Antibacterial, Antibiofilm, and Wound Healing Activities of Rutin and Quercetin and Their Interaction with Gentamicin on Excision Wounds in Diabetic Mice
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Chemicals and Bacterial Cultures
2.2. Animals
2.3. Minimum Inhibitory Concentration (In Vitro)
2.4. Antibiofilm Activity (In Vitro)
2.5. Formulation of Rutin and Quercetin Ointment
2.6. Induction of Diabetes
2.7. Antibiofilm Activity In Vivo
3. Results
3.1. Antibacterial Activity
3.2. Antibiofilm Activity
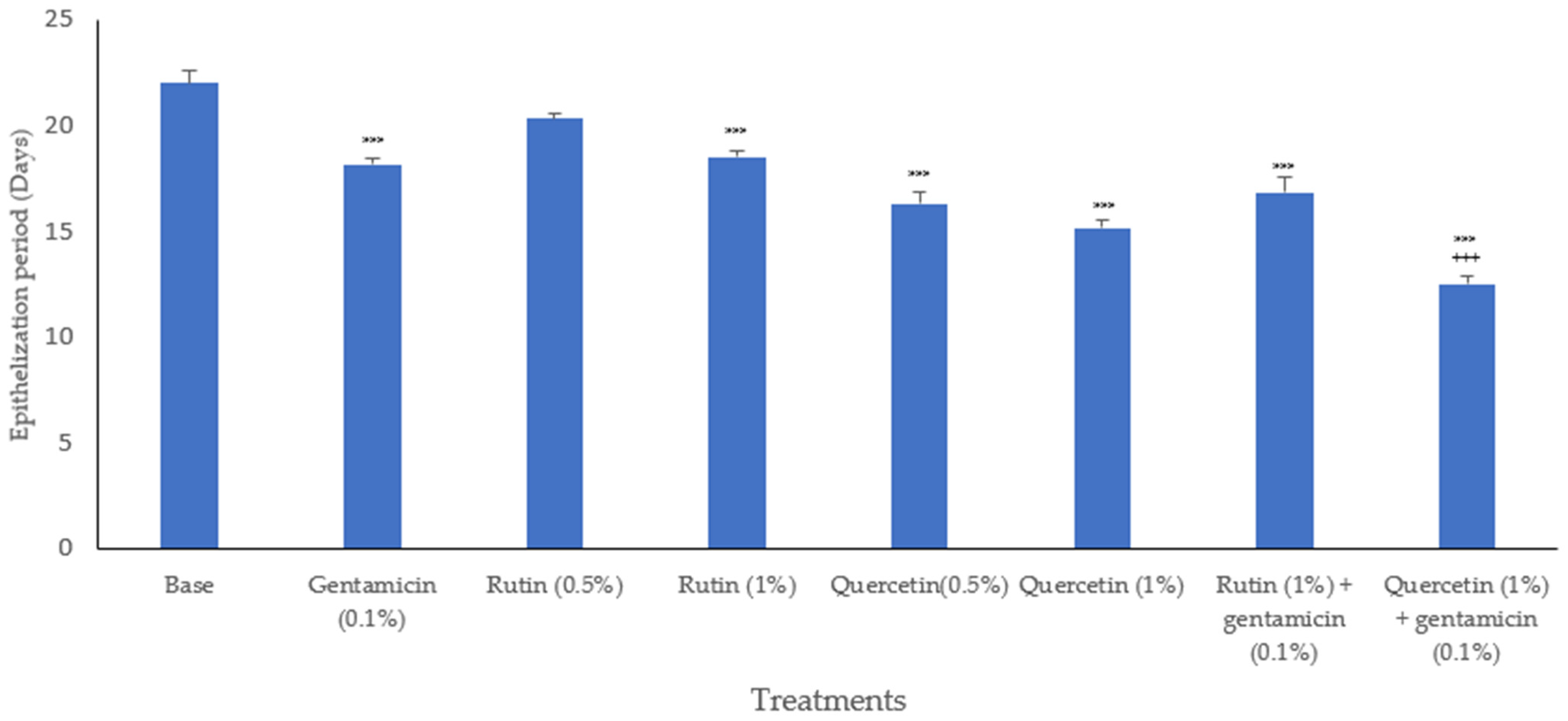
3.3. Epithelization Period
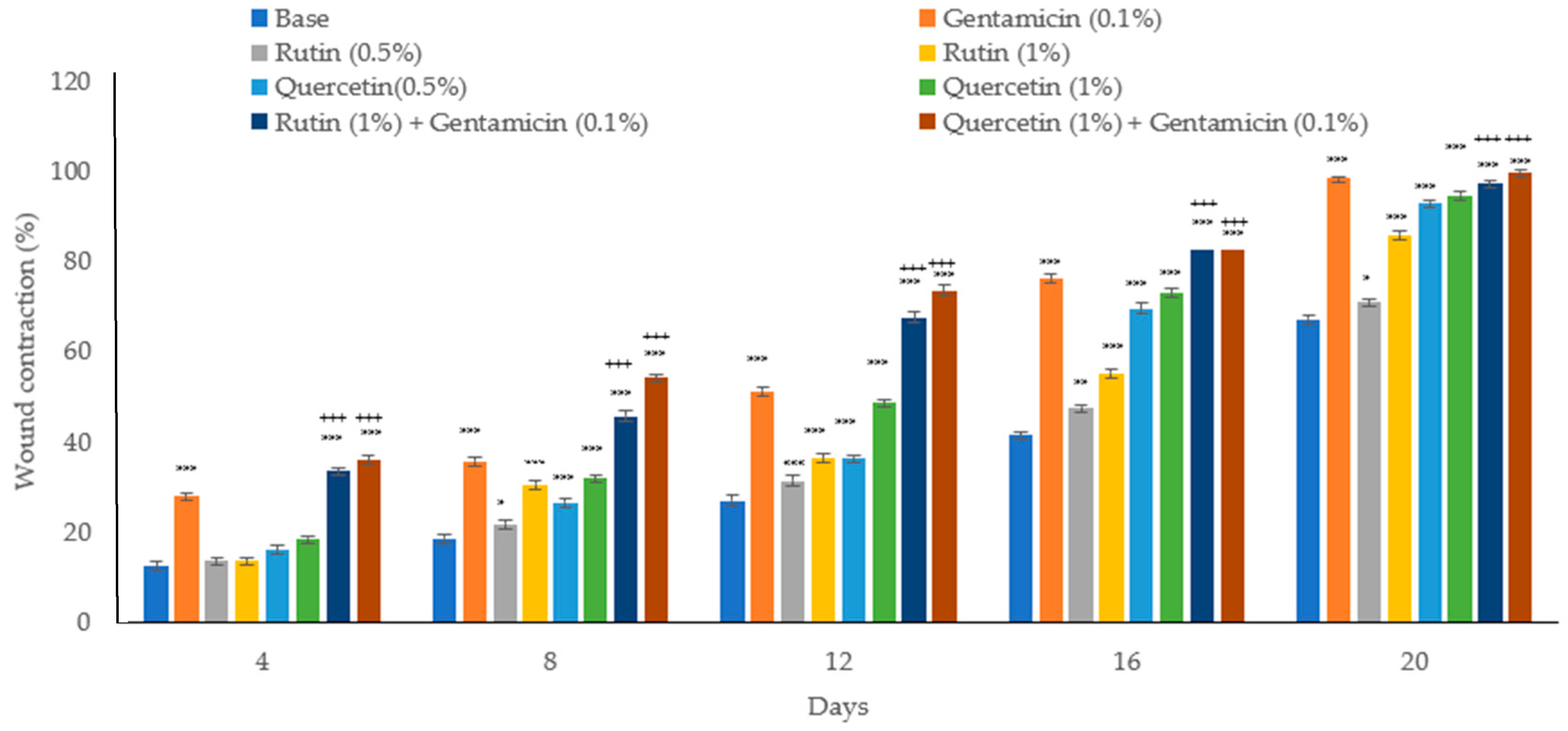
3.4. Wound Healing
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Orfali, R.; Ghaffar, S.; AlAjlan, L.; Perveen, S.; Al-Turki, E.; Ameen, F. Diabetes-related lower limb wounds: Antibiotic susceptibility pattern and biofilm formation. Saudi Pharm. J. 2024, 32, 102069. [Google Scholar] [CrossRef]
- Oguntibeju, O.O. Medicinal plants and their effects on diabetic wound healing. Vet. World 2019, 12, 653–663. [Google Scholar] [CrossRef] [PubMed]
- Falcone, M.; De Angelis, B.; Pea, F.; Scalise, A.; Stefani, S.; Tasinato, R.; Zanetti, O.; Dalla Paola, L. Challenges in the management of chronic wound infections. J. Glob. Antimicrob. Resist. 2021, 26, 140–147. [Google Scholar] [CrossRef]
- Chinemerem Nwobodo, D.; Ugwu, M.C.; Oliseloke Anie, C.; Al-Ouqaili, M.T.S.; Chinedu Ikem, J.; Victor Chigozie, U.; Saki, M. Antibiotic resistance: The challenges and some emerging strategies for tackling a global menace. J. Clin. Lab. Anal. 2022, 36, e24655. [Google Scholar] [CrossRef] [PubMed]
- Al-Ghanayem, A.A.; Alhussaini, M.S.; Asad, M.; Joseph, B. Kaempferol promotes wound-healing in diabetic rats through antibacterial and antioxidant effects, devoid of proliferative action. Biosci. J. 2024, 40, e40015. [Google Scholar] [CrossRef]
- Al-Ghanayem, A.A.; Alhussaini, M.S.; Alyahya, A.A.I.; Asad, M.; Joseph, B. Wound Healing Activity of Chlorogenic Acid in Diabetic Rats is Mediated Through Antibacterial, Antioxidant, Proliferative Effects. Online J. Biol. Sci. 2024, 24, 255–262. [Google Scholar] [CrossRef]
- Yudaev, P.A.; Chistyakov, E.M. Progress in dental materials: Application of natural ingredients. Russ. Chem. Rev. 2024, 93, 5108. [Google Scholar] [CrossRef]
