1. Introduction
Implantable biomedical devices such as blood pressure monitors, cardiac defibrillators, electrocardiograms, electromyography, thermometers, pacemakers, neural stimulators, heart rate sensors, and glucose meters are commonly used to improve the quality of life of millions of patients [
1]. Ultrasound can be defined as cyclic sound pressure with a frequency greater than the upper limit of human hearing. Some animals, for example, bats and dolphins, use ultrasonic waves for locating prey and obstacles. In recent years, the range of ultrasound applications open to humans has expanded considerably, and includes the medical, chemical, industrial and military fields [
2]. An ultrasonic sensor is an audio sensor, and can be divided into three main categories: Transmitter, receiver and transceiver. To improve medical implant devices, several investigators [
3,
4] have used ultrasonic waves to optimize transfer efficiency and increase transfer distances in percutaneous coronary intervention. In [
5], this was done to alter the operating frequency to optimize transfer distances between receiver and transmitter sensors. Other researchers have used a thermal and vibration hybrid based on ultrasonic sensors to develop transfer power [
6]. One study used microelectronics devices to optimize transfer efficiency and compared it with inductive power transfer. Ultrasonic wave–based transfer power is an alternative method to active wearable medical sensors as compared with the electromagnetic method [
7]. Additional components were used in medical implant devices, such as matching layers, to improve transfer efficiencies [
