Dermal Targeting Delivery of Terbinafine Hydrochloride Using Novel Multi-Ethosomes: A New Approach to Fungal Infection Treatment
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.1.1. Chemicals
2.1.2. Animals
2.2. TH Solubility Determination
2.3. Preparation of Vesiclular Systems
2.4. Characterization of Formulations
2.4.1. Hydrodynamic Diameter and Zeta Potential
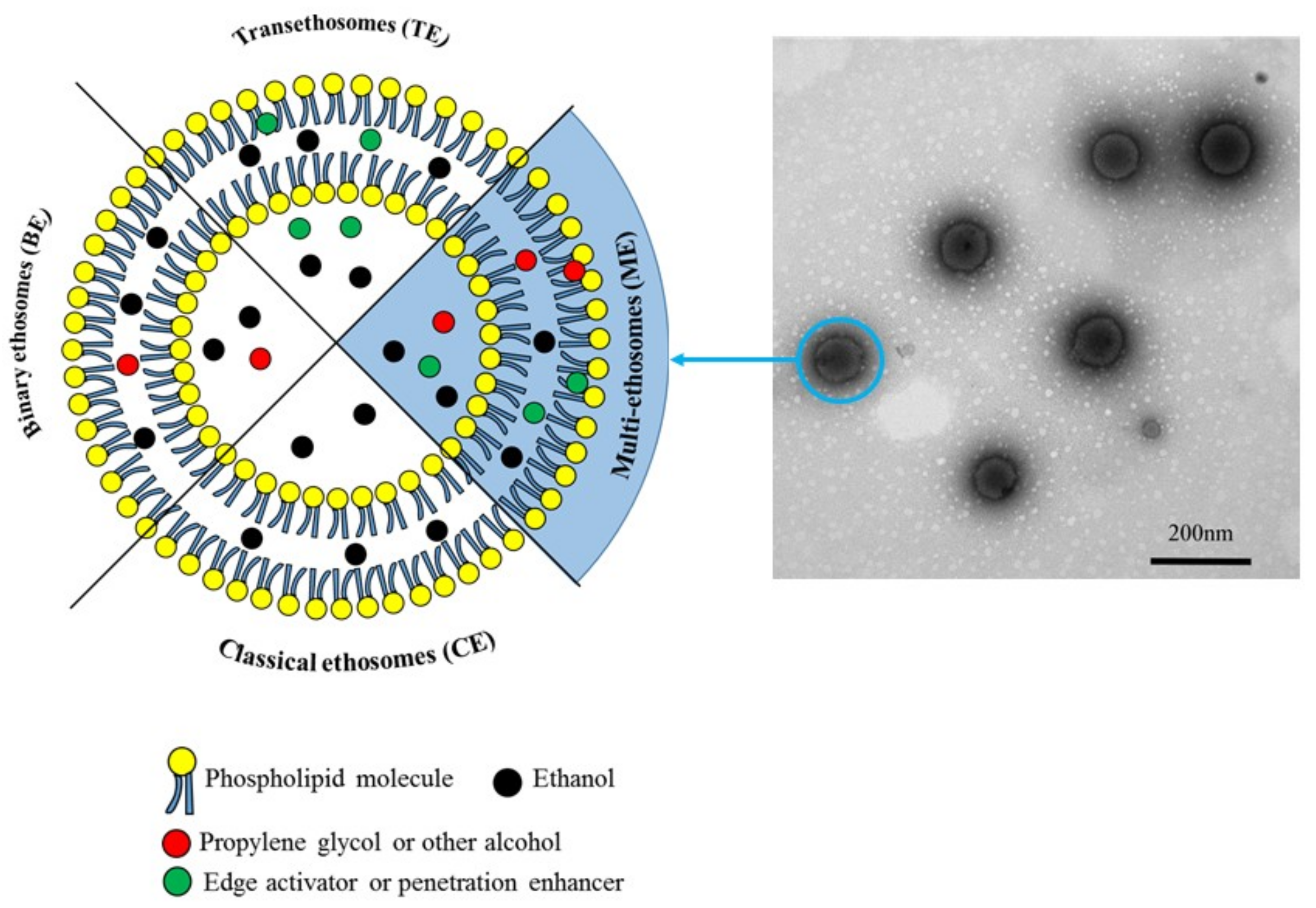
2.4.2. Transmission Electron Microscopy (TEM)
2.4.3. Drug Entrapment Efficiency (EE)
2.4.4. Physical Stability Studies
2.5. Ex Vivo Drug Permeation and Deposition Studies
2.5.1. Franz Diffusion Cell Methods
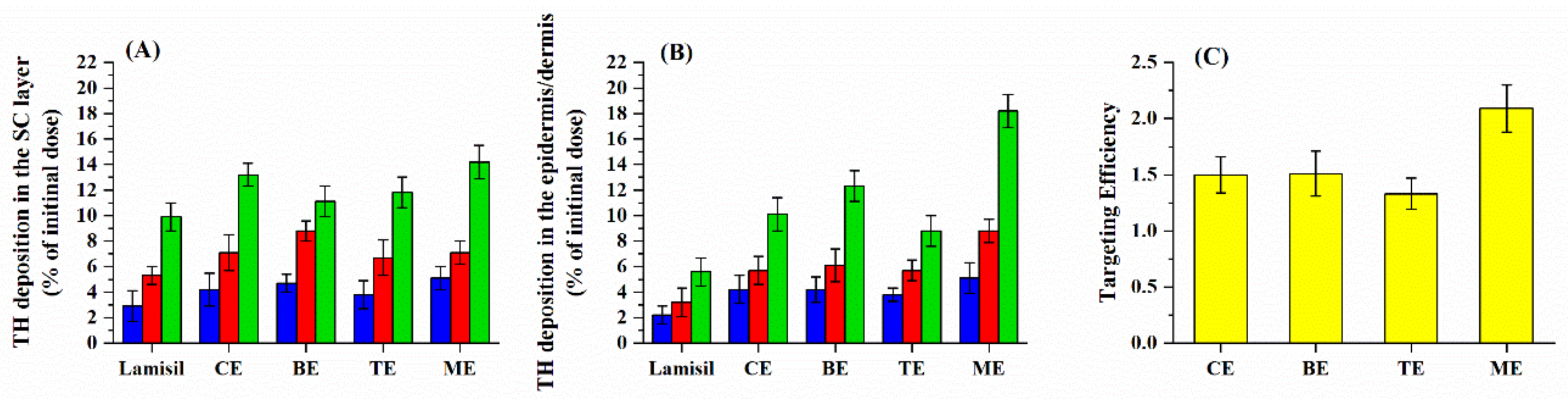
formulations/total amount of TH deposited into skin with Lamisil®
2.5.2. Visualization by Confocal Laser Scanning Microscopy (CLSM)
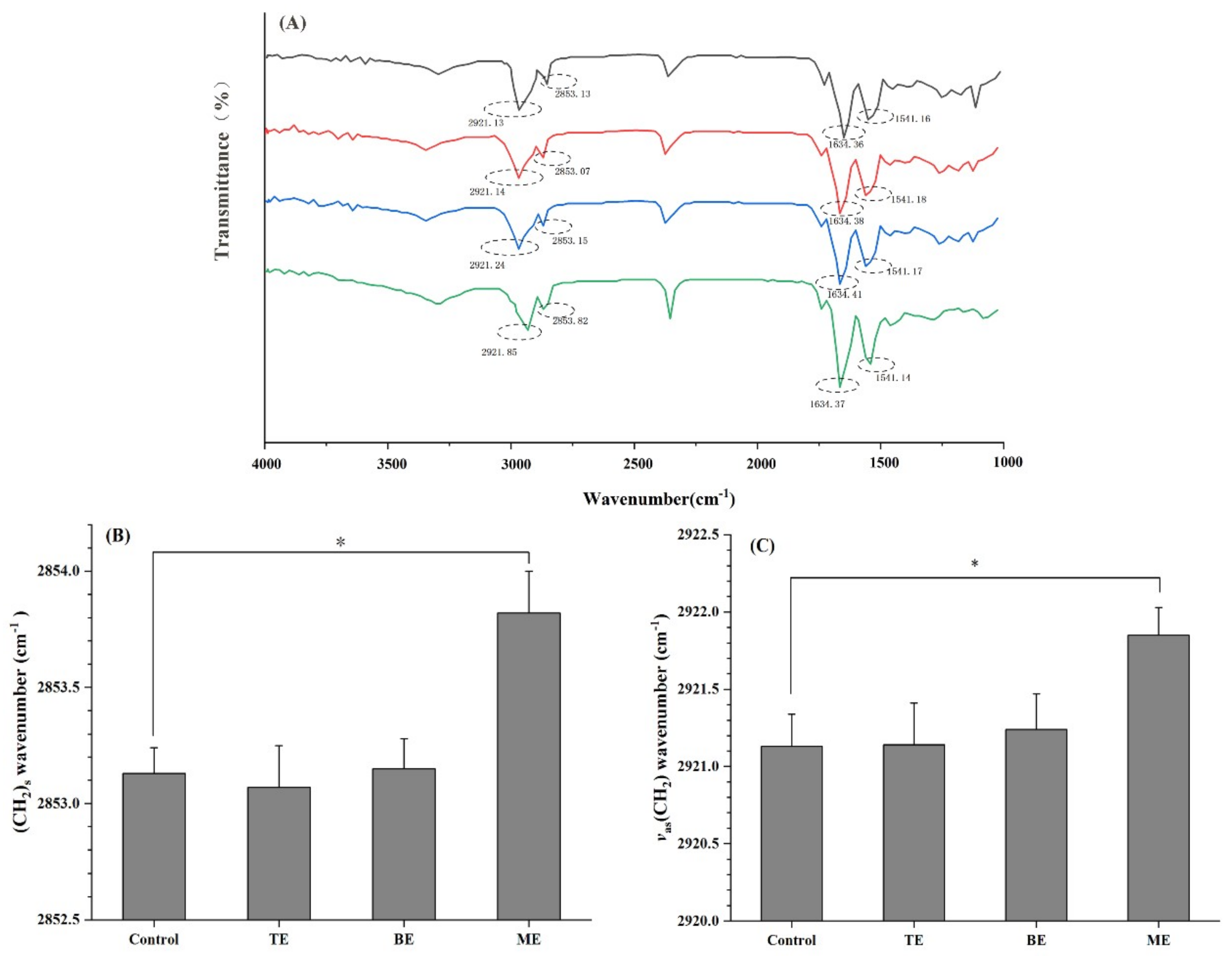
2.6. Attenuated Total Reflection Fourier Transform Infrared Spectroscopy (ATR-FTIR)
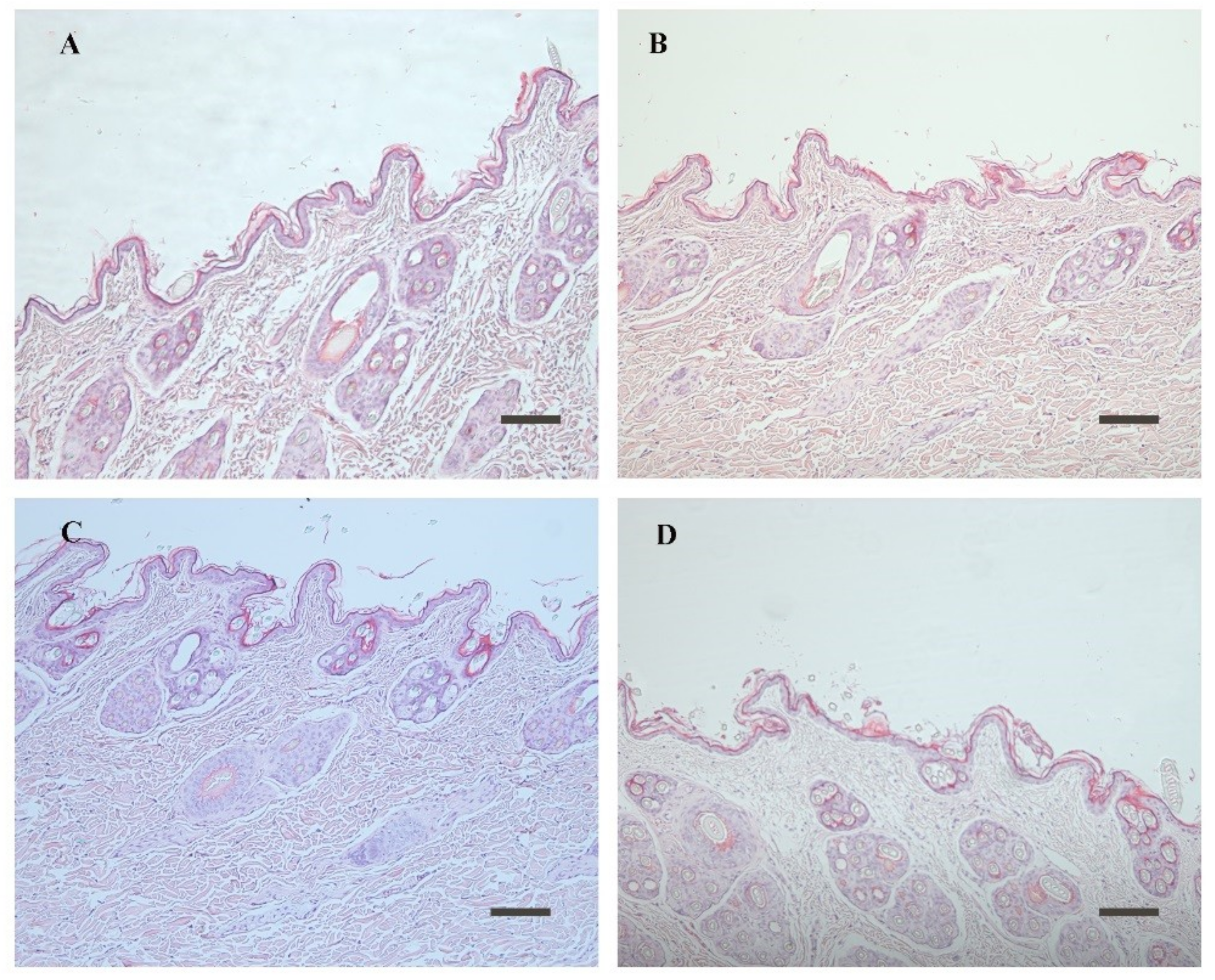
2.7. Skin Irritation Test and Histopathological Study
2.8. In Vitro Antifungal Activity
2.8.1. Inoculum Preparation
2.8.2. Minimum Inhibitory Concentration (MIC) Determination
2.9. Statistical Analysis
3. Results and Discussion
3.1. Preparation and Characterization of the MEs
3.2. Stability Investigation
3.3. Skin Permeation and Deposition Studies
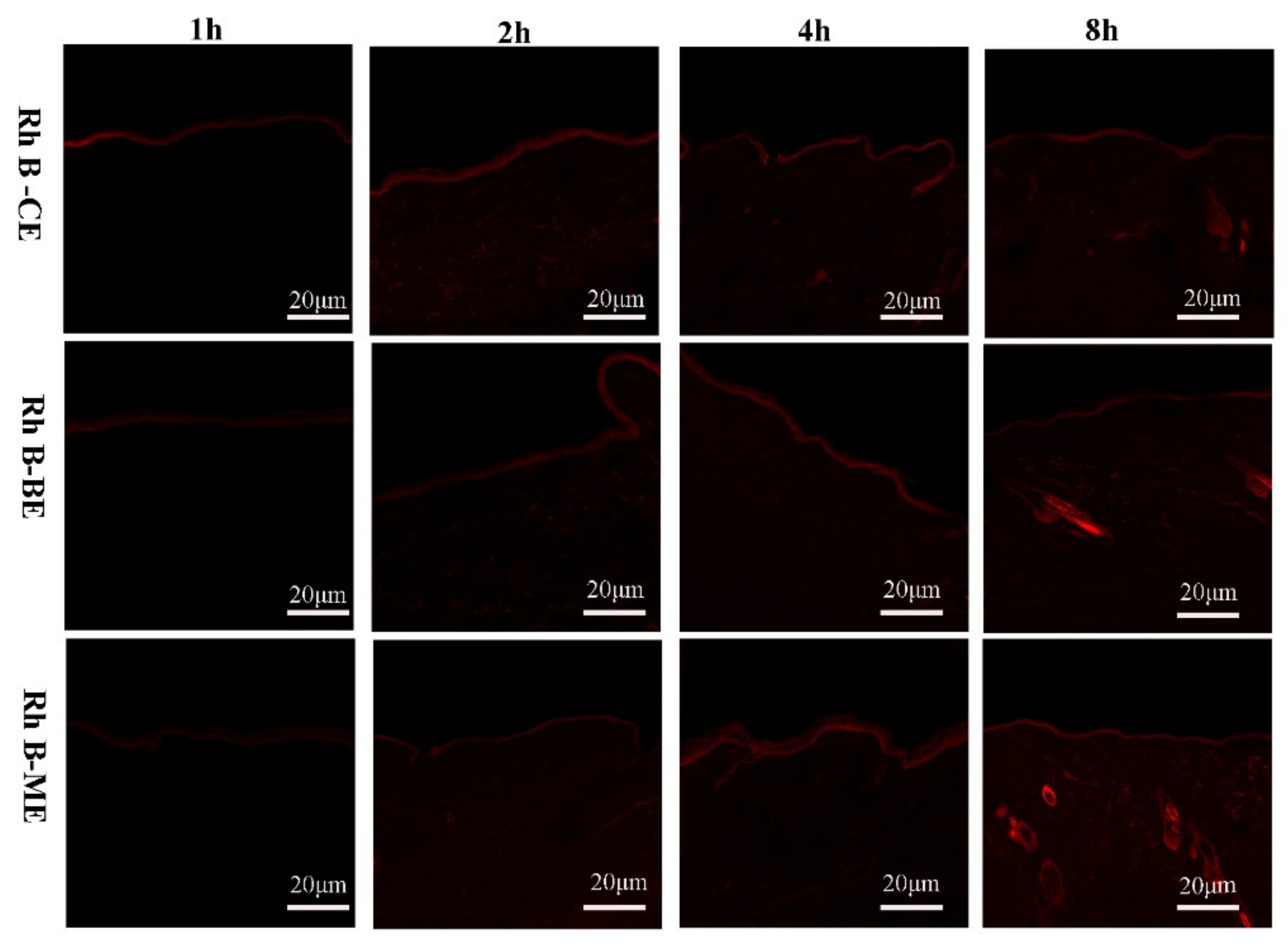
3.4. Tracking the Fluorescently-Labeled Vesicles in the Rat Skin Layers Using CLSM
3.5. ATR-FTIR
3.6. Skin Irritation Study and Histological Observation
3.7. Antifungal Activity
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Chowdhary, A.; Prakash, A.; Sharma, C.; Kordalewska, M.; Kumar, A.; Sarma, S.; Tarai, B.; Singh, A.; Upadhyaya, G.; Upadhyay, S.; et al. A multicentre study of antifungal susceptibility patterns among 350 Candida auris isolates (2009-17) in India: Role of the ERG11 and FKS1 genes in azole and echinocandin resistance. J. Antimicrob. Chemother. 2018, 73, 891–899. [Google Scholar] [CrossRef] [PubMed]
