Development and Validation of a Predictive Tool for Postpartum Hemorrhage after Vaginal Delivery: A Prospective Cohort Study
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
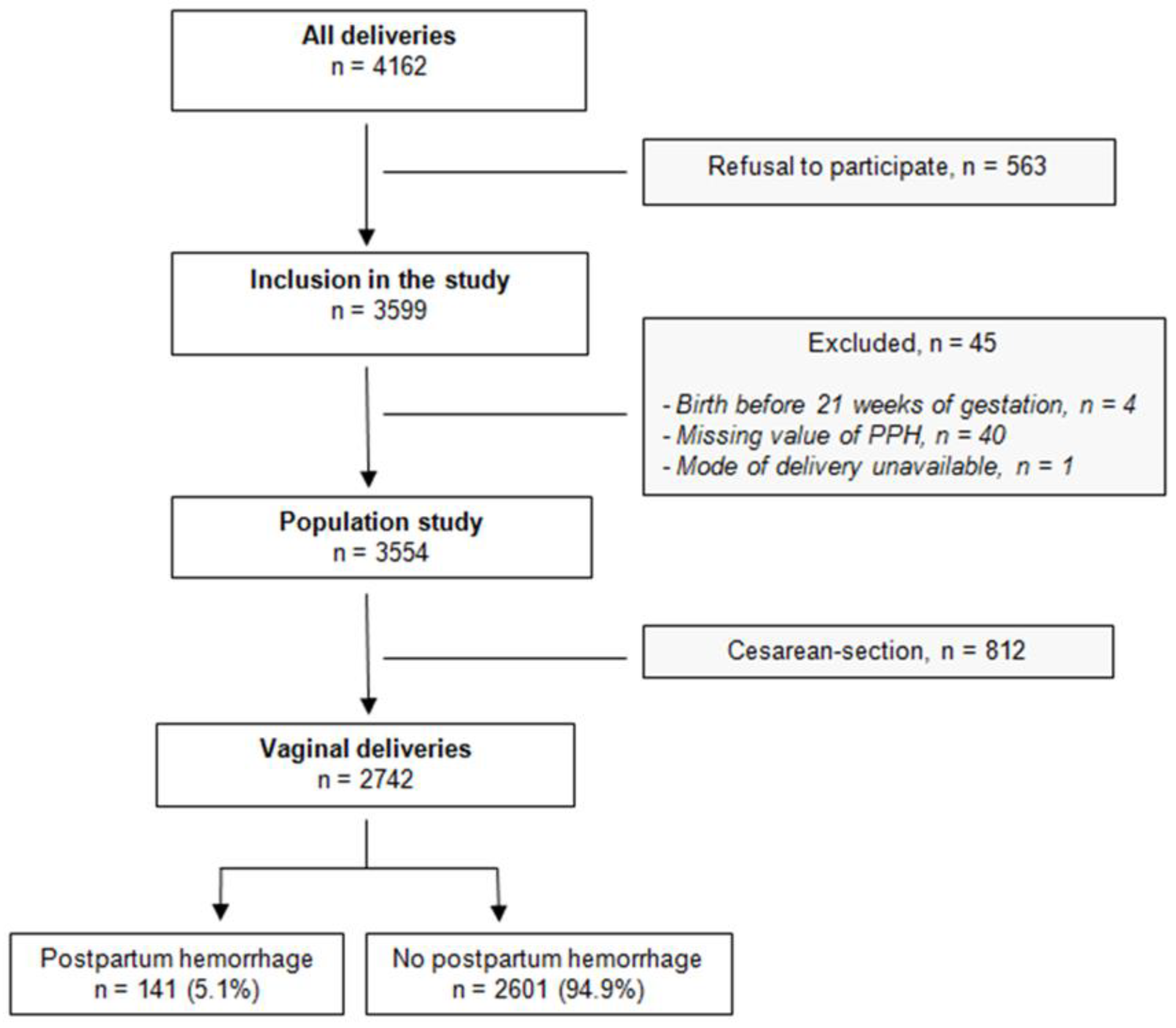
2.1. Study Design and Participants
2.2. Data Collection
2.3. Statistical Analysis
2.3.1. Description
2.3.2. Combination of Multiple Imputation and Variable Selection with Bootstrap
2.3.3. Predictive Model, Score and External Validation
3. Results
3.1. Descriptive Analysis
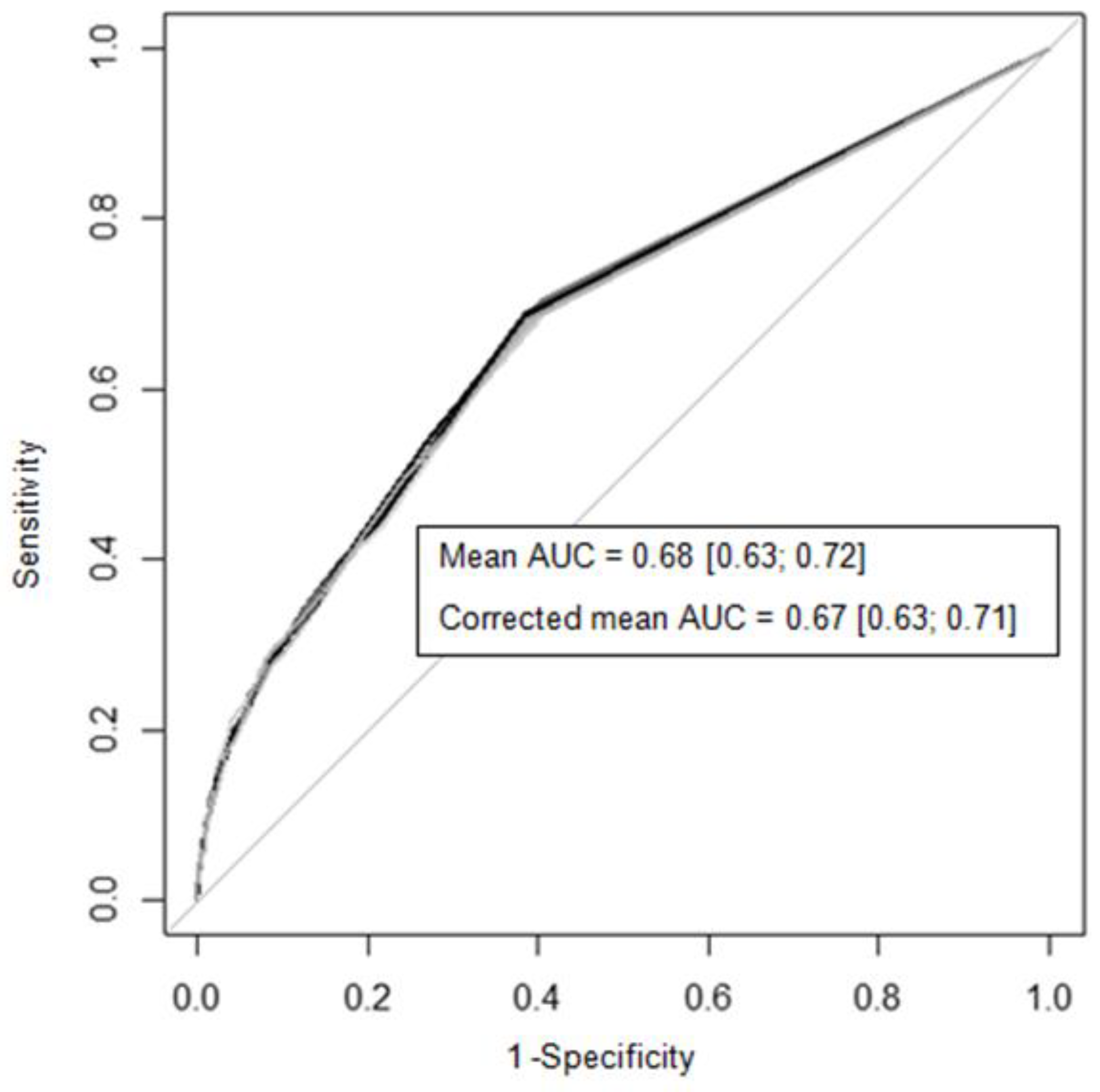
3.2. Predictive Model
3.3. Predictive Score
3.4. External Validation
4. Discussion
4.1. Main Findings
4.2. Strengths and Limitations
4.3. Interpretation
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Morau, E.; Ducloy, J.C.; Le Roux, S.; Weber, P.; Dreyfus, M. Maternal deaths due to haemorrhage: Results from the French confidential enquiry into maternal deaths, 2010–2012. Gynecol. Obstet. Fertil. Senol. 2017, 45, S24–S30. [Google Scholar] [PubMed]
- Biguzzi, E.; Franchi, F.; Ambrogi, F.; Ibrahim, B.; Bucciarelli, P.; Acaia, B.; Radaelli, T.; Biganzoli, E.; Mannucci, P.M. Risk factors for postpartum hemorrhage in a cohort of 6011 Italian women. Thromb. Res. 2012, 129, e1–e7. [Google Scholar] [CrossRef] [PubMed]
- Koopmans, C.M.; Van der Tuuk, K.; Groen, H.; Doornbos, J.P.; De Graaf, I.M.; Van Der Salm, P.C.; Porath, M.M.; Kuppens, S.M.; Wijnen, E.J.; Aardenburg, R.; et al. Prediction of postpartum hemorrhage in women with gestational hypertension or mild preeclampsia at term. Acta Obstet. Gynecol. Scand. 2014, 93, 399–407. [Google Scholar] [CrossRef] [PubMed]
- Rubio-Álvarez, A.; Molina-Alarcón, M.; Arias-Arias, Á.; Hernández-Martínez, A. Development and validation of a predictive model for excessive postpartum blood loss: A retrospective, cohort study. Int. J. Nurs. Stud. 2018, 79, 114–121. [Google Scholar] [CrossRef]
- Neary, C.; Naheed, S.; McLernon, D.J.; Black, M. Predicting risk of postpartum haemorrhage: A systematic review. BJOG: Int. J. Obstet. Gynaecol. 2021, 128, 46–53. [Google Scholar] [CrossRef]
- Salomon, C.; de Moreuil, C.; Hannigsberg, J.; Trémouilhac, C.; Drugmanne, G.; Gatineau, F.; Nowak, E.; Anouilh, F.; Briend, D.; Le Moigne, E.; et al. Haematological parameters associated with postpartum haemorrhage after vaginal delivery: Results from a French cohort study. J. Gynecol. Obstet. Hum. Reprod. 2021, 50, 102168. [Google Scholar] [CrossRef]
