Ethnobotany of the Himalayas: Safeguarding Medical Practices and Traditional Uses of Kashmir Regions
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
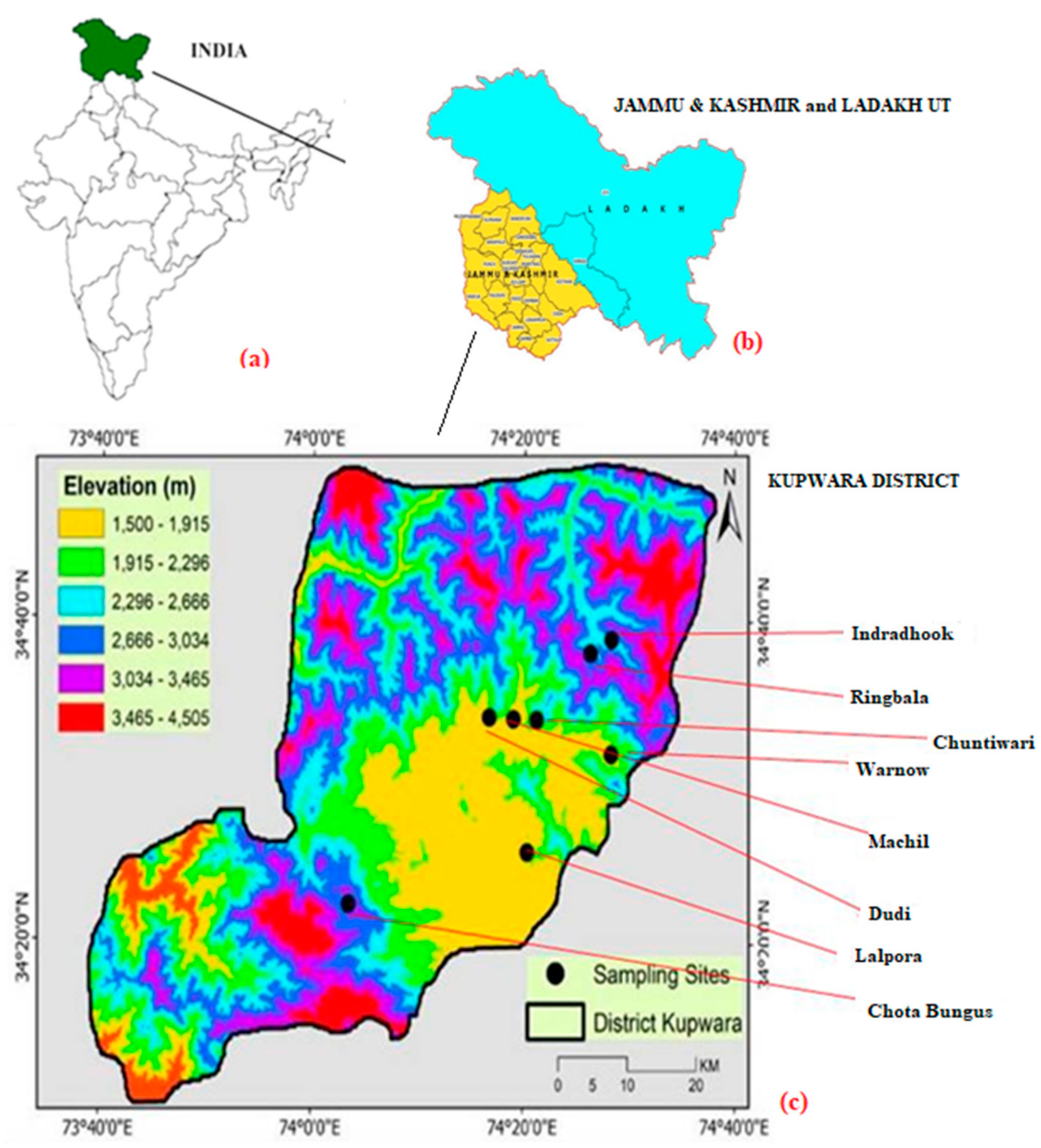
2.1. Research Site
2.2. Medicinal Plant Survey and Data Collection
2.2.1. Field Expeditions and Recording
2.2.2. Sampling Methods and Informants
2.2.3. Disease Categorization
2.3. Data Analysis
2.3.1. Species Use Value (UV) and Use Frequency (Fq)
2.3.2. Family Use Value (FUV)
2.3.3. Informant Consensus Factor (ICF)
2.3.4. Relative Importance (RI)
2.4. Literature Review
2.4.1. Species Identification and Voucher Number
2.4.2. Use of Website Databases
3. Results
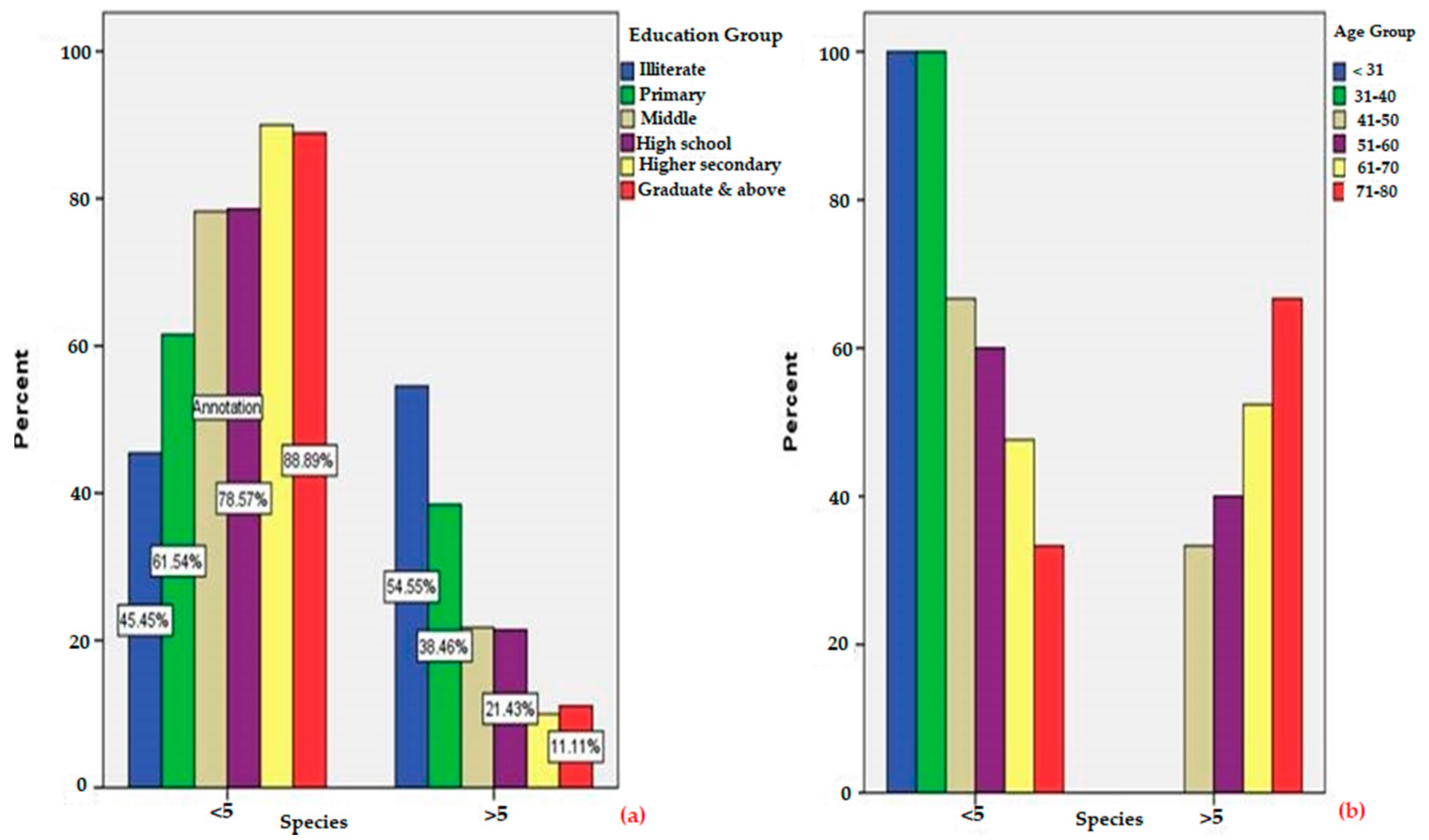
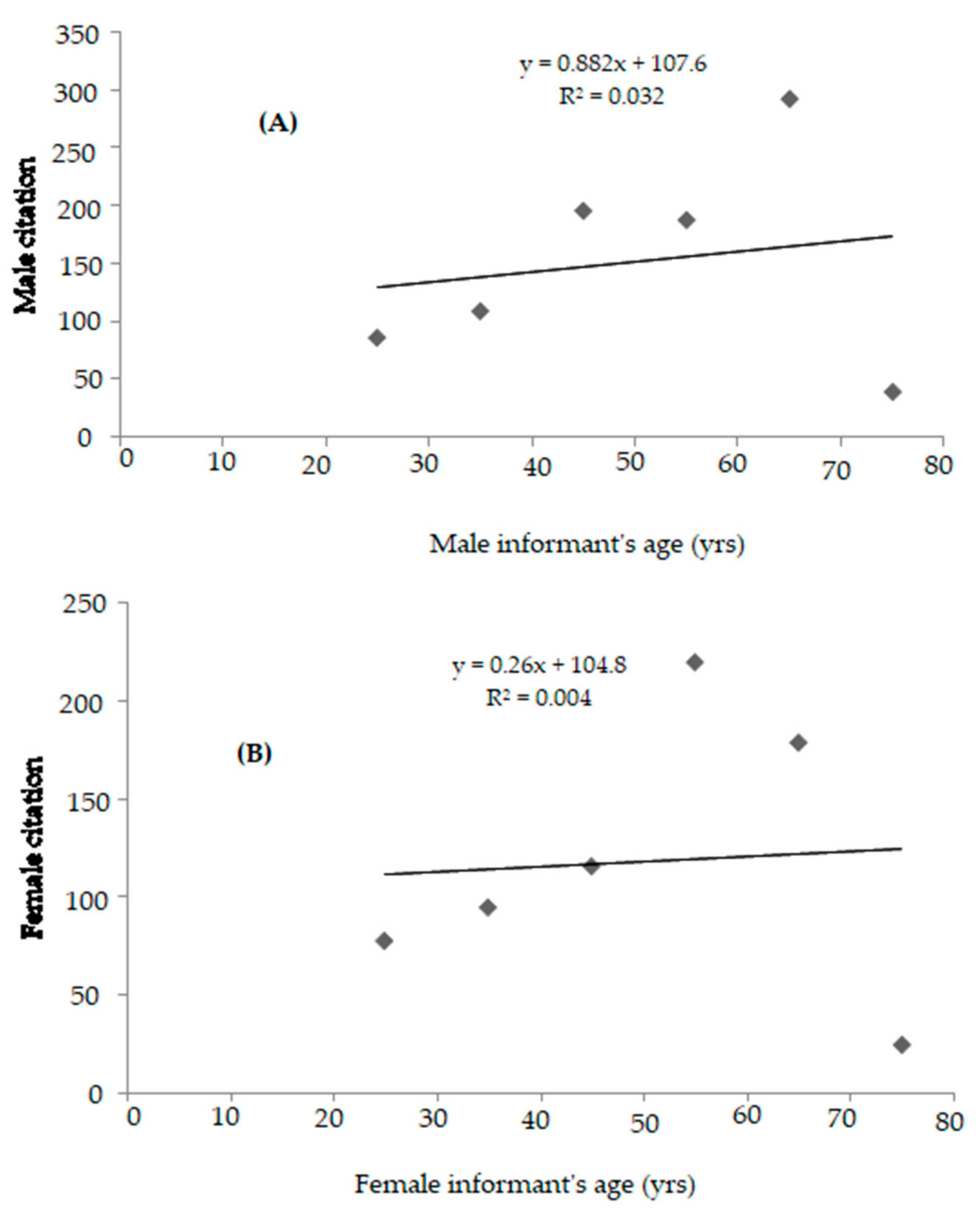
3.1. Characteristics of Participants and Correlation
3.2. Floristic Composition of Medicinal Plants
3.3. Family Use Value (FUV)
3.4. Plant Taxa, Use-Reports (URs) and Associated Plant Knowledge
3.5. Plant Parts Used as Medicine
3.6. Methods of Preparation and Administration
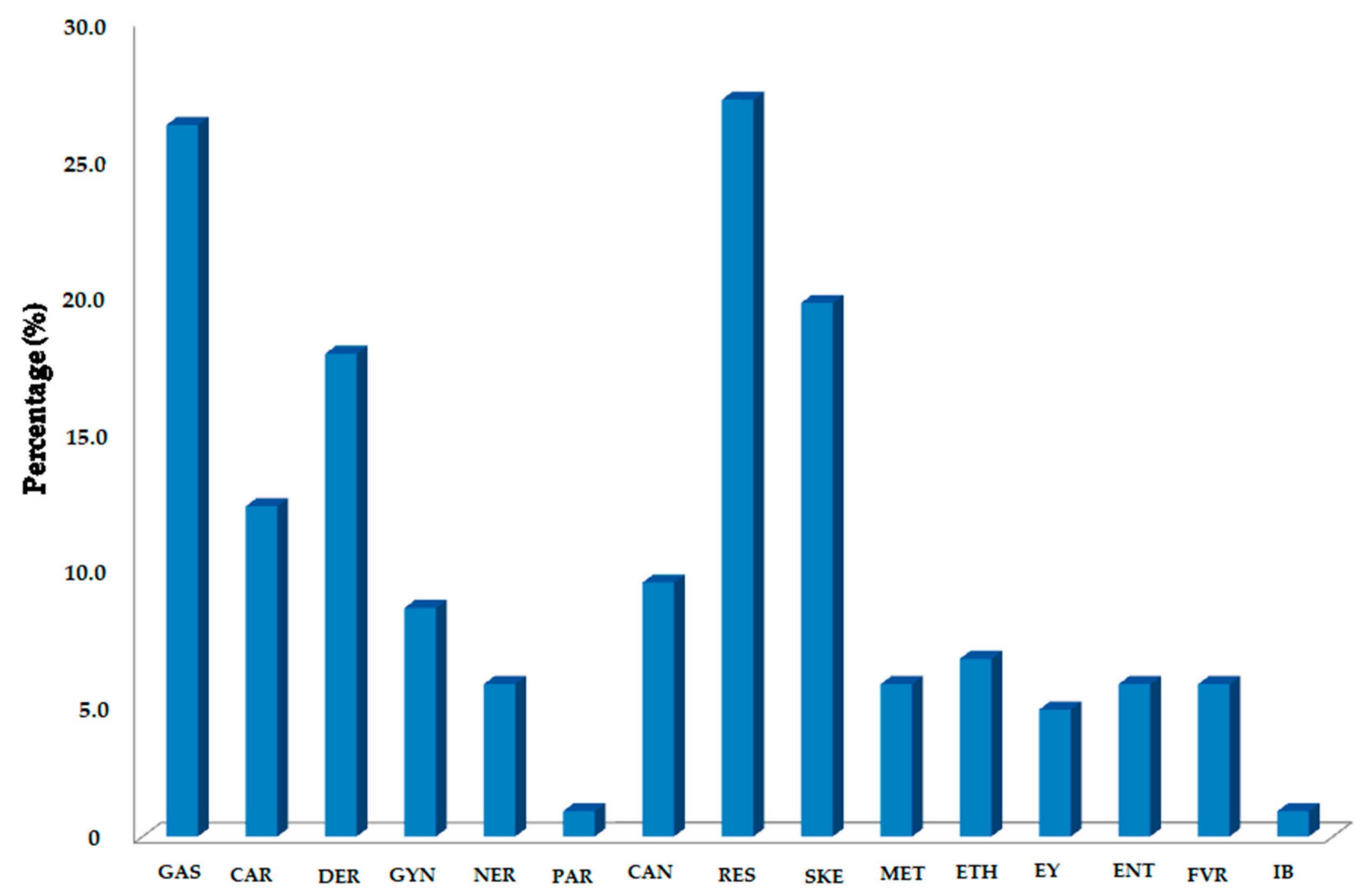
3.7. Informant Consensus Factor (ICF) and Disease Category
3.8. Exotic Medicinal Plants
3.9. Rare Plant Species and Loss of Traditional Knowledge
4. Novelty
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Singh, B.; Singh, B.; Kishor, A.; Singh, S.; Bhat, M.N.; Surmal, O.; Musarella, C.M. Exploring plant-based ethnomedicine and quantitative ethnopharmacology: Medicinal plants utilized by the population of Jasrota Hill in Western Himalaya. Sustainability 2020, 12, 7526. [Google Scholar] [CrossRef]
- Grover, J.K.; Yadav, S.; Vats, V. Medicinal plants of India with anti-diabetic potential. J. Ethnopharmacol. 2002, 81, 81–100. [Google Scholar] [CrossRef]
- WHO World Health Organization. Traditional Medicine Strategy Report, Document WHO/EDM/TRH/2002.1; Hong Kong SAR Press: Hong Kong, China, 2002. [Google Scholar]
- Shewamene, Z.; Dune, T.; Smith, C.A. Use of traditional and complementary medicine for maternal health and wellbeing by African migrant women in Australia: A mixed method study. BMC Complementary Med. Ther. 2020, 20, 60. [Google Scholar] [CrossRef] [PubMed]
- Thakur, V.V.; Tiwari, S.; Tripathi, N.; Tiwari, G. Molecular identification of medicinal plants with amplicon length polymorphism using universal DNA barcodes of the atpF–atpH, trnL and trnH–psbA regions. 3 Biotech 2019, 9. [Google Scholar] [CrossRef]
- Bruchac, M.M. Indigenous Knowledge and Traditional Knowledge. Encycl. Glob. Archaeol. 2020, 5686–5696. [Google Scholar] [CrossRef]
- Byg, A.; Balslev, H. Diversity and use of palms in Zahamena, eastern Madagascar. Biodivers. Conserv. 2001, 10, 951–970. [Google Scholar] [CrossRef]
- Petrovska, B.B. Historical review of medicinal plants’ usage. Pharmacogn. Rev. 2012, 6, 1–5. [Google Scholar] [CrossRef]
- Chen, S.L.; Yu, H.; Luo, H.M.; Wu, Q.; Li, C.F.; Steinmetz, A. Conservation and sustainable use of medicinal plants: Problems, progress, and prospects. Chin. Med. 2016, 11. [Google Scholar] [CrossRef] [PubMed]
- Romero-Daza, N. Traditional medicine in Africa. Ann. Am. Acad. Political Soc. Sci. 2002, 583, 173–176. [Google Scholar] [CrossRef]
- Sen, S.; Chakraborty, R.; De, B. Challenges and opportunities in the advancement of herbal medicine: India’s position and role in a global context. J. Herb. Med. 2011, 1, 67–75. [Google Scholar] [CrossRef]
- Baydoun, S.A.; Kanji, D.; Rafat, K.; Ela, M.A.; Chalak, L.; Apostolides, N.A. Ethnobotanical and economic importance of wild plant species of Jabal Moussa Bioreserve, Lebanon. J. Ecosyst. Ecography 2017, 7, 10–4172. [Google Scholar] [CrossRef]
- Singh, A.; Nautiyal, M.C.; Kunwar, R.M.; Bussmann, R.W. Ethnomedicinal plants used by local inhabitants of Jakholi block, Rudraprayag district, western Himalaya, India. J. Ethnobiol. Ethnomed. 2017, 13, 49. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, P.K.; Kumar, V.; Mal, M.; Houghton, P.J. Acorus calamus: Scientific validation of ayurvedic tradition from natural resources. Pharm. Biol. 2007, 45, 651–666. [Google Scholar] [CrossRef]
- Nyero, A.; Achaye, I.; Odongo, W.; Anywar, G.; Malinga, G.M. Wild and semi-wild edible plants used by the communities of acholi sub-region, northern uganda. Ethnobot. Res. Appl. 2021, 21. [Google Scholar] [CrossRef]
- Verma, R.K. An ethnobotanical study of plants used for the treatment of livestock diseases in Tikamgarh District of Bundelkhand, Central India. Asian Pac. J. Trop. Biomed. 2014, 4, S460–S467. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.; Borthakur, S.K.; Phukan, S.J. A survey of ethnomedicinal plants utilized by the indigenous people of Garo hills with special reference to the nokrek biosphere reserve (Meghalaya), India. J. Herbs Spices Med. Plants 2014, 20, 1–30. [Google Scholar] [CrossRef]
- Célida de Oliveira, T.A. Medicinal plants: Uses and beliefs of elderly carriers of arterial hypertension. Rev. Eletrônica Enferm. 2007, 9, 93–105. [Google Scholar]
- Abebe, B.A.; Chane Teferi, S. Ethnobotanical study of medicinal plants used to treat human and livestock ailments in hulet eju enese woreda, east gojjam zone of amhara region, Ethiopia. Evid. Based Complementary Altern. Med. 2021, 2021. [Google Scholar] [CrossRef]
- Khan, S.M.; Page, S.E.; Ahmad, H.; Harper, D.M. Sustainable utilization and conservation of plant biodiversity in montane ecosystems: The western Himalayas as a case study. Ann. Bot. 2013, 112, 479–501. [Google Scholar] [CrossRef]
- Jardine, T.D. Indigenous knowledge as a remedy for shifting baseline syndrome. Front. Ecol. Environ. 2019, 17, 13–14. [Google Scholar] [CrossRef]
- Cohen, J.I.; Alcorn, J.B.; Potter, C.S. Utilization and conservation of genetic resources: International projects for sustainable agriculture. Econ. Bot. 1991, 45, 190–199. [Google Scholar] [CrossRef]
- Singh, B.; Shanpru, R. Ethno-botanical Plants in Sacred Forests of Meghalaya. Ann. For. 2010, 18, 270–282. [Google Scholar]
- Grumbine, R.E.; Xu, J. Mountain futures: Pursuing innovative adaptations in coupled social–ecological systems. Front. Ecol. Environ. 2021, 19, 342–348. [Google Scholar] [CrossRef]
- Natarajan, B.; Paulsen, B.S.; Korneliussen, V. An Ethnopharmacological Study from Kulu District, Himachal Pradesh, India: Traditional Knowledge Compared with Modern Biological Science. Pharm. Biol. 2000, 38, 129–138. [Google Scholar] [CrossRef]
- Mahapatra AK, P.P. Ethno-pharmacological knowledge of Juang and Munda tribes of eastern India. J. Sustain. Dev. World Ecol. 2002, 9, 151–158. [Google Scholar]
- Harsha, V.H.; Hebbar, S.S.; Shripathi, V.; Hegde, G.R. Ethnomedicobotany of Uttara Kannada district in Karnataka, India—Plants in treatment of skin diseases. J. Ethnopharmacol. 2003, 84, 37–40. [Google Scholar] [CrossRef]
- Singh, B.; Singh, S.; Kishor, A.; Singh, B. Traditional usage of medicinal plants in humans and animals health care and their chemical constituents from hills and valleys of jammu province, western himalaya. Indian J. Nat. Prod. Resour. 2021, 12, 84–100. [Google Scholar]
- Musarella, C.M.; Paglianiti, I.; Cano-Ortiz, A.; Spampinato, G. Indagine Etnobotanica Nel Territorio Del Poro E Delle Preserre Calabresi (Vibo Valentia, S-Italia). Atti Della Soc. Toscana Sci. Nat. Mem. Ser. B 2019, 126, 13–28. [Google Scholar] [CrossRef]
- Singh, B.; Singh, S.; Singh, B.; Kitchlu, S.; Babu, V. Assessing Ethnic Traditional Knowledge, Biology and Chemistry of Lepidium didymum L., Lesser-Known Wild Plants of Western Himalaya. Proc. Natl. Acad. Sci. India Sect. B Biol. Sci. 2019, 89, 1087–1094. [Google Scholar] [CrossRef]
- Kala, C.P. Current Status of Medicinal Plants Used by Traditional Vaidyas in Uttaranchal State of India. Ethnobot. Res. Appl. 2005, 3, 267. [Google Scholar] [CrossRef]
- Singh, P.; Bajpai, V.; Khandelwal, N.; Varshney, S.; Gaikwad, A.N.; Srivastava, M.; Singh, B.; Kumar, B. Determination of bioactive compounds of Artemisia Spp. plant extracts by LC–MS/MS technique and their in-vitro anti-adipogenic activity screening. J. Pharm. Biomed. Anal. 2021, 193, 113707. [Google Scholar] [CrossRef]
- Katare, A.K.; Singh, B.; Shukla, P.; Gupta, S.; Singh, B.; Yalamanchili, K.; Kulshrestha, N.; Bhanwaria, R.; Sharma, A.K.; Sharma, S.; et al. Rapid determination and optimisation of berberine from Himalayan Berberis lycium by soxhlet apparatus using CCD-RSM and its quality control as a potential candidate for COVID-19. Nat. Prod. Res. 2020. [Google Scholar] [CrossRef] [PubMed]
- Goel, B.; Sharma, A.; Tripathi, N.; Bhardwaj, N.; Sahu, B.; Kaur, G.; Singh, B.; Jain, S.K. In-vitro antitumor activity of compounds from Glycyrrhiza glabra against C6 glioma cancer cells: Identification of natural lead for further evaluation. Nat. Prod. Res. 2020. [Google Scholar] [CrossRef]
- Tripathi, S. Perspectives of Forest Biodiversity Conservation in Northeast India. J. Biodivers. Bioprospecting Dev. 2016, 3, 157. [Google Scholar] [CrossRef]
- Gowthami, R.; Sharma, N.; Pandey, R.; Agrawal, A. Status and consolidated list of threatened medicinal plants of India. Genet. Resour. Crop Evol. 2021, 68, 2235–2263. [Google Scholar] [CrossRef]
