IR-UWB Radar-Based Robust Heart Rate Detection Using a Deep Learning Technique Intended for Vehicular Applications
Abstract
:1. Introduction
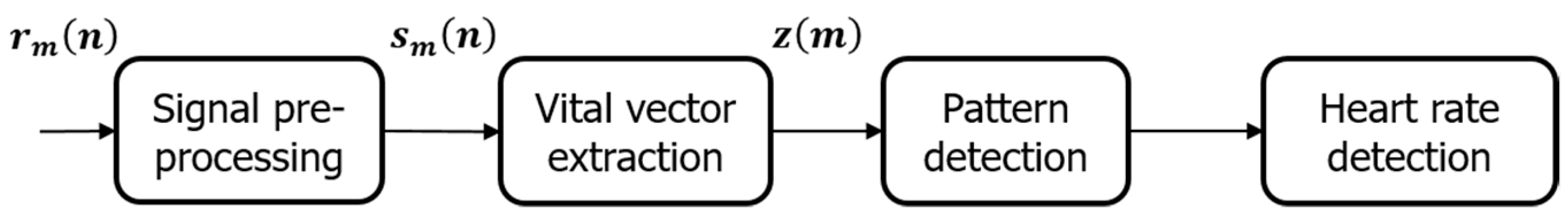
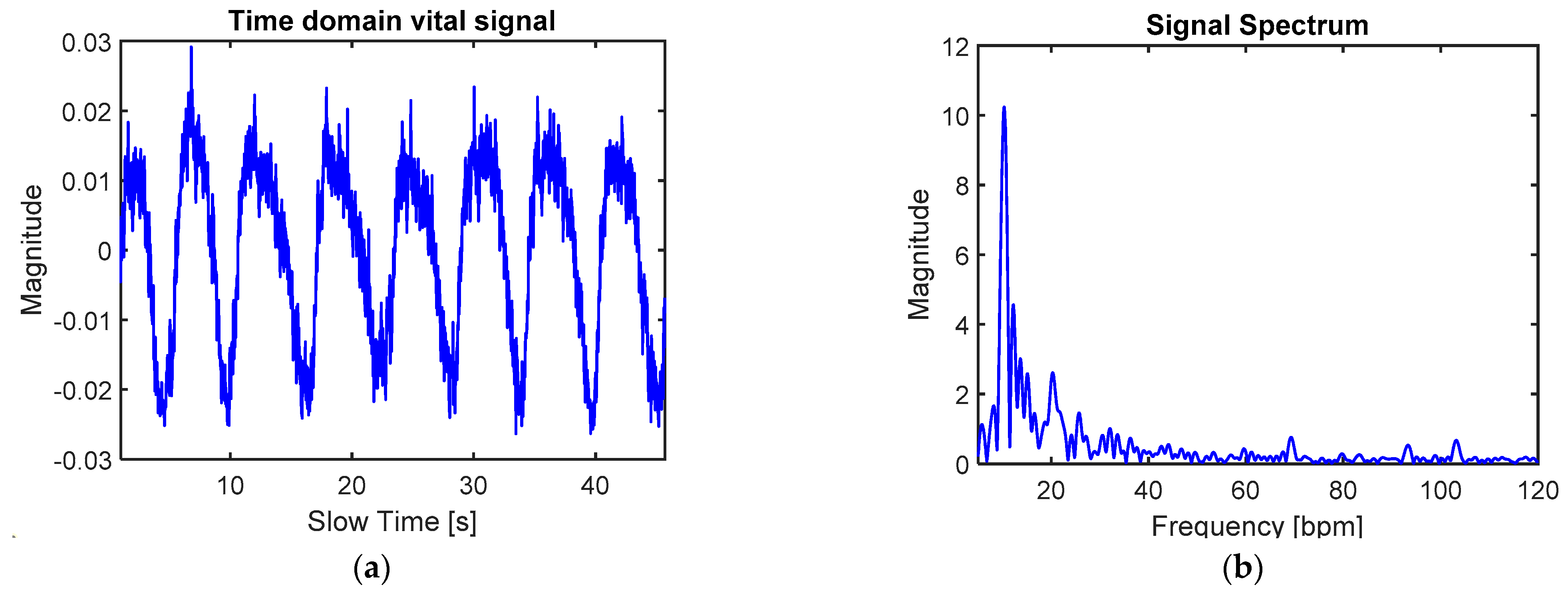
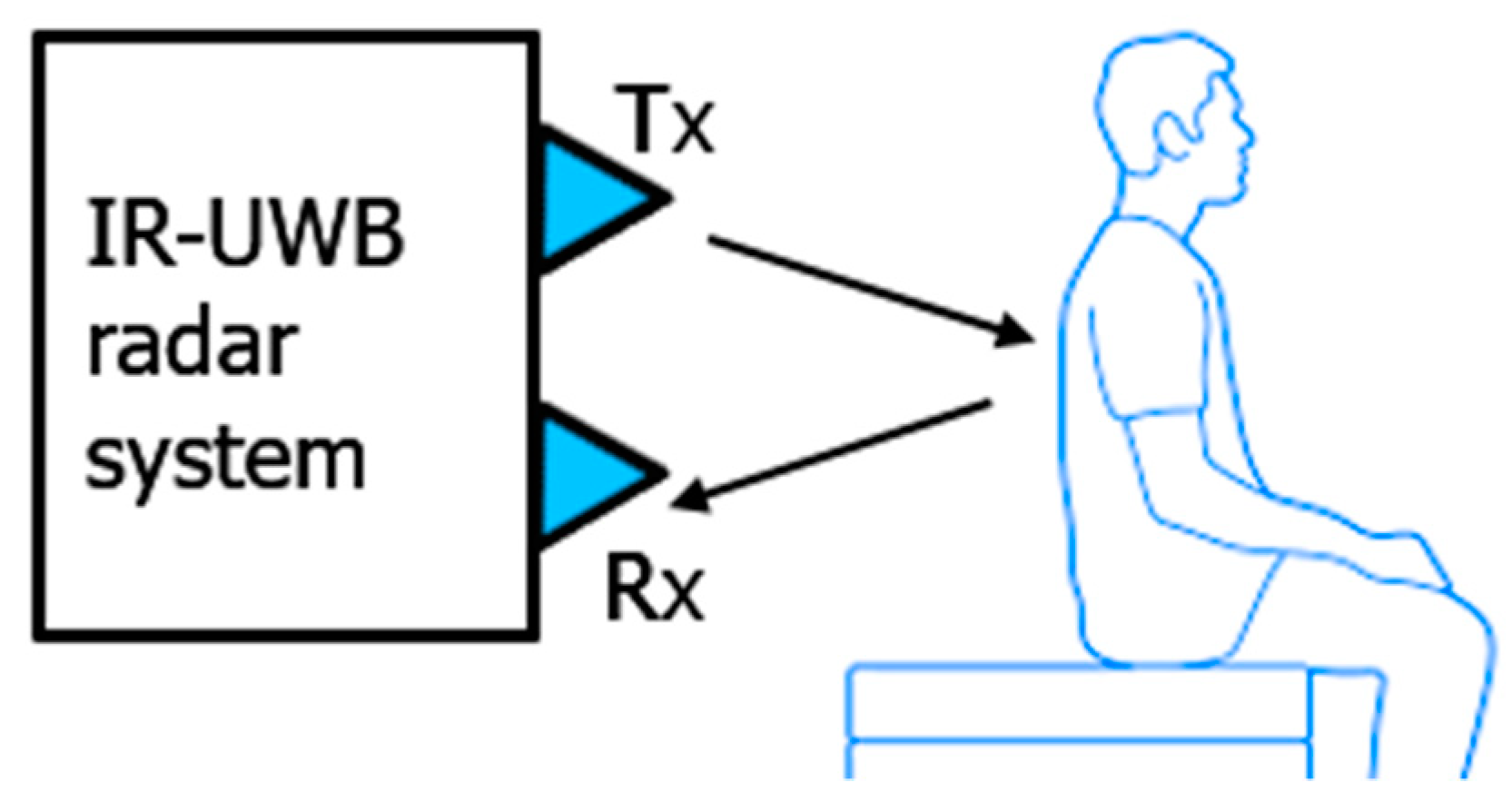
2. Signal Pre-Processing and Problem Statement
3. Proposed Algorithm
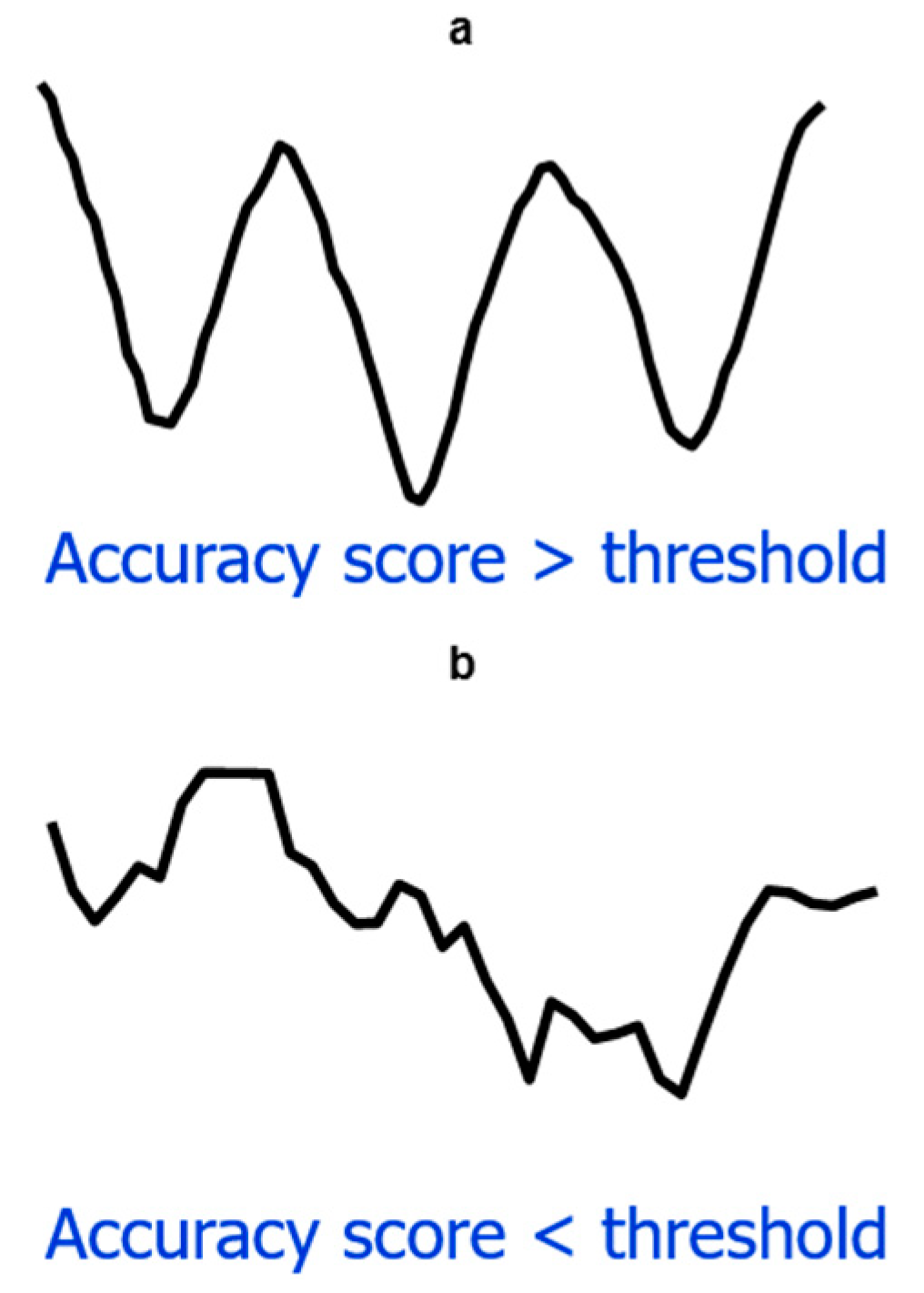
3.1. Signal Segmentation and Image Transformation
3.2. Pattern Classification
3.3. Heart Rate Detection
4. Results
4.1. Experimental Setup
4.1.1. Hardware and Software Setup
4.1.2. Subjects Involved in the Experiments
4.2. Signal Processing and HR Results
5. Conclusions and Future Work
- We propose an algorithm based on time series data, which is the original vital signal, instead of converting it into frequency domain.
- We have determined an optimal location for radar sensor, so that the radar signal is least affected by the interference from RBM and other external interfering movements inside the car.
- A deep learning classifier is used to detect the pattern of the heart rate signal.
- The methods proposed in this work have a better performance than state-of-the-art algorithms on real data.
