Effect of Tibolone on Bone Mineral Density in Postmenopausal Women: Systematic Review and Meta-Analysis
Abstract
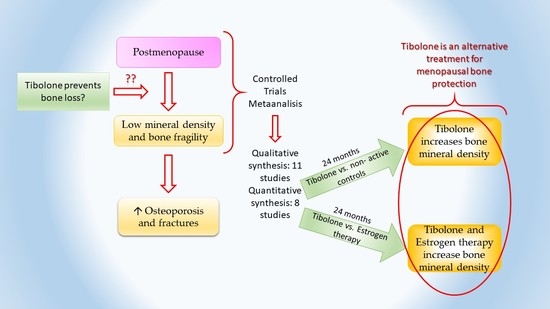
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
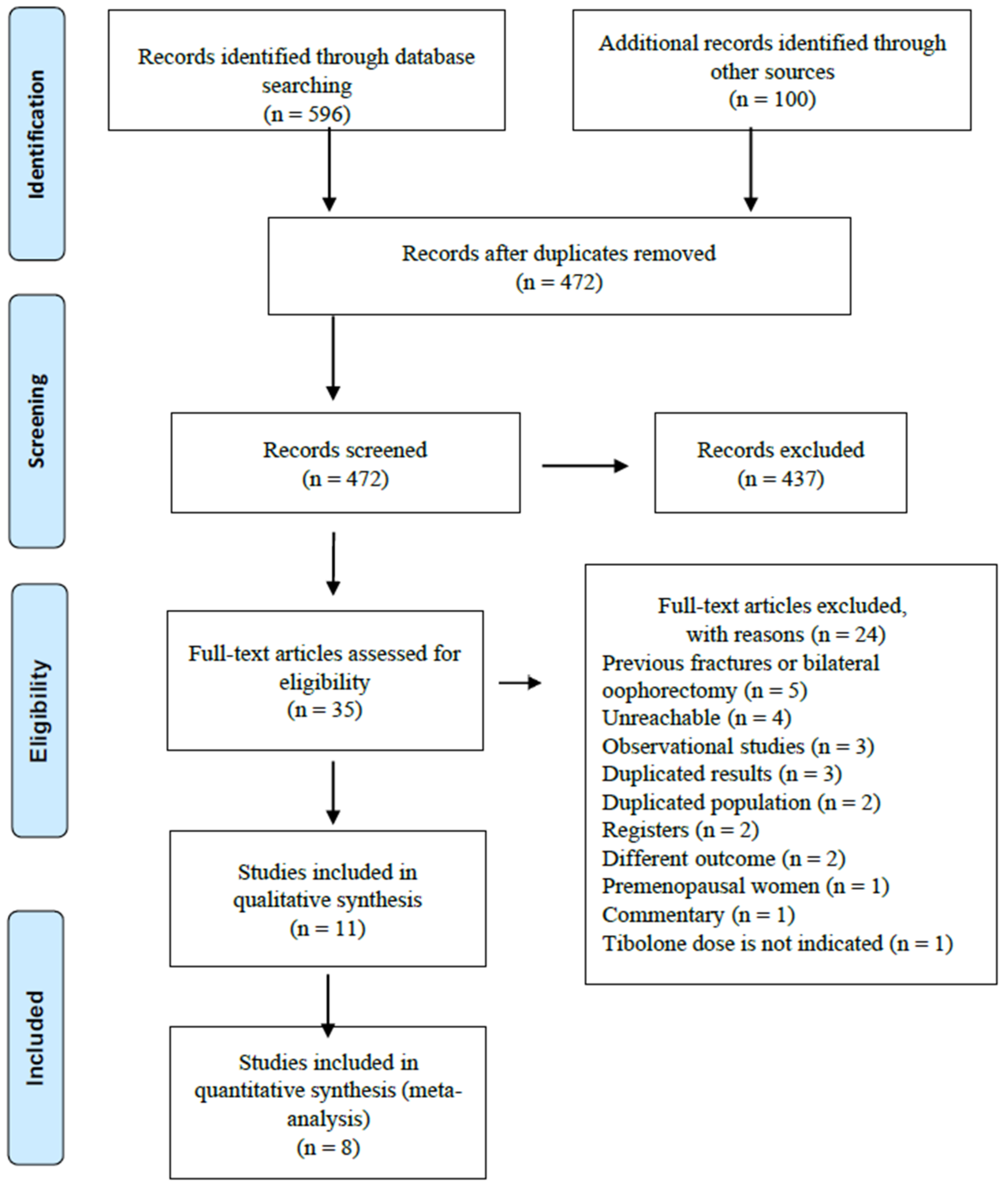
2.2. Study Selection
2.3. Data Collection
2.4. Risk of Bias Assessment
2.5. Statistical Methods
3. Results
3.1. Literature Search and Study Characteristics
| Author, Year | Study Design | Tibolone (Dose) | n | Comparator (Dose) | n | Follow-Up, Years | Age, Years | PO, Year | Assessment of BMD | Measurement Site | Included in the Meta-Analysia |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Rymer et al., 1994 [14] | Non-randomized | 2.5 mg | 46 | No medication | 45 | 2 | 49.5 | 1.7 | DXA, Hologic | Lumbar spine (L1–L4) Femoral neck | Yes |
| Berning et al., 1996 [15] | Controlled double-blind randomized | 2.5 mg 1.25 mg | 33 34 | Placebo | 23 | 2 | 52.1 | 1.8 | Quantitative computed tomography | Lumbar spine (L1–L3) | No |
| Bjarnason et al., 1996 [24] | Controlled double-blind randomized | 2.5 mg + 400 mg Ca 1.25 mg + 400 mg Ca | 28 28 | Placebo + 400 mg Ca | 13 | 2 | 66.8 | 19 | DXA, Hologic | Lumbar spine (L2–L4) | Yes |