- Rodrigues, C.F.; Kaushik, K.S.; Light, C. Biofilms in Wounds: New Advances in Therapy and in Healing Management. Biomedicines 2021, 9, 193. [Google Scholar] [CrossRef]
- Fik-Jaskółka, M.; Mittova, V.; Motsonelidze, C.; Vakhania, M.; Vicidomini, C.; Roviello, G.N. Antimicrobial Metabolites of Caucasian Medicinal Plants as Alternatives to Antibiotics. Antibiotics 2024, 13, 487. [Google Scholar] [CrossRef]
- Yudaev, P.; Butorova, I.; Chuev, V.; Posokhova, V.; Klyukin, B.; Chistyakov, E. Wound Gel with Antimicrobial Effects Based on Polyvinyl Alcohol and Functional Aryloxycyclotriphosphazene. Polymers 2023, 15, 2831. [Google Scholar] [CrossRef]
- Muvhulawa, N.; Dludla, P.V.; Ziqubu, K.; Mthembu, S.X.H.; Mthiyane, F.; Nkambule, B.B.; Mazibuko-Mbeje, S.E. Rutin ameliorates inflammation and improves metabolic function: A comprehensive analysis of scientific literature. Pharmacol. Res. 2022, 178, 106163. [Google Scholar] [CrossRef]
- Enogieru, A.B.; Haylett, W.; Hiss, D.C.; Bardien, S.; Ekpo, O.E. Rutin as a Potent Antioxidant: Implications for Neurodegenerative Disorders. Oxid. Med. Cell. Longev. 2018, 6241017. [Google Scholar] [CrossRef]
- Deng, L.; Du, C.; Song, P.; Chen, T.; Rui, S.; Armstrong, D.G.; Deng, W. The Role of Oxidative Stress and Antioxidants in Diabetic Wound Healing. Oxid. Med. Cell. Longev. 2021, 8852759. [Google Scholar] [CrossRef] [PubMed]
- Miklasińska-Majdanik, M.; Kępa, M.; Wąsik, T.J.; Zapletal-Pudełko, K.; Klim, M.; Wojtyczka, R.D. The Direction of the Antibacterial Effect of Rutin Hydrate and Amikacin. Antibiotics 2023, 12, 1469. [Google Scholar] [CrossRef]
- Alizadeh, S.R.; Ebrahimzadeh, M.A. Quercetin derivatives: Drug design, development, and biological activities, a review. Eur. J. Med. Chem. 2022, 229, 114068. [Google Scholar] [CrossRef]
- Bhat, I.U.H.; Bhat, R. Quercetin: A Bioactive Compound Imparting Cardiovascular and Neuroprotective Benefits: Scope for Exploring Fresh Produce, Their Wastes, and By-Products. Biology 2021, 10, 586. [Google Scholar] [CrossRef] [PubMed]
- Do Socorro Chagas, M.S.; Behrens, M.D.; Moragas-Tellis, C.J.; Penedo, G.X.M.; Silva, A.R.; Gonçalves-De-Albuquerque, C.F. Flavonols and Flavones as Potential anti-Inflammatory, Antioxidant, and Antibacterial Compounds. Oxid. Med. Cell. Longev. 2022, 9966750. [Google Scholar] [CrossRef]
