1. Introduction
As a side effect of acne, scars can form after skin inflammation. The wound healing process, which comprises three stages—inflammatory, healing, and remodeling—includes the production of scars [
1]. When macrophages are activated during the inflammatory phase, a variety of cytokines and growth factors are created, which in turn promotes fibroblasts and white blood cells. Numerous factors encourage the development of new blood vessels and epithelialization. The proliferative phase of wound healing is the second stage. It often lasts between 10 days and several weeks. In this stage, cytokines like platelet-derived growth factor (PDGF), ergothioneine (EGT), transforming growth factor beta (TGF β), and fibroblast growth factor (FGF) encourage an increase in the number of fibroblasts. Collagen production and the development of granulation tissue begin. Granulation tissue with a network of capillaries, fibroblasts, and white blood cells fill the skin deficit. Type I collagen replaces type III collagen once it has first been generated. Epithelization takes place as granulation tissue is being produced, and new blood vessels are created. The final stage, the remodeling phase, is when the scar matures and is rebuilt. Fibrous tissue takes the place of granulation. Scars of different kinds can form as a result of improper collagen formation and deterioration during the healing process [
2,
3].
Delayed therapy and the severity of acne are associated with scarring to a higher extent. According to tissue loss (such as ice pick, rolling, and boxcar-type scars) and accelerated tissue development (such as hypertrophic and keloid scars), there are two types of acne scarring [
4]. Depending on the clinical presentation, a variety of treatment options, including surgical and nonsurgical methods, are available for acne scars [
5]. Laser treatment for acne scars is also secure and efficient. Far-infrared light, produced by a fractional carbon dioxide (FCO
2) laser, is a useful therapeutic option for acne scars. A laser of this type produces numerous micro thermal treatment zones (MTZs) to encourage the production of new collagen and re-epithelialization. However, it is still difficult for specialists to effectively treat acne scars and decrease issues. Finding an alternative form of treatment is essential due to the detrimental side effects of ablative fractional lasers, which include inflammation, edema, pain, and hyper pigmentation. It has been shown that non-ablative lasers can lessen acne scarring and improve patient satisfaction [
6]. Fractional non-ablative 1410 nm diode laser technology has little to no downtime for skin rejuvenation. It uses fractional photothermolysis as its operating system. Pulses are delivered as a variety of micro beams to cause columns of coagulation in the epidermis and dermis while preserving the surrounding tissue. The body then uses fresh collagen and elastin to rebuild the damaged tissue as part of its normal healing process. As a result, a pattern of laser micro beams treats small parts of tissues that are surrounded by untreated areas in a less intrusive manner than other fractional lasers [
7].
Given this background, the goal of this research was to evaluate and compare the clinical and immunohistochemical results of FCO2 laser versus fractional non-ablative diode laser for treating facial acne scars.
2. Materials and Methods
This prospective comparative study was performed between October 2020 and October 2022 and was approved by the Dermatology Research Ethical Committee of the National Institute of Laser Enhanced Sciences, Cairo University and the Ethical Committee of the National Research Center (NILES-EC-CU 23/3/7).
Thirty patients were enrolled in this study. Patients with Fitzpatrick skin types II, III, and IV had different types of acne scars on both sides of the face.
Patients were excluded from the study for any of the following reasons: under age 18, keloid or hypertrophic scars, active inflammation, viral skin infections, or a history of topical or systemic therapy for acne scars within the previous six months.
All the patients who participated in this study signed informed written consent forms.
2.1. Treatment Protocol
2.1.1. Fractional CO2 Laser
The SmartXide Dot Fractionated Carbon Dioxide Laser System [FCO2] (Deka, Florence, Italy) with a wavelength of 10,600 nm was used to treat the right side of the face in a non-overlapping manner using the smart stack scanning method with a power of 12 to 15 W depending on the skin type, a spacing of 500 um, a dwell time of 500 us, and stack 2.
2.1.2. Diode Laser
An Emerge Palomar Diode Laser System (Medical Technology Device) with a wavelength of 1410 nm was used to treat the left side of the patient’s face in a triple pass with Palomar Preset Control–Preset information [Energy: 30 mJ, Pitch: 1.1 mm, Pattern: 7 × 10].