| Lippuner et al., 1997 [16] | Open semi-randomized | 2.5 mg | 30 | Estradiol 2 mg + DYD Transdermal estradiol patch 50 μg + DYD No medication | 28 26 31 | 2 | -- | -- | DXA, Hologic | Lumbar spine (L2–L4) Femoral neck | Yes |
| Thiebaud et al., 1999 [17] | Randomized | 2.5 mg | 16 | CEE 0.625 mg + MPA | 20 | 3 | 54.2 | 1.2 | DXA, Hologic | Lumbar spine Femoral neck Total hip | Yes |
| Beardsworth et al., 1999 [18] | Controlled randomized | 2.5 mg | 22 | No treatment | 20 | 2 | 53.2 | 5.2 | DXA, Lunar | Lumbar spine (L2–L4) Femoral neck | No |
| CasteloBranco et al., 2000 [19] | Open semi-randomized | 2.5 mg | 23 | Estradiol valerate 4 mg + androgens Transdermal estradiol patch 50 μg No treatment | 23 26 24 | 1 | 53.1 | 2.7 | DXA, Lunar | Lumbar spine | Yes |
| Milner et al., 2000 [20] | Open semi-randomized | 2.5 mg | 14 | CEE 0.625 mg plus norgestrel No treatment | 18 38 | 2 | 53.9 | 4.5 | DXA, Lunar | Lumbar spine (L1–L4) Femoral neck | No |