8].
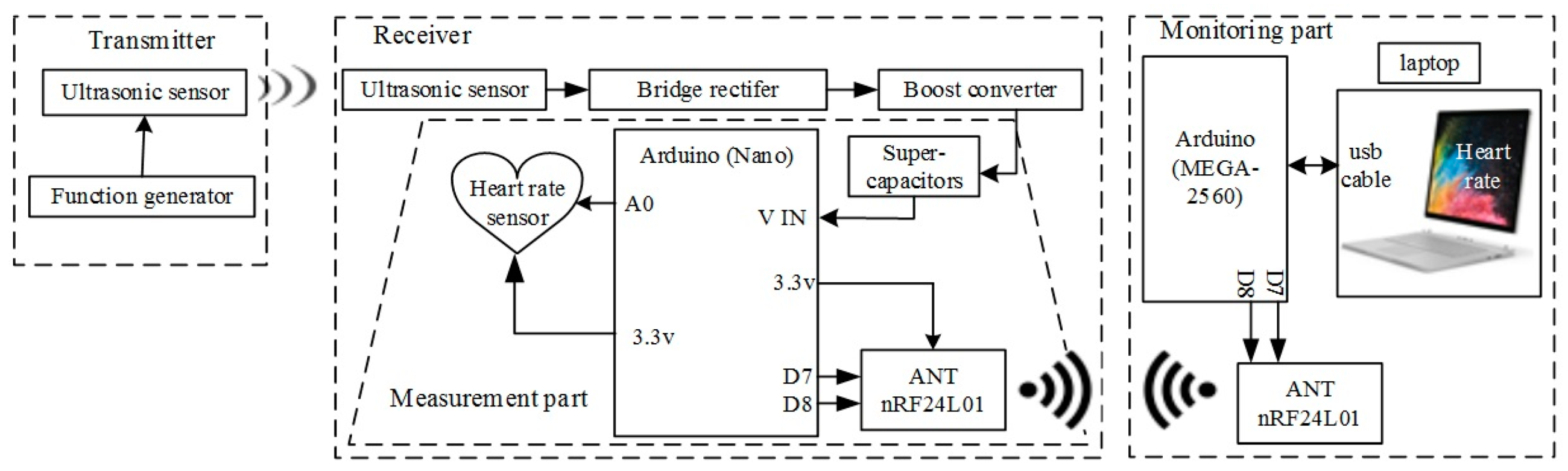
The present study involved an ultrasonic power transfer (UPT) system consisting of a transmitter (Tx) ultrasonic sensor, receiver (Rx) ultrasonic sensor, bridge rectifier, boost converter and load (super-capacitor). Furthermore, the system contains a measurement unit and monitoring unit. The measurement unit involves a microcontroller heart rate sensor and wireless protocol nRF24L01. The monitoring unit has a microcontroller, wireless protocol nRF24L01 and a laptop. The main objective of the present study is to optimize the transfer distance, power and efficiency.
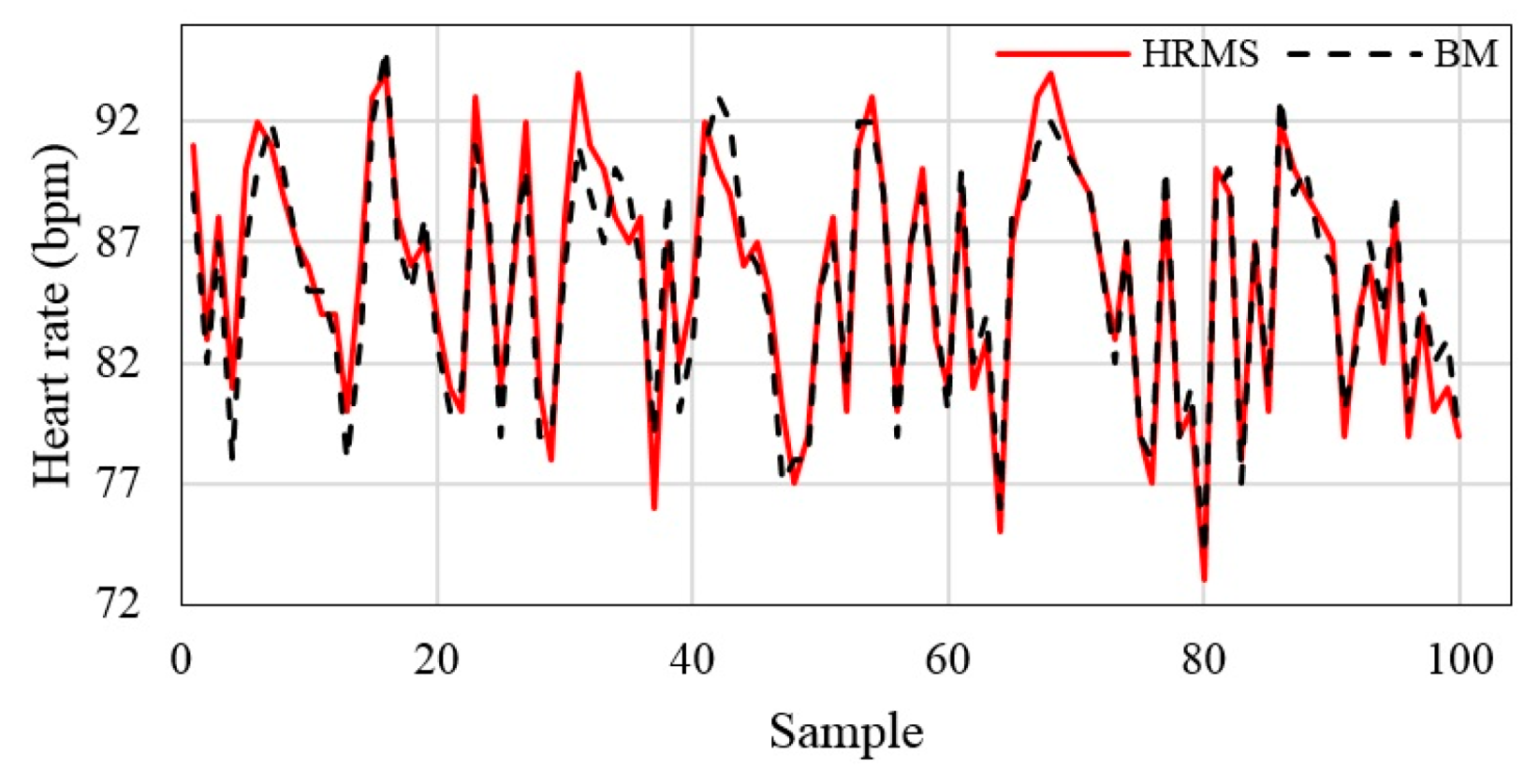
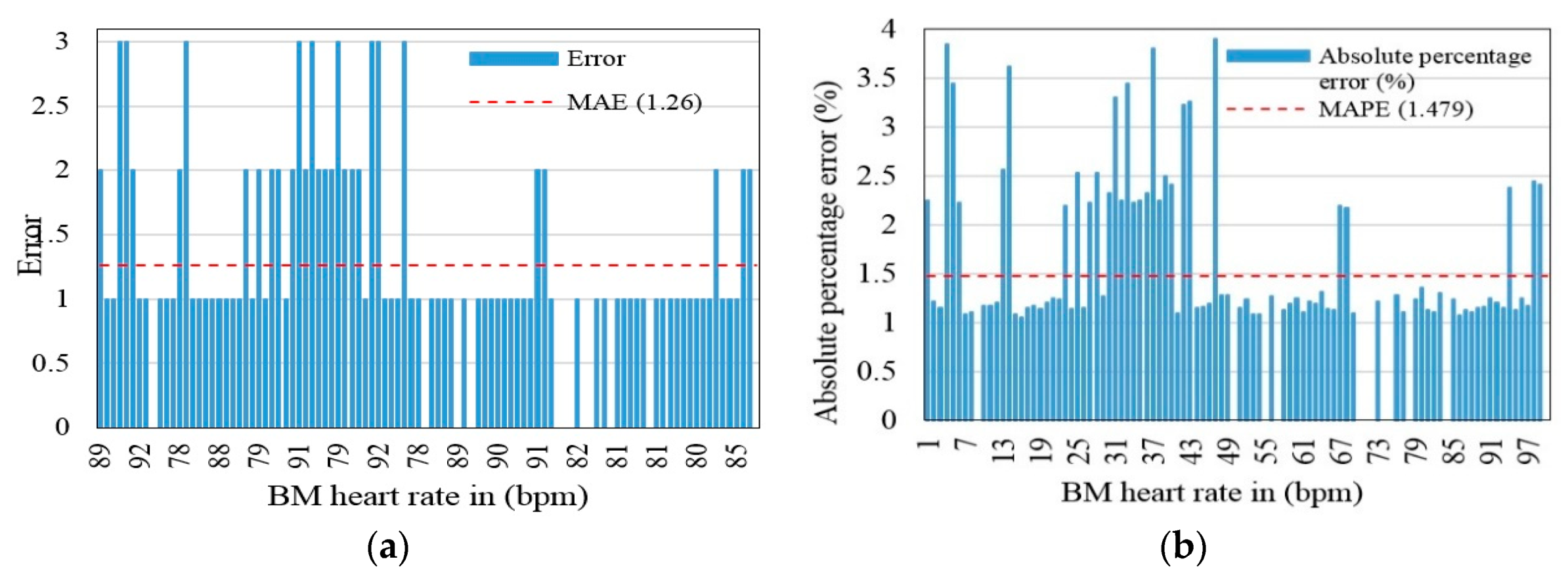
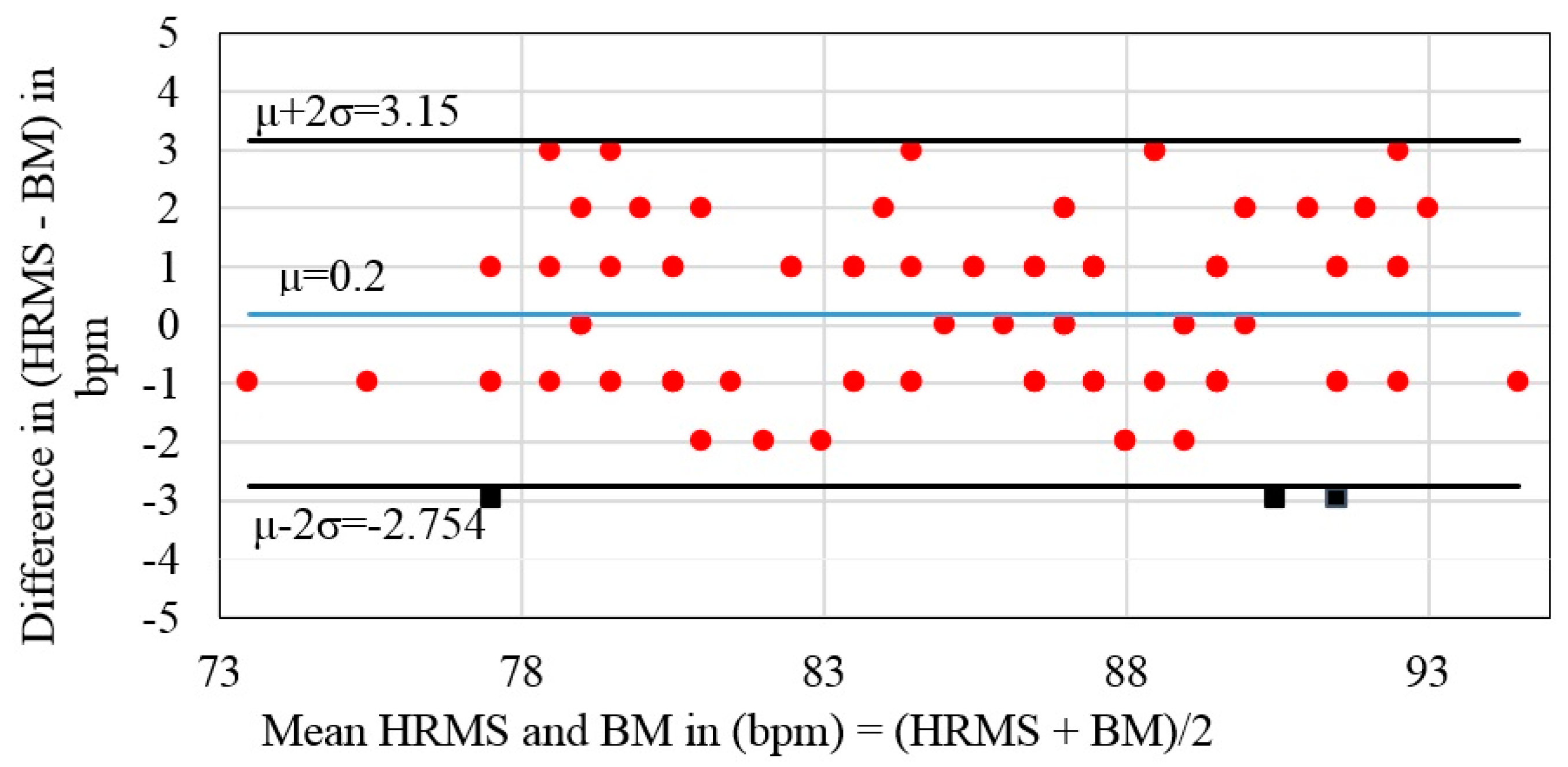
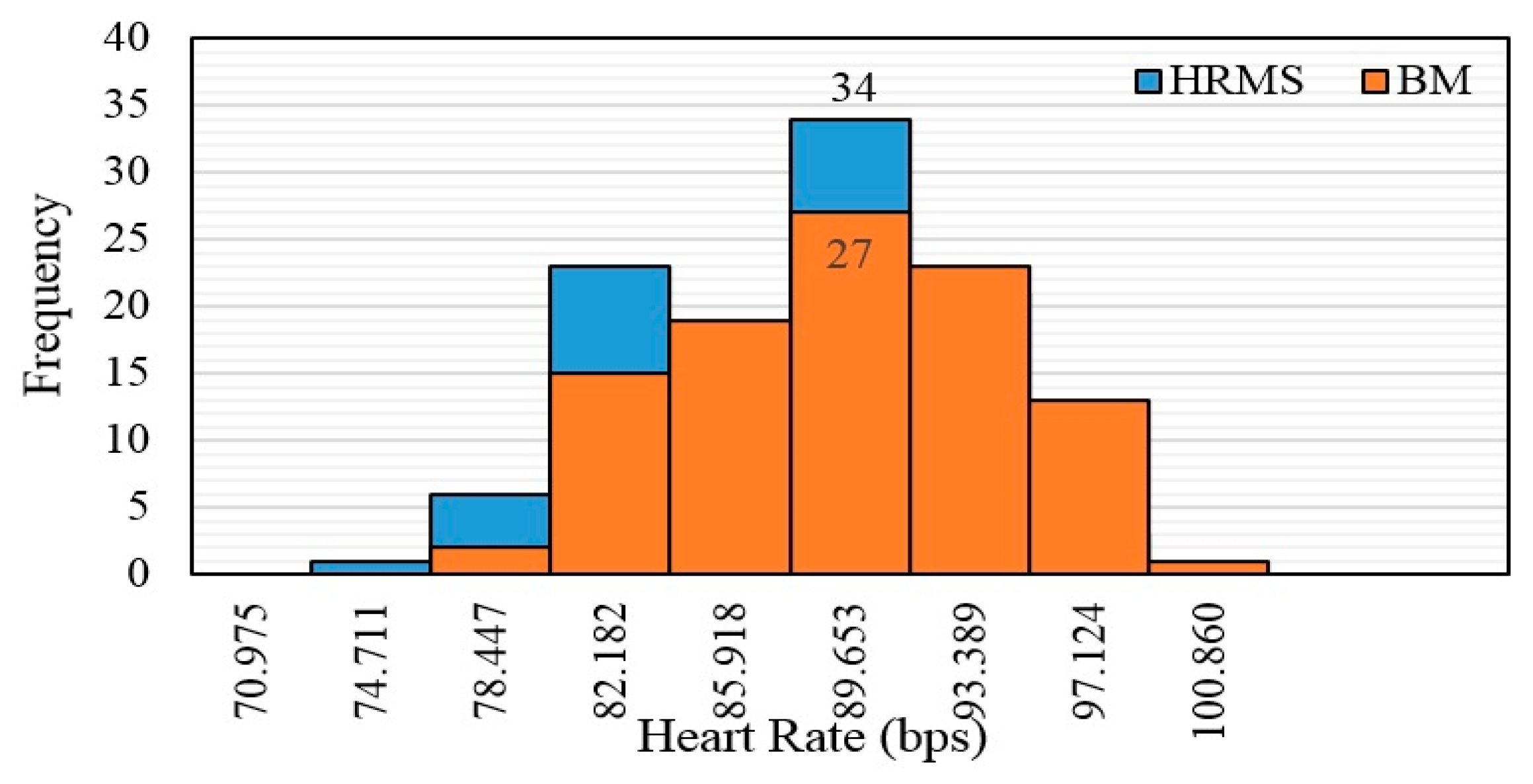
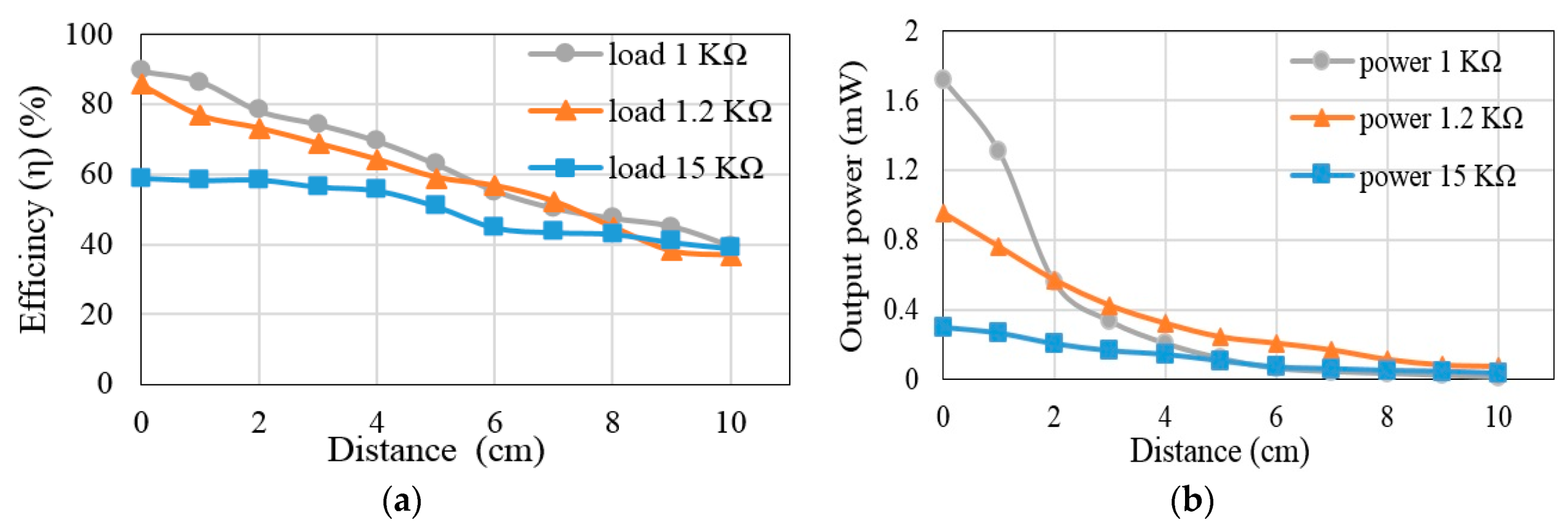
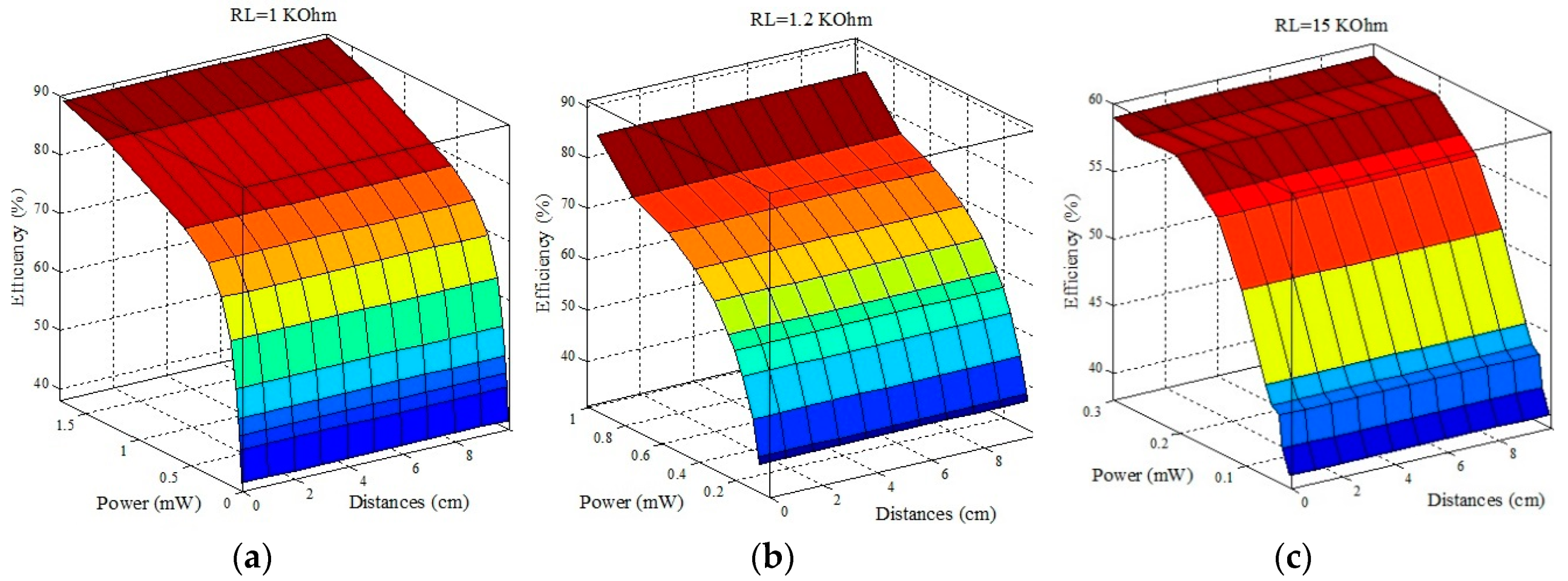
UPT-based transfer power and efficiency were achieved using 1-, 4- and 8-Farad (F) super-capacitors. The transfer power was adequate for supplying a wearable heart rate sensor. The system was tested using transfer distances of 1–10 cm. Several super-capacitors were considered to select the best capacitor that could yield high transfer power and efficiency relative to the other capacitors. At 4 F, the system achieved 69.4% transfer efficiency and 0.318 mW power at 4 cm. In addition, 97% heart rate measurement accuracy was achieved relative to the benchmark device. The heart rate measurements were validated with statistical analysis. Our results show that, with a 4-cm gap between the ultrasound transmitter and receiver, this work outperforms previous works in terms of transfer power and efficiency.
