Periorbital Hyperpigmentation—Dark Circles under the Eyes; Treatment Suggestions and Combining Procedures
Abstract
1. Introduction
2. Diagnosis
3. Treatment
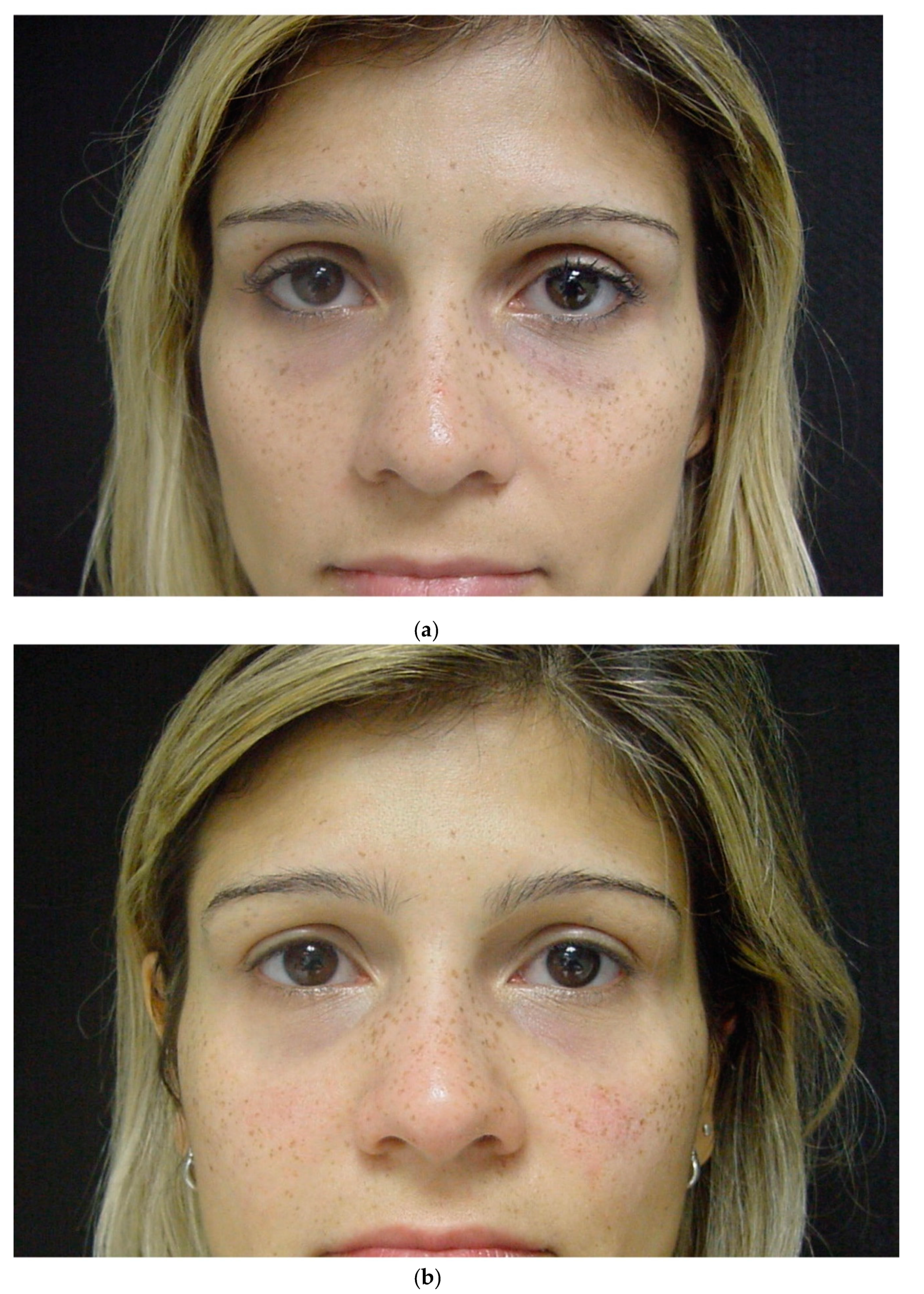
