Simple Summary
Zygomatic dental implants have been proposed as an alternative to atrophic total edentulous maxillae rehabilitation with the necessity of bone grafting procedures. However, surgical, prosthetic, and maxillary sinus complications have been associated with this surgical procedure. Therefore, it is necessary to produce a systematic review and meta-analysis that provides evidence associated with the prognosis when using zygomatic dental implants as an alternative to atrophic total edentulous maxillae rehabilitation.
Abstract
The aim of this systematic review and meta-analysis was to analyze and compare the survival rate and prosthetic and sinus complications of zygomatic dental implants for the rehabilitation of the atrophic edentulous maxilla. Materials and methods: We conducted a systematic literature review and meta-analysis, based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) recommendations, of clinical studies that evaluated the survival rate and prosthetic and sinus complications of zygomatic dental implants for the rehabilitation of the atrophic edentulous maxilla. Four databases were consulted during the literature search: Pubmed–Medline, Scopus, Embase, and Web of Science. After eliminating duplicate articles and applying the inclusion criteria, 46 articles were selected for the qualitative analysis and 32 for the quantitative analysis. Results: Four randomized controlled trials, 19 prospective clinical studies, 20 retrospective studies, and 3 case series were included in the meta-analysis. Conventional dental implants failure (n = 3549) were seen in 2.89% (IC-95% 1.83–3.96%), while zygomatic dental implants failure (n = 1895) were seen in 0.69% (IC-95% 0.21–1.16%). The measure of the effect size used was the Odds Ratio, which was estimated at 2.05 with a confidence interval of 95% between 1.22 and 3.44 (z test = 2.73; p-value = 0.006). The failure risk of conventional dental implants is 2.1 times higher than that of zygomatic dental implants. Slight heterogeneity was determined in the meta-analysis between 23 combined studies (Q test = 32.4; p-value = 0.070; I2 = 32.1%). Prosthetic complications were recorded in 4.9% (IC-95% 2.7–7.3%) and mild heterogeneity was observed in a meta-analysis of 28 combined studies (Q test = 88.2; p-value = 0.001; I2 = 69.4%). Sinus complications were seen in 4.7% (IC-95% 2.8–6.5%) and mild heterogeneity was observed in a meta-analysis of 32 combined studies (Q test = 75.3; p-value = 0.001; I2 = 58.8%). Conclusions: The high survival rate and low prosthetic and sinus complications related to zygomatic dental implants suggest the use of zygomatic dental implants for the rehabilitation of the atrophic edentulous maxilla.
1. Introduction
The rehabilitation of extremely atrophic, fully edentulous maxillae is a concern and constitutes a challenge for dental professionals due to the lack of bone availability, which influences the placement of conventional length dental implants [1]. Various therapeutic alternatives have been proposed to rehabilitate the atrophic maxilla by bone-augmentation procedures to increase the bone availability, allowing implant-supported rehabilitation, including grafting procedures, sinus lift, and apposition graft with or without Le Fort I osteotomy, with success rates of 60–90% [2,3,4]. However, most of these approaches require delayed approaches and two-stage procedures, including bone grafts that increase the risk of potential postoperative complications [5]. In addition, a higher implant failure rate has been associated with a lack of bone availability and/or low, inadequate bone density in edentulous patients with atrophic maxilla [6,7]. Moreover, bacterial infection has been correlated to the development of peri-implant disease; thus, it is important to analyze the bacterial biotypes and biomarkers associated with implant failure. Isola et al. reported significantly higher serum and salivary Galectin-3 levels in patients affected with periodontitis compared with healthy subjects. They also reported that periodontitis and Endothelin-1 were significant predictors of serum and salivary Galectin-3 levels, respectively [8]. Furthermore, Ghassib et al. conducted a systematic review and meta-analysis and reported that pro-inflammatory cytokines in peri-implant crevicular fluid, such as interleukin-1β and interleukin-6, can be used as adjunct tools to clinical parameters to differentiate healthy patients from peri-implant mucositis and peri-implantitis [9]. Therefore, zygomatic dental implants have been proposed as an alternative to atrophic fully edentulous maxillae rehabilitation with the necessity of bone-grafting procedures [10]. The zygomatic implants approach has been used in conjunction with conventional-length dental implants in patients with severe resorption of the maxilla, with a survival rate of 96–100% [11,12,13]. Unfortunately, postoperative complications have been reported in terms of the effect on the maxillary sinus, especially when placing intrasinusal zygomatic dental implants. A sinusitis incidence rate of 5–6% has been reported (range: 0–26.6%); however, antibiotic therapy has been shown to be broadly effective in all patients [14,15]. Prosthetic complications have also been reported in implant-supported restorations using zygomatic dental implants. Prosthetic complications have also been reported, related to adjustments of the retention elements of overdentures, the fracture of fixed dental prostheses, mucosal overgrowth, or hyperplasia and discomfort [16].
The aim of this systematic review and meta-analysis was to analyze and compare the survival rate and prosthetic and sinus complications of zygomatic dental implants for the rehabilitation of the atrophic edentulous maxilla, with a null hypothesis (H0) stating that there would be no difference between the survival rate and prosthetic and sinus complications of zygomatic dental implants and conventional-length dental implants for the rehabilitation of the atrophic edentulous maxilla.
2. Materials and Methods
2.1. Study Design
A bibliographic search was conducted following the PRISMA (Preferred Reporting Items for Systemic Reviews and Meta-Analyses http://www.prisma-statement.org, accessed on 17 June 2021) guidelines for systematic reviews and meta-analyses (PROSPERO registration number: CRD42021226821). The review also fulfilled the PRISMA 2009 Checklist [17].
2.2. Focused Question
The PICO (population, intervention, comparison, outcome) question was “What is the survival rate, and what are the prosthetic and sinus complications, of zygomatic dental implants for the rehabilitation of the atrophic edentulous maxilla?” with the following components: population: atrophic edentulous maxilla patients treated with zygomatic dental implants; intervention: rehabilitation of the atrophic edentulous maxilla through zygomatic dental implants; comparison: zygomatic dental implants and conventional dental implants; and outcomes: survival rate and prosthetic and sinus complications.