- Heymans, M.W.; van Buuren, S.; Knol, D.L.; van Mechelen, W.; de Vet, H.C.W. Variable selection under multiple imputation using the bootstrap in a prognostic study. BMC Med. Res. Methodol. 2007, 7, 33. [Google Scholar] [CrossRef]
- WHO. Recommendations for the Prevention and Treatment of Postpartum Haemorrhage; WHO Guidelines Approved by the Guidelines Review Committee; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- Institute of Medicine (US) and National Research Council (US) Committee to Reexamine IOM Pregnancy Weight Guidelines. In Weight Gain During Pregnancy: Reexamining the Guidelines; The National Academies Collection: Reports funded by National Institutes of Health; Rasmussen, K.M., Yaktine, A.L., Eds.; National Academies Press: Washington, DC, USA, 2009. [Google Scholar]
- Van Buuren, S.; Groothuis-Oudshoorn, K. mice: Multivariate imputation by chained equations in R. J. Stat. Softw. 2011, 45, 1–67. [Google Scholar] [CrossRef]
- Rubin, D.B. Multiple Imputation for Nonresponse in Surveys; John Wiley & Sons: Hoboken, NJ, USA, 2004; Volume 81. [Google Scholar]
- Cox, D. Two further applications of a model for binary regression. Biometrika 1958, 45, 562–565. [Google Scholar] [CrossRef]
- Miller, M.E.; Langefeld, C.D.; Tierney, W.M.; Hui, S.L.; McDonald, C.J. Validation of probabilistic predictions. Med. Decis. Mak. 1993, 13, 49–58. [Google Scholar] [CrossRef]
- Austin, P.C.; Tu, J.V. Bootstrap methods for developing predictive models. Am. Stat. 2004, 58, 131–137. [Google Scholar] [CrossRef]
- Dupont, C.; Rudigoz, R.C.; Cortet, M.; Touzet, S.; Colin, C.; Rabilloud, M.; Lansac, J.; Harvey, T.; Tessier, V.; Chauleur, C.; et al. Frequency, causes and risk factors of postpartum haemorrhage: A population-based study in 106 French maternity units. J. Gynecol. Obstet. Biol. Reprod. 2014, 43, 244–253. [Google Scholar] [CrossRef]
- Venkatesh, K.K.; Strauss, R.A.; Grotegut, C.A.; Heine, R.P.; Chescheir, N.C.; Stringer, J.S.A.; Stamilio, D.M.; Menard, K.M.; Jelovsek, J.E. Machine Learning and Statistical Models to Predict Postpartum Hemorrhage. Obstet. Gynecol. 2020, 135, 935–944. [Google Scholar] [CrossRef] [PubMed]