- Abid, H.M.U.; Hanif, M.; Mahmood, K.; Aziz, M.; Abbas, G.; Latif, H. Wound-Healing and Antibacterial Activity of the Quercetin–4-FormylPhenyl Boronic Acid Complex against Bacterial Pathogens of DiabeticFoot Ulcer. ACS Omega 2022, 7, 24415. [Google Scholar] [CrossRef]
- Li, Y.J.; Wei, S.C.; Chu, H.W.; Jian, H.J.; Anand, A.; Nain, A.; Huang, Y.F.; Chang, H.T.; Huang, C.C.; Lai, J.Y. Poly-quercetin-based nanoVelcro as a multifunctional wound dressing for effective treatment of chronic wound infections. Chem. Eng. J. 2022, 437, 135315. [Google Scholar] [CrossRef]
- Khare, T.; Anand, U.; Dey, A.; Assaraf, Y.G.; Chen, Z.S.; Liu, Z.; Kumar, V. Exploring Phytochemicals for Combating Antibiotic Resistance in Microbial Pathogens. Front. Pharmacol. 2021, 12, 1726. [Google Scholar] [CrossRef]
- Koohsari, H.; Ghaemi, E.A.; Sadegh Sheshpoli, M.; Jahedi, M.; Zahiri, M. The investigation of antibacterial activity of selected native plants from North of Iran. J. Med. Life 2015, 8, 38. [Google Scholar]
- Revision of the ARRIVE Guidelines|NC3Rs. Available online: https://nc3rs.org.uk/our-portfolio/revision-arrive-guidelines (accessed on 3 June 2024).
- Ekom, S.E.; Tamokou, J.D.D.; Kuete, V. Methanol extract from the seeds of Persea americana displays antibacterial and wound healing activities in rat model. J. Ethnopharmacol. 2022, 282, 114573. [Google Scholar] [CrossRef]
- Almutairi, M.B.F.; Alrouji, M.; Almuhanna, Y.; Asad, M.; Joseph, B. In-Vitro and In-Vivo Antibacterial Effects of Frankincense Oil and Its Interaction with Some Antibiotics against Multidrug-Resistant Pathogens. Antibiotics 2022, 11, 1591. [Google Scholar] [CrossRef]
- O’Toole, G.A. Microtiter Dish Biofilm Formation Assay. J. Vis. Exp. 2011, 47, 2437. [Google Scholar]
- Özay, Y.; Güzel, S.; Yumrutaş, Ö.; Pehlivanoğlu, B.; Erdoğdu, İ.H.; Yildirim, Z.; Türk, B.A.; Darcan, S. Wound Healing Effect of Kaempferol in Diabetic and Nondiabetic Rats. J. Surg. Res. 2019, 233, 284–296. [Google Scholar] [CrossRef]
- Nayeem, N.; Mohammed Basheeruddin Asdaq, S.; Alamri, A.S.; Alsanie, W.F.; Alhomrani, M.; Mohzari, Y.; Alrashed, A.A.; Alotaibi, N.; Aalhathal, A.S.; Alharbi, M.A.; et al. Wound healing potential of Dodonaea viscosa extract formulation in experimental animals. J. King Saud Univ. Sci. 2021, 33, 101476. [Google Scholar] [CrossRef]
