Discrepancy in Therapeutic and Prophylactic Antibiotic Prescribing in General Dentists and Maxillofacial Specialists in Australia
Abstract
1. Introduction
2. Results
2.1. Demographics
2.2. Antibiotic Prophylaxis and Antimicrobial Regimens for Surgical Procedures in Non-Medically Compromised Patients
2.2.1. Prescribing Frequency
2.2.2. Preferred Timing of Antibiotic Administration
2.2.3. Preferred Antibiotic Agent
2.2.4. Justification
2.2.5. Antiseptic Disinfection
2.3. Prophylactic Antibiotics for Medically Compromised Patients
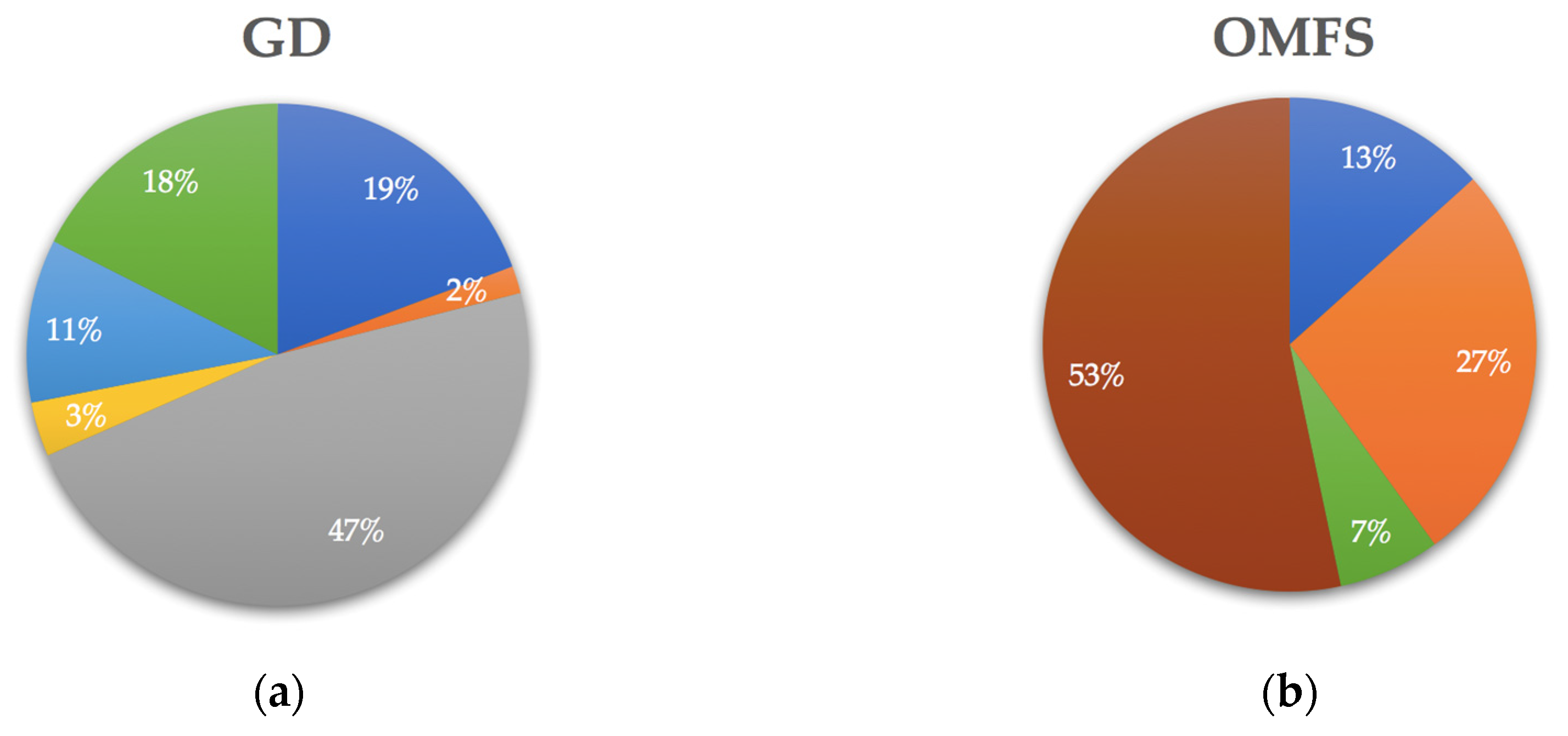
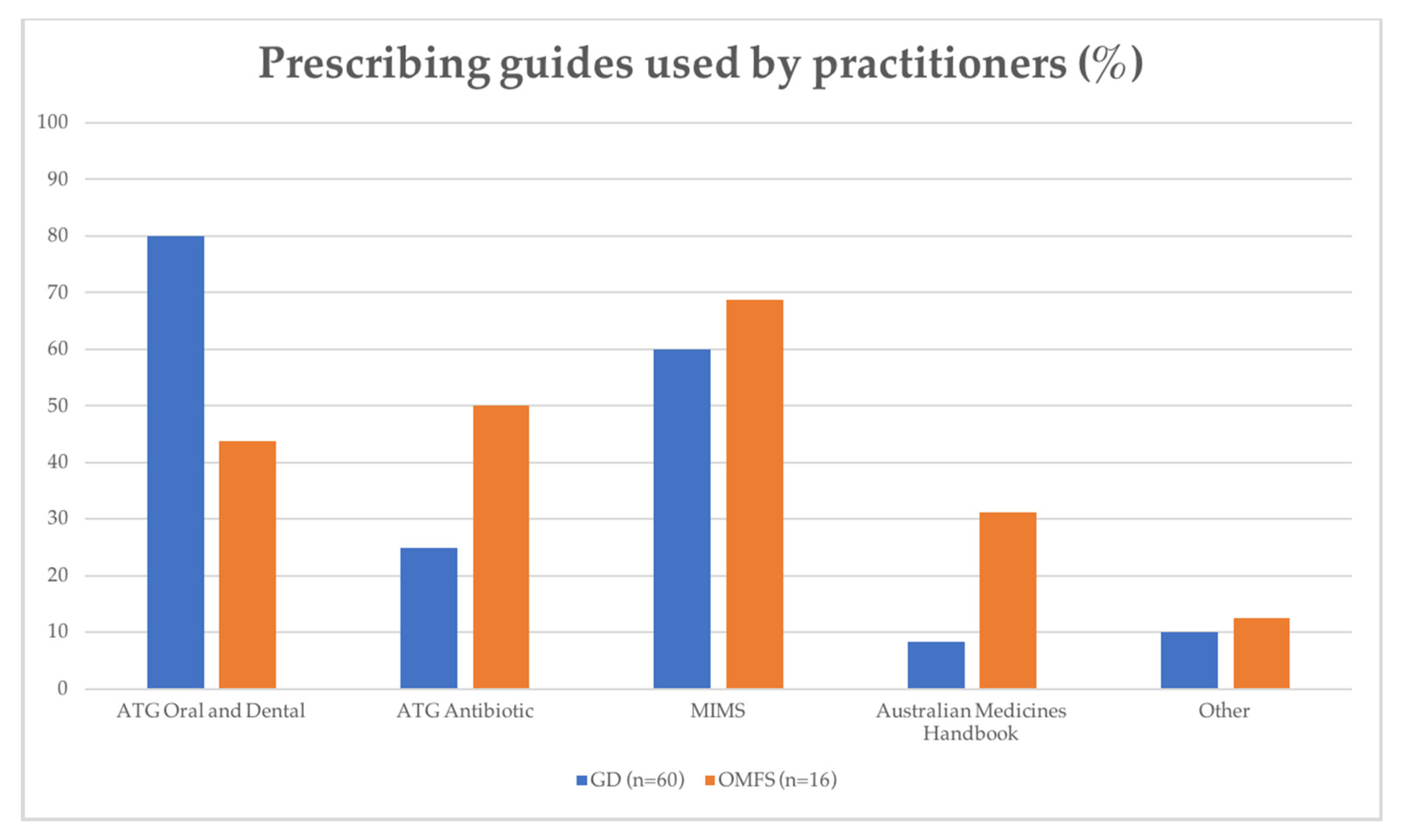
2.4. Factors Affecting Practitioners’ Prescribing Practices
2.5. Adverse Drug Reactions
3. Discussion
4. Materials and Methods
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
References
- Oberoi, S.S.; Dhingra, C.; Sharma, G.; Sardana, D. Antibiotics in dental practice: How justified are we. Int. Dent. J. 2015, 65, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Ford, P.; Saladine, C.; Zhang, K.; Hollingworth, S. Prescribing patterns of dental practitioners in Australia from 2001 to 2012. Antimicrobials. Aust. Dent. J. 2017, 62, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Merlos, A.; Vinuesa, T.; Jané-Salas, E.; López-López, J.; Viñas, M. Antimicrobial prophylaxis in dentistry. J. Glob. Antimicrob. Resist. 2014, 2, 232–238. [Google Scholar] [CrossRef] [PubMed]
- Teoh, L.; Stewart, K.; Marino, R.; McCullough, M. Antibiotic resistance and relevance to general dental practice in Australia. Aust. Dent. J. 2018, 63, 414–421. [Google Scholar] [CrossRef] [PubMed]
- Marra, F.; George, D.; Chong, M.; Sutherland, S.; Patrick, D.M. Antibiotic prescribing by dentists has increased: Why? J. Am. Dent. Assoc. 2016, 147, 320–327. [Google Scholar] [CrossRef]
- Cope, A.; Wood, F.; Francis, N.; Chestnutt, I. General dental practitioners’ perceptions of antimicrobial use and resistance: A qualitative interview study. Br. Dent. J. 2014, 217, E9. [Google Scholar] [CrossRef]
- Dar-Odeh, N.S.; Abu-Hammad, O.A.; Al-Omiri, M.K.; Khraisat, A.S.; Shehabi, A.A. Antibiotic prescribing practices by dentists: A review. Ther. Clin. Risk Manag. 2010, 6, 301–306. [Google Scholar] [CrossRef]
- Jaunay, T.; Sambrook, P.; Goss, A. Antibiotic prescribing practices by South Australian general dental practitioners. Aust. Dent. J. 2000, 45, 179–186. [Google Scholar] [CrossRef]
- Epstein, J.B.; Chong, S.; Le, N.D. A survey of antibiotic use in dentistry. J. Am. Dent. Assoc. 2000, 131, 1600–1609. [Google Scholar] [CrossRef]
- Teoh, L.; Stewart, K.; Marino, R.J.; McCullough, M.J. Current prescribing trends of antibiotics by dentists in Australia from 2013 to 2016. Part 1. Aust. Dent. J. 2018, 63, 329–337. [Google Scholar] [CrossRef]
- Sukumar, S.; Martin, F.E.; Hughes, T.E.; Adler, C.J. Think before you prescribe: How dentistry contributes to antibiotic resistance. Aust. Dent. J. 2020, 65, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Ballini, A.; Cantore, S.; Scacco, S.; Coletti, D.; Tatullo, M. Mesenchymal Stem Cells as Promoters, Enhancers, and Playmakers of the Translational Regenerative Medicine 2018. Stem Cells Int. 2018, 2018, 6927401. [Google Scholar] [CrossRef] [PubMed]
- Marrazzo, P.; Paduano, F.; Palmieri, F.; Marrelli, M.; Tatullo, M. Highly Efficient In Vitro Reparative Behaviour of Dental Pulp Stem Cells Cultured with Standardised Platelet Lysate Supplementation. Stem Cells Int. 2016, 2016, 7230987. [Google Scholar] [CrossRef] [PubMed]
- Poveda Roda, R.; Bagán Sebastián, J.V.; Sanchís Bielsa, J.M.; Carbonell Pastor, E. Antibiotic use in dental practice: A review. Med. Oral Patol. Oral Cir. Bucal 2007, 12, E186–E192. [Google Scholar]
- Park, J.; Tennant, M.; Walsh, L.; Kruger, E. Is there a consensus on antibiotic usage for dental implant placement in healthy patients? Aust. Dent. J. 2018, 63, 25–33. [Google Scholar] [CrossRef]
- Koyuncuoglu, C.; Aydin, M.; Kirmizi, N.I.; Aydin, V.; Aksoy, M.; Isli, F.; Akici, A. Rational use of medicine in dentistry: Do dentists prescribe antibiotics in appropriate indications? Eur. J. Clin. Pharmacol. 2017, 73, 1027–1032. [Google Scholar] [CrossRef]
- Segura-Egea, J.; Martin-Gonzalez, J.; Jimenez-Sanchez, M.D.; Crespo-Gallardo, I.; Sauco-Marquez, J.; Velasco-Ortega, E. Worldwide pattern of antibiotic prescription in endodontic infections. Int. Dent. J. 2017, 67, 197–205. [Google Scholar] [CrossRef]
- Halling, F.; Neff, A.; Heymann, P.; Ziebart, T. Trends in antibiotic prescribing by dental practitioners in Germany. J. Craniomaxillofac. Surg. 2017, 45, 1854–1859. [Google Scholar] [CrossRef]
- Mainjot, A.; D’hoore, W.; Vanheusden, A.; Van Nieuwenhuysen, J.P. Antibiotic prescribing in dental practice in Belgium. Int. Endo.d J. 2009, 42, 1112–1117. [Google Scholar] [CrossRef]
- Palmer, N.A.; Pealing, R.; Ireland, R.S.; Martin, M.V. A study of prophylactic antibiotic prescribing in National Health Service general dental practice in England. Br. Dent. J. 2000, 189, 43–46. [Google Scholar] [CrossRef]
- Durkin, M.J.; Hsueh, K.; Sallah, Y.H.; Feng, Q.; Jafarzadeh, S.R.; Munshi, K.D.; Lockhart, P.B.; Thornhill, M.H.; Henderson, R.R.; Fraser, V.J. An evaluation of dental antibiotic prescribing practices in the United States. J. Am. Dent. Assoc. 2017, 148, 878–886.e871. [Google Scholar] [CrossRef] [PubMed]
- Pipalova, R.; Vlcek, J.; Slezak, R. The trends in antibiotic use by general dental practitioners in the Czech Republic (2006-2012). Int. Dent. J. 2014, 64, 138–143. [Google Scholar] [CrossRef] [PubMed]
- Aragoneses, J.M.; Aragoneses, J.; Brugal, V.A.; Algar, J.; Suarez, A. Antimicrobial prescription habits of dentists performing dental implant treatments in Santo Domingo, Dominican Republic. Antibiotics 2020, 9, 376. [Google Scholar] [CrossRef] [PubMed]
- Datta, R.; Grewal, Y.; Batth, J.; Singh, A. Current trend of antimicrobial prescription for oral implant surgery among dentists in India. J. Maxillofac. Oral Surg. 2014, 13, 503–507. [Google Scholar] [CrossRef] [PubMed]
- Khalil, D.; Hultin, M.; Andersson Fred, L.; Parkbring Olsson, N.; Lund, B. Antibiotic prescription patterns among Swedish dentists working with dental implant surgery: Adherence to recommendations. Clin. Oral Implant. Res. 2015, 26, 1064–1069. [Google Scholar] [CrossRef] [PubMed]
- Deeb, G.R.; Soung, G.Y.; Best, A.M.; Laskin, D.M. Antibiotic prescribing habits of oral and maxillofacial surgeons in conjunction with routine dental implant placement. J. Oral Maxillofac. Surg. 2015, 73, 1926–1931. [Google Scholar] [CrossRef]
- Froum, S.J.; Weinberg, M.A. An evaluation of antