A Systematic Review of the Effectiveness of Dry Needling in Subacromial Syndrome
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Selection Criteria
2.3. Measures
2.4. Data Sources
2.5. Exclusion Criteria
2.6. Data Extraction
2.7. Methodological Quality Assessment
3. Results
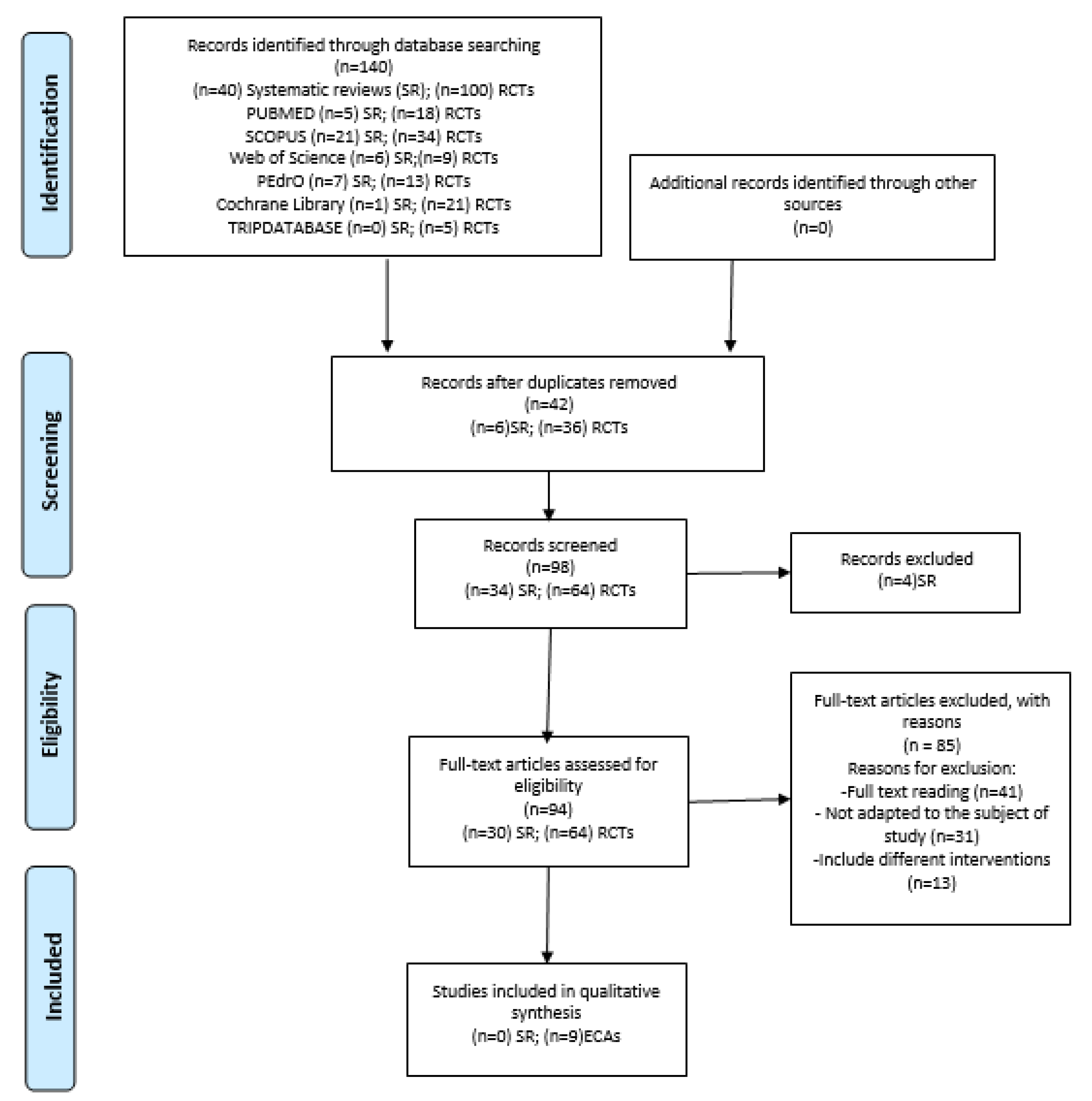
3.1. Selection of Studies
3.2. Quality of Studies Included
3.3. Study Characteristics
- ▪
- Intensity of Pain
- ▪
- Range of Movement
- ▪
- Pain Pressure Threshold
- ▪
- Functional Assessment
- ▪
- Cost–Benefit Ratio
3.4. Characteristics of the Interventions
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Databases | Search Strategy |
|---|---|
| PUBMED (up to current date, 2021) (SR no limit date; RCTs from 2016 until 16 December 2021) |
|
| SCOPUS (up to current date, 2021) (SR no limit date; RCTs from 2016 until 16 December 2021) | I./II. [no MeSH terms]: “Dry” AND “needling” AND “Shoulder” AND “pain” AND “physiotherapy” |
| Web of Science (up to current date, 2021) (SR no limit date; RCTs from 2016 until 16 December 2021) | I./II. [no MeSH terms]: “Dry” AND “needling” AND “Shoulder” AND “pain” AND “physiotherapy” |
| PEDro (up to current date, 2021) (SR no limit date; RCTs from 2016 until 16 December 2021) | I./II. [no MeSH terms]: “Dry” AND “shoulder” |
| Cochrane Library (up to current date, 2021) (SR no limit date; RCTs from 2016 until 16 December 2021) | I./II. [MeSH tems]: “Impigement syndrome” AND “needles” |
| Tripdatabase (up to current date, 2021) (SR no limit date; RCTs from 2016 until 16 December 2021) | I./II. [no MeSH terms]: “Dry” AND “Needling” AND “Shoulder” AND “pain” AND “physiotherapy” |
References
- Michener, L.A.; McClure, P.W.; Karduna, A.R. Anatomical and biomechanical mechanisms of subacromial impingement syndrome. Clin. Biomech. 2003, 18, 369–379. [Google Scholar] [CrossRef]
- Kachingwe, A.F.; Phillips, B.; Sletten, E.; Plunkett, S.W. Comparison of manual therapy techniques with therapeutic exercise in the treatment of shoulder impingement: A randomized controlled pilot clinical trial. J. Man. Manip. Ther. 2008, 16, 238–247. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Javed, M.A.; Saleem, S.; Raza, M.K.H. Management of muscle trigger points causing subacromial pain using dry needling technique—A case report. J. Pak. Med. Assoc. 2020, 27, 28. [Google Scholar] [CrossRef]
- Abad Querol, J.; Morales Jimenez, M.; Martínez Lentisco, M. Effectiveness of Different Models of Phisiotherapy for the treatment subacromial sindrome in primary care. Rev sanit Investig. 2021, 2, 1–12. [Google Scholar]
- Navarro-Santana, M.J.; Gómez-Chiguano, G.F.; Cleland, J.A.; Arias-Buría, J.L.; Fernández-De-Las-Peñas, C.; Plaza-Manzano, G. Effects of trigger point dry needling for nontraumatic shoulder pain of musculoskeletal origin: A systematic review and meta-analysis. Phys. Ther. 2020, 101, 1–11. [Google Scholar] [CrossRef]
- Tejera-Falcón, E.; Del Carmen Toledo-Martel, N.; Sosa-Medina, F.M.; Santana-González, F.; Gallego-Izquierdo, T.; Pecos-Martín, D. Dry needling in a manual physiotherapy and therapeutic exercise protocol for patients with chronic mechanical shoulder pain of unspecific origin: A protocol for a randomized control trial. BMC Musculoskelet. Disord. 2017, 18, 400. [Google Scholar] [CrossRef] [Green Version]
- Kalichman, L.; Vulfsons, S. Dry needling in the management of musculoskeletal pain. J. Am. Board Fam. Med. 2010, 23, 640–646. [Google Scholar] [CrossRef] [Green Version]
- Hall, M.L.; Mackie, A.C.; Ribeiro, D.C. Effects of dry needling trigger point therapy in the shoulder region on patients with upper extremity pain and dysfunction: A systematic review with meta-analysis. Physiotherapy 2018, 104, 167–177. [Google Scholar] [CrossRef]
- Travell, J.G.; Simons, D.G. Myofascial Pain and Dysfunction: The Trigger Point Manual; Williams & Wilkins: Philadelphia, PA, USA, 1999. [Google Scholar]
- Lewit, K. The needle effect in the relief of myofascial pain. Pain 1979, 6, 83–90. [Google Scholar] [CrossRef]
- De Meulemeester, K.E.; Castelein, B.; Coppieters, I.; Barbe, T.; Cools, A.; Cagnie, B. Comparing trigger point dry needling and manual pressure technique for the management of myofascial neck/shoulder pain: A randomized clinical trial. J. Manip. Physiol. Ther. 2017, 40, 11–20. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stone, P.W. Popping the (PICO) question in research and evidence-based practice. Appl. Nurs. Res. 2002, 15, 197–198. [Google Scholar] [CrossRef] [PubMed]
- McCormack, H.M.; De LHorne, D.J.; Sheather, S. Clinical applications of visual analogue scales: A critical review. Psychol. Med. 1988, 18, 1007–1019. [Google Scholar] [CrossRef] [PubMed]
- Haefeli, M.; Elfering, A. Pain assessment. Eur. Spine J. 2005, 15 (Suppl. 1), S17–S24. [Google Scholar] [CrossRef]
- Vartiainen, P.; Mäntyselkä, P.; Heiskanen, T.; Hagelberg, N.; Mustola, S.; Forssell, H.; Kautiainen, H.; Kalso, E. Validation of EQ-5D and 15D in the assessment of health-related quality of life in chronic pain. Pain 2017, 158, 1577–1585. [Google Scholar] [CrossRef]
- Salomon, J.A. Quality Adjusted Life Years. In The International Encyclopedia of Public Health. Elsevier; 2017. p. 224–228. In The International Encyclopedia of Public Health; Elsevier: Amsterdam, The Netherlands, 2017; pp. 224–228. [Google Scholar] [CrossRef]
- Park, G.; Kim, C.W.; Park, S.B.; Kim, M.J.; Jang, S.H. Reliability and usefulness of the pressure pain threshold measurement in patients with myofascial pain. Ann. Rehabil. Med. 2011, 35, 412–417. [Google Scholar] [CrossRef] [Green Version]
- De Groef, A.; Van Kampen, M.; Dieltjens, E.; Christiaens, M.-R.; Neven, P.; Geraerts, I.; Devoogdt, N. Effectiveness of postoperative physical therapy for upper-limb impairments after breast cancer treatment: A systematic review. Arch. Phys. Med. Rehabil. 2015, 96, 1140–1153. [Google Scholar] [CrossRef]
- Leggin, B.G.; Michener, L.A.; Shaffer, M.A.; Brenneman, S.K.; Iannotti, J.P.; Williams, G.R. The Penn Shoulder Score: Reliability and validity. J. Orthop. Sports Phys. Ther. 2006, 36, 138–151. [Google Scholar] [CrossRef]
- Haley, S.M.; Fragala-Pinkham, M.A. Interpreting change scores of tests and measures used in physical therapy. Phys. Ther. 2006, 86, 735–743. [Google Scholar] [CrossRef] [Green Version]
- Breckenridge, J.D.; McAuley, J.H. Shoulder Pain and Disability Index (SPADI). J. Physiother. 2011, 57, 197. [Google Scholar] [CrossRef] [Green Version]
- Horn, K.K.; Jennings, S.; Richardson, G.; Vliet DVan Hefford, C.; Abbott, J.H. The patient-specific functional scale: Psychometrics, clinimetrics, and application as a clinical outcome measure. J. Orthop. Sports Phys. Ther. 2012, 42, 30–42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verhagen, A.P.; De Vet, H.C.W.; De Bie, R.A.; Boers, M.; Van Den Brandt, P.A. The art of quality assessment of RCTs included in systematic reviews. J. Clin. Epidemiol. 2001, 54, 651–654. [Google Scholar] [CrossRef]
- Kamali, F.; Sinaei, E.; Morovati, M. Comparison of upper trapezius and infraspinatus myofascial trigger point therapy by dry needling in overhead athletes with unilateral shoulder impingement syndrome. J. Sport Rehabil. 2019, 28, 243–249. [Google Scholar] [CrossRef]
- Jalilipanah, P.; Okhovatian, F.; Serri, R.A.; Bagban, A.A.; Zamani, S. The effect of dry needling and muscle energy technique separately and in combination in patients suffering shoulder impingement syndrome and active trigger points of infraspinatus. J. Bodyw. Mov. Ther. 2020, 26, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Koppenhaver, S.; Embry, R.; Ciccarello, J.; Waltrip, J.; Pike, R.; Walker, M.; Fernández-De-Las-Peñas, C.; Croy, T.; Flynn, T. Effects of dry needling to the symptomatic versus control shoulder in patients with unilateral subacromial pain syndrome. Man. Ther. 2016, 26, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Arias-Buría, J.L.; Fernández-de-Las-Peñas, C.; Palacios-Ceña, M.; Koppenhaver, S.L.; Salom-Moreno, J. Exercises and Dry Needling for Subacromial Pain Syndrome: A Randomized Parallel-Group Trial. J. Pain 2016, 18, 11–18. [Google Scholar] [CrossRef] [Green Version]
