Potential of Whole-Body Vibration in Parkinson’s Disease: A Systematic Review and Meta-Analysis of Human and Animal Studies
Abstract
:Simple Summary
Abstract
1. Introduction
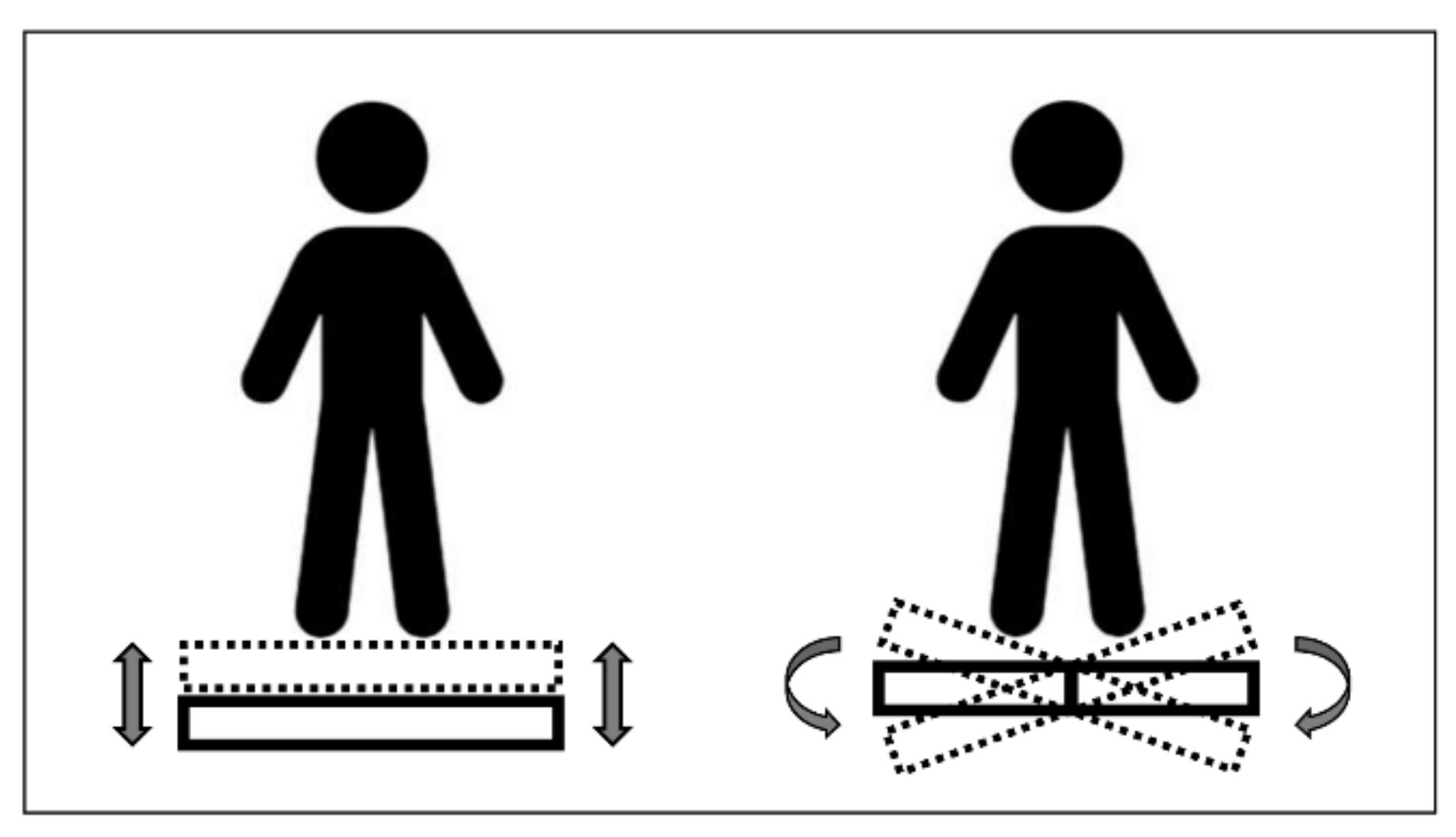
2. Methods
2.1. Information Sources
2.2. Search Strategy
2.3. Study Selection
2.4. Eligibility Criteria
2.5. Data Extraction
2.6. Quality Assessment
2.7. Data Synthesis for Meta-Analyses
3. Results
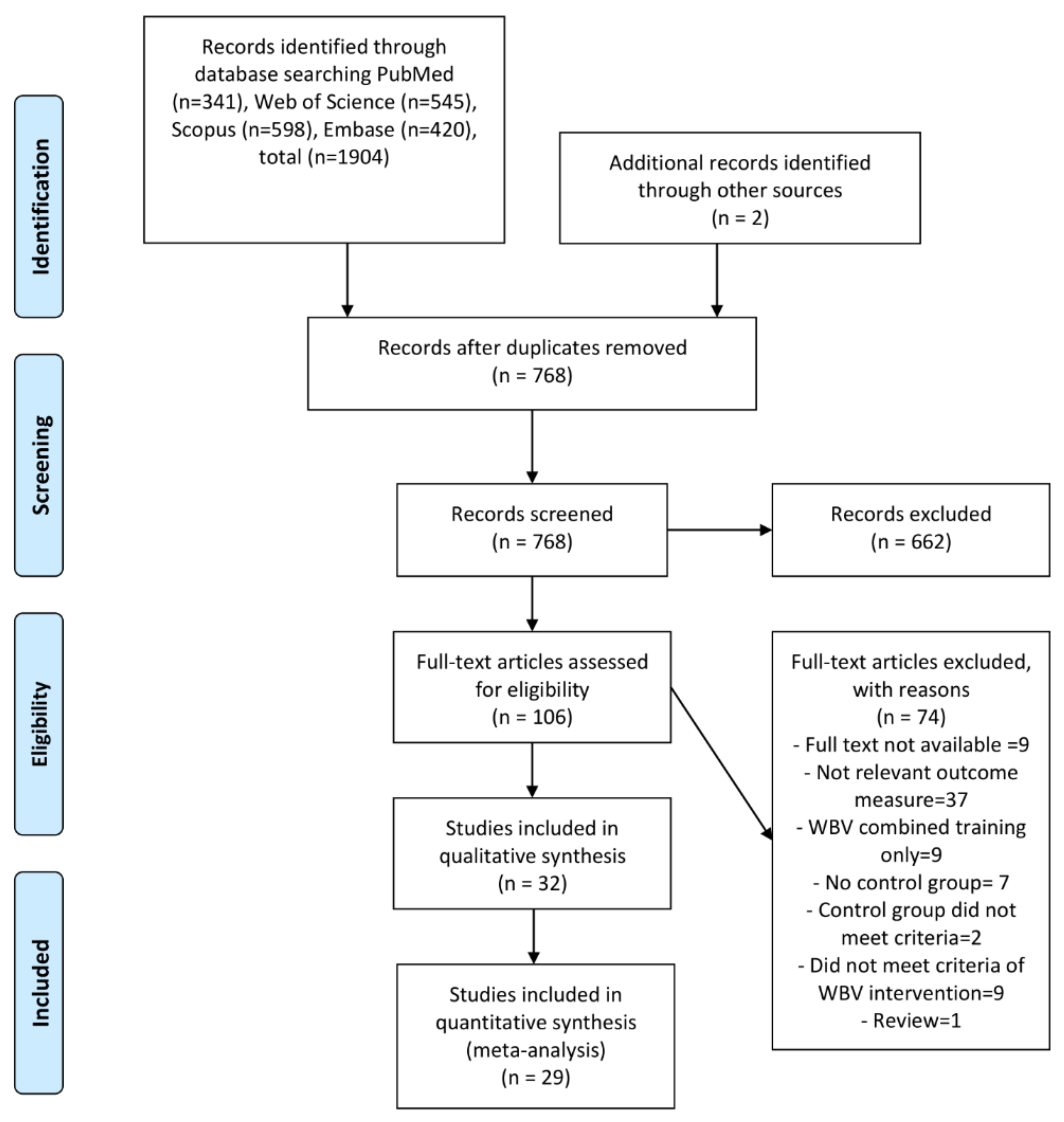
3.1. Study Selection
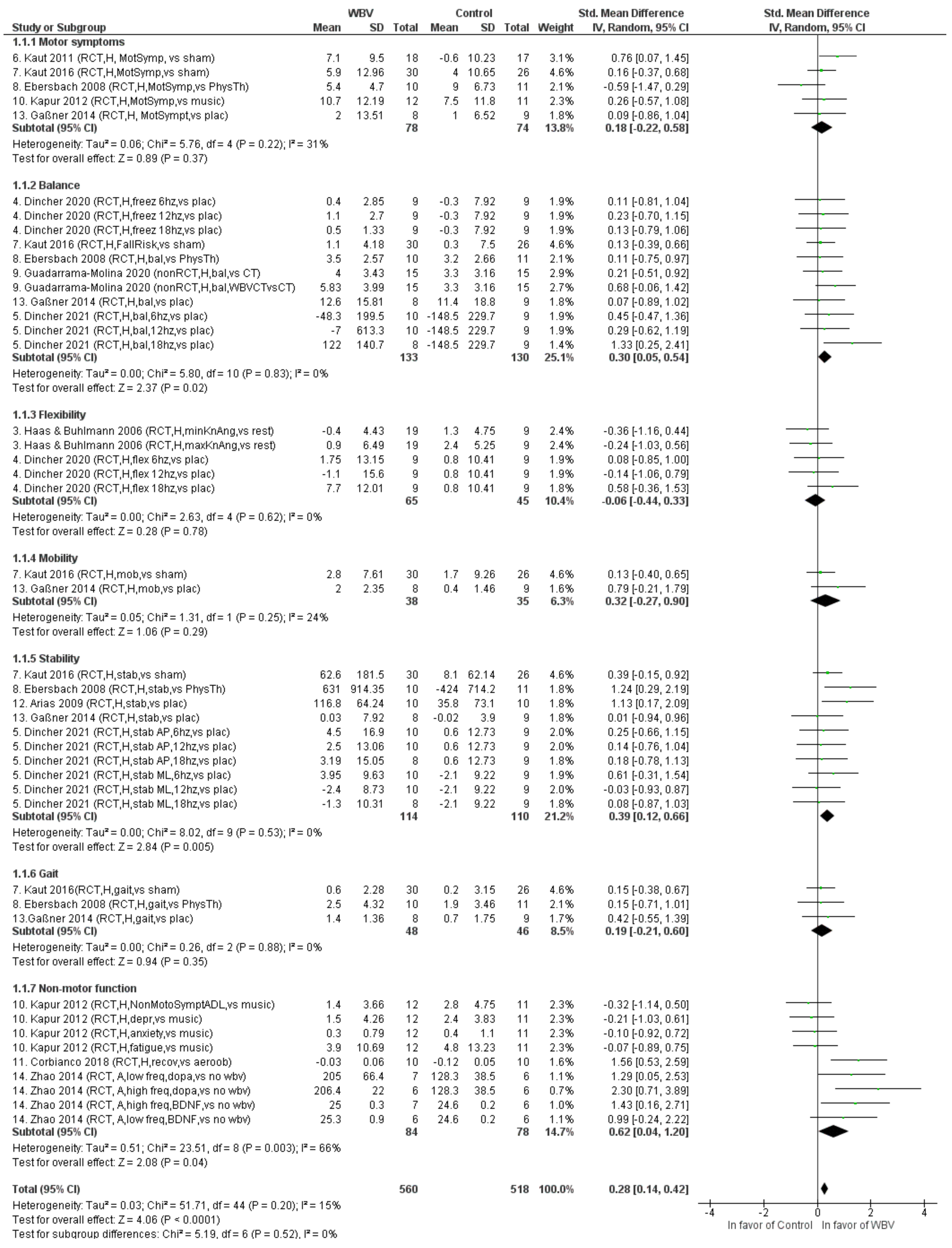
3.2. Effects of WBV on PD Populations
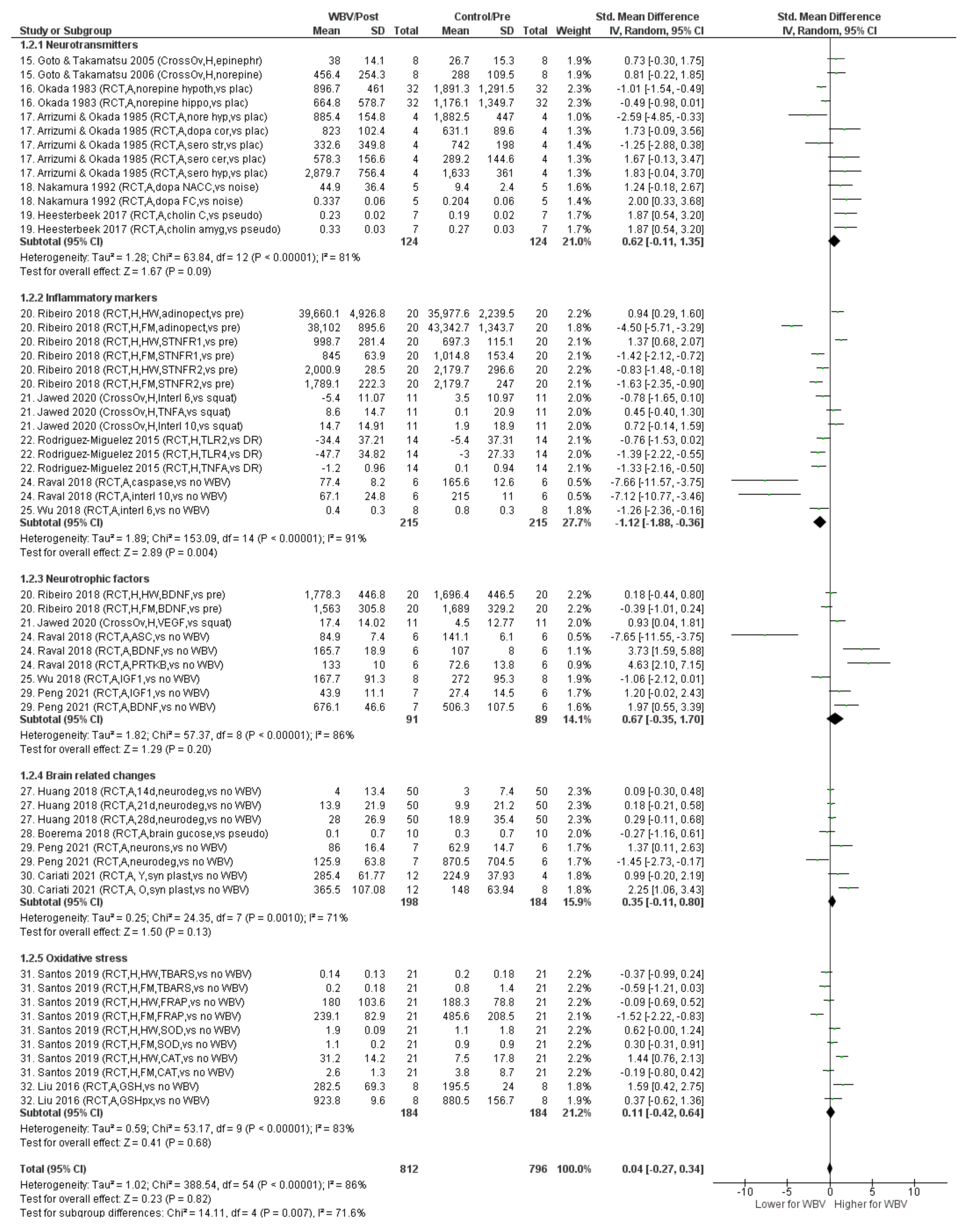
3.3. Effects of WBV on PD Neuropathological Mechanisms
4. Discussion
4.1. WBV in Human PD Populations
4.2. WBV Related to the Neuropathological Mechanisms of PD
4.3. General Considerations
4.4. Recommendations for Further Research
4.5. Recommendations for Sports and Rehabilitation Practices
4.6. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| PubMed | (“Whole Body Vibrat*”[tiab] OR “Vibration Therap*”[tiab] OR “Vibration exercise*”[tiab] OR “Vibration Training*”[tiab]) AND ((“Parkinsonian disorders”[Mesh] OR “Parkinson*” [tiab] OR “MPTP” [tiab]) OR (“Parkinson Disease/physiopathology”[Mesh] OR “Neurotransmitter Agents”[Mesh] OR “Neurotransmitter Agents” [Pharmacological Action] OR “Serotonin”[Mesh] OR “Dopamine”[Mesh] OR “Cytokines”[Mesh] OR “Nerve Growth Factors”[Mesh] OR “Calcium”[Mesh] OR “gamma-Aminobutyric Acid”[Mesh] OR “Blood Circulation”[Mesh] OR “Blood”[tiab] OR “Brain*” [tiab] OR “Neural Activation*”[tiab] OR “neurotransmitter*” [tiab] OR “serotonin*” [tiab] OR “dopamine*”[tiab] OR “acetylcholine*”[tiab] OR lewy bod*[tiab] OR “Oxidative stress*”[tiab] OR “Cytokine*”[tiab] OR “neurotrophic factor*” [tiab] OR “calcium*”[tiab] OR “gamma-amminobutyric acid*”[tiab] OR “bdnf” [tiab] OR “gaba”[tiab] OR “gdnf” [tiab])) | 341 results. |
| Web of Science | TS = (“Whole Body Vibrat*” OR “Vibration Therap*” OR “Vibration exercise*”OR “Vibration Training*”) AND TS = (“Parkinsonian disorders” OR “Parkinson*” OR “MPTP” OR “Neurotransmitter Agents” OR “neurotransmitter*” OR “Serotonin” OR “Dopamine” OR “Cytokine*” OR “Nerve Growth Factor*” OR “Calcium*” OR “acetylcholine*” OR “gamma-Aminobutyric Acid” OR “Blood Circulation” OR “Blood” OR “Brain*” OR “Neural Activation*” OR “lewy bod*” OR “Oxidative stress*”OR “neurotrophic factor*” OR “bdnf” OR “gaba” OR “gdnf”) | 545 results after duplication removal with PubMed (583) |
| Scopus | (TITLE-ABS-KEY (“Whole Body Vibrat*” OR “Vibration Therap*” OR “Vibration exercise*” OR “Vibration Training*”) AND TITLE-ABS-KEY (“Parkinsonian disorders” OR “Parkinson*” OR “MPTP” OR “Neurotransmitter Agents” OR “Neurotransmitter Agents” OR “neurotransmitter*” OR “Serotonin” OR “Dopamine” OR “Cytokine*” OR “Nerve Growth Factor*” OR “Calcium*” OR “acetylcholine*” OR “gamma-Aminobutyric Acid” OR “Blood Circulation” OR “Blood” OR “Brain*” OR “Neural Activation*” OR “lewy bod*” OR “Oxidative stress*” OR “neurotrophic factor*” OR “bdnf” OR “gaba” OR “gdnf”)) | 598 results after duplication removal with PubMed (658) |
| EMbase | (‘whole body vibrat*’:ti,ab,kw OR ‘vibration therap*’:ti,ab,kw OR ‘vibration exercise*’:ti,ab,kw OR ‘vibration training*’:ti,ab,kw) AND (‘parkinsonian disorders’:ti,ab,kw OR ‘parkinson*’:ti,ab,kw OR ‘mptp’:ti,ab,kw OR ‘neurotransmitter agents’:ti,ab,kw OR ‘neurotransmitter*’:ti,ab,kw OR ‘serotonin’:ti,ab,kw OR ‘dopamine’:ti,ab,kw OR ‘cytokine*’:ti,ab,kw OR ‘nerve growth factor*’:ti,ab,kw OR ‘calcium*’:ti,ab,kw OR ‘acetylcholine*’:ti,ab,kw OR ‘gamma-aminobutyric acid’:ti,ab,kw OR ‘blood circulation’:ti,ab,kw OR ‘blood’:ti,ab,kw OR ‘brain*’:ti,ab,kw OR ‘neural activation*’:ti,ab,kw OR ‘lewy bod*’:ti,ab,kw OR ‘oxidative stress*’:ti,ab,kw OR ‘neurotrophic factor*’:ti,ab,kw OR ‘bdnf’:ti,ab,kw OR ‘gaba’:ti,ab,kw OR ‘gdnf’:ti,ab,kw) | 420 results after duplication removal with PubMed (759) |
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | PEDro |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Max (11) | ||||||||||||
| Turbanski et al. (2005) | + | – | – | + | – | – | – | + | + | + | – | 5 |
| Kaut et al. (2016) | + | + | – | + | + | – | + | + | + | + | + | 9 |
| Corbianco et al. (2018) | + | – | – | + | – | – | – | + | + | + | – | 5 |
| Ebersbach et al. (2008) | + | + | + | – | + | – | – | + | + | + | + | 8 |
| Guadarrama-Molina et al. (2020) | + | + | + | – | ? | – | – | + | + | + | – | 6 |
| Haas and Turbanski et al. (2006) | + | + | ? | – | ? | ? | + | + | + | – | – | 5 |
| Haas and Buhlmann et al. (2006) | + | – | – | + | ? | ? | ? | + | + | + | + | 6 |
| Kapur et al. (2012) | + | + | – | + | – | – | + | + | + | + | – | 7 |
| Kaut et al. (2011) | + | + | – | + | + | + | – | + | ? | + | – | 7 |
| Dincher et al., (2020) | + | + | – | + | + | + | + | + | + | + | + | 10 |
| Dincher et al. (2021) | + | + | ? | – | + | + | + | + | + | + | + | 9 |
| Gabner et al. (2014) | + | + | – | + | + | – | – | + | – | + | + | 7 |
| Goto and Takamatsu a | ||||||||||||
| Simao et al. (2019) | + | + | + | + | + | + | + | + | + | + | – | 10 |
| Ribeiro et al. (2018) | + | – | – | – | ? | + | ? | + | + | + | + | 6 |
| Rodriguez-Miguelez et al. (2015) | + | + | – | – | ? | ? | ? | + | + | + | + | 6 |
| Arias el al. (2009) | + | + | – | + | ? | ? | ? | + | + | + | + | 7 |
| Choi et al. (2019) a | ||||||||||||
| Santos et al. (2019) | + | – | – | ? | + | ? | – | + | + | + | + | 6 |
| Jawed et al. (2020) | + | – | – | + | – | ? | ? | + | + | – | + | 5 |
| Study | 1a | 1b | 2a | 2b | 3a | 3b | 4 | 5 | 6 | 7a | 7b | 8a | 8b | 8c | 9a | 9b | 10a | 10b | ARRIVE |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (Max 18) | |||||||||||||||||||
| Okada et al. (1983) | + | + | + | – | – | – | – | ? | + | + | + | + | + | + | + | – | ? | ? | 10 |
| Ariizumi and Okada (1985) | + | + | + | – | – | – | – | – | + | + | – | + | + | + | + | – | – | – | 9 |
| Heesterbeek et al. (2017) | + | + | + | – | – | – | + | – | + | + | + | + | + | + | + | + | + | – | 13 |
| Raval et al. (2018) | – | + | – | – | + | + | + | – | + | + | – | + | + | + | + | + | + | + | 13 |
| Wu et. (2018) | + | + | + | – | + | – | + | – | – | + | + | + | + | + | + | – | + | – | 12 |