- Jun, H.W.; Bayoumi, S.M. A Diffusion Model for Studying the Drug Release from Semisolid Dosage Forms I. Methodology Using Agar Gel as Diffusion Medium. Drug Dev. Ind. Pharm. 1986, 12, 899–914. [Google Scholar] [CrossRef]
- Nayeem, N.; Rohini, R.; Asdaq, S.M.; Das, A. Wound healing activity of the hydro alcoholic extract of Ficus religiosa leaves in rats. Internet J. Altern. Med. 2009, 6, 1–5. [Google Scholar]
- Almuhanna, Y.; Alqasmi, M.H.; AlSudais, H.; Alrouji, M.; Kuriri, F.A.; Alissa, M.; Alsuwat, M.A.; Asad, M.; Joseph, B. Effect of Achillea fragrantissima Extract on Excision Wound Biofilms of MRSA and Pseudomonas aeruginosa in Diabetic Mice. Int. J. Mol. Sci. 2023, 24, 9774. [Google Scholar] [CrossRef]
- Al Bahadly, W.K.; Bdioui, A.M.; Al-Gazally, M.E.; Al-Saedi, H.F.; Salah, S.H.; Al-Mahmood, O.A.; Al, W.K. The effect of levofloxacin ointment against imiquimod induced-psoriasis in mice model. Iraqi J. Vet. Sci. 2023, 37, 935–941. [Google Scholar] [CrossRef]
- Yan, L.J. The Nicotinamide/Streptozotocin Rodent Model of Type 2 Diabetes: Renal Pathophysiology and Redox Imbalance Features. Biomolecules 2022, 12, 1225. [Google Scholar] [CrossRef]
- Ghasemi, A.; Jeddi, S. Streptozotocin as a tool for induction of rat models of diabetes: A practical guide. EXCLI J. 2023, 22, 274. [Google Scholar] [PubMed]
- Alrouji, M.; Kuriri, F.A.; Alqasmi, M.H.; AlSudais, H.; Alissa, M.; Alsuwat, M.A.; Asad, M.; Joseph, B.; Almuhanna, Y. A Simple In-Vivo Method for Evaluation of Antibiofilm and Wound Healing Activity Using Excision Wound Model in Diabetic Swiss Albino Mice. Microorganisms 2023, 11, 692. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, M.F.; Hamed, M.I.; Panitch, A.; Seleem, M.N. Targeting Methicillin-Resistant Staphylococcus aureus with Short Salt-Resistant Synthetic Peptides. Antimicrob. Agents Chemother. 2014, 58, 4113. [Google Scholar] [CrossRef] [PubMed]
- Anesthesia (Guideline)|Vertebrate Animal Research. Available online: https://animal.research.uiowa.edu/iacuc-guidelines-anesthesia (accessed on 3 June 2024).
- Agarwal, P.; Singh, A.; Gaurav, K.; Goel, S.; Khanna, H.; Goel, R. Evaluation of wound healing activity of extracts of plantain banana (Musa sapientum var. paradisiaca) in rats. Indian J. Exp. Biol. 2009, 47, 32–40. [Google Scholar]