- Arias-Buría, J.L.; Martín-Saborido, C.; Cleland, J.; Koppenhaver, S.L.; Plaza-Manzano, G.; Fernández-de-Las-Peñas, C. Cost-effectiveness evaluation of the inclusion of dry needling into an exercise program for subacromial pain syndrome: Evidence from a randomized clinical trial. Pain Med. 2018, 19, 2336–2347. [Google Scholar] [CrossRef]
- Imani, M.; Abbasi, L.; Taghizadeh, S.; Amiri, M. Comparison of the effect of two different types of dry-needling techniques on subacromial impingement syndrome. J. Bodyw. Mov. Ther. 2020, 25, 35–40. [Google Scholar] [CrossRef]
- Kheradmandi, A.; Kamali, F.; Ebrahimian, M.; Abbasi, L. Comparison between dry needling plus manual therapy with manual therapy alone on pain and function in overhead athletes with scapular dyskinesia: A randomized clinical trial. J. Bodyw. Mov. Ther. 2020, 26, 339–346. [Google Scholar] [CrossRef]
- Halle, R.; Crowell, M.; Goss, D. Dry needling and physical therapy versus physical therapy alone following shoulder stabilization repair: A randomized clinical trial. Int. J. Sports Phys. Ther. 2020, 15, 81–102. [Google Scholar] [CrossRef]
- Ekici, G.; Özcan, Ş.; Öztürk, B.Y.; Öztürk, B.; Ekici, B. Effects of deep friction massage and dry needling therapy on night pain and shoulder internal rotation in subacromial pain syndrome: 1-year follow up of a randomised controlled trial. Int. J. Ther. Rehabil. 2021, 28, 1–12. [Google Scholar] [CrossRef]
- Jadad, A.R.; Moore, R.A.; Carroll, D.; Jenkinson, C.; Reynolds, D.J.; Gavaghan, D.J.; McQuay, H.J. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control. Clin. Trials 1996, 17, 1–12. [Google Scholar] [CrossRef]
- Hando, B.R.; Rhon, D.I.; Cleland, J.A.; Snodgrass, S.J. Dry needling in addition to standard physical therapy treatment for sub-acromial pain syndrome: A randomized controlled trial protocol. Braz. J. Phys. Ther. 2018, 23, 355–363. [Google Scholar] [CrossRef] [PubMed]
- Diercks, R.; Bron, C.; Dorrestijn, O.; Meskers, C.; Naber, R.; de Ruiter, T.; Willems, J.; Winters, J.; van der Woude, H.J. Guideline for diagnosis and treatment of subacromial pain syndrome. Acta Orthop. 2014, 85, 314–322. [Google Scholar] [CrossRef] [Green Version]
- Mejuto-Vázquez, M.J.; Salom-Moreno, J.; Ortega-Santiago, R.; Truyols-Domínguez, S.; Fernández-de-Las-Peñas, C. Short-term changes in neck pain, widespread pressure pain sensitivity, and cervical range of motion after the application of trigger point dry needling in patients with acute mechanical neck pain: A randomized clinical trial. J. Orthop. Sports Phys. Ther. 2014, 44, 252–260. [Google Scholar] [CrossRef] [Green Version]
- Chaitow, L. Muscle Energy Techniques; Elsevier: Amsterdam, The Netherlands, 2006. [Google Scholar]
- Kietrys, D.M.; Palombaro, K.M.; Mannheimer, J.S. Dry needling for management of pain in the upper quarter and craniofacial region. Curr. Pain Headache Rep. 2014, 18, 437. [Google Scholar] [CrossRef]
- Segura-Pérez, M.; Hernández-Criado, M.T.; Calvo-Lobo, C.; Vega-Piris, L.; Fernández-Martín, R.; Rodríguez-Sanz, D. A Multimodal Approach for Myofascial Pain Syndrome: A Prospective Study. J. Manip. Physiol. Ther. 2017, 40, 397–403. [Google Scholar] [CrossRef]
- Sutlive, T.G.; Golden, A.; King, K.; Morris, W.B.; Morrison, J.E.; Moore, J.H.; Koppenhaver, S. Short-term effects of trigger point dry needling on pain and disability in subjects with patellofemoral pain syndrome. Int. J. Sports Phys. Ther. 2018, 13, 462–473. [Google Scholar] [CrossRef] [Green Version]
- Gattie, E.; Cleland, J.A.; Snodgrass, S. The effectiveness of trigger point dry needling for musculoskeletal conditions by physical therapists: A systematic review and meta-analysis. J. Orthop. Sports Phys. Ther. 2017, 47, 133–149. [Google Scholar] [CrossRef]
- Izquierdo, M. Biomecánica y Bases Neuromusculares de La Actividad Física y El Deporte; Editorial Médica Panamericana: Madrid, Spain, 2008. [Google Scholar]
