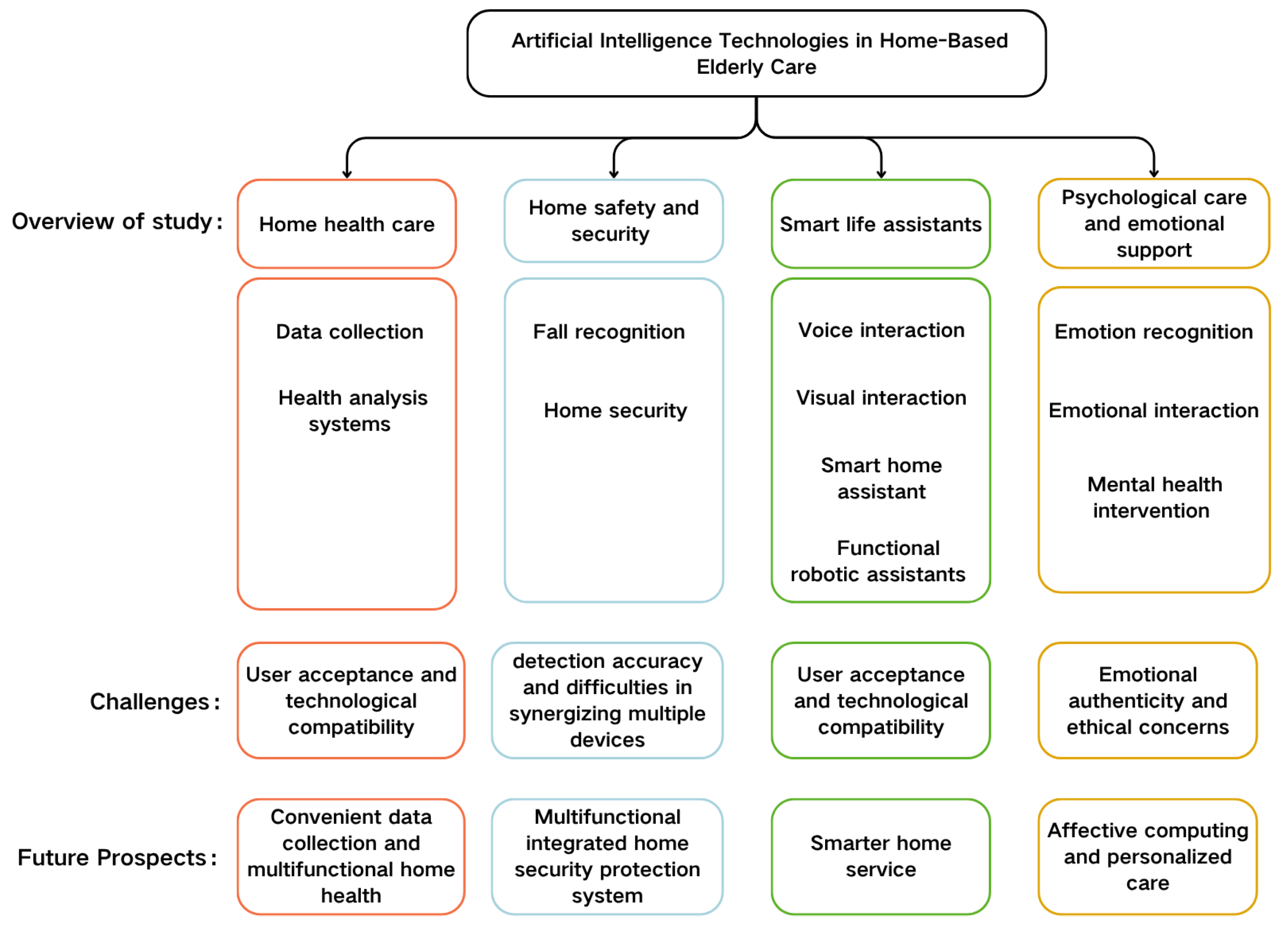
2. Overview of This Survey
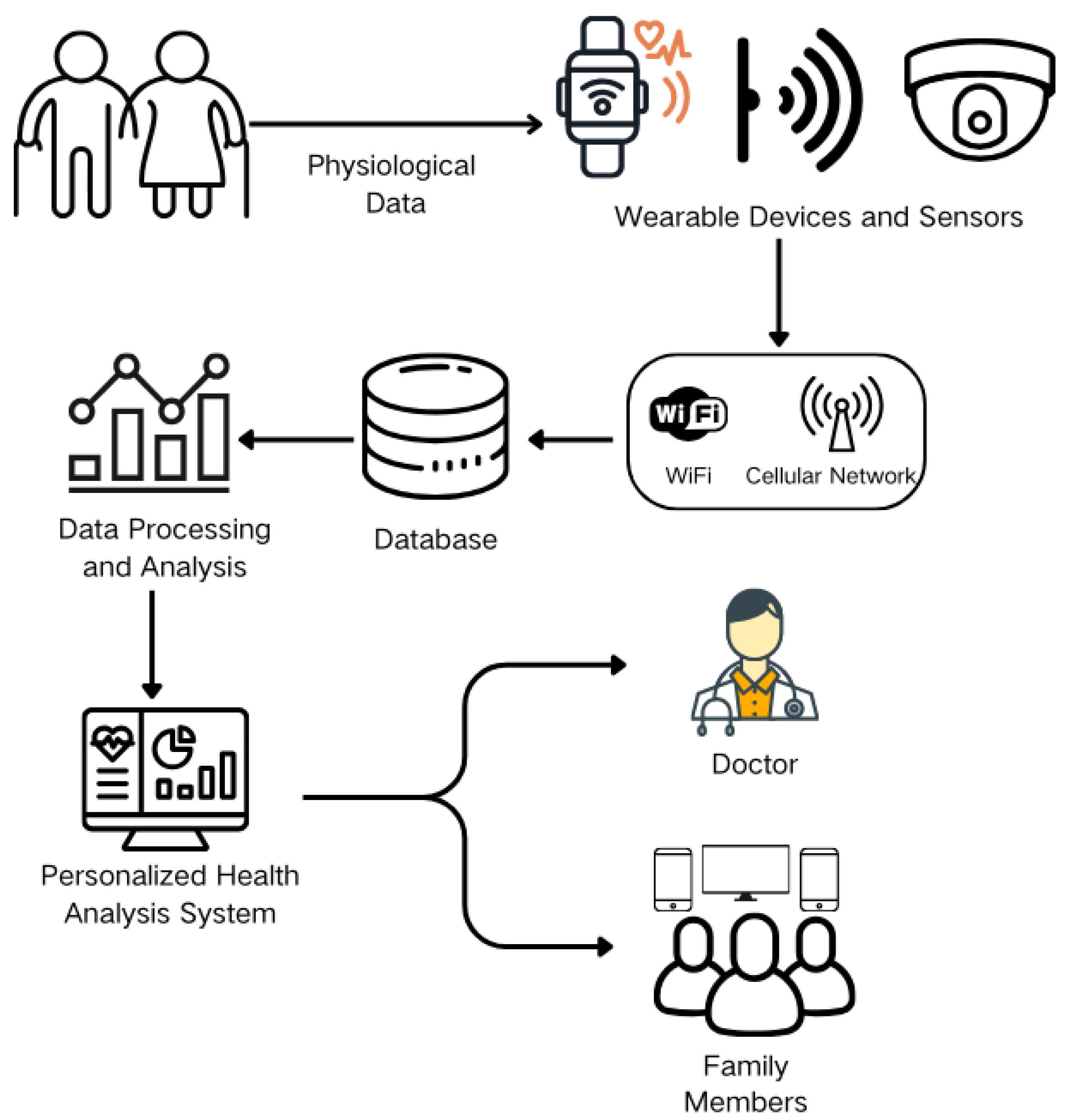
2.1. Home Health Care
2.1.1. Data Collection
2.1.2. Health Analysis Systems
2.1.3. Challenges: Data Reliability Issues and Performance of Health Analysis Systems
2.1.4. Future Prospects: Convenient Data Collection and Multifunctional Home Health
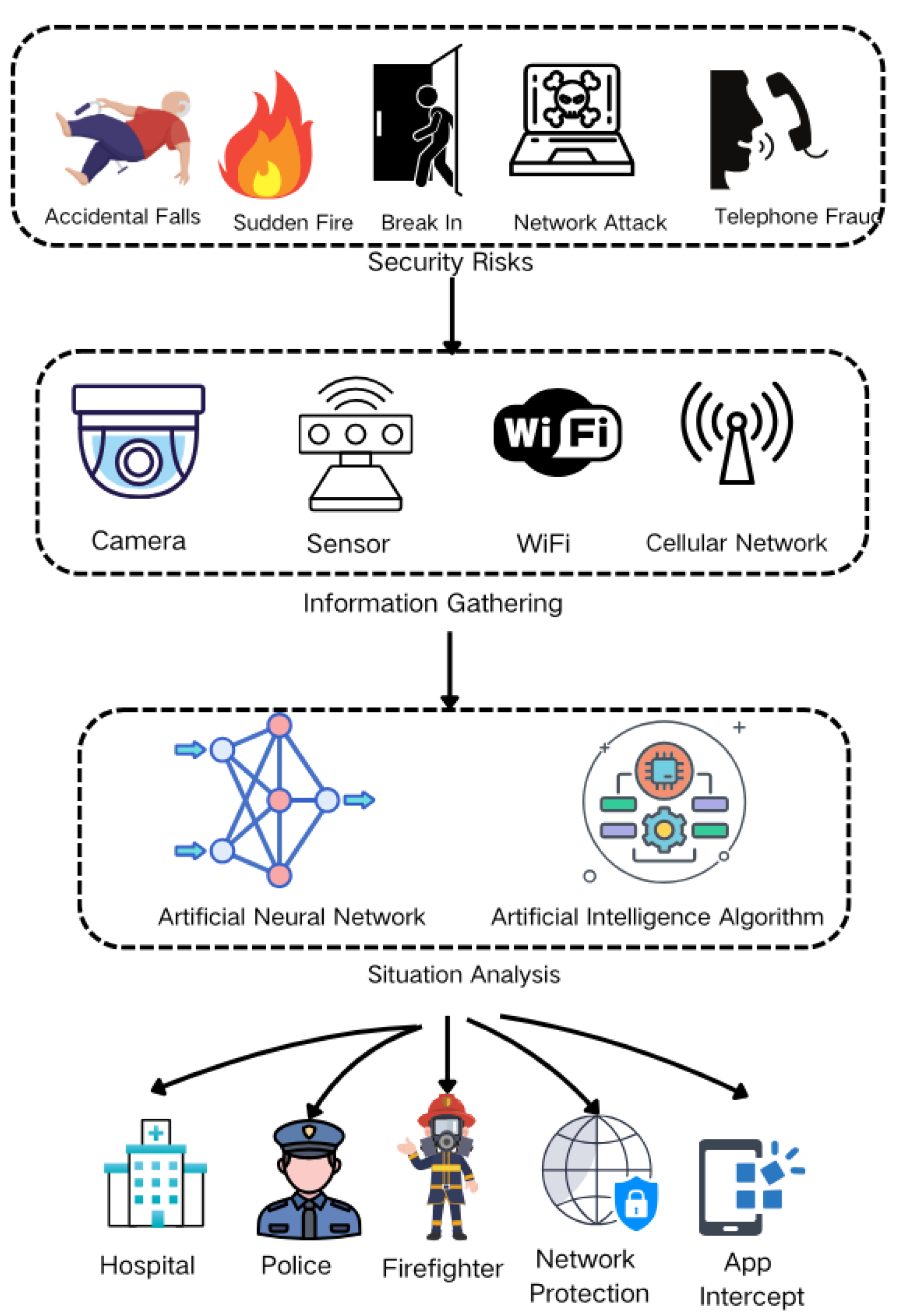
2.2. Home Safety and Security
2.2.1. Fall Recognition
2.2.2. Home Security
2.2.3. Challenges: Insufficient Detection Accuracy and Difficulties in Synergizing Multiple Devices
2.2.4. Future Prospects: Multifunctional Integrated Home Security Protection System
2.3. Smart Life Assistants
2.3.1. Voice Interaction
2.3.2. Visual Interaction
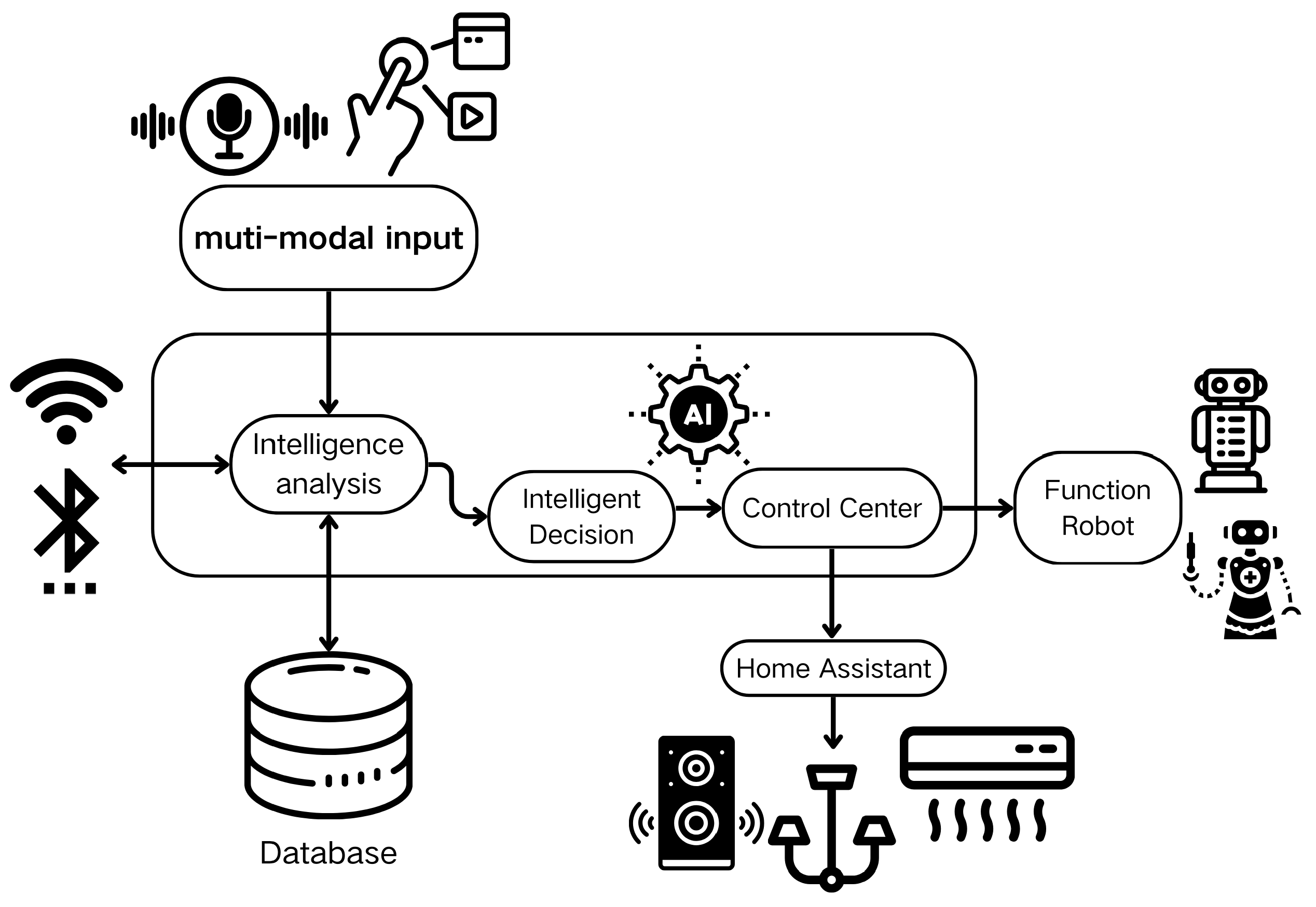
2.3.3. Smart Home Assistant
2.3.4. Functional Robotic Assistants
2.3.5. Challenges: User Acceptance and Technological Compatibility
2.3.6. Future Prospect: Smarter Home Service
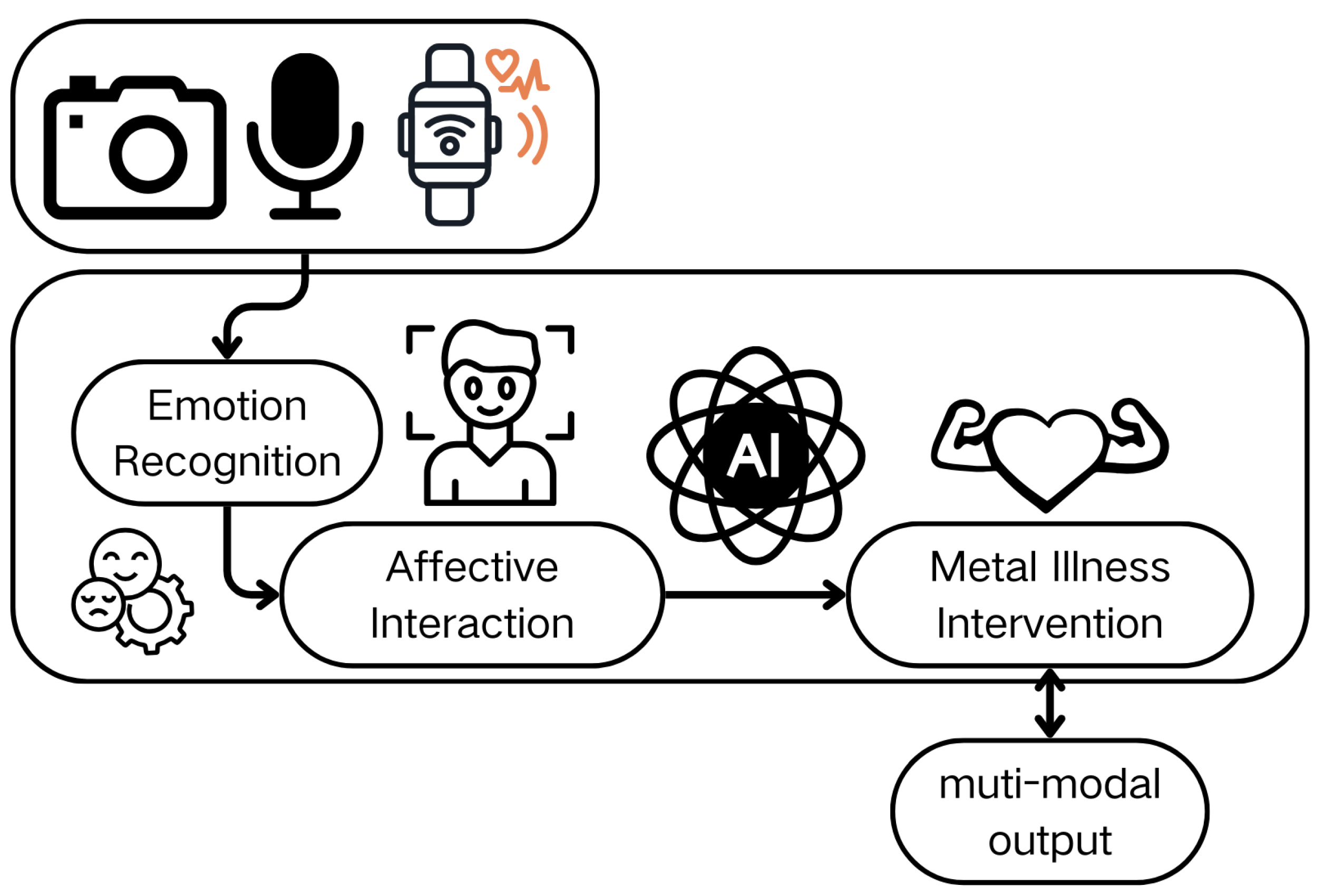
2.4. Psychological Care and Emotional Support
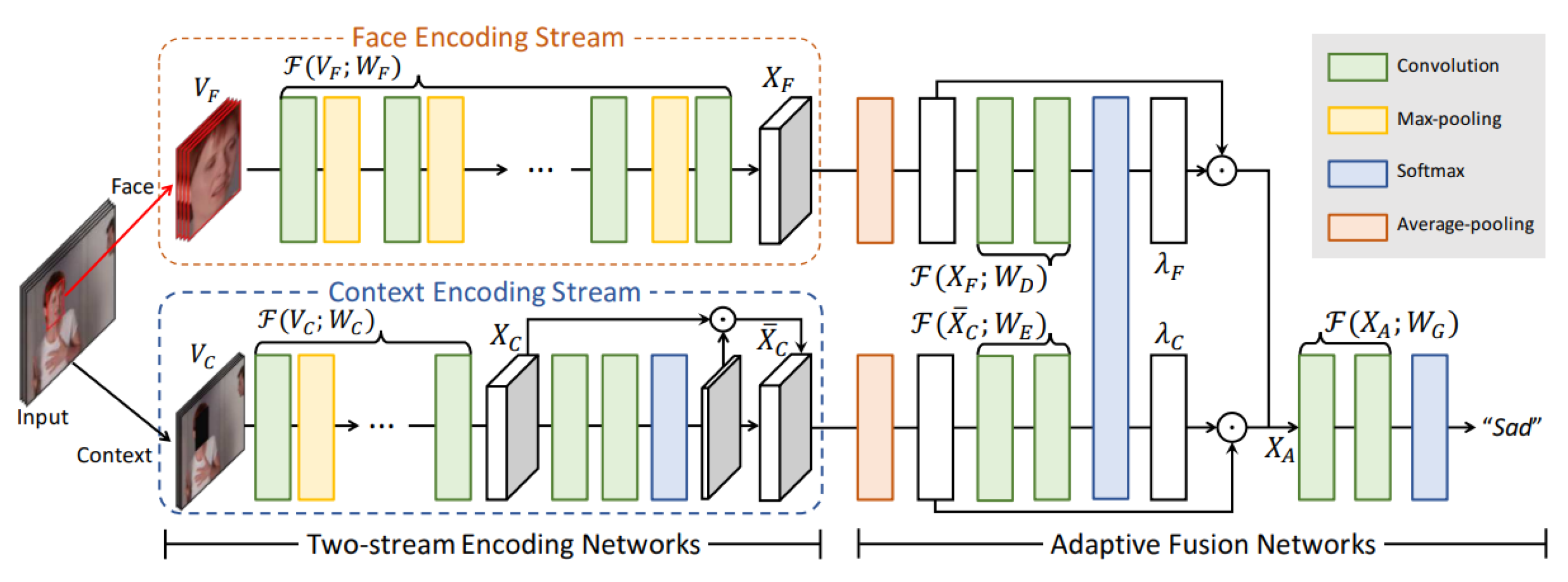
2.4.1. Emotion Recognition
2.4.2. Emotional Interaction
2.4.3. Mental Health Intervention
2.4.4. Challenges: Emotional Authenticity and Ethical Concerns
2.4.5. Future Prospect: Affective Computing and Personalized Care
3. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- National Bureau of Statistics of China. Statistical Bulletin on National Economic and Social Development of the People’s Republic of China in 2024; National Bureau of Statistics of China: Beijing, China, 2025. [Google Scholar]
- Xiao, F.; Huo, Z.; Li, D.; Zhou, B. Research on the spatial-temporal evolution and countermeasures of China’s population aging based on the “seven census” data. In Proceedings of the 2022 China Urban Planning Annual Conference (14 Regional Planning and Urban Economy), Wuhan, China, 25–27 February 2023; Guangzhou Urban Planning Survey and Design Institute: Guangzhou, China, 2023. [Google Scholar]
- Wiwatkunupakarn, N.; Pateekhum, C.; Aramrat, C.; Jirapornchaoren, W.; Pinyopornpanish, K.; Angkurawaranon, C. Social networking site usage: A systematic review of its relationship with social isolation, loneliness, and depression among older adults. Aging Ment. Health 2022, 26, 1318–1326. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, Y.; Nyawa, S.; Fosso Wamba, S. Combating loneliness with artificial intelligence: An AI-based emotional support model. In Proceedings of the 56th Hawaii International Conference on System Sciences, Kauai, HI, USA, 3–6 January 2023. [Google Scholar]
- Iqbal, S. Artificial Intelligence tools and applications for elderly healthcare-review. In Proceedings of the 2023 9th International Conference on Computing and Artificial Intelligence, Tianjin, China, 13–16 April 2023; pp. 394–397. [Google Scholar]