- Goad, L.; Rockhill, K.; Schwarz, J.; Heyborne, K.; Fabbri, S. Development and validation of a prediction model for postpartum hemorrhage at a single safety net tertiary care center. Am. J. Obstet. Gynecol. MFM 2021, 3, 100404. [Google Scholar] [CrossRef] [PubMed]
- Akazawa, M.; Hashimoto, K.; Katsuhiko, N.; Kaname, Y. Machine learning approach for the prediction of postpartum hemorrhage in vaginal birth. Sci. Rep. 2021, 11, 22620. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Xu, Y.; Li, J.; Guan, Z.; Liu, C.; He, F. Development and validation of a predictive model for severe postpartum hemorrhage in women undergoing vaginal delivery: A retrospective cohort study. Int. J. Gynaecol. Obstet. 2022, 157, 353–358. [Google Scholar] [CrossRef]
- Zheutlin, A.B.; Vieira, L.; Shewcraft, R.A.; Li, S.; Wang, Z.; Schadt, E.; Gross, S.; Dolan, S.M.; Stone, J.; Schadt, E.; et al. Improving postpartum hemorrhage risk prediction using longitudinal electronic medical records. J. Am. Med. Inform. Assoc. 2022, 29, 296–305. [Google Scholar] [CrossRef]
- Colalillo, E.L.; Sparks, A.D.; Phillips, J.M.; Onyilofor, C.L.; Ahmadzia, H.K. Obstetric hemorrhage risk assessment tool predicts composite maternal morbidity. Sci. Rep. 2021, 11, 14709. [Google Scholar] [CrossRef]
- Hussain, S.A.; Guarini, C.B.; Blosser, C.; Poole, A.T. Obstetric Hemorrhage Outcomes by Intrapartum Risk Stratification at a Single Tertiary Care Center. Cureus 2019, 11, e6456. [Google Scholar] [CrossRef]
- Dilla, A.J.; Waters, J.H.; Yazer, M.H. Clinical validation of risk stratification criteria for peripartum hemorrhage. Obstet. Gynecol. 2013, 122, 120–126. [Google Scholar] [CrossRef]
- Deneux- Tharaux, C.; Bonnet, M.-P.; Tort, J. Epidemiology of post-partum haemorrhage. J. Gynecol. Obstet. Biol. Reprod. 2014, 43, 936–950. [Google Scholar] [CrossRef] [PubMed]
- Sosa, C.G.; Althabe, F.; Belizán, J.M.; Buekens, P. Risk factors for postpartum hemorrhage in vaginal deliveries in a Latin-American population. Obstet. Gynecol. 2009, 113, 1313–1319. [Google Scholar] [CrossRef] [PubMed]
- Reese, J.A.; Peck, J.D.; Deschamps, D.R.; McIntosh, J.J.; Knudtson, E.J.; Terrell, D.R.; Vesely, S.K.; George, J.N. Platelet Counts during Pregnancy. N. Engl. J. Med. 2018, 379, 32–43. [Google Scholar] [CrossRef] [PubMed]