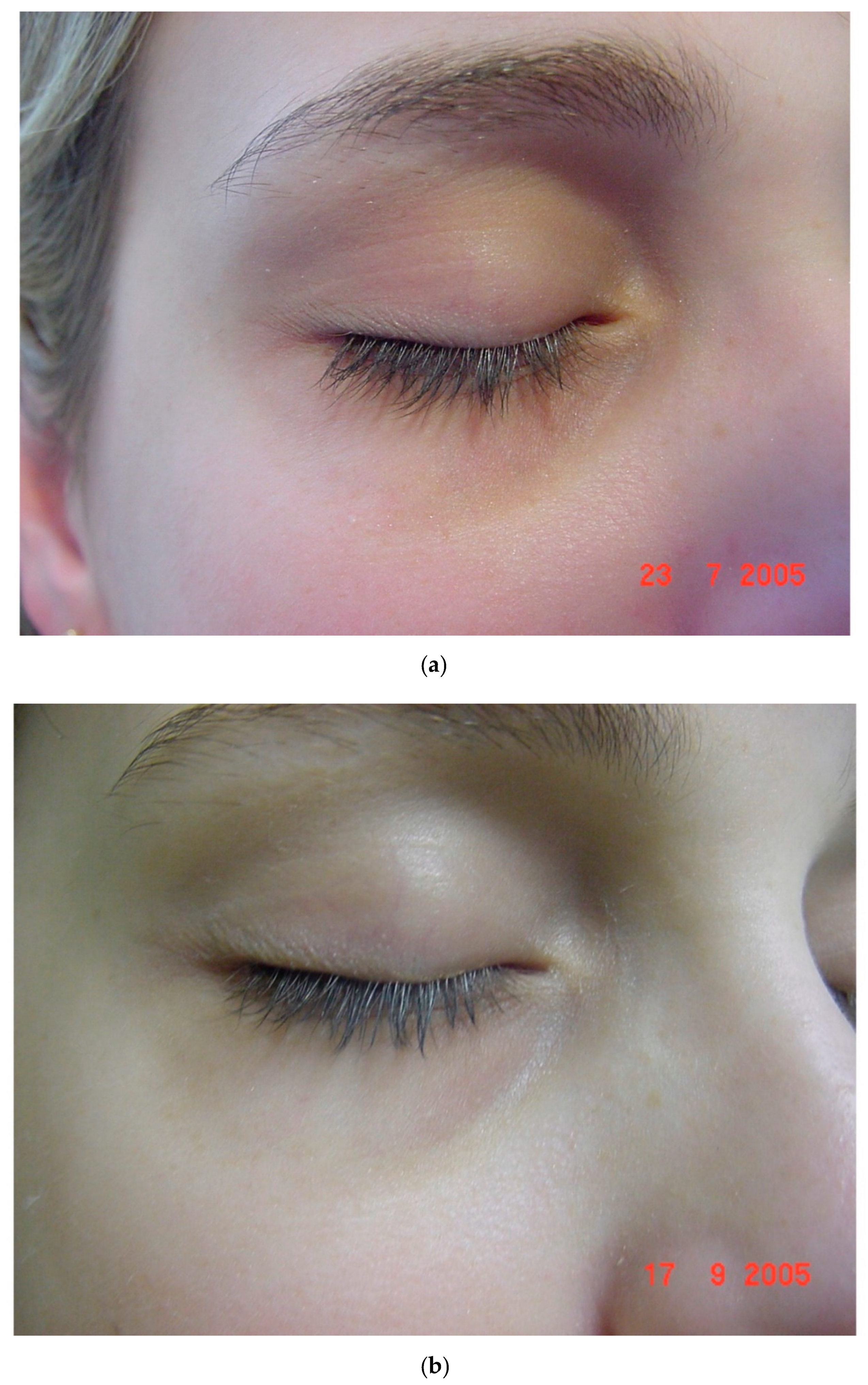
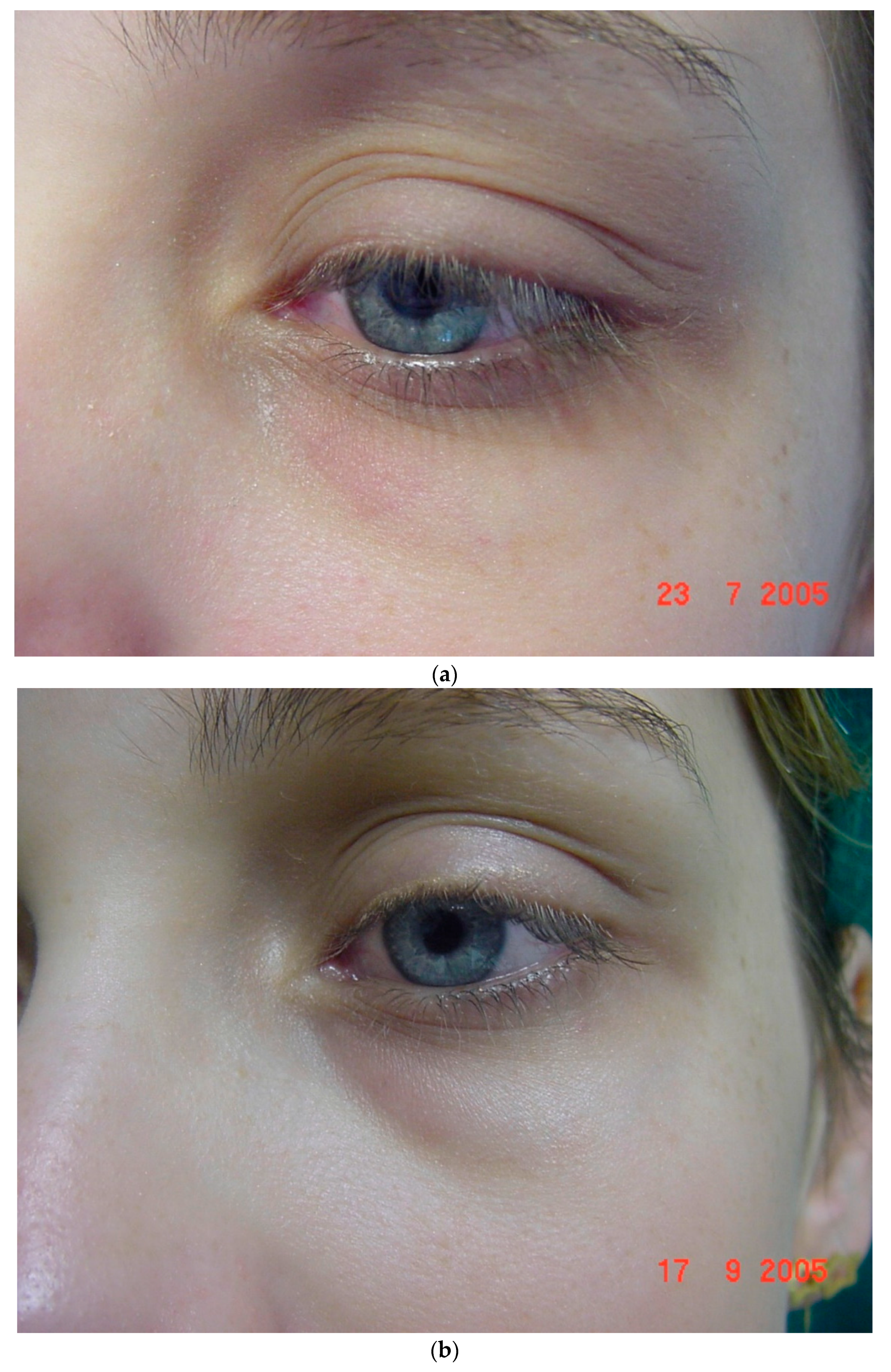
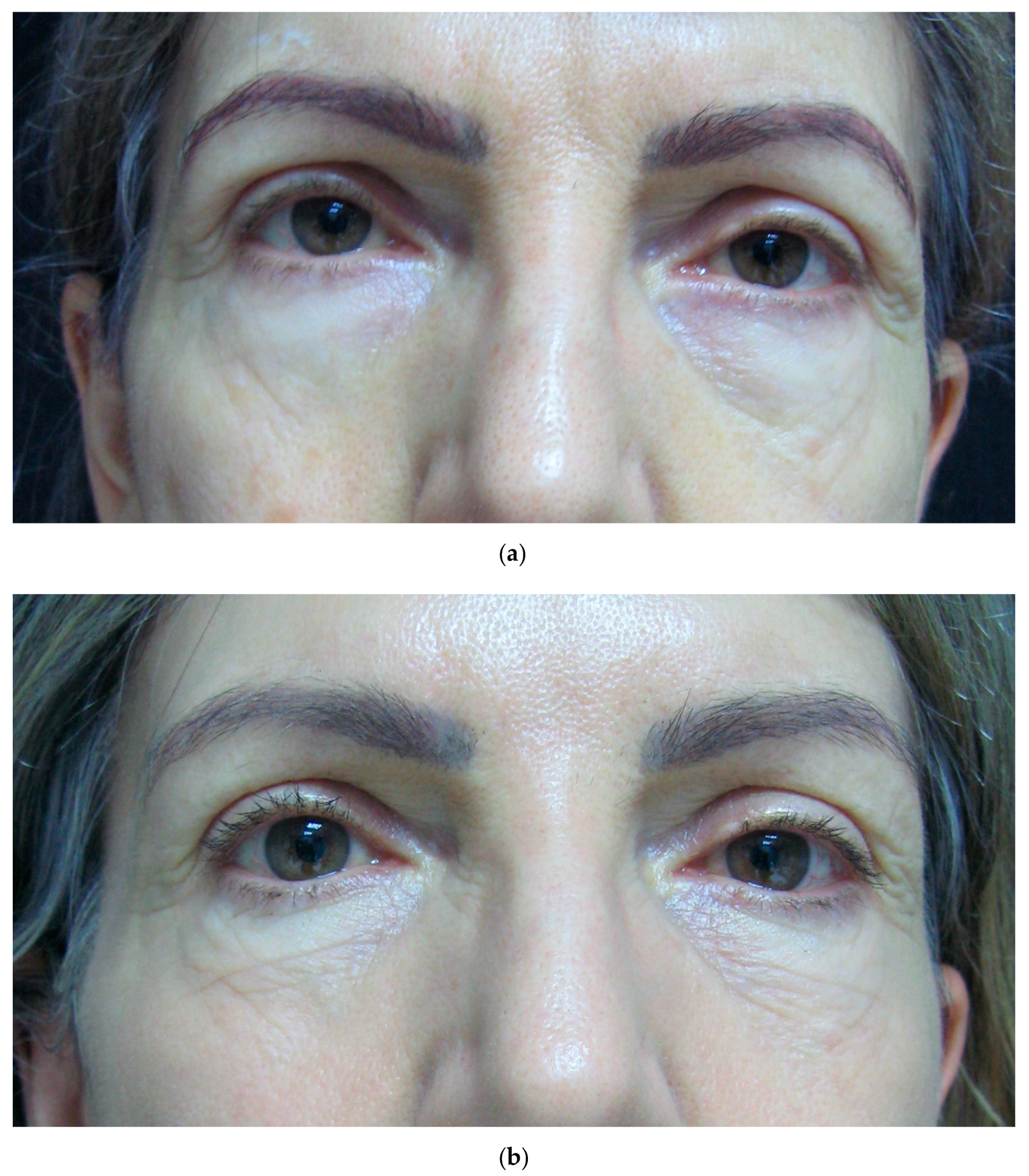
4. Our Patients and Concept
- -
- Presence, intensity, and extension of melanin.