2.3. Databases and Search Strategy
An electronic search was conducted in the following databases and gray literature: PubMed; Scopus; Embase, Web of Sciences and OpenGrey (www.opengrey.eu, accessed on 17 June 2021) (A.Z.-M J.M.M.C). The search covered all the literature published internationally up to June 2020. The search included seven medical subject heading (MeSH) terms: “zygomatic implants”, “survival rate”, “prognosis”, “implant failure”, “prosthetic rehabilitation”, “complications”, “maxillary sinus”, and “sinusitis.” The Boolean operators applied were OR and The search terms were structured as follows: ((“zygomatic implants”) AND (“survival rate”) OR (“prognosis”) OR (“implant failure”) AND (“prosthetic rehabilitation”) AND (“complication”) AND (“maxillary sinus”) OR (“sinusitis”)). Two researchers (S.H.M. and A.Z.-M.) conducted the database searches in duplicate, independently. Titles and abstracts were selected by applying the inclusion and exclusion criteria.
2.4. Study Selection
Titles and abstracts were selected after applying inclusion and exclusion criteria by two authors (C.O.A. and J.R.G.R.).
Inclusion criteria: studies recorded in databases as prospective randomized clinical trials (RCTs), retrospective studies, and case series from five patients. The review was not restricted to RCTs because of the paucity of studies with this experimental design and external validity, but also to provide a complete picture of the topic.
Samples of patients aged 18 years old or over; patients treated with zygomatic dental implants to rehabilitate atrophic edentulous maxilla; follow-up period of at least 3 months. No restriction was placed on the year of publication or language.
Exclusion criteria: systematic literature reviews, clinical cases, case series of up to five patients, and editorials; studies including patients under the age of 18; studies with samples of five or fewer patients. The following data were extracted from each article by two authors (C.O.A. and J.R.G.R.): author and year of publication; title and journal in which the article was published; sample size (n); follow-up time and success rate, periapical healing reduction, and bone density. Studies that analyzed implant failure rate and prosthetic and sinus complications were included in the systematic review and network meta-analysis.
2.5. Data Extraction and Study Outcomes
Data extraction was conducted in duplicate (by C.O.A. and J.R.G.R.) using predefined Excel spreadsheets and accounting for the following items: author and year, study type, sample size, follow-up in months, implant failures, prosthetic complications, and presence of sinusitis.
2.6. Methodological Quality Assessment
The risk of bias in the studies selected for review was assessed by two authors (M.P.D; D.P.O) using the Jadad scale for methodological quality assessment of clinical trials. The Jadad scale consists of five items that evaluate randomization, researcher and patient blinding, and description of losses during follow-up producing a score of 0–5; scores of less than three are considered to indicate low quality [18]. The level of agreement between evaluators was determined using Kappa scores.
2.7. Quantitative Synthesis—Meta-Analysis
The statistical data collection and analysis were conducted by two authors (A.Z.-M. and J.M.M.-C.). The studies included for the meta-analysis were combined using a random-effects model with various methods according to the estimated effect size. The inverse method of variance was used to estimate the root apex location success rate, the Mantel Haenszel method for the Odds Ratio (OR), and the inverse method of variance for the mean difference. For all the estimated variables, a 95% confidence interval was calculated. Heterogeneity between the combined studies was assessed using the Q test (p-value < 0.05) and quantified with the I2, with a slight heterogeneity if it is 25–50%, moderate at 50–75%, and high if >75%. Statistical significance was assessed using the Z test (p-value < 0.05). Meta-analyses were represented with a forest plot. Publication bias was assessed using the Trim and Fill adjustment method, represented with Funnel plots. The R software was employed for meta-evidence analysis.
3. Results
3.1. Flow Diagram
The initial electronic search identified 37 articles in PubMed, 40 in Web of Sciences, 31 in Embase, 21 in Scopus, and none in the gray literature. Of the 129 works, 32 were discarded as duplicates. After reading the titles and abstracts, a further 35 were eliminated, leaving a total of 62. A further 15 were rejected as they failed to fulfill the following inclusion criteria: they did not include survival rate data, did not include prosthetic or sinus complications data, or presented a minimum follow-up time of 3 months. A final total of 46 articles were included in the qualitative synthesis. Thirty-two articles were included in the quantitative synthesis, as these included all the data and variables required (Figure 1).
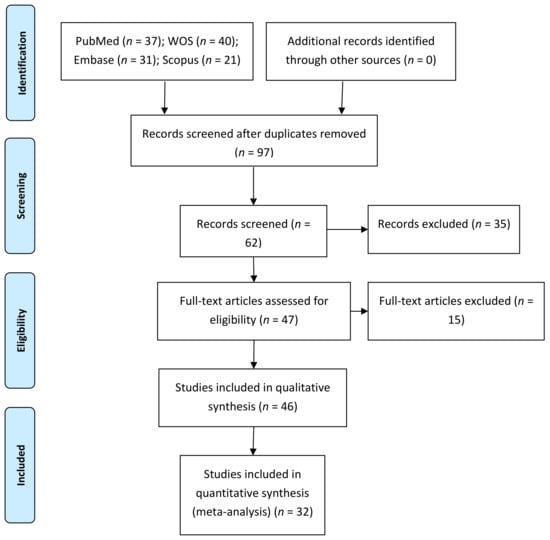
Figure 1.
Preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow diagram.