- American College of Sports Medicine (Estados Unidos). Manual ACSM Para La Valoración y Prescripción Del Ejercicio; Paidotribo: Barcelona, Spain, 2014. [Google Scholar]
- Abdulla, S.Y.; Southerst, D.; Côté, P.; Shearer, H.M.; Sutton, D.; Randhawa, K.; Varatharajan, S.; Wong, J.J.; Yu, H.; Marchand, A.-A.; et al. Is exercise effective for the management of subacromial impingement syndrome and other soft tissue injuries of the shoulder? A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Man. Ther. 2015, 20, 646–656. [Google Scholar] [CrossRef]
- Faber, E.; Kuiper, J.I.; Burdorf, A.; Miedema, H.S.; Verhaar, J.A.N. Treatment of impingement syndrome: A systematic review of the effects on functional limitations and return to work. J. Occup. Rehabil. 2006, 16, 6–24. [Google Scholar] [CrossRef] [PubMed]
- Roy, J.-S.; MacDermid, J.C.; Woodhouse, L.J. Measuring shoulder function: A systematic review of four questionnaires. Arthritis Care Res. 2009, 61, 623–632. [Google Scholar] [CrossRef] [PubMed]
- Romero-Morales, C.; Bravo-Aguilar, M.; Abuín-Porras, V.; Almazán-Polo, J.; Calvo-Lobo, C.; Martínez-Jiménez, E.M.; López-López, D.; Navarro-Flores, E. Current advances and novel research on minimal invasive techniques for musculoskeletal disorders. Disease-a-Month 2021, 67, 101210. [Google Scholar] [CrossRef] [PubMed]
| VARIABLES |
|---|
| Pain: VAS, NPRS |
| Function: PSFS, ROM, PSFS, scapular dyskinesia, infraspinatus muscle function. |
| Shoulder assessment: DASH, PSS, GROC, SPADI. |
| Quality of life: Euro-QoL-D5, QALY |
| Muscular sensitivity: PPT, pressure algometer |
| PEDro Criterion | Arias-Buría et al. [16] | Arias-Buría et al. [17] | Kheradmandi et al. [19] | Imani et al. [18] | Kamali et al. [23] | Halle et al. [20] | Ekici et al. [21] | Jalilipaanah et al. [22] | Koppenhaver et al. [15] |
|---|---|---|---|---|---|---|---|---|---|
| 1 * | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 3 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | - |
| 4 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 5 | 1 | 1 | 1 | 1 | - | 1 | - | - | - |
| 6 | 1 | 1 | 1 | 1 | - | 1 | 1 | - | 1 |
| 7 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | - | - |
| 8 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 9 | 1 | 1 | - | - | - | 1 | 1 | - | 1 |
| 10 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 11 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Total | 10/10 | 10/10 | 9/10 | 9/10 | 7/10 | 10/10 | 9/10 | 6/10 | 7/10 |
| JADAD SCALE | TOTAL | ||||||
|---|---|---|---|---|---|---|---|
| Author | Title | 1 | 2 | 3 | 4 | 5 | Σ |
| Arias-Buría J.L., et al., 2017 [28] | Exercises and Dry Needling for Subacromial Pain Syndrome: A Randomized Parallel-Group Trial. J pain. 2017;18(1):11–18. doi:10.1016/j.jpain.2016.08.013 | 1 | 1 | 0 | 1 | 1 | 4 |
| Arias-Buría J.L., et al., 2018 [29] | Cost-effectiveness Evaluation of the Inclusion of Dry Needling into an Exercise Program for Subacromial Pain Syndrome: Evidence from a Randomized Clinical Trial. Pain Med. 2018;19(12):2336–2347. doi:10.1093/pm/pny021 | 1 | 1 | 0 | 1 | 1 | 4 |
| Kheradmandi A., Kamali F., Ebrahimian M., Abbasi L. 2021 [31] | Comparison between dry needling plus manual therapy with manual therapy alone on pain and function in overhead athletes with scapular dyskinesia; A randomized clinical trial. J Bodyw Mov Ther. 2021 Apr:26:339–346. Doi:10.1016/j.jbmt.2020.11.017. Epub 2020 Nov 24. PMID: 33992267. | 1 | 1 | 0 | 1 | 1 | 4 |
| Imani M., Abbasi L., Taghizadeh S., Amiri M., 2021 [30] | Comparison of the effect of two different types of dry-needling techniques on subacromial impingement syndrome. J Bodyw Mov Ther. 2021;25:35–40. doi:10.1016/j.jbmt.2020.10.018 | 1 | 1 | 0 | 1 | 0 | 3 |
| Kamali F., et al., 2019 [25] | Comparison of Upper Trapezius and Infraspinatus Myofascial Trigger Point Therapy by Dry Needling in Overhead Athletes With Unilateral Shoulder Impingement Syndrome. J Sport Rehabil. 2019;28(3):243–249. doi:10.1123/jsr.2017-0207 | NA | NA | NA | NA | NA | NA |