The contribution of this paper can be summarized as follows:
Designed and implemented lightweight UPT.
The ultrasound transducer was designed and implemented to supply adequate power to a wearable heart rate sensor. We achieved transfer power and efficiency at different distances with several super-capacitors.
Improved transfer power and efficiency between transmitter and receiver relative to related previous works.
Heart rate monitoring (HRM), which includes heart rate sensor, microcontroller and wireless protocol (i.e., nRF24L01), was successfully provided by UPT-based power.
Heart rate measurement was validated with a benchmark (BM) based on statistical analysis.
The rest of the paper is as follows. Related work such as that for the performance metrics of the transfer energy is discussed in
Section 2.
Section 3 presents the proposed system design.
Section 4 describes and introduces the system experiment configurations. Validation of the heart rate monitoring system based on statistical analyses is described in
Section 5.
Section 6 highlights the overall results and discussion of the UPT system. The results of the proposed system are compared with that of previous related works in
Section 7. Finally, conclusions with trends for future work are drawn in
Section 8.
2. Related Works
This section highlights previous works using ultrasonic sensors to generate power for vital signs patient monitoring systems. Islam et al. [
3] proposed a vibration to optimize transfer distance and efficiency for implantable devices in percutaneous coronary intervention. The system operates at a frequency of 14 MHz. The system consists of ultrasonic power, polyvinylidene fluoride (PVDF), rectifier and autonomous active stent (AAS) sensor. The experimental results showed that the power transfer efficiency based on AAS and PVDF was approximately 14.8%, while power transfer efficiency of 11.5% was achieved with lead zirconate titanate. The output voltage was 200 mV at the short distance of 2.5 mm and low resonant frequency. At the same distance, the transfer power efficiency of the system using AAS and PVDF was better than the lead zirconate titanate system. The system has several advantages, such as small size, wearability and low cost. However, it has a short transfer distance. Shi et al. [
4] designed and implemented a vibration for medical implant devices to improve transfer power and efficiency based on the piezoelectric material sensor harvesting technique. The system operated at frequencies of 250–240 kHz. The system includes the ultrasonic transmitter/receiver and load. The experimental results revealed that the output voltage of the device was 0 dB at 0 cm, whereas this decreased as the distance increased. The transfer power was improved from 12.0 nW to 77.1 nW at 1 cm based on the piezoelectric ultrasonic energy harvester. The piezoelectric ultrasonic energy harvester system was better than that without it in terms of transfer power efficiency at the same distance. The system had several advantages such as small size, wearability and low cost. However, it has a short transfer distance.