- -
- Presence of small blood vessels under the skin.
- -
- Presence of eyelids fat pads.
- -
- Presence of tear trough deformity.
- -
- Presence of skin excess and skin texture changes (lines and wrinkles).
5. Results
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Correction Statement
References
- Friedmann, D.P.; Goldman, M.P. Dark circles: Etiology and management options. Clin. Plast. Surg. 2015, 42, 33–50. [Google Scholar] [CrossRef]
- Blanc, S.; Bourrier, T.; Albertini, M.; Chiaverini, C.; Giovannini-Chami, L. Dennie-Morgan fold plus dark circles: Suspect atopy at first sight. J. Pediatr. 2015, 166, 1541. [Google Scholar] [CrossRef] [PubMed]
- Nettis, E.; Ferrucci, S.M.; Ortoncelli, M.; Pellacani, G.; Foti, C.; Di Leo, E.; Patruno, C.; Rongioletti, F.; Argenziano, G.; Macchia, L.; et al. Use of dupilumab for 543 adult patients with moderate-to-severe atopic dermatitis: A multicenter, retrospective study. J. Investig. Allergol. Clin. Immunol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Oogi, S.; Nakakura, S.; Terao, E.; Fujisawa, Y.; Tabuchi, H.; Kiuchi, Y. One-year follow-up study of changes in prostaglandin-associated periorbital syndrome after switch from conventional prostaglandin f2alfa to omidenepag isopropyl. Cureus 2020, 12, e10064. [Google Scholar] [CrossRef] [PubMed]
- Vinay, K.; Yanamandra, U.; Dogra, S.; Handa, S.; Suri, V.; Kumari, S.; Khadwal, A.; Prakash, G.; Lad, D.; Varma, S.; et al. Long-term mucocutaneous adverse effects of imatinib in Indian chronic myeloid leukemia patients. Int. J. Dermatol. 2018, 57, 332–338. [Google Scholar] [CrossRef]
- Amini, F.; Thazin Oo, N.M.; Okechukwu, P.N.; Seghayat, M.S.; Ng, E.S.C. Polymorphisms in P53 and VEGFA genes in different subtypes of periorbital hyperpigmentation in a Malaysian Chinese population. Australas J. Dermatol. 2019, 60, e99–e104. [Google Scholar] [CrossRef]
- Matsui, M.S.; Schalka, S.; Vanderover, G.; Fthenakis, C.G.; Christopher, J.; Bombarda, P.C.; Bueno, J.R.; Viscomi, B.L.; Bombarda Júnior, M.S. Physiological and lifestyle factors contributing to risk and severity of peri-orbital dark circles in the Brazilian population. An. Bras. Dermatol. 2015, 90, 494–503. [Google Scholar] [CrossRef]
- Sheth, P.B.; Shah, H.A.; Dave, J.N. Periorbital hyperpigmentation: A study of its prevalence, common causative factors and its association with personal habits and other disorders. Indian J. Dermatol. 2014, 59, 151–157. [Google Scholar] [CrossRef]
- Barone, C.R.; Boza, J.C.; Machado, P.G.; Cestari, T.F. Association between clinical characteristics, quality of life, and sleep quality in patients with periorbital hyperchromia. J. Cosmet. Dermatol. 2018. [Google Scholar] [CrossRef]
- Kikuchi, K.; Masuda, Y.; Hirao, T. Imaging of hemoglobin oxygen saturation ratio in the face by spectral camera and its application to evaluate dark circles. Skin Res. Technol. 2013, 19, 499–507. [Google Scholar] [CrossRef]