| Halle R, Crowell M, Goss D., 2020 [32] | Dry needling and physical therapy versus physical therapy alone following shoulder stabilization repair: a randomized clinical trial. Int J Sports Phys Ther. 2020;15(1):81–102. | 1 | 1 | 0 | 1 | 1 | 4 |
| Ekici G, Özcan Ş, Öztürk BY, Öztürk B, Ekici B., 2021 [33] | Effects of Deep Friction Massage and Dry Needling therapy on Night Pain and Shoulder Internal Rotation in Subacromial Pain Syndrome: 1-year Follow up of a Randomised Controlled Trial. Int J Ther Rehabil. 2021;28(2):1–12. doi:10.12968/ijtr.2020.0018 | 1 | 1 | 0 | 1 | 1 | 4 |
| Jalilipanah P., Okhovatian F., Serri R.A., Bagban A.A., Zamani S., 2021 [26] | The effect of Dry Needling and Muscle Energy Technique Separately and in Combination in Patients Suffering Shoulder Impingement Syndrome and Active Trigger Points of Infraspinatus. J Bodyw Mov Ther. 2021; 26:94–100. doi:10.1016/j.jbmt.2020.12.030 | 1 | 1 | 0 | 1 | 0 | 3 |
| Koppenhaver S., et al., 2016 [27] | Effects of Dry Needling to the Symptomatic versus Control Shoulder in Patients with Unilateral Subacromial Pain Syndrome. Man Ther. 2016;26:62–69. doi:10.1016/j.math.2016.07.009 | NA | NA | NA | NA | NA | NA |
| References | Participant Profile | Intervention | Follow-Up | Variables | Results | Conclusions | Adverse Effects and Limitations |
|---|---|---|---|---|---|---|---|
| Koppenhaver S., et al., 2016 [27] | n = 57 Female: n = 35.7% Male: n = 64.3% Age 44.1 ± 10.1 yo Department of Defense beneficiaries, from Joint Base San Antonio, Texas. Individuals who would seek healthcare for unilateral SAPS without any contraindications to DN. | DN in ISP muscle | Duration: 1 W Measurements: Basal immediately after treatment. |
|
| Found changes in shoulder ROM and pain sensitivity, but not in muscle function, after DN. These changes generally occurred 3–4 days after DN and only in the symptomatic shoulders. | No adverse effects or pain. |
| Arias-Buría J.L., et al., 2017 [28] | n = 50 (EG: 25/CG: 25) Female: n = 6 Male: n = 19 Age ± 48 yo Consecutive subjects with diagnosis of SAPS from a Spanish regional hospital. | EG: TE CG: TE + DDN | Duration: twice a day for 5 W Measurements: Basal:
|
| DASH: S.I. in EG, 1 week after, at 3/6 and 12 M compared to the CG (p < 0.001) PI: Improvement in both groups. No significant differences in worst pain (p = 0.43) Losses (n = 3): CG (n = 2) EG (n = 1) | The inclusion of two sessions of TrP-DN into a TE program was effective for improving shoulder pain-related disability in the short, medium, and long term | No greater improvement in shoulder pain was observed. |
| Arias-Buría J.L., et al., 2018 [29] | N = 50 (EG: 25/CG:25) Female: n = 13 Male: n = 37 Age EG 48 ± 5 yo Age CG 49 ± 4 yo Patients with unilateral nontraumatic shoulder pain of at least 3 M duration and PI of at least 4 points on an 11-point NPRS, from an urban hospital in Madrid, Spain. | EG: Exercise program + TrP-DN CG: Exercise program alone | Duration: twice a day for W Measurements: Basal, 1/3/6 and 12 M | EuroQol-D5 | EuroQol-D5: Greater number of visits to orthopedic surgeon and greater number of treatments added in CG (p < 0.001) Statistically significant differences in relation to absenteeism from work which is greater in CG (p = 0.001) Greater quality of life in EG (+2.87 QALY) Cost-benefit: EUR −12,933.54 per year in EG Losses (n = 0) | The inclusion of TrP-DN into an exercise program was more cost-effective for individuals with SAPS than exercise alone. | No greater improvement in shoulder pain was observed. |
| Imani M., Abbasi L., Taghizadeh S., Amiri M., 2021 [30] | n= 66 (EG1 = EG2 = CG: 22) Female: n = 42 Male: n = 24 Age 43.24 ± 9.961 yo Patients with shoulder impingement syndrome. | EG1: TE + E + TM + SDDN EG2: TE + E + TM + HDDN CG: TE + E + TM | Duration: nine physiotherapy sessions Measurements: Basal immediately after, and at 4 W |
| PI: Significant reduction in all groups immediately after treatment (p = < 0.05), positive trend maintained for EG1 Level of disability: S.I. in EG1 at the end of the study (p < 0.05) Losses (n = 8): CG (n = 2), EG1(n = 3),EG2 (n = 1) | There was no significant difference between the three groups in pressure pain tolerance threshold and pain reduction. | No greater improvement in shoulder pain was observed. |