| Nakamura et al. (1992) | + | + | + | – | – | – | – | – | + | + | + | + | + | + | + | – | – | – | 10 |
| Cariati et al. (2021) | + | + | + | – | – | – | – | – | + | + | + | + | + | + | – | – | ? | – | 9 |
| Boerema et al. (2018) | + | + | + | – | – | – | + | – | + | + | + | + | + | + | + | – | + | + | 13 |
| Huang et al. (2018) | + | + | + | – | + | + | – | – | + | + | + | + | + | + | + | + | + | – | 14 |
| Peng (2021) | + | + | + | + | – | – | + | – | + | + | + | + | + | + | + | + | + | – | 14 |
| Zhao et al. (2014) | + | + | + | – | + | + | + | ? | + | + | + | + | + | + | + | + | + | – | 15 |
| Liu et al. (2016) | + | + | + | – | ? | – | + | ? | + | + | + | + | + | + | + | + | + | – | 13 |
References
- Ou, Z.; Pan, J.; Tang, S.; Duan, D.; Yu, D.; Nong, H.; Wang, Z. Global Trends in the Incidence, Prevalence, and Years Lived with Disability of Parkinson’s Disease in 204 Countries/Territories from 1990 to 2019. Front. Public Health 2021, 9, 776847. [Google Scholar] [CrossRef] [PubMed]
- Maiti, P.; Manna, J.; Dunbar, G.L.; Maiti, P.; Dunbar, G.L. Current Understanding of the Molecular Mechanisms in Parkinson’s Disease: Targets for Potential Treatments. Transl. Neurodegener. 2017, 6, 1–35. [Google Scholar] [CrossRef] [PubMed]
- Klingelhoefer, L.; Reichmann, H. Parkinson’s Disease as a Multisystem Disorder. J. Neural Transm. 2017, 124, 709–713. [Google Scholar] [CrossRef] [PubMed]
- Vardi, G.; Merrick, J. Neurological Disorders: Public Health Challenges. J. Policy Pract. Intellect. Disabil. 2008, 5, 75. [Google Scholar] [CrossRef]
- Moroz, A.; Edgley, S.R.; Lew, H.L.; Chae, J.; Lombard, L.A.; Reddy, C.C.; Robinson, K.M. Rehabilitation Interventions in Parkinson Disease. PM R 2009, 1, S42–S48. [Google Scholar] [CrossRef]
- Reuter, I.; Engelhardt, M. Exercise Training and Parkinson’s Disease: Placebo or Essential Treatment? Phys. Sportsmed. 2002, 30, 43–50. [Google Scholar] [CrossRef]
- Xu, X.; Fu, Z.; Le, W. Exercise and Parkinson’s Disease. Int. Rev. Neurobiol. 2019, 147, 45–74. [Google Scholar] [CrossRef]
- Abbruzzese, G.; Marchese, R.; Avanzino, L.; Pelosin, E. Rehabilitation for Parkinson’s Disease: Current Outlook and Future Challenges. Park. Relat. Disord. 2016, 22, S60–S64. [Google Scholar] [CrossRef]
- Alam, M.M.; Khan, A.A.; Farooq, M. Effect of Whole-Body Vibration on Neuromuscular Performance: A Literature Review. Work 2018, 59, 571–583. [Google Scholar] [CrossRef]
- Wu, S.; Ning, H.; Xiao, S.; Hu, M.; Wu, X.; HW, D.; Feng, H. Effects of Vibration Therapy on Muscle Mass, Muscle Strength and Physical Function in Older Adults with Sarcopenia: A Systematic Review and Meta-Analysis. Eur. Rev. Aging Phys. Act. 2020, 17, 14. [Google Scholar] [CrossRef]
- Cardinale, M.; Bosco, C. The Use of Vibration as an Exercise Intervention. Exerc. Sport Sci. Rev. 2003, 31, 3–7. [Google Scholar] [CrossRef]
- Pel, J.J.M.; Bagheri, J.; van Dam, L.M.; van den Berg-Emons, H.J.G.; Horemans, H.L.D.; Stam, H.J.; van der Steen, J. Platform Accelerations of Three Different Whole-Body Vibration Devices and the Transmission of Vertical Vibrations to the Lower Limbs. Med. Eng. Phys. 2009, 31, 937–944. [Google Scholar] [CrossRef]
- Van Heuvelen, M.J.G.; Rittweger, J.; Judex, S.; Sañudo, B.; Seixas, A.; Fuermaier, A.B.M.; Tucha, O.; Nyakas, C.; Marín, P.J.; Taiar, R.; et al. Reporting Guidelines for Whole-Body Vibration Studies in Humans, Animals and Cell Cultures: A Consensus Statement from an International Group of Experts. Biology 2021, 10, 965. [Google Scholar] [CrossRef]
- Cochrane, D.J.; North, P.; Zealand, N. Vibration Exercise: The Potential Benefits. Int. J. Sport. Med. 2011, 32, 75–99. [Google Scholar] [CrossRef]
- Oroszi, T.; van Heuvelen, M.J.G.; Nyakas, C.; van der Zee, E.A. Vibration Detection: Its Function and Recent Advances in Medical Applications. F1000Research 2020, 9, 619. [Google Scholar] [CrossRef]
- Lau, R.W.K.; Liao, L.R.; Yu, F.; Teo, T.; Chung, R.C.K.; Pang, M.Y.C. The Effects of Whole Body Vibration Therapy on Bone Mineral Density and Leg Muscle Strength in Older Adults: A Systematic Review and Meta-Analysis. Clin. Rehabil. 2011, 25, 975–988. [Google Scholar] [CrossRef]
- Rogan, S.; Taeymans, J.; Radlinger, L.; Naep, S.; Ruppen, S.; Bruelhart, Y.; Hil, R. Effects of Whole-Body Vibration on Postural Control in Elderly: An Update of a Systematic Review and Meta-Analysis. Arch. Gerontol. Geriatr. 2017, 73, 95–112. [Google Scholar] [CrossRef]
- DadeMatthews, O.O.; Agostinelli, P.J.; Neal, F.K.; Oladipupo, S.O.; Hirschhorn, R.M.; Wilson, A.E.; Sefton, J.E.M. Systematic Review and Meta-Analyses on the Effects of Whole-Body Vibration on Bone Health. Complement. Ther. Med. 2022, 65, 102–811. [Google Scholar] [CrossRef]
- Yang, F.; King, G.A.; Dillon, L.; Su, X. Controlled Whole-Body Vibration Training Reduces Risk of Falls among Community-Dwelling Older Adults. J. Biomech. 2015, 48, 3206–3212. [Google Scholar] [CrossRef]
- Wang, J.; Leung, K.S.; Chow, S.K.H.; Cheung, W.H. The Effect of Whole Body Vibration on Fracture Healing—A Systematic Review. Eur. Cells Mater. 2017, 34, 108–127. [Google Scholar] [CrossRef]
- Wano, N.; Sanguanrungsirikul, S.; Keelawat, S.; Somboonwong, J. The Effects of Whole-Body Vibration on Wound Healing in a Mouse Pressure Ulcer Model. Heliyon 2021, 7, e06893. [Google Scholar] [CrossRef]
- Jiménez-Cebrián, A.M.; López-López, L.; Losa-Iglesias, M.E.; Becerro-de-Bengoa-Vallejo, R.; Romero-Morales, C.; López-López, D.; Montiel-Luque, A.; Navarro-Flores, E.; de Labra, C. The Implications of the Foot Health Status in Parkinson Patients: A Case–Control Study. Int. Wound J. 2022, 1–9. [Google Scholar] [CrossRef]
- Navarro-Flores, E.; Jiménez-Cebrián, A.M.; Becerro-de-Bengoa-Vallejo, R.; Calvo-Lobo, C.; Losa-Iglesias, M.E.; Romero-Morales, C.; López-López, D.; Palomo-López, P. Effect of Foot Health and Quality of Life in Patients with Parkinson Disease: A Prospective Case-Control Investigation. J. Tissue Viability 2022, 31, 69–72. [Google Scholar] [CrossRef]