- Ma, B.; Yang, J.; Wong, F.K.Y.; Wong, A.K.C.; Ma, T.; Meng, J.; Zhao, Y.; Wang, Y.; Lu, Q. Artificial intelligence in elderly healthcare: A scoping review. Ageing Res. Rev. 2023, 83, 101808. [Google Scholar] [CrossRef]
- Stavropoulos, T.G.; Papastergiou, A.; Mpaltadoros, L.; Nikolopoulos, S.; Kompatsiaris, I. IoT wearable sensors and devices in elderly care: A literature review. Sensors 2020, 20, 2826. [Google Scholar] [CrossRef]
- Park, K.W.; Mirian, M.S.; McKeown, M.J. Artificial intelligence-based video monitoring of movement disorders in the elderly: A review on current and future landscapes. Singap. Med J. 2024, 65, 141–149. [Google Scholar] [CrossRef]
- Irfan, M.; Jawad, H.; Felix, B.B.; Abbasi, S.F.; Nawaz, A.; Akbarzadeh, S.; Awais, M.; Chen, L.; Westerlund, T.; Chen, W. Non-wearable IoT-based smart ambient behavior observation system. IEEE Sens. J. 2021, 21, 20857–20869. [Google Scholar] [CrossRef]
- Sundas, A.; Badotra, S.; Shahi, G.S.; Verma, A.; Bharany, S.; Ibrahim, A.O.; Abulfaraj, A.W.; Binzagr, F. Smart patient monitoring and recommendation (spmr) using cloud analytics and deep learning. IEEE Access 2024, 12, 54238–54255. [Google Scholar] [CrossRef]
- Vaiyapuri, T.; Lydia, E.L.; Sikkandar, M.Y.; Díaz, V.G.; Pustokhina, I.V.; Pustokhin, D.A. Internet of things and deep learning enabled elderly fall detection model for smart homecare. IEEE Access 2021, 9, 113879–113888. [Google Scholar] [CrossRef]