| Gallagher et al., 2001 [21] | Controlled double-blind randomized | 0.3 mg + 500 mg Ca 0.625 mg + 500 mg Ca 1.25 mg + 500 mg Ca 2.5 mg + 500 mg Ca | 132 136 127 131 | Placebo + 500 mg Ca | 130 | 2 | 52.4 | 2.5 | DXA, Hologic and Lunar | Lumbar spine (L1–L4) Femoral neck Total hip | Yes |
| Roux et al., 2002 [22] | Double blind, randomized | 2.5 mg + 500 mg Ca 1.25 mg + 500 mg Ca | 70 73 | Estradiol 2 mg + NETA + 500 mg Ca | 68 | 2 | 54.1 | 3.9 | DXA, Hologic | Lumbar spine (L2–L4), Femoral neck Total hip | Yes |
| Gambacciani et al., 2004 [23] | Open randomized | 2.5 mg + 1 g Ca 1.25 mg + 1 g Ca | 15 27 | Ca 1 g | 11 | 2 | 52.7 | 2.3 | DXA, Lunar | Lumbar spine (L2–L4) Femoral neck | Yes |
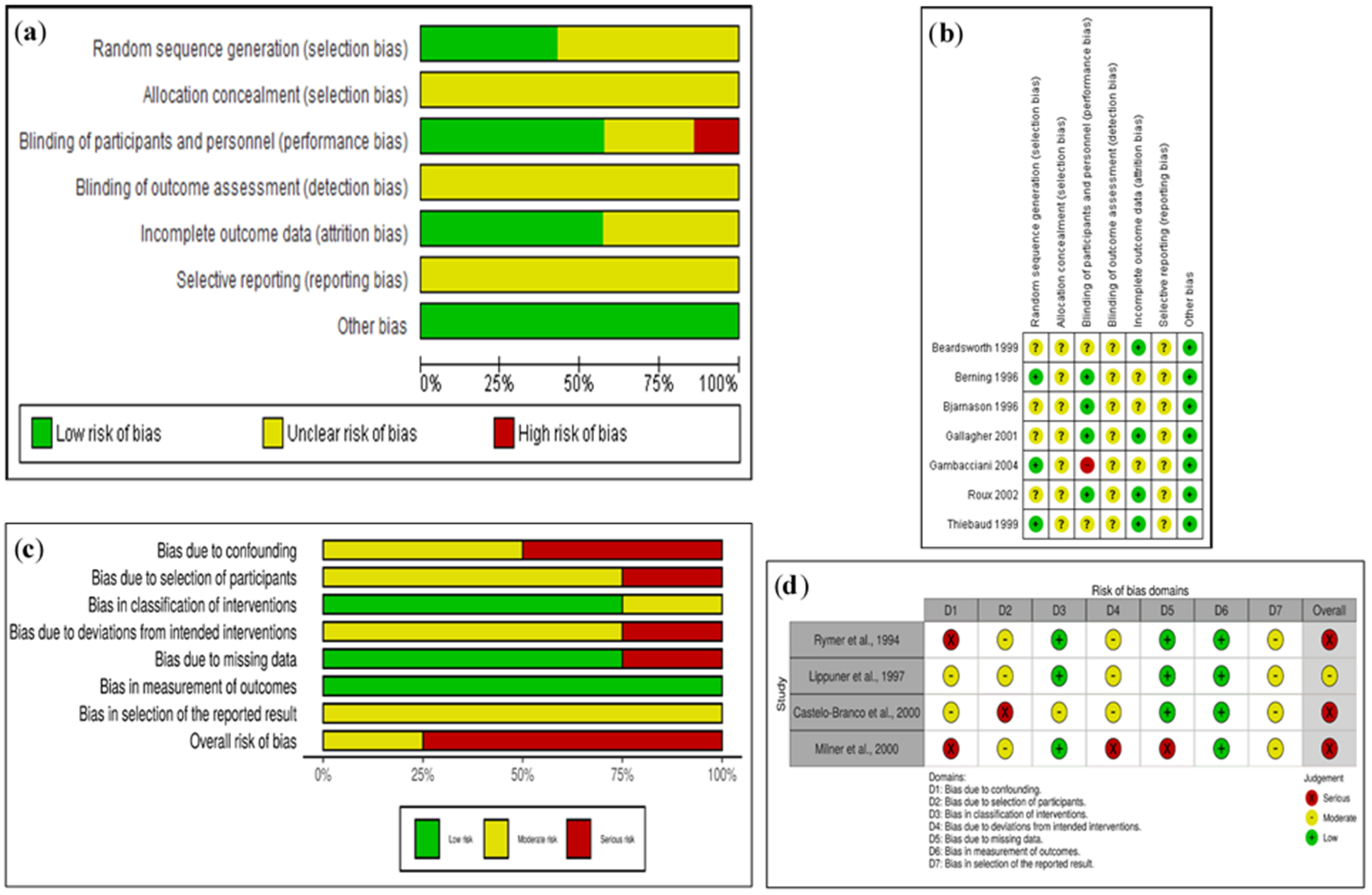
3.2. Risk of Bias Assessment in Randomized Trials
3.3. Risk of Bias Assessment in Non-Randomized Trials
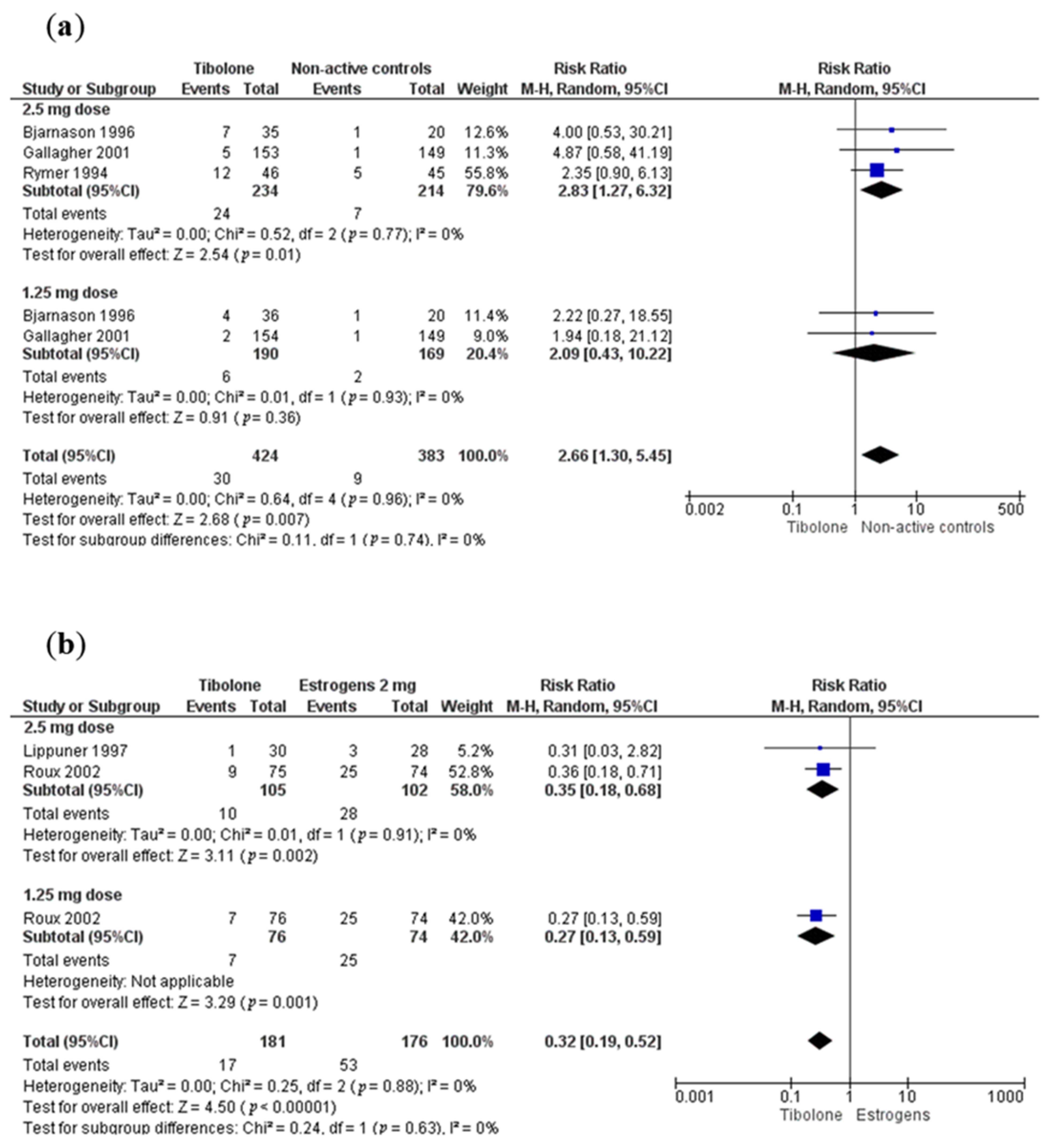
3.4. Tibolone Compared with Non-Active Controls
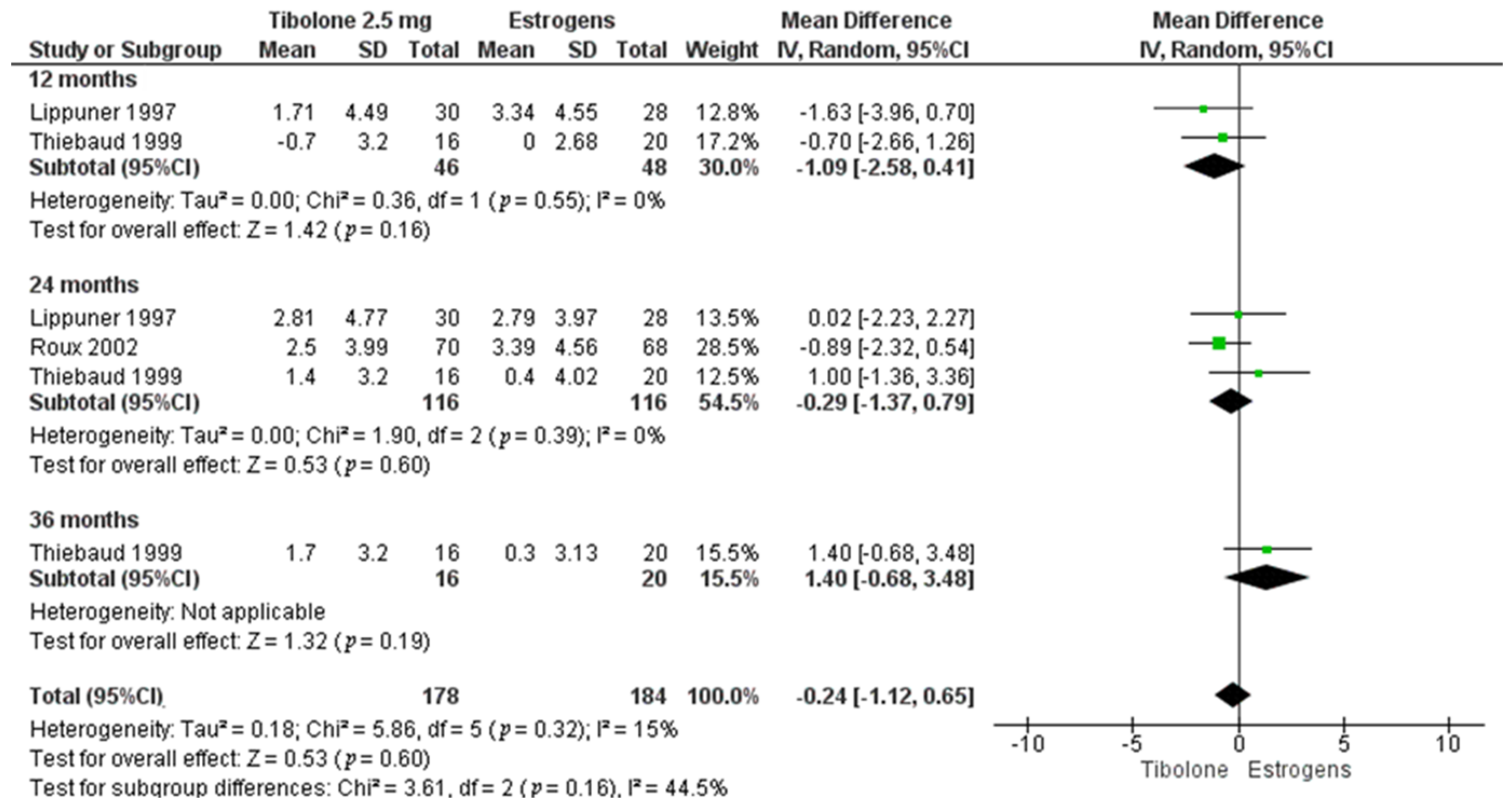
3.5. Tibolone Compared with Estrogens
3.6. Adverse Events
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rizzoli, R. Postmenopausal osteoporosis: Assessment and management. Best Pract. Res. Clin. Endocrinol. Metab. 2018, 32, 739–757. [Google Scholar] [CrossRef] [PubMed]