Vihvelin et al. [
5] presented a vibration for medical implant devices to improve transfer efficiency. The system was powered based on the energy harvesting technique (i.e., ultrasonic wave). The system operates at 1.2–1.4 MHz and includes a piezoelectric transmitter/receiver and load. The authors tested two types of media. The experimental results showed that the transfer efficiencies and distance between transmitter and receiver differed based on frequency and media. In water, the transfer efficiency was 45% at transfer distances of 5.9 mm and 6.1 mm at 1.35 and 1.29 MHz, respectively. In air, transfer efficiency was 48% at 4 mm at 1.02–1.60 MHz. The results show that the corresponding transfer efficiency for varying frequencies was 35–100% whereas it was 8–25% for fixed frequencies. The advantages of the system were its low cost, wearable device and small size. Nevertheless, it has a short transfer distance. Semsudin et al. [
6] merged two harvesting techniques (vibration and thermal) for supplying power to micro biomedical devices. The operating frequency of the system is 2 kHz. The system includes triboelectric generators/thermal, rectifier, DC–DC converter and load. The authors tested three inductance variation values (i.e., 0.4, 0.9, 1.2 μH). Experimental results revealed that the output voltages were 2 V, 3.2 V and 4 V, for 0.4 μH, 0.9 μH and 1.2 μH, respectively, using a 0.3 V vibration source. When a 0.2 V thermal source was used, the output voltages were 2.2 V, 3 V and 4 V for 0.9 μH, 1.7 μH and 2.9 μH, respectively. When thermal and vibration were hybridized, the output voltages were 2 V, 3.5 V and 4 V for 0.3 μH, 0.6 μH and 0.9 μH, respectively, based on 0.5 V input voltage. The proposed system was low cost and wearable. Nevertheless, it had high power consumption.
Meng et al. [
7] designed a wearable sensor for implantable microelectronic devices to optimize transfer efficiency. The wearable sensor was powered based on the energy harvesting technique (i.e., vibration of the ultrasonic sensors). The system operated at 1 MHz, 10 MHz and 15 MHz, and included an ultrasonic transmitter/receiver, rectifier, regulator and load. The authors tested three types of frequencies, and the experimental results showed that transfer efficiency was 6%, 0.03% and 0.15% at 3 cm and 5%, ~0.043% and ~0.06% at 8 cm for 1 MHz, 10 MHz and 15 MHz, respectively. In addition, they showed that inductive transfer efficiency was better than ultrasonic at 3 m, being 0.27% and 0.03%, respectively; however, at 8 cm, ultrasonic had better transfer efficiency than inductive, being 0.04% and 0.0025%, respectively. The system has several advantages, such as small size, long distance, wearability and low cost. However, it has poor transfer efficiencies. Miao et al. [
8] proposed a vibration technique to supply power to medical implant devices. The transfer distance and efficiency were improved using ultrasonic waves. The system operates at 1.1–1.8 MHz and includes a piezoelectric transmitter/receiver, rectifier, regulator and load. The authors examined two types of piezoelectric and the experimental results revealed that the transfer efficiency between the piezoelectric transmitter and receiver was 2.11% and 1.15% for 1.8 MHz and 1.4 MHz, respectively, at 3 cm. However, the transfer efficiencies were improved when the matching layer was considered at 1.1 MHz; then, the transfer efficiencies were 65% and 18% at a transfer distance of 3 and 6 cm, respectively. The advantages of the system are the wearable device, small size, safety and low cost. Nevertheless, it has a short transfer distance.
The previous works are summarized in
Table 1. The table compares the performance metrics of the previous studies in terms of operating frequency, harvesting technique, transfer power and efficiency at different distances.
4. Experiment Configuration
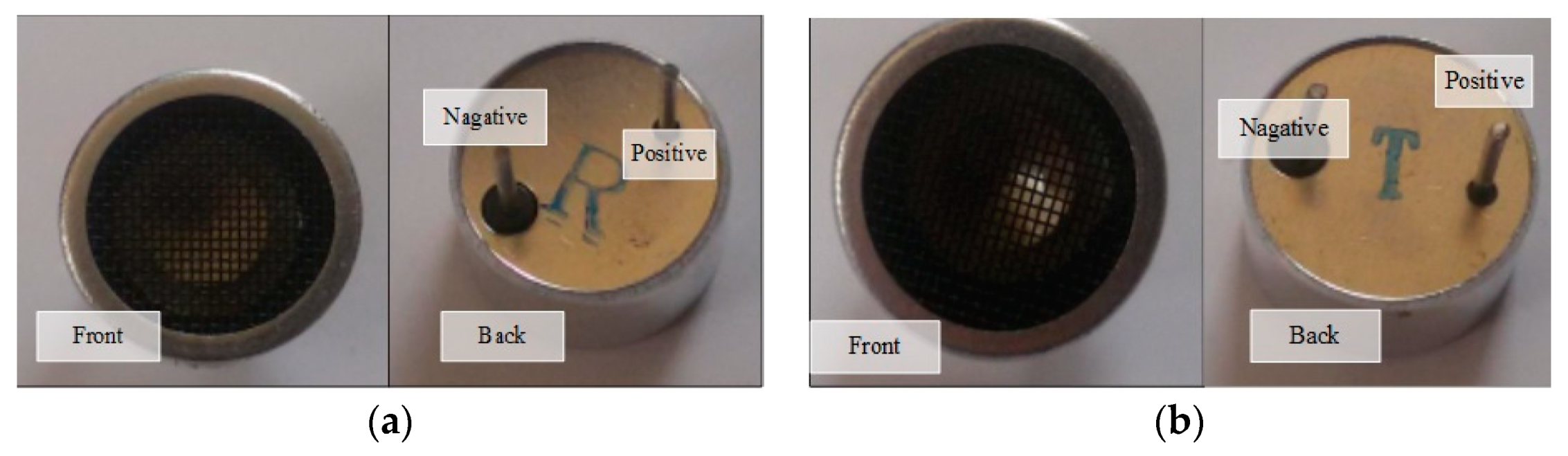
The ultrasonic sensor was a HC-SR04 model. The Tx (45 × 20 × 15 mm
3) converted electrical signals to ultrasound signals; the input voltage was square wave, 10 V
peak-to-peak at 40 KHz from the function generator (model VC2002) (
Figure 2a). The Rx (45 × 20 × 15 mm
3) converted the ultrasound signal to an electrical signal with amplitude and frequency (
Figure 2b) [
18].