- Govindappagari, S.; Moyle, K.; Burwick, R.M. Mild thrombocytopenia and postpartum hemorrhage in nulliparous women with term singleton, vertex deliveries. Obstet. Gynecol. 2020, 135, 1338–1344. [Google Scholar] [CrossRef]
- Durán-Nah, J.J.; Sosa-Ek, M.V.; Chacón-Hernández, L. Hemostatic profile in patients with and without postpartum hemorrhage. Rev. Med. Inst. Mex. Seguro Soc. 2019, 56, 517–524. [Google Scholar]
- Shakur, H.; Roberts, I.; Fawole, B.; Chaudhri, R.; El-Sheikh, M.; Akintan, A.; Qureshi, Z.; Kidanto, H.; Vwalika, B.; Abdulkadir, A.; et al. Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with post-partum haemorrhage (WOMAN): An international, randomised, double-blind, placebo-controlled trial. Lancet 2017, 389, 2105–2116. [Google Scholar] [CrossRef]
- Sentilhes, L.; Winer, N.; Azria, E.; Senat, M.V.; Le Ray, C.; Vardon, D.; Perrotin, F.; Desbrière, R.; Fuchs, F.; Kayem, G.; et al. Tranexamic Acid for the Prevention of Blood Loss after Vaginal Delivery. N. Engl. J. Med. 2018, 379, 731–742. [Google Scholar] [CrossRef]
| Variables | Overall * (n = 2742) | No PPH * (n = 2601) | PPH * (n = 141) |
|---|---|---|---|
| Maternal characteristics | |||
| Age (years) | 30.0 (26.0, 33.0) | 30.0 (26.0, 33.0) | 31.0 (26.0, 34.0) |
| Age < 35 years | 2229 (81.3%) | 2123 (81.6%) | 106 (75.2%) |
| Age ≥ 35 years | 513 (18.7%) | 478 (18.4%) | 35 (24.8%) |
| Body mass index (kg/m2) | 22.1 (20.1, 25.7) | 22.1 (20.1, 25.6) | 22.9 (20.1, 27.3) |
| Underweight | 230 (8.4%) | 221 (8.5%) | 9 (6.4%) |
| Normal | 1729 (63.2%) | 1645 (63.4%) | 84 (59.6%) |
| Overweight | 483 (17.7%) | 460 (17.7%) | 23 (16.3%) |
| Obese | 293 (10.7%) | 268 (10.3%) | 25 (17.7%) |
| Ethnicity | |||
| Europe | 2221 (88.1%) | 2112 (88.5%) | 109 (82.0%) |
| Africa | 150 (6.0%) | 143 (6.0%) | 7 (5.3%) |
| Asia | 24 (1.0%) | 21 (0.9%) | 3 (2.3%) |
| Overseas departments and territories | 81 (3.2%) | 71 (3.0%) | 10 (7.5%) |
| Others | 44 (1.7%) | 40 (1.7%) | 4 (3.0%) |
| Medical history | |||
| Bleeding history | 38 (1.4%) | 35 (1.3%) | 3 (2.1%) |
| Cardiac disease | 31 (1.1%) | 29 (1.1%) | 2 (1.4%) |
| Arterial disease | 6 (0.2%) | 5 (0.2%) | 1 (0.7%) |
| Diabetes mellitus | 18 (0.7%) | 17 (0.7%) | 1 (0.7%) |
| Infectious disease | 262 (9.6%) | 254 (9.8%) | 8 (5.7%) |