To reduce discomfort, a local anesthetic pridocaine cream (lidocaine/prilocaine; Global Napi Pharmaceuticals Egypt) was applied under occlusion 45 min before the procedure and then was cleansed with routine disinfection. Appropriate eyewear and masks were worn, and a smoke evacuator was used. After therapy, cold compresses were used to lessen discomfort and edema. Following the session, patients were advised to use sunscreen throughout the day and an emollient at night to prevent the occurrence of temporary erythema, edema, hyper pigmentation, and dryness. Three sessions were given to patients, spaced one month apart. One month following the third session, the final evaluation was conducted.
2.2. Evaluation Methods
2.2.1. Physician Assessment
At baseline, before each session, and a month after the third session, regular photos were taken using a smart phone camera (resolution of 1080 × 2400 pixels; OPPO Reno 4 smart phone, Dongguan, Guangdong, China).
The atrophic acne scars were graded before and after treatment by a single non-treating physician using the Goodman and Baron qualitative and quantitative global scarring grading system [
8]. To evaluate the clinical improvement in skin smoothness, the investigator’s global assessment with a five-point scale was used (IGA: grade 0—no improvement; 1—0–25% minimal improvement; 2—26–50% mild improvement; 3—51–75% moderate improvement; 4—76–100% marked improvement).
2.2.2. Patient Assessment
Patients’ subjective satisfaction score was calculated using a three-point Likert scale with three anchors: satisfied, partially satisfied, or dissatisfied. Patients were also asked to report post-treatment sequelae including erythema, edema, and crust formation after both laser treatments.
2.3. Histopathologic Evaluation
Whenever possible, punch biopsies (3 mm) were taken from one side before and again from both sides of the face one month following the third session. The biopsy specimens were sectioned, fixed in 10% buffered formalin solution for 48 h, dehydrated in ascending grades of alcohol, cleared in xylol, and embedded in paraffin blocks. Serial sections of 5 μm were mounted on glass slides and then washed in a water bath and left in an oven for dewaxing. Two sections were cut from each block; one section was stained with hematoxylin and eosin (H–E) for histopathological examination. One section was processed for immunohistochemical staining for Collagen 1.
2.4. Immunohistochemical Staining
The slides were deparaffinized and hydrated in xylene. Then, they were treated for antigen retrieval (using a microwave oven for 30 min) with an automated Omnis DAKO immunostainer at a high PH of 8. After this, the sections were treated with antibodies [Rabbit Anti-Collagen I [MD44R]: RM0406RTU7] using avidin–biotin–peroxidase 3% (Thermo Scientific, Waltham, MA, USA) for 30 min [
9,
10,
11].
Diaminobenzidine tetrahydrochloride was used as a substrate and chromogen. Hematoxylin was used as a counterstain.
2.5. Morphometric Analysis
The morphometric analysis was performed at the Pathology Department, Research Center, using a Leica Qwin 500 Image Analyzer (Leica Imaging Systems Ltd., Cambridge, UK). Morphometric analysis was carried out on Rabbit Anti-collagen I immunohistochemical stained slides in a frame area of 3905.5 μm2 at a magnification of ×100. The slides to be examined were placed on the stage of the microscope. The light source was set to the required level. The successful adjustment of illumination was verified on the monitor, the area of fibrosis to be measured was determined as an area per field in micrometers squared, and area fraction and area percentage were determined by using the interactive software of the system. The results appear automatically on the monitor in the form of a table with the total, mean, standard deviation, standard error, minimum area, and maximum area measured. The area measured included five fields in each slide. The area was measured using an objective lens with a magnification of 20×. All histological changes were assessed with an electrical light microscope (Olympus CX 41, Tokyo, Japan). Photomicrographs were taken, and Adobe Photoshop, version 8.0, was used for image processing.
2.6. Statistical Analysis
Data were statistically described in terms of mean, standard deviation (SD), range, or frequencies (number of cases), and percentages when appropriate. Comparisons between the right and left sides as well as between baseline and 1 month post-treatment were performed using the McNemar test. Two-sided p values less than 0.05 were considered statistically significant. IBM SPSS (Statistical Package for the Social Sciences; IBM Corp., Armonk, NY, USA) release 22 for Microsoft Windows was used for all statistical analyses.
3. Results
Thirty patients participated in this split-face intra-patient comparative study; three patients relocated to other cities, one patient stopped her therapy because she became pregnant, and two patients stopped their treatment due to side effects. Eight males (33.3%) and sixteen (66.7%) females finished the prescribed course of therapy. Their mean age was (27.4 ± 6.6), with ages ranging from 18 to 40.