- Sarhan, Q.I. Arduino based smart home warning system. In Proceedings of the 2020 IEEE 6th International Conference on Control Science and Systems Engineering (ICCSSE), Beijing, China, 17–19 July 2020; pp. 201–206. [Google Scholar]
- Portet, F.; Vacher, M.; Golanski, C.; Roux, C.; Meillon, B. Design and evaluation of a smart home voice interface for the elderly: Acceptability and objection aspects. Pers. Ubiquitous Comput. 2013, 17, 127–144. [Google Scholar] [CrossRef]
- Madhusanka, B.; Ramadass, S.; Rajagopal, P.; Herath, H. Biofeedback method for human–computer interaction to improve elder caring: Eye-gaze tracking. In Predictive Modeling in Biomedical Data Mining and Analysis; Elsevier: Amsterdam, The Netherlands, 2022; pp. 137–156. [Google Scholar]
- Ashwini, G.; Rathnakara, S. A Novel Approach to Elderly Care Robotics Enhanced with Leveraging Gesture Recognition and Voice Assistance. In Proceedings of the 2024 Asia Pacific Conference on Innovation in Technology (APCIT), Bangalore, India, 15–17 March 2024; pp. 1–6. [Google Scholar]
- Noreen, I.; Siddiqui, U.; Akbar, A. AI-enabled elderly care robot. J. Inf. Commun. Technol. Robot. Appl. 2020, 11, 22–29. [Google Scholar] [CrossRef]
- Fadel, W.; Bouchentouf, T.; Buvet, P.A.; Ghrissi, M.; Bourja, O.; Guendoul, O. Deep Learning Approaches for Speech Emotion Recognition Using Cnns and Self-Supervised Models. Available online: https://ssrn.com/abstract=4936468 (accessed on 1 February 2025).
