Abstract
Debonding and detachment of artificial teeth from the denture base is frequently encountered in prosthodontic practice. This study aims to assess the effect of modifications in the ridge-lap surface of denture teeth with various combinations of mechanical and chemical surface treatments with hydrofluoric acid on bond strength with the acrylic denture base resin and to identify the failure modes (adhesive, cohesive, or mixed). Seventy acrylic resin teeth samples were randomly divided into seven groups (n = 10): a control group (unmodified) and six treatment groups, in which various combinations of mechanical and chemical surface treatments were performed. Then, these teeth were attached to a heat-cured denture base resin block at 45° angulation. The acrylized test samples were thermocycled, and the compressive bond strength was evaluated using a universal mechanical testing machine. The results suggest that roughening with diamond burs yields the highest bond strength, whereas etching/grooving and air abrasion result in the lowest bond strength. Acid etching complemented air abrasion to improve bond strength, while negative effects were noted with acid etching in other groups. Furthermore, roughening at the neck portion of the acrylic teeth can be used by the manufacturing companies as a standard to provide higher bond strength while maintaining the esthetics of the anterior teeth.
1. Introduction
Geriatric patients often seek the replacement of missing natural teeth (partial or complete) to restore speech, function, and esthetics. A durable, strong, and biologically acceptable denture necessitates the use of a favorable and superior-quality denture base [1]. Polymethyl methacrylate (PMMA) has been widely used for manufacturing denture bases in conglomeration with artificial teeth for a variety of prostheses. In addition, the use of acrylic teeth and denture bases has emerged as a common practice in implant dentistry in either implant- or implant-tissue-supported dentures [2].
PMMA has been commonly used for the manufacturing of several prostheses owing to its advantages, such as low cost, low-water sorption and solubility, excellent translucency impersonating natural teeth (even in the thinnest sections), ability to bond chemically to the denture base, superior strength, durability, and reparability [3].
Dentures are usually subjected to considerable variations in stress during function [4]. Debonding and detachment of artificial teeth from the denture base is one of the most common and frequently encountered failures or complications in prosthodontic practice. Debonding or detachment between the denture base resin and the artificial tooth may be attributed to unwarranted stress or fatigue. Numerous studies have been conducted to evaluate the reasons associated with the failure and strengthen the bond between the two. Kawara et al. highlighted that failures occur owing to the gap and crack propagations in areas of load deliberation [5]. In addition, they consume the dentist’s time and effort as well as impose added costs and distress to the patient; approximately 26–33% of the dentures are repaired owing to debonding [6,7].
The mutual solubility or miscibility of both the polymers is critical to the development of an interwoven polymer, thus enhancing the strength of the bond between the two. The bond between both the components is influenced considerably by the physical contact of the polymerizing denture base resin with the tooth resin and the chemical reaction between the two, thereby resulting in the formation of the aforementioned interwoven polymer network. The adhesion between the two components is one of the most imperative factors for achieving desirable prosthetic performance and durability [8].
The most common reasons for detachment and debonding are the smaller ridge-lap surface area obtained for bonding; the course of stresses stumbled upon during function; incompatible surface conditions or the presence of impurities or residual wax at the interface between the teeth and the denture base; presence of deficient monomers during polymerization; and futile or wretched curing methods [9].
Implant-supported dentures and prostheses exert a higher biting force on the dentition and are associated with improved masticatory function; therefore, there is a higher chance of debonding. Additionally, the presence of attachments in the anterior region of the implant-supported dentures may result in an insufficient acrylic resin thickness in the anterior segment; this may, in turn, lead to fractures and the debonding of teeth from the base [10].
Prior studies have reported a wide disparity of biting force on the anterior teeth between natural dentition and acrylic prostheses such as complete dentures, removable partial dentures, or hybrid prostheses. Debonding or detachment is frequently encountered in the anterior region and may be attributed to the smaller ridge-lap surface areas available for bonding as well as the direction of the stresses encountered during function. This highlights the importance of improving the bond strength between the acrylic teeth and the denture base [11]. Debonding is also observed when porcelain teeth are used with denture base resin, as the bond between the two is purely mechanical [12]. The failure or detachment can be classified into three types, namely, adhesive, cohesive, and a mixture of the two (i.e., mixed). Adhesive failure arises at the interface of the acrylic tooth and the denture base contact and is manifested by the absence of component (tooth and/or denture base contact) fragments on the opposing surface. Cohesive failure may be described as a complete fracture within the artificial tooth or denture base resin. Mixed failure may be characterized by the presence of a part of denture base material on the tooth surface or vice versa [13].