| Kheradmandi A., Kamali F., Ebrahimian M., Abbasi L. 2021 [31] | n = 40 Female: n = 25 Male: n = 15 (EG: 20/CG:20) Age: 18–45 yo Athletes with SD With at least three points NRS PI during training | EG: MT + DN in TP of Subescapularis, pectoralis minor, Serratus anterior, upper and lower Trapezius muscles CG: MT alone | Duration: three sessions with the interval of every 3 days. |
| Pain, disability and SD were improved in EG (p < 0.05) CG: reduction in pain and disability (p < 0.001). Scapular slide only improved in hands on waist position. Comparing the differences between groups improvement in SD in EG (p = 0.02). PPT significantly increased in the CG (p = 0.004). Losses (n = 0) | DN is an easy and applicable method that can synergistically reduce pain, disability and SD when it is combined with MT techniques to treat shoulder dysfunctions. | No adverse effects reported by the participants. |
| Halle R, Crowell M, Goss D., 2020 [32] | N = 39 (EG: 19/CG: 20) Female: n = 6 Male: n = 34 Age 20.78 ± 3.33 Post-operative shoulder patients. | EG: SPP + HDDN CG: SPP | Duration: 6 M Measurements: 4/8/12 W, and 6 M post-operation |
| No significant differences, except in shoulder flexion in CG (p = 0.019) | DN in a postsurgical population is safe. | Without significant risk of iatrogenic infection or other adverse events. |
| Ekici G, Özcan Ş, Öztürk BY, Öztürk B, Ekici B., 2021 [33] | n = 40 (EG1: 19/EG2: 21) Female: n = 31 Male: n = 18 Age EG1: 50.90 ± 7.88 yo Age EG2: 52.04 ± 8.98 yo Outpatients diagnosed with SAPS. | GE1:TrP Deep friction massage GE2: TrP-DN | Duration: 4 W (six physiotherapy sessions) Measurements: Basal: 4 W, 12 M |
| Improvement in all parameters measured, but with NO significant differences between groups except for internal rotation of shoulder after 12 M follow-up (p < 0.05) in favor of the EG and reduction of night pain. Losses (n = 19): CG (n = 11) EG (n = 8) | Both interventions produced good results, TrP deep friction massage treatments were completed in a shorter time and so demonstrated earlier improvements. TrP deep friction massage may be regarded as the preferred option, particularly as no equipment is needed and it is a non-invasive method of treatment. | No adverse effects reported by the participants. |
| Jalilipanah p., Okhovatian F., Serri R.A., Bagban A.A., Zamani S., 2021 [26] | n = 39 (EG1 = E2 = EG3: 13) Age: 20–50 yo Patients with shoulder impingement Syndrome and active TrP in the ISP muscle. | EG1: HDDN EG2: Post-isometric relaxation GE3: HDDN + post-isometric relaxation | Duration: 1 W Measurements: Basal |
| PI: Improvement in all groups, NO significant differences between groups. PPT: Improvement in all groups, NO significant differences between groups Shoulder ROM: Improvement in all groups, Significant differences in EG1 and EG2 compared to EG2 Losses (n = 0) | Both techniques are effective in the treatment of TrP. DN is more effective in enhancing the ROM of flexion and abduction. | No adverse effects reported by the participants. |
| Kamali F., et al., 2019 [25] | n = 40 Females: n = 20 Males: n = 20 (EG1: 21/EG2:19) Age: 36 ± 16 yo Overhead athletes. | EG1: HDDN in descending Trapezius EG2: DDN in Infraspinatus | Measurements: Basal and 3 days after treatment |
| PI: SI in both groups. PPT: SI in EG2 (p = 0.02), although NO significant difference between groups. DASH: NO significant differences. Losses (n = 6) | Application of DN for active MTrPs in the ISP can be as effective as direct DN of active MTrPs in the UT in improving pain and disability in athletes with SP, and may be preferred due to greater patient comfort in comparison with direct UT needling. | No adverse effects reported by the participants. |
| Author/Year | n/Number of Therapeutic Groups | Type | Time Per Session | Number of Sessions | Length of Intervention | Observations |
|---|---|---|---|---|---|---|