- Ma, W. IntelliJoyCare: A Realistic Interactive Audiovisual System for AI-based Elderly Care Companionship. In Proceedings of the 2024 10th International Conference on Humanities and Social Science Research (ICHSSR 2024), Xiamen, China, 24–26 April 2024; Atlantis Press: Amsterdam, Netherlands, 2024; pp. 852–860. [Google Scholar]
- Waycott, J.; Davidson, J.; Baker, F.; Yuan, S. Supporting creativity in aged care: Lessons from group singing, music therapy, and immersive virtual reality programs. In Proceedings of the 34th Australian Conference on Human-Computer Interaction, Melbourne, Australia, 29 November–2 December 2022; pp. 272–282. [Google Scholar]
- Chang, T.; Li, H.; Zhang, N.; Jiang, X.; Yu, X.; Yang, Q.; Jin, Z.; Meng, H.; Chang, L. Highly integrated watch for noninvasive continual glucose monitoring. Microsyst. Nanoeng. 2022, 8, 25. [Google Scholar] [CrossRef]
- Li, L.; Li, Y.; Yang, L.; Fang, F.; Yan, Z.; Sun, Q. Continuous and accurate blood pressure monitoring based on wearable optical fiber wristband. IEEE Sens. J. 2020, 21, 3049–3057. [Google Scholar] [CrossRef]
- Das, S.; Adhikary, A.; Laghari, A.A.; Mitra, S. Eldo-care: EEG with Kinect sensor based telehealthcare for the disabled and the elderly. Neurosci. Inform. 2023, 3, 100130. [Google Scholar] [CrossRef]
- Krizhevsky, A.; Sutskever, I.; Hinton, G.E. Imagenet classification with deep convolutional neural networks. Adv. Neural Inf. Process. Syst. 2012, 25. [Google Scholar] [CrossRef]
- Kim, J.Y.; Chu, C.H.; Kang, M.S. IoT-based unobtrusive sensing for sleep quality monitoring and assessment. IEEE Sens. J. 2020, 21, 3799–3809. [Google Scholar] [CrossRef]
- Salvade, C.; Tasso, V.; Carloni, F.; Santambrogio, M.D. Improving sleep quality through an arduino-based environment sleep monitoring system. In Proceedings of the IEEE EUROCON 2023—20th International Conference on Smart Technologies, Bologna, Italy, 6–8 July 2023; pp. 6–11. [Google Scholar]
- Dahou, A.; Al-qaness, M.A.; Abd Elaziz, M.; Helmi, A. Human activity recognition in IoHT applications using arithmetic optimization algorithm and deep learning. Measurement 2022, 199, 111445. [Google Scholar] [CrossRef]
- Abualigah, L.; Diabat, A.; Mirjalili, S.; Abd Elaziz, M.; Gandomi, A.H. The arithmetic optimization algorithm. Comput. Methods Appl. Mech. Eng. 2021, 376, 113609. [Google Scholar] [CrossRef]
- Cortes, C.; Vapnik, V. Support-vector networks. Mach. Learn. 1995, 20, 273–297. [Google Scholar] [CrossRef]
- Bibbo, L.; Carotenuto, R.; Della Cort, F.; Merenda, M.; Messina, G. Home care system for the elderly and pathological conditions. In Proceedings of the 2022 7th International Conference on Smart and Sustainable Technologies (SpliTech), Split, Croatia, 5–8 July 2022; pp. 1–7. [Google Scholar]
- Shanmugathashan, M.; Naveen, S.; Kamaleswaran, M.; Weerasinghe, D.M.; Chathurika, K.B.A.B. Air care—Machine learning approach to develop a supportive and monitoring system for an elder. Int. Res. J. Innov. Eng. Technol. 2022, 6, 5–11. [Google Scholar] [CrossRef]
- MacQueen, J. Some methods for classification and analysis of multivariate observations. In Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability, Volume 1: Statistics; University of California Press: Oakland, CA, USA, 1967; Volume 5, pp. 281–298. [Google Scholar]
- Lingmei, H.; Luping, D.; Yu, D.; Shuhua, N. Smart System for Elderly Care Based on Portable Sensor Positioning and Video Surveillance. In Proceedings of the 2024 Second International Conference on Inventive Computing and Informatics (ICICI), Coimbatore, India, 22–23 February 2024; pp. 330–335. [Google Scholar]
- Hochreiter, S.; Schmidhuber, J. Long short-term memory. Neural Comput. 1997, 9, 1735–1780. [Google Scholar] [CrossRef]
- Zhang, B.; Zhu, L.; Pei, Z.; Zhai, Q.; Zhu, J.; Zhong, X.; Yi, J.; Liu, T. A framework for remote interaction and management of home care elderly adults. IEEE Sens. J. 2022, 22, 11034–11044. [Google Scholar] [CrossRef]
- Yazici, A.; Zhumabekova, D.; Nurakhmetova, A.; Yergaliyev, Z.; Yatbaz, H.Y.; Makisheva, Z.; Lewis, M.; Ever, E. A smart e-health framework for monitoring the health of the elderly and disabled. Internet Things 2023, 24, 100971. [Google Scholar] [CrossRef]
- Breiman, L. Random forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef]
- Huang, X.; Palaoag, T.D. Implementation of Intelligent Elderly Care System Based on Cloud Platform and NNB Algorithm. In Proceedings of the 2024 IEEE 2nd International Conference on Control, Electronics and Computer Technology (ICCECT), Jilin, China, 26–28 April 2024; pp. 841–846. [Google Scholar]
- Freund, Y.; Schapire, R.E. A decision-theoretic generalization of on-line learning and an application to boosting. J. Comput. Syst. Sci. 1997, 55, 119–139. [Google Scholar] [CrossRef]
- Elman, J.L. Finding structure in time. Cogn. Sci. 1990, 14, 179–211. [Google Scholar] [CrossRef]
- Hassen, H.B.; Ayari, N.; Hamdi, B. A home hospitalization system based on the Internet of things, Fog computing and cloud computing. Inform. Med. Unlocked 2020, 20, 100368. [Google Scholar] [CrossRef] [PubMed]
- Iranpak, S.; Shahbahrami, A.; Shakeri, H. Remote patient monitoring and classifying using the internet of things platform combined with cloud computing. J. Big Data 2021, 8, 120. [Google Scholar] [CrossRef]
- Liyakathunisa; Alsaeedi, A.; Jabeen, S.; Kolivand, H. Ambient assisted living framework for elderly care using Internet of medical things, smart sensors, and GRU deep learning techniques. J. Ambient Intell. Smart Environ. 2022, 14, 5–23. [Google Scholar] [CrossRef]
- Cho, K.; Van Merriënboer, B.; Bahdanau, D.; Bengio, Y. On the properties of neural machine translation: Encoder-decoder approaches. arXiv 2014, arXiv:1409.1259. [Google Scholar]
- Wu, Q.; Chen, X.; Zhou, Z.; Zhang, J. Fedhome: Cloud-edge based personalized federated learning for in-home health monitoring. IEEE Trans. Mob. Comput. 2020, 21, 2818–2832. [Google Scholar] [CrossRef]
- Nahavandi, D.; Alizadehsani, R.; Khosravi, A.; Acharya, U.R. Application of artificial intelligence in wearable devices: Opportunities and challenges. Comput. Methods Programs Biomed. 2022, 213, 106541. [Google Scholar] [CrossRef]
- Krishnapriya, G.; Prema, S. Enhancing Elderly Care Through Telehealth Monitoring System Utilizing xDNN Model: A Review. In Proceedings of the 2024 International Conference on Signal Processing, Computation, Electronics, Power and Telecommunication (IConSCEPT), Karaikal, India, 4–5 July 2024; pp. 1–6. [Google Scholar]
- Teixeira, E.; Fonseca, H.; Diniz-Sousa, F.; Veras, L.; Boppre, G.; Oliveira, J.; Pinto, D.; Alves, A.J.; Barbosa, A.; Mendes, R.; et al. Wearable devices for physical activity and healthcare monitoring in elderly people: A critical review. Geriatrics 2021, 6, 38. [Google Scholar] [CrossRef] [PubMed]