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chioukh, L.; Boutayeb, H.; Deslandes, D.; Wu, K. Noise and sensitivity of harmonic radar architecture for remote sensing and detection of vital signs. IEEE Trans. Microw. Theory Tech. 2014, 62, 1847–1855. [Google Scholar] [CrossRef]
- Lin, J.C. Microwave sensing of physiological movement and volume change: A review. Bioelectromagnetics 1992, 13, 557–565. [Google Scholar] [CrossRef] [PubMed]
- Lauteslager, T.; Maslik, M.; Siddiqui, F.; Marfani, S.; Leschziner, G.D.; Williams, A.J. Validation of a New Contactless and Continuous Respiratory Rate Monitoring Device Based on Ultra-Wideband Radar Technology. Sensors 2021, 21, 4027. [Google Scholar] [CrossRef] [PubMed]
- Su, W.-C.; Tang, M.-C.; El Arif, R.; Horng, T.-S.; Wang, F.-K. Stepped-frequency continuous-wave radar with self-injection-locking technology for monitoring multiple human vital signs. IEEE Trans. Microw. Theory Tech. 2019, 67, 5396–5405. [Google Scholar] [CrossRef]
- Li, K.L.; Lai, S.-H.; Cheng, K.; Henrickson, L.; Chen, I.; Wu, V.; Chen, J. Exercise vital signs detection employing fmcw radar and artificial neural networks. In Proceedings of the CLEO: Applications and Technology 2021, San Jose, CA, USA, 9–14 May 2021. [Google Scholar]
- Chen, W.; Lan, S.; Zhang, G. Multiple-target vital signs sensing using 77GHz FMCW radar. In Proceedings of the 15th European Conference on Antennas and Propagation (EuCAP), Düsseldorf, Germany, 22 March 2021; pp. 1–3. [Google Scholar]
- Su, G.; Petrov, N.; Yarovoy, A. Dynamic Estimation of Vital Signs with mm-wave FMCW Radar. In Proceedings of the 2020 17th European Radar Conference (EuRAD), Utrecht, The Netherlands, 13–15 January 2021; pp. 206–209. [Google Scholar]
- Wang, G.; Munoz-Ferreras, J.-M.; Gu, C.; Li, C.; Gomez-Garcia, R. Application of linear-frequency-modulated continuous-wave (LFMCW) radars for tracking of vital signs. IEEE Trans. Microw. Theory Tech. 2014, 62, 1387–1399. [Google Scholar] [CrossRef]
- Lazaro, A.; Girbau, D.; Villarino, R. Analysis of vital signs monitoring using an IR-UWB radar. Prog. Electromagn. Res. 2010, 100, 265–284. [Google Scholar] [CrossRef] [Green Version]
- Khan, F.; Ghaffar, A.; Khan, N.; Cho, S.H. An overview of signal processing techniques for remote health monitoring using impulse radio UWB transceiver. Sensors 2020, 20, 2479. [Google Scholar] [CrossRef]
- Khan, F.; Azou, S.; Youssef, R.; Morel, P.; Radoi, E.; Dobre, O.A. An IR-UWB multi-sensor approach for collision avoidance in indoor environments. IEEE Trans. Instrum. Meas. 2022, 71, 1–13. [Google Scholar] [CrossRef]
- Khan, F.; Leem, S.K.; Cho, S.H. Human–computer interaction using radio sensor for people with severe disability. Sens. Actuators A Phys. 2018, 282, 39–54. [Google Scholar] [CrossRef]
- Ahmed, S.; Cho, S.H. Hand gesture recognition using an IR-UWB radar with an inception module-based classifier. Sensors 2020, 20, 564. [Google Scholar] [CrossRef] [Green Version]
- Khan, F.; Leem, S.K.; Cho, S.H. In-air continuous writing using uwb impulse radar sensors. IEEE Access 2020, 8, 99302–99311. [Google Scholar] [CrossRef]
- Leem, S.K.; Khan, F.; Cho, S.H. Detecting mid-air gestures for digit writing with radio sensors and a CNN. IEEE Trans. Instrum. Meas. 2019, 69, 1066–1081. [Google Scholar] [CrossRef]
- Khan, N.; Khan, K.; Khan, A.; Alam, I.; Khan, F.U.; Khan, S.U.; Ali, A. Accommodate Data Loss in Monitoring Vital Signs Through Autoregressive Model. J. Med. Imaging Health Inform. 2019, 9, 1205–1214. [Google Scholar] [CrossRef]