- Domínguez-Muñoz, F.J.; Villafaina, S.; García-Gordillo, M.A.; Hernández-Mocholi, M.Á.; Collado-Mateo, D.; Adsuar, J.C.; Gusi, N. Effects of 8-Week Whole-Body Vibration Training on the HbA1c, Quality of Life, Physical Fitness, Body Composition and Foot Health Status in People with T2DM: A Double-Blinded Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2020, 17, 1317. [Google Scholar] [CrossRef]
- Boerema, A.S.; Heesterbeek, M.; Boersma, S.A.; Schoemaker, R.; de Vries, E.F.J.J.; van Heuvelen, M.J.G.G.; Van der Zee, E.A. Beneficial Effects of Whole Body Vibration on Brain Functions in Mice and Humans. Dose-Response 2018, 16, 1–10. [Google Scholar] [CrossRef]
- Fuermaier, A.B.M.; Tucha, L.; Koerts, J.; Van Heuvelen, M.J.G.; Van Der Zee, E.A.; Lange, K.W.; Tucha, O. Good Vibrations-Effects of Whole Body Vibration on Attention in Healthy Individuals and Individuals with ADHD. PLoS ONE 2014, 9, e90747. [Google Scholar] [CrossRef]
- Regterschot, G.R.H.; Van Heuvelen, M.J.G.; Zeinstra, E.B.; Fuermaier, A.B.M.; Tucha, L.; Koerts, J.; Tucha, O.; Van Der Zee, E.A. Whole Body Vibration Improves Cognition in Healthy Young Adults. PLoS ONE 2014, 9, e100506. [Google Scholar] [CrossRef]
- Huang, M.; Miller, T.; Ying, M.; Pang, M.Y.C. Whole-Body Vibration Modulates Leg Muscle Reflex and Blood Perfusion among People with Chronic Stroke: A Randomized Controlled Crossover Trial. Sci. Rep. 2020, 10, 1473. [Google Scholar] [CrossRef]
- Abbasi, M.; Kordi Yoosefinejad, A.; Poursadeghfard, M.; Parsaei Jahromi, F.; Motealleh, A.; Sobhani, S. Whole Body Vibration Improves Core Muscle Strength and Endurance in Ambulant Individuals with Multiple Sclerosis: A Randomized Clinical Trial. Mult. Scler. Relat. Disord. 2019, 32, 88–93. [Google Scholar] [CrossRef]
- Krause, A.; Lee, K.; Freyler, K.; Bührer, T.; Gollhofer, A.; Ritzmann, R. Whole-Body Vibration Impedes the Deterioration of Postural Control in Patients with Multiple Sclerosis. Mult. Scler. Relat. Disord. 2019, 31, 134–140. [Google Scholar] [CrossRef]
- Lam, F.M.H.; Liao, L.R.; Kwok, T.C.Y.; Pang, M.Y.C. Effects of Adding Whole-Body Vibration to Routine Day Activity Program on Physical Functioning in Elderly with Mild or Moderate Dementia: A Randomized Controlled Trial. Int. J. Geriatr. Psychiatry 2018, 33, 21–30. [Google Scholar] [CrossRef] [PubMed]
- Dincher, A.; Schwarz, M.; Wydra, G. Analysis of the Effects of Whole-Body Vibration in Parkinson Disease–Systematic Review and Meta-Analysis. PM R 2019, 11, 640–653. [Google Scholar] [CrossRef] [PubMed]
- Lau, R.W.K.; Teo, T.; Yu, F.; Chung, R.C.K.; Pang, M.Y.C. Effects of Whole-Body Vibration on Sensorimotor Performance in People with Parkinson Disease: A Systematic Review. Phys. Ther. 2011, 91, 198–209. [Google Scholar] [CrossRef] [PubMed]
- Sharififar, S.; Coronado, R.A.; Romero, S.; Azari, H.; Thigpen, M. The Effects of Whole Body Vibration on Mobility and Balance in Parkinson Disease: A Systematic Review. Iran. J. Med. Sci. 2014, 39, 318–326. [Google Scholar] [PubMed]
- Alashram, A.R.; Padua, E.; Annino, G. Effects of Whole-Body Vibration on Motor Impairments in Patients with Neurological Disorders: A Systematic Review. Am. J. Phys. Med. Rehabil. 2019, 98, 1084–1098. [Google Scholar] [CrossRef] [PubMed]
- Sitjà Rabert, M.; Rigau Comas, D.; Fort Vanmeerhaeghe, A.; Santoyo Medina, C.; Roqué i Figuls, M.; Romero-Rodríguez, D.; Bonfill Cosp, X. Whole-Body Vibration Training for Patients with Neurodegenerative Disease (Review). Cochrane Database Syst. Rev. 2012, CD009097. [Google Scholar] [CrossRef]
- Marazzi, S.; Kiper, P.; Palmer, K.; Agostini, M.; Turolla, A. Effects of Vibratory Stimulation on Balance and Gait in Parkinson’s Disease: A Systematic Review and Meta-Analysis. Eur. J. Phys. Rehabil. Med. 2020, 57, 254–264. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Ansah, T.A.; Ferguson, M.C.; Nayyar, T.; Deutch, A.Y. Age- and Duration-Dependent Effects of MPTP on Cortical Serotonin Systems. Neurosci. Lett. 2011, 504, 160–164. [Google Scholar] [CrossRef]
- Sánchez, M.G.; Morissette, M.; Di Paolo, T. Estradiol and Brain Serotonin Reuptake Transporter in Long-Term Ovariectomized Parkinsonian Monkeys. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2013, 45, 170–177. [Google Scholar] [CrossRef]
- Hurley, M.J.; Brandon, B.; Gentleman, S.M.; Dexter, D.T. Parkinson’s Disease Is Associated with Altered Expression of Ca V1 Channels and Calcium-Binding Proteins. Brain 2013, 136, 2077–2097. [Google Scholar] [CrossRef]
- Hirsch, E.C.; Jenner, P.; Przedborski, S. Pathogenesis of Parkinson’s Disease. Mov. Disord. 2013, 28, 24–30. [Google Scholar] [CrossRef]
- Dextera, D.T.; Jenner, P. Parkinson Disease: From Pathology to Molecular Disease Mechanisms. Free Radic. Biol. Med. 2013, 62, 132–144. [Google Scholar] [CrossRef]
- Titova, N.; Padmakumar, C.; Lewis, S.J.G.; Chaudhuri, K.R. Parkinson’s: A Syndrome Rather than a Disease? J. Neural Transm. 2017, 124, 907–914. [Google Scholar] [CrossRef]
- Schardt, C.; Adams, M.B.; Owens, T.; Keitz, S.; Fontelo, P. Utilization of the PICO Framework to Improve Searching PubMed for Clinical Questions. BMC Med. Inform. Decis. Mak. 2007, 7, 16. [Google Scholar] [CrossRef]
- Drevon, D.; Fursa, S.; Malcolm, A. Intercoder Reliability and Validity of WebPlotDigitizer in Extracting Graphed Data. Behav. Modif. 2017, 41, 323–339. [Google Scholar] [CrossRef]
- Verhagen, A.P.; De Vet, H.C.W.; De Bie, R.A.; Kessels, A.G.H.; Boers, M.; Bouter, L.M.; Knipschild, P.G. The Delphi List: A Criteria List for Quality Assessment of Randomized Clinical Trials for Conducting Systematic Reviews Developed by Delphi Consensus. J. Clin. Epidemiol. 1998, 51, 1235–1241. [Google Scholar] [CrossRef]
- Du Sert, N.P.; Hurst, V.; Ahluwalia, A.; Alam, S.; Avey, M.T.; Baker, M.; Browne, W.J.; Clark, A.; Cuthill, I.C.; Dirnagl, U.; et al. The Arrive Guidelines 2.0: Updated Guidelines for Reporting Animal Research. PLoS Biol. 2020, 40, 1769–1777. [Google Scholar] [CrossRef]
- Review Manager (RevMan); Version 5.4.; The Cochrane Collaboration, Wiley: Hoboken, NJ, USA, 2020; Available online: https://training.cochrane.org/online-learning/core-software-cochrane-reviews/revman/revman-non-cochrane-reviews (accessed on 23 June 2022).