- Rosen, T.; Gold, L.F.S. Antifungal drugs for onychomycosis: Efficacy, safety, and mechanisms of action. Semin. Cutan. Med. Surg. 2016, 35, S51–S55. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lusiana Muller-Goymann, C.C. Preparation, characterization, and in vitro permeation study of terbinafine HCl in poloxamer 407-based thermogelling formulation for topical application. AAPS PharmSciTech 2011, 12, 496–506. [Google Scholar] [CrossRef] [PubMed]
- Nozawa, M.; Goto, M.; Wada, Y.; Kumazawa, M.; Shimokawa, K.-I.; Ishii, F. Generic selection criteria for safety and patient benefit VII: Comparing the physicochemical and pharmaceutical properties of brand-name and generic terbinafine hydrochloride cream. Drug Discov. Ther. 2018, 12, 16–20. [Google Scholar] [CrossRef]
- Ashtikar, M.; Nagarsekar, K.; Fahr, A. Transdermal delivery from liposomal formulations—Evolution of the technology over the last three decades. J. Control. Release 2016, 242, 126–140. [Google Scholar] [CrossRef]
- Zhang, J.P.; Wei, Y.H.; Zhou, Y.; Li, Y.Q.; Wu, X.A. Ethosomes, binary ethosomes and transfersomes of terbinafine hydrochloride: A comparative study. Arch. Pharm. Res. 2012, 35, 109–117. [Google Scholar] [CrossRef]
- Moolakkadath, T.; Aqil, M.; Ahad, A.; Imam, S.S.; Praveen, A.; Sultana, Y.; Mujeeb, M.; Iqbal, Z. Fisetin loaded binary ethosomes for management of skin cancer by dermal application on UV exposed mice. Int. J. Pharm. 2019, 560, 78–91. [Google Scholar] [CrossRef]
- Song, C.K.; Balakrishnan, P.; Shim, C.K.; Chung, S.J.; Chong, S.; Kim, D.D. A novel vesicular carrier, transethosome, for enhanced skin delivery of voriconazole: Characterization and in vitro/in vivo evaluation. Colloid Surf. B-Biointerfaces 2012, 92, 299–304. [Google Scholar] [CrossRef]