- Khan, F.; Choi, J.W.; Cho, S.H. Design issues in vital sign monitoring through IR UWB radar. In Proceedings of the 18th IEEE International Symposium on Consumer Electronics (ISCE 2014), Jeju, South Korea, 22–25 June 2014; pp. 1–2. [Google Scholar]
- Liu, S.; Qi, Q.; Cheng, H.; Sun, L.; Zhao, Y.; Chai, J. A Vital Signs Fast Detection and Extraction Method of UWB Impulse Radar Based on SVD. Sensors 2022, 22, 1177. [Google Scholar] [CrossRef]
- Paterniani, G.; Sgreccia, D.; Davoli, A.; Guerzoni, G.; di Viesti, P.; Valenti, A.C.; Vitolo, M.; Vitetta, G.M.; Boriani, G. Radar-based Monitoring of Vital Signs: A Tutorial Overview. TechRxiv 2022, preprint. [Google Scholar] [CrossRef]
- Fallatah, A.; Bolic, M.; MacPherson, M.; la Russa, D.J. Monitoring Respiratory Motion during VMAT Treatment Delivery Using Ultra-Wideband Radar. Sensors 2022, 22, 2287. [Google Scholar] [CrossRef]
- Yen, H.T.; Kurosawa, M.; Kirimoto, T.; Hakozaki, Y.; Matsui, T.; Sun, G. A medical radar system for non-contact vital sign monitoring and clinical performance evaluation in hospitalized older patients. Biomed. Signal Process. Control. 2022, 75, 103597. [Google Scholar] [CrossRef]
- Choi, I.; Kim, M.; Choi, J.; Park, J.; Park, S.; Kim, K. Robust cardiac rate estimation of an individual. IEEE Sens. J. 2021, 21, 15053–15064. [Google Scholar] [CrossRef]
- Rohman, B.P.; Andra, M.B.; Nishimoto, M. Through-the-Wall human respiration detection using UWB impulse radar on hovering drone. IEEE J. Sel. Top. Appl. Earth Obs. Remote Sens. 2021, 14, 6572–6584. [Google Scholar] [CrossRef]
- Yang, X.; Zhang, X.; Ding, Y.; Zhang, L. Indoor Activity and Vital Sign Monitoring for Moving People with Multiple Radar Data Fusion. Remote Sens. 2021, 13, 3791. [Google Scholar] [CrossRef]
- Regev, N.; Wulich, D. Remote sensing of vital signs using an ultra-wide-band radar. Int. J. Remote Sens. 2019, 40, 6596–6606. [Google Scholar] [CrossRef]
- Regev, N.; Wulich, D. Multi-modal, remote breathing monitor. Sensors 2020, 20, 1229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, M.; Yang, X.; Li, L.; Zhang, L. In-car multiple targets vital sign monitoring using location-based vmd algorithm. In Proceedings of the 2018 10th International Conference on Wireless Communications and Signal Processing (WCSP), Hangzhou, China, 18–20 October 2018; pp. 1–6. [Google Scholar]
- Khan, F.; Leem, S.K.; Cho, S.H. Hand-based gesture recognition for vehicular applications using IR-UWB radar. Sensors 2017, 17, 833. [Google Scholar] [CrossRef]
- Choi, J.W.; Nam, S.S.; Cho, S.H. Multi-human detection algorithm based on an impulse radio ultra-wideband radar system. IEEE Access 2016, 4, 10300–10309. [Google Scholar] [CrossRef]
- Leem, S.; Khan, F.; Cho, S. Vital sign monitoring and mobile phone usage detection using IR-UWB radar for intended use in car crash prevention. Sensors 2017, 17, 1240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, Z.; Bocca, M.; Jain, V.; Mohapatra, P. Contactless breathing rate monitoring in vehicle using UWB radar. In Proceedings of the 7th international workshop on real-world embedded wireless systems and networks, Shenzhen, China, 4 November 2018; pp. 13–18. [Google Scholar]
- Sahu, M.; Dash, R. A Survey on deep learning: Convolution Neural Network (CNN). In Intelligent and Cloud Computing; Springer: Berlin/Heidelberg, Germany, 2021; pp. 317–325. [Google Scholar]