3.2. Qualitative Analysis
Of the 46 articles included, 4 were randomized clinical trials [19,20,21,22], 19 were nonrandomized clinical trials [10,11,14,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38], 20 were retrospective studies [7,8,13,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54], and 3 were case series [55,56,57]. In addition, 31 articles compared the success rate of conventional and zygomatic dental implants [7,8,9,11,13,17,19,21,22,23,24,25,26,27,28,29,32,33,34,36,38,41,42,43,44,46,48,53,54,55]. Fifteen articles described an intrasinusal placement of the zygomatic dental implants [1,7,13,20,21,24,27,29,32,33,40,42,47,54], six articles described an extrasinusal placement of the zygomatic dental implants [11,23,34,36,43,46], five articles described the sinus slot placement technique of the zygomatic dental implants [45,48,50,52,55], three articles described intra and extrasinusal placement of the zygomatic dental implants [26,35,39], one article described the sinus slot technique and intrasinusal placement of the zygomatic dental implants [9], and two articles did not describe the placement technique of the zygomatic dental implants [8,37]. Twenty-eight articles analyzed the prosthetic complications [7,8,10,11,14,17,18,19,21,22,23,24,25,26,31,34,36,38,41,42,43,44,46,48,49,50,54] and thirty-two articles described the sinus complications [7,11,13,20,21,23,24,25,26,27,29,32,33,34,35,36,37,38,39,40,41,42,43,45,46,47,48,50,52,54,55]. Most of the studies presented a follow-up time of approximately 36 months, ranging from 3 months in the study by Fernández et al., 2015 [20], to 163 months in Agbara’s study from 2017 [37]. The results are presented in Table 1.

Table 1.
Qualitative analysis of articles included in the systematic review.
3.3. Quality Assessment
The results of the methodological quality assessment using the Jadad scale were performed by one author (A.Z.-M.) and are shown in Table 2. The Jadad scale returned 23 articles as “not applicable”, because 20 were retrospective [7,8,13,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52] and 3 were case series [53,54,55], and the authors of these articles did not blind or randomize the studies. Two articles [17,20] obtained scores of five, indicating high methodological quality. Again, quality was most frequently compromised by a failure to fulfill items related to the subject, treatment, or measurement blinding.

Table 2.
Assessment of methodological quality according to the Jadad scale.
3.4. Quantitative Analysis
3.4.1. Failure Rate of Zygomatic and Conventional Dental Implants
The incidence of implant failure of conventional dental implants (n = 3549) has been estimated at 2.89% (CI-95% 1.83–3.96%), while the incidence of implant failure of zygomatic dental implants (n = 1895) has been estimated at 0.69% (CI-95% 0.21–1.16%). The follow-up time of the studies selected was 3–163 months.
Thirty-one studies [7,8,9,11,13,17,19,21,22,23,24,25,26,27,28,29,32,33,34,36,38,41,42,43,44,46,48,53,54,55] that compared the incidence of dental implant failure between conventional and zygomatic dental implants were included in the meta-analysis and combined using a random effects model with the Mantel–Haenszel method. The effect size measure used was the Odds Ratio, which was estimated at 1.33 with a 95% confidence interval between 0.79 and 2.23 (z-test = 1.09; p-value = 0.278). The risk of implant failure is 1.3 times greater with conventional than with zygomatic dental implants. Meta-analysis has shown a slight heterogeneity between the combined studies (Q test = 44.48 p-value = 0.039; I2 = 33.1%) (Figure 2).
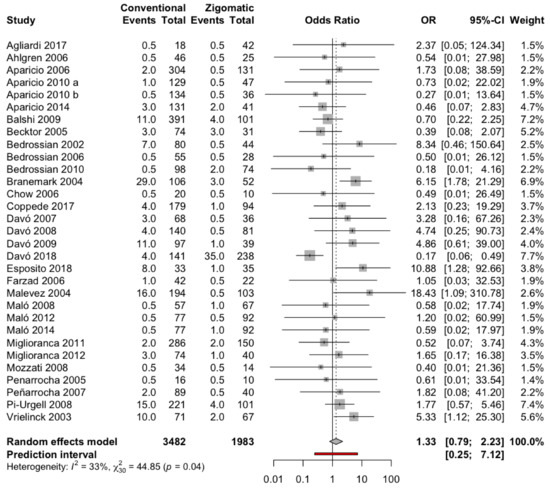
Figure 2.
Forest plot of the OR meta-analysis of implant failure: conventional dental implant group versus zygomatic dental implant group.
3.4.2. Incidence of Prosthetic Complications in Patients with Zygomatic Implants
Twenty-eight studies [7,8,10,11,14,17,18,19,21,22,23,24,25,26,31,34,36,38,41,42,43,44,46,48,49,50,54] with a total of 921 patients were combined using a random effects model (inverse variance method), estimating an incidence of prosthetic complications of 4.9% with a 95% confidence interval between 2.7% and 7.3% of patients with zygomatic implants. The meta-analysis detected moderate heterogeneity between the combined studies (Q-test = 88.2; p-value = 0.0001; I2 = 69.4%) (Figure 3).
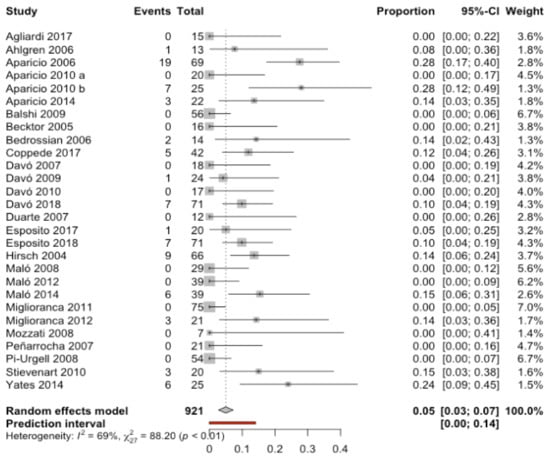
Figure 3.
Forest plot of the incidence of prosthetic complications in patients with zygomatic implants.
3.4.3. Incidence of Sinusitis in Patients with Zygomatic Implants
Thirty-two studies [7,11,13,20,21,23,24,25,26,27,29,32,33,34,35,36,37,38,39,40,41,42,43,45,46,47,48,50,52,54,55] with a total of 1119 patients, combined using a random effects model (inverse variance method), obtained an estimate of the incidence of sinusitis of 4.7% with a 95% confidence interval between 2.8% and 6.5% of patients with zygomatic implants. The meta-analysis detected moderate heterogeneity between the combined studies (Q test = 75.3; p-value < 0.0001; I2 = 58.8%) (Figure 4).