- Iandola, F.N.; Han, S.; Moskewicz, M.W.; Ashraf, K.; Dally, W.J.; Keutzer, K. SqueezeNet: AlexNet-level accuracy with 50x fewer parameters and < 0.5 MB model size. arXiv 2016, arXiv:1602.07360. [Google Scholar]
- Bae, C.; Yeh, W.C.; Wahid, N.; Chung, Y.Y.; Liu, Y. A new simplified swarm optimization (SSO) using exchange local search scheme. Int. J. Innov. Comput. Inf. Control 2012, 8, 4391–4406. [Google Scholar]
- Villegas-Ch, W.; Barahona-Espinosa, S.; Gaibor-Naranjo, W.; Mera-Navarrete, A. Model for the detection of falls with the use of artificial intelligence as an assistant for the care of the elderly. Computation 2022, 10, 195. [Google Scholar] [CrossRef]
- Papan, V.; Maheswari, S. Intelligent Fall Detection and Alert System for the Elderly Using Yolov8 and Cloud-Based Analytics. In Proceedings of the 2024 5th International Conference on Electronics and Sustainable Communication Systems (ICESC), Coimbatore, India, 7–9 August 2024; pp. 580–588. [Google Scholar]
- Redmon, J.; Divvala, S.; Girshick, R.; Farhadi, A. You only look once: Unified, real-time object detection. In Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition, Las Vegas, NV, USA, 27–30 June 2016; pp. 779–788. [Google Scholar]
- Yao, C.B.; Lu, C.T. Dynamic Tracking and Real-Time Fall Detection Based on Intelligent Image Analysis with Convolutional Neural Network. Sensors 2024, 24, 7448. [Google Scholar] [CrossRef]
- Felzenszwalb, P.F.; Girshick, R.B.; McAllester, D.; Ramanan, D. Object detection with discriminatively trained part-based models. IEEE Trans. Pattern Anal. Mach. Intell. 2009, 32, 1627–1645. [Google Scholar] [CrossRef]
- Cao, Z.; Simon, T.; Wei, S.E.; Sheikh, Y. Realtime multi-person 2d pose estimation using part affinity fields. In Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition, Honolulu, HI, USA, 21–26 July 2017; pp. 7291–7299. [Google Scholar]
- Taiwo, O.; Ezugwu, A.E.; Oyelade, O.N.; Almutairi, M.S. Enhanced intelligent smart home control and security system based on deep learning model. Wirel. Commun. Mob. Comput. 2022, 2022, 9307961. [Google Scholar] [CrossRef]
- Akhmetzhanov, B.; Akhmetzhanov, B.; ÖZDEMİR, S.; Zhakiyev, N. Advancing affordable IoT solutions in smart homes to enhance independence and autonomy of the elderly. J. Infrastruct. Policy Dev. 2024, 8, 2899. [Google Scholar] [CrossRef]
- Malhotra, S.; Arora, G.; Bathla, R. Detection and analysis of fraud phone calls using artificial intelligence. In Proceedings of the 2023 International Conference on Recent Advances in Electrical, Electronics & Digital Healthcare Technologies (REEDCON), New Delhi, India, 27–28 May 2023; pp. 592–595. [Google Scholar]
- Elahi, H.; Castiglione, A.; Wang, G.; Geman, O. A human-centered artificial intelligence approach for privacy protection of elderly App users in smart cities. Neurocomputing 2021, 444, 189–202. [Google Scholar] [CrossRef]
- Bhatia, M. An AI-enabled secure framework for enhanced elder healthcare. Eng. Appl. Artif. Intell. 2024, 131, 107831. [Google Scholar] [CrossRef]
- Grieves, M.W. Product lifecycle management: The new paradigm for enterprises. Int. J. Prod. Dev. 2005, 2, 71–84. [Google Scholar] [CrossRef]
- Liu, W.; Lin, Y.; Qi, Z.; Wu, Z.; Zhang, G.; Wang, K.; Fan, S.; Yang, Z. LoginSoEasy: A System Enabling both Authentication and Protection of Personal Information based on Trusted User Agent. In Proceedings of the 2021 IEEE Sixth International Conference on Data Science in Cyberspace (DSC), Guangzhou, China, 9–11 October 2021; pp. 122–129. [Google Scholar]
- Yu, R.; Zhang, X.; Zhang, M. Smart home security analysis system based on the internet of things. In Proceedings of the 2021 IEEE 2nd International Conference on Big Data, Artificial Intelligence and Internet of Things Engineering (ICBAIE), Nanchang, China, 26–28 March 2021; pp. 596–599. [Google Scholar]
- Xue, J.; Shen, B. A novel swarm intelligence optimization approach: Sparrow search algorithm. Syst. Sci. Control Eng. 2020, 8, 22–34. [Google Scholar] [CrossRef]
- Chen, Y.; Liu, J.; Peng, L.; Wu, Y.; Xu, Y.; Zhang, Z. Auto-encoding variational bayes. Camb. Explor. Arts Sci. 2024, 2, 1–8. [Google Scholar] [CrossRef]
- Gharghan, S.K.; Hashim, H.A. A comprehensive review of elderly fall detection using wireless communication and artificial intelligence techniques. Measurement 2024, 226, 114186. [Google Scholar] [CrossRef]
- Verma, G.; Pachauri, S.; Kumar, A.; Patel, D.; Kumar, A.; Pandey, A. Smart home automation with smart security system over the cloud. In Proceedings of the 2023 14th International Conference on Computing Communication and Networking Technologies (ICCCNT), Delhi, India, 6–8 July 2023; pp. 1–7. [Google Scholar]
- Touqeer, H.; Zaman, S.; Amin, R.; Hussain, M.; Al-Turjman, F.; Bilal, M. Smart home security: Challenges, issues and solutions at different IoT layers. J. Supercomput. 2021, 77, 14053–14089. [Google Scholar] [CrossRef]
- Pradhan, A.; Lazar, A.; Findlater, L. Use of intelligent voice assistants by older adults with low technology use. ACM Trans. Comput.-Hum. Interact. (TOCHI) 2020, 27, 1–27. [Google Scholar] [CrossRef]
- Pujol, P.; Pol, S.; Nadeu, C.; Hagen, A.; Bourlard, H. Comparison and combination of features in a hybrid HMM/MLP and a HMM/GMM speech recognition system. IEEE Trans. Speech Audio Process. 2004, 13, 14–22. [Google Scholar] [CrossRef]
- Islam, M.U.; Chaudhry, B.M. A framework to enhance user experience of older adults with speech-based intelligent personal assistants. IEEE Access 2022, 11, 16683–16699. [Google Scholar] [CrossRef]
- Bures, V. Interactive digital television and voice interaction: Experimental evaluation and subjective perception by elderly. Elektron. Elektrotechnika 2012, 122, 87–90. [Google Scholar] [CrossRef]
- Gu, J.; Wang, X.; Yao, X.; Hu, A. Understanding the influence of AI voice technology on visually impaired elders’ psychological well-being: An affordance perspective. In Proceedings of the Human Aspects of IT for the Aged Population. Technology and Society: 6th International Conference, ITAP 2020, Held as Part of the 22nd HCI International Conference, HCII 2020, Copenhagen, Denmark, 19–24 July 2020; Proceedings, Part III 22. Springer: Berlin/Heidelberg, Germany, 2020; pp. 226–240. [Google Scholar]
- Mnih, V.; Kavukcuoglu, K.; Silver, D.; Graves, A.; Antonoglou, I.; Wierstra, D.; Riedmiller, M. Playing atari with deep reinforcement learning. arXiv 2013, arXiv:1312.5602. [Google Scholar]
- Minzhi, J. Evaluating the Voice Interface of Conversational Speech Systems in Human-Robot Interaction for Elderly People. Ph.D. Thesis, Seoul National University Graduate School, Seoul, Republic of Korea, 2018. [Google Scholar]
- O’Brien, K.; Liggett, A.; Ramirez-Zohfeld, V.; Sunkara, P.; Lindquist, L.A. Voice-controlled intelligent personal assistants to support aging in place. J. Am. Geriatr. Soc. 2020, 68, 176–179. [Google Scholar] [CrossRef] [PubMed]