- Zhou, Y.; Wei, Y.H.; Liu, H.X.; Zhang, G.Q.; Wu, X.A. Preparation and in vitro evaluation of ethosomal total alkaloids of sophora alopecuroides loaded by a transmembrane pH-gradient method. AAPS PharmSciTech 2010, 11, 1350–1358. [Google Scholar] [CrossRef]
- Sala, M.; Diab, R.; Elaissari, A.; Fessi, H. Lipid nanocarriers as skin drug delivery systems: Properties, mechanisms of skin interactions and medical applications. Int. J. Pharm. 2018, 535, 1–17. [Google Scholar] [CrossRef]
- Abdel-Messih, H.A.; Ishak, R.A.H.; Geneidi, A.S.; Mansour, S. Tailoring novel soft nano-vesicles ‘Flexosomes’ for enhanced transdermal drug delivery: Optimization, characterization and comprehensive ex vivo—In vivo evaluation. Int. J. Pharm. 2019, 560, 101–115. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Wang, Z.; Liu, L.; Qu, S.; Mao, Y.Y.; Peng, X.; Li, Y.X.; Tian, J. Cinnamaldehyde inhibits Candida albicans growth by causing apoptosis and its treatment on vulvovaginal candidiasis and oropharyngeal candidiasis. Appl. Microbiol. Biotechnol. 2019, 103, 9037–9055. [Google Scholar] [CrossRef] [PubMed]
- Feng, X.; Chen, Y.T.; Li, L.Y.; Zhang, Y.Q.; Zhang, L.T.; Zhang, Z.Q. Preparation, evaluation and metabolites study in rats of novel amentoflavone-loaded TPGS/soluplus mixed nanomicelles. Drug Deliv. 2020, 27, 137–150. [Google Scholar] [CrossRef] [PubMed]
- Sharma, G.; Goyal, H.; Thakur, K.; Raza, K.; Katare, O.P. Novel elastic membrane vesicles (EMVs) and ethosomes-mediated effective topical delivery of aceclofenac: A new therapeutic approach for pain and inflammation. Drug Deliv. 2016, 23, 3135–3145. [Google Scholar] [CrossRef] [PubMed]