| Venous thromboembolism | 37 (1.4%) | 35 (1.3%) | 2 (1.4%) |
| Nephrological disease | 24 (0.9%) | 22 (0.8%) | 2 (1.4%) |
| Transfusion history | 60 (2.2%) | 55 (2.1%) | 5 (3.5%) |
| Autoimmune disease | 31 (1.1%) | 28 (1.1%) | 3 (2.1%) |
| Gynecological history | |||
| Bleeding history | 18 (0.7%) | 17 (0.7%) | 1 (0.7%) |
| Uterine myoma | 12 (0.4%) | 10 (0.4%) | 2 (1.4%) |
| Obstetric history | |||
| Previous C-section ** | 155 (9.6%) | 143 (9.3%) | 12 (16.7%) |
| Previous PPH ** | 64 (4.0%) | 57 (3.7%) | 7 (9.7%) |
| Ongoing pregnancy | |||
| Assisted reproductive technology | 125 (4.6%) | 109 (4.2%) | 16 (11.4%) |
| Multiple pregnancy | 63 (2.3%) | 53 (2.0%) | 10 (7.1%) |
| Parity | |||
| 0 | 1130 (41.2%) | 1061 (40.8%) | 69 (48.9%) |
| 1 or 2 | 1417 (51.7%) | 1356 (52.1%) | 61 (43.3%) |
| ≥3 | 195 (7.1%) | 184 (7.1%) | 11 (7.8%) |
| Weight gain | |||
| Adequate | 862 (33.7%) | 823 (33.9%) | 39 (30.5%) |
| Excessive | 906 (35.4%) | 849 (35.0%) | 57 (44.5%) |
| Insufficient | 789 (30.9%) | 757 (31.2%) | 32 (25.0%) |
| Smoking during pregnancy | 677 (24.8%) | 648 (25.0%) | 29 (20.7%) |
| Alcohol during pregnancy | 37 (1.4%) | 35 (1.4%) | 2 (1.4%) |
| Placenta previa, accreta, percreta | 53 (1.9%) | 47 (1.8%) | 6 (4.3%) |
| Pathological outcomes during pregnancy | |||
| Gestational hypertension | 17 (0.6%) | 15 (0.6%) | 2 (1.4%) |
| Pre-eclampsia | 27 (1.0%) | 20 (0.8%) | 7 (5.0%) |
| Gestational diabetes | 310 (11.3%) | 289 (11.1%) | 21 (14.9%) |
| Premature delivery threat | 160 (5.8%) | 151 (5.8%) | 9 (6.4%) |
| Antepartum bleeding | 198 (7.2%) | 176 (6.8%) | 22 (15.6%) |
| Intrauterine growth restriction | 25 (0.9%) | 24 (0.9%) | 1 (0.7%) |
| Premature rupture of membranes | 67 (2.4%) | 66 (2.5%) | 1 (0.7%) |
| Hydramnios | 12 (0.4%) | 11 (0.4%) | 1 (0.7%) |
| Intrahepatic cholestasis | 32 (1.2%) | 29 (1.1%) | 3 (2.1%) |
| Treatments during pregnancy | |||
| Anticoagulants | 60 (2.2%) | 58 (2.2%) | 2 (1.4%) |
| Antiplatelets | 63 (2.3%) | 59 (2.3%) | 4 (2.8%) |
| Anti-inflammatory drugs | 27 (1.0%) | 23 (0.9%) | 4 (2.8%) |
| Psychiatric drugs | 22 (0.8%) | 21 (0.8%) | 1 (0.7%) |
| Labor | |||
| Labor induction | 713 (26.0%) | 661 (25.4%) | 52 (36.9%) |
| Anesthesia | |||
| None | 421 (15.4%) | 406 (15.6%) | 15 (10.9%) |
| Epidural | 2294 (83.9%) | 2174 (83.7%) | 120 (87.6%) |