- Ranu, H.; Thng, S.; Goh, B.K.; Burger, A.; Goh, C.L. Periorbital hyperpigmentation in Asians: An epidemiologic study and a proposed classification. Dermatol. Surg. 2011, 37, 1297–1303. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.L.; Chang, S.L.; Ma, L.; Lee, M.C.; Hu, S. Clinical analysis and classification of dark eye circle. Int. J. Dermatol. 2014, 53, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Park, S.R.; Kim, H.J.; Park, H.K.; Kim, J.Y.; Kim, N.S.; Byun, K.S.; Moon, T.K.; Byun, J.W.; Moon, J.H.; Choi, G.S. Classification by causes of dark circles and appropriate evaluation method of dark circles. Skin Res. Technol. 2016, 22, 276–283. [Google Scholar] [CrossRef] [PubMed]
- Fatin, A.M.; Mathana Sundram, T.K.; Tan, S.S.E.; Seghayat, M.S.; Lee, C.K.; Rehman, N.; Tan, C.K. Classification and characteristics of periorbital hyperpigmentation. Skin Res. Technol. 2020, 26, 564–570. [Google Scholar] [CrossRef] [PubMed]
- Graziosi, A.C.; Quaresma, M.R.; Michalany, N.S.; Ferreira, L.M. Cutaneous idiopathic hyperchromia of the orbital region (CIHOR): A histopathological study. Aesthetic Plast. Surg. 2013, 37, 434–438. [Google Scholar] [CrossRef] [PubMed]
- Ranjan, R.; Sarkar, R.; Garg, V.K.; Gupta, T. A comparative study of two modalities, 4% hydroquinone versus 30% salicylic acid in periorbital hyperpigmentation and assessment of quality of life before and after treatment. Indian J. Dermatol. 2016, 61, 413–417. [Google Scholar] [CrossRef]
- Vavouli, C.; Katsambas, A.; Gregoriou, S.; Teodor, A.; Salavastru, C.; Alexandru, A.; Kontochristopoulos, G. Chemical peeling with trichloroacetic acid and lactic acid for infraorbital dark circles. J. Cosmet Dermatol. 2013, 12, 204–209. [Google Scholar] [CrossRef]
- Chan, R.; Park, K.C.; Lee, M.H.; Lee, E.S.; Chang, S.E.; Leow, Y.H.; Tay, Y.K.; Legarda-Montinola, F.; Tsai, R.Y.; Tsai, T.H.; et al. A randomized controlled trial of the efficacy and safety of a fixed triple combination (fluocinolone acetonide 0.01%, hydroquinone 4%, tretinoin 0.05%) compared with hydroquinone 4% cream in Asian patients with moderate to severe melasma. Br. J. Dermatol. 2008, 159, 697–703. [Google Scholar] [CrossRef]
- Ertam, I.; Mutlu, B.; Unal, I.; Alper, S.; Kivçak, B.; Ozer, O. Efficiency of ellagic acid and arbutin in melasma: A randomized, prospective, open-label study. J. Dermatol. 2008, 35, 570–574. [Google Scholar] [CrossRef]
- Ohshima, H.; Mizukoshi, K.; Oyobikawa, M.; Matsumoto, K.; Takiwaki, H.; Kanto, H.; Itoh, M. Effects of vitamin C on dark circles of the lower eyelids: Quantitative evaluation using image analysis and echogram. Skin Res. Technol. 2009, 15, 214–217. [Google Scholar] [CrossRef]
- Ellabban, N.F.; Eyada, M.; Nada, H.; Kamel, N. Efficacy and tolerability of using platelet-rich plasma versus chemical peeling in periorbital hyperpigmentation. J. Cosmet. Dermatol. 2019, 18, 1680–1685. [Google Scholar] [CrossRef] [PubMed]
- Dayal, S.; Sangal, B.; Sahu, P. Ferulic acid 12% peel: An innovative peel for constitutional type of periorbital melanosis-Comparing clinical efficacy and safety with 20% glycolic peel and 15% lactic peel. J. Cosmet. Dermatol. 2020, 19, 2342–2348. [Google Scholar] [CrossRef] [PubMed]
- Lowe, N.J.; Wieder, J.M.; Shorr, N.; Boxrud, C.; Saucer, D.; Chalet, M. Infraorbital pigmented skin. Preliminary observations of laser therapy. Dermatol. Surg. 1995, 21, 767–770. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.L.; Cohen, J.L. Treatment of periorbital veins with long-pulse Nd:YAG laser. J. Drugs Dermatol. 2015, 14, 1360–1362. [Google Scholar] [PubMed]