- Ahmadullah, M.; Nayar, M.P. Red Data Book of Indian Plants (Peninsular India); Botanical Survey of India: Calcutta, India, 1999.
- Robson, T. An Introduction to Complementary Medicine; Reprint Routledge, Tayor & Fracis Group: London, UK, 2003. [Google Scholar]
- Mao, A.A.; Hynniewta, T.M.; Sanjappa, M. Plant wealth of Northeast India with reference to ethnobotany. Indian J. Tradit. Knowl. 2009, 8, 96–103. [Google Scholar]
- Singh, B.; Sinha, B.K.; Phukan, S.J.; Borthakur, S.K.; Singh, V.N. Wild edible plants used by Garo tribes of Nokrek Biosphere Reserve in Meghalaya, India. Indian J. Tradit. Knowl. 2012, 11, 166–171. [Google Scholar]
- Chander, D.; Nisha, B.; Shevita, P. Oral traditional knowledge on medicinal plants in jeopardy among Gaddi shepherds in hills of northwestern Himalaya, J&K, India. J. Ethnopharmacol. 2015, 168, 337–348. [Google Scholar] [CrossRef]
- Dar, G.H.; Khuroo, A.A. Biodiversity of the Himalaya: Jammu and Kashmir State; Springer: Singapore, 2020. [Google Scholar]
- Behera, M.D.; Kushwaha, S.P.S. High plant endemism in an Indian hotspot--eastern Himalaya. Biodivers. Conserv. 2007, 16, 669–682. [Google Scholar] [CrossRef]
- Singh, B.; Sultan, P.; Hassan, Q.P.; Gairola, S.; Bedi, Y.S. Ethnobotany, Traditional Knowledge, and Diversity of Wild Edible Plants and Fungi: A Case Study in the Bandipora District of Kashmir Himalaya, India. J. Herbs Spices Med. Plants 2016, 22, 247–278. [Google Scholar] [CrossRef]
- Haq, S.M.; Singh, B. Ethnobotany as a Science of Preserving Traditional Knowledge: Traditional Uses of Wild Medicinal Plants from District Reasi, J&K (Northwestern Himalaya), India. Bot. Leads Drug Discov. 2020, 277–293. [Google Scholar] [CrossRef]
- Azad, S.A.; Bhat, A.R. Ethnomedicinal Plants Recorded from Rajouri-Poonch Districts of J&K State. Indian J. Life Sci. 2013, 2, 7879. [Google Scholar]
- Kloos, S. The pharmaceutical assemblage: Rethinking Sowa Rigpa and the herbal pharmaceutical industry in Asia. Curr. Anthropol. 2017, 58, 693–717. [Google Scholar] [CrossRef]
- Shukla, S.; Sinclair, A.J. Becoming a traditional medicinal plant healer: Divergent views of practicing and young healers on traditional medicinal plant knowledge skills in India. Ethnobot. Res. Appl. 2009, 7, 39–52. [Google Scholar] [CrossRef]
- Raghuvanshi, D.; Dhalaria, R.; Sharma, A.; Kumar, D.; Kumar, H.; Valis, M.; Kuča, K.; Verma, R.; Puri, S. Ethnomedicinal plants traditionally used for the treatment of jaundice (Icterus) in himachal pradesh in western Himalaya—A review. Plants 2021, 10, 232. [Google Scholar] [CrossRef] [PubMed]
- Ganie, M.A.; Charoo, B.A.; Sahar, T.; Bhat, M.H.; Ali, S.A.; Niyaz, M.; Sidana, S.; Yaseen, A. Thyroid Function, Urinary Iodine, and Thyroid Antibody Status among the Tribal Population of Kashmir Valley: Data From Endemic Zone of a Sub-Himalayan Region. Front. Public Health 2020, 8, 632. [Google Scholar] [CrossRef] [PubMed]
- Lone1, M.A.; Lone, M.A. Traditional Plant Remedies from Bungus Valley of District Kupwara Kashmir. Int. J. Innov. Sci. Res. Technol. 2018, 3, 120–125. [Google Scholar]
- Bhat, M.N.; Singh, B.; Chowdhary, M.A.; Singh, S.; Surmal, O.; Bhanwaria, R.; Singh, B. Medicinal Plants of District Kupwara Used in the Treatment of Human Diseases and Their Associated Biological Functions. In Botanical Leads for Drug Discovery; Singh, B., Ed.; New India Publishing Agency: New Delhi, India, 2020; pp. 325–347. [Google Scholar] [CrossRef]
- Chandra Kanta, I.P.S. and M.A.S. Ethnobotanical studies on Medicinal Plants of Langate area, Kupwara, Jammu and Kashmir, India. J. Med. Plants Stud. 2018, 6, 94–97. [Google Scholar]
- Mir, M.Y. Indigenous knowledge of using medicinal plants in treating skin disease by tribal’s of Kupwara, J&K, India. Indian J. Herb. Med. 2014, 1, 62–68. [Google Scholar]
- Maruca, G.; Spampinato, G.; Turiano, D.; Laghetti, G.; Musarella, C.M. Ethnobotanical notes about medicinal and useful plants of the Reventino Massif tradition (Calabria region, Southern Italy). Genet. Resour. Crop Evol. 2019, 66, 1027–1040. [Google Scholar] [CrossRef]
- Malik, A.H.; Khuroo, A.A.; Dar, G.H.; Khan, Z.S. Ethnomedicinal uses of some plants in the Kashmir Himalaya. Indian J. Tradit. Knowl. 2011, 10, 362–366. [Google Scholar]
- Bhatia, H.; Pal Sharma, Y.; Manhas, R.K.; Kumar, K. Traditional phytoremedies for the treatment of menstrual disorders in district Udhampur, J&K, India. J. Ethnopharmacol. 2015, 160, 202–210. [Google Scholar] [CrossRef]
- Panel, P.K.; Sharma, V. Singh Ethnobotanical studies in NorthWest AND Trans-Himalaya. V. Ethno-veterinary medicinal plants used in Jammu and Kashmir, India. J. Ethnopharmacol. 1989, 27, 63–70. [Google Scholar]
- Khan, M.; Kumar, S.; Hamal, I.A. Medicinal Plants of Sewa River Catchment Area in the Northwest Himalaya and its Implication for Conservation. Ethnobot. Leafl. 2009, 13, 1113–1152. [Google Scholar]
- Bhattacharyya, A. Ethnobotanical observations in the Ladakh Region of Northern Jammu and Kashmir state, India. Econ. Bot. 1991, 45, 305–308. [Google Scholar] [CrossRef]
- Sciences, A.; Kashmir, T. Wealth of Non Timber Forest Products and Their Trade in Jammu and Kashmir. Indian For. 2017, 143, 827–833. [Google Scholar]
- Showkat, S.; Akhtar, R. An Ethnobotanical Study of Wild Edible Plants of District Baramulla Jammu and Kashmir. Inter. J. Res. 2018, 5, 166–169. [Google Scholar]
- Haq, S.M.; Singh, B.; Bashir, F.; Farooq, A.J.; Singh, B.; Calixto, E.S. Exploring and understanding the floristic richness, lifeform, leaf-size spectra and phenology of plants in protected forests: A case study of Dachigam National Park in Himalaya, Asia. Acta Ecol. Sin. 2021. [Google Scholar] [CrossRef]
- Gupta, O.P.; Srivastava, T.N.; Gupta, S.C.; Badola, D.P. An ethnobotany and phytochemical screening of higher altitude plants of Ladakh. Bull. Med. Ethnobot Res 1982, 1, 301–317. [Google Scholar]
- Ballabh, B.; Chaurasia, O.P. Medicinal plants of cold desert Ladakh used in the treatment of stomach disorders. Indian J. Tradit. Knowl. 2009, 8, 185–190. [Google Scholar]
- Sanwal, C.S. Raheel Anwar Lone An assessment of the Asiatic black bear-human conflicts in Kupwara district, Jammu & Kashmir, India. Indian For. 2012, 138, 881–886. [Google Scholar]
- Forest Survey of India. India State of Forest Report 2011; Forest Survey of India: Dehradun, India, 2011; pp. 236–240. [Google Scholar]
- Baqai, H. Water-related Issues in South Asia: Conflicts in the Making. Pak. Horiz. 2005, 58, 77–88. [Google Scholar]
- IUCN Red List of Threatened Species. 2012; [cited 21 Jan 2021]. pp. 49-6872-49–6872. [CrossRef]
- Heinrich, M. Ethnobotany and its role in drug development. Phytother. Res. 2000, 14, 479–488. [Google Scholar] [CrossRef]
- Batool, N.; Shah, S.A.; Dar, S.N.; Skinder, S. Rainfall variability and dynamics of cropping pattern in Kashmir Himalayas: A case study of climate change and agriculture. SN Appl. Sci. 2019, 1, 606. [Google Scholar] [CrossRef]
- Wani, M.B.; Ali, S.A.; Ali, U. Flood assessment of Lolab valley from watershed characterization using remote sensing and GIS techniques. In Hydrologic Modeling; Singh, V., Yadav, S., Yadava, R., Eds.; Springer: Singapore, 2018; Volume 81, pp. 367–390. [Google Scholar] [CrossRef]
- Bhat, F.; Mahajan, D.M.; Bhat, A. Assessment of anthropogenic activities and exotic flora of Lolab valley, Kashmir. Int. J. Bioassays 2015, 4, 4483–4491. [Google Scholar]
- Heinrich, M.; Barnes, J.; Gibbons, S.; Williamson, E.M. Fundamental Pharmacognosy Phytotherapy; Churchill Livingstone: London, UK, 2004; pp. 24–25. [Google Scholar]
- Jain, S.K.; Rao, R.R. A Handbook of Field and Herbarium Methods; Today and Tomorrow’s Printer: New Delhi, India, 1977; p. 150. [Google Scholar]
- Weckerle, C.S.; de Boer, H.J.; Puri, R.K.; van Andel, T.; Bussmann, R.W.; Leonti, M. Recommended standards for conducting and reporting ethnopharmacological field studies. J. Ethnopharmacol. 2018, 210, 125–132. [Google Scholar] [CrossRef]
- Dosne, A.G.; Bergstrand, M.; Karlsson, M.O. An automated sampling importance resampling procedure for estimating parameter uncertainty. J. Pharmacokinet. Pharmacodyn. 2017, 44, 509–520. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, M.O.; Jonsson, E.N.; Wiltse, C.G.; Wade, J.R. Assumption testing in population pharmacokinetic models: Illustrated with an analysis of moxonidine data from congestive heart failure patients. J. Pharmacokinet. Biopharm. 1998, 26, 207–246. [Google Scholar] [CrossRef]
- Espinosa, M.M.; Bieski, I.G.C.; de Oliveira Martins, D.T. Probability sampling design in ethnobotanical surveys of medicinal plants. Braz. J. Pharmacogn. 2012, 22, 1362–1367. [Google Scholar] [CrossRef]
- Holmgren, P.K.; Holmgren, N.H. Index Herbariorum: A Global Directory of Public Herbaria and Associated Staff. 1998. Available online: https://academic.microsoft.com/paper/2753127192/citedby/search?q=Index%20Herbariorum%3A%20A%20global%20directory%20of%20public%20herbaria%20and%20associated%20staff&qe=RId%253D2753127192&f=&orderBy=0 (accessed on 30 August 2021).