- Higgins, J.P.T.; Thompson, S.G. Quantifying Heterogeneity in a Meta-Analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Dincher, A.; Wydra, G. Effect of Whole Body Vibration on Balance in Parkinson’s Disease-A Randomized Controlled Pilot Study. In Alzheimer’s Disease & Treatment; MedDocs Publishers: Reno, NV, USA, 2021; Volume 3, Chapter 3; pp. 21–25. [Google Scholar]
- Turbanski, S.; Haas, C.T.; Schmidtbleicher, D.; Friedrich, A.; Duisberg, P. Effects of Random Whole-Body Vibration on Postural Control in Parkinson’s Disease. Res. Sport. Med. 2005, 13, 243–256. [Google Scholar] [CrossRef]
- Kaut, O.; Brenig, D.; Marek, M.; Allert, N.; Wüllner, U. Postural Stability in Parkinson’s Disease Patients Is Improved after Stochastic Resonance Therapy. Parkinson’s Dis. 2016, 2016, 7948721. [Google Scholar] [CrossRef]
- Kaut, O.; Allert, N.; Coch, C.; Paus, S.; Grzeska, A.; Minnerop, M.; Wüllner, U. Stochastic Resonance Therapy in Parkinson’s Disease. NeuroRehabilitation 2011, 28, 353–358. [Google Scholar] [CrossRef]
- Kapur, S.S.; Stebbins, G.T.; Goetz, C.G. Vibration Therapy for Parkinson’s Disease: Charcot’s Studies Revisited. J. Parkinsons. Dis. 2012, 2, 23–27. [Google Scholar] [CrossRef]
- Haas, C.T.; Turbanski, S.; Kessler, K.; Schmidtbleicher, D. The Effects of Random Whole-Body-Vibration on Motor Symptoms in Parkinson’s Disease. NeuroRehabilitation 2006, 21, 29–36. [Google Scholar] [CrossRef]
- Haas, C.T.; Buhlmann, A.; Turbanski, S.; Schmidtbleicher, D. Proprioceptive and Sensorimotor Performance in Parkinson’s Disease. Res. Sport. Med. 2006, 14, 273–287. [Google Scholar] [CrossRef]
- Guadarrama-Molina, E.; Barrón-Gámez, C.E.; Estrada-Bellmann, I.; Meléndez-Flores, J.D.; Ramírez-Castañeda, P.; Hernández-Suárez, R.M.G.; Menchaca-Pérez, M.; Salas-Fraire, O. Comparison of the Effect of Whole-Body Vibration Therapy versus Conventional Therapy on Functional Balance of Patients with Parkinson’s Disease: Adding a Mixed Group. Acta Neurol. Belg. 2020, 121, 721–728. [Google Scholar] [CrossRef]
- Gaßner, H.; Janzen, A.; Schwirtz, A.; Jansen, P. Random Whole Body Vibration over 5 Weeks Leads to Effects Similar to Placebo: A Controlled Study in Parkinson’s Disease. Parkinson’s Dis. 2014, 2014, 386495. [Google Scholar] [CrossRef]
- Ebersbach, G.; Edler, D.; Kaufhold, O.; Wissel, J. Whole Body Vibration Versus Conventional Physiotherapy to Improve Balance and Gait in Parkinson’s Disease. Arch. Phys. Med. Rehabil. 2008, 89, 399–403. [Google Scholar] [CrossRef]
- Dincher, A.; Becker, P.; Wydra, G. Effect of Whole-Body Vibration on Freezing and Flexibility in Parkinson’s Disease-a Pilot Study. Neurol. Sci. 2020, 42, 2795–2801. [Google Scholar] [CrossRef]
- Corbianco, S.; Cavallini, G.; Baldereschi, G.; Carboncini, M.C.; Fiamingo, F.L.; Bongioanni, P.; Dini, M. Whole Body Vibration and Treadmill Training in Parkinson’s Disease Rehabilitation: Effects on Energy Cost and Recovery Phases. Neurol. Sci. 2018, 39, 2159–2168. [Google Scholar] [CrossRef]
- Arias, P.; Chouza, M.; Vivas, J.; Cudeiro, J. Effect of Whole Body Vibration in Parkinson’s Disease: A Controlled Study. Mov. Disord. 2009, 24, 891–898. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.; He, L.X.; Huang, S.N.; Gong, L.J.; Li, L.; Lv, Y.Y.; Qian, Z.M. Protection of Dopamine Neurons by Vibration Training and Up-Regulation of Brain-Derived Neurotrophic Factor in a MPTP Mouse Model of Parkinson’s Disease. Physiol. Res. 2014, 63, 649–657. [Google Scholar] [CrossRef] [PubMed]
- Hoehn, M.M.; Yahr, M.D. Parkinsonism: Onset, Progression and Mortality. Neurology 1967, 17, 427–442. [Google Scholar] [CrossRef] [PubMed]
- Simão, A.P.; Mendonça, V.A.; Avelar, N.C.P.; da Fonseca, S.F.; Santos, J.M.M.; de Oliveira, A.C.C.; Tossige-Gomes, R.; Ribeiro, V.G.C.; Neves, C.D.C.; Balthazar, C.H.; et al. Whole Body Vibration Training on Muscle Strength and Brain-Derived Neurotrophic Factor Levels in Elderly Woman with Knee Osteoarthritis: A Randomized Clinical Trial Study. Front. Physiol. 2019, 10, 756. [Google Scholar] [CrossRef]
- Santos, J.M.; Mendonça, V.A.; Ribeiro, V.G.C.; Tossige-Gomes, R.; Fonseca, S.F.; Prates, A.C.N.; Flor, J.; Oliveira, A.C.C.; Martins, J.B.; Garcia, B.C.C.; et al. Does Whole Body Vibration Exercise Improve Oxidative Stress Markers in Women with Fibromyalgia? Brazilian J. Med. Biol. Res. 2019, 52, e8688. [Google Scholar] [CrossRef]
- Rodriguez-Miguelez, P.; Fernandez-Gonzalo, R.; Collado, P.S.; Almar, M.; Martinez-Florez, S.; de Paz, J.A.; González-Gallego, J.; Cuevas, M.J. Whole-Body Vibration Improves the Anti-Inflammatory Status in Elderly Subjects through Toll-like Receptor 2 and 4 Signaling Pathways. Mech. Ageing Dev. 2015, 150, 12–19. [Google Scholar] [CrossRef]
- Ribeiro, V.G.C.; Mendonça, V.A.; Souza, A.L.C.; Fonseca, S.F.; Camargos, A.C.R.; Lage, V.K.S.; Neves, C.D.C.; Santos, J.M.; Teixeira, L.A.C.; Vieira, E.L.M.; et al. Inflammatory Biomarkers Responses after Acute Whole Body Vibration in Fibromyalgia. Brazilian J. Med. Biol. Res. 2018, 51, e6775. [Google Scholar] [CrossRef]
- Jawed, Y.; Beli, E.; March, K.; Kaleth, A.; Loghmani, M.T. Whole-Body Vibration Training Increases Stem/Progenitor Cell Circulation Levels and May Attenuate Inflammation. Mil. Med. 2020, 185, 404–412. [Google Scholar] [CrossRef]
- Choi, D.S.; Lee, H.J.; Shin, Y.I.; Lee, A.; Kim, H.G.; Kim, Y.H. Modulation of Cortical Activity by High-Frequency Whole-Body Vibration Exercise: An FNIRS Study. J. Sport Rehabil. 2019, 28, 665–670. [Google Scholar] [CrossRef]
- Goto, K.; Takamatsu, K. Hormone and Lipolytic Responses to Whole Body Vibration in Young Men. Jpn. J. Physiol. 2005, 55, 279–284. [Google Scholar] [CrossRef]
- Okada, A.; Ariizumi, M.; Okamoto, G. Changes in Cerebral Norepinephrine Induced by Vibration or Noise Stress. Eur. J. Appl. Physiol. Occup. Physiol. 1983, 52, 94–97. [Google Scholar] [CrossRef]
- Cariati, I.; Bonanni, R.; Pallone, G.; Annino, G.; Tancredi, V.; D’Arcangelo, G.; D’arcangelo, G.; D’Arcangelo, G. Modulation of Synaptic Plasticity by Vibratory Training in Young and Old Mice. Brain Sci. 2021, 11, 82. [Google Scholar] [CrossRef]
- Huang, D.; Yang, Z.; Wang, Z.; Wang, P.; Qu, Y. The Macroscopic and Microscopic Effect of Low-Frequency Whole-Body Vibration after Cerebral Ischemia in Rats. Metab. Brain Dis. 2018, 33, 15–25. [Google Scholar] [CrossRef]
- Liu, Y.; Zhai, M.; Guo, F.; Shi, T.; Liu, J.; Wang, X.; Zhang, X.; Jing, D.; Hai, C. Whole Body Vibration Improves Insulin Resistance in Db/Db Mice: Amelioration of Lipid Accumulation and Oxidative Stress. Appl. Biochem. Biotechnol. 2016, 179, 819–829. [Google Scholar] [CrossRef]
- Nakamura, H.H.; Moroji, T.; Nohara, S.; Nakamura, H.H.; Okada, A. Activation of Cerebral Dopaminergic Systems by Noise and Whole-Body Vibration. Environ. Res. 1992, 57, 10–18. [Google Scholar] [CrossRef]
- Peng, G.; Yang, L.; Wu, C.Y.; Zhang, L.L.; Wu, C.Y.; Li, F.; Shi, H.W.; Hou, J.; Zhang, L.M.L.M.; Ma, X.; et al. Whole Body Vibration Training Improves Depression-like Behaviors in a Rat Chronic Restraint Stress Model. Neurochem. Int. 2021, 142, 104926. [Google Scholar] [CrossRef]
- Raval, A.P.; Schatz, M.; Bhattacharya, P.; D’adesky, N.; Rundek, T.; Dietrich, W.D.; Bramlett, H.M. Whole Body Vibration Therapy after Ischemia Reduces Brain Damage in Reproductively Senescent Female Rats. Int. J. Mol. Sci. 2018, 19, 2749. [Google Scholar] [CrossRef]
- Heesterbeek, M.; Jentsch, M.; Roemers, P.; Keijser, J.N.; Toth, K.; Nyakas, C.; Schoemaker, R.G.; Van Heuvelen, M.J.G.; Van Der Zee, E.A. Whole Body Vibration Enhances Choline Acetyltransferase- Immunoreactivity in Cortex and Amygdale. J. Neurol. Transl. Neurosci. 2017, 5, 1079. [Google Scholar]
- Ariizumi, M.; Okada, A. Effects of Whole Body Vibration on Biogenic Amines in Rat Brain. Br. J. Ind. Med. 1985, 42, 133–136. [Google Scholar] [CrossRef]
- Wu, H.; Zhang, Y.; Yang, X.; Li, X.; Shao, Z.; Zhou, Z.; Li, Y.; Pan, S.; Liu, C. Whole Body Vibration Retards Progression of Atherosclerosis via Insulin-Like Growth Factor 1 in Apolipoprotein E-Deficient Mice. Biomed. Res. Int. 2018, 2018, 4934861. [Google Scholar] [CrossRef]
- Chanou, K.; Gerodimos, V.; Karatrantou, K.; Jamurtas, A. Whole-Body Vibration and Rehabilitation of Chronic Diseases: A Review of the Literature. J. Sport. Sci. Med. 2012, 11, 187–200. [Google Scholar]
- Heesterbeek, M.; Van Der Zee, E.A.; Van Heuvelen, M.J.G. Feasibility of Three Novel Forms of Passive Exercise in a Multisensory Environment in Vulnerable Institutionalized Older Adults with Dementia. J. Alzheimer’s Dis. 2019, 70, 681–690. [Google Scholar] [CrossRef]
- Berner, K.; Albertyn, S.C.S.; Dawnarain, S.; Hendricks, L.J.; Johnson, J.; Landman, A.; Burger, M. The Effectiveness of Combined Lower Limb Strengthening and Whole-Body Vibration, Compared to Strengthening Alone, for Improving Patient-Centred Outcomes in Adults with COPD: A Systematic Review. South Afr. J. Physiother. 2020, 76, 1412. [Google Scholar] [CrossRef]
- Ritzmann, R.; Krause, A.; Freyler, K.; Gollhofer, A. Acute Whole-Body Vibration Increases Reciprocal Inhibition. Hum. Mov. Sci. 2018, 60, 191–201. [Google Scholar] [CrossRef]
- Homberg, J.R.; Adan, R.A.H.; Alenina, N.; Asiminas, A.; Bader, M.; Beckers, T.; Begg, D.P.; Blokland, A.; Burger, M.E.; van Dijk, G.; et al. The Continued Need for Animals to Advance Brain Research. Neuron 2021, 109, 2374–2379. [Google Scholar] [CrossRef]