| Koppenhaver S., et al., 2016 [27] | 57/1 | DN technique used disposable 0.25 × 40 mm stainless Steel Seirin J-type needles. Treatment location was standardized for each participant. Needles were inserted into three general locations (superior, medial, inferior) in each ISP based on prior research and depictions of common locations of MTrP. Prior to needle insertion, manual palpation of the ISP was performed to localize treatment to the most painful area at each of the three locations. Each needle insertion lasted approximately 5–10 s, using a “sparrow pecking” (in and out motion) technique in an attempt to elicit as many local twitch responses as possible. | 5 min | One | 1 D | No statistically significant changes found in either resting or contracted infraspinatus muscle function in either shoulder at any time point. |
| Arias-Buría J.L., et al., 2017 [28] * | 50/2 | The protocol included the same exercise program. Each exercise was performed in three sets of 12 repetitions; each repetition included a concentric phase after the eccentric phase of the exercise. First session was taught by an experienced physical therapist and monitored in the subsequent four sessions. The program consisted of three exercises focusing on the SSP, ISP, and scapular stabilizer musculature. The TrP-DN group also received TrP-DN to active TrPs in shoulder muscles that had pain or showed shoulder symptoms during the second and fourth treatment sessions. Participants received TrP-DN with disposable stainless steel needles of 0.32mm × 40mm (Novasa, Madrid, Spain) that were inserted into the skin over the TrP. Fast-in and fast-out technique as described by Hong was applied. | 20–25 min (Exercise program) 5–10 min (TrP-DN intervention) | Exercise program, on an individual basis, twice daily for 5 weeks TrP-DN: four sessions (during the second and fourth treatment sessions) once per week. | 5 W | The current trial suggests that TrP-DN can be clinically used for improving the effects of exercise programs in people with subacromial pain syndrome. |
| Arias-Buría J.L., et al., 2018 [29] * | 50/2 | The protocol included the same exercise program. Each exercise was performed in three sets of 12 repetitions; each repetition consisted of a concentric phase after the eccentric phase of the exercise. The first session was taught by a physical therapist, monitored in the subsequent four sessions. The program consisted of three exercises focusing on the SSP, ISP, and scapular stabilizer musculature. TrP-DN group also received TrP-DN to active TrPs in shoulder muscles that had pain or showed shoulder symptoms during the second and fourth treatment sessions. Participants received TrP-DN with disposable stainless dteel needles of 0.32 mm x 40 mm (Novasa, Madrid, Spain) that were inserted into the skin over the TrP. Fast-in and fast-out technique as described by Hong was applied | 20–25 min (Exercise program) 5–10 min (TrP-DN intervention) | Exercise program, on an individual basis, twice daily for 5 weeks TrP-DN: four sessions, (during the second and fourth treatment sessions) once per week. | 5 W | NA |
| Imani M., Abbasi L., Taghizadeh S., Amiri M., 2021 [30] | 66/3 | The protocol included the same routine physiotherapy: 20 min interferential current (50–120 Hz; NOVIN Co, Multisti, 735X) with a hot pack and some exercises. DN was performed only for active TrPs and then released for 10 min to induce a local reaction. Hong’s DN technique + routine physiotherapy. Hong’s method, the needles were moved pyramidally and removed immediately after the local response appeared. | ±5min | 10 sessions routine physiotherapy 3 sessions of DN/Hong DN (performed in the third, fifth and seventh sessions) | 4 W | NA |
| Kheradmandi A., Kamali F., Ebrahimian M., Abbasi L. 2021 [31] | 40 | The protocol included scapular mobilization (three sets of 10 repetitions with 30 s rest between each set) DN: the patients received treatment on the Subscapularis, Pectoralis minor, Serratus anterior, UT and LT. | NA | Three sessions with intervals of 3 D. | NA | DN plus manual therapy is more effective at improving pain function than manual therapy alone. Improving dyskinesia helps overhead athletes have a functional and painless workout. |