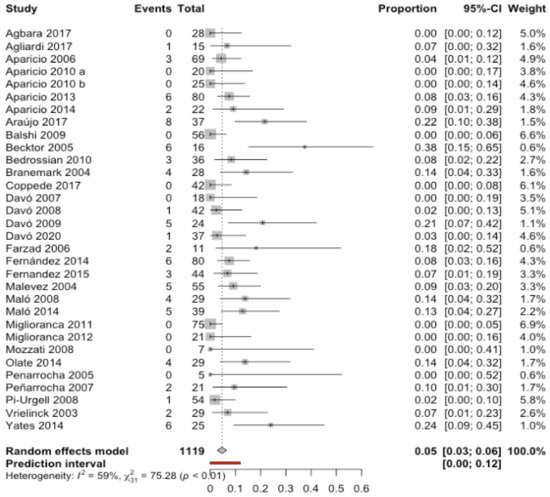
Figure 4.
Forest plot of the cumulative incidence of sinus complications in patients with zygomatic implants.
The cumulative incidence of sinus complications in patients with zygomatic implants placed using an intrasinusal technique was 7.2% (CI-95% 4.6–9.8%), significantly higher (Q test between groups = 8.85; p-value = 0.0029) than with the extrasinusal technique, which showed a cumulative incidence of 1.8% (CI-95% 0.0–4.2%) (Figure 5).
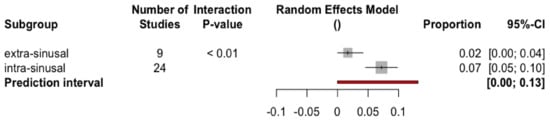
Figure 5.
Forest plot of the cumulative incidence of sinus complications in patients with zygomatic implants by subgroup.
3.5. Publication Bias
No study has been added to the 32 studies initially combined, using the Trim and Fill method to obtain symmetry in the funnel plot. The Odds Ratio estimation of dental implant failure, adjusted by the Mantel–Haenszel random-effects model, was 1.33 (95% CI between 0.79 and 2.23), showing no difference from the initial Odds Ratio estimation. Figure 6 shows the two funnel plots (initial and adjusted). These data indicate the absence of publication bias.
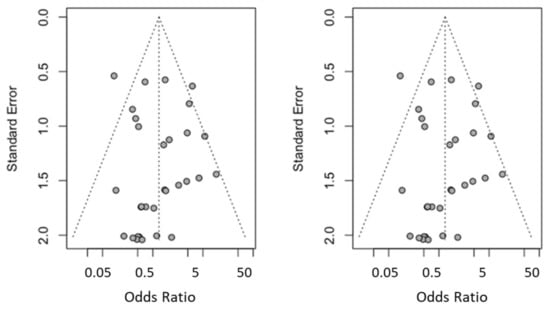
Figure 6.
Initial funnel plot and after trim and fill adjustment.
4. Discussion
The results obtained in the present study led us to reject the null hypothesis (H0), stating that there would be no difference between the survival rate and prosthetic and sinus complications of zygomatic dental implants for the rehabilitation of the atrophic edentulous maxilla.
The study showed that zygomatic dental implants had a lower failure rate than conventional-length dental implants. In addition, the prosthetic rehabilitations of zygomatic dental implants showed low prevalence values. Finally, the maxillary sinus complications of the atrophic edentulous maxilla rehabilitated by zygomatic dental implants also showed low prevalence values.
The meta-analysis showed a predictable outcome for the zygomatic dental implants, with a failure rate of 0.69% (CI-95% 0.21–1.16%) at 4–120 months follow-up. Some studies have reported the influence of the dental implant length on the long-term outcome of dental implants; therefore, the survival rate of zygomatic dental implants is higher than that of conventional-length dental implants (2.89% (CI-95% 1.83–3.96%)). A higher length of zygomatic dental implants creates a larger osseointegration surface that promotes the integration and stability of the zygomatic dental implants and improves the distribution of occlusal loads, since the length of zygomatic dental implants ranges from 30 mm to 52.5 mm [24] and conventional-length dental implants’ length ranges from 10 mm to 15 mm [38,42]. Some authors have reported the combined use of zygomatic dental implants in the atrophic edentulous posterior maxilla and conventional length dental implants in the anterior area [17,18,20,21,22,24,27,29,32,35,37,38,43,45,48,50]. Bedrossian et al. (2010) proposed treatment guidelines based on the bone availability and recommended placing four conventional-length dental implants in zones I and II; conventional-length dental implants in zones I, II, and III; combined conventional-length dental implants and zygomatic dental implants in zone I only; and four zygomatic dental implants in cases of insufficient bone availability [27]. The location of conventional-length dental implants and their shorter length simplify the explantation procedure and the posterior bone regeneration technique if necessary. Additionally, bacterial contamination has been highlighted as a relevant factor related to periodontal disease and implant failure; therefore, advances in microbial molecular diagnostics have allowed for better identification and thus a greater understanding of the causative agents and related biomarkers involved in both diseases [8,9]. In addition, Bedrossian et al. described the ideal number and location of zygomatic dental implants and conventional-length dental implants for atrophic edentulous maxilla rehabilitation by placing a minimum of two premaxillary conventional-length dental implants in the canine position, or ideally four premaxillary conventional-length dental implants in the canine and the central incisor positions and two zygomatic dental implants introduced into the second premolar area [30].
Zygomatic dental implants’ placement is still a challenge that poses risks because the lack of bone availability in the atrophic edentulous maxilla requires longer implants to attach to distant anatomical structures and can lead to clinical complications [35]. Therefore, both static and dynamic navigation systems have been widely used in dental implants [58,59,60,61,62,63,64,65,66,67]. Computer-aided static navigation systems have shown a mean horizontal deviation at the coronal entry point and apical endpoint of 1.2 mm (1.04–1.44 mm) and 1.4 mm (1.28–1.58 mm), respectively, and a mean angular deviation of 3.5° (3.0–3.96°). However, computer-aided dynamic navigation systems have demonstrated lower deviation values at the coronal entry point (0.71 ± 0.40 mm), apical endpoint (1.00 ± 0.49 mm), and angular deviation (2.26 ± 1.62°). Therefore, these results have encouraged us to apply computer-aided navigation techniques to zygomatic dental implants in order to improve the accuracy of zygomatic dental implants and prevent intraoperative complications [33,36].