- Van der Zee, E.; Heesterbeek, M.; Tucha, O.; Fuermaier, A.; Van Heuvelen, M. Whole Body Vibration, Cognition, and the Brain. In Whole Body Vibrations: Physical and Biological Effects on The Human Body; Taiar, R., Machado, C.B., Chiementin, X., Bernardo-Filho, M., Eds.; CRC Press: Boca Raton, FL, USA, 2018; pp. 151–171. [Google Scholar]
- Wang, Q.; Liu, Y.; Zhou, J. Neuroinflammation in Parkinson’s Disease and Its Potential as Therapeutic Target. Transl. Neurodegener. 2015, 4, 19. [Google Scholar] [CrossRef]
- Ward, P.A.; Lentsch, A.B. The Acute Inflammatory Response and Its Regulation. Arch. Surg. 1999, 134, 666–669. [Google Scholar] [CrossRef]
- Chen, T.; Liu, W.B.; Ren, X.; Li, Y.F.; Li, W.; Hang, C.H.; Wang, Y.H. Whole Body Vibration Attenuates Brain Damage and Neuroinflammation Following Experimental Traumatic Brain Injury. Front. Cell Dev. Biol. 2022, 10, 847859. [Google Scholar] [CrossRef]
- Voss, M.W.; Nagamatsu, L.S.; Liu-Ambrose, T.; Kramer, A.F. Exercise, Brain, and Cognition across the Life Span. J. Appl. Physiol. 2011, 111, 1505–1513. [Google Scholar] [CrossRef]
- Hemmati-Dinarvand, M.; Saedi, S.; Valilo, M.; Kalantary-Charvadeh, A.; Alizadeh Sani, M.; Kargar, R.; Safari, H.; Samadi, N. Oxidative Stress and Parkinson’s Disease: Conflict of Oxidant-Antioxidant Systems. Neurosci. Lett. 2019, 709, 134296. [Google Scholar] [CrossRef]
- Emerenziani, G.P.; Meucci, M.; Gallotta, M.C.; Buzzachera, C.F.; Guidetti, L.; Baldari, C. Whole Body Vibration: Unsupervised Training or Combined with a Supervised Multi-Purpose Exercise for Fitness? J. Sports Sci. 2014, 32, 1033–1041. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.H.; Sun, T.L. Evaluation of Postural Stability Based on a Force Plate and Inertial Sensor during Static Balance Measurements. J. Physiol. Anthropol. 2018, 37, 27. [Google Scholar] [CrossRef] [PubMed]
- Stebbins, G.T.; Goetz, C.G.; Lang, A.E.; Cubo, E. Factor Analysis of the Motor Section of the Unified Parkinson’s Disease Rating Scale during the off-State. Mov. Disord. 1999, 14, 585–589. [Google Scholar] [CrossRef]
- Stebbins, G.T.; Goetz, C.G. Factor Structure of the Unified Parkinson’s Disease Rating Scale: Motor Examination Section. Mov. Disord. 1998, 13, 633–636. [Google Scholar] [CrossRef]
- Camicioli, R.; Grossmann, S.J.; Spencer, P.S.; Hudnell, K.; Kent Anger, W. Discriminating Mild Parkinsonism: Methods for Epidemiological Research. Mov. Disord. 2001, 16, 33–40. [Google Scholar] [CrossRef]
- Goetz, C.; Poewe, W.; Rascol, O.; Sampaio, C.S.G. State of the Art Review: The Unified Parkinson’s Disease Rating Scale (UPDRS): Status and Recommendations. Movt. Disord. 2013, 18, 738–750. [Google Scholar]
- Siderowf, A.; McDermott, M.; Kieburtz, K.; Blindauer, K.; Plumb, S.; Shoulson, I. Test-Retest Reliability of the Unified Parkinson’s Disease Rating Scale in Patients with Early Parkinson’s Disease: Results from a Multicenter Clinical Trial. Mov. Disord. 2002, 17, 758–763. [Google Scholar] [CrossRef]
- Hancock, G.E.; Hepworth, T.; Wembridge, K. Accuracy and Reliability of Knee Goniometry Methods. J. Exp. Orthop. 2018, 5, 46. [Google Scholar] [CrossRef]
- Mayorga-Vega, D.; Viciana, J.; Cocca, A.; Merino-Marban, R. Criterion-Related Validity of Toe-Touch Test for Estimating Hamstring Extensibility: A Metaanalysis. J. Hum. Sport Exerc. 2014, 9, 188–200. [Google Scholar] [CrossRef]
- Harro, C.C.; Marquis, A.; Piper, N.; Burdis, C. Reliability and Validity of Force Platform Measures of Balance Impairment in Individuals with Parkinson Disease. Phys. Ther. 2016, 96, 1955–1964. [Google Scholar] [CrossRef]
- Hebert, J.R.; Manago, M.M. Reliability and Validity of the Computerized Dynamic Posturography Sensory Organization Test in People with Multiple Sclerosis. Int. J. MS Care 2017, 19, 151–157. [Google Scholar] [CrossRef]
- Christopher, A.; Kraft, E.; Olenick, H.; Kiesling, R.; Doty, A. The Reliability and Validity of the Timed Up and Go as a Clinical Tool in Individuals with and without Disabilities across a Lifespan: A Systematic Review: Psychometric Properties of the Timed Up and Go. Disabil. Rehabil. 2021, 43, 1799–1813. [Google Scholar] [CrossRef]
- Alghadir, A.H.; Al-Eisa, E.S.; Anwer, S.; Sarkar, B. Reliability, Validity, and Responsiveness of Three Scales for Measuring Balance in Patients with Chronic Stroke. BMC Neurol. 2018, 18, 141. [Google Scholar] [CrossRef]
- Kegelmeyer, D.A.; Kloos, A.D.; Thomas, K.M.; Kostyk, S.K. Reliability and Validity of the Tinetti Mobility Test for Individuals with Parkinson Disease. Phys. Ther. 2007, 87, 1369–1378. [Google Scholar] [CrossRef]
- Combs, S.A.; Diehl, M.D.; Filip, J.; Long, E. Short-Distance Walking Speed Tests in People with Parkinson Disease: Reliability, Responsiveness, and Validity. Gait Posture 2014, 39, 784–788. [Google Scholar] [CrossRef]
- Qutubuddin, A.A.; Pegg, P.O.; Cifu, D.X.; Brown, R.; McNamee, S.; Carne, W. Validating the Berg Balance Scale for Patients with Parkinson’s Disease: A Key to Rehabilitation Evaluation. Arch. Phys. Med. Rehabil. 2005, 86, 789–792. [Google Scholar] [CrossRef]
- Martinez-Martin, P.; Rodriguez-Blazquez, C.; Alvarez-Sanchez, M.; Arakaki, T.; Bergareche-Yarza, A.; Chade, A.; Garretto, N.; Gershanik, O.; Kurtis, M.M.; Martinez-Castrillo, J.C.; et al. Expanded and Independent Validation of the Movement Disorder Society-Unified Parkinson’s Disease Rating Scale (MDS-UPDRS). J. Neurol. 2013, 260, 228–236. [Google Scholar] [CrossRef]
- Gallagher, D.A.; Goetz, C.G.; Stebbins, G.; Lees, A.J.; Schrag, A. Validation of the MDS-UPDRS Part I for Nonmotor Symptoms in Parkinson’s Disease. Mov. Disord. 2012, 27, 79–83. [Google Scholar] [CrossRef]
- García-Batista, Z.E.; Guerra-Peña, K.; Cano-Vindel, A.; Herrera-Martínez, S.X.; Medrano, L.A. Validity and Reliability of the Beck Depression Inventory (BDI-II) in General and Hospital Population of Dominican Republic. PLoS ONE 2018, 13, e0199750. [Google Scholar] [CrossRef]
- Wilod Versprille, L.J.F.; van de Loo, A.J.A.E.; Mackus, M.; Arnoldy, L.; Sulzer, T.A.L.; Vermeulen, S.A.; Abdulahad, S.; Huls, H.; Baars, T.; Scholey, A.; et al. Development and Validation of the Immune Status Questionnaire (ISQ). Int. J. Environ. Res. Public Health 2019, 16, 4743. [Google Scholar] [CrossRef]
- Cameron, K.; Williamson, P.; Short, M.A.; Gradisar, M. Validation of the Flinders Fatigue Scale as a Measure of Daytime Fatigue. Sleep Med. 2017, 30, 105–112. [Google Scholar] [CrossRef]
- Crouter, S.E.; Antczak, A.; Hudak, J.R.; DellaValle, D.M.; Haas, J.D. Accuracy and Reliability of the ParvoMedics TrueOne 2400 and MedGraphics VO2000 Metabolic Systems. Eur. J. Appl. Physiol. 2006, 98, 139–151. [Google Scholar] [CrossRef]
- Weiner, D.K.; Duncan, P.W.; Chandler, J.; Studenski, S.A. Functional Reach: A Marker of Physical Frailty. J. Am. Geriatr. Soc. 1992, 40, 203–207. [Google Scholar] [CrossRef]
- Ferreira, S.; Raimundo, A.; Marmeleira, J. Test-Retest Reliability of the Functional Reach Test and the Hand Grip Strength Test in Older Adults Using Nursing Home Services. Ir. J. Med. Sci. 2021, 190, 1625–1632. [Google Scholar] [CrossRef]
- Perez-Cruzado, D.; González-Sánchez, M.; Cuesta-Vargas, A.I. Parameterization and Reliability of Single-Leg Balance Test Assessed with Inertial Sensors in Stroke Survivors: A Cross-Sectional Study. Biomed. Eng. Online 2014, 13, 127. [Google Scholar] [CrossRef]
| Reference | Design | Sample | Disease Severity (Mean H&Y 1) | Groups (n) | Intervention Duration | Vibration Protocol | |||
|---|---|---|---|---|---|---|---|---|---|
| Type (Device, Vibration Type) | Temporal Aspects 2 | Intensity (Frequency, Amplitude 3) | Posture | ||||||
| Human studies | |||||||||
| 1. Turbanski et al. (2005) | RCT | N = 52 Sex M/F = 38/14 Mean age = 69.1 | 3.3 | 2 groups - WBV (26) - Moderate walking (26) | 1 day | Zeptor Med System Vertical | 1 session 5 × 60 s | 6 Hz +/– 1 Hz/s 3 mm | N.R. |
| 2. Haas and Turbanski et al. (2006) | Cross-over design | N = 68 Sex M/F = 53/15 Mean age = 65 | 2–4 | 2 groups - WBV → Rest (34) - Rest → WBV (34) | 1 day | Zeptor Med System Vertical | 1 session 5 × 60 s | 6 Hz+/– 1 Hz/s 3 mm | Semi-squat |
| 3. Haas and Buhlmann et al. (2006) | RCT | N = 28 Sex M/F = N.R. Mean age: 63.1 | 2–4 | 2 Groups - WBV (19) - Rest (9) | 1 day | SRT Medical® System Vertical | 1 session 5 × 60 s | 6 Hz N.R. | N.R. |
| 4. Dincher et al. (2020) | RCT | N = 36 Sex M/F = 18/18 Mean age = 69.3 | 2.1 | 4 groups - 6 Hz WBV (9) - 12 Hz WBV (9) - 18 Hz WBV (9) - Placebo: (9) | 1 day | Galileo Med Advanced Side-alternating | 1 session 5 × 60 s | 6 Hz, 12 Hz, 18 Hz 4 mm | Semi-squat |
| 5. Dincher et al. (2021) | RCT | N = 54 Sex M/F = 24/30 Mean age = 72.5 | 2.11 | 4 groups - 6 Hz PD (10) - 12 Hz PD (10) -18 Hz PD (8) - Placebo (9) | 1 day | Galileo Med Advanced Side-alternating | 1 session 5 × 60 s | 6 Hz, 12 Hz, 18 Hz N.R. | Semi-squat |
| 6. Kaut et al. (2011) | RCT | N = 35 Sex M/F = 28/7 Mean age = 69.4 | 2.6 | 2 groups - WBV (18) - Sham WBV (17) | 5 days | SR Zeptor Device Vertical | 3 sessions 5 × 60 s | 6.5 Hz N.R. | Semi-squat |
| 7. Kaut et al. (2016) | RCT | N = 56 Sex M/F = 36/20 Mean age = 67.0 | 2.7 | 2 groups - WBV (30) - Sham vibration (26) | 8 days | SR Zeptor Device Vertical | 4 sessions 6 × 60 s | 7 Hz 3 mm | Semi-squat |
| 8. Ebersbach et al. (2008) | RCT | N = 21 Sex M/F = 14/7 Mean age = 73.8 | N.R. | 2 groups - WBV (10) - Physical therapy (11) | 3 weeks | Galileo Device Side-alternating | 20 sessions/ 5 sessions/wk 2 × 15 min | 25 Hz 7–14 mm | Semi-squat |