- Staub, P.O.; Geck, M.S.; Weckerle, C.S.; Casu, L.; Leonti, M. Classifying diseases and remedies in ethnomedicine and ethnopharmacology. J. Ethnopharmacol. 2015, 174, 514–519. [Google Scholar] [CrossRef] [PubMed]
- Phillips, O.; Gentry, A.H.; Reynel, C.; Wilkin, P.; Galvez-Durand, B.C. Quantitative Ethnobotany and Amazonian Conservation. Conserv. Biol. 1994, 8, 225–248. [Google Scholar] [CrossRef]
- Friedman, J.; Yaniv, Z.; Dafni, A.; Palewitch, D. A preliminary classification of the healing potential of medicinal plants, based on a rational analysis of an ethnopharmacological field survey among Bedouins in the Negev Desert, Israel. J. Ethnopharmacol. 1986, 16, 275–287. [Google Scholar] [CrossRef]
- Nadaf, M.; Joharchi, M.; Amiri, M.S. Ethnomedicinal uses of plants for the treatment of nervous disorders at the herbal markets of Bojnord, North Khorasan Province, Iran. Avicenna J. Phytomedicine 2019, 9, 153–163. [Google Scholar] [CrossRef]
- Heinrich, M.; Ankli, A.; Frei, B.; Weimann, C.; Sticher, O. Medicinal plants in Mexico: Healers’ consensus and cultural importance. Soc. Sci. Med. 1998, 47, 1859–1871. [Google Scholar] [CrossRef]
- Gazzaneo, L.R.S.; Paiva de Lucena, R.F.; de Albuquerque, U.P. Knowledge and use of medicinal plants by local specialists in an region of Atlantic Forest in the state of Pernambuco (Northeastern Brazil). J. Ethnobiol. Ethnomed. 2005, 1, 9. [Google Scholar] [CrossRef]
- Bennett, B.C.; Prance, G.T. Introduced plants in the indigenous pharmacopoeia of northern South America. Econ. Bot. 2000, 54, 90–102. [Google Scholar] [CrossRef]
- Dhar, U.; Kachroo, P. Alpine Flora of Kashmir Himalaya. Brittonia 1983, 35, 379. [Google Scholar] [CrossRef]
- Uniyal, B.; Singh, P.; Singh, D. Flora of Jammu and Kashmir; Botanical Survey of India: Kolkata, India, 2002; p. 365.
- Riyaz, M.; Ignacimuthu, S.; Shah, R.A.; Sivasankaran, K.; Pandikumar, P. Ethnobotany of the Himalayas—Kashmir, India. In Ethnobiology of Mountain Communities in Asia. Ethnobiology; Abbasi, A.M., Bussmann, R.W., Eds.; Springer: Cham, Switzerland, 2021; pp. 27–45. [Google Scholar] [CrossRef]
- Wagay, J.A.; Nayik, G.A.; Wani, S.A.; Mir, R.A.; Ahmad, M.A.; Rahman, Q.I.; Vyas, D. Phenolic profiling and antioxidant capacity of Morchella esculenta L. by chemical and electrochemical methods at multiwall carbon nanotube paste electrode. J. Food Meas. Charact. 2019, 13, 1805–1819. [Google Scholar] [CrossRef]
- Upreti, K.; Jalal, J.S.; Tewari, L.M.; Joshi, G.C.; Pangtey, Y.P.S.; Tewari, G. Ethnomedicinal uses of Pteridophytes of Kumaun Himalaya, Uttarakhand, India. Marsland Press J. Am. Sci. 2009, 5, 167–170. [Google Scholar]
- Carneiro, D.M.; Jardim, T.V.; Araújo, Y.C.L.; Arantes, A.C.; de Sousa, A.C.; Barroso, W.K.S.; Sousa, A.L.L.; da Cunha, L.C.; Cirilo, H.N.C.; Bara, M.T.F. Equisetum arvense: New Evidences Supports Medical use in Daily Clinic. Pharmacogn. Rev. 2021, 13, 50–58. [Google Scholar] [CrossRef]
- Dehdari, S.; Hajimehdipoor, H. Medicinal properties of Adiantum capillus-veneris linn. In traditional medicine and modern phytotherapy: A review article. Iran. J. Public Health 2018, 47, 188–197. [Google Scholar] [PubMed]
- Gupta, S.K.; Sharma, O.M.P.; Raina, N.S.; Sehgal, S. Ethno-botanical study of medicinal plants of Paddar Valley of Jammu and Kashmir, India. Afr. J. Tradit. Complementary Altern. Med. AJTCAM 2013, 10, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Roshan, R.; Ahmed, S.; Hasan, M.M. Arisaema jacquemontii Blume (Araceae): A review of medicinal uses, phytochemistry and pharmacology. J. Pharmacogn. Phytochem. 2017, 6, 429–432. [Google Scholar] [CrossRef]
- Rahman, A.H.M.M.; Anisuzzaman, M.; Haider, S.A.; Ahmed, F.; Islam, A.K.M.R.; Naderuzzaman, A.T.M. Study of Medicinal Plants in the Graveyards of Rajshahi City. Res. J. Agric. Biol. Sci. 2008, 4, 70–74. [Google Scholar]
- Dangwal, L.R.; Chauhan, A.S. Dioscorea deltoidea Wall. ex griseb. A highly threatened Himalayan medicinal plant: An overview. Int. J. Pharma Bio Sci. 2015, 6, B452–B460. [Google Scholar]
- Amin, A.; Wani, S.H.; Mokhdomi, T.A.; Bukhari, S.; Wafai, A.H.; Mir, J.I.; Hassan, Q.P.; Qadri, R.A. Investigating the pharmacological potential of Iris kashmiriana in limiting growth of epithelial tumors. Pharmacogn. J. 2013, 5, 170–175. [Google Scholar] [CrossRef]
- Wang, J.; Seyler, B.C.; Ticktin, T.; Zeng, Y.; Ayu, K. An ethnobotanical survey of wild edible plants used by the Yi people of Liangshan Prefecture, Sichuan Province, China. J. Ethnobiol. Ethnomed. 2020, 16. [Google Scholar] [CrossRef] [PubMed]
- Sadiq, A.; Ahmad, S.; Ali, R.; Ahmad, F.; Ahmad, S.; Zeb, A.; Ayaz, M.; Ullah, F.; Siddique, A.N. Antibacterial and antifungal potentials of the solvents extracts from Eryngium caeruleum, Notholirion thomsonianum and Allium consanguineum. BMC Complementary Altern. Med. 2016, 16, 478. [Google Scholar] [CrossRef]
- Harun, N.; Chaudhry, A.S.; Shaheen, S.; Ullah, K.; Khan, F. Ethnobotanical studies of fodder grass resources for ruminant animals, based on the traditional knowledge of indigenous communities in Central Punjab Pakistan. J. Ethnobiol. Ethnomed. 2017, 13. [Google Scholar] [CrossRef]
- Cabanting, R.M.F.; Perez, L.M. An ethnobotanical study of traditional rice landraces (Oryza sativa L.) used for medical treatment in selected local communities of the Philippines. J. Ethnopharmacol. 2016, 194, 767–773. [Google Scholar] [CrossRef]
- Khayal, A.Y. Elemental, antimicrobial and antioxidant activities of a medicinal plant Sorghum halepense. Pure Appl. Biol. 2019, 8, 795–803. [Google Scholar] [CrossRef]
- Amjad, M.S.; Qaeem, M.F.; Ahmad, I.; Khan, S.U.; Chaudhari, S.K.; Malik, N.Z.; Shaheen, H.; Khan, A.M. Descriptive study of plant resources in the context of the ethnomedicinal relevance of indigenous flora: A case study from Toli Peer National Park, Azad Jammu and Kashmir, Pakistan. PLoS ONE 2017, 12. [Google Scholar] [CrossRef]
- Ibrahim, O.; Adama, H.; Pierre, S.; Moussa, C.; Jeanne, M.; Germaine, N.O. Ethnobotanical studies on food and medicinal uses of four Amaranthaceae in Mossi Plate, Burkina Faso. World J. Environ. Biosci. 2012, 1, 115–118. [Google Scholar]
- Moein, M.R.; Zomorodian, K.; Pakshir, K.; Yavari, F.; Motamedi, M.; Zarshenas, M.M. Trachyspermum ammi (L.) Sprague: Chemical composition of essential oil and antimicrobial activities of respective fractions. J. Evid. Based Complementary Altern. Med. 2015, 20, 50–56. [Google Scholar] [CrossRef]
- Wang, D.; Bădărau, A.S.; Swamy, M.K.; Shaw, S.; Maggi, F.; da Silva, L.E.; López, V.; Yeung, A.W.K.; Mocan, A.; Atanasov, A.G. Arctium species secondary metabolites chemodiversity and bioactivities. Front. Plant Sci. 2019, 10, 834. [Google Scholar] [CrossRef] [PubMed]
- Nigam, M.; Atanassova, M.; Mishra, A.P.; Pezzani, R.; Devkota, H.P.; Plygun, S.; Salehi, B.; Setzer, W.N.; Sharifi-Rad, J. Bioactive compounds and health benefits of Artemisia species. Nat. Prod. Commun. 2019, 14. [Google Scholar] [CrossRef]
- Nwafor, I.C.; Shale, K.; Achilonu, M.C. Chemical Composition and Nutritive Benefits of Chicory (Cichorium intybus) as an Ideal Complementary and/or Alternative Livestock Feed Supplement. Sci. World J. 2017, 2017. [Google Scholar] [CrossRef]
- Negi, V.S.; Pathak, R.; Sekar, K.C.; Rawal, R.S.; Bhatt, I.D.; Nandi, S.K.; Dhyani, P.P. Traditional knowledge and biodiversity conservation: A case study from Byans Valley in Kailash Sacred Landscape, India. J. Environ. Plan. Manag. 2018, 61, 1722–1743. [Google Scholar] [CrossRef]
- Šavikin, K.; Zdunić, G.; Menković, N.; Živković, J.; Ćujić, N.; Tereščenko, M.; Bigović, D. Ethnobotanical study on traditional use of medicinal plants in South-Western Serbia, Zlatibor district. J. Ethnopharmacol. 2013, 146, 803–810. [Google Scholar] [CrossRef]
- Pandey, M.M.; Rastogi, S.; Rawat, A.K.S. Saussurea costus: Botanical, chemical and pharmacological review of an ayurvedic medicinal plant. J. Ethnopharmacol. 2007, 110, 379–390. [Google Scholar] [CrossRef]
- Menković, N.; Šavikin, K.; Tasić, S.; Zdunić, G.; Stešević, D.; Milosavljević, S.; Vincek, D. Ethnobotanical study on traditional uses of wild medicinal plants in Prokletije Mountains (Montenegro). J. Ethnopharmacol. 2011, 133, 97–107. [Google Scholar] [CrossRef]
- Malik, K.; Ahmad, M.; Zafar, M.; Ullah, R.; Mahmood, H.M.; Parveen, B.; Rashid, N.; Sultana, S.; Shah, S.N. Lubna an ethnobotanical study of medicinal plants used to treat skin diseases in northern Pakistan. BMC Complementary Altern. Med. 2019, 19. [Google Scholar] [CrossRef]
- Chaurasia, O.P.; Ballabh, B.; Tayade, A.; Kumar, R.; Kumar, G.P.; Singh, S.B. Podophyllum: An endergered and anticancerous medicinal plant-an overview. Indian J. Tradit. Knowl. 2012, 11, 234–241. [Google Scholar]
- Rana, J.C.; Pradheep, K.; Chaurasia, O.P.; Sood, S.; Sharma, R.M.; Singh, A.; Negi, R. Traditional medicinal plants of cold desert Ladakh-used against kidney and urinary disorders. Genet. Resour. Crop Evol. 2012, 59, 331–339. [Google Scholar] [CrossRef]
- Tariq, A.; Sadia, S.; Pan, K.; Ullah, I.; Mussarat, S.; Sun, F.; Abiodun, O.O.; Batbaatar, A.; Li, Z.; Song, D.; et al. A systematic review on ethnomedicines of anti-cancer plants. Phytother. Res. 2017, 31, 202–264. [Google Scholar] [CrossRef] [PubMed]
- Hadi, F.; Rahman, A.-U.; Ibrar, M.; Dastagir, G.; Arif, M.; Naveed, K.; Adnan, M.; Hadi, F.; Ibrar, M.; Dastagir, G.; et al. Weed Diversity in Wheat and Maize With Special Reference To Their Ethnomedicinal Uses At Rech Valley, Hindokush Range, Chitral, Pakistan. J. Weed Sci. Res. J. Weed Sci. Res 2014, 20, 335–346. [Google Scholar]
- Rana Man, S.; Samant, S.S. Diversity, indigenous uses and conservation status of medicinal plants in manali wildlife sanctuary, North Western Himalaya. Indian J. Tradit. Knowl. 2011, 10, 439–459. [Google Scholar]
- Bullitta, S.; Piluzza, G.; Viegi, L. Plant resources used for traditional ethnoveterinary phytotherapy in Sardinia (Italy). Genet. Resour. Crop Evol. 2007, 54, 1447–1464. [Google Scholar] [CrossRef]
- Barik, S.K.; Tiwari, O.N.; Adhikari, D.; Singh, P.P.; Tiwary, R.; Barua, S. Geographic distribution pattern of threatened plants of India and steps taken for their conservation. Curr. Sci. 2018, 114, 470–503. [Google Scholar] [CrossRef]
- Zou, S.; Kumar, U. Cannabinoid receptors and the endocannabinoid system: Signaling and function in the central nervous system. Int. J. Mol. Sci. 2018, 19, 833. [Google Scholar] [CrossRef]
- Sufyan, M.; Badshah, I.; Ahmad, M.; Zafar, M.; Bahadur, S.; Rashid, N. Identification of Medicinally Used Flora Using Pollen Features Imaged in the Scanning Electron Microscopy in the Lower Margalla Hills Islamabad Pakistan. Microsc. Microanal. 2018, 24, 292–299. [Google Scholar] [CrossRef]
- Singh, J.; Rajashekaran, A.; Negi, A.K.; Pala, N.A. Wild vegetable plants used by tribal people of Kinnaur District, Himachal Pradesh. Inter. J. For. Usufr. Manag. 2014, 15, 47–56. [Google Scholar]
- Uprety, Y.; Asselin, H.; Boon, E.K.; Yadav, S.; Shrestha, K.K. Indigenous use and bio-efficacy of medicinal plants in the Rasuwa District, Central Nepal. J. Ethnobiol. Ethnomedicine 2010, 6. [Google Scholar] [CrossRef] [PubMed]
- Salam, J.S.; Joylani, S.D.; Rebika, N.D.; Priyadarshini, S. Secondary metabolites, antioxidant status and nutritive composition of two non-conventional leafy vegetables-Stellaria media L. and Chenopodium album L. Indian J. Agric. Biochem. 2011, 24, 136–140. [Google Scholar]
- Gairolaa, S.; Sharma, J.; Bedi, Y.S. A cross-cultural analysis of Jammu, Kashmir and Ladakh (India) medicinal plant use. J. Ethnopharmacol. 2014, 155, 925–986. [Google Scholar] [CrossRef]
- Zhuang, W.; Yue, L.; Dang, X.; Chen, F.; Gong, Y.; Lin, X.; Luo, Y. Rosenroot (Rhodiola): Potential applications in aging-related diseases. Aging Dis. 2019, 10, 134–146. [Google Scholar] [CrossRef]
- Krishnamoorthy, K.; Senguttuvan, J. Evaluation of Anti-inflammatory and Antioxidant Properties of Crude Extract and Forskolin from Solena amplexicaulis Leaf. Indian J. Pharm. Sci. 2016, 78, 377–387. [Google Scholar] [CrossRef]
- Ashraf, M.U.; Muhammad, G.; Hussain, M.A.; Bukhari, S.N.A. Cydonia oblonga, a medicinal plant rich in phytonutrients for pharmaceuticals. Front. Pharmacol. 2016, 7, 163. [Google Scholar] [CrossRef]