- Sooraj, S.; Sundaravel, E.; Shreesh, B.; Sireesha, K. IoT smart home assistant for physically challenged and elderly people. In Proceedings of the 2020 International Conference on Smart Electronics and Communication (ICOSEC), Trichy, India, 10–12 September 2020; pp. 809–814. [Google Scholar]
- Ganesh, D.; Seshadri, G.; Sokkanarayanan, S.; Rajan, S.; Sathiyanarayanan, M. Iot-based google duplex artificial intelligence solution for elderly care. In Proceedings of the 2019 International Conference on contemporary Computing and Informatics (IC3I), Bangalore, India, 12–14 December 2019; pp. 234–240. [Google Scholar]
- Yang, G.Z.; Yang, G. Body Sensor Networks; Springer: Berlin/Heidelberg, Germany, 2006; Volume 1. [Google Scholar]
- He, K.; Zhang, X.; Ren, S.; Sun, J. Deep residual learning for image recognition. In Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition, Las Vegas, NV, USA, 27–30 June 2016; pp. 770–778. [Google Scholar]
- Vercelli, A.; Rainero, I.; Ciferri, L.; Boido, M.; Pirri, F. Robots in elderly care. Digit.-Sci. J. Digit. Cult. 2018, 2, 37–50. [Google Scholar]
- Padhan, S.; Mohapatra, A.; Ramasamy, S.K.; Agrawal, S.; Ramasamy, S. Artificial intelligence (AI) and robotics in elderly healthcare: Enabling independence and quality of life. Cureus 2023, 15, e42905. [Google Scholar] [CrossRef]
- Hermann, J.; Oktay, S.; Lisetschko, A.; Dogangün, A. A Systematic Literature Review on the Use of Social Robots in Elderly Care. In Proceedings of the 35th Australian Computer-Human Interaction Conference, Wellington, New Zealand, 2–6 December 2023; pp. 221–230. [Google Scholar]
- Cantone, A.A.; Esposito, M.; Perillo, F.P.; Romano, M.; Sebillo, M.; Vitiello, G. Enhancing elderly health monitoring: Achieving autonomous and secure living through the integration of artificial intelligence, autonomous robots, and sensors. Electronics 2023, 12, 3918. [Google Scholar] [CrossRef]
- Gardner-Thorpe, J.; Love, N.; Wrightson, J.; Walsh, S.; Keeling, N. The value of Modified Early Warning Score (MEWS) in surgical in-patients: A prospective observational study. Ann. R. Coll. Surg. Engl. 2006, 88, 571–575. [Google Scholar] [CrossRef]
- Ribeiro, T.; Gonçalves, F.; Garcia, I.S.; Lopes, G.; Ribeiro, A.F. CHARMIE: A collaborative healthcare and home service and assistant robot for elderly care. Appl. Sci. 2021, 11, 7248. [Google Scholar] [CrossRef]
- Zhou, H.; Chou, W.; Tuo, W.; Rong, Y.; Xu, S. Mobile manipulation integrating enhanced AMCL high-precision location and dynamic tracking grasp. Sensors 2020, 20, 6697. [Google Scholar] [CrossRef]
- Deng, J.; Dong, W.; Socher, R.; Li, L.J.; Li, K.; Fei-Fei, L. Imagenet: A large-scale hierarchical image database. In Proceedings of the 2009 IEEE Conference on Computer Vision and Pattern Recognition, Miami, FL, USA, 20–25 June 2009; pp. 248–255. [Google Scholar]
- Mišeikis, J.; Caroni, P.; Duchamp, P.; Gasser, A.; Marko, R.; Mišeikienė, N.; Zwilling, F.; De Castelbajac, C.; Eicher, L.; Früh, M.; et al. Lio-a personal robot assistant for human-robot interaction and care applications. IEEE Robot. Autom. Lett. 2020, 5, 5339–5346. [Google Scholar] [CrossRef]
- Qin, C.; Song, A.; Wei, L.; Zhao, Y. A multimodal domestic service robot interaction system for people with declined abilities to express themselves. Intell. Serv. Robot. 2023, 16, 373–392. [Google Scholar] [CrossRef]
- Zhou, L.; Li, J.; Mo, Y.; Zhang, X.; Zhang, Y.; Wei, S. AoECR: AI-ization of Elderly Care Robot. arXiv 2025, arXiv:2502.19706. [Google Scholar]
- Du, Z.; Qian, Y.; Liu, X.; Ding, M.; Qiu, J.; Yang, Z.; Tang, J. Glm: General language model pretraining with autoregressive blank infilling. arXiv 2021, arXiv:2103.10360. [Google Scholar]
- Hu, E.J.; Shen, Y.; Wallis, P.; Allen-Zhu, Z.; Li, Y.; Wang, S.; Wang, L.; Chen, W. Lora: Low-rank adaptation of large language models. ICLR 2022, 1, 3. [Google Scholar]
- Barber, R.; Ortiz, F.J.; Garrido, S.; Calatrava-Nicolás, F.M.; Mora, A.; Prados, A.; Vera-Repullo, J.A.; Roca-González, J.; Méndez, I.; Mozos, Ó.M. A multirobot system in an assisted home environment to support the elderly in their daily lives. Sensors 2022, 22, 7983. [Google Scholar] [CrossRef] [PubMed]
- Yazdani-Darki, M.; Rahemi, Z.; Adib-Hajbaghery, M.; Izadi-Avanji, F.S. Older adults’ barriers to use technology in daily life: A qualitative study. Nurs. Midwifery Stud. 2020, 9, 229–236. [Google Scholar]
- Abeywickrama, T.; Cheema, M.A.; Taniar, D. K-nearest neighbors on road networks: A journey in experimentation and in-memory implementation. arXiv 2016, arXiv:1601.01549. [Google Scholar] [CrossRef]
- Khare, S.K.; Blanes-Vidal, V.; Nadimi, E.S.; Acharya, U.R. Emotion recognition and artificial intelligence: A systematic review (2014–2023) and research recommendations. Inf. Fusion 2024, 102, 102019. [Google Scholar] [CrossRef]
- Hsu, W.N.; Bolte, B.; Tsai, Y.H.H.; Lakhotia, K.; Salakhutdinov, R.; Mohamed, A. Hubert: Self-supervised speech representation learning by masked prediction of hidden units. IEEE/ACM Trans. Audio Speech Lang. Process. 2021, 29, 3451–3460. [Google Scholar] [CrossRef]
- Gaya-Morey, F.X.; Buades-Rubio, J.M.; Palanque, P.; Lacuesta, R.; Manresa-Yee, C. Deep Learning-Based Facial Expression Recognition for the Elderly: A Systematic Review. arXiv 2025, arXiv:2502.02618. [Google Scholar]
- Gupta, A.; Sawhney, S.; Ahmed, S. CareTaker. ai—A Smart Health-Monitoring and Caretaker-Assistant System for Elder Healthcare. Eng. Proc. 2025, 78, 7. [Google Scholar]
- Dalvi, C.; Rathod, M.; Patil, S.; Gite, S.; Kotecha, K. A survey of ai-based facial emotion recognition: Features, ml & dl techniques, age-wise datasets and future directions. Ieee Access 2021, 9, 165806–165840. [Google Scholar]
- Yamazaki, Y.; Ishii, M.; Ito, T.; Hashimoto, T. Frailty care robot for elderly and its application for physical and psychological support. J. Adv. Comput. Intell. Intell. Informatics 2021, 25, 944–952. [Google Scholar] [CrossRef]
- Kiran, A.; Balaram, A.; Parshapu, P.; Naik, S.L.; Purushotham, P.; Silparaj, M. AI-Enhanced Elderly Care Companion. In Proceedings of the 2024 International Conference on Science Technology Engineering and Management (ICSTEM), Singapore, 15–16 March 2024; pp. 1–5. [Google Scholar]
- Chen, T.; Guestrin, C. Xgboost: A scalable tree boosting system. In Proceedings of the 22nd Acm Sigkdd International Conference on Knowledge Discovery and Data Mining, San Francisco, CA, USA, 13–17 August 2016; pp. 785–794. [Google Scholar]
- Lee, J.; Kim, S.; Kim, S.; Park, J.; Sohn, K. Context-aware emotion recognition networks. In Proceedings of the IEEE/CVF International Conference on Computer Vision, Seoul, Republic of Korea, 27 October–2 November 2019; pp. 10143–10152. [Google Scholar]
- Rodríguez-Martínez, A.; Amezcua-Aguilar, T.; Cortés-Moreno, J.; Jiménez-Delgado, J.J. Qualitative analysis of conversational chatbots to alleviate loneliness in older adults as a strategy for emotional health. Healthcare 2023, 12, 62. [Google Scholar] [CrossRef] [PubMed]

| Applications | Representative Publications | Main Content |