- Nuti, R.; Brandi, M.L.; Checchia, G.; Di Munno, O.; Dominguez, L.; Falaschi, P.; Fiore, C.E.; Iolascon, G.; Maggi, S.; Michieli, R.; et al. Guidelines for the management of osteoporosis and fragility fractures. Intern. Emerg. Med. 2019, 14, 85–102. [Google Scholar] [CrossRef] [PubMed]
- Pinkerton, J.V.; Aguirre, F.S.; Blake, J.; Cosman, F.; Hodis, H.; Hoffstetter, S.; Kaunitz, A.M.; Kingsberg, S.A.; Maki, P.M.; Manson, J.A.E.; et al. The 2017 hormone therapy position statement of the North American Menopause Society. Menopause 2017, 24, 728–753. [Google Scholar] [CrossRef]
- De Medeiros, S.F.; Yamamoto, M.M.W.; Barbosa, J.S. Abnormal bleeding during menopause hormone therapy: Insights for clinical management. Clin. Med. Insights Women Health 2013, 6, CMWH.S10483. [Google Scholar] [CrossRef]
- Kloosterboer, H.J. Tissue-selectivity: The mechanism of action of tibolone. Maturitas 2004, 48, 30–40. [Google Scholar] [CrossRef]
- Biglia, N.; Maffei, S.; Lello, S.; Nappi, R.E. Tibolone in postmenopausal women: A review based on recent randomised controlled clinical trials. Gynecol. Endocrinol. 2010, 26, 804–814. [Google Scholar] [CrossRef]
- Kloosterboer, H.J. Tibolone: A steroid with a tissue-specific mode of action. J. Steroid Biochem. Mol. Biol. 2001, 76, 231–238. [Google Scholar] [CrossRef]
- Formoso, G.; Perrone, E.; Maltoni, S.; Balduzzi, S.; Wilkinson, J.; Basevi, V.; Marata, A.M.; Magrini, N.; D’Amico, R.; Bassi, C.; et al. Short-term and long-term effects of tibolone in postmenopausal women. Cochrane Database Syst. Rev. 2016, 2016. [Google Scholar] [CrossRef]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; The PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 349, g7647. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, 1–9. [Google Scholar] [CrossRef]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, 4–10. [Google Scholar] [CrossRef]
- The Cochrane Collaboration. Review Manager (RevMan) [Computer Program]. Version 5.3; The Nordic Cochrane Centre, The Cochrane Collaboration: Copenhagen, Denmark, 2014. [Google Scholar]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions. Version 6.1. Cochrane, 2020. (updated September 2020). Available online: https://training.cochrane.org/handbook/current (accessed on 15 October 2020).