- Rahman, T.U.; Zeb, M.A.; Liaqat, W.; Sajid, M.; Hussain, S.; Choudhary, M.I. Phytochemistry and pharmacology of genus Indigofera: A review. Rec. Nat. Prod. 2018, 12, 1–13. [Google Scholar] [CrossRef]
- Kolodziejczyk-Czepas, J. Trifolium species—the latest findings on chemical profile, ethnomedicinal use and pharmacological properties. J. Pharm. Pharmacol. 2016, 68, 845–861. [Google Scholar] [CrossRef] [PubMed]
- Bano, D.; Tabassum, H.; Ahmad, A.; Mabood, A.; Ahmad, I.Z. The Medicinal Significance of the Bioactive Compounds of Trigonella Foenum-Graecum: A Review. Int. J. Res. Ayurveda Pharm. 2016, 7, 84–91. [Google Scholar] [CrossRef]
- Mubashir, K.; Ghazanfar, K.; Ganai, B.A.; Akbar, S.; Malik, A.H.; Masood, A. Scientific Validation of Gentiana kurroo Royle for Anti-Inflammatory and Immunomodulatory Potential. ISRN Inflamm. 2014, 2014, 1–5. [Google Scholar] [CrossRef]
- Qureshi, R.A.; Ghufran, M.A.; Gilani, S.A.; Yousaf, Z.; Abbas, G.; Batool, A. Indigenous medicinal plants used by local women in southern Himalayan regions of Pakistan. Pak. J. Bot. 2009, 41, 19–25. [Google Scholar]
- Ali, N.; Ali Shah, S.W.; Shah, I.; Ahmed, G.; Ghias, M.; Khan, I.; Ali, W. Anthelmintic and relaxant activities of Verbascum Thapsus Mullein. BMC Complementary Altern. Med. 2012, 12, 29. [Google Scholar] [CrossRef] [PubMed]
- Delaviz, H.; Mohammadi, J.; Ghalamfarsa, G.; Mohammadi, B.; Farhadi, N. A review study on phytochemistry and pharmacology applications of Juglans regia plant. Pharmacogn. Rev. 2017, 11, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Kelayeh, T.P.S.; Abedinzade, M.; Ghorbani, A. A review on biological effects of Lamium album (white dead nettle) and its components. J. Herb. Med. Pharmacol. 2018, 8, 185–193. [Google Scholar] [CrossRef]
- Shah, P.; Mello, P. A review of medicinal uses and pharmacological effects of Mentha piperita. Indian J. Nat. Prod. Resour. (IJNPR) 2004, 3, 214–221. [Google Scholar]
- Zomorodian, K.; Saharkhiz, M.J.; Shariati, S.; Pakshir, K.; Rahimi, M.J.; Khashei, R. Chemical Composition and Antimicrobial Activities of Essential Oils from Nepeta cataria L. against Common Causes of Food-Borne Infections. ISRN Pharm. 2012, 2012, 1–6. [Google Scholar] [CrossRef]
- Huang, M.; Wang, Y.; Xu, L.; You, M. Anti-tumor Properties of Prunella vulgaris. Curr. Pharmacol. Rep. 2015, 1, 401–419. [Google Scholar] [CrossRef]
- Qadir, M.I.; Parveen, A.; Abbas, K.; Ali, M. Analgesic, anti-inflammatory and anti-pyretic activities of Thymus Linearis. Pak. J. Pharm. Sci. 2016, 29, 591–594. [Google Scholar] [PubMed]
- Ravi, L.; Manasvi, V.; Praveena Lakshmi, B. Antibacterial and antioxidant activity of saponin from Abutilon indicum leaves. Asian J. Pharm. Clin. Res. 2016, 9, 344–347. [Google Scholar] [CrossRef]
- Fahamiya, N.; Shiffa, M.; Mohd, A. A comprehensive review on Althaea Rosea Linn. Indo Am. J. Pharm. Res. 2016, 6, 6–7. [Google Scholar]
- Kamble, S.Y.; Patil, S.R.; Sawant, P.S.; Sawant, S.; Pawar, S.G.; Singh, E.A. Studies on plants used in traditional medicine by Bhilla tribe of Maharashtra. Indian J. Tradit. Knowl. 2010, 9, 591–598. [Google Scholar]
- Hakeem, R. Ethno-Medicinal Study of Kulgam District (Jammu and Kashmir). Int. J. Sci. Res. (IJSR) 2019, 8, 186–190. [Google Scholar]
- Rathore, S.; Walia, S.; Devi, R.; Kumar, R. Review on Trillium govanianum Wall. ex D. Don: A threatened medicinal plant from the Himalaya. J. Herb. Med. 2020, 24, 100395. [Google Scholar] [CrossRef]
- Bouyahya, A.; Bensaid, M.; Bakri, Y.; Dakka, N. Phytochemistry and Ethnopharmacology of Ficus carica. Int. J. Biochem. Res. Rev. 2016, 14, 1–12. [Google Scholar] [CrossRef]
- Rodrigues, E.L.; Marcelino, G.; Silva, G.T.; Figueiredo, P.S.; Garcez, W.S.; Corsino, J.; de Guimarães, R.C.A.; de Freitas, K.C. Nutraceutical and medicinal potential of the Morus species in metabolic dysfunctions. Int. J. Mol. Sci. 2019, 20, 301. [Google Scholar] [CrossRef]
- Sivakumaran, N.; Samarakoon, S.R.; Adhikari, A.; Ediriweera, M.K.; Tennekoon, K.H.; Malavige, N.; Thabrew, I.; Shrestha, R.L.S. Cytotoxic and Apoptotic Effects of Govaniadine Isolated from Corydalis govaniana Wall. Roots on Human Breast Cancer (MCF-7) Cells. BioMed Res. Int. 2018, 2018. [Google Scholar] [CrossRef]
- Masihuddin, M.; Jafri, M.; Siddiqui, A.; Chaudhary, S. Traditional Uses, Phytochemistry and Pharmacological Activities of Papaver Somniferum With Special Reference of Unani Medicine an Updated Review. J. Drug Deliv. Ther. 2018, 8, 110–114. [Google Scholar] [CrossRef]
- Kumar, S.; Singh, B.; Bajpai, V. Andrographis paniculata (Burm.f.) Nees: Traditional uses, phytochemistry, pharmacological properties and quality control/quality assurance. J. Ethnopharmacol. 2021, 275, 114054. [Google Scholar] [CrossRef] [PubMed]
- Kafle, G.; Bhattarai, I.; Siwakoti, M.; Shrestha, A.K. Demand, End-Uses, and Conservation of Alpine Medicinal Plant Neopicrorhiza scrophulariiflora (Pennell) D. Y. Hong in Central Himalaya. Evid. Based Complementary Altern. Med. 2018, 2018. [Google Scholar] [CrossRef]
- Najafian, Y.; Hamedi, S.S.; Kaboli Farshchi, M.; Feyzabadi, Z. Plantago major in Traditional Persian Medicine and modern phytotherapy: A narrative review. Electron. Physician 2018, 10, 6390–6399. [Google Scholar] [CrossRef]
- Kakar, M.; Amin, M.U.; Alghamdi, S.; Sahibzada, M.U.K.; Ahmad, N.; Ullah, N. Antimicrobial, Cytotoxic, and Antioxidant Potential of a Novel Flavone “6,7,4′-Trimethyl Flavone” Isolated from Wulfenia amherstiana. Evid. Based Complementary Altern. Med. 2020, 2020. [Google Scholar] [CrossRef]
- Huq, A.K.M.M.; Jamal, J.A.; Stanslas, J. Ethnobotanical, phytochemical, pharmacological, and toxicological aspects of Persicaria hydropiper (L.) delarbre. Evid. Based Complementary Altern. Med. 2014, 2014. [Google Scholar] [CrossRef] [PubMed]
- Cock, I.E.; Van Vuuren, S.F. The traditional use of southern African medicinal plants in the treatment of viral respiratory diseases: A review of the ethnobotany and scientific evaluations. J. Ethnopharmacol. 2020, 262. [Google Scholar] [CrossRef]
- Pandith, S.A.; Dar, R.A.; Lattoo, S.K.; Shah, M.A.; Reshi, Z.A. Rheum australe, an endangered high-value medicinal herb of North Western Himalayas: A review of its botany, ethnomedical uses, phytochemistry and pharmacology. Phytochem. Rev. 2018, 17, 573–609. [Google Scholar] [CrossRef] [PubMed]
- Bello, O.M.; Fasinu, P.S.; Bello, O.E.; Ogbesejana, A.B.; Adetunji, C.O.; Dada, A.O.; Ibitoye, O.S.; Aloko, S.; Oguntoye, O.S. Wild vegetable Rumex acetosa Linn.: Its ethnobotany, pharmacology and phytochemistry—A review. South Afr. J. Bot. 2019, 125, 149–160. [Google Scholar] [CrossRef]
- Zhou, Y.X.; Xin, H.L.; Rahman, K.; Wang, S.J.; Peng, C.; Zhang, H. Portulaca oleracea L.: A review of phytochemistry and pharmacological effects. BioMed Res. Int. 2015, 2015. [Google Scholar] [CrossRef] [PubMed]
- Al-Snafi, A.E. The chemical contents and pharmacological effects of Anagallis arvensis—A review. Int. J. Pharm. 2015, 5, 37–41. [Google Scholar]
- Shyaula, S.L. Phytochemicals, Traditional Uses and Processing of Aconitum Species in Nepal. Nepal J. Sci. Technol. 2012, 12, 171–178. [Google Scholar] [CrossRef]
- Majid, A.; Ahmad, H.; Saqib, Z.; Rahman, I.U.; Khan, U.; Alam, J.; Shah, A.H.; Jan, S.A.; Ali, N. Exploring threatened traditional knowledge; ethnomedicinal studies of rare endemic flora from Lesser Himalayan region of Pakistan. Rev. Bras. Farmacogn. 2019, 29, 785–792. [Google Scholar] [CrossRef]
- Balslev, H.; Srisanga, P.; Srithi, K.; Trisonthi, C.; Wangpakapattanawong, P. Medicinal plant knowledge and its erosion among the Mien (Yao) in northern Thailand. J. Ethnopharmacol. 2009, 123, 335–342. [Google Scholar]
- Akassh, M.; Fathima, T.; Mruthunjaya, K. Health promoting effects of Ziziphus mauritiana: An overview. Int. J. Res. Pharm. Sci. 2020, 11, 1067–1072. [Google Scholar] [CrossRef]
- Ashraf, A.; Sarfraz, R.A.; Rashid, M.A.; Shahid, M. Antioxidant, antimicrobial, antitumor, and cytotoxic activities of an important medicinal plant (Euphorbia royleana) from Pakistan. J. Food Drug Anal. 2015, 23, 109–115. [Google Scholar] [CrossRef]
- Thakur, S.; Tashi, N.; Singh, B.; Dutt, H.C.; Singh, B. Ethnobotanical plants used for gastrointestinal ailments by the inhabitants of Kishtwar Plateau in Northwestern Himalaya, India. Indian J. Tradit. Knowl. 2020, 19, 288–298. [Google Scholar]
- Chakraborty, T.; Saha, S.; Bisht, N.S. First report on the ethnopharmacological uses of medicinal plants by Monpa tribe from the Zemithang region of Arunachal Pradesh, Eastern Himalayas, India. Plants 2017, 6, 13. [Google Scholar] [CrossRef]
- Khuda, F.; Iqbal, Z.; Khan, A.; Zakiullah; Nasir, F.; Khan, M.S. Validation of some of the ethnopharmacological uses of Xanthium strumarium and Duchesnea Indica. Pak. J. Bot. 2012, 44, 1199–1201. [Google Scholar]
- Alamgeer; Younis, W.; Asif, H.; Sharif, A.; Riaz, H.; Bukhari, I.A.; Assiri, A.M. Traditional medicinal plants used for respiratory disorders in Pakistan: A review of the ethno-medicinal and pharmacological evidence Milen Georgiev, Ruibing Wang. Chin. Med. 2018, 13. [Google Scholar] [CrossRef]
- Rashid, A.; SHARMA, A. Exploration of Economically I Mportant Fodder Plants of District Rajouri-Jammu and Kashmir State. Life 2012, 2, 142–149. [Google Scholar]
- Hl, R.; Kekuda, P.T. Ethnobotanical uses, phytochemistry and biological activities of Salix tetrasperma roxb. (Salicaceae)—A review. J. Med. Plants Stud. 2017, 5, 201–206. [Google Scholar]
- Ahmad, M.; Butt, M.A.; Zhang, G.; Sultana, S.; Tariq, A.; Zafar, M. Bergenia ciliata: A comprehensive review of its traditional uses, phytochemistry, pharmacology and safety. Biomed. Pharmacother. 2018, 97, 708–721. [Google Scholar] [CrossRef]
- Bharate, S.B.; Kumar, V.; Bharate, S.S.; Singh, B.; Singh, G.; Singh, A.; Gupta, M.; Singh, D.; Kumar, A.; Singh, S.; et al. Discovery and preclinical development of IIIM-160, a Bergenia ciliata-based anti-inflammatory and anti-arthritic botanical drug candidate. J. Integr. Med. 2019, 17, 192–204. [Google Scholar] [CrossRef] [PubMed]
- Hussain, K.; Shahazad, A.; Zia-Ul-Hussnain, S. An Ethnobotanical Survey of Important Wild Medicinal Plants of Hattar District Haripur, Pakistan. Ethnobot. Leafl. 2008, 12, 29–35. [Google Scholar]
- Hussain, M.; Akram, W.; Ahmad, J.; Qasim, T.B.; Bibi, R. Ethnopharmacological Investigations of Phytochemical Constituents Isolated from the Genus Atropa. Int. J. Sci. Eng. Res. 2019, 10, 589–612. [Google Scholar] [CrossRef]
- Soni, P.; Siddiqui, A.A.; Dwivedi, J.; Soni, V. Pharmacological properties of Datura stramonium L. as a potential medicinal tree: An overview. Asian Pac. J. Trop. Biomed. 2012, 2, 1002–1008. [Google Scholar] [CrossRef]
- Dhouibi, R.; Affes, H.; Ben Salem, M.; Hammami, S.; Sahnoun, Z.; Zeghal, K.M.; Ksouda, K. Screening of pharmacological uses of Urtica dioica and others benefits. Prog. Biophys. Mol. Biol. 2020, 150, 67–77. [Google Scholar] [CrossRef] [PubMed]
- Mahboubi, M.; Taghizadeh Kashani, L.M. A Narrative study about the role of Viola odorata as traditional medicinal plant in management of respiratory problems. Adv. Integr. Med. 2018, 5, 112–118. [Google Scholar] [CrossRef]
- Arora, P.; Ansari, S.H.; Najmi, A.K.; Anjum, V.; Ahmad, S. Investigation of anti-asthmatic potential of dried fruits of Vitis vinifera L. in animal model of bronchial asthma. Allergy Asthma Clin. Immunol. 2016, 12. [Google Scholar] [CrossRef] [PubMed]
- Bais, S.; Gill, N.S.; Rana, N.; Shandil, S. A Phytopharmacological Review on a Medicinal Plant: Juniperus communis. Int. Sch. Res. Not. 2014, 2014, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Medinipur, P.; Bengal, W. Importance of Cedrus Deodara (Roxb. Ex D. Don) G. Don: A Review of Its Ethnobotany, Phytochemical Constituents and Antioxidant Potential Importance of Cedrus deodara (Roxb. Ex D. Don) G. Don: A Review of Its Ethnobotany, Phytochemical Consti. 2019. Available online: https://www.researchgate.net/publication/336702402_A_review_on_phytochemical_ethnobotanical_pharmacological_and_antimicrobial_importance_of_Cedrus_deodara_Roxb_Ex_D_Don_G_Don (accessed on 30 August 2021).