- Lavanya, P.; Sasikala, E. Deep learning techniques on text classification using Natural Language Processing (NLP) in social healthcare network: A comprehensive survey. In Proceedings of the 2021 3rd International Conference on Signal Processing and Communication (ICPSC), Coimbatore, India, 13–14 May 2021; pp. 603–609. [Google Scholar]
- Ahmed, S.; Khan, F.; Ghaffar, A.; Hussain, F.; Cho, S.H. Finger-counting-based gesture recognition within cars using impulse radar with convolutional neural network. Sensors 2019, 19, 1429. [Google Scholar] [CrossRef] [Green Version]
- Leem, S.K.; Khan, F.; Cho, S.H. Remote authentication using an ultra-wideband radio frequency transceiver. In Proceedings of the 2020 IEEE 17th Annual Consumer Communications & Networking Conference (CCNC), Las Vegas, NV, USA, 10–13 January 2020; pp. 1–8. [Google Scholar]
- Cristianini, N.; Shawe-Taylor, J. An Introduction to Support Vector Machines and Other Kernel-Based Learning Methods; Cambridge University Press: Cambridge, UK, 2000. [Google Scholar]
- Schölkopf, B.; Smola, A.J.; Bach, F. Learning with Kernels: Support Vector Machines, Regularization, Optimization, and Beyond; MIT Press: Cambridge, MA, USA, 2002. [Google Scholar]
- Heidari, A.A.; Mirjalili, S.; Faris, H.; Aljarah, I.; Mafarja, M.; Chen, H. Harris hawks optimization: Algorithm and applications. Future Gener. Comput. Syst. 2019, 97, 849–872. [Google Scholar] [CrossRef]
- Gogna, A.; Tayal, A. Metaheuristics: Review and application. J. Exp. Theor. Artif. Intell. 2013, 25, 503–526. [Google Scholar] [CrossRef]









| Parameters | Value |
|---|---|
| Output power | −12.6 dBm |
| Center frequency | 8.748 GHz |
| Pulse repetition frequency | 40 MHz |
| Bandwidth (−10 dB) | 2.95 GHz |
| Range resolution | 6.4 mm |
| Beamwidth | 65° |
| Sampling frequency | 23.3 GHz |
| No. of antenna arrays per radar chip | 1 Tx & 1 Rx |
| Gender | Age (Years) | Height (cm) | Weight (kg) |
|---|---|---|---|
| M | 33 | 182 | 72 |
| M | 21 | 173 | 73 |
| M | 28 | 174 | 77 |
| F | 26 | 170 | 60 |
| M | 24 | 165 | 62 |
| CNN Layers | Average Accuracy |
|---|---|
| Conv1 | 64.3% |
| Conv2 | 78.6% |
| Conv3 | 89.5% |
| Conv4 | 97.4% |
| Conv5 | 97.4% |
| CNN Layers | Average Error |
|---|---|
| Conv1 | 19.78% |
| Conv2 | 12.40% |
| Conv3 | 6.95% |
| Conv4 | 2.31% |
| Conv5 | 2.32% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khan, F.; Azou, S.; Youssef, R.; Morel, P.; Radoi, E. IR-UWB Radar-Based Robust Heart Rate Detection Using a Deep Learning Technique Intended for Vehicular Applications. Electronics 2022, 11, 2505. https://doi.org/10.3390/electronics11162505
Khan F, Azou S, Youssef R, Morel P, Radoi E. IR-UWB Radar-Based Robust Heart Rate Detection Using a Deep Learning Technique Intended for Vehicular Applications. Electronics. 2022; 11(16):2505. https://doi.org/10.3390/electronics11162505
Chicago/Turabian StyleKhan, Faheem, Stéphane Azou, Roua Youssef, Pascal Morel, and Emanuel Radoi. 2022. "IR-UWB Radar-Based Robust Heart Rate Detection Using a Deep Learning Technique Intended for Vehicular Applications" Electronics 11, no. 16: 2505. https://doi.org/10.3390/electronics11162505
APA StyleKhan, F., Azou, S., Youssef, R., Morel, P., & Radoi, E. (2022). IR-UWB Radar-Based Robust Heart Rate Detection Using a Deep Learning Technique Intended for Vehicular Applications. Electronics, 11(16), 2505. https://doi.org/10.3390/electronics11162505