- Li, J.; Chou, H.; Li, L.; Li, H.; Cui, Z. Wound healing activity of neferine in experimental diabetic rats through the inhibition of inflammatory cytokines and nrf-2 pathway. Artif. Cells Nanomed. Biotechnol. 2020, 48, 96–106. [Google Scholar] [CrossRef] [PubMed]
- Morgan, S.J.; Lippman, S.I.; Bautista, G.E.; Harrison, J.J.; Harding, C.L.; Gallagher, L.A.; Cheng, A.C.; Siehnel, R.; Ravishankar, S.; Usui, M.L.; et al. Bacterial fitness in chronic wounds appears to be mediated by the capacity for high-density growth, not virulence or biofilm functions. PLoS Pathog. 2019, 15, e1007511. [Google Scholar] [CrossRef]
- Ghosh, D.; Mondal, S.; Ramakrishna, K. A topical ointment formulation containing leaves extract of Aegialitis rotundifolia Roxb., accelerates excision, incision and burn wound healing in rats. Wound Med. 2019, 26, 100168. [Google Scholar] [CrossRef]
- Abass, S.; Parveen, R.; Irfan, M.; Malik, Z.; Husain, S.A.; Ahmad, S. Mechanism of antibacterial phytoconstituents: An updated review. Arch. Microbiol. 2024, 206, 325. [Google Scholar] [CrossRef] [PubMed]
- Al Akeel, M.; Al Ghamdi, W.; Al Habib, S.; Koshm, M.; Al Otaibi, F. Herbal medicines: Saudi population knowledge, attitude, and practice at a glance. J. Fam. Med. Prim. Care 2018, 7, 865. [Google Scholar] [CrossRef] [PubMed]
- Gęgotek, A.; Ambrożewicz, E.; Jastrząb, A.; Jarocka-Karpowicz, I.; Skrzydlewska, E. Rutin and ascorbic acid cooperation in antioxidant and antiapoptotic effect on human skin keratinocytes and fibroblasts exposed to UVA and UVB radiation. Arch. Dermatol. Res. 2019, 311, 203–219. [Google Scholar] [CrossRef]
- Beken, B.; Serttas, R.; Yazicioglu, M.; Turkekul, K.; Erdogan, S. Quercetin Improves Inflammation, Oxidative Stress, and Impaired Wound Healing in Atopic Dermatitis Model of Human Keratinocytes. Pediatr. Allergy Immunol. Pulmonol. 2020, 33, 69–79. [Google Scholar] [CrossRef]
- Otake, H.; Mano, Y.; Deguchi, S.; Ogata, F.; Kawasaki, N.; Nagai, N. Effect of Ointment Base on the Skin Wound-Healing Deficits in Streptozotocin-Induced Diabetic Rat. Biol. Pharm. Bull. 2023, 46, 707–712. [Google Scholar] [CrossRef]
- Ademosun, A.O.; Oboh, G.; Bello, F.; Ayeni, P.O. Antioxidative Properties and Effect of Quercetin and Its Glycosylated Form (Rutin) on Acetylcholinesterase and Butyrylcholinesterase Activities. J. Evidence Based Complement. Altern. Med. 2016, 21, NP11–NP17. [Google Scholar] [CrossRef]