- Kaushik, P.; Kaushik, D.; Khokra, S.L. Ethnobotany and phytopharmacology of Pinus roxburghii Sargent: A plant review. J. Integr. Med. 2013, 11, 371–376. [Google Scholar] [CrossRef]
- Khan, R.U.; Mehmood, S.; Ullah, S.; Subhan, M. Ethnobotanical study of common weed flora of sugarcane in District Bannu, Khyber Pakhtunkhawa, Pakistan. J. Med. Plant Stud. 2013, 1, 49–78. [Google Scholar]
- Reyes-García, V.; Guèze, M.; Luz, A.C.; Paneque-Gálvez, J.; Macía, M.J.; Orta-Martínez, M.; Pino, J.; Rubio-Campillo, X. Evidence of traditional knowledge loss among a contemporary indigenous society. Evol. Hum. Behav. 2013, 34, 249–257. [Google Scholar] [CrossRef]
- Voeks, R.A.; Leony, A. Forgetting the forest: Assessing medicinal plant erosion in eastern Brazil. Econ. Bot. 2004, 58. [Google Scholar] [CrossRef]
- Singh, B.; Bedi, Y.S. Eating from raw wild plants in Himalaya: Traditional knowledge documentary on sheena tribe in Kashmir. Indian J. Nat. Prod. Resour. 2017, 8, 269–275. [Google Scholar]
- Voeks, R.A. Tropical forest healers and habitat preference. Econ. Bot. 1996, 50, 381–400. [Google Scholar] [CrossRef]
- Lone, M.A.; Shrivastava, P.N.; Saxena, R.C.; Lone, M.A. Survey of ethnomedicinal plants of Lolab valley of Kashmir for skin diseases. Biosci. Biotechnol. Res. Asia 2009, 6, 355–358. [Google Scholar]
- Shankar, U.; Lama, S.D.; Bawa, K.S. Ecology and economics of domestication of non-timber forest products: An illustration of broomgrass in Darjeeling Himalaya. J. Trop. For. Sci. 2001, 13, 171–191. [Google Scholar]
- Cano, E.; Cano-Ortiz, A.; Musarella, C.M.; Piñar Fuentes, J.C.; Quinto-Canas, R.; Spampinato, G.; Pinto Gomes, C.J. Endemic and Rare Species of Asteraceae from the Southern Iberian Peninsula: Ecology, Distribution and Syntaxonomy. In AA.VV. Asteraceae: Characteristics, Distribution and Ecology; Nova Science Publishers, Inc.: New York, NY, USA, 2019; pp. 147–175. ISBN 9781536166323. [Google Scholar]
- Bell, E.A. Plant science research. Science 1971, 174, 454. [Google Scholar] [CrossRef]
- Sicari, V.; Loizzo, M.R.; Silva, A.S.; Romeo, R.; Spampinato, G.; Tundis, R.; Leporini, M.; Musarella, C.M. The effect of blanching on phytochemical content and bioactivity of Hypochaeris and Hyoseris species (Asteraceae), vegetables traditionally used in Southern Italy. Foods 2021, 10, 32. [Google Scholar] [CrossRef]
- Frezza, C.; Venditti, A.; Giuliani, C.; Foddai, S.; Cianfaglione, K.; Maggi, F.; Fico, G.; Guiso, M.; Nicoletti, M.; Bianco, A. Occurrence of flavonoids in different Lamiaceae taxa for a preliminary study on their evolution based on phytochemistry. Biochem. Syst. Ecol. 2021, 96. [Google Scholar] [CrossRef]
- Panuccio, M.R.; Fazio, A.; Musarella, C.M.; Mendoza-fernández, A.J.; Mota, J.F.; Spampinato, G. Seed germination and antioxidant pattern in Lavandula multifida (Lamiaceae): A comparison between core and peripheral populations. Plant Biosyst. 2018, 152, 398–406. [Google Scholar] [CrossRef]
- Vescio, R.; Abenavoli, M.R.; Araniti, F.; Musarella, C.M.; Sofo, A.; Laface, V.L.A.; Spampinato, G.; Sorgonà, A. The assessment and the within-plant variation of the morpho-physiological traits and vocs profile in endemic and rare salvia ceratophylloides ard. (lamiaceae). Plants 2021, 10, 474. [Google Scholar] [CrossRef]
- Dutta, A.; Sharma, Y.P.; Singh, B. Ethno-medicinal plants and their role in the traditional healthcare system of the local populace of District Poonch, Jammu & Kashmir. In Human-Plant Relations and Future Drug Discovery; Sharma, Y.P., Singh, B., Eds.; New India Publishing Agency: New Delhi, India, 2021; pp. 233–247. [Google Scholar]
- Singh, B.; Surmal, O.; Singh, B.; Singh, S.; Bhat, M.N.; Chowdhary, M.A.; Sneha; Shahnawaz, M. Folklore plants used in Tibetan mountain-based Sowa-Rigpa system of food and medicine: A close look on plant-people perception to herbal cure. In Plants for Novel Drug Molecules-Ethnobotany to Ethnopharmacology; Singh, B., Sharma, Y.P., Eds.; New India Publishing Agency: New Delhi, India, 2021; pp. 1–43. [Google Scholar]
- Valerio, F.; Mezzapesa, G.N.; Ghannouchi, A.; Mondelli, D.; Logrieco, A.F.; Perrino, E.V. Characterization and Antimicrobial Properties of Essential Oils from Four Wild Taxa of Lamiaceae Family Growing in Apulia. Agronomy 2021, 11, 1431. [Google Scholar] [CrossRef]
- Verma, R.S.; Padalia, R.C.; Chanotiya, C.S.; Chauhan, A. Chemical investigation of essential oil of Thymus linearis (Benth. ex Benth) from Western Himalaya India. Nat. Prod. Res. 2010, 24, 1890–1896. [Google Scholar] [CrossRef]
- Wink, M. Modes of action of herbal medicines and Plant secondary metabolites. Medicines 2015, 2, 251–286. [Google Scholar] [CrossRef] [PubMed]
- Subash, A.K.; Augustine, A. Hypolipidemic effect of methanol fraction of Aconitum heterophyllum wall ex Royle and the mechanism of action in diet-induced obese rats. J. Adv. Pharm. Technol. Res. 2012, 3, 224–228. [Google Scholar] [CrossRef] [PubMed]
- Paramanick, D.; Panday, R.; Shukla, S.S.; Sharma, V. Primary pharmacological and other important findings on the medicinal plant “Aconitum heterophyllum” (Aruna). J. Pharmacopunct. 2017, 20, 89–92. [Google Scholar] [CrossRef]
- Al-Shamaony, L.; Al-Khazraji, S.M.; Twaij, H.A.A. Hypoglycaemic effect of Artemisia herba alba. II. Effect of a valuable extract on some blood parameters in diabetic animals. J. Ethnopharmacol. 1994, 43, 167–171. [Google Scholar] [CrossRef]
- Singh, M.; Pnadey, M.; Agnihotri, V.; Singh, K.K.; Pandey, A. Antioxidant, Antimicrobial and bioactive compounds of Bergenia ciliata Sternb.: A valuable medicinal Herb of Sikkim Himalaya. J. Tradit. Complementary Med. 2017, 7, 152–157. [Google Scholar] [CrossRef]
- Petrakou, K.; Iatrou, G.; Lamari, F.N. Ethnopharmacological survey of medicinal plants traded in herbal markets in the Peloponnisos, Greece. J. Herb. Med. 2020, 19. [Google Scholar] [CrossRef]
- Andrade-Cetto, A. Ethnobotanical study of the medicinal plants from Tlanchinol, Hidalgo, México. J. Ethnopharmacol. 2009. [Google Scholar] [CrossRef] [PubMed]
- Boschi-Pinto, C.; Velebit, L.; Shibuya, K. Estimating child mortality due to diarrhoea in developing countries. Bull. World Health Organ. 2008. [Google Scholar] [CrossRef] [PubMed]
- Ojha, S.N.; Tiwari, D.; Anand, A.; Sundriyal, R.C. Ethnomedicinal Knowledge of marginal hill community of central Himalaya: Diversity, usage pattern, and conservation cpncerns. J. Ethnobiol. Ethnomed. 2020, 16, 1–21. [Google Scholar] [CrossRef]
- Perrino, E.V.; Valerio, F.; Gannouchi, A.; Trani, A.; Mezzapesa, G. Ecological and plant community implication on essential oils composition in useful wild officinal species: A pilot case study in Apulia (Italy). Plants 2021, 10, 574. [Google Scholar] [CrossRef]
- Ullah, M.; Khan, M.U.; Mahmood, A.; Malik, R.N.; Hussain, M.; Wazir, S.M.; Daud, M.; Shinwari, Z.K. An ethnobotanical survey of indigenous medicinal plants in Wana district south Waziristan agency Pakistan. J. Ethnopharmocol. 2013, 150, 918–924. [Google Scholar] [CrossRef]
- ElAmri, J.; ELBadaoui, K.; Zair, T.; Bouharb, H.; Chakir, S.; Alaoui, T.E. Ethnobotanical study of medicinal plants in the region El Hajeb (central Morocco). J. Res. Biol. 2014, 4, 1568–1580. [Google Scholar]
- Schlage, C.; Mabula, C.; Mahunnah, R.L.A.; Heinrich, M. Medicinal plants of the Washambaa (Tanzania): Documentation and ethnopharmacological evaluation. Plant Biol. 2000, 2, 83–92. [Google Scholar] [CrossRef]
- Farooq, A.; Amjad, M.S.; Ahmad, K.; Altaf, M.; Umair, M.; Abbasi, A.M. Ethnomedicinal knowledge of the rural communities of Dhirkot, Azad Jammu and Kashmir, Pakistan. J. Ethnobiol. Ethnomedicine 2019, 15. [Google Scholar] [CrossRef] [PubMed]
- Kayani, S.; Ahmad, M.; Sultana, S.; Khan Shinwari, Z.; Zafar, M.; Yaseen, G.; Hussain, M.; Bibi, T. Ethnobotany of medicinal plants among the communities of Alpine and Sub-alpine regions of Pakistan. J. Ethnopharmacol. 2015, 164, 186–202. [Google Scholar] [CrossRef] [PubMed]
- Noctor, G.; Foyer, C.H. Ascorbate and Glutathione: Keeping Active Oxygen under Control. Annu. Rev. Plant Biol. 1998, 49, 249–279. [Google Scholar] [CrossRef]
- Umair, M.; Altaf, M.; Abbasi, A.M. An ethnobotanical survey of indigenous medicinal plants in Hafizabad district, Punjab-Pakistan. PLoS ONE 2017, 12. [Google Scholar] [CrossRef]
- Samuelsen, A.B. The traditional uses, chemical constituents and biological activities of Plantago major L. A review. J. Ethnopharmacol. 2000, 71, 1–21. [Google Scholar] [CrossRef]
- Singh, K.P. Entamoeba histolytica and Holarrhena antidysenterica. Anc. Sci. Life 1986, 5, 228–234. [Google Scholar]
- Kavitha, D.; Shilpa, P.N.; Niranjali Devaraj, S. Antibacterial and antidiarrhoeal effects of alkaloids of Holarrhena antidysenterica Wall. Indian J. Exp. Biol. 2004, 42, 589–594. [Google Scholar] [PubMed]
- Negi, V.S.; Maikhuri, R.K.; Maletha, A.; Phondani, P.C. Ethnobotanical Knowledge and Population Density of Threatened Medicinal Plants of Nanda Devi Biosphere Reserve, Western Himalaya, India. Iran. J. Sci. Technol. Trans. A Sci. 2019, 43, 63–73. [Google Scholar] [CrossRef]
- Kumar, V.L.; Roy, S. Calotropis procera latex extract affords protection against inflammation and oxidative stress in Freund’s complete adjuvant-induced monoarthritis in rats. Mediat. Inflamm. 2007, 2007. [Google Scholar] [CrossRef]
- Grieve, M.; Leyel, C.F. A Modern Herbal: The Medicinal, Culinary, Cosmetic and Economic Properties, Cultivation and Folklore of Herbs, Grasses, Fungi, Shrubs and Trees with All Their Modern Scientific Uses; Dover publications: New York, NY, USA, 1980; p. 912. [Google Scholar]
- Di Napoli, A.; Zucchetti, P. A comprehensive review of the benefits of Taraxacum officinale on human health. Bull. Natl. Res. Cent. 2021, 45. [Google Scholar] [CrossRef]
- Debnath, P.; Rathore, S.; Walia, S.; Kumar, M.; Devi, R.; Kumar, R. Picrorhiza kurroa: A promising traditional therapeutic herb from higher altitude of western Himalayas. J. Herb. Med. 2020, 23. [Google Scholar] [CrossRef]
- Gaire, B.P.; Subedi, L. A review on the pharmacological and toxicological aspects of Datura stramonium L. J. Chin. Integr. Med. 2013, 11, 73–79. [Google Scholar] [CrossRef]
- Srivastava, R. The Medicinal Significance of Datura stramonium: A Review. Biomed. J. Sci. Tech. Res. 2020, 29. [Google Scholar] [CrossRef]
- Guarrera, P.M. Traditional antihelmintic, antiparasitic and repellent uses of plants in Central Italy. J. Ethnopharm. 2001, 68, 183–192. [Google Scholar] [CrossRef]
- Bhatia, H.; Sharma, Y.P.; Manhas, R.K.; Kumar, K. Ethnomedicinal plants used by the villagers of district Udhampur, J&K, India. J. Ethnopharmacol. 2014, 151, 1005–1018. [Google Scholar] [CrossRef]
- Adzu, B.; Gamaniel, K. Sedative effects of Cassia singueana root bark. J. Nat. Remedies 2003, 3, 134–137. [Google Scholar] [CrossRef]
- Ahmad, M.; Khan, M.A.; Zafar, M.; Arshad, M.; Sultana, S.; Abbasi, B.H.; Siraj-Ud-Din. Use of chemotaxonomic markers for misidentified medicinal plants used in traditional medicines. J. Med. Plants Res. 2010, 4, 1244–1252. [Google Scholar] [CrossRef]
- Ali, S.; Khan, M.R.; Sajid, M.; Zahra, Z. Phytochemical investigation and antimicrobial appraisal of Parrotiopsis jacquemontiana (Decne) Rehder. BMC Complementary Altern. Med. 2018, 18. [Google Scholar] [CrossRef]