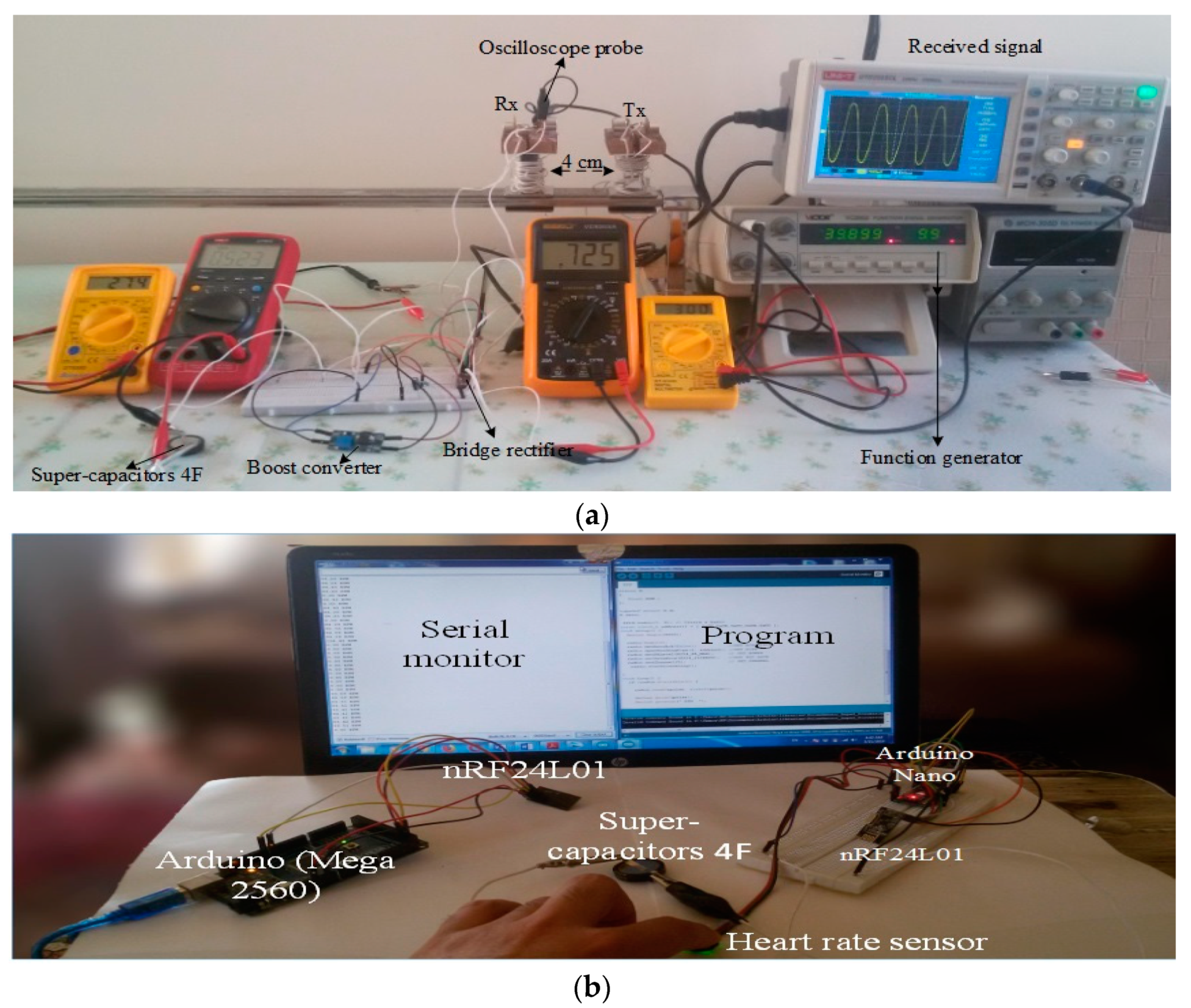
The UPT depended on the distance between the Tx and Rx. The next stage was converting AC to DC voltage using the rectifier (model LTC-3588, 2 × 1.25 cm
2); this model functioned at low voltage. The Rx received the voltage and frequency to attach to the bridge to rectify input elements at piezoelectric 1 and piezoelectric 2. The output voltage was direct from the element at VIN pin. Subsequently, the voltage for that was low, so we used a boost converter to increase the voltage. In the present experiment, we used a DC boost model MT3608, which has up to 93% efficiency. The model is low cost and small, and the board dimensions are 36 × 17 × 14 mm
3 [
19].
The measurement unit supplied power to the Arduino Nano microcontroller by connecting a 4-F capacitor in the input voltage (VIN) and ground (GND) pins. At the same time, the wireless protocol nRF24L01 and heart rate sensor were supplied with 3.3 V power, as shown in
Figure 1. The Arduino Nano and the wireless protocol are based on the processor ATmega 328P (old bootloader). Further, the Arduino Nano in the receiver was selected because it is small, targeted at low-power consumption, lightweight and low cost. In addition, it is programmed with C++ language. The wireless protocol nRF24L01 is low-power consumption, low cost, small and can send data over long distances of up to 100 meters. The board dimensions are 28.5 × 15.2 mm
2. The heart rate sensor was linked at low voltage to decrease power consumption. The monitoring unit was supplied by power via Universal Serial Bus (USB) cable from the laptop to power the Arduino Mega and wireless protocol nRF24L01 [
20].