- Amin, M.U.; Khurram, M.; Khattak, B.; Khan, J. Antibiotic additive and synergistic action of rutin, morin and quercetin against methicillin resistant Staphylococcus aureus. BMC Complement. Altern. Med. 2015, 15, 59. [Google Scholar] [CrossRef]
- Deepika, M.S.; Thangam, R.; Vijayakumar, T.S.; Sasirekha, R.; Vimala, R.T.V.; Sivasubramanian, S.; Arun, S.; Babu, M.D.; Thirumurugan, R. Antibacterial synergy between rutin and florfenicol enhances therapeutic spectrum against drug resistant Aeromonas hydrophila. Microb. Pathog. 2019, 135, 103612. [Google Scholar] [CrossRef] [PubMed]
- Xia, X.; Song, X.; Li, Y.; Hou, W.; Lv, H.; Li, F.; Li, Y.; Liu, J.; Li, X. Antibacterial and anti-inflammatory ZIF-8@Rutin nanocomposite as an efficient agent for accelerating infected wound healing. Front. Bioeng. Biotechnol. 2022, 10, 1026743. [Google Scholar] [CrossRef]
- Chen, L.Y.; Huang, C.N.; Liao, C.K.; Chang, H.M.; Kuan, Y.H.; Tseng, T.J.; Yen, K.J.; Yang, K.L.; Lin, H.C. Effects of Rutin on Wound Healing in Hyperglycemic Rats. Antioxidants 2020, 9, 1122. [Google Scholar] [CrossRef]
- Gopalakrishnan, A.; Ram, M.; Kumawat, S.; Tandan, S.K.; Kumar, D. Quercetin accelerated cutaneous wound healing in rats by increasing levels of VEGF and TGF-β1. Indian J. Exp. Biol. 2016, 54, 187–195. [Google Scholar]
- Liu, Y.; Dai, E.; Yang, J. Quercetin suppresses glomerulosclerosis and TGF-β signaling in a rat model. Mol. Med. Rep. 2019, 19, 4589. [Google Scholar] [CrossRef]
- Mi, Y.; Zhong, L.; Lu, S.; Hu, P.; Pan, Y.; Ma, X.; Yan, B.; Wei, Z.; Yang, G. Quercetin promotes cutaneous wound healing in mice through Wnt/β-catenin signaling pathway. J. Ethnopharmacol. 2022, 290, 115066. [Google Scholar] [CrossRef] [PubMed]
- Manach, C.; Morand, C.; Demigné, C.; Texier, O.; Régérat, F.; Rémésy, C. Bioavailability of rutin and quercetin in rats. FEBS Lett. 1997, 409, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.L.A.; Bhattacharya, D. Antimicrobial Activity of Quercetin: An Approach to Its Mechanistic Principle. Molecules 2022, 27, 2494. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.; Wang, T.; Long, M.; Li, P. Quercetin: Its Main Pharmacological Activity and Potential Application in Clinical Medicine. Oxid. Med. Cell. Longev. 2020, 8825387. [Google Scholar] [CrossRef] [PubMed]
- Lovering, A.M.; Reeves, D.S. Aminoglycosides and aminocyclitols. Antibiot. Chemother. Expert Consult. 2010, 145–169. [Google Scholar]