- Vanaman Wilson, M.J.; Jones, I.T.; Bolton, J.; Larsen, L.; Wu, D.C.; Goldman, M.P. Prospective studies of the efficacy and safety of the picosecond 755, 1,064, and 532 nm lasers for the treatment of infraorbital dark circles. Lasers Surg Med. 2018, 50, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Del Duca, E.; Zingoni, T.; Bennardo, L.; Di Raimondo, C.; Garofalo, V.; Sannino, M.; Petrini, N.; Cannarozzo, G.; Bianchi, L.; Nisticò, S.P. Long-term follow-up for Q-switched Nd:YAG treatment of Nevus of Ota: Are high number of treatments really required? A case report. Photobiomodul. Photomed. Laser Surg. 2021, 39, 137–140. [Google Scholar] [CrossRef]
- Michelle, L.; Pouldar Foulad, D.; Ekelem, C.; Saedi, N.; Mesinkovska, N.A. Treatments of periorbital hyperpigmentation: A systematic review. Dermatol. Surg. 2021, 47, 70–74. [Google Scholar] [CrossRef]
- Momosawa, A.; Kurita, M.; Ozaki, M.; Miyamoto, S.; Kobayashi, Y.; Ban, I.; Harii, K. Combined therapy using Q-switched ruby laser and bleaching treatment with tretinoin and hydroquinone for periorbital skin hyperpigmentation in Asians. Plast. Reconstr. Surg. 2008, 121, 282–288. [Google Scholar] [CrossRef]
- Corduff, N. An alternative periorbital treatment option using calcium hydroxyapatite for hyperpigmentation associated with the tear trough deformity. Plast. Reconstr. Surg. Glob. Open 2020, 8, e2633. [Google Scholar] [CrossRef]
- Wollina, U. Improvement of tear trough by monophasic hyaluronic Acid and calcium hydroxylapatite. J. Clin. Aesthet. Dermatol. 2014, 7, 38–43. [Google Scholar]
- Shue, S.; Kurlander, D.E.; Guyuron, B. Fat injection: A systematic review of injection volumes by facial subunit. Aesthetic Plast. Surg. 2018, 42, 1261–1270. [Google Scholar] [CrossRef]
- Loeb, R. Naso-jugal groove leveling with fat tissue. Clin. Plast. Surg. 1993, 20, 393–400. [Google Scholar] [CrossRef]
- Nassif, P.S. Lower blepharoplasty: Transconjunctival fat repositioning. Facial Plast. Surg. Clin. N. Am. 2005, 13, 553–559. [Google Scholar] [CrossRef]
- Hamra, S.T. Arcus marginalis release and orbital fat preservation in midface rejuvenation. Plast. Reconstr. Surg. 1995, 96, 354–362. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Wang, X.; Chen, R.; Xia, X.; Sun, S.; Hu, K. Tear trough deformity: Different types of anatomy and treatment options. Postepy Dermatol Alergol. 2016, 33, 303–308. [Google Scholar] [CrossRef]
- Goldman, A.; Lotti, T.; Tchernev, G.; Wollina, U. Successful treatment of reticular blue veins of the lower eyelid by long-pulse Nd: YAG—Case report with 8-year follow-up. Open Access Maced. J. Med. Sci. 2017, 6, 58–60. [Google Scholar] [CrossRef] [PubMed]
- Goldman, A.; Prati, C.; Rossato, F. Hand rejuvenation using intense pulsed light. J. Cutan. Med. Surg. 2008, 12, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Wollina, U.; Goldman, A. Management of stretch marks (with a focus on striae rubrae). J. Cutan. Aesthet. Surg. 2017, 10, 124–129. [Google Scholar] [CrossRef]
- Wollina, U. Hyaluronsäure in der ästhetischen Dermatologie. Praktische Erfahrungen mit einem topischen Hyaluronsäure-Serum. Kosmet. Med. 2006, 27, 16–18. [Google Scholar]