- Malik, M.A.; Bhat, S.A.; Fatima, B.; Ahmad, B.S.; Sidiqui, S.; Shrivastava, P. Rheum emodi as valuable medicinal Plant. Int. J. Gen. Med. Pharm. 2018, 5, 35–44. [Google Scholar]
- Guan, Y.S.; He, Q. Plants Consumption and Liver Health. Evid. Based Complementary Altern. Med. 2015, 2015. [Google Scholar] [CrossRef]
- Srivastava, T.; Badola, D.; Shah, D.; Gupta, O. Ethno-medico-botanical exploration of Figurez Valley Kashmir. Bull Med. Ethnobot Res. 1984, 5, 15–54. [Google Scholar]
- Amjad, M.S.; Zahoor, U.; Bussmann, R.W.; Altaf, M.; Gardazi, S.M.H.; Abbasi, A.M. Ethnobotanical survey of the medicinal flora of Harighal, Azad Jammu & Kashmir, Pakistan. J. Ethnobiol. Ethnomed. 2020, 16. [Google Scholar] [CrossRef]
- Rafiq, N.; Bhat, G.M.; Islam, M.A.; Bakshi, M.R.; Pala, N.A.; Bhat, R.A.; Fatima, S. Effect of spacing and rhizome diameter on different growth parameters and oil content of Bergenia ciliata L. under temperate conditions of Kashmir Valley. Emergent Life Sci. Res. 2020, 06, 82–89. [Google Scholar] [CrossRef]
- Palabaş Uzun, S.; Koca, C. Ethnobotanical survey of medicinal plants traded in herbal markets of Kahramanmaraş. Plant Divers. 2021. [Google Scholar] [CrossRef]
- Kayani, S.; Ahmad, M.; Zafar, M.; Sultana, S.; Khan, M.P.Z.; Ashraf, M.A.; Hussain, J.; Yaseen, G. Ethnobotanical uses of medicinal plants for respiratory disorders among the inhabitants of Gallies-Abbottabad, Northern Pakistan. J. Ethnopharmacol. 2014, 156, 47–60. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, S.K.; Maulik, S.K. Effect of garlic on cardiovascular disorders: A review. Nutr. J. 2002, 1, 1–14. [Google Scholar] [CrossRef]
- Street, R.A.; Sidana, J.; Prinsloo, G. Cichorium intybus: Traditional uses, phytochemistry, pharmacology, and toxicology. Evid. -Based Complementary Altern. Med. 2013. [Google Scholar] [CrossRef]
- Kaur, M.; Singhal, V.K.; Singh, J. Use of Some Ethnomedicinal Herbs By the Natives of Solang Valley, Kullu District, Himachal Pradesh. Int. J. Pharm. Pharm. Sci. 2017, 9, 222. [Google Scholar] [CrossRef]
- Orch, H.; Zidane, L.; Douira, A. Ethnobotanical study of plants used in the treatment of respiratory diseases in a population bordering the forest of Izarène. J. Pharm. Pharmacogn. Res. 2020, 8, 392–409. [Google Scholar]
- Shukla, V.; Singh, P.; Kumar, D.; Konwar, R.; Singh, B.; Kumar, B. Phytochemical analysis of high value medicinal plant Valeriana jatamansi using LC-MS and it’s in-vitro anti-proliferative screening. Phytomed. Plus 2021, 1, 100025. [Google Scholar] [CrossRef]
- Kumar, M.; Paul, Y.; Anand, V.K. An Ethnobotanical Study of Medicinal Plants used by the Locals in Kishtwar, Jammu and Kashmir, India. J. Ethnobiol. Ethnomedicine 2009, 13, 1240–1256. [Google Scholar]
- Kumar, R.; Gupta, Y.K.; Singh, S. Anti-inflammatory and anti-granuloma activity of Berberis aristata DC. in experimental models of inflammation. Indian J. Pharmacol. 2016, 48, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Wani, Z.A.; Pant, S. Ethnomedicinal study of plants used to cure skin diseases and healing of wounds in gulmarg wildlife sanctuary (GWLS), Jammu & Kashmir. Indian J. Tradit. Knowl. 2020, 19, 327–334. [Google Scholar]
- Alamgir, A.N.M. Therapeutic Use of Medicinal Plants and Their Extracts. Prog. Drug Res. 2017, 73, 105–123. [Google Scholar]
- Tangjitman, K.; Wongsawad, C.; Kamwong, K.; Sukkho, T.; Trisonthi, C. Ethnomedicinal plants used for digestive system disorders by the Karen of northern Thailand. J. Ethnobiol. Ethnomed. 2015, 11. [Google Scholar] [CrossRef] [PubMed]
- Jan, M.; Mir, T.A.; Ganie, A.H.; Khare, R.K. Ethnomedicinal use of some Plant species by Gujjar and bakerwal community in Gulmarg Mountainous regions of Kashmir Himalaya. Ethnobot. Res. Appl. 2021, 23, 1–23. [Google Scholar]
- Khanday, Z.H.; Singh, S. Ethnomedicinal Plants used for curing various Skin diseases in Shopian district of Jammu and Kashmir. J. Phytol. 2017, 9. [Google Scholar] [CrossRef][Green Version]
- Slathia, P.; Bhagat, G.; Singh, S.; Kher, S.; Paul, N. Traditional knowledge on utility of Cedrus deodara (Roxb.) Loud. in Doda district of Jammu province. Indian J. Tradit. Knowl. (IJTK) 2007, 06, 518–520. [Google Scholar]
- Anwar, S.; Ahmed, N.; Habibatni, S.; Abusamra, Y. Ajwain (Trachyspermum ammi L.) oils. Essent. Oils Food Preserv. Flavor Saf. 2016, 181–192. [Google Scholar] [CrossRef]
- Tayade, A.; Dhar, P.; Ballabh, B.; Kumar, R.; Chaurasia, O.P.; Bhatt, R.P.; Srivastava, R.B. Rheum webbianum royle: A potential medicinal plant from trans-himalayan cold deserts of Ladakh, India. Plant Arch. 2012, 12, 603–606. [Google Scholar]
- Asati, A.; Sahoo, H.; Sahu, S.; Dwivedi, A. Phytochemical and pharmacological profile of Cannabis sativa L. Drugs 2017, 2, 37–45. [Google Scholar]
- Kaunda, J.S.; Zhang, Y.J. The Genus Solanum: An Ethnopharmacological, Phytochemical and Biological Properties Review. Nat. Prod. Bioprospect. 2019, 9, 77–137. [Google Scholar] [CrossRef]
- Shahzad Aslam, M.; Choudhary, B.A.; Uzair, M.; Subhan Ijaz, A. The genus Ranunculus: A phytochemical and ethnopharmacological review. Int. J. Pharm. Pharm. Sci. 2012, 4, 15–22. [Google Scholar]
- Liu, J.; Liang, S.C.; Liu, F.H.; Wang, R.Q.; Dong, M. Invasive alien plant species in China: Regional distribution patterns. Divers. Distrib. 2005, 11, 341–347. [Google Scholar] [CrossRef]
- Walther, G.R.; Roques, A.; Hulme, P.E.; Sykes, M.T.; Pyšek, P.; Kühn, I.; Zobel, M.; Bacher, S.; Botta-Dukát, Z.; Bugmann, H.; et al. Alien species in a warmer world: Risks and opportunities. Trends Ecol. Evol. 2009, 24, 686–693. [Google Scholar] [CrossRef] [PubMed]
- Laface, V.L.A.; Musarella, C.M.; Ortiz, A.C.; Canas, R.Q.; Cannavò, S.; Spampinato, G. Three new alien taxa for europe and a chorological update on the alien vascular flora of calabria (Southern Italy). Plants 2020, 9, 1181. [Google Scholar] [CrossRef]
- Reddy, C.S. Catalogue of invasive alien flora of India. Life Sci. J. 2008, 5, 84–89. [Google Scholar]
- Musarella, C.M. Solanum torvum Sw. (Solanaceae): A new alien species for Europe. Genet. Resour. Crop Evol. 2020, 67, 515–522. [Google Scholar] [CrossRef]
- Wu, S.H.; Sun, H.T.; Teng, Y.C.; Rejmánek, M.; Chaw, S.M.; Yang, A.Y.A.; Hsieh, C.F. Patterns of plant invasions in China: Taxonomic, biogeographic, climatic approaches and anthropogenic effects. Biol. Invasions 2010, 12, 2179–2206. [Google Scholar] [CrossRef]
- Khuroo, A.A.; Weber, E.; Malik, A.H.; Dar, G.H.; Reshi, Z.A. Taxonomic and biogeographic patterns in the native and alien woody flora of Kashmir Himalaya, India. Nord. J. Bot. 2010, 28, 685–696. [Google Scholar] [CrossRef]
- Randall, B.R.P.; Weed, A.; Waterhouse, B.; Mitchell, A.; Williams, P.; Cooke, D.; Virtue, J. The Introduced Flora of Australia and Its Weed Status. CRC for Australian Weed Management Glen Osmond Australia. 2007. Available online: https://www.cabi.org/isc/abstract/20093033838 (accessed on 30 August 2021).
- Diez, J.M.; D’Antonio, C.M.; Dukes, J.S.; Grosholz, E.D.; Olden, J.D.; Sorte, C.J.B.; Blumenthal, D.M.; Bradley, B.A.; Early, R.; Ibáñez, I.; et al. Will extreme climatic events facilitate biological invasions? Front. Ecol. Environ. 2012, 10, 249–257. [Google Scholar] [CrossRef]
- Lambdon, P.W.; Pyšek, P.; Basnou, C.; Arianoutsou, M.; Essl, F.; Hejda, M.; Jarošík, V.; Pergl, J.; Winter, M.; Anastasiu, P.; et al. Alien flora of Europe: Species diversity, temporal trends, geographical patterns and research needs. Preslia 2010, 80, 101–149. [Google Scholar]
- Rosati, L.; Fascetti, S.; Romano, V.A.; Potenza, G.; Lapenna, M.R.; Capano, A.; Nicoletti, P.; Farris, E.; de Lange, P.J.; Vico, E.D.; et al. New chorological data for the italian vascular flora. Diversity 2020, 12, 22. [Google Scholar] [CrossRef]
- Musarella, C.M.; Stinca, A.; Cano-Ortíz, A.; Laface, V.L.A.; Petrilli, R.; Esposito, A.; Spampinato, G. New data on the alien vascular flora of calabria (Southern Italy). Ann. Bot. 2020, 10, 55–66. [Google Scholar] [CrossRef]
- Kohli, R.K.; Dogra, K.S.; Batish, D.R.; Singh, H.P. Impact of Invasive Plants on the Structure and Composition of Natural Vegetation of Northwestern Indian Himalayas 1. Weed Technol. 2004, 18, 1296–1300. [Google Scholar] [CrossRef]
- Khuroo, A.A.; Reshi, Z.A.; Malik, A.H.; Weber, E.; Rashid, I.; Dar, G.H. Alien flora of India: Taxonomic composition, invasion status and biogeographic affiliations. Biol. Invasions 2012, 14, 99–113. [Google Scholar] [CrossRef]
- Adhikari, D.; Tiwary, R.; Barik, S.K. Modelling Hotspots for Invasive Alien Plants in India. PLoS ONE 2015, 10, e0134665. [Google Scholar] [CrossRef]





| Factor | Study Area (km2) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Chota Bungus (924) | Ringbala (93) | Indradhook (129) | Dudi (176) | Machil (948) | Lalpora (67) | Warnow (98) | Chuntiwari (75) | Total | ||
| GPS Coordinates | Latitude (N) | 34°22′20″ | 34°38′01″ | 34°33′51″ | 34°33′53″ | 34°38′51″ | 34°25′38″ | 34°31′43″ | 34°33′59″ | - |
| Longitude (E) | 74°03′29″ | 74°27′36″ | 74°20′31″ | 74°18′59″ | 74°27′05″ | 74°20′21″ | 74°28′15″ | 74°16′42″ | - | |
| Population * | Male | 800 | 300 | 300 | 500 | 813 | 1097 | 1101 | 731 | 5642 |
| Female | 684 | 250 | 200 | 467 | 722 | 930 | 1033 | 600 | 4886 | |
| Total | 1484 | 550 | 500 | 967 | 1535 | 2027 | 2134 | 1331 | 10,528 | |
| Informants interviewed | Male | 5 | 6 | 16 | 8 | 7 | 12 | 14 | 9 | 77 |
| Female | 2 | 2 | 5 | 4 | 1 | 4 | 4 | 3 | 25 | |
| Total | 7 | 8 | 21 | 12 | 8 | 16 | 18 | 12 | 102 | |
| Education | Graduate | 0 | 1 | 0 | 1 | 0 | 4 | 0 | 0 | 6 |
| Illiterate | 2 | 2 | 9 | 1 | 4 | 2 | 4 | 1 | 25 | |
| Middle | 2 | 2 | 5 | 0 | 1 | 2 | 7 | 5 | 24 | |
| Post graduate | 0 | 0 | 0 | 0 | 0 | 3 | 0 | 0 | 3 | |
| Primary | 2 | 2 | 3 | 2 | 2 | 2 | 3 | 2 | 18 | |
| Matriculation | 0 | 0 | 1 | 5 | 0 | 1 | 2 | 0 | 9 | |
| Senior Secondary | 1 | 1 | 3 | 3 | 1 | 2 | 2 | 4 | 17 | |
| Total | 7 | 8 | 21 | 12 | 8 | 16 | 18 | 12 | 102 | |
| Community (Informants) | Dard | 7 | 8 | 0 | 12 | 8 | 0 | 0 | 0 | 35 |
| Gujjar | 0 | 0 | 21 | 0 | 0 | 0 | 0 | 0 | 21 | |
| Kashmiri | 0 | 0 | 0 | 0 | 0 | 16 | 18 | 12 | 46 | |
| Total | 7 | 8 | 21 | 12 | 8 | 16 | 18 | 12 | 102 | |
| Use-reports mentioned (URs) ** | 361 | 174 | 223 | 127 | 388 | 172 | 86 | 94 | 1631 | |
| Plant Taxa Identified *** | 67 | 54 | 49 | 34 | 77 | 56 | 29 | 36 | - | |
| Relative frequency (Rf,%) | 62.62 | 50.47 | 45.79 | 31.78 | 71.96 | 52.34 | 27.10 | 33.64 | 100.00 | |
| Category | Taxa Reported | Chi-Square Test Value | p-Value | ||
|---|---|---|---|---|---|
| ≤5 | >5 | ||||
| Gender | F | 15 | 20 | 0.885 | 0.347 |
| M | 54 | 13 | |||
| Place | Chuntiwari | 7 | 13 | 14.516 | 0.043 |
| Dudi | 8 | 12 | |||
| Indradhook | 12 | 21 | |||
| Khurhamma | 4 | 8 | |||
| Lalpora | 10 | 12 | |||
| Machil | 6 | 8 | |||
| Chota Bungus | 9 | 10 | |||
| Warnow | 13 | 18 | |||
| Community | Dard | 21 | 12 | 2.120 | 0.347 |
| Kashmiri | 19 | 12 | |||
| Gujjar | 9 | 29 | |||
| Education category | Illiterate | 15 | 18 | 13.734 | 0.017 |
| Primary | 8 | 5 | |||
| Middle | 18 | 5 | |||
| Matric | 11 | 3 | |||
| Senior Secondary | 9 | 1 | |||
| Graduate | 8 | 1 | |||