- El-Kayal, M.; Nasr, M.; Elkheshen, S.; Mortada, N. Colloidal (-)-epigallocatechin-3-gallate vesicular systems for prevention and treatment of skin cancer: A comprehensive experimental study with preclinical investigation. Eur. J. Pharm. Sci. 2019, 137, 15. [Google Scholar] [CrossRef] [PubMed]
- Kassem, A.A.; Mohsen, A.M.; Ahmed, R.S.; Essam, T.M. Self-nanoemulsifying drug delivery system (SNEDDS) with enhanced solubilization of nystatin for treatment of oral candidiasis: Design, optimization, in vitro and in vivo evaluation. J. Mol. Liq. 2016, 218, 219–232. [Google Scholar] [CrossRef]
- Ma, M.; Wang, J.P.; Guo, F.; Lei, M.Z.; Tan, F.P.; Li, N. Development of nanovesicular systems for dermal imiquimod delivery: Physicochemical characterization and in vitro/in vivo evaluation. J. Mater. Sci. Mater. Med. 2015, 26, 1–11. [Google Scholar] [CrossRef]
- Chu, Y.; Li, D.; Luo, Y.F.; He, X.J.; Jiang, M.Y. Preparation and in vitro evaluation of glycyrrhetinic acid-modified curcumin-loaded nanostructured lipid carriers. Molecules 2014, 19, 2445–2457. [Google Scholar] [CrossRef]
- Ahmed, O.A.A.; Badr-Eldin, S.M. Development of an optimized avanafil-loaded invasomal transdermal film: Ex vivo skin permeation and in vivo evaluation. Int. J. Pharm. 2019, 570, 118657. [Google Scholar] [CrossRef]
- Lademann, J.; Ilgevicius, A.; Zurbau, O.; Liess, H.D.; Schanzer, S.; Weigmann, H.J.; Antoniou, C.; Pelchrzim, R.V.; Sterry, W. Penetration studies of topically applied substances: Optical determination of the amount of stratum corneum removed by tape stripping. J. Biomed. Opt. 2006, 11, 054026. [Google Scholar] [CrossRef]
- Marttin, E.; Neelissen-Subnel, M.T.; De Haan, F.H.; Bodde, H.E. A critical comparison of methods to quantify stratum corneum removed by tape stripping. Skin Pharm. Off. J. Skin Pharmacol. Soc. 1996, 9, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Godin, B.; Touitou, E. Mechanism of bacitracin permeation enhancement through the skin and cellular membranes from an ethosomal carrier. J. Control. Release Off. J. Control. Release Soc. 2004, 94, 365–379. [Google Scholar] [CrossRef] [PubMed]
- Kazarian, S.G.; Chan, K.L.A. Applications of ATR-FTIR spectroscopic imaging to biomedical samples. Biochim. Biophys. Acta 2006, 1758, 858–867. [Google Scholar] [CrossRef] [PubMed]
- Morales, M.; Perez, D.; Correa, L.; Restrepo, L. Evaluation of fibrin-based dermal-epidermal organotypic cultures for in vitro skin corrosion and irritation testing of chemicals according to OECD TG 431 and 439. Toxicol. In Vitro 2016, 36, 89–96. [Google Scholar] [CrossRef]
- Negi, P.; Singh, B.; Sharma, G.; Beg, S.; Raza, K.; Katare, O.P. Phospholipid microemulsion-based hydrogel for enhanced topical delivery of lidocaine and prilocaine: QbD-based development and evaluation. Drug Deliv. 2016, 23, 951–967. [Google Scholar] [CrossRef]
- Fekrazad, R.; Barghi, V.G.; Mir, A.P.B.; Shams-Ghahfarokhi, M. In vitro photodynamic inactivation of Candida albicans by phenothiazine dye (new methylene blue) and lndocyanine green (EmunDo (R)). Photodiagnosis Photodyn. Ther. 2015, 12, 52–57. [Google Scholar] [CrossRef]
- Elshikh, M.; Ahmed, S.; Funston, S.; Dunlop, P.; McGaw, M.; Marchant, R.; Banat, I.M. Resazurin-based 96-well plate microdilution method for the determination of minimum inhibitory concentration of biosurfactants. Biotechnol. Lett. 2016, 38, 1015–1019. [Google Scholar] [CrossRef]
- Bilbao-Sainz, C.; Chiou, B.-S.; Du, W.-X.; Gregorsky, K.S.; Orts, W.J. Influence of disperse phase characteristics on stability, physical and antimicrobial properties of emulsions containing cinnamaldehyde. J. Am. Oil Chem. Soc. 2013, 90, 233–241. [Google Scholar] [CrossRef]