- Colvan, L.; Fleck, T.; Vega, V.L. Global periorbital skin rejuvenation by a topical eye cream containing low molecular weight heparan sulfate (LMW-HS) and a blend of naturally derived extracts. J. Cosmet. Dermatol. 2019, 18, 530–538. [Google Scholar] [CrossRef]
- Mendiratta, V.; Rana, S.; Jassi, R.; Chander, R. Study of causative factors and clinical patterns of periorbital pigmentation. Indian Dermatol. Online J. 2019, 10, 293–295. [Google Scholar] [CrossRef] [PubMed]
- Wollina, U. Pre- and post-laser treatment in cosmetic dermatology. Eur. Dermatol. 2010, 5, 47–49. [Google Scholar]

| Constitutional | • Patients show a curved band of brownish to black skin pigmentation on lower eyelids approximating the shape of the orbital rim with frequent involvement of upper eyelids. |
| Post-inflammatory | Here, irregular patches of brownish or gray pigmentation can be found on the upper, lower, or both eyelids with lichenification, and eczematous lesions in the surrounding areas. |
| Vascular | • Patients present with erythema predominantly involving the inner aspect of lower eyelids, with prominent capillaries or telangiectasia, often with a thin translucent skin. There may be a bluish discoloration of the lower eyelid and visible bluish veins. |
| Shadow effect | This type is mainly due to structural anatomical factors (e.g., overhanging tarsal muscle, eye bags, or a deep tear trough). |
| Others | • Such as internal disorders (e.g., anemia, hormonal disturbances, nutritional deficiencies), skin disease (e.g., acanthosis nigricans, cutis laxa, nevus Ota, nevus Hori, erythema dyschromicum perstans, fixed drug eruption), and drugs (latanoprost and bimatoprost eye drops). |
| Grade | Remarks |
|---|---|
| 0 | Skin color not different from other facial skin areas |
| 1 | Faint pigmentation of infraorbital folds |
| 2 | More pronounced |
| 3 | Deep dark color, all eyelids involved |
| 4 | Grade 3 pigmentation spreading beyond the infraorbital fold |
| No. of Subjects | 74 |
|---|---|
| Average age (yrs) | 36.1 (range, 18−57) |
| Sex | |
| Female | 64 (86.5%) |
| Male | 10 (13.3%) |
| Average time of condition (yrs) | 3.8 (range, 1–30) |
| Follow-up | 6 to 32 months |
| Improvement | n (%) |
|---|---|
| Poor (no improvement) | 3 (4.0%) |
| Fair (limited improvement) | 9 (12.1%) |
| Good (significant improvement) | 36 (48.6%) |
| Excellent (market improvement) | 26 (35.1%) |
| Total | 74 (100%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goldman, A.; Goldust, M.; Wollina, U. Periorbital Hyperpigmentation—Dark Circles under the Eyes; Treatment Suggestions and Combining Procedures. Cosmetics 2021, 8, 26. https://doi.org/10.3390/cosmetics8020026
Goldman A, Goldust M, Wollina U. Periorbital Hyperpigmentation—Dark Circles under the Eyes; Treatment Suggestions and Combining Procedures. Cosmetics. 2021; 8(2):26. https://doi.org/10.3390/cosmetics8020026
Chicago/Turabian StyleGoldman, Alberto, Mohamad Goldust, and Uwe Wollina. 2021. "Periorbital Hyperpigmentation—Dark Circles under the Eyes; Treatment Suggestions and Combining Procedures" Cosmetics 8, no. 2: 26. https://doi.org/10.3390/cosmetics8020026
APA StyleGoldman, A., Goldust, M., & Wollina, U. (2021). Periorbital Hyperpigmentation—Dark Circles under the Eyes; Treatment Suggestions and Combining Procedures. Cosmetics, 8(2), 26. https://doi.org/10.3390/cosmetics8020026