Modern technology has introduced numerous advances and methods to enhance the bond strength between denture bases and artificial teeth. These may include chemical treatments (surface treatment), mechanical procedures, and the combination of both in conjunction with different polymerization techniques. Mechanical procedures incorporate the use of diatoric pins, grooves, undercuts, roughening of the ridge-lap surface of teeth, and sandblasting, which is known to enhance mechanical interlocking during processing [14]. Chemical procedures incorporate the use of monomers, solvents, or adhesive bonding agents such as the Silane coupling agent (SCA) and non-polymerizable solvents such as dichloromethane, trichloromethane ethyl acetate, acetone, and dissolved PMMA applied to the contact surfaces to augment the chemical bonding. A variety of polymerization techniques have been used, including chemical, heat, light, and microwave irradiation [15].
Strength may be defined as the maximum stress that a structure can withstand without sustaining a specific amount of plastic strain (yield strength). There are several types of stresses that the denture may be subjected to during function, including tensile, shear, flexural, and compressive stresses [16,17]. Tensile strength represents the ability of an object or material to endure loads, tending to lengthen it. Flexural strength reflects the complex stresses applied to the denture during mastication and is an indicator of rigidity. Compressive strength may be defined as the resistance applied by a material or object upon application of force or load to shorten or compress it [18]. In the current study, compressive bond strength is evaluated. The relation between maxillary and mandibular anterior teeth is such that when the patient bites with anterior teeth, the forces act at an angle of 30–45° to the long axis of these teeth. Anterior teeth are under compression that comes off the long axis of the tooth. This off-axis compressive load is one of the reasons for debonding denture teeth from hybrid dentures [12,13].
The use of hydrofluoric (HF) acid for composite repair is well documented; however, the current literature lacks substantial information on the effect of hydrofluoric acid and the roughening of the cervical part of acrylic teeth on the bond strength between the acrylic denture base and the teeth. So, this study aims to assess the effect of modifications in the ridge-lap surface of denture teeth with various combinations of mechanical and chemical surface treatments with HF acid on the bond strength with the acrylic denture base resin and to identify the failure modes (adhesive, cohesive, or mixed).
2. Materials and Methods
The investigation was conducted by a single researcher. Seventy acrylic resin teeth samples (Maxillary Central Incisors, Yamahachi, Gamagori, Japan) attached to a heat-cured denture base resin block (Eco-Cryl Hot-Protechno, Vilamalla Girona, Spain) were used. The long axes of the teeth were aligned at 45° with respect to the base of the block (Figure 1). The angulation of the tooth in each block was measured using a profile projector to omit the chances of any incongruity of alignment between the teeth and the base.
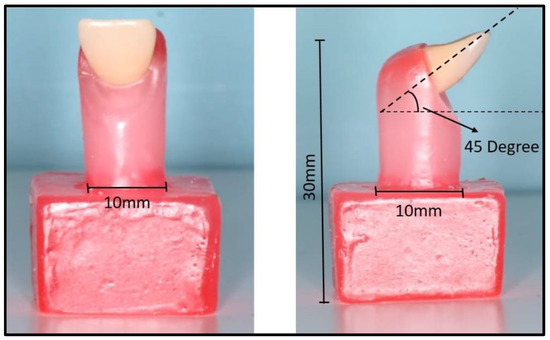
Figure 1.
Acrylic tooth attached to the block with the long axes aligned at 45° with respect to the base of the block.
To ensure standardization of the test specimens, a prototype model (size: 10 × 10 × 30 mm) was fabricated (Figure 1), followed by the duplication of the prototype model with silicone and the formation of the split mold (Figure 2).
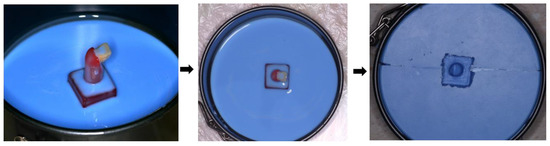
Figure 2.
Duplication of the prototype model with silicone and the formation of the split mold.
Seven study groups were considered (ten samples each):
- Group 1: Negative control (unmodified group; Figure 3A).
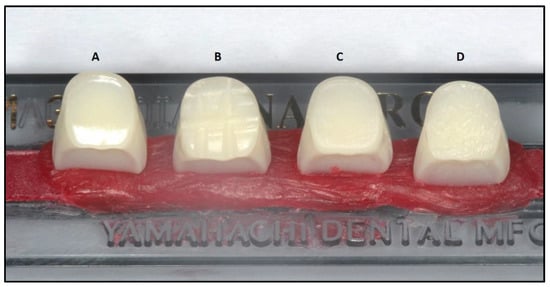 Figure 3. Mechanical treatments performed on teeth: (A) No treatment, (B) grooves, (C) treatment with 50 μm aluminum oxide particles, and (D) roughening with a flame-shaped diamond sintered bur.
Figure 3. Mechanical treatments performed on teeth: (A) No treatment, (B) grooves, (C) treatment with 50 μm aluminum oxide particles, and (D) roughening with a flame-shaped diamond sintered bur. - Group 2: Mechanical treatment was performed by preparing 2 mm grooves on the ridge-lap surfaces of the teeth with a round bur (Figure 3B).