- Rymer, J.; Chapman, M.G.; Fogelman, I. Effect of tibolone on postmenopausal bone loss. Osteoporos. Int. 1994, 4, 314–319. [Google Scholar] [CrossRef] [PubMed]
- Berning, B.; Kuijk, C.V.; Kuiper, J.W.; Coelingh Bennink, H.J.T.; Kicovic, P.M.; Fauser, B.C.J.M. Effects of two doses of tibolone on trabecular and cortical bone loss in early postmenopausal women: A two-year randomized, placebo-controlled study. Bone 1996, 19, 395–399. [Google Scholar] [CrossRef]
- Lippuner, K.; Haenggi, W.; Birkhaeuser, M.H.; Casez, J.P.; Jaeger, P. Prevention of postmenopausal bone loss using tibolone or conventional peroral or transdermal hormone replacement therapy with 17β-estradiol and dydrogesterone. J. Bone Miner. Res. 1997, 12, 806–812. [Google Scholar] [CrossRef]
- Thiebaud, D.; Bigler, J.M.; Renteria, S.; Pache, T.; Welti, H.J.; Landry, M.; Bruckhardt, P. A 3-year study of prevention of postmenopausal bone loss: Conjugated equine estrogens plus medroxyprogesterone acetate versus tibolone. J. Menopause 1999, 6, 19–26. [Google Scholar]
- Beardsworth, S.A.; Kearney, C.E.; Purdie, D.W. Prevention of postmenopausal bone loss at lumbar spine and upper femur with tibolone: A two-year randomised controlled trial. BJOG Int. J. Obstet. Gynaecol. 1999, 106, 678–683. [Google Scholar] [CrossRef]
- Castelo-Branco, C.; Vicente, J.J.; Figueras, F.; Sanjuan, A.; Martínez De Osaba, M.J.; Casals, E.; Pons, F.; Balasch, J.; Vanrell, J.A. Comparative effects of estrogens plus androgens and tibolone on bone, lipid pattern and sexuality in postmenopausal women. Maturitas 2000, 34, 161–168. [Google Scholar] [CrossRef]
- Milner, M.; Harrison, R.F.; Gilligan, E.; Kelly, A. Bone density changes during two years treatment with tibolone or conjugated estrogens and norgestrel, compared with untreated controls in postmenopausal women. Menopause 2000, 7, 327–333. [Google Scholar] [CrossRef]
- Gallagher, J.C.; Baylink, D.J.; Freeman, R.; McClung, M. Prevention of bone loss with tibolone in postmenopausal women: Results of two randomized, double-blind, placebo-controlled, dose-finding studies. J. Clin. Endocrinol. Metab. 2001, 86, 4717–4726. [Google Scholar] [CrossRef]
- Roux, C.; Pelissier, C.; Fechtenbaum, J.; Loiseau-Peres, S.; Benhamou, C.L. Randomized, double-masked, 2-year comparison of tibolone with 17β-estradiol and norethindrone acetate in preventing postmenopausal bone loss. Osteoporos. Int. 2002, 13, 241–248. [Google Scholar] [CrossRef]
- Gambacciani, M.; Ciaponi, M.; Cappagli, B.; Monteleone, P.; Benussi, C.; Bevilacqua, G.; Genazzani, A.R. A longitudinal evaluation of the effect of two doses of tibolone on bone density and metabolism in early postmenopausal women. Gynecol. Endocrinol. 2004, 18, 9–16. [Google Scholar] [CrossRef]
- Bjarnason, N.H.; Bjarnason, K.; Haarbo, J.; Rosenquist, C.; Christiansen, C. Tibolone: Prevention of bone loss in late postmenopausal women. J. Clin. Endocrinol. Metab. 1996, 81, 2419–2422. [Google Scholar] [CrossRef] [PubMed]
- Harlow, S.D.; Gass, M.; Hall, J.E.; Lobo, R.; Maki, P.; Rebar, R.W.; Sherman, S.; Sluss, P.M.; De Villiers, T.J. Executive summary of the stages of reproductive aging workshop + 10: Addressing the unfinished agenda of staging reproductive aging. J. Clin. Endocrinol. Metab. 2012, 97, 1159–1168. [Google Scholar] [CrossRef]