- Nainwal, N.; Jawla, S.; Singh, R.; Saharan, V.A. Transdermal applications of ethosomes—A detailed review. J. Liposome Res. 2019, 29, 103–113. [Google Scholar] [CrossRef]
- Wang, J.; Ma, C.; Guo, C.; Yuan, R.; Zhan, X. CTG-loaded liposomes as an approach for improving the intestinal absorption of asiaticoside in Centella Total Glucosides. Int. J. Pharm. 2016, 509, 296–304. [Google Scholar] [CrossRef]
- Liu, J.; Hu, W.; Chen, H.; Ni, Q.; Xu, H.; Yang, X. Isotretinoin-loaded solid lipid nanoparticles with skin targeting for topical delivery. Int. J. Pharm. 2007, 328, 191–195. [Google Scholar] [CrossRef] [PubMed]
- Dayan, N.; Touitou, E. Carrrers for skin delivery of trihexyphenidyl HCl: Ethosomes vs. liposmes. Biomaterials 2000, 21, 1879–1885. [Google Scholar] [CrossRef]
- Verma, P.; Pathak, K. Nanosized ethanolic vesicles loaded with econazole nitrate for the treatment of deep fungal infections through topical gel formulation. Nanomed. Nanotechnol. Biol. Med. 2012, 8, 489–496. [Google Scholar] [CrossRef]
- Verma, D.D.; Verma, S.; Blume, G.; Fahr, A. Particle size of liposomes influences dermal delivery of substance into skin. Int. J. Pharm. 2003, 258, 141–151. [Google Scholar] [CrossRef]
- Obata, Y.; Utsumi, S.; Watanabe, H.; Suda, M.; Tokudome, Y.; Otsuka, M.; Takayama, K. Infrared spectroscopic study of lipid interaction in stratum corneum treated with transdermal absorption enhancers. Int. J. Pharm. 2010, 389, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Tian, Q.; Quan, P.; Liu, C.; Fang, L. Probing the role of ion-pair strategy in controlling dexmedetomidine penetrate through drug-in-adhesive patch: Mechanistic insights based on release and percutaneous absorption process. AAPS PharmSciTech 2020, 21, 1–14. [Google Scholar] [CrossRef]
- Hertzberg, O.; Bauer, A.; Kuederle, A.; Pleitez, M.A.; Maentele, W. Depth-selective photothermal IR spectroscopy of skin: Potential application for non-invasive glucose measurement. Analyst 2017, 142, 495–502. [Google Scholar] [CrossRef]
- Yang, Y.; Ou, R.J.; Guan, S.X.; Ye, X.L.; Hu, B.; Zhang, Y.; Lu, S.F.; Zhou, Y.B.; Yuan, Z.W.; Zhang, J.; et al. A novel drug delivery gel of terbinafine hydrochloride with high penetration for external use. Drug Deliv. 2015, 22, 1086–1093. [Google Scholar] [CrossRef]
- Iizhar, S.A.; Syed, I.A.; Satar, R.; Ansari, S.A. In vitro assessment of pharmaceutical potential of ethosomes entrapped with terbinafine hydrochloride. J. Adv. Res. 2016, 7, 453–461. [Google Scholar] [CrossRef]
- Abdulbaqi, I.M.; Darwis, Y.; Khan, N.A.K.; Abou Assi, R.; Khan, A.A. Ethosomal nanocarriers: The impact of constituents and formulation techniques on ethosomal properties, in vivo studies, and clinical trials. Int. J. Nanomed. 2016, 11, 26. [Google Scholar] [CrossRef]
- Koutsoulas, C.; Pippa, N.; Demetzos, C.; Zabka, M. Preparation of liposomal nanoparticles incorporating terbinafine in vitro drug release studies. J. Nanosci. Nanotechnol. 2014, 14, 4529–4533. [Google Scholar] [CrossRef] [PubMed]
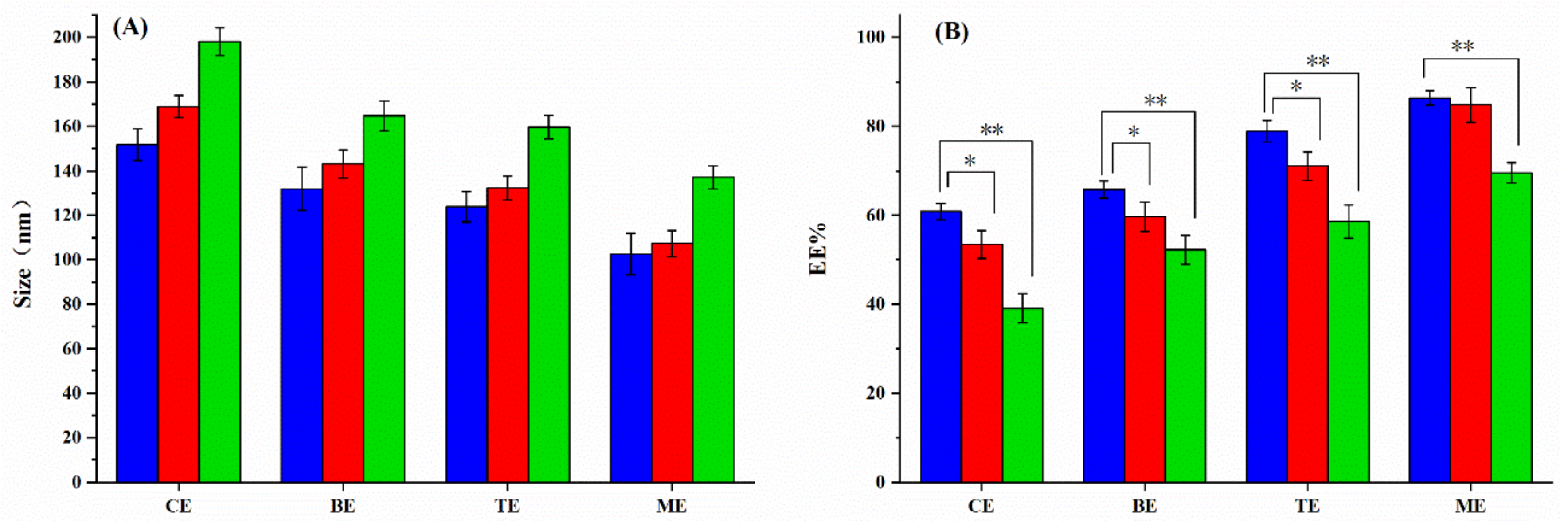
| Formulation | CA (%, w/v) | PGa (%, v/v) | Size (nm) | PDI | Zeta (mv) | EE (%) |
|---|---|---|---|---|---|---|
| ME-1 | 0.1 | 30 | 120 ± 8.2 | 0.28 ± 0.08 | −7.01 ± 1.29 | 77.6 ± 3.0 |
| ME-2 | 0.3 | 30 | 103 ± 9.3 | 0.22 ± 0.05 | −11.95 ± 1.42 | 86.4 ± 1.7 |
| ME-3 | 0.5 | 30 | 100 ± 8.9 | 0.21 ± 0.03 | −13.02 ± 1.21 | 76.3 ± 1.8 |
| BE | 0 | 30 | 132 ± 9.7 | 0.30 ± 0.05 | −5.40 ± 1.83 | 65.9 ± 1.9 |
| TE | 0.3 | 0 | 124 ± 6.9 | 0.28 ± 0.06 | −10.11 ± 1.29 | 78.9 ± 2.4 |
| CE | 0 | 0 | 152 ± 7.2 | 0.30 ± 0.04 | −10.91 ± 2.63 | 60.9 ± 1.9 |