Prosthetic rehabilitations of the zygomatic dental implants have demonstrated a low prosthetic complication incidence (4.9% (CI-95% 2.7–7.3%)), regardless of the prosthetic treatment. Many prosthetic treatments have been proposed to rehabilitate zygomatic dental implants, but problems have been reported, such as allergy to the gold alloy of the overdenture bar [22], losing the zygomatic implant gold screw, fracture of the gold screw [24], fracture of the metal–porcelain prostheses, fracture of the abutment screw [26], fracture of the framework, losing the gold zygomatic dental implant screws, fracture of the gold screws, losing the abutment screw, fracture of ceramic prosthetic teeth, fracture of the resin prostheses, disconnected abutments [1], partial fractures in the denture around the zygomatic implant cylinder [8], fractures or detachments of one or more acrylic teeth, fracture of provisional prosthesis [36], and fracture of the metal bar [34].
Most authors reported an absence of sinus pathology related to zygomatic dental implants; however, some of them were placed in an extrasinusal location. The authors also reported that the sinusitis observed after the placement of zygomatic dental implants was resolved favorably after the administration of antiseptics (chlorhexidine 0.2%), antibiotics (amoxicillin and clavulanic acid 1000 mg), and corticosteroids. The results obtained in this meta-analysis showed a low sinus complication incidence (4.7% (CI-95% 2.8–6.5%)) regarding the relationship between the zygomatic dental implants and the maxillary sinus.
The results of the present work can be extrapolated to those patients with atrophied maxilla requiring full-arch rehabilitation by means of zygomatic implants. There is a need for a larger body of evidence with more randomized studies, until today scarce in the literature. Thus, more studies are warranted; of special interest are those implementing new technologies (e.g., CAD-CAM, intraoral scanners, guided surgery) or concomitant regenerative procedures.
In addition, the studies selected in the present systematic review and meta-analysis showed low methodological quality; therefore, the authors highlight the necessity of improving the methodological design for future studies. Moreover, the present review has endeavored to summarize the best available evidence, but not always the least biased. The majority of the articles showed a risk of bias, which is inherent to the observational design. Additionally, blinding methods were frequently not applied, which increased the risk of bias. Despite the abovementioned drawbacks, the inconsistency of the results proves to be low to moderate, with I2 values < 75%. Moreover, the hints of meta-bias were properly inspected using funnel plots and showed a symmetrical distribution. All this, together with the comprehensive electronic searches and prospective protocol registration, increases our confidence in the review findings.
5. Conclusions
Meta-evidence suggests that zygomatic implants have higher survival rates than conventional implants in patients with severely atrophied maxilla; however, zygomatic implants are not recommended as a first treatment option. The incidence of prosthetic complications and sinusitis is low. The impact of covariates such as surgical technique on biological complications requires further study.
Author Contributions
Conceptualization, D.G.M., C.O.A. and Á.Z.-M.; design, H.G.M.; data acquisition, J.L.C.; formal analysis, D.P.-O.; statistical analyses, Á.Z.-M. and J.M.M.-C.; review and editing, S.H.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are available on request due to restrictions, e.g., privacy or ethical.
Acknowledgments
The authors would like to express their thanks to Carmen Caballero for his advice, guidance, and help during this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Aparicio, C.; Manresa, C.; Francisco, K.; Ouazzani, W.; Claros, P.; Potau, J.M.; Aparicio, A. The long-term use of zygomatic implants: A 10-year clinical and radiographic report. Clin. Implant Dent. Relat. Res. 2014, 16, 447–459. [Google Scholar] [CrossRef] [PubMed]
- Nystrom, L.; Ahlqvist, J.; Legrell, P.E.; Kahnberg, K. Bone graft remodelling and implant success rate in the treatment of the severely resorbed maxilla: A 5-year longitudinal study. Int. J. Oral Maxillofac. Surg. 2002, 31, 158–164. [Google Scholar] [CrossRef]
- Nyström, E.; Nilson, H.; Gunne, J.; Lundgren, S. Reconstruction of the atrophic maxilla with interpositional bone grafting/Le Fort I osteotomy and endosteal implants: A 11–16 year follow-up. Int. J. Oral Maxillofac. Surg. 2009, 38, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Jensen, J.; Sindet-Pedersen, S.; Oliver, A.J. Varying treatment strategies for reconstruction of maxillary atrophy with implants: Results in 98 patients. J. Oral Maxillofac. Surg. 1994, 52, 210–218. [Google Scholar] [CrossRef]
- Kahnberg, K.E.; Nilsson, P.; Rasmusson, L. Le Fort I osteotomy with interpositional bone grafts and implants for rehabilitation of the severely resorbed maxilla: A 2-stage procedure. Int. J. Oral Maxillofac. Implants 1999, 14, 571–578. [Google Scholar]
- Jemt, T.; Lekholm, U. Implant treatment in edentulous maxillae: A 5-year follow-up report on patients with different degrees of jaw resorption. Int. J. Oral Maxillofac. Implants 1995, 10, 303–311. [Google Scholar]