| Halle R, Crowell M, Goss D., 2020 [32] | 39/2 | The protocol included standard rehabilitation, protocols: manual PROM into flexion, abduction, external rotation, and internal rotation. DN treatment: needling techniques utilized included pistoning (inserting and withdrawing needle rapidly from each TPs), needle left in situ for 10 to 15 min, needling with electrical stimulation, and a combination of these techniques. | Equal amounts of time both groups | Weekly DN (four treatments) | 4 W | NA |
| Ekici G, Özcan Ş, Öztürk BY, Öztürk B, Ekici B., 2021 [33] | 40/2 | A protocol including TrP deep friction massage was applied transversely and deeply, following the fibre direction of the affected connective tissue, until analgesia occurred. TrP-DN therapy: the needle type and depth of placement were changed according to the estimated muscle thickness (0.25–25 mm, 0.25–30 mm, 0.25–40 mm). A fast input/output technique was preferred for the TrPs, through the taut band of the muscle. The process was continued until no more local twitch response was achieved. Movements were in the vertical direction between 3 and 5 mm. | NA | Six sessions, twice a week over a 3-week period. DN group received six treatments over a 4-week period, with a treatment every 5 D. | 4 W | Both groups received six treatment sessions and a programme of post-treatment exercises. |
| Jalilipanah P., Okhovatian F., Serri R.A., Bagban A.A., Zamani S., 2021 [26] | 39/3 | MET: PIR, treatment administered according to L. Chaitow’s guidelines [38]. DN: needles were inserted directly into the muscle, then partly removed and then re-inserted; this process was repeated until no further local twitch responses were elicited. The treatment was done with a 25 mm, 0.25 G acupuncture needle. | NA | Three sessions in a one-week period, with at least a 2 D break between sessions. | 1 W | DN was more effective than MET and their combination in enhancing the abduction and flexion ROMs. In healthy subjects, we have to note that combinations of the DN and MET methods can be equally effective with latent TrPs. The most effective method is the one that can quickly reduce pain and enhance the ROM. |
| Kamali F., et al.,2019 [25] | 40/2 | A protocol with DN was applied directly onto TrPs in the UT. The needle should be inserted perpendicular to the skin, toward the therapist’s finger. Indirect DN needling in the ISP; direct needling into TrPs towards the scapula while the patient lay in the prone position. In both techniques a 0.2 × 50 mm acupuncture needle with a guiding tube was used. | NA | Three sessions (2 D intervals between sessions) | 2 W | Patients were not allowed to receive any drug or other type of treatment during the trial. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Blanco-Díaz, M.; Ruiz-Redondo, R.; Escobio-Prieto, I.; De la Fuente-Costa, M.; Albornoz-Cabello, M.; Casaña, J. A Systematic Review of the Effectiveness of Dry Needling in Subacromial Syndrome. Biology 2022, 11, 243. https://doi.org/10.3390/biology11020243
Blanco-Díaz M, Ruiz-Redondo R, Escobio-Prieto I, De la Fuente-Costa M, Albornoz-Cabello M, Casaña J. A Systematic Review of the Effectiveness of Dry Needling in Subacromial Syndrome. Biology. 2022; 11(2):243. https://doi.org/10.3390/biology11020243
Chicago/Turabian StyleBlanco-Díaz, María, Rubén Ruiz-Redondo, Isabel Escobio-Prieto, Marta De la Fuente-Costa, Manuel Albornoz-Cabello, and José Casaña. 2022. "A Systematic Review of the Effectiveness of Dry Needling in Subacromial Syndrome" Biology 11, no. 2: 243. https://doi.org/10.3390/biology11020243
APA StyleBlanco-Díaz, M., Ruiz-Redondo, R., Escobio-Prieto, I., De la Fuente-Costa, M., Albornoz-Cabello, M., & Casaña, J. (2022). A Systematic Review of the Effectiveness of Dry Needling in Subacromial Syndrome. Biology, 11(2), 243. https://doi.org/10.3390/biology11020243