- Berning, B.; Bennink, H.J.T.C.; Fauser, B.C.J.M. Tibolone and its effects on bone: A review. Climacteric 2001, 4, 120–136. [Google Scholar] [CrossRef] [PubMed]
- Dören, M.; Nilsson, J.Å.; Johnell, O. Effects of specific post-menopausal hormone therapies on bone mineral density in post-menopausal women: A meta-analysis. Hum. Reprod. 2003, 18, 1737–1746. [Google Scholar] [CrossRef][Green Version]
- Almeida, M.; Laurent, M.R.; Dubois, V.; Claessens, F.; O’Brien, C.A.; Bouillon, R.; Vanderschueren, D.; Manolagas, S.C. Estrogens and androgens in skeletal physiology and pathophysiology. Physiol. Rev. 2017, 97, 135–187. [Google Scholar] [CrossRef]
- Fan, B.; Lu, Y.; Genant, H.; Fuerst, T.; Shepherd, J. Does standardized BMD still remove differences between Hologic and GE-Lunar state-of-the-art DXA systems? Osteoporos. Int. 2010, 21, 1227–1236. [Google Scholar] [CrossRef]
- Shepherd, J.A.; Fan, B.; Lu, Y.; Wu, X.P.; Wacker, W.K.; Ergun, D.L.; Levine, M.A. A multinational study to develop universal standardization of whole-body bone density and composition using GE Healthcare Lunar and Hologic DXA systems. J. Bone Min. Res. 2012, 27, 2208–2216. [Google Scholar] [CrossRef]
- Notelovitz, M. Postmenopausal tibolone therapy: Biologic principles and applied clinical practice. Medscape Gen. Med. 2007, 9, 1–22. [Google Scholar]
- Kaunitz, A.M.; Manson, J.E. Management of menopausal symptoms. Obstet. Gynecol. 2015, 126, 859–876. [Google Scholar] [CrossRef]
- Kanis, J.A.; Cooper, C.; Rizzoli, R.; Reginster, J.Y. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos. Int. 2019, 30, 3–44. [Google Scholar] [CrossRef]
- Tella, S.H.; Gallagher, J.C. Prevention and treatment of postmenopausal osteoporosis. J. Steroid Biochem. Mol. Biol. 2014, 142, 155–170. [Google Scholar] [CrossRef]
- Bouxsein, M.L.; Eastell, R.; Lui, L.Y.; Wu, L.A.; de Papp, A.E.; Grauer, A.; Marin, F.; Cauley, J.A.; Bauer, D.C.; Black, D.M. Change in bone density and reduction in fracture risk: A meta-regression of published trials. J. Bone Miner. Res. 2019, 34, 632–642. [Google Scholar] [CrossRef] [PubMed]
- Barrionuevo, P.; Kapoor, E.; Asi, N.; Alahdab, F.; Mohammed, K.; Benkhadra, K.; Almasri, J.; Farah, W.; Sarigianni, M.; Muthusamy, K.; et al. Efficacy of pharmacological therapies for the prevention of fractures in postmenopausal women: A network meta-analysis. J. Clin. Endocrinol. Metab. 2019, 104, 1623–1630. [Google Scholar] [CrossRef]
- Kim, S.E.; Lee, D.Y.; Choi, D. Tissue-selective estrogen complex for women who experience breast discomfort or vaginal bleeding when on hormone therapy. Menopause 2019, 26, 383–386. [Google Scholar] [CrossRef]
- Gülseren, L.; Kalafat, D.; Mandaci, H.; Gülseren, S.; Çamli, L. Effects of tibolone on the quality of life, anxiety-depression levels and cognitive functions in natural menopause: An observational follow-up study. Aust. N. Z. J. Obstet. Gynaecol. 2005, 45, 71–73. [Google Scholar] [CrossRef]
- Fluck, E.; File, S.E.; Rymer, J. Cognitive effects of 10 years of hormone-replacement therapy with tibolone. J. Clin. Psychopharmacol. 2002, 22, 62–67. [Google Scholar] [CrossRef]
- Marjoribanks, J.; Farquhar, C.; Roberts, H.; Lethaby, A.; Lee, J. Long-term hormone therapy for perimenopausal and postmenopausal women. Cochrane Database Syst. Rev. 2017, 2017, 1–173. [Google Scholar] [CrossRef]