We had 2 patients with type II skin (8.3%), 17 with type III (70.8%), and 5 with type IV skin (20.8%). Severe scar quality was reported in 13 patients (54.2%), while 9 patients (37.5%) had moderate scar quality, and 2 (8.3%) had mild scars. Regarding scar quantity, 10 patients (41.7%) had more than 20 lesions, 6 patients (25%) had 11–20 lesions, and 8 patients (33.3%) had 1–10 lesions. A total of 6 patients (25%) had the boxcar scar subtype, another 6 (25%) had icepick scars, 3 (12.5%) had rolling scars, and 9 (37.5%) had SFM and SPS scar subtypes.
3.1. Clinical Improvement of Scars
At 3 months after starting treatment, Goodman and Baron quantitative and qualitative global scores showed statistically significant differences compared to baseline on both sides of the face. However, there was no statistically significant difference between both sides of the face according to Goodman and Baron quantitative and qualitative global scores (
p > 0.999,
p = 0.102) (
Table 1 and
Table 2).
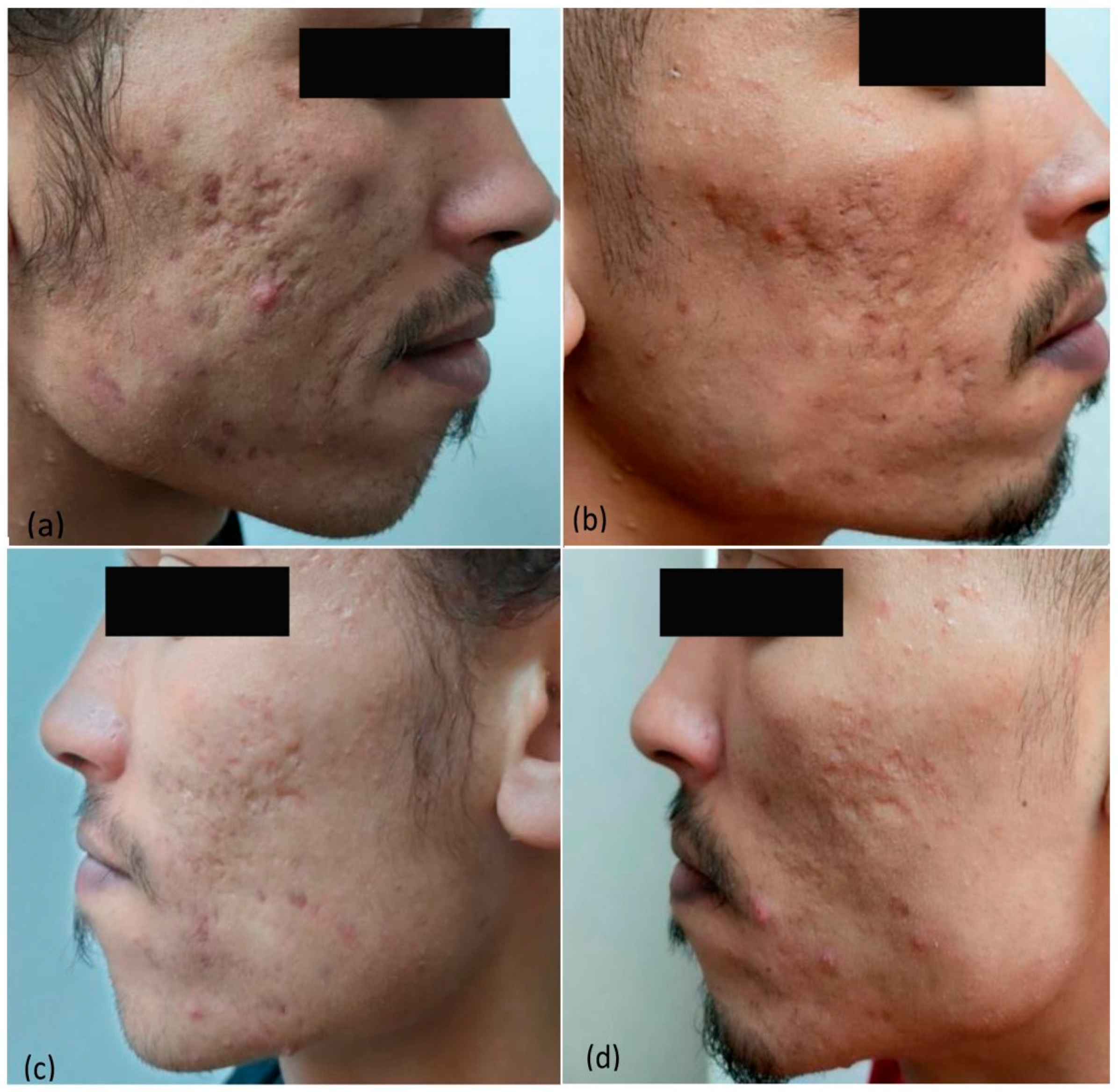
Improvements in skin texture and smoothness in each scar subtype according to IGA were achieved with both FCO
2 and diode lasers. However, the difference between the two treatments was not significant in each scar subtype (
Table 3;
Figure 1,
Figure 2 and
Figure 3).