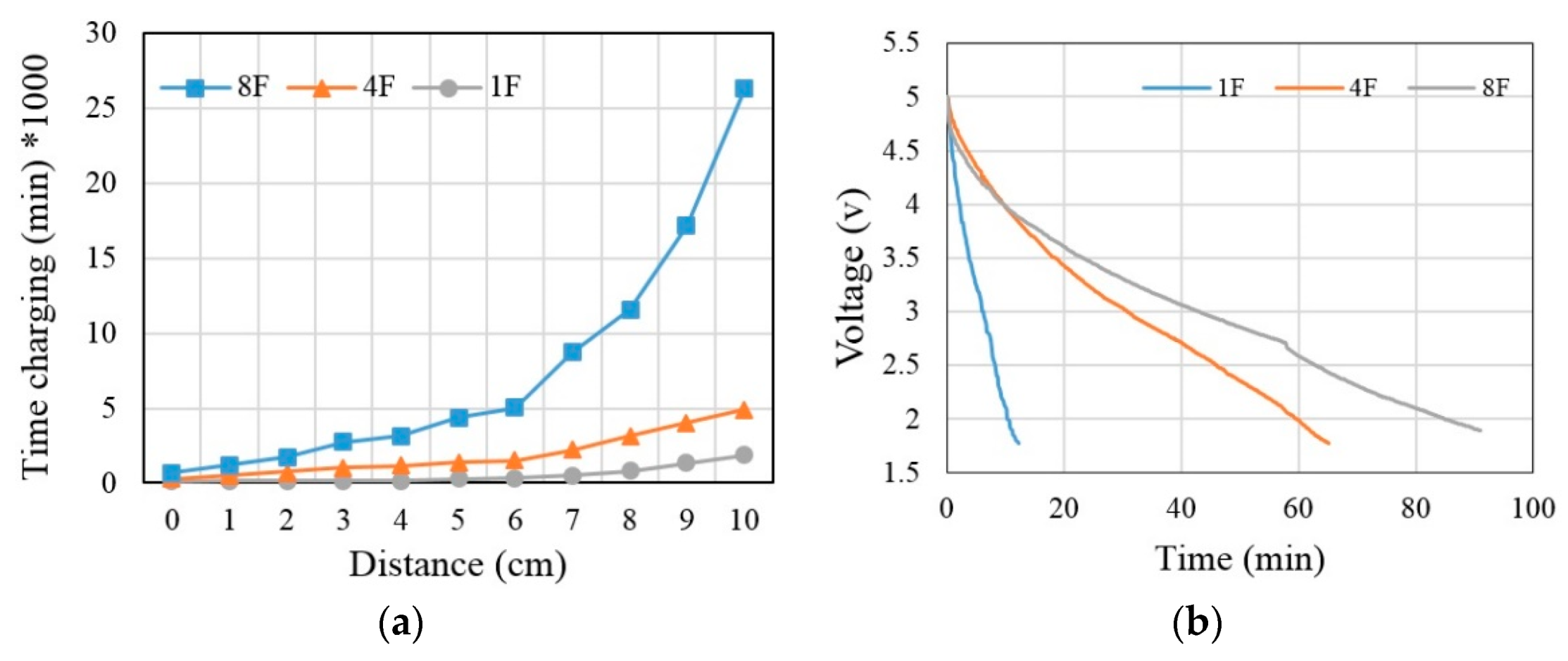
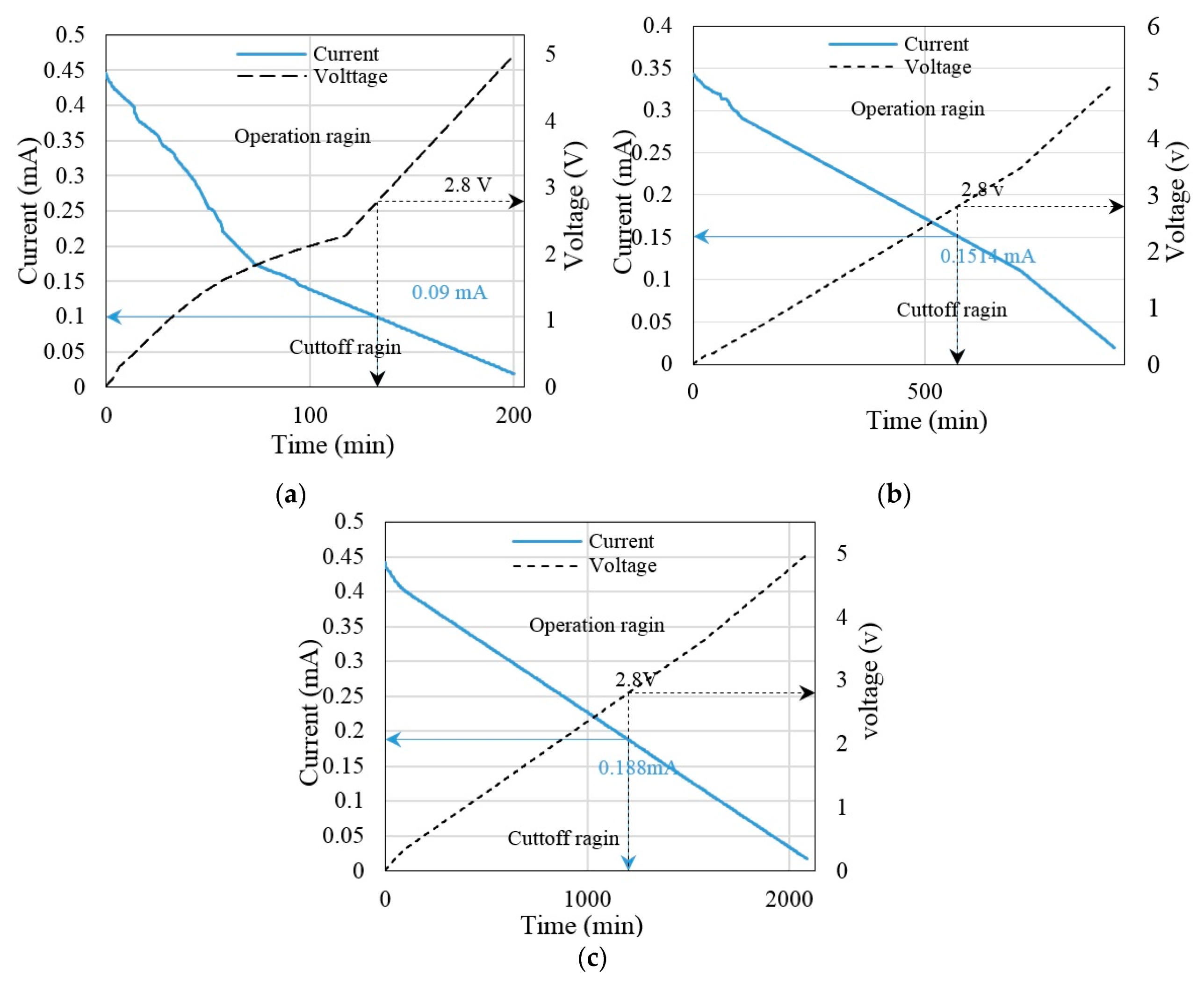
The experiment is designed to transfer energy between the Tx and Rx based on UPT. The experimental distance was 4 cm for charging a 4-F super-capacitor. Capacitors have different charging times, as related to Equations (1)–(3) (
Figure 3a). The function generator supplied the Tx at a voltage with frequency. The Rx detected a voltage with frequency at 4 cm. The Rx wave was displayed in the storage oscilloscope (model UTD2025CL). Next, the rectifier converted AC to DC, followed by DC converter boosting and super-capacitor action. The digital Avometer describes the relationship between voltage and current in the charging input and output. As a voltage increases, the current decreases to charge. The super-capacitor supplied power for the measurement unit containing the HRM. We selected the Arduino Nano and wireless protocol nRF24L01 at the data rate of 9600 bps to improve the transmission time between the wireless protocol and the microcontroller. Furthermore, the monitoring unit in the HRM involving the Arduino Mega 2560 has the same data rate as the monitoring unit.
In addition, the data rate of wireless protocol nRF24L01 was 250 kbps for transferring data between two models, and it was connected at an input voltage of 3.3 V; the chip-enabled activation of Rx or Tx mode (CE) and SPI chip select (SCN) in the microcontroller on digital pin D7 and D8, respectively. Finally, the laptop was used to demonstrate the result of serial monitoring by using Arduino version 1.8.8. Moreover, heart rate sensor was analog to attach with A0 at the microcontroller (
Figure 3b). The heart rate in minutes was calculated using Equation (4) [
21].
where
BPM is beats per minute,
frequency is the sampling frequency and
signal is the input signal to the microcontroller to pin A0.
7. Comparison of Results
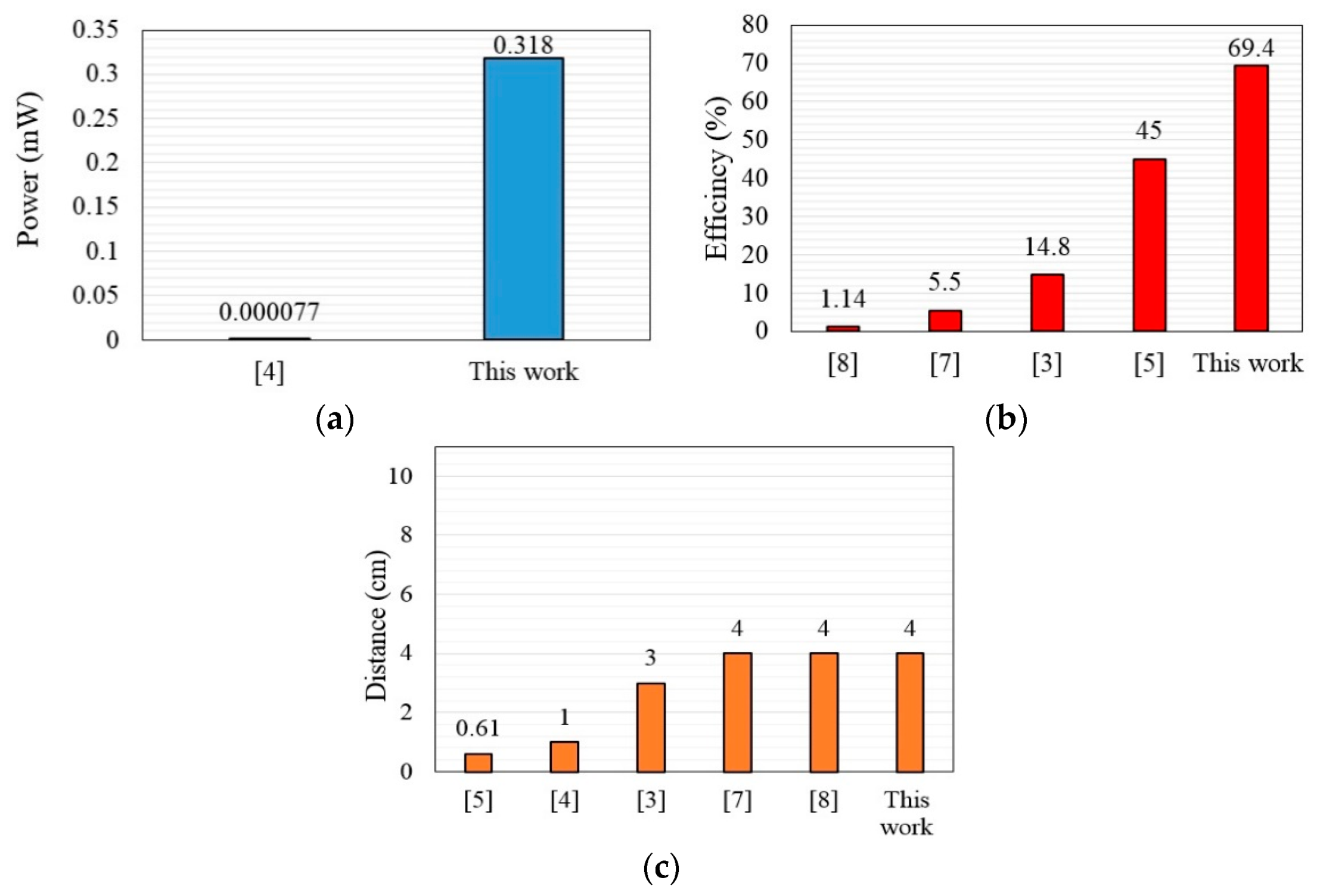
The previous works were clarified based on UPT and transfer powers, efficiencies and distances at different loads. The bar chart compares the performance metrics of the previous studies in terms of transfer power, efficiency and distance with reference to the present study.
Figure 14a shows the transfer power of the references; in the present study, the transfer power was equivalent to 0.318 mW at 4 cm, whereas it was 77 nW in [
4].
Figure 14b reviews the transfer efficiencies of the references; here, we observed high transfer efficiency of 69.4% at 4 cm compared with [
7,
8], which were 5.5% and 1.14%, respectively, at 4 cm. In addition, transfer efficiency was 45% at 0.61 cm in [
5].
Figure 14c shows the distance as compared with the previous works, where we compared our results with those of [
7,
8] based on transfer power and efficiency at 4 cm.
8. Conclusions
This paper introduces the design and implementation of UPT for supplying low-power medical devices such as a heart rate sensor. The UPT system was tested on transfer distances of 1–10 cm with 1-, 4-, and 8-F super-capacitors. These super-capacitors were considered to identify the best capacitor that could yield high transfer efficiency and power relative to the other capacitors’ values. Therefore, the UPT system achieved 69.4% transfer efficiency and 0.318 mW power when a 4-F super-capacitor was adopted at 4-cm gap between the ultrasound transmitter and receiver. Consequently, the obtained transfer power was adequate for supplying power to the HRM at this distance. However, the transfer power and efficiency decreased as the air gap increased to more than 4-cm. In addition, the experiments show that, at different super-capacitor values, the capacitor charging time increased with distance, especially with a high super-capacitor value such as 8-F. Therefore, we recommend using the proposed UPT with an air gap of <4 cm to obtain adequate voltage in a short time. The results disclosed that the resultant transfer power and efficiency at a 4-cm air gap between the UPT transmitter and receiver was superior to that of previous studies.
Moreover, 97% heart rate measurement accuracy was achieved relative to the benchmark device. The heart rate measurements were validated with statistical analysis. Our results show that this work outperforms previous works in terms of transfer power and efficiency with a 4-cm gap between the ultrasound transmitter and receiver. We can draw that this study demonstrated close agreement between the measured data acquired by the proposed HRM and BM. The results show high measurement accuracy and low MAE. Future work will focus on increasing the transfer power, efficiency and distance of the UPT. In addition, a standalone microcontroller can be used to reduce the power consumption of the measurement system.