| 9. Guadarrama-Molina et al. (2020) | Non-randomized clinical trial | N = 45 Sex M/F = 27/18 Mean age = 63.5 | 2 | 3 groups - WBV (15) - Conventional therapy (15) - Combined (15) | 3 weeks | Fitvibe Excel Pro Vibration Trainer Vertical | 20 sessions/ 3 sessions/wk 8 × 20 s | 20 Hz 2 mm | Eight active postures |
| 10. Kapur et al. (2012) | RCT | N = 23 Sex M/F = 16/7 Mean age = 65.4 | 2–3 | 2 Groups - WBV (12) - Listening to music (11) | 4 weeks | SMART Lounge, Vertical | 28 sessions/ 7 sessions/wk 1 × 30 min | 30–500 Hz N.R. | Sitting on a vibrating chair |
| 11. Corbianco et al. (2018) | RCT | N = 20 Sex M/F = 20/0 Mean age = 57.9 | 2 | 2 groups: - WBV (10) - Aerobic treadmill training (10) | 4 weeks | Galileo Med L2000 Side-alternating | 16 sessions/ 4 sessions/wk 20 × 60 s | 26 Hz 4 mm | Semi-squat |
| 12. Arias et al. (2009) | RCT | N = 21 Sex M/F = 12/9 Mean age = 66.7 | N.R. | 2 groups - WBV (10) - Placebo (11) | 5 weeks | N.R. | 12 sessions/ 2–3 sessions/wk 5 × 60 s | 6 Hz N.R. | Semi-squat |
| 13. Gaβner et al. (2014) | RCT | N = 17 Sex M/F = 13/4 Mean age = 69.7 | 2.6 | 2 groups - WBV (8) - Placebo (9) | 5 weeks | SRT Zeptor Medical Vertical | 12 sessions 2–3 session/wk 5 × 60 s | 6 Hz ± 1 Hz noise 3 mm | Semi-squat |
| Animal studies | |||||||||
| 14. Zhoa et al. (2014) | RCT | N = 25 MPTP mice 2 injections of MPTP (30 mg/kg) Brains decapitated | N.R. | 4 groups - MPTP LAV LF (7) - MPTP LAV HF (6) - MPTP (6) - Healthy mice, no vibration (6) | 4 weeks | Columbus Instruments Vertical | 28 sessions/ 7 sessions/wk 15 × 60 s | 10 Hz, 20 Hz 5 mm | Not fixated |
| Reference | Examined Domains | Outcome Measure | WBV (Mean ± SD) 2 | Control (Mean ± SD) 2 | WBV vs. Control | Effect Size (g) 1 | Main Finding | ||
|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | ||||||
| Human studies | |||||||||
| 1. Turbanski et al. (2005) | Postural stability | Sway reduction narrow stance (%) Sway reduction Tandem stance (%) | N.R. N.R. | ↓14.9% ** ↓24% * | N.R. N.R. | –7.1% * –11.3% | ns. p = 0.04 | – | “Random whole-body vibration can improve postural stability in PD but these effects depend on the test condition (narrow position vs. tandem stance)”. |
| 2. Haas and Turbanski et al. (2006) | Motor symptoms | UPDRS-III (%change) | N.R. | WBV→Rest ↓16.8% ** Rest→WBV ↓14.7% ** | N.R. | N.R. | p < 0.01 p < 0.01 | – | “As the treatment was connected each time with significant improvements in the UPDRS motor score while the control condition led to small, insignificant changes only, one has to conclude that the treatment has beneficial effects on PD motor symptoms”. |
| 3. Haas and Buhlmann et al. (2006) | Proprioceptive performance | Minimum knee angle (°) Maximum knee angle (°) | 103.1 ± 4.9 125.6 ± 5.7 | 103.5 ± 3.9 126.5 ± 7.2 | 101.9 ± 5.4 124.1 ± 5.1 | 100.6 ± 4.0 126.5 ± 5.4 | ns. ns. | –0.36 –0.24 | “This study did not identify changes in proprioceptive performance after short-term mechanical training stimuli that reduced PD symptoms and especially postural control disturbances”. |
| 4. Dincher et al. (2020) | Flexibility Freezing | Sit and reach test (best of 3) 360° turn test combined (s) | 6 Hz: –11 ± 13.0 12 Hz: –5.4 ± 15.3 18 Hz: –5.8 ± 13.1 6 Hz: 8.8 ± 3.0 12 Hz: 8.4 ± 2.7 18 Hz: 6.3 ± 1.6 | 6 Hz: –9.25 ± 13.3 12 Hz: –6.5 ± 15.9 18 Hz: 1.9 ± 10.8 * 6 Hz: 8.4 ± 2.7 12 Hz: 7.3 ± 2.7 18 Hz: 5.8 ± 1.0 | –12.0 ± 8.8 12.3 ± 7.3 | –11.2 ± 11.8 12.6 ± 8.5 | N.R. N.R. N.R. N.R. N.R. N.R. | 0.08 –0.14 0.58 0.11 0.23 0.13 | “It could be shown that higher frequencies seem to achieve a greater improvement from pretest to posttest than lower frequencies”. |
| 5. Dincher et al. (2021) | Balance Stability | 95% ellipse of sway (cm2) Anterior–posterior stability (cm) Medio-lateral stability (cm) | 6 Hz: 451.6 ± 196.15 12 Hz: 555 ± 624.16 18 Hz: 333.5 ± 138.3 6 Hz: –18.7 ±16.5 12 Hz: –16.4 ± 13.6 18 Hz: –20.01 ± 12.4 6 Hz: –6.05 ± 10.8 12 Hz: –4.5 ± 9.4 18 Hz –2.3 ± 9.8 | 6 Hz: 499.9 ± 202.7 12 Hz: 562 ± 602.2 18 Hz: 211.5 ± 143 * 6 Hz: –23.2 ± 17.3 12 Hz: –18.9 ± 12.5 18 Hz: –23.2 ± 17.3 6 Hz: –2.1 ± 8.3 12 Hz: –6.9 ± 8.0 18 Hz: –3.6 ± 10.8 | 388 ± 188.2 –14.8 ± 11.2 –1.3 ± 9.8 | 536.5 ± 264.8 –15.4 ± 14.1 –3.4 ± 8.6 | N.R. N.R. N.R. N.R. N.R. N.R. N.R. N.R. N.R. | 0.45 0.29 1.33 0.25 0.14 0.18 0.61 –0.03 0.08 | “WBV can cause an increase in the sway area and an improvement to anterior–posterior center displacement. Vibration frequency seems to play a subordinate role”. |
| 6. Kaut et al. (2011) | Motor symptoms | UPDRS-III sum score | 26.9 ± 10.4 | 19.8 ± 8.5 * | 24.4 ± 9.4 | 25.0 ± 11.0 | N.R. | 0.76 | “A significant number of responders was found for bradykinesia and postural stability. The extent of improvement of bradykinesia in the treatment group was evident in comparison to the sham-treated group and baseline”. |
| 7. Kaut et al. (2016) | Postural stability Mobility Fall risk Gait Motor symptoms | Mean sway (mm) TUG (s) Tinetti score 8 MW (s) UPDRS-III sum score | 356.5 ± 212.1 11.1 ± 10.1 23.1 ± 4.9 6.7 ± 2.6 24.8 ± 13.4 | 293.9 ± 144.5 * 8.3 ± 3.7 24.2 ± 3.3 * 6.1 ± 1.9 * 18.9 ± 12.5 ** | 272.0 ± 59.9 12.2 ± 10.6 21.6 ± 7.4 6.7 ± 3.3 25.4 ± 10.5 | 263.9 ± 64.3 10.5 ± 7.7 21.9 ± 7.6 6.5 ± 3.0 21.4 ± 10.8 ** | ns. ns. ns. ns. ns. | 0.39 0.13 0.13 0.15 0.16 | “Stochastic resonance therapy significantly enhanced postural stability even in individuals with an increased risk of falling. Thus it offers a potential supplementation to canonical treatments of PD”. |
| 8. Ebersbach et al. (2008) | Balance Postural stability Gait Motor symptoms | Tinetti score Mean sway (mm) Time walk 10 m (s) UPDRS-III sum score | 9.3 ± 3.1 1937.0 ± 1250.0 17.6 ± 5.0 23.0 ± 4.9 | 12.8 ± 1.9 ** 1306.0 ± 331.0 15.1±3.5 ** 17.6 ± 4.5 ** | 8.3 ± 2.9 1832.0 ± 746.0 18.4 ± 4.2 25.9 ± 8.1 | 11.5 ± 2.4 ** 2256.0 ± 681.0 16.5 ± 2.5** 16.9 ± 5.0 ** | ns. ns. ns. ns. | 0.11 1.24 0.15 –0.59 | “Equilibrium and gait improved in patients with PD receiving conventional WBV or PT after treatment and follow up. There was no conclusive evidence for superior efficacy of WBV compared with conventional balance training”. |
| 9. Guadarrama-Molina et al. (2020) | Balance | Berg balance scale (score) | - WBV 47.3 ± 4.1 - CT + WBV 45.3 ± 4.5 | - WBV 51.3 ± 2.6 * - CT + WBV 51.13 ± 3.4 * | - CT 48.0 ± 2.9 | - CT 51.3 ± 3.4 * | ns. p = 0.02 | 0.21 0.68 | “Rehabilitation therapy, either conventional, WBV or combined, improved functional balance in patients with PD. Combined therapy had a greater improvement compared to conventional therapy”. |
| 10. Kapur et al. (2012) | Motor symptoms Non-motor symptoms Depression Anxiety Fatigue | MDS-UPDRS-III score MDS-UPDRS I score BD1 score ISQ anxiety FFS score | 36.3 ±9.0 8.3 ± 3.9 6.7 ± 4.6 0.8 ± 1.0 29.9 ± 9.2 | 25.6 ± 14.7 * 6.9 ± 3.4 * 5.2 ± 3.9 * 0.5 ± 0.5 * 26.0 ± 12.0 * | 41.7 ± 9.8 9.5 ± 5.9 7.4 ± 4.9 1.1 ± 1.2 28.6 ± 14.1 | 34.2 ± 13.5 * 6.7 ± 3.2 * 5.0 ± 2.3 * 0.7 ± 1.0 * 23.8 ± 12.3 * | ns. ns. ns. ns. ns. | 0.26 –0.32 –0.21 –0.10 –0.07 | “Auditory sensory stimuli with relaxation in the lounge chair has equivalent benefit as vibration on motor function and mental state”. |
| 11. Corbianco et al. (2018) | Recovery phase Metabolic effects | RER Free fatty acids Branched-chain AAs | 0.90 ± 0.07 N.R. N.R. | 0.87 ± 0.05 N.R. ↑ p < 0.05 * | 0.87 ± 0.05 N.R. N.R. | 0.75 ± 0.04 * ↑ p < 0.01 * ↑ p < 0.01 * | N.R. N.R. N.R. | 1.56 – – | “Both exercise groups, were significantly consumed BCAAs, whereas free Trp, the serotonin precursor, increased. The WBVT does not appear to require a long recovery time and leads to feeling less fatigued, whereas AER needs an appropriate recovery time after the training session”. |
| 12. Arias et al. (2009) | Gait stability Motor symptoms Balance | Gait velocity (m/s) FRT (mm) UPDRS III score Berg balance scale (score) | 0.7 ± 0.2 207.3 ±74.7 27.8 ± 7.5 44.1 ± 8.7 | 0.90 ± 0.2 ** 324.1 ± 51.7 ** 23.0 ± 6.8 * 48.4 ± 7.4 ** | N.R. 221.4 ± 73.6 N.R. N.R. | N.R. 257.2 ± 72.5 * N.R. N.R. | ns. ns. ns. ns. | 1.13 | “There was no difference between the experimental (vibration) and placebo groups in any outcomes. These results suggest that reported benefits of vibration are due to a placebo response”. |
| 13. Gaßner et al. (2014) | Motor symptoms Mobility Stability Gait Balance | UPDRS-III score TUG (s) FRT (m) Step–walk–turn (s) One-leg test (s) | 29 ± 14 11 ± 2.5 0.89 ± 7.4 8.9 ± 1.2 18.9 ± 14.4 | 27 ± 13 9.0 ± 2.2 * 0.92 ± 8.4 7.45 ± 1.5 * 31.5 ± 17.1 * | 19 ± 7 10.1 ± 1.6 0.91 ± 3.9 8.03 ± 1.8 29.4 ± 18 | 18 ± 6 9.7 ± 1.3 * 0.89 ± 3.9 7.29 ± 1.7 * 40.8 ± 19.6* | ns. p = 0.041 p = 0.004 ns. ns. | 0.09 0.79 0.01 0.42 0.07 | “In most of the parameters, a significant interaction of the main outcome measure “time∗group” could not be established. An intervention with random WBV could lead to effects similar to a placebo treatment”. |
| Animal studies | |||||||||
| 14. Zhoa et al. (2014) | Dopamine in striatum BDNF levels striatum | HLPC analysis of dopamine (ng dopamine/mL) Enzyme-linked immunosorbent assay (pg/mL) | – – – – | - MPTP LAV LF 205 ± 66.4 - MPTP LAV HF 206.4 ± 22.0 - MPTP LAV LF 25.0 ± 0.3 - MPTP LAV HF 25.3 ± 0.9 | – – – – | - MPTP 128.3 ± 38.5 - MPTP 24.6 ± 0.2 | p < 0.01 p < 0.01 p < 0.05 p < 0.05 | 1.29 2.30 0.99 1.43 | “Data show that four weeks of vibration training almost completely prevented the MPTP-induced loss of DA neurons in the substantia nigra and reduction in DA levels in the striatum and an upregulation of BDNF”. |