| Spinal or general anesthesia | 18 (0.7%) | 16 (0.6%) | 2 (1.5%) |
| Total labor duration (hours) | 5.00 (3.00, 7.00) | 5.00 (3.00, 6.54) | 6.00 (4.00, 8.00) |
| Second stage of labor duration (minutes) | 41 (15–102) | 40 (15–101) | 67 (20–110) |
| Delivery | |||
| Temperature > 38 °C | 6 (0.3%) | 5 (0.2%) | 1 (0.9%) |
| Macrosomia *** | 189 (6.9%) | 171 (6.6%) | 18 (12.8%) |
| Instrumental birth | 507 (18.5%) | 474 (18.2%) | 33 (23.4%) |
| Term of delivery (weeks of gestation) | |||
| <37 | 250 (9.1%) | 237 (9.1%) | 13 (9.2%) |
| (37; 41) | 2194 (80.1%) | 2093 (80.6%) | 101 (71.6%) |
| >41 | 295 (10.8%) | 268 (10.3%) | 27 (19.1%) |
| Vaginal lacerations | 1043 (38.1%) | 997 (38.4%) | 46 (32.6%) |
| Episiotomy | 762 (27.8%) | 697 (26.8%) | 65 (46.1%) |
| Retained placenta | 226 (8.2%) | 151 (5.8%) | 75 (53.2%) |
| Biological parameters at admission in the delivery room | |||
| Blood group O | 1244 (45.4%) | 1179 (45.3%) | 65 (46.1%) |
| Hemoglobin (g/dL) | 12.30 (11.50, 13.00) | 12.30 (11.50, 13.00) | 12.20 (11.30, 12.85) |
| Hematocrit (%) | 36.10 (34.30, 37.90) | 36.10 (34.30, 37.90) | 35.70 (34.00, 37.80) |
| Platelets (Giga/L) | 229 (194, 273) | 230 (195, 274) | 210 (174, 252) |
| Prothrombin time (%) | 100.0 (94.0, 100.0) | 100.0 (94.0, 100.0) | 98.0 (92.0, 100.0) |
| aPTT ratio | 1.00 (0.94, 1.06) | 1.00 (0.94, 1.06) | 1.01 (0.96, 1.07) |
| Fibrinogen (g/L) | 5.08 (4.57, 5.68) | 5.09 (4.58, 5.68) | 4.89 (4.43, 5.60) |
| D-Dimers (µg/mL) | 1.58 (1.15, 2.12) | 1.57 (1.14, 2.11) | 1.87 (1.31, 2.34) |
| Fibrin monomers (µg/mL) | 5 (4, 8) | 5 (4, 8) | 6 (4, 8) |
| Immature platelet fraction (%) | 5.0 (3.3, 7.5) | 5.0 (3.3, 7.5) | 5.2 (3.3, 8.0) |
| Mean corpuscular volume (fL) | 87.2 (83.8, 90.4) | 87.3 (83.8, 90.4) | 86.7 (83.4, 90.2) |
| White blood cells (G/L) | 11.2 (9.4, 13.6) | 11.3 (9.4, 13.6) | 10.7 (9.0, 12.6) |
| Neutrophils (G/L) | 8.16 (6.48, 10.24) | 8.18 (6.49, 10.25) | 7.43 (6.11, 9.70) |
| Lymphocytes (G/L) | 2.03 (1.64, 2.49) | 2.04 (1.64, 2.49) | 1.85 (1.56, 2.36) |
| Monocytes (G/L) | 0.79 (0.64, 0.97) | 0.79 (0.64, 0.97) | 0.75 (0.60, 0.92) |
| Variable | Adjusted OR | 95% CI | p-Value * |
|---|---|---|---|
| Clinical parameters | |||
| Pre-eclampsia | 6.41 | [2.47–16.65] | <0.001 |
| Antepartum bleeding | 2.50 | [1.52–4.11] | <0.001 |