| Tibolone vs. Non-Active Controls | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Measurement Site and Follow-Up Months | Tibolone Dose (mg) | Hologic | Lunar | ||||||
| No. of Comparisons (References) | MD (95%CI), Participants Random Effect Model | Heterogeneity | No. of Comparisons [References] | MD (95%CI), Participants Random Effect Model | Heterogeneity | ||||
| I2 (%) | p Value | I2 (%) | p Value | ||||||
| Lumbar spine 12 m | 2.5 | 4 [14,16,21,24] | 2.75 (2.22 to 3.29), 328 | 0 | 0.60 | 2 [18,20] | 4.39 (3.34 to 5.44), 173 | 0 | 0.35 |
| 1.25 | 2 [21,24] | 3.21 (2.12 to 4.30), 169 | 34 | 0.22 | 1 [20] | 3.59 (2.53 to 4.65), 129 | - | - | |
| Lumbar spine 24 m | 2.5 | 4 [14,16,21,24] | 4.87 (4.16 to 5.57), 328 | 0 | 0.81 | 2 [20,22] | 7.35 (2.68 to 12.01), 152 | 68 | 0.08 |
| 1.25 | 2 [21,24] | 4.15 (3.27 to 5.03), 169 | 0 | 0.32 | 2 [20,22] | 4.84 (3.59 to 6.10), 167 | 0 | 0.36 | |
| Femoral neck 12 m | 2.5 | 3 [14,16,21] | 2.23 (0.89 to 3.57), 287 | 31 | 0.24 | 1 [20] | 2.94 (1.65 to 4.23), 126 | - | - |
| 1.25 | 1 [21] | 1.01 (0.12 to 1.96), 128 | - | - | 1 [20] | 2.74 (1.32 to 4.16), 129 | - | - | |
| Femoral neck 24 m | 2.5 | 3 [14,16,21] | 4.85 (1.55 to 8.15), 287 | 96 | <0.0001 | 2 [20,22] | 4.21 (2.99 to 5.42), 152 | 0 | 0.65 |
| 1.25 | 1 [21] | 2.45 (1.48 to 3.42), 128 | - | - | 2 [20,22] | 3.61 (2.41 to 4.80) 167 | 0 | 0.87 | |
| Tibolone vs. Estrogens | |||||||||
| Lumbar spine 12 m | 2.5 | 3 [16,17,22] | −1.21 (−2.87 to 0.46), 232 | 67 | 0.05 | 1 [18] | −0.30 (−2.82 to 2.22), 46 | - | - |
| 24 m | 3 [16,17,22] | −0.58, (−3.77 to 2.60), 232 | 88 | 0.0002 | - | - | - | - | |
| 36 m | 1 [17] | 2.0, (−0.66 to 4.66), 36 | - | - | - | - | - | - | |
| Total hip 12 m | 2.5 | 2 [17,22] | −0.81, (−1.58 to −0.03), 174 | 0 | 0.52 | - | - | - | - |
| 24 m | 2 [17,22] | 0.12, (−2.28 to 2.53), 174 | 68 | 0.08 | - | - | - | - | |
| 36 m | 1 [17] | 2.90, (0.62 to 5.18), 36 | - | - | - | - | - | - | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castrejón-Delgado, L.; Castelán-Martínez, O.D.; Clark, P.; Garduño-Espinosa, J.; Mendoza-Núñez, V.M.; Sánchez-Rodríguez, M.A. Effect of Tibolone on Bone Mineral Density in Postmenopausal Women: Systematic Review and Meta-Analysis. Biology 2021, 10, 211. https://doi.org/10.3390/biology10030211
Castrejón-Delgado L, Castelán-Martínez OD, Clark P, Garduño-Espinosa J, Mendoza-Núñez VM, Sánchez-Rodríguez MA. Effect of Tibolone on Bone Mineral Density in Postmenopausal Women: Systematic Review and Meta-Analysis. Biology. 2021; 10(3):211. https://doi.org/10.3390/biology10030211
Chicago/Turabian StyleCastrejón-Delgado, Lizett, Osvaldo D. Castelán-Martínez, Patricia Clark, Juan Garduño-Espinosa, Víctor Manuel Mendoza-Núñez, and Martha A. Sánchez-Rodríguez. 2021. "Effect of Tibolone on Bone Mineral Density in Postmenopausal Women: Systematic Review and Meta-Analysis" Biology 10, no. 3: 211. https://doi.org/10.3390/biology10030211
APA StyleCastrejón-Delgado, L., Castelán-Martínez, O. D., Clark, P., Garduño-Espinosa, J., Mendoza-Núñez, V. M., & Sánchez-Rodríguez, M. A. (2021). Effect of Tibolone on Bone Mineral Density in Postmenopausal Women: Systematic Review and Meta-Analysis. Biology, 10(3), 211. https://doi.org/10.3390/biology10030211