|---|---|---|
| Home health care | Non-Wearable IoT-Based Smart Ambient Behavior Observation System [9] | A non-wearable intelligent environmental behavior observation system based on the IOT, which achieves seamless monitoring of daily activities of the elderly through environmental and behavior sensors. |
| Smart patient monitoring and recommendation using cloud analytics and deep learning [10] | A chronic disease health monitoring framework that can be deployed in the cloud and on premises. | |
| Home safety and security | Internet of things and deep learning enabled elderly fall detection model for smart homecare [11] | A fall detection model for elderly people based on the Internet of Things and deep learning. |
| Arduino Based Smart Home Warning System [12] | A smart home warning system based on Arduino, capable of detecting abnormal situations such as fires, gas leaks, and intrusions, and sending notifications. | |
| Smart life assistants | Design and evaluation of a smart home voice interface for the elderly: acceptability and objection aspects [13] | Through user evaluation, it has been found that voice technology has great potential in improving the security and comfort of smart homes, but there may be certain privacy issues. |
| Biofeedback method for human–computer interaction to improve elder caring: Eye-gaze tracking [14] | A biofeedback method based on eye tracking, which utilizes the CNN-SVM model to achieve real-time classification of user gaze direction and improve human-computer interaction in elderly care. | |
| A Novel Approach to Elderly Care Robotics Enhanced With Leveraging Gesture Recognition and Voice Assistance [15] | A new type of elderly care robot aims to improve the safety, health, and quality of life of the elderly by integrating gesture recognition and voice assistance functions. | |
| AI-Enabled Elderly Care Robot [16] | An artificial intelligence-based elderly care robot that uses convolutional neural networks to recognize objects and people, helping elderly people with dementia recognize daily items and family and friends. | |
| Psychological care and emotional support | Deep Learning Approaches for Speech Emotion Recognition Using CNNs and Self-Supervised Models [17] | The method of using convolutional neural networks and self-supervised models for speech emotion recognition achieved a recognition accuracy of over 75% on the dataset. |
| IntelliJoyCare: A Realistic Interactive Audiovisual System for AI-based Elderly Care Companionship [18] | A smart application called IntelliJoyCare combines artificial intelligence, voice therapy, virtual portrait technology, and more to provide emotional support and mental health care for the elderly. | |
| Supporting Creativity in Aged Care: Lessons from Group Singing, Music Therapy, and Immersive Virtual Reality Programs [19] | The article explores the importance of creativity in elderly care, emphasizing the use of group singing, music therapy, and immersive virtual reality activities to meet the psychological and social needs of the elderly. |
| Publications | Physiological Data | Physical Activity (Video) | Physical Activity (Non-Video) | Position | Environmental Data | Household Appliance Data | Lifestyle Habits | Medical History and Symptom Data |
|---|---|---|---|---|---|---|---|---|
| [20] | ✔ | |||||||
| [21] | ✔ | |||||||
| [22] | ✔ | ✔ | ||||||
| [24] | ✔ | ✔ | ||||||
| [25] | ✔ | |||||||
| [9] | ✔ | ✔ | ✔ | |||||
| [26] | ✔ | |||||||
| [29] | ✔ | ✔ | ✔ | |||||
| [30] | ✔ | |||||||
| [32] | ✔ | ✔ | ||||||
| [34] | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| [35] | ✔ | ✔ | ✔ | |||||
| [37] | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ |
| [10] | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| [40] | ✔ | ✔ | ✔ | |||||
| [41] | ✔ | ✔ | ✔ | |||||
| [42] | ✔ | ✔ | ✔ | |||||
| [44] | ✔ | ✔ |
| Publications | Physiological Data | Physical Activity (Video) | Physical Activity (Non Video) | Position | Environmental Data | Household Appliance Data | Digital Information |
|---|---|---|---|---|---|---|---|
| [11] | ✔ | ||||||
| [50] | ✔ | ||||||
| [51] | ✔ | ✔ | |||||
| [53] | ✔ | ✔ | |||||
| [56] | ✔ | ✔ | ✔ | ||||
| [57] | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |
| [12] | ✔ | ✔ | ✔ | ||||
| [58] | ✔ | ||||||
| [59] | |||||||
| [60] | ✔ | ||||||
| [62] | ✔ | ||||||
| [63] | ✔ | ✔ |
| Publications | Physiological Data | Physical Activity (Video) | Physical Activity (Non Video) | Voice Data | Environmental Data | Household Appliance Data | Lifestyle Habits | Medical History and Symptom Data |
|---|---|---|---|---|---|---|---|---|
| [70] | ✔ | |||||||
| [71] | ✔ | ✔ | ✔ | |||||
| [72] | ✔ | ✔ | ||||||
| [73] | ✔ | ✔ | ✔ | ✔ | ||||
| [74] | ✔ | ✔ | ||||||
| [75] | ✔ | ✔ | ✔ | ✔ | ||||
| [76] | ✔ | ✔ | ✔ | |||||
| [13] | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| [14] | ✔ | ✔ | ||||||
| [77] | ✔ | ✔ | ✔ | ✔ | ||||
| [78] | ✔ | |||||||
| [15] | ✔ | ✔ | ✔ | |||||
| [80] | ✔ | |||||||
| [81] | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||
| [82] | ✔ | ✔ | ✔ | ✔ | ||||
| [84] | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||
| [85] | ✔ | ✔ | ||||||
| [86] | ✔ | ✔ | ✔ | |||||
| [87] | ✔ | ✔ | ✔ | ✔ | ||||
| [16] | ✔ | ✔ | ✔ | |||||
| [89] | ✔ | ✔ | ✔ | |||||
| [90] | ✔ | ✔ | ✔ | |||||
| [91] | ✔ | ✔ | ||||||
| [94] | ✔ | ✔ | ✔ | ✔ | ✔ |
| Publications | Physiological Data | Physical Activity (Video) | Physical Activity (Non-Video) | Voice Data | Environmental Data | Household Appliance Data | Lifestyle Habits | Medical History and Symptom Data |
|---|---|---|---|---|---|---|---|---|
| [17] | ✔ | ✔ | ||||||
| [98] | ✔ | ✔ | ||||||
| [99] | ✔ | |||||||
| [100] | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| [101] | ✔ | |||||||
| [102] | ✔ | ✔ | ✔ | ✔ | ||||
| [103] | ||||||||
| [104] | ✔ | |||||||
| [18] | ✔ | ✔ | ✔ | ✔ | ||||
| [19] | ✔ | |||||||
| [106] | ✔ | ✔ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shi, J.; Zhang, N.; Wu, K.; Wang, Z. Application Status, Challenges, and Development Prospects of Smart Technologies in Home-Based Elder Care. Electronics 2025, 14, 2463. https://doi.org/10.3390/electronics14122463
Shi J, Zhang N, Wu K, Wang Z. Application Status, Challenges, and Development Prospects of Smart Technologies in Home-Based Elder Care. Electronics. 2025; 14(12):2463. https://doi.org/10.3390/electronics14122463
Chicago/Turabian StyleShi, Jialin, Ning Zhang, Kai Wu, and Zongjie Wang. 2025. "Application Status, Challenges, and Development Prospects of Smart Technologies in Home-Based Elder Care" Electronics 14, no. 12: 2463. https://doi.org/10.3390/electronics14122463
APA StyleShi, J., Zhang, N., Wu, K., & Wang, Z. (2025). Application Status, Challenges, and Development Prospects of Smart Technologies in Home-Based Elder Care. Electronics, 14(12), 2463. https://doi.org/10.3390/electronics14122463