- Group 3: Grooves were created in a manner similar to those in Group 2 in addition to chemical surface treatment with (HF) acid and SCA. First, the samples were etched with 10% HF acid Acido Gel 10 (Maquira Dental Products, Maringá, Brazil) for 60 s followed by the application of SCA (Pulpdent Corporation, Watertown, MA, USA), coated in two layers on the ridge-lap surfaces and cured according to the manufacturer recommendations (Figure 3B and Figure 4).
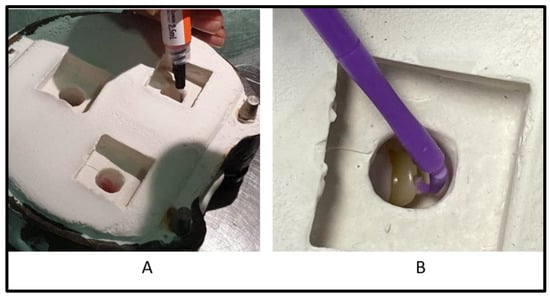 Figure 4. Chemical surface treatment of teeth with (A) hydrofluoric acid and (B) Silane coupling agent.
Figure 4. Chemical surface treatment of teeth with (A) hydrofluoric acid and (B) Silane coupling agent. - Group 4: The samples were mechanically treated with 50 μm aluminum oxide particles (Protechno, Spain) using a sandblasting machine (SandStorm Prestige 80150) for 10 s at a pressure of 2.5 bar and at a distance of 10 mm between the plunger and the tooth surface. The slack was removed using an air–water spray for 10 s, followed by drying for 3 s (Figure 3C).
- Group 6: The teeth were roughened with a flame-shaped diamond sintered bur using a low-speed handpiece with a water spray. A new diamond bur was used for each sample (Figure 3D).
The acrylized test samples were then thermocycled (6000 cycles, equivalent to 30 days) in distilled water between 5 to 55 °C (Model 1100, SD Mechatronik, Bayern, Germany) [19]. A universal mechanical testing machine (Model 4301, Instron, Canton, MA, USA) was used for applying a point compressive load at 45 degrees from the long axis of each denture tooth on the palatal surface (Figure 5). The machine was run at a constant crosshead speed of 5.0 mm/min, temperature 18.00 ± 1 °C, and humidity 50 ± 1%. The size of the point compressing the palatal surface of teeth was 5 mm and was directed towards the cingulum of each tooth to be fractured. Upon failure, each specimen was removed, and the maximum load at failure was recorded in newton (N); compressive stress (in MPa) at maximum compressive load was calculated by using the formula S = Force/Area, where F is the maximum load required to cause the failure and A is the interface area of a test specimen measured in mm2. The results collected were tabulated in a Microsoft Excel spreadsheet (version 1910, 2019, Microsoft Inc., Redmond, WA, USA).

Figure 5.
Specimen subjected to testing in a universal testing machine.
Mean compressive stress (MPa) at maximum compressive load and mean maximum load (N) were compared between all the groups using the one-way analysis of variance (ANOVA) test. The intergroup comparison of mean compressive stress at maximum compressive and mean maximum loads was completed using the posthoc Bonferroni test. The modes of failure were evaluated using loupes and were compared using the chi-square test.
3. Results
The investigation was conducted on 70 acrylic central incisors attached to heat-cured denture base resin blocks. Scheme 1A,B depicts compressive stress vs. time curves for each experimental group.
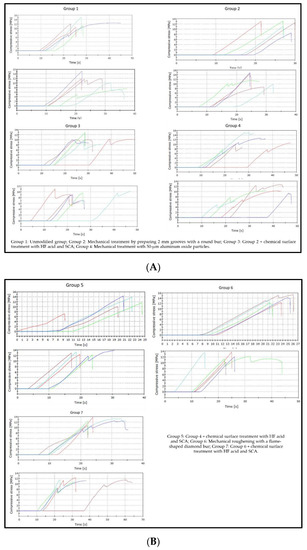
Scheme 1.
(A). Compressive stress vs. time curve for Groups 1 to 4. (B). Compressive stress vs. time curve for Groups 5 to 7.
Mean compressive stress (MPa) at maximum compressive load was compared among Groups 1–7 by conducting the one-way ANOVA test. There were significant differences among Groups 1–7. The intergroup comparison was conducted using the posthoc Bonferroni test. Herein, significantly better outcomes were obtained for Group 1 (11.8 ± 2.25 MPa) than those obtained for Groups 3 (10.11+ 1.17 MPa) and 4 (10.52 + 2.49 MPa); however, the outcome was significantly worse than that of Group 6 (12.90 + 1.42 MPa). Additionally, the outcomes pertaining to Group 3 (10.11+ 1.17 MPa) were worse than those obtained for Groups 5 (12.14 + 2.18 MPa), 6 (12.90 + 1.42 MPa), and 7 (11.95 + 1.05 MPa). The compressive strength was significantly smaller in the case of Group 4 ((10.52 + 2.49 MPa) than those in Groups 5 ((12.14 + 2.18 MPa), 6 (12.90 + 1.42 MPa), and 7 ((11.95 + 1.05 MPa). The intergroup comparison among Groups 5, 6, and 7 yielded insignificant results (Table 1 and Table 2, and Scheme 2).

Table 1.
One-way ANOVA for mean compressive stress (MPa) at maximum compressive load.

Table 2.
Intergroup comparison of mean compressive stress (MPa) at maximum compressive load conducted using the posthoc Bonferroni test.
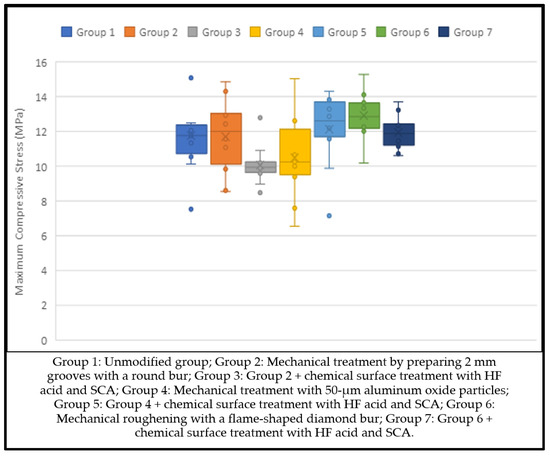
Scheme 2.
Intergroup comparison of mean compressive stress (MPa) at maximum compressive load.
The mean maximum compressive load (N) was compared for Groups 1–7 using the one-way ANOVA test, and the results suggested a significant difference among all the groups. N was significantly higher in Group 1 (926.83 + 176.84) than those in Groups 3 (793.72 + 91.87) and 4 (825.99 + 195.79). In addition, N was significantly higher in Group 2 (921.47 + 174.13) than those in Groups 3 (793.72 + 91.87) and 4 (825.99 + 195.79), but significantly smaller than that in Group 6 (1013.44 + 111.26); N was significantly smaller in the case of Group 3 (793.72 + 91.87) than those in Groups 5 (953.68 + 171.18), 6 (1013.44 + 111.26), and 7 (938.48 + 82.22). Further, N was significantly smaller in the case of Group 4 (825.99 + 195.79) than those in Groups 5 (953.68 + 171.18), 6 (1013.44 + 111.26), and 7 (938.48 + 82.22), and no significant difference was found for intergroup comparisons of the mean maximum load between Groups 5, 6, and 7 (Table 3 and Table 4, and Scheme 3).

Table 3.
One-way ANOVA for mean maximum load (N).

Table 4.
Intergroup comparison of mean maximum compressive load (N) assessed using the posthoc Bonferroni test.
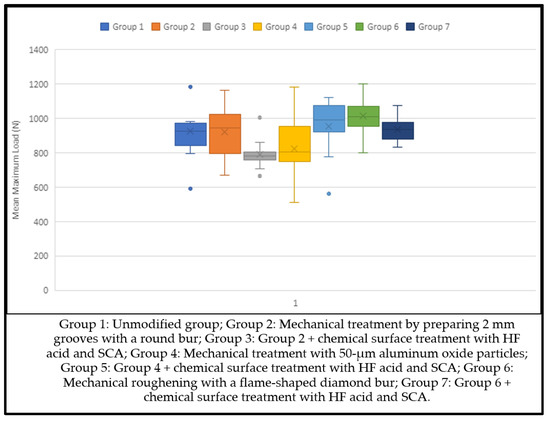
Scheme 3.
Mean compressive load at failure (N) (Groups 1–7).
The modes of failure were compared between Groups 1–7 using the chi-square test, and the results are shown in Scheme 4. In addition, the mean compressive load at failure is shown in Scheme 2. Adhesive failure (i.e., clean failure) occurred significantly more frequently at the tooth/denture base interface (clean) in Groups 3 (70%) and 7 (40%). Significantly more cohesive tooth failure was observed in Groups 1 (70%), 2 (50%), 5 (60%), 6 (100%), and 7 (50%). Mixed areas of simultaneous adhesive and cohesive failures appeared significantly more often in Groups 4 (80%) and 5 (40%) (Scheme 4, Figure 6).
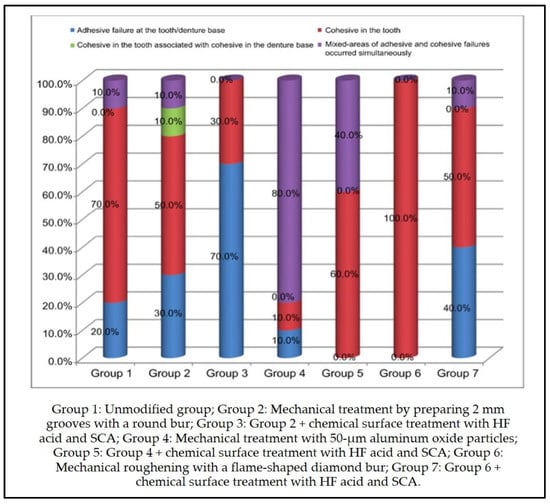
Scheme 4.
Types of failure modes (Groups 1–7).
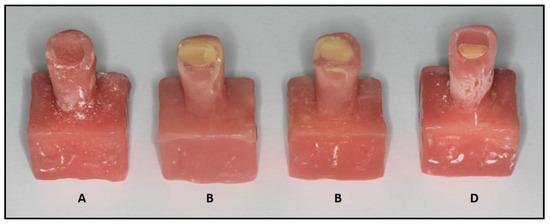
Figure 6.
Types of failure modes: (A) adhesive, (B) cohesive in tooth, (C) cohesive in tooth and denture base, (D) mixed: adhesive and cohesive.
4. Discussion
This study has analyzed the effects of modifications in the ridge-lap surface of denture teeth with various combinations of mechanical and chemical surface treatments on bond strength with the acrylic denture base resin. The samples in the study were subjected to thermal cycling, which represents mechanical fatigue in a moist oral condition. A significant difference in mean compressive bond strength was observed when the seven groups were compared.
The chemical or mechanical surface treatment on the denture tooth surface preceding bonding yielded mixed results on bond strength. Our study revealed significant differences in all the groups regarding mean compressive stress at maximum compressive load. The results of this study showed that the maximum compressive load and stress were generated in Group 6, wherein the teeth were roughened with a flame-shaped diamond sintered bur using a low-speed handpiece. Roughening tends to augment bond strength as it increases the surface area of the denture teeth available for interaction with the polymerizing denture base resin and facilitates better penetration of the acrylic resin by generating surface irregularities [20]. Our results are in agreement with those reported by Bragaglia et al. [21] in terms of comparing the bond strength between the denture base and teeth, subjected to six surface treatments. This study concluded that roughening the tooth base with an abrasive stone provided the greatest bond strength [10].
Group 5 displayed smaller compressive stress and loads than Group 6, wherein the teeth were treated with air abrasion followed by chemical treatment with HF acid and SCA. Air abrasion increases the surface area of the ridge-lap part of the denture teeth, increasing the roughening on the surface through the formation of irregularities and undercuts, creating micromechanical retention pits for the repair resin, and thus improving the bond strength [22]. Similar results were highlighted by Qaw et al. [23] and Al Zaher et al. [2], who emphasized that the application of bonding agents to the ridge-lap surface after alumina air abrasion improved bond strength. Studies conducted by Bahrani and Khaledi [24] and Fletcher et al. [25] also reported a considerable improvement in bond strength when SCA was applied as a surface conditioner.
In the current study, when compared to the control group, the compressive bond strengths of Groups 6 and 5 were significantly higher. This may be because the free surface energy of the newly exposed acrylic will be different from that of untreated acrylic [25]. Chemical surface treatments with HF acids, along with SCA, increase bond strength by the formation of covalent bonds between the functional groups of denture resin, the hydrolyzable groups of SCA, and acrylic teeth [26,27]. This is accompanied by the penetration of SCA in the micropores, thus facilitating the interlocking of the material within the irregularities formed by alumina-blasting.
The compressive bond strength and load reflected by Group 2 were smaller than those exhibited by Group 1, wherein 2-mm grooves were incorporated on the ridge-lap surfaces of the teeth with a round bur. Our results disagreed with those reported in recent studies, which have shown an improvement in strength with the incorporation of grooves owing to improvements in physical retention [28]. This was followed by Group 4, wherein only the teeth were treated with 50 μm aluminum oxide particles based on a sandblasting machine [29,30]. The minimum compressive strength and load were obtained for Group 3, wherein grooves were treated initially and then followed by chemical treatment with hydrofluoric acid and SCA.
The compressive strength of Groups 2 and 3 was significantly less compared to the control group. This is in partial agreement with the results of the study by Büyükyilmaz et al. [31], who reported that the advantage of the horizontal groove is unclear for increasing bond strength. Barpal et al. [32] reported adhesive failures in most tested specimens in which mechanical retention in the form of diatoric or grooves was tried. It can be assumed that rough surfaces of retention grooves may trap wax residues, tinfoil substitutes, oils, or other contaminants and may decrease the bond strength adversely [33,34]. Additionally, acrylic resin might not flow completely into deep grooves and may lead to a poor bond between teeth and the resin.
The results of this study cannot be compared directly with other studies due to the difference in the composition of acrylic teeth, the chemical used, and the denture base resin, which may affect bonding strength to varying degrees. In the current study, we used highly crosslinked teeth that had nano-silica filler particles to increase fracture strength and wear resistance. These fillers and crosslinking agents have been shown to decrease the chemical bond between teeth and denture base resin compared to non-crosslinked teeth [35,36]. The use of different products may explain the inconsistent results compared to other studies comparing the effect of chemical and mechanical surface treatments on teeth–resin bond strength [37].
Comparison of the modes of failures indicated that adhesive failure at the tooth/denture base interface (clean failure) was predominant among Groups 2, 3, and 7. Cohesive failure was predominant among Groups 1, 2, 5, 6, and 7. Mixed failures occurred more frequently in the cases of Groups 4 and 5. According to the British Standard (BS EN ISO 22112: 2017) [38], satisfactory bond strength is attained when the failure is cohesive. When discussing the serviceability of the prosthesis, cohesive failures can be considered more favorable compared to adhesive failures [2]. Using acrylic teeth or denture bases with high crosslinking and more filler particles can avert such cohesive failures, thus prolonging the life of the prosthesis. In the current study, the majority of specimens demonstrated cohesive modes of failure, whereas a relatively smaller number of specimens exhibited mixed or adhesive failures. These findings are in concordance with the results presented by another study [9,38].
It is well accepted that in-vivo performance differs from that in an in-vitro setting. Hence, the proposed method’s relevance to increasing the bond strength between the denture base and acrylic resin by roughening with diamond burs and surface treatment with hydrofluoric acid and air abrasion should be studied in actual clinical situations.
5. Conclusions
This study aimed to assess the effect of modifications in the ridge-lap surface of denture teeth with various combinations of mechanical and chemical surface treatments on the bond strength with the acrylic denture base resin. Within the limitations of the study, the following conclusions can be drawn:
- Roughening the ridge-lap surface of denture teeth with diamond burs yielded the highest bond strength (12.9 MPa) compared with all other groups. The failure mode in this group was cohesive (100%) in terms of fracture of the acrylic tooth, which explains the improved bond strength between the tooth and the acrylic resin. These results are in agreement with those reported by Bragaglia et al. [21]. The surface irregularities produced increased the surface area for interaction with the polymerizing denture base resin and facilitated better acrylic resin penetration [20,21].
- Grooving/etching and air abrasion alone resulted in the lowest bond strength (10.1 MPa and 10.5 MPa, respectively). The failure mode in Group 3 was predominantly adhesive (70%) in nature, while mixed areas of adhesive and cohesive failures (80%) were predominant in Group 4.
- Acid etching complemented air abrasion to improve bond strength (12.1 MPa). The failure mode in this group was a combination of cohesive (60%) and mixed failures (40%). The results are in agreement with those reported by Bahrani and Khaledi [24], who suggested that etching eliminates debris, increases surface area, and amends surface topography, thus leading to an increase in bond strength.
- Roughening at the neck portion of the acrylic teeth may be adopted by the manufacturing companies as a standard to provide higher bond strengths while maintaining the esthetics of the anterior teeth.
Future studies in actual clinical situations by using dentures used by patients should be carried out to research the additional effects of the buffering action of saliva, temperature change, and by-products from food ingredients on compressive bond strength.
Author Contributions
Conceptualization, M.E.S. and H.L.; methodology, I.F. and M.J.; software, A.T. and T.M.; validation, A.J.; formal analysis, M.E.S. and S.J.; investigation, I.F. and M.J.; data curation, A.T. and T.M.; writing—original draft preparation, M.E.S. and H.L.; writing—review and editing, M.E.S., S.J., M.I.A. and H.L.; visualization, H.L. and A.J.; supervision, M.E.S., M.I.A. and S.J. All authors have read and agreed to the published version of the manuscript.
Funding
The research received no external funding.
Institutional Review Board Statement
The research protocol was approved by the research board at the college of Dentistry, Jazan University (Reference Number: CODJU-2031I).
Informed Consent Statement
Not applicable.