| Reference | Design | Target Population | Sample | Groups (n) | Intervention Duration | Vibration Protocol | |||
|---|---|---|---|---|---|---|---|---|---|
| Type (device, vibration) | Temporal aspects 1 | Intensity (frequency, amplitude 2) | Posture | ||||||
| Outcome measure: neurotransmitters | |||||||||
| Human studies | |||||||||
| 15. Goto and Takamatsu (2005) | Cross-over design | Healthy, young men | N = 8 Sex M/F = 8/0 Mean age = 23.4 | 1 group - WBV + Control (8) | 2 weeks | Galileo 900 Side- alternating | 2 sessions/ 1 session/wk 10 × 60 s | 26 Hz Q2.5 mm | Static squat position |
| Animal studies | |||||||||
| 16. Okada et al. (1983) | RCT | Wistar rats | N = 64 Sex M/F = 64/0 Brains decapitated | 2 groups - WBV (32) - Placebo (32) | 5 h | EMIC 505 Vertical | 1 session 1 × 240 min | 20 Hz N.R | Not fixated |
| 17. Ariizumi and Okada (1985) | RCT | Wistar rats | N = 8 Sex M/F = 8/0 Brains decapitated | 2 groups - WBV (4) - Placebo (4) | 5 h | Emic 505 Vertical | 1 session 1 × 240 min | 20 Hz N.R. | Not fixated |
| 18. Nakamura et al. (1992) | RCT | Wistar rats | N = 10 Sex M/F = 10/0 Brains decapitated | 2 groups - WBV (5) - Noise (5) | 1 day | 505-D: EMIC Vertical | 1 session 1 × 90 min | 20 Hz N.R | Not fixated |
| 19. Heesterbeek et al. (2017) | RCT | C57BI/6J mice | N = 14 Sex M/F = 14/0 | 2 groups - WBV (7) - Pseudo WBV (7) | 5 weeks | LEVELL R.C. Vertical | 25 sessions/ 5 sessions/wk 1 × 10 min | 30 Hz 40–60 µm, 29–75 µm, 14–54 µm | Not fixated |
| Outcome measure: inflammatory markers and neurotrophic factors | |||||||||
| Human studies | |||||||||
| 20. Ribeiro et al. (2018) | RCT | Women with fibromyalgia (FM) and healthy women (HW) | N = 40 Sex M/F = 0/40 Mean age = 51.6 | 2 groups - FM+ WBV (20) - HW + WBV (20) | 1 day | FitVibe Vertical | 1 session 8 × 40 s | 40 Hz 4 mm | Active squats |
| 21. Jawed et al. (2020) | Cross-over design | Young and old adults | N = 11 Sex = N.R. Mean age young = 24 Mean age old = 55 | 1 group - WBV + standing - WBV + squat - Squatting | 2–3 weeks | Power Plate Vertical | 3 sessions/ 1 session/wk 8 × 60 s | 35 Hz 4 mm | Dynamic squatting and standing |
| 22. Rodriguez-Miguelez et al. (2015) | RCT | Elderly subjects | N = 28 Sex M/F = 8/20 Mean age = 70.7 | 2 groups - WBV exercise training program (14) - Daily routine (14) | 8 weeks | Fitvibe Vertical | 16 sessions/ 2 sessions/wk 4 × 30–45–60 s | 20–35 Hz 4 mm | Static and dynamic squats |
| 23. Simao et al. (2019) | RCT | Elderly women with knee osteoarthritis | N = 15 Sex M/F = 0/15 Mean age = 3 | 2 groups - WBV +squats (7) - Squats (8) | 12 weeks | FitVibe Vertical | 36 sessions/ 3 sessions/wk 6 × 20 s, 8 × 40 s | 35–40 Hz 4 mm | Active squats |
| Animal studies | |||||||||
| 24. Raval et al. (2018) | RCT | Senescent female rats + artery occlusion | N = 12 Sex M/F = 0/12 Blood sample | 2 groups - WBV (6) - No WBV (6) | 6 weeks | N.R. | 30 sessions/ 5 sessions/wk 2 sessions/day 2 × 15 min | 40 Hz N.R | Not fixated |
| 25. Wu et al. (2018) | RCT | Apolipoprotein E-deficient mice (atherosclerosis) | N = 16 Sex M/F = 16/0 Blood sample | 2 groups - WBV (8) - No WBV (8) | 12 weeks | Huanzhen Machinery Limited Company Vertical | 72 sessions/ 6 sessions/wk 1 × 10–30–60–120 min | 15 Hz 2 mm | Not fixated |
| Outcome measure: brain-related changes | |||||||||
| Human studies | |||||||||
| 26. Choi et al. (2019) | Cross-over design | Healthy male adults | N = 18 Sex M/F = 18/0 Mean age = 23.4 | 1 group - WBV 27 Hz - WBV 20 Hz - WBV 10 Hz - WBV 0 Hz | 1 day | Galileo® Advanced Plus Side-alternating | 1 session 8 ×/30 s | 0 Hz, 10 Hz, 20 Hz, 27 Hz 4 mm | Slight squat position |
| Animal studies | |||||||||
| 27. Huang et al. (2018) | RCT | Sprague Dawley rats with cerebral ischemia | N = 115 Sex M/F = 115/0 | 3 groups - WBV (50) - No WBV (50) - No cerebral ischemia and WBV (15) | 4 weeks | N.R. | 20 sessions/ 5 session/wk 1 × 30 min | 15 Hz 5 mm | Not fixated |
| 28. Boerema et al. (2018) | RCT | C57Bl/6J mice | N = 20 Sex M/F = 20/0 | 2 groups - WBV (10) - Pseudo-WBV (10) | 5 weeks | LEVELL R.C. Oscillator + Power Amplifier Vertical | 27 sessions/ 5 sessions/wk 1 × 10 min | 30 Hz 0.0537 mm | Not fixated |
| 29. Peng et al. (2021) | RCT | Chronic restraint stress rat model (CRS) | N = 18 Sex M/F = 18/0 Mean age = 3 months | 3 groups - CRS (6) - CRS + WBV (7) - Control (5) | 8 weeks | ZB series- 0977234 Side- alternating | 48 sessions/ 6 sessions/wk 1 × 30 min | 30 Hz 4.5 mm | Not fixated |
| 30. Cariati et al. (2021) | RCT | Wild-type BALB/c male mice (infectious disease) | N = 32 Sex M/F = 32/0 Brains decapitated | 4 groups - Young mice WBV (12) - Old mice WBV (12) - Young mice no WBV (4) - Old mice no WBV (8) | 12 weeks | Power Club Vigarano Mainard Vertical | 36 sessions/ 3 sessions/wk 5 × 3 min, 3 × 2 min | 45 Hz 1.5 mm | Not fixated |
| Outcome measure: oxidative stress | |||||||||
| Human studies | |||||||||
| 31. Santos et al. (2019) | Experimental matched case–control study | Women with fibromyalgia (FM) and healthy women (HW) | N = 42 Sex M/F = 0/42 Mean age = 51.1 | 2 groups - FM (21) - HW (21) | 1 day | FitVibe, Gyma- Uniphy Vertical | 1 session 8 × 40 s | 40 Hz 4 mm | Squatting exercises |
| Animal studies | |||||||||
| 32. Liu et al. (2016) | RCT | Db/db mice (diabetes type 2) | N = 24 Sex M/F = 0/24 Mean age = 8 weeks | 3 groups - Db/db WBV (8) - Db/db (8) - No Db/db and WBV(8) | 12 weeks | N.R. | 84 sessions 1 × 60 min | 45 Hz N.R. | Not fixated |
| Reference | Examined Domains | Outcome Measure | WBV (Mean ± SD) 2 | Control (Mean ± SD) 2 | WBV vs. Control | Effect Size (g) 1 | Main Findings |
|---|---|---|---|---|---|---|---|
| Outcome measure: Neurotransmitters | |||||||
| Human studies | |||||||
| 15. Goto and Takamatsu (2005) | Epinephrine Noradrenaline | Plasma epinephrine (pg/mL) Plasma norepinephrine (pg/mL) | pre 26.7 ± 15.3 post 38.0 ± 14.1 * pre 288.0 ± 109.5 post 456.4 ± 254.3 * | – – | – – | 0.73 0.81 | “A single bout of a WBV session enhanced acute epinephrine and norepinephrine secretion in the blood”. |
| Animal studies | |||||||
| 16. Okada et al. (1983) | Norepinephrine | Norepinephrine in hypothalamus (ng/g) Norepinephrine in hippocampus (ng/g) | post 896.7 ± 461.0 post 664.8 ± 578.7 | post 1891.3 ± 1291.5 post 1176.1 ± 1349.7 | p < 0.01 ns. | –1.01 –0.49 | “WBV caused a decrease in cerebral noradrenalin. The decrease does not occur in the brain generally, but only in particular regions. The hypothalamic content of norepinephrine was most affected, but there was a tendency for norepinephrine content to decrease in the hippocampus”. |
| 17. Ariizumi and Okada (1985) | Cerebral neurotransmitters | Norepinephrine in hypothalamus (ng/g) Dopamine cortex (n/ng) Dopamine striatum (n/ng) Serotonin cerebellum (ng/g) Serotonin in hypothalamus (ng/g) | post 885.4 ± 154.8 post 823.0 ± 102.4 post 332.6 ± 349.8 post 578.3 ± 156.6 * post 2879.7 ± 756.4 * | post 1882.5 ± 447 ** post 631.1 ± 89.6 post 742.0 ± 198 post 289.2 ± 144.6 post 1633.0 ± 361 | p < 0.01 ns. ns. p < 0.05 p < 0.05 | –2.59 1.73 –1.25 1.67 1.83 | “Norepinephrine in the whole brain and especially in the hypothalamus is a better indicator of vibration exposure than serotonin, and norepinephrine is affected by the intensity but not the frequency of vibrations. Noradrenalin and serotonin in the hypothalamus change in the opposite direction. Dopamine concentrations in the brain are basically unaffected by vibration”. |
| 18. Nakamura et al. (1992) | Cerebral dopamine systems in several regions of the brain | Dopamine protein (nucleus accumbens) (ng/mg) Homovanillic acid/dopamine ratio (frontal cortex) (ng/mg) | post 44.9 ± 36.4 post 0.337 ± 0.06 | post 9.4 ± 2.4 post 0.204 ± 0.06 | p = 0.016 p = 0.032 | 1.24 2.00 | “These results suggest that the responses of organisms via acute whole-body vibrations may be critically mediated by cerebral dopamine systems, in particular, by the mesocortical dopamine system.” |
| 19. Heesterbeek et al. (2017) | ChAT- immunoreactivity | Chat-corrected optical density in SS cortex Chat-corrected optical density in basolateral amygdala | post 0.23 ± 0.02 post 0.33 ± 0.03 | post 0.19 ± 0.02 post 0.27 ± 0.03 | p < 0.05 p < 0.01 | 1.87 1.87 | “The results of this study reveal that the positive effects of WBV on attention may be (at least in part) mediated by an increased activity of the NBM cholinergic system. WBV could therefore be a suitable intervention strategy in conditions where a reduced cholinergic forebrain activity plays a role”. |
| Outcome measure: Inflammatory markers and neurotrophic growth factors | |||||||
| Human studies | |||||||
| 20. Ribeiro et al. (2018) | Inflammatory markers Growth factors | Adiponectin (pg/mL) sTNFR1(pg/mL) sTNFR2 (pg/mL) Plasma BDNF (pg/mL) | - HW + WBV: pre 35,977.6 ± 2239.5 post 39,660.1 ± 4926.8 - FM + WBV: pre 43,342.7 ± 1343.7 post 38,102 ± 895.6 * - HW + WBV: pre 697.3 ± 115.1 post 998.7 ± 281.4 * - FM + WBV: pre 1014.8 ± 153.4 post 845.0 ± 63.9 * - HW + WBV: pre 2179.7 ± 296.6 post 2000.9 ± 28.5 - FM + WBV: pre 2179.7 ± 247 post 1789.1 ± 222.3 * - HW + WBV: pre 1696.4 ± 446.5 post 1778.3 ± 446.8 - FM + WBV: pre 1689 ± 329.2 post 1563.0 ± 305.8 | – – – – – – – – | – – – – – – – – | 0.94 –4.50 1.37 –1.42 –0.83 –1.63 0.18 –0.39 | “A single acute session of mild and short WBV can improve the inflammatory status in patients with fibromyalgia (FM), reaching values close to those of matched healthy women (HW) at basal status. The neuroendocrine mechanism seems to be an exercise-induced modulation towards greater adaptation to stress response in these patients”. |
| 21. Jawed et al. (2020) | Inflammatory markers Growth factors | Interleuking 6 (pg/mL) TNF-a (pg/mL) Interleuklin 10 (pg/mL) Vascular endothelial growth factor (VEGF) (pg/mL) | - Standing + WBV 3: pre 24.8 ± 12.6 post 19.4 ± 9.3 pre 21.2 ± 12.9 post 29.8 ± 16.3 * pre 43.1 ± 12.60 post 57.8 ± 16.9 * pre 252.1 ± 12.6 post 269.5 ± 15.3 * | - Squat: pre 19.8 ± 11.6 post 23.4 ± 10.3 pre 29.8 ± 20.6 post 29.9 ± 21.2 pre 44.6 ± 18.6 post 46.5 ± 19.2 pre 253.7 ± 9.6 post 258.2 ± 15.3 | N.R. N.R. N.R. N.R. | –0.78 0.45 0.72 0.93 | “WBV has the potential to positively influence inflammation. Significant increases in TNF-α,VEGF, and IL-10 only occurred during vibration alone, although IL-6 approached a significant drop with vibration alone, with no differences detected with age”. |
| 22. Rodriguez-Miguelez et al. (2015) | Inflammatory markers | TLR2 (% content) TLR4 (%content) TNFa (arbitrary units) | pre 94.3 ± 34.2 post 59.9 ± 40 * pre: 107.8 ± 43.8 post 60.1 ± 22.5 * pre 2.9 ± 1.1 post 1.7 ± 0.8 * | pre 99.7 ± 34.4 post 94.3 ± 40.0 pre 100.1 ± 15.3 post 97.1 ± 35.5 pre 2.9 ± 1.1 post 3.0 ± 0.75 | p < 0.05 p < 0.05 p < 0.05 | –0.76 –1.39 –1.33 | “WBV counteracts, at least in part, age-related low-grade chronic inflammation. This response seems to be mediated by a downregulation of the TLR2 and TLR4 MyD88- and TRIF-dependent signaling pathways”. |
| 23. Simao et al. (2019) | Growth factors | Plasma BDNF (%Δ) | pre 4.78 post +4.2% | pre 3.0 post –32.5% | p < 0.05 | – | “The addition of WBV to squat-exercise training improves lower-limb muscle performance in elderly women with knee osteoarthritis, likely by increasing BDNF, suggestive of a modulation in neuromuscular plasticity”. |
| Animal studies | |||||||
| 24. Raval et al. (2018) | Inflammatory markers Growth factors | Caspase 1 (% region) Interleukin 10 (% region) ASC (% region) b BDNF (% region) pTrK-B (% region) | post 77.4 ± 8.2 post 67.1 ± 24.8 post 84.9 ± 7.4 post 165.7 ± 18.9 post 133.0 ± 10.0 | post 165.6 ± 12.6 post 215.0 ± 11.0 post 141.1 ± 6.1 post 107.0 ± 8.0 post 72.6 ± 13.8 | p < 0.05 p < 0.05 p < 0.05 p < 0.05 p < 0.05 | –7.66 –7.12 –7.65 3.73 4.63 | “WBV induces a significant reduction in inflammatory markers and infarct volume with significant increases in brain-derived neurotrophic factor and improvement in functional activity after tMCAO in middle-aged female rats that were treated with WBV as compared to the non-WBV group”. |
| 25. Wu et al. (2018) | Inflammatory markers Growth factors | Relative protein level IL-6/GAPDH IGF-1 (ng/mL) | post 0.4 ± 0.3 post 167.7 ± 91.3 | post 0.8 ± 0.3 post 272.0 ± 95.3 | p < 0.05 p < 0.05 | –1.26 –1.06 | “The levels of IGF-1 in serum and expression of IL-6 protein in mice aorta decreased significantly in the WBV group compared to control”. |
| Outcome measure: brain-related changes | |||||||
| Human studies | |||||||
| 26. Choi et al. (2019) | Cortical activation during different frequencies of WBV | FNIRS results of: OxyHb concentration 10 Hz OxyHb concentration 20 Hz OxyHb concentration 27 Hz | N.R. | N.R. | p < 0.05 | – | “The results from the present study show that oxyHb concentrations of the motor, prefrontal, and somatosensory cortex areas are higher during the 27 Hz vibration condition than the control or 10 Hz conditions”. |
| Animal studies | |||||||
| 27. Huang et al. (2018) | Neurogenesis | Neu/BrdU-labelled cells in cortex | - Ischemia + WBV: 14 d: post 4.0 ± 13.4 21 d: post 13.9± 21.9 28 d: post 28.0± 26.9 | - Ischemia: 14 d: post 3.0 ± 7.4 21 d: post 9.9 ± 21.2 28 d: post 18.9 ± 35.4 | ns. p < 0.001 p < 0.001 | 0.09 0.18 0.29 | “WBV promoted neurogenesis after long-term exposure after cerebral ischemia in rats.” |
| 28. Boerema et al. (2018) | Brain glucose uptake | F-FDG uptake (%ID/g) | pre 3.8 ± 0.7 post 3.9 ± 0.7 | pre 3.7 ± 0.7 post 4.0 ± 0.7 | ns. ns. | –0.27 | “The 18F-FDG PET data does not reveal any significant difference in brain uptake ratio due to WBV. There was a small but not significant increase in the pseudo WBV group post-treatment”. |
| 29. Peng et al. (2021) | Neurons Neural degeneration Neurotropic factors | Neun (n of surviving neurons) F-Jade C (% of control) IGF-1 (ng/mL) BDNF (ng/mL) | - CRS + WBV: post 86.0 ± 16.4 - CRS + WBV: post 125.9 ± 63.8 - CRS+ WBV: post 43.9 ± 11.1 - CRS + WBV: post 676.1 ± 46.6 | - CRS: post 62.9 ± 14.7 - Control 4: post 109.2 ± 18.8 - CRS: post 870.5 ± 704.5 - Control4: post 80.4 ± 53.9 - CRS post 27.4 ± 14.5 - Control 4 post 41.7 ± 9.4 - CRS: post 506.3 ± 107.5 - Control 4 post 831.2 ± 327.1 | p < 0.05 p < 0.05 p < 0.05 p < 0.05 | 1.37 –1.45 1.20 1.97 | “WBV could reverse behavioral dysfunction, inhibit the degeneration of neurons, alleviate the damage of neurons and the pathological changes of glial cells, enhance trophic factor expression, and ameliorate the downregulation of dendritic and synaptic proteins after CRS. The effect of WBV in rats may be mediated via the reduction in hippocampal neuronal degeneration and by improving expression of synaptic proteins”. |
| 30. Cariati et al. (2021) | Hippocampal synaptic plasticity | %PS amplitude | - Young mice + WBV: pre 101.4 ± 3.1 post 386.8 ± 87.3 * - Old mice + WBV: pre 101.4 ± 3.1 post 466.9 ± 151.4 ** | - Young mice: pre 100.3 ± 2.0 post 325.2 ± 53.6 * - Old mice: pre 101.5 ± 2.0 post 249.5 ± 90.4 * | ns. p < 0.05 | 0.99 2.25 | “Vibratory training can modulate synaptic plasticity differently, depending on the protocol used, and that the best effects are related to the training protocol characterized by a low vibration frequency and a longer recovery time (3 × 150 s, 45 Hz WBV)”. |
| Outcome measure: Oxidative Stress | |||||||
| Human studies | |||||||
| 31. Santos et al. (2019) | Oxidative stress markers | TBARS FRAP SOD CAT | - HW + WBV: post 0.14 ± 0.13 - FM + WBV: post 0.2 ± 0.18 * - HW + WBV: post 180.0 ± 103.6 - FM + WBV: post 239.1 ± 82.9 * - HW + WBV: post 1.9 ± 0.09 * - FM + WBV: post 1.1 ± 0.18 * - HW + WBV: post 31.2 ± 14.2 * - FM + WBV: post 2.6 ± 1.3 | - HW: post 0.2 ± 0.18 - FM: post 0.8 ± 1.4 - HW: post 188.3 ± 78.8 - FM: post 485.6 ± 208.5 - HW: post 1.1 ± 1.8 - FM: post 0.9 ± 0.91 - HW: post 7.5 ± 17.8 - FM: post 3.8 ± 8.7 | ns. p < 0.05 ns. p < 0.05 p < 0.05 p < 0.05 p < 0.05 p < 0.05 | –0.37 –0.59 –0.09 –1.52 0.62 0.30 1.44 –0.19 | “A single trial of WBV exercise improved all oxidant and antioxidant parameters towards a greater adaptation to the stress response in women with fibromyalgia (FM) as compared to the healthy women group (HW)”. |
| Animal studies | |||||||
| 32. Liu et al. (2016) | Oxidative stress | GSH (µmol/L) GSH-Px (u/mgprotein) | - Db/db + WBV: post 282.5 ± 69.3 - Db/db + WBV: post 923.8 ± 9.6 | - Db/db: post 195.5 ± 24.0 - Db/db: post 880.5 ± 156.7 | p < 0.05 ns. | 1.59 0.37 | “WBV attenuates oxidative stress to ameliorate liver steatosis and thus improves insulin resistance in db/db mice. Therefore, WBV administration is a promising treatment for individuals who suffered from central obesity and IR”. |
| Recommendations for Practice | Recommendations for Further Research |
|---|---|
| Apply WBV if moderate-to-high conventional exercise not possible or additional to conventional exercise | High-quality research with sufficient duration (≥3 weeks), session frequency (≥3 sessions/week) and vibration frequency (≥20 Hz) |
| At least three sessions per week | RCTs with contrasting control groups |
| Vibration frequency of at least 20 Hz | RCTs with different levels for frequency and/or peak-to-peak displacement |
| Start under adequate supervision | Trials with side-alternating WBV |
| Add cognitive function and other non-motor variables affected by PD to outcomes | |
| Animal research using PD mouse models and/or PD-disease-relevant cellular models | |
| Improve reporting on WBV studies using guidelines (van Heuvelen et al., 2021) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arenales Arauz, Y.L.; Ahuja, G.; Kamsma, Y.P.T.; Kortholt, A.; van der Zee, E.A.; van Heuvelen, M.J.G. Potential of Whole-Body Vibration in Parkinson’s Disease: A Systematic Review and Meta-Analysis of Human and Animal Studies. Biology 2022, 11, 1238. https://doi.org/10.3390/biology11081238
Arenales Arauz YL, Ahuja G, Kamsma YPT, Kortholt A, van der Zee EA, van Heuvelen MJG. Potential of Whole-Body Vibration in Parkinson’s Disease: A Systematic Review and Meta-Analysis of Human and Animal Studies. Biology. 2022; 11(8):1238. https://doi.org/10.3390/biology11081238
Chicago/Turabian StyleArenales Arauz, Y. Laurisa, Gargi Ahuja, Ype P. T. Kamsma, Arjan Kortholt, Eddy A. van der Zee, and Marieke J. G. van Heuvelen. 2022. "Potential of Whole-Body Vibration in Parkinson’s Disease: A Systematic Review and Meta-Analysis of Human and Animal Studies" Biology 11, no. 8: 1238. https://doi.org/10.3390/biology11081238
APA StyleArenales Arauz, Y. L., Ahuja, G., Kamsma, Y. P. T., Kortholt, A., van der Zee, E. A., & van Heuvelen, M. J. G. (2022). Potential of Whole-Body Vibration in Parkinson’s Disease: A Systematic Review and Meta-Analysis of Human and Animal Studies. Biology, 11(8), 1238. https://doi.org/10.3390/biology11081238