- Becktor, J.P.; Isaksson, S.; Abrahamsson, P.; Sennerby, L. Evaluation of 31 zygomatic implants and 74 regular dental implants used in 16 patients for prosthetic reconstruction of the atrophic maxilla with cross-arch fixed bridges. Clin. Implant Dent. Relat. Res. 2005, 7, 159–165. [Google Scholar] [CrossRef] [Green Version]
- Isola, G.; Polizzi, A.; Alibrandi, A.; Williams, R.C.; Lo Giudice, A. Analysis of galectin-3 levels as a source of coronary heart disease risk during periodontitis. J. Periodontal Res. 2021, 56, 597–605. [Google Scholar] [CrossRef]
- Ghassib, I.; Chen, Z.; Zhu, J.; Wang, H.L. Use of IL-1 β, IL-6, TNF-α, and MMP-8 biomarkers to distinguish peri-implant diseases: A systematic review and meta-analysis. Clin. Implant Dent. Relat. Res. 2019, 21, 190–207. [Google Scholar] [CrossRef]
- Bedrossian, E.; Rangert, B.; Stumpel, L.; Indresano, T. Immediate function with the zygomatic implant: A graftless solution for the patient with mild to advanced atrophy of the maxilla. Int. J. Oral Maxillofac. Implants 2006, 21, 937–942. [Google Scholar]
- Davó, R.; Malevez, C.; Rojas, J.; Rodríguez, J.; Regolf, J. Clinical outcome of 42 patients treated with 81 immediately loaded zygomatic implants: A 12-to-42 month retrospective study. Eur. J. Oral Implantol. 2008, 1, 141–150. [Google Scholar]
- Duarte, L.; Filho, H.; Francischone, C.; Peredo, L.; Branemark, P. The establishment of a protocol for the total rehabilitation of atrophic maxillae employing four zygomatic fixtures in an immediate loading system: A 30-month clinical and radiographic follow-up. Clin. Implant Dent. Relat. Res. 2007, 9, 186–196. [Google Scholar] [CrossRef]
- Maló, P.; de Araujo, M.; Lopes, I. A new approach to rehabilitate the severely atrophic maxilla using extramaxillary anchored implants in immediate function: A pilot study. J. Prosthet. Dent. 2008, 100, 354–366. [Google Scholar] [CrossRef]
- Aparicio, C.; Ouazzani, W.; Hatano, N. The use of zygomatic implants for prosthetic rehabilitation of the severely resorbed maxilla. Periodontology 2000 2008, 47, 162–171. [Google Scholar] [CrossRef]
- Malevez, C.; Abarca, M.; Durdu, F.; Daelemans, P. Clinical outcome of 103 consecutive zygomatic implants: A 6–48 months follow-up study. Clin. Oral Implants Res. 2004, 15, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Davo, R.; Pons, O.; Rojas, J.; Carpio, E. Immediate function of four zygomatic implants: A 1-year report of a prospective study. Eur. J. Oral Implantol. 2010, 3, 323–334. [Google Scholar] [PubMed]
- Liberati, A.; Banzi, R.; Moja, L. Measuring the impact of evidence: The Cochrane systematic review of organized stroke care. Intern. Emerg. Med. 2009, 4, 507–510. [Google Scholar]
- Jadad, A.R.; Moore, R.A.; Carroll, D.; Jenkinson, C.; Reynolds, D.J.M.; Gavaghan, D.J.; McQuay, H.J. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control. Clin. Trials 1996, 17, 1–12. [Google Scholar] [CrossRef]
- Davó, R.; Felice, P.; Pistilli, R.; Barausse, C.; Marti-Pages, C.; Ferrer-Fuertes, A.; Ippolito, D.R.; Esposito, M. Immediately loaded zygomatic implants vs conventional dental implants in augmented atrophic maxillae: 1-year post-loading results from a multicentre randomised controlled trial. Eur. J. Oral Implantol. 2018, 11, 145–161. [Google Scholar]
- Esposito, M.; Barausse, C.; Balercia, A.; Pistilli, R.; Ippolito, D.R.; Felice, P. Conventional drills vs. piezoelectric surgery preparation for placement of four immediately loaded zygomatic oncology implants in edentulous maxillae: Results from 1-year split-mouth randomised controlled trial. Eur. J. Oral Implantol. 2017, 10, 147–158. [Google Scholar]
- Esposito, M.; Davó, R.; Marti-Pages, C.; Ferrer-Fuertes, A.; Barausse, C.; Pistilli, R.; Ippolito, D.R.; Felice, P. Immediately loaded zygomatic implants vs conventional dental implants in augmented atrophic maxillae: 4 months post-loading results from a multicentre randomised controlled trial. Eur. J. Oral Implantol. 2018, 11, 11–28. [Google Scholar]
- Fernández Olarte, H.; Gómez-Delgado, A.; Trujillo-Saldarriaga, S.; Castro-Núñez, J. Inferior Meatal Antrostomy as a Prophylactic Maneuver to Prevent Sinusitis After Zygomatic Implant Placement Using the Intrasinusal Technique. Int. J. Oral Maxillofac. Implants 2015, 30, 862–867. [Google Scholar] [CrossRef] [Green Version]
- Agliardi, E.L.; Romeo, D.; Panigatti, S.; de Araújo Nobre, M.; Maló, P. Immediate full-arch rehabilitation of the severely atrophic maxilla supported by zygomatic implants: A prospective clinical study with minimum follow-up of 6 years. Int. J. Oral Maxillofac. Surg. 2017, 46, 1592–1599. [Google Scholar] [CrossRef]
- Ahlgren, F.; Størksen, K.; Tornes, K. A study of 25 zygomatic dental implants with 11 to 49 months’ follow-up after loading. Int. J. Oral Maxillofac. Implants 2006, 21, 421–425. [Google Scholar]
- Aparicio, C.; Ouazzani, W.; Aparicio, A.; Fortes, V.; Muela, R.; Pascual, A.; Codesal, M.; Barluenga, N.; Manresa, C.; Franch, M. Extrasinus zygomatic implants: Three year experience from a new surgical approach for patients with pronounced buccal concavities in the edentulous maxilla. Clin. Implant Dent. Relat. Res. 2010, 12, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Aparicio, C.; Ouazzani, W.; Garcia, R.; Arevalo, X.; Muela, R.; Fortes, V. A prospective clinical study on titanium implants in the zygomatic arch for prosthetic rehabilitation of the atrophic edentulous maxilla with a follow-up of 6 months to 5 years. Clin. Implant Dent. Relat. Res. 2006, 8, 114–122. [Google Scholar] [CrossRef]
- Aparicio, C.; Manresa, C.; Francisco, K.; Claros, P.; Alández, J.; González-Martín, O.; Albrektsson, T. Zygomatic implants: Indications, techniques and outcomes, and the zygomatic success code. Periodontology 2000 2014, 66, 41–58. [Google Scholar] [CrossRef] [PubMed]
- Aparicio, C.; Ouazzani, W.; Aparicio, A.; Fortes, V.; Muela, R.; Pascual, A.; Codesal, M.; Barluenga, N.; Franch, M. Immediate/Early loading of zygomatic implants: Clinical experiences after 2 to 5 years of follow-up. Clin. Implant Dent. Relat. Res. 2010, 12, e77–e82. [Google Scholar] [CrossRef] [PubMed]
- Bedrossian, E. Rehabilitation of the edentulous maxilla with the zygoma concept: A 7-year prospective study. Int. J. Oral Maxillofac. Implants 2010, 25, 1213–1221. [Google Scholar]
- Bedrossian, E.; Stumpel, L., 3rd; Beckely, M.L.; Indresano, T. The zygomatic implant: Preliminary data on treatment of severely resorbed maxillae. A clinical report. Int. J. Oral Maxillofac. Implants 2002, 17, 861–865, Erratum in 2003, 18, 292. [Google Scholar]
- Brånemark, P.I.; Gröndahl, K.; Öhrnell, L.O.; Nilsson, P.; Petruson, B.; Svensson, B.; Engstrand, P.; Nannmark, U. Zygoma fixture in the management of advanced atrophy of the maxilla: Technique and long-term results. Scand. J. Plast. Reconstr. Surg. Hand Surg. 2004, 38, 70–85. [Google Scholar] [CrossRef]
- Boyes-Varley, J.G.; Howes, D.G.; Lownie, J.F.; Blackbeard, G.A. Surgical modifications to the Brånemark zygomaticus protocol in the treatment of the severely resorbed maxilla: A clinical report. Int. J. Oral Maxillofac. Implants 2003, 18, 232–237. [Google Scholar]
- Hirsch, J.-M.; Öhrnell, L.-O.; Henry, P.J.; Andreasson, L.; Brånemark, P.-I.; Chiapasco, M.; Gynther, G.; Finne, K.; Higuchi, K.W.; Isaksson, S.; et al. A clinical evaluation of the Zygoma fixture: One year of follow-up at 16 clinics. J. Oral Maxillofac. Surg. 2004, 62, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Farzad, P.; Andersson, L.; Gunnarsson, S.; Johansson, B. Rehabilitation of severely resorbed maxillae with zygomatic implants: An evaluation of implant stability, tissue conditions, and patients’ opinion before and after treatment. Int. J. Oral Maxillofac. Implants 2006, 21, 399–404. [Google Scholar]
- Vrielinck, L.; Politis, C.; Schepers, S.; Pauwels, M.; Naert, I. Image-based planning and clinical validation of zygoma and pterygoid implant placement in patients with severe bone atrophy using customized drill guides. Preliminary results from a prospective clinical follow-up study. Int. J. Oral Maxillofac. Surg. 2003, 32, 7–14. [Google Scholar] [CrossRef]
- Migliorança, R.M.; Sotto-Maior, B.S.; Senna, P.M.; Francischone, C.E.; Del Bel Cury, A.A. Immediate occlusal loading of extrasinus zygomatic implants: A prospective cohort study with a follow-up period of 8 years. Int. J. Oral Maxillofac. Surg. 2012, 41, 1072–1076. [Google Scholar] [CrossRef]
- Aparicio, C.; Manresa, C.; Francisco, K.; Aparicio, A.; Nunes, J.; Claros, P.; Potau, J.M. Zygomatic implants placed using the zygomatic anatomy-guided approach versus the classical technique: A proposed system to report rhinosinusitis diagnosis. Clin. Implant Dent. Relat. Res. 2014, 16, 627–642. [Google Scholar] [CrossRef] [PubMed]
- Coppedê, A.; de Mayo, T.; de Sá Zamperlini, M.; Amorin, R.; de Pádua, A.P.A.T.; Shibli, J.A. Three-year clinical prospective follow-up of extrasinus zygomatic implants for the rehabilitation of the atrophic maxilla. Clin. Implant Dent. Relat. Res. 2017, 19, 926–934. [Google Scholar] [CrossRef]
- Agbara, R.; Goetze, E.; Koch, F.; Wagner, W. Zygoma implants in oral rehabilitation: A review of 28 cases. Dent. Res. J. 2017, 14, 370–375. [Google Scholar] [CrossRef] [PubMed]
- Balshi, S.F.; Wolfinger, G.J.; Balshi, T.J. A retrospective analysis of 110 zygomatic implants in a single-stage immediate loading protocol. Int. J. Oral Maxillofac. Implants 2009, 24, 335–341. [Google Scholar]
- Davó, R.; Bankauskas, S.; Laurincikas, R.; Koçyigit, I.D.; de Val, J.E.M.S. Clinical Performance of Zygomatic Implants—Retrospective Multicenter Study. J. Clin. Med. 2020, 9, 480. [Google Scholar] [CrossRef] [Green Version]
- Davo, R.; Malevez, C.; Rojas, J. Immediate function in the atrophic maxilla using zygoma implants: A preliminary study. J. Prosthet. Dent. 2007, 97, S44–S51. [Google Scholar] [CrossRef]
- Davó, R. Zygomatic implants placed with a two-stage procedure: A 5-year retrospective study. Eur. J. Oral Implantol. 2009, 2, 115–124. [Google Scholar] [PubMed]
- Pi Urgell, J.; Revilla Gutiérrez, V.; Gay Escoda, C.G. Rehabilitation of atrophic maxilla: A review of 101 zygomatic implants. Med. Oral Patol. Oral Cir. Bucal 2008, 13, E363–E370. [Google Scholar] [PubMed]
- Maló, P.; Nobre Mde, A.; Lopes, A.; Ferro, A.; Moss, S. Five-year outcome of a retrospective cohort study on the rehabilitation of completely edentulous atrophic maxillae with immediately loaded zygomatic implants placed extra-maxillary. Eur. J. Oral Implantol. 2014, 7, 267–281. [Google Scholar]
- Maló, P.; Nobre, M.D.; Lopes, A.; Francischone, C.; Rigolizzo, M. Three-year outcome of a retrospective cohort study on the rehabilitation of completely edentulous atrophic maxillae with immediately loaded extra-maxillary zygomatic implants. Eur. J. Oral Implantol. 2012, 5, 37–46. [Google Scholar] [PubMed]
- Rodríguez-Chessa, J.G.; Olate, S.; Netto, H.D.; Shibli, J.; de Moraes, M.; Mazzonetto, R. Treatment of atrophic maxilla with zygomatic implants in 29 consecutives patients. Int. J. Clin. Exp. Med. 2014, 7, 426–430. [Google Scholar] [PubMed]
- Migliorança, R.M.; Coppedê, A.; Dias Rezende, R.C.; de Mayo, T. Restoration of the edentulous maxilla using extrasinus zygomatic implants combined with anterior conventional implants: A retrospective study. Int. J. Oral Maxillofac. Implants 2011, 26, 665–672. [Google Scholar]
- Fernández, H.; Gómez-Delgado, A.; Trujillo-Saldarriaga, S.; Varón-Cardona, D.; Castro-Núñez, J. Zygomatic implants for the management of the severely atrophied maxilla: A retrospective analysis of 244 implants. J. Oral Maxillofac. Surg. 2014, 72, 887–891. [Google Scholar] [CrossRef]
- Peñarrocha, M.; García, B.; Martí, E.; Boronat, A. Rehabilitation of severely atrophic maxillae with fixed implant-supported prostheses using zygomatic implants placed using the sinus slot technique: Clinical report on a series of 21 patients. Int. J. Oral Maxillofac. Implants 2007, 22, 645–650. [Google Scholar]
- Stiévenart, M.; Malevez, C. Rehabilitation of totally atrophied maxilla by means of four zygomatic implants and fixed prosthesis: A 6-40-month follow-up. Int. J. Oral Maxillofac. Surg. 2010, 39, 358–363. [Google Scholar] [CrossRef]
- Yates, J.; Brook, I.; Patel, R.; Wragg, P.; Atkins, S.; El-Awa, A.; Bakri, I.; Bolt, R. Treatment of the edentulous atrophic maxilla using zygomatic implants: Evaluation of survival rates over 5–10 years. Int. J. Oral Maxillofac. Surg. 2014, 43, 237–242. [Google Scholar] [CrossRef] [PubMed]
- Peñarrocha-Diago, M.; Bernabeu-Mira, J.C.; Fernández-Ruíz, A.; Aparicio, C.; Peñarrocha-Oltra, D. Bone Regeneration and Soft Tissue Enhancement Around Zygomatic Implants: Retrospective Case Series. Materials 2020, 13, 1577. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Araújo, R.T.; Sverzut, A.T.; Trivellato, A.E.; Sverzut, C.E. Retrospective Analysis of 129 Consecutive Zygomatic Implants Used to Rehabilitate Severely Resorbed Maxillae in a Two-Stage Protocol. Int. J. Oral Maxillofac. Implants 2017, 32, 377–384. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chow, J.; Hui, E.; Lee, P.K.; Li, W. Zygomatic implants—Protocol for immediate occlusal loading: A preliminary report. J. Oral Maxillofac. Surg. 2006, 64, 804–811. [Google Scholar] [CrossRef]
- Mozzati, M.; Monfrin, S.B.; Pedretti, G.; Schierano, G.; Bassi, F. Immediate loading of maxillary fixed prostheses retained by zygomatic and conventional implants: 24-month preliminary data for a series of clinical case reports. Int. J. Oral Maxillofac. Implants 2008, 23, 308–314. [Google Scholar]
- Peñarrocha, M.; Uribe, R.; García, B.; Martí, E. Zygomatic implants using the sinus slot technique: Clinical report of a patient series. Int. J. Oral Maxillofac. Implants 2005, 20, 788–792. [Google Scholar]
- Kaewsiri, D.; Panmekiate, S.; Subbalekha, K.; Mattheos, N.; Pimkhaokham, A. The accuracy of static vs. dynamic computer-assited implant surgery in single tooth space: A randomized controlled trial. Clin. Oral Implants Res. 2019, 30, 505–514. [Google Scholar]
- Herklotz, I.; Beuer, F.; Kunz, A.; Hildebrand, D.; Happe, A. Navigation in implantology. Int. J. Comput. Dent. 2017, 20, 9–19. [Google Scholar]
- Widmann, G.; Bale, R.J. Accuracy in Computer-Aided Implant Surgery—A review. Int. J. Oral Maxillofac. Implants 2006, 21, 305–313. [Google Scholar]
- Lal, K.; White, G.S.; Morea, D.N.; Wright, R.F. Use of stereolithographic templates for surgical and prosthodontic implant planning and placement. Part II. A clinical report. J. Prosthodont. 2006, 15, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Jorba-García, A.; Figueiredo, R.; González-Barnadas, A.; Camps-Font, O.; Valmaseda-Castellón, E. Accuracy and the role of experience in dynamic computer guided dental implant surgery: An in-vitro study. Med. Oral Patol. Oral Cir. Bucal 2019, 24, 76–83. [Google Scholar] [CrossRef]
- Tahmaseb, A.; Wu, V.; Wismeijer, D.; Coucke, W.; Evans, C. The accuracy of static computer-aided implant surgery: A systematic review and meta-analysis. Clin. Oral Implants Res. 2018, 16, 416–435. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stefanelli, L.V.; DeGroot, B.S.; Lipton, D.I.; Mandelaris, G.A. Accuracy of a Dynamic Dental Implant Navigation System in a Private Practice. Int. J. Oral Maxillofac. Implants 2019, 34, 205–213. [Google Scholar] [CrossRef]
- Hoffmann, J.; Westendorff, C.; Gomez-Roman, G.; Reinert, S. Accuracy of navigation-guided socket drilling before implant installation compared to the conventional free-hand method in a synthetic edentulous lower jaw model. Clin. Oral Implants Res. 2005, 16, 609–614. [Google Scholar] [CrossRef]
- Chen, C.K.; Yuh, D.Y.; Huang, R.Y.; Fu, E.; Tsai, C.F.; Chiang, C.Y. Accuracy of implant placement with a navigation system, a laboratory guide, and freehand drilling. Int. J. Oral Maxillofac. Implants 2018, 33, 1213–1218. [Google Scholar] [CrossRef]
- Gargallo-Albiol, J.; Barootchi, S.; Salomó-Coll, O.; Wang, H. Advantages and disadvantages of implant navigation surgery. A systematic review. Ann. Anat. 2019, 225, 1–10. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).