Data Availability Statement
All data are available within the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Cervino, G.; Cicciù, M.; Herford, A.S.; Germanà, A.; Fiorillo, L. Biological and chemo-physical features of denture resins. Materials 2020, 13, 3350. [Google Scholar] [CrossRef] [PubMed]
- AlZaher, Z.A.; Almaskin, D.F.; Qaw, M.S.; Abu Showmi, T.H.; Abualsaud, R.; Akhtar, S.; Gad, M.M. Chemo-mechanical approach to improve repair bond strength of denture teeth. Int. J. Dent. 2020, 4, 8870361. [Google Scholar] [CrossRef] [PubMed]
- Radford, D.R.; Juszczyk, A.S.; Clark, R.K.F. The bond between acrylic resin denture teeth and the denture base: Recommendations for best practice. Br. Dent. J. 2014, 216, 165–167. [Google Scholar] [CrossRef] [PubMed]
- Ravi, N.; Krishna, D.P.; Manoj, S.; Chethan, H. A Functional stress analysis in the maxillary complete denture influenced by the position of artificial teeth and load levels: An in-vitro study. J. Indian Prosthodont. Soc. 2010, 10, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Chittaranjan, B.; Taruna, M.; Sudheer, N.; Patil, N.S. Evaluation of shear bond strength of three different types of artificial teeth to heat cure denture base resin: An in vitro study. Indian J. Dent. Res. 2013, 24, 321–325. [Google Scholar] [CrossRef]
- Jain, G.; Palekar, U.; Awinashe, V.; Mishra, S.K.; Kawadkar, A.; Rahangdale, T. The effect of different chemical surface treatments of denture teeth on shear bond strength: A comparative study. J. Clin. Diagn. Res. 2014, 8, ZC15–ZC18. [Google Scholar] [CrossRef] [PubMed]
- BinMahfooz, A.M.; Qutub, O.A. Effect of Surface Treatments and Adhesive Materials on the Shear Bond Strength of Artificial Denture Teeth to Denture Base Resins. J. Contemp. Dent. Pract. 2018, 19, 631–636. [Google Scholar] [CrossRef] [PubMed]
- Yadav, N.S.; Somkuwar, S.; Mishra, S.K.; Hazari, P.; Chitumalla, R.; Pandey, S.K. Evaluation of bond strength of acrylic teeth to denture base using different polymerization techniques: A comparative study. J. Int. Oral Health 2015, 7, 54–56. [Google Scholar]
- Zidan, S.; Silikas, N.; Haider, J.; Alhotan, A.; Jahantigh, J.; Yates, J. Assessing Tensile bond strength between denture teeth and nano-zirconia impregnated PMMA denture base. Int. J. Nanomed. 2020, 15, 9611–9625. [Google Scholar] [CrossRef]
- Patil, S.B.; Naveen, B.H.; Patil, N.P. Bonding acrylic teeth to acrylic resin denture bases: A review. Gerodontology 2006, 23, 131–139. [Google Scholar] [CrossRef]
- Flanagan, D. Bite force and dental implant treatment: A short review. Med. Devices 2017, 10, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Sadar, L.; Dhume, S.; Maniar, N.; Prakash Patil, J.; Rane, P.; Gandhewar, M. Comparative evaluation of shear compressive bond strength between cross-linked acrylic resin denture base and cross-linked acrylic resin teeth with different modifications of their ridge lap surfaces. J. Contemp. Dent. Pract. 2013, 14, 898–903. [Google Scholar] [CrossRef]
- Moffitt, A.R.; Woody, R.D.; Parel, S.M.; Miller, B.H. Failure Modes with point loading of three commercially available denture teeth. J. Prosthodont. 2008, 17, 432–438. [Google Scholar] [CrossRef] [PubMed]
- Ravi, S.Y.; Pridhvi, K.; Sumeet, S.; Srinivas, K.; Surapaneni, H. Evaluation of bond strength of acrylic teeth to the denture base resins with chemical surface treatment and mechanical modification—An in-vitro comparative study. Baba Farid Univ. Dent. J. 2014, 5, 148–157. [Google Scholar]
- Krishna, V.P.; Premalatha, A.; Babu, P.J.; Raju, D.S.; Kumar, M.P.; Rao, D.B. Effect of various chemicals on the bond strength of acrylic tooth and denture base–An invitro comparative study. J. Int. Oral Health 2014, 6, 100–105. [Google Scholar]
- Khosravani, M.R. Mechanical behavior of restorative dental composites under various loading conditions. J. Mech. Behav. Biomed. Mater. 2019, 93, 151–157. [Google Scholar] [CrossRef]
- Nowak, J.F.; Samuel, J. Quantifying machining outputs of pristine human teeth relevant to dental preparation procedures. J. Mech. Behav. Biomed. Mater. 2019, 91, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Gad, M.; Rahoma, A.; Abualsaud, R.; Mahmoud, M. Tensile strength of denture base material reinforced with zirconia nanoparticle and glass fibers. Al-Azhar Dent. J. Girls 2018, 5, 285–295. [Google Scholar] [CrossRef][Green Version]