| Age category | ≤30 | 22 | 0 | 25.673 | 0.001 |
| 31–40 | 9 | 0 | |||
| 41–50 | 12 | 6 | |||
| 51–60 | 12 | 8 | |||
| 61–70 | 10 | 11 | |||
| 71–80 | 4 | 8 | |||
| Taxon/Specimen Code | Common Name | Life-Form | Plant Parts Used | Mode of Administration | Ethnobotanicalusage (EU)* | Use-Reports Mentioned By Informants (URs) | Use Frequency (Fq, %) | Relative Importance (RI) | Nativity (N)/Exotic (E) | Earlier Supported Studies |
|---|---|---|---|---|---|---|---|---|---|---|
| FUNGI | ||||||||||
| Morchellaceae | ||||||||||
| Morchella esculenta (L.) Pers./RRLH10182 | Sedguchchi | H | Wp | Decoction | GAS: 11 CAR: 18 | 29 | 28.43 | 35.23 | N | Wagay et al. [91] |
| LYCOPHYTES AND FERNS | ||||||||||
| Aspleniaceae | ||||||||||
| Asplenium crinicaule Hance /RRLH24815 | Dade | H | Wp | Juice/extract | CAR | 16 | 15.69 | 38.64 | N | Upreti et al. [92] |
| Equisetaceae | ||||||||||
| Equisetum arvense L./RRLH 24766 | Gundum gud | H | Wp | Juice/extract | GAS | 12 | 11.76 | 87.50 | N | Carneiro et al. [93] |
| Pteridaceae | ||||||||||
| Adiantum capillus-veneris L./RRLH24785 | Gawtheer | H | Wp | Powder | RES: 8 GAS: 11 | 19 | 18.63 | 26.14 | N | Dehdari and Hajimehdipoor [94] |
| MONOCOTYLEDONS | ||||||||||
| Acoraceae | ||||||||||
| Acorus calamus L./RRLH24859 | Vai gasnder | H | Rh | Powder | CAR: 10 RES: 18 GAS: 5 | 33 | 32.35 | 39.77 | N | Mukherjee et al. [14] |
| Amaryllidaceae | ||||||||||
| Allium sativum L./RRLH24756 | Rohun | H | Bb | Paste | RES: 9 MET: 3 | 12 | 11.76 | 43.18 | E | Gupta et al. [95] |
| Araceae | ||||||||||
| Arisaema jacquemontii Blume/RRLH24773 | Noel | H | Tu/Lv | Juice/extract | CAR: 13 DER: 14 RES: 10 | 37 | 36.27 | 57.95 | N | Roshan et al. [96] |
| Asparagaceae | ||||||||||
| Asparagus racemosus Willd./RRLH24869 | Satavir | H | Rh | Decoction | GYN | 36 | 35.29 | 47.73 | N | Rahman et al. [97] |
| Dioscoreaceae | ||||||||||
| Dioscorea deltoidea Wall.ex Griseb./RRLH24782 | Kraeth | L | Bb | Powder | GAS: 9 GYN: 4 | 13 | 12.75 | 43.18 | N | Dangwal and Chauhan [98] |
| Iridaceae | ||||||||||
| Iris kashmiriana Baker/RRLH24800 | Mazarmund | H | Rh | Powder | SKE: 17 FVR: 5 | 22 | 21.57 | 48.86 | N | Amin et al. |
| Liliaceae | [99] | |||||||||
| Fritillaria cirrhosa D.Don/RRLH25738 | Sheeth kar | H | Fr | Chew/Roasted | CAN: 21 DER: 13 GYN: 11 | 45 | 44.12 | 48.86 | N | Wang et al. [100] |
| Notholirion thomsonianum (Royle) Stapf./RRLH24321 | Shala misri | H | Se | Powder | SKE | 2 | 1.96 | 26.14 | N | Sadiq et al. [101] |
| Poaceae | ||||||||||
| Avena fatua L./RRLH24887 | Kandael | H | Rt | Juice/extract | EY | 11 | 10.78 | 34.09 | E | Khan et al. [20] |
| Cynodon dactylon (L.) Pers./RRLH24863 | Dramun | H | Wp | Powder | RES: 9 SKE: 5 | 14 | 13.73 | 35.23 | E | Harun et al. [102] |
| Oryza sativa L./RRLH23741 | Dhane | H | Fr | Decoction | DER | 12 | 11.76 | 53.41 | E | Cabanting and Perez [103] |
| Sorghum halepense (L.) Pers./ RRLH24858 | Durham, garneel | H | Rt | Paste | DER | 13 | 12.75 | 35.23 | E | Khayal [104] |
| DICOTYLEDONS | ||||||||||
| Adoxaceae | ||||||||||
| Sambucus wightiana Wall. ex Wight & Arn./RRLH24861 | Hapat fal | S | Lv | Paste | SKE: 8 ETH: 4 | 12 | 11.76 | 34.09 | N | Amjad et al. [105] |
| Amaranthaceae | 0.00 | |||||||||
| Amaranthus viridis L./RRLH24771 | Lessa/Ganhar | H | Lv | Juice/extract | FVR | 10 | 9.80 | 44.32 | E | Ibrahim et al. [106] |
| Apiaceae | ||||||||||
| Trachyspermum ammi (L.) Sprague/RRLH24784 | Ajwain | H | Se | Powder | GAS | 24 | 23.53 | 35.23 | N | Anwar et al. [107] |
| Asteraceae | ||||||||||
| Arctium lappa L./RRLH24814 | Pughood | H | Wp | Juice/extract | CAR: 12 DER: 11 | 23 | 22.55 | 39.77 | E | Wang et al. [108] |
| Artemisia absinthium L./RRLH24857 | Tethwayen | H | Lv | Decoction | CAN: 8 MET: 11 SKE: 7 | 26 | 25.49 | 48.86 | N | Nigam et al. [109] |
| Artemisia brevifolia Wall. ex DC./RRLH24803 | Moree | H | Wp | Decoction | GAS | 16 | 15.69 | 53.41 | N | Nigam et al. [109] |
| Artemisia imponens Pamp./RRLH24865 | Janglee tethwayeen | H | Wp | Decoction | GAS: 2 PAR: 7 | 9 | 8.82 | 44.32 | N | Nigam et al. [109] |
| Cichorium intybus L./RRLH24868 | Kasi hand | H | Fr | Chew/Roasted | DER: 7 GYN: 2 ETH: 6 | 15 | 14.71 | 53.41 | E | Nwafor et al. [110] |
| Dolomiaea macrocephala DC. ex Royle/RRLH24799 | Mera | H | Lv | Powder | GAS: 16 ETH: 5 | 21 | 20.59 | 26.14 | N | Negi et al. [111] |
| Matricaria chamomilla L./RRLH24800 | Fuk gass | H | Lv | Decoction | RES | 3 | 2.94 | 48.86 | E | Šavikin et al. [112] |
| Dolomiaea costus (Falc.) Kasana & A.K.Pandey/RRLH24765 | Kuth | H | Rt | Powder | SKE: 4 GAS: 7 DER: 13 RES: 6 | 26 | 25.49 | 65.91 | N | Pandey et al. [113] |
| Taraxacum officinale F.W. Wigg./RRLH24746 | Mudaan hand | H | Wp | Paste | DER: 17 EY: 13 | 30 | 29.41 | 62.50 | E | Menković et al. [114] |
| Berberidaceae | ||||||||||
| Berberis aristata DC./RRLH24754 | Daenlider | S | St | Powder | RES: 14, SKE: 6 | 20 | 19.61 | 44.32 | N | Malik et al. [115] |
| Podophyllum hexandrum Royle/RRLH24770 | Wanwangun/kakdi | H | Rt/Lv | Powder | MET: 9 SKE: 4 CAN: 11 | 24 | 23.53 | 53.41 | N | Chaurasia et al. [116] |
| Boraginaceae | 0.00 | |||||||||
| Arnebia benthamii (Wall. ex G. Don) I.M. Johnst./RRLH24798 | Kahzaban | H | Rt | Chew | CAN: 12, RES: 2 | 14 | 13.73 | 48.86 | N | Rana et al. [117] |
| Hackelia uncinata(Royle ex Benth.) C.E.C. Fisch./RRLH20240 | Neelan | H | Rt | Chew | DER | 12 | 11.76 | 35.23 | N | Tariq et al. [118] |
| Brassicaceae | ||||||||||
| Capsella bursa-pastoris (L.) Medik./RRLH24752 | Kral mund | H | Wp | Powder | GAS | 20 | 19.61 | 53.41 | E | Hadi et al. [119] |
| Cardamine impatiens L./RRLH19899 | Pahal laish | H | Lv | Juice/extract | RES | 5 | 4.90 | 39.77 | N | Rana and Samant [120] |
| Nasturtium officinale W.T.Aiton/RRLH25799 | Nag babed | H | Wp | Powder | ETH: 8, SKE: 4 | 12 | 11.76 | 56.82 | E | Bullitta et al. [121] |
| Campanulaceae | ||||||||||
| Codonopsis rotundifolia Benth./RRLH24796 | Belphul | H | Wp | Juice/extract | MET | 33 | 32.35 | 51.14 | N | Gupta et al. [122] |
| Cannabaceae | 0.00 | |||||||||
| Cannabis sativa L./RRLH24816 | Charas/Bang | S | Inf | Powder | NER | 16 | 15.69 | 56.82 | E | Zou and Kumar [123] |
| Celtis australis L./RRLH24748 | Brimij | T | Sh | Juice/extract | CAR | 2 | 1.96 | 48.86 | E | Sufyan et al. [124] |
| Caprifoliaceae | ||||||||||
| Dipsacus inermis Wall./RRLH24804 | Wtkrm | H | Lv | Powder | SKE | 2 | 1.96 | 26.14 | N | Singh et al. [125] |
| Valeriana jatamansi Jones ex Roxb./RRLH26596 | Mushkbala | H | Lv | Juice/extract | DER: 31 SKE: 16 | 47 | 46.08 | 56.82 | N | Uprety et al. [126] |
| Caryophyllaceae | ||||||||||
| Stellaria media (L.) Vill./RRLH24808 | Nik hak | H | Lv | Powder | CAR | 5 | 4.90 | 47.73 | E | Salam et al. [127] |
| Convolvulaceae | ||||||||||
| Cuscuta cassytoides Nees ex Engelm./RRLH24856 | Kukliporte | P | Wp | Powder | MET: 4 SKE: 9 | 13 | 12.75 | 26.14 | N | Gairola et al. [128] |
| Crassulaceae | ||||||||||
| Rhodiola himalensis (D.Don) S.H.Fu./RRLH20227 | Dand jari | H | Wp | Powder | CAN | 16 | 15.69 | 90.91 | N | Zhuang et al. [129] |
| Cucurbitaceae | ||||||||||
| Solena amplexicaulis (Lam.) Gandhi/RRLH24484 | Kharken | L | Rt | Decoction | GAS | 8 | 7.84 | 38.64 | N | Krishnamoorthy and Senguttuvan [130] |
| Euphorbiaceae | ||||||||||
| Euphorbia royleana Boiss./RRLH24794 | Gandi booti | H | Wp | Powder | GAS: 5 SKE: 2 | 7 | 6.86 | 52.27 | E | Ashraf et al. [131] |
| Fabaceae | ||||||||||
| Indigofera heterantha Wall. ex Brandis/RRLH24776 | Brand pathri/Zand | H | Se | Paste | RES | 4 | 3.92 | 26.14 | N | Rahman et al. [97,132] |
| Trifolium repens L./RRLH 24793 | Pancha/Gulnaksha ka phool | H | Wp | Chew//Roasted | RES | 9 | 8.82 | 53.41 | E | Kolodziejczyk-Czepas [133] |
| Trigonella foenum-graecum L./RRLH29542 | Meth | H | Wp | Paste | GAS | 7 | 6.86 | 39.77 | E | Bano et al. [134] |
| Gentianaceae | ||||||||||
| Gentiana kurrao Royle/RRLH24870 | Nelkanth | H | Wp | Paste | FVR | 12 | 11.76 | 69.32 | N | Mubashir et al. [135] |
| Geraniaceaeae | ||||||||||
| Geranium wallichianum D.Don ex Sweet/RRLH24777 | Rathan joti | H | Wp | Powder | ENT: 7 SKE: 9 | 16 | 15.69 | 21.59 | N | Qureshi et al. [136] |
| Hamamelidaceae | ||||||||||
| Parrotiopsis jacquemontiana (Decne.) Rehder/RRLH24819 | Poh | S | Rt | Juice/extract | DER | 4 | 3.92 | 56.82 | N | Ali et al. [137] |
| Juglandaceae | ||||||||||
| Juglans regia L./RLH20859 | Dun kul | T | Fr | Juice/extract | SKE | 23 | 22.55 | 39.77 | E | Delaviz et al. [138] |
| Lamiaceae | ||||||||||
| Ajuga bracteosa Buch.-Ham. ex. D. Don/RRLH24822 | Janeadam | H | Lv | Decoction | GAS: 19 ETH: 13 | 32 | 31.37 | 38.64 | N | Not found |
| Lamium album L./RRLH24769 | Khash khash | H | Lv | Juice/extract | CAR | 21 | 20.59 | 69.32 | N | Kelayeh et al. [139] |
| Mentha piperita L./RRLH24635 | Sed guch | H | Lv | Powder | RES | 12 | 11.76 | 53.41 | E | Shah and Mello [140] |
| Nepeta cataria L./RRLH24769 | Gansoi | H | Wp | Powder | ETH: 5 MET: 3 | 8 | 7.84 | 52.27 | N | Zomorodian et al. [141] |
| Prunella vulgaris L./RRLH24813 | Kalyuth | H | Lv | Paste | CAN | 8 | 7.84 | 30.68 | N | Huang et al. [142] |
| Thymus linearis Benth./RRLH24807 | Jayind | H | Wp | Powder | GAS: 7 FVR: 5 | 12 | 11.76 | 60.23 | N | Qadir et al.[143] |
| Malvaceae | ||||||||||
| Abutilon indicum (L.) Sweet/RRLH22614 | Ronsh pater | S | LV | Powder | GAS | 5 | 4.90 | 46.59 | E | Ravi et al. [144] |
| Alcea rosea L./RRLH22615 | Gulkher | S | Inf/Fl | Paste | RES | 3 | 2.94 | 26.14 | E | Fahamiya et al. [145] |
| Eriolaena candollei Wall./RRLH24871 | Mushkbala | H | Lv | Paste | GAS | 2 | 0.98 | 30.68 | E | Kamble et al. [146] |
| Malva cashemiriana (Cambess.) Alef./RRLH24783 | Sazeposh | S | Fl | Paste | DER | 3 | 2.94 | 35.23 | E | Riyaz et al. [90] |
| Malva sylvestris L./RRLH21484 | Sochal | H | Se | Powder | ENT | 3 | 2.94 | 61.36 | N | Hakeem [147] |
| Melanthiaceae | ||||||||||
| Trillium govanianum Wall. ex D.Don/RRLH25024 | Trepater/Surm gunda | H | Rt | Powder | CAN | 21 | 20.59 | 35.23 | N | Rathore et al. [148] |
| Moraceae | ||||||||||
| Ficus carica L./RRLH24864 | Anjeer | T | Lv/Sh/Lt | Juice/extract | GYN: 9 RES: 7 | 16 | 15.69 | 56.82 | E | Bouyahya et al. [149] |
| Morus alba L./RRLH24821 | Tul | T | Fr/Lv | Chew | GAS | 13 | 12.75 | 48.86 | E | Rodrigues et al. [150] |
| Papaveraceae | ||||||||||
| Corydalis govaniana Wall./RRLH24797 | Bhukesi | H | Wp | Powder | CAN | 13 | 12.75 | 35.23 | N | Sivakumaran et al. [151] |
| Papaver somniferum L./RRLH20326 | Khash Khash | H | Sh | Juice/extract | NER | 12 | 11.76 | 44.32 | E | Masihuddin et al. [152] |
| Phytolaccaceae | ||||||||||
| Phytolacca acinosa Roxb./RRLH24792 | Hapat chur | S | Se | Juice/extract | NER | 10 | 9.80 | 35.23 | N | Kumar et al. [153] |
| Plantaginaceae | ||||||||||
| Picrorhiza kurroa Royle ex Benth./RRLH24867 | Kod | H | Rt | Powder | GAS: 16 SKE: 11 | 27 | 26.47 | 26.14 | N | Kafle et al. [154] |
| Plantago lanceolata L./RRLH24817 | Penkatch | H | Rt | Chew | CAR | 12 | 11.76 | 44.32 | N | Najafian et al. [155] |
| Wulfeniopsis amherstiana (Benth.) D.Y.Hong/RRLH24866 | Kakpae | H | Lv | Decoction | DER | 11 | 10.78 | 48.86 | N | Kakar et al. [156] |
| Polygonaceae | ||||||||||