| Groups | Score ± SD | |
|---|---|---|
| BE (group I) | Erythema | 0.50 ± 0.57 |
| Edema | 0.50 ± 0.57 | |
| ME (group II) | Erythema | 0.75 ± 0.50 |
| Edema | 0.50 ± 0.57 | |
| Lamisil® (groupIII) | Erythema | 1.75 ± 0.50 |
| Edema | 1.25 ± 0.50 | |
| PBS (group IV) | Erythema | 0.00 ± 0.00 |
| Edema | 0.00 ± 0.00 | |
| Formaline (group V) | Erythema | 2.75 ± 0.50 |
| Edema | 2.25 ± 0.50 | |
| Antifungal Agent | MIC Range, µg/mL | MIC50 (µg/mL) | MIC90 (µg/mL) |
|---|---|---|---|
| TH-DMSO | 0.125–1 | 0.25 | 1 |
| BE | 0.0312–0.25 | 0.0625 * | 0.25 * |
| ME | 0.0156–0.125 | 0.0313 ** | 0.0625 ** |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, L.; Li, X.; Zhu, S.; Zhang, T.; Maimaiti, A.; Ding, M.; Shi, S. Dermal Targeting Delivery of Terbinafine Hydrochloride Using Novel Multi-Ethosomes: A New Approach to Fungal Infection Treatment. Coatings 2020, 10, 304. https://doi.org/10.3390/coatings10040304
Zhang L, Li X, Zhu S, Zhang T, Maimaiti A, Ding M, Shi S. Dermal Targeting Delivery of Terbinafine Hydrochloride Using Novel Multi-Ethosomes: A New Approach to Fungal Infection Treatment. Coatings. 2020; 10(4):304. https://doi.org/10.3390/coatings10040304
Chicago/Turabian StyleZhang, Lijun, Xue Li, Shunyao Zhu, Ting Zhang, Aikebaier Maimaiti, Meihong Ding, and Senlin Shi. 2020. "Dermal Targeting Delivery of Terbinafine Hydrochloride Using Novel Multi-Ethosomes: A New Approach to Fungal Infection Treatment" Coatings 10, no. 4: 304. https://doi.org/10.3390/coatings10040304
APA StyleZhang, L., Li, X., Zhu, S., Zhang, T., Maimaiti, A., Ding, M., & Shi, S. (2020). Dermal Targeting Delivery of Terbinafine Hydrochloride Using Novel Multi-Ethosomes: A New Approach to Fungal Infection Treatment. Coatings, 10(4), 304. https://doi.org/10.3390/coatings10040304