- Jain, S.; Sayed, M.; Ahmed, W.M.; Halawi, A.H.A.; Najmi, N.M.A.; Aggarwal, A.; Bhandi, S.; Patil, S. An In-Vitro Study to Evaluate the Effect of Denture Cleansing Agents on Color Stability of Denture Bases Fabricated Using CAD/CAM Milling, 3D-Printing and Conventional Techniques. Coatings 2021, 11, 962. [Google Scholar] [CrossRef]
- Ranjith Kumar, P.; Sivaprasad, K.K.; Karunakaran, A. Comparative evaluation of bond strength of denture base resin to acrylic resin teeth following different surface treatments: An in vitro study. Int. J. Appl. Dent. Sci. 2021, 7, 74–78. [Google Scholar] [CrossRef]
- Bragaglia, L.E.; Prates, L.H.M.; Calvo, M.C.M. The role of surface treatments on the bond between acrylic denture base and teeth. Braz. Dent. J. 2009, 20, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, S.A., Jr.; Ferracane, J.L.; Bona, A.D. Influence of Surface treatments on the bond strength of repaired composite restorative materials. Dent. Mater. 2008, 25, 442–451. [Google Scholar] [CrossRef]
- Qaw, M.S.; Abushowmi, T.H.; Almaskin, D.F.; AlZaher, Z.A.; Gad, M.M.; Al-Harbi, F.A.; Abualsaud, R.; Ammar, M.M. A novel approach to improve repair bond strength of repaired acrylic resin: An in vitro study on the shear bond strength. J. Prosthodont. 2020, 29, 323–333. [Google Scholar] [CrossRef] [PubMed]
- Bahrani, F.; Khaledi, A.A. Effect of surface treatments on shear bond strength of denture teeth to denture base resins. Dent. Res. J. 2014, 11, 114–118. [Google Scholar]
- Fletcher, A.M.; Al-Mulla, M.A.S.; Amin, W.M.; Dodd, A.W.; Ritchie, G.M. A method of improving the bonding between artificial teeth and PMMA. J. Dent. 1985, 13, 102–108. [Google Scholar] [CrossRef]
- Lung, C.Y.; Matinlinna, J.P. Aspects of silane coupling agents and surface conditioning in dentistry: An overview. Dent. Mater. 2012, 28, 467–477. [Google Scholar] [CrossRef] [PubMed]
- Antonucci, J.M.; Dickens, S.H.; Fowler, B.O.; Xu, H.H.; McDonough, W.G. Chemistry of silanes: Interfaces in dental polymers and composites. J. Res. Natl. Inst. Stand. Technol. 2005, 110, 541–558. [Google Scholar] [CrossRef]
- Radford, D.R.; Juszczyk, A.S.; Clark, R.K.F. Achieving a good bond in acrylic resin denture teeth. BDJ Team 2015, 1, 14061. [Google Scholar] [CrossRef]
- Alkurt, M.; Yeşil Duymuş, Z.; Gundogdu, M. Effect of repair resin type and surface treatment on the repair strength of heat-polymerized denture base resin. J. Prosthet. Dent. 2014, 111, 71–78. [Google Scholar] [CrossRef]
- Minami, H.; Suzuki, S.; Minesaki, Y.; Kurashige, H.; Tanaka, T. In vitro evaluation of the influence of repairing condition of denture base resin on the bonding of autopolymerizing resins. J. Prosthet. Dent. 2004, 91, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Büyükyilmaz, S.; Ruyter, I.E. The effects of polymerization temperature on the acrylic resin denture base-tooth bond. Int. J. Prosthodont. 1997, 10, 49–54. [Google Scholar] [PubMed]
- Barpal, D.; Curtis, D.A.; Finzen, F.; Perry, J.; Gansky, S.A. Failure load of acrylic resin denture teeth bonded to high impact acrylic resins. J. Prosthet. Dent. 1998, 80, 666–671. [Google Scholar] [CrossRef]
- Spratley, M.H. An investigation of the adhesion of acrylic resin teeth to dentures. J. Prosthet. Dent. 1987, 58, 389–392. [Google Scholar] [CrossRef]
- Morrow, R.M.; Matvias, F.M.; Windeler, A.S.; Fuchs, R.J. Bonding of plastic teeth to two heat-curing denture base resins. J. Prosthet. Dent. 1978, 39, 565–568. [Google Scholar] [CrossRef]
- Sorensen, S.E.; Fjeldstad, E. Bonding of plastic teeth to acrylic resin denture base material. Odont. Tidskrift. 1961, 69, 467–477. [Google Scholar]
- Clancy, J.M.; Boyer, D.B. Comparative bond strengths of light-cured, heat-cured, and autopolymerizing denture resins to denture teeth. J. Prosthet. Dent. 1989, 61, 457–462. [Google Scholar] [CrossRef]
- Choi, J.J.E.; Uy, C.E.; Plaksina, P.; Ramani, R.S.; Ganjigatti, R.; Waddell, J.N. Bond Strength of Denture Teeth to Heat-Cured, CAD/CAM and 3D Printed Denture Acrylics. J. Prosthodont. 2020, 29, 415–421. [Google Scholar] [CrossRef]
- Gad, M.M.; Abualsaud, R.; Rahoma, A.; Al-Thobity, A.M.; Al-Abidi, K.S.; Akhtar, S. Effect of zirconium oxide nanoparticles addition on the optical and tensile properties of polymethyl methacrylate denture base material. Int. J. Nanomed. 2018, 9, 283–292. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).