| Persicaria hydropiper (L.) Delarbre/RRLH24790 | Marchawangan gss | H | Rt/Sh | Powder | IB: 6 GAS: 2 | 8 | 7.84 | 21.59 | E | Huq et al. [157] |
| Persicaria mitis (Schrank) Assenov/RRLH24818 | Chittahola | H | Rt/Sh | Powder | GAS | 4 | 3.92 | 21.59 | E | Cock and Van Vuuren [158] |
| Rheum australe D.Don/RRLH24779 | Pamb chalan | H | LV | Paste | CAR | 17 | 16.67 | 43.18 | N | Bhat et al. [52], Kanta et al. [53] |
| Rheum emodi D.Don/RRLH22121 | Mamekh | H | Wp | Juice/extract | MET | 10 | 9.80 | 26.14 | N | Pandith et al. [159] |
| Rumex acetosa L./RRLH24778 | Chitta ula | H | Lv/Rt | Decoction | RES: 18 EY: 17 | 35 | 34.31 | 44.32 | N | Bello et al. [160] |
| Portulacaceae | ||||||||||
| Portulaca oleracea L./RRLH24375 | Nunner | S | Wp | Juice/extract | CAN: 15 CAR: 8 SKE: 10 | 33 | 32.35 | 21.59 | N | Zhou et al. [161] |
| Lysimachia arvensis (L.) U.Manns & Anderb./RRLH28948 | Janglee aam | H | Fr | Powder | DER: 3 ENT: 9 RES: 3 | 15 | 14.71 | 47.73 | E | Al-Snafi [162] |
| Ranunculaceae | ||||||||||
| Aconitum chasmanthum Stapf ex Holmes/RRLH24795 | Mohund | H | Lv/Rt | Powder | GYN | 13 | 12.75 | 78.41 | N | Shyaula [159] |
| Aconitum heterophyllum Wall. ex Royle/RRLH24801 | Patrees | H | Rt | Powder | RES: 7 GYN: 11 | 18 | 17.65 | 47.73 | N | Shyaula [163] |
| Anemonastrum obtusilobum (D.Don) Mosyakin/RRLH24787 | Charisaban | H | Wp | Powder | CAR: 13 NER: 4 | 17 | 6.86 | 55.68 | N | Majid et al. [164] |
| Aquilegia vulgaris L./RRLH24862 | Kavashud | H | Rt/Inf | Chew | GYN: 2 DER: 9 | 11 | 10.78 | 48.86 | N | Malik et al. [165] |
| Ranunculus hirtellus Royle/RRLH21083 | Songul | H | Lv | Decoction | ETH: 3 RES: 9 | 12 | 11.76 | 53.41 | N | Not found |
| Rhamnaceae | ||||||||||
| Zizyphus mauritiama Lam./RRLH51077 | Brey kul | T | Fr | Decoction | CAR: 21 DER: 3 | 24 | 20.59 | 30.68 | E | Akassh et al. [166] |
| Rosaceae | ||||||||||
| Cormus domestica (L.) Spach/RRLH54217 | Chount | T | Fr | Juice/extract | RES | 15 | 14.71 | 48.86 | N | Not found |
| Cydonia oblonga Mill./RRLH21489 | Bumb chaent | T | Fr | Juice/extract | RES | 12 | 11.76 | 44.32 | E | Ashraf et al. [167] |
| Fragaria vesca L./RRLH24753 | Gonch | H | Fr | Chew | ENT: 13 GAS: 2 | 15 | 14.71 | 44.32 | N | Thakur et al. [168] |
| Geum elatum Wall. ex G.Don/RRLH24796 | Shonkar | H | Rt | Paste | RES | 4 | 3.92 | 48.86 | N | Chakraborty et al. [169] |
| Potentilla indica (Andrews) Teschem/RRLH21268 | Gonch | H | Rt | Powder | RES | 11 | 10.78 | 47.73 | N | Khuda et al. [170] |
| Rosa webbiana Wall. ex Royle/RRLH24780 | Janglee gulab | S | Fl | Paste | RES: 8 EY: 4 | 12 | 11.76 | 53.41 | N | Alamgeer et al. [171] |
| Rubiaceae | ||||||||||
| Galium aparine L./RRLH24824 | Lothar | H | Wp | Decoction | GAS | 9 | 8.82 | 26.14 | N | Amjad et al. [105] |
| Scrophulariaceae | ||||||||||
| Verbascum thapsus L./RRLH24755 | Hamesh bahar | H | Lv/Rt | Powder | RES | 8 | 7.84 | 35.23 | N | Ali et al. [137] |
| Salicaceae | ||||||||||
| Populus alba L./RRLH24745 | Phrass | T | Lv | Powder | RES | 7 | 6.86 | 73.86 | E | Rashid and Sharma [172] |
| Salix alba L./RRLH24763 | Yeer | T | Lv | Decoction | ETH: 2 RES: 6 SKE: 2 | 10 | 9.80 | 21.59 | E | Prashith-Kekuda et al. [173] |
| Sapindaceae | ||||||||||
| Aesculus indica Wall.ex Cambess./RRLH24812 | Haandoon | T | Fr | Chew/Roasted | DER: 4 GAS: 5 | 9 | 8.82 | 26.14 | E | Not found |
| Saxifragaceae | ||||||||||
| Bergenia ciliata (Haw.) Sternb./RRLH24775 | Zakhmihayat | H | Rt | Powder | ENT: 14 GAS: 11 FVR: 4 | 29 | 28.43 | 39.77 | N | Ahmad et al. [174] Bharate et al. [175] |
| Solanaceae | ||||||||||
| Atropa acuminata Royle ex Lindl./RRLH23347 | Brand | S | Wp | Juice/extract | GYN | 13 | 12.75 | 38.64 | N | Hussain et al. [176,177] |
| Datura stramonium L./RRLH24789 | Datura | S | Lv | Juice/extract | DER: 7 SKE: 9 | 16 | 15.69 | 44.32 | E | Soni et al. [178] |
| Hyoscyamus niger L./RRLH 24772 | Hapatagra | S | Fl | Juice/extract | NER | 21 | 20.59 | 30.68 | N | Nadaf et al. [84] |
| Solanum pseudocapsicum L./RRLH21501 | Sharbat | H | Fr | Decoction | CAN | 7 | 6.86 | 30.68 | E | Not found |
| Urticaceae | ||||||||||
| Urtica dioica L./RRLH24762 | Soi | H | Rt | Powder | SKE | 16 | 15.69 | 48.86 | N | Dhouibi et al. [179] |
| Violaceae | 0.00 | |||||||||
| Viola odorata L./RRLH24751 | Nun posh | H | Wp | Powder | RES: 5 FVR: 18 | 23 | 22.55 | 55.68 | N | Mahboubi and Taghizadeh Kashani [180] |
| Vitaceae | ||||||||||
| Vitis vinifera L./RRLH10183 | Dach | L | Fr/Lv | Juice/extract | RES | 11 | 10.78 | 39.77 | E | Arora et al. [181] |
| GYMNOSPERMS | ||||||||||
| Cupressaceae | ||||||||||
| Juniperus communis L./RRLH24379 | Yathur | T | Rt | Powder | GAS | 9 | 8.82 | 65.91 | N | Bais et al. [182] |
| Pinaceae | ||||||||||
| Cedrus deodara (Roxb. ex D.Don) G.Don/RRLH24750 | Deodar | T | B | Powder | DER: 16 NER: 11 | 27 | 26.47 | 47.73 | N | Medinipur and Bengal [183] |
| Pinus roxburghii Sarg./RRLH24860 | Chad | T | Rt | Powder | GAS: 4 EY: 11 | 15 | 14.71 | 44.32 | N | Kaushik et al. [184] |
| Family | Taxon | Total Use-Reports (URs) | Use Value (UV) | Family Use Value (FUV) |
|---|---|---|---|---|
| Liliaceae | Fritillaria cirrhosa D.Don, Notholirion thomsonianum (Royle) Stapf. | 47 | 0.47 | 0.24 |
| Poaceae | Avena fatua L., Cynodon dactylon (L.) Pers., Oryza sativa L., Sorghum halepense (L.) Pers. | 50 | 0.5 | 0.13 |
| Asteraceae | Arctium lappa L., Artemisia absinthium L., Artemisia brevifolia Wall. ex DC., Artemisia imponens Pamp., Cichorium intybus L., Dolomiaea macrocephala DC. ex Royle, Matricaria chamomilla L., Dolomiaea costus (Falc.) Kasana & A.K.Pandey, Taraxacum officinale F.W. Wigg. | 169 | 1.66 | 0.17 |
| Berberidaceae | Berberis aristata DC., Podophyllum hexandrum Royle | 44 | 0.44 | 0.22 |
| Boraginaceae | Arnebia benthamii (Wall. ex G.Don) I.M. Johnst., Hackelia uncinata (Royle ex Benth.) C.E.C. Fisch. | 26 | 0.26 | 0.13 |
| Brassicaceae | Capsella bursa-pastoris (L.) Medik., Cardamine impatiens L., Nasturtium officinale W.T. Aiton | 37 | 0.37 | 0.12 |
| Cannabaceae | Cannabis sativa L., Celtis australis L. | 18 | 0.18 | 0.09 |
| Caprifoliaceae | Dipsacus inermis Wall., Valeriana jatamansi Jones ex Roxb. | 49 | 0.48 | 0.24 |
| Fabaceae | Indigofera heterantha Wall. ex Brandis, Trifolium repens L., Trigonella foenum-graecum L. | 20 | 0.20 | 0.07 |
| Lamiaceae | Ajuga bracteosa Buch.- Ham. ex. D.Don, Lamium album L., Mentha piperita L., Nepeta cataria L., Prunella vulgaris L., Thymus linearis Benth. | 93 | 0.92 | 0.15 |
| Malvaceae | Abutilon indicum (L.) Sweet, Althaea rosea L., Eriolaena candollei Wall., Malva cashemiriana (Cambess.) Alef., Malva sylvestris L. | 15 | 0.15 | 0.03 |
| Moraceae | Ficus carica L., Morus alba L. | 29 | 0.29 | 0.15 |
| Papaveraceae | Corydalis govaniana Wall., Papaver somniferum L. | 25 | 0.25 | 0.13 |
| Plantaginaceae | Picrorhiza kurroa Royle ex Benth., Plantago lanceolata L., Wulfeniopsis amherstiana (Benth.) D.Y. Hong | 50 | 0.49 | 0.16 |
| Polygonaceae | Persicaria hydropiper (L.) Delarbre, Persicaria mitis (Schrank) Assenov, Rheum australe D.Don, Rheum emodi D.Don, Rumex acetosa L. | 74 | 0.73 | 0.15 |
| Portulacaceae | Portulaca oleracea L., Lysimachia arvensis (L.) U. Manns & Anderb. | 48 | 0.47 | 0.24 |
| Ranunculaceae | Aconitum chasmanthum Stapf ex Holmes, Aconitum heterophyllum Wall. ex Royle, Anemonastrum obtusilobum (D.Don) Mosyakin, Aquilegia vulgaris L., Ranunculus hirtellus Royle | 61 | 0.61 | 0.12 |
| Rosaceae | Cormus domestica (L.) Spach, Cydonia oblonga Mill., Fragaria vesca L., Geum elatum Wall. ex G.Don, Potentilla indica (Andrews) Teschem, Rosa webbiana Wall. ex Royle | 69 | 0.69 | 0.12 |
| Salicaceae | Populus alba L., Salix alba L. | 17 | 0.17 | 0.09 |
| Solanaceae | Atropa acuminata Royle ex Lindl., Datura stramonium L., Hyoscyamus niger L., Solanum pseudocapsicum L. | 57 | 0.57 | 0.14 |
| Pinaceae | Cedrus deodara (Roxb. ex D.Don) G.Don, Pinus roxburghii Sarg. | 42 | 0.41 | 0.21 |
| Disease Category | No. of Taxa (Nt) | Nt% | Use-Reports (Nur) | Nur% | ICF |
|---|---|---|---|---|---|
| GAS: Gastrointestinal problems (hepatotoxic, ulcer, choleretic, constipation/indigestion, dysentery, diarrhea, excess gas, heartburn, nausea, stomach pain, vomiting, kidney stone) | 28 | 26.17 | 262 | 16.19 | 0.90 |
| CAR: Cardiovascular problems (blood purifier, heart disorders, heart attacks, strokes) | 13 | 12.15 | 155 | 9.58 | 0.92 |
| DER: Dermatological disorders (abscess, eczema, acne, itching, ringworm, alopecia, blemishes, leukoderma, dandruff, boils, cuts, burns, scabies, wounds) | 19 | 17.76 | 203 | 12.55 | 0.91 |
| GYN: Gynecological problems (abortifacient, oxytocic, uterine hemorrhage, menstrual problem, genital tract problems, lactation in women) | 9 | 8.41 | 101 | 6.24 | 0.92 |
| NER: Nervous system disorders (anxiety, psychosis, major depressive, narcolepsy, neuropathic pain, vascular dementia) | 6 | 5.61 | 74 | 4.57 | 0.93 |
| PAR: Parasitic problems (antihelminthic) | 1 | 0.93 | 7 | 0.43 | 1.00 |
| CAN: Cancer (persistent cough, loss in weight, fatigue) | 10 | 9.35 | 132 | 8.16 | 0.93 |
| RES: Respiratory complaints (asthma, bronchitis, common cold, pneumonia, shortness of breathing, allergies, tuberculosis) | 29 | 27.10 | 243 | 15.02 | 0.88 |
| SKE: Skeleto-muscular system disorder (swelling, arthritis, rheumatic pain, neck pain, back pain, muscle pain, joint inflammation, bone fracture) | 21 | 19.63 | 175 | 10.82 | 0.89 |
| MET: Metabolic syndromes (obesity, diabetes, blood pressure, excessive body fat, abnormal cholesterol, jaundice) | 6 | 5.61 | 70 | 4.33 | 0.93 |
| ETH: Ethnoveterinary ailments (application in treatment of wounds, stomach problems, milk yielding problems, etc., in cows, goats, horses) | 7 | 6.54 | 40 | 2.47 | 0.85 |
| EY: Energy yielding (tonic, laxative) | 5 | 4.67 | 56 | 3.46 | 0.93 |
| ENT: Eyes, ears and nose inflammation problems (throat pain, toothache, sinus infection, bronchitis) | 6 | 5.61 | 53 | 3.28 | 0.90 |
| FVR: Fever (malaria, typhoid, high body temperature) | 6 | 5.61 | 54 | 3.34 | 0.91 |
| IB: Insect bites (bees, scorpion) | 1 | 0.93 | 6 | 0.37 | 1.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bhat, M.N.; Singh, B.; Surmal, O.; Singh, B.; Shivgotra, V.; Musarella, C.M. Ethnobotany of the Himalayas: Safeguarding Medical Practices and Traditional Uses of Kashmir Regions. Biology 2021, 10, 851. https://doi.org/10.3390/biology10090851
Bhat MN, Singh B, Surmal O, Singh B, Shivgotra V, Musarella CM. Ethnobotany of the Himalayas: Safeguarding Medical Practices and Traditional Uses of Kashmir Regions. Biology. 2021; 10(9):851. https://doi.org/10.3390/biology10090851
Chicago/Turabian StyleBhat, Mudasir Nazir, Bikarma Singh, Opender Surmal, Bishander Singh, Vijay Shivgotra, and Carmelo Maria Musarella. 2021. "Ethnobotany of the Himalayas: Safeguarding Medical Practices and Traditional Uses of Kashmir Regions" Biology 10, no. 9: 851. https://doi.org/10.3390/biology10090851
APA StyleBhat, M. N., Singh, B., Surmal, O., Singh, B., Shivgotra, V., & Musarella, C. M. (2021). Ethnobotany of the Himalayas: Safeguarding Medical Practices and Traditional Uses of Kashmir Regions. Biology, 10(9), 851. https://doi.org/10.3390/biology10090851