None of the patients were partially satisfied nor dissatisfied with both laser modalities. Half of the patients, 12 (50%), were satisfied with fractional non-ablative diode laser whilst only 4 patients (16%) were satisfied with ablative FCO2 laser; yet, comparison was not statistically significant (p = 0.099).
Erythema, edema, and crust formation were reported on the right side treated by FCO2 laser by all patients and faded away 5–7 days after the laser session. On the other hand, only transient erythema was noticed in the first 24 h on the left side treated by a diode laser. No pigmentation or scarring was reported on both sides of the face.
3.2. Histopathologic Results
Biopsy specimens were obtained from 10 out of 24 patients. Compared to baseline, at 1 month after the third session of treatment, dermal collagen increased significantly with both FCO
2 and diode laser treatments, as revealed by H–E. In addition, immunohistochemical staining showed an increase in collagen 1 area percentage expression with both treatment modalities. Although the mean percentage of collagen 1 expression per unit area on the right side treated by the FCO
2 laser was higher (39.7%) than the left side treated by the diode laser (37.8%), this difference did not have any significance (
p value = 0.392) (
Figure 4).
3.3. Proportion of Collagen I Area Percentage in Various Forms of Scarring
Within the boxcar scar subtype, the mean and SD of collagen 1 on the right side (FCO
2 laser) was 45.3 ± 6.3 (%), while on the left side (diode laser), it was 43.4 ± 6.7 (%). There was no statistically significant difference between the two sides (
p = 0.729). In the rolling scar subtype, the values were 32.7 ± 5.7 (%) and 32.1 ± 1.3 (%), respectively, with no statistically significant difference (
p = 0.86). Regarding the SFM and SPS scar subtype, the right side had a mean ± SD of 39.2 ± 3.1 (%), while the left side values were 36.1 ± 6.4 (%). The comparison showed no statistically significant difference (
p = 0.245) (
Figure 5 and
Figure 6).
4. Discussion
Owing to the fact that non-ablative lasers are better alternative modalities for the treatment of acne scars with minimal downtime and minimal complications, this motivated us to conduct a study evaluating the effectiveness of an ablative FCO2 laser versus a fractional non-ablative 1410 nm diode laser in the treatment of various types of acne scars clinically, histopathologically, and immunohistochemically (IHC) in a split-face manner. Such a split-face intra-patient comparative study would enable the more accurate assessment of results and prevent individual variability in doing so.
Fractional lasers operate according to the principle of fractional photothemolysis, in which selective thermal damage is induced and MTZs are created in regularly spaced arrays leaving areas of intervening skin unaffected. Consequently, this stimulates neocollagenesis as part of the body’s natural healing process [
12,
13,
14]. In our study, there was a trend that ablative FCO
2 laser-treated sides had better outcomes than fractional non-ablative diode laser-treated sides. The reason is that the CO
2 laser produces a wider zone of residual thermal damage (RTD) and a greater degree of tissue injury, promoting more collagen synthesis compared to a diode laser. Yet, the comparison between the two laser modalities failed to show a significant difference.
In the present study, 1 month after the third treatment session, Goodman and Baron’s quantitative and qualitative global scores showed a statistically significant reduction and an improvement in both FCO
2 and diode laser-treated skin compared to the baseline. Nevertheless, there was no significant difference between them. A split-face comparative study was conducted by Kar and Raj [
15] on 30 patients with moderate to severe acne scars. The patients underwent three sessions of FCO
2 laser and FCO
2 laser + topical PRP (platelet-rich plasma) on right and left sides of the face, respectively, at monthly intervals. There was a significant improvement on both sides of the face when baseline scores were compared to end scores, but the difference between the right and the left sides of the face was not statistically significant (
p = 0.2891). Moreover, the symptoms of redness, edema, and pain on the treated areas with laser were significantly lesser on the FCO
2 + PRP (left) side as compared to the FCO
2-only (right) side.