| Multiple pregnancy | 3.15 | [1.49–6.65] | 0.003 |
| Labor duration ≥ 8 h | 2.30 | [1.56–3.38] | <0.001 |
| Macrosomia ** | 2.33 | [1.36–3.99] | 0.002 |
| Biological parameters | |||
| Platelets < 150 Giga/L | 2.45 | [1.40–4.30] | 0.002 |
| aPTT ratio ≥ 1.1 | 1.96 | [1.22–3.13] | 0.005 |
| Characteristics | Coefficients * | Modalities | Score |
|---|---|---|---|
| Pre-eclampsia | 1.83 | No | +0 |
| Yes | +3 | ||
| Antepartum bleeding | 0.91 | No | +0 |
| Yes | +1 | ||
| Multiple pregnancy | 1.15 | No | +0 |
| Yes | +2 | ||
| Labor duration | 0.83 | <8 h | +0 |
| ≥8 h | +1 | ||
| Macrosomia ** | 0.86 | No | +0 |
| Yes | +1 | ||
| Platelets | 0.90 | ≥150 Giga/L | +0 |
| <150 Giga/L | +1 | ||
| aPTT ratio | 0.67 | <1.1 | +0 |
| ≥1.1 | +1 | ||
| Maximum total score | +10 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bihan, L.; Nowak, E.; Anouilh, F.; Tremouilhac, C.; Merviel, P.; Tromeur, C.; Robin, S.; Drugmanne, G.; Le Roux, L.; Couturaud, F.; et al. Development and Validation of a Predictive Tool for Postpartum Hemorrhage after Vaginal Delivery: A Prospective Cohort Study. Biology 2023, 12, 54. https://doi.org/10.3390/biology12010054
Bihan L, Nowak E, Anouilh F, Tremouilhac C, Merviel P, Tromeur C, Robin S, Drugmanne G, Le Roux L, Couturaud F, et al. Development and Validation of a Predictive Tool for Postpartum Hemorrhage after Vaginal Delivery: A Prospective Cohort Study. Biology. 2023; 12(1):54. https://doi.org/10.3390/biology12010054
Chicago/Turabian StyleBihan, Line, Emmanuel Nowak, François Anouilh, Christophe Tremouilhac, Philippe Merviel, Cécile Tromeur, Sara Robin, Guillaume Drugmanne, Liana Le Roux, Francis Couturaud, and et al. 2023. "Development and Validation of a Predictive Tool for Postpartum Hemorrhage after Vaginal Delivery: A Prospective Cohort Study" Biology 12, no. 1: 54. https://doi.org/10.3390/biology12010054
APA StyleBihan, L., Nowak, E., Anouilh, F., Tremouilhac, C., Merviel, P., Tromeur, C., Robin, S., Drugmanne, G., Le Roux, L., Couturaud, F., Le Moigne, E., Abgrall, J.-F., Pan-Petesch, B., & de Moreuil, C. (2023). Development and Validation of a Predictive Tool for Postpartum Hemorrhage after Vaginal Delivery: A Prospective Cohort Study. Biology, 12(1), 54. https://doi.org/10.3390/biology12010054