| Antibacterial Activity | |||
|---|---|---|---|
| MIC (µg/mL) | MBC (µg/mL) | FIC Index | |
| Rutin | 512 | 1024 | 1.5003 * |
| Quercetin | 256 | 512 | 1.5017 * |
| Gentamicin | 2 | 4 | |
| Parameter | Rutin | Quercetin |
|---|---|---|
| Color | Slightly yellowish | Dark yellowish |
| Odor | Odorless | Odorless |
| Taste | Bitter | Bitter |
| Spreadability (s) | 13 s | 10 s |
| Diffusion | 0.6 cm | 0.8 cm |
| Stability | Stable at 40 °C, 24 °C and 37 °C | Stable at 40 °C, 24 °C and 37 °C |
| Washability | Satisfactory | Satisfactory |
| Homogeneity | Good | Good |
| Treatment | Log10 CFU/g of Tissue |
|---|---|
| Base | 5.981 ± 0.529 |
| Gentamicin (0.1%) | 1.254 ± 0.247 *** |
| Rutin (0.5%) | 5.987 ± 0.697 |
| Rutin (1%) | 4.987 ± 0.784 * |
| Quercetin (0.5%) | 4.254 ± 0.248 * |
| Quercetin (1%) | 2.954 ± 0.541 *** |
| Rutin (1%) + Gentamicin (0.1%) | 0.885 ± 0.028 |
| Quercetin (1%) + Gentamicin (0.1%) | 0.623 ± 0.035 + |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Almuhanna, Y.; Alshalani, A.; AlSudais, H.; Alanazi, F.; Alissa, M.; Asad, M.; Joseph, B. Antibacterial, Antibiofilm, and Wound Healing Activities of Rutin and Quercetin and Their Interaction with Gentamicin on Excision Wounds in Diabetic Mice. Biology 2024, 13, 676. https://doi.org/10.3390/biology13090676
Almuhanna Y, Alshalani A, AlSudais H, Alanazi F, Alissa M, Asad M, Joseph B. Antibacterial, Antibiofilm, and Wound Healing Activities of Rutin and Quercetin and Their Interaction with Gentamicin on Excision Wounds in Diabetic Mice. Biology. 2024; 13(9):676. https://doi.org/10.3390/biology13090676
Chicago/Turabian StyleAlmuhanna, Yasir, Abdulrahman Alshalani, Hamood AlSudais, Fuad Alanazi, Mohammed Alissa, Mohammed Asad, and Babu Joseph. 2024. "Antibacterial, Antibiofilm, and Wound Healing Activities of Rutin and Quercetin and Their Interaction with Gentamicin on Excision Wounds in Diabetic Mice" Biology 13, no. 9: 676. https://doi.org/10.3390/biology13090676
APA StyleAlmuhanna, Y., Alshalani, A., AlSudais, H., Alanazi, F., Alissa, M., Asad, M., & Joseph, B. (2024). Antibacterial, Antibiofilm, and Wound Healing Activities of Rutin and Quercetin and Their Interaction with Gentamicin on Excision Wounds in Diabetic Mice. Biology, 13(9), 676. https://doi.org/10.3390/biology13090676