Regarding the diode laser, a study was conducted by Rathod et al. [
16] on forty-eight patients with atrophic acne scars who were treated with a non-ablative 1450 nm diode laser. Their results revealed that after the first month, 79.2% of the patients had improved by 30%, and by the end of the third month, 92.9% had improved by more than 30% with a 1450 nm diode laser, which was more successful for both rolling and boxcar kinds than for boxcar scars exclusively. They also showed greater efficacy in rolling scars than boxcar scars. This study was in accordance with our diode laser results. Our comparison showed a statistically significant improvement (
p = 0.009) compared to baseline, but there were some variations, as in our study, boxcar scars showed marked improvement compared to rolling scars treated with a 1410 nm diode laser.
In the current study, histopathologic evaluations revealed disorganized, thin collagen fiber networks in untreated atrophic acne scars. At one month after the third session of both lasers, collagen fibers in the papillary dermis were found to be increased in density and number by H–E staining. Collagen deposition was more compact and denser with the FCO2 laser than with the diode laser, and collagen deposition corresponded to clinical improvements observed by physicians.
Immunohistochemical staining in this study exhibited an increase in collagen 1 area percentage expression on both sides of the face at one month after the third session of treatment. Despite the higher percentage of collagen 1 expression following FCO2 laser compared to that following diode laser, the p-value was non-significant. This might be due to the multidirectional pattern of the differences between the patients and the relatively small number of patients that underwent biopsies 3 months after starting treatment.
A split-face intra-patient comparative study was conducted by Min et al. [
17] on 24 patients with atrophic acne scars who were treated for three months with non-ablative bipolar radiofrequency combined with diode laser (BRDL) on the left side of the face and fractional ablative Er–YAG laser on the right side of the face. Both treatment modalities resulted in increased expression of collagen 1 with time; however, the expression level of collagen 1 was higher on the Er–YAG laser-treated side with significance (
p = 0.01) compared to BRDL treatment. Their results demonstrated the superior efficacy of Er–YAG laser for the treatment of all scar types compared to baseline, as dermal collagen became thicker and denser at day 84 after both treatment modalities. The histologic results of this study support our study and were in line with our results.
Osman et al. [
18] conducted another randomized split-face study using fractional Er–YAG laser on one side of the face and micro-needling on the other side. Thirty patients with atrophic acne scars received 5 treatments at 1 month intervals. At the 3 month follow-up, both treatment modalities induced noticeable histological improvement, and collagen fibers in the papillary dermis were found to be increased in density and number by H–E and Masson trichrome staining. There was a significantly higher increase in the mean number of collagen fibers following fractional Er–YAG laser treatment (
p < 0.001).
Similarly, Kwon et al. [
19] evaluated the histopathological efficacy of 3 monthly sessions of non-ablative fractional laser (NAF) alone versus its sequential application with fractional micro-needling radiofrequency (FMR) in a randomized split-face study of 26 subjects with atrophic acne scars. In H–E and Masson trichrome, they noticed increased collagen fiber deposition in both treatment regimens as compared with baseline, but the side treated with the combined regimen exhibited denser dermal interstitial fiber accumulation. IHC staining for type I collagen further supported the above-mentioned findings.
Many studies have reported that ablative FCO
2 laser is one of the most effective techniques in atrophic acne scar treatment while symptoms of redness, edema, pain, and post-inflammatory hyper-pigmentation are still the most common side effects [
20,
21,
22]. These findings bolster our results.
Unlike ablative fractional lasers which remove the epidermis, non-ablative fractional lasers deliver heat to the underlying skin tissue, without the ablation of the stratum corneum, harming the epidermis, or the extrusion of the dermal contents [
23]. This may explain the prolonged erythema reported on ablative FCO
2 laser-treated sides, which faded away 5–7 days after the laser session, compared to those which disappeared in the first 24 h on non-ablative fractional diode laser-treated sides.
It is worth noting that despite the superiority of the FCO2 laser over the diode laser in the present study, patient satisfaction was only 16% with the FCO2 laser in comparison to 50% satisfaction with the diode laser. This might be due to prolonged healing time and post-operative sequelae associated with FCO2, which would interfere with daily life activities.
The strengths of the present study include the intra-individual study design. Moreover, all acne scar evaluations were performed by the same blinded and trained physician.
A limitation of the current study might include the short follow-up period. Given that collagen remodeling may last for up to one year, a longer follow-up may have been essential to observe the full effect of ablative FCO2 and fractional non-ablative diode laser treatment on acne scar appearance. Another limitation is the lack of randomization of the treatment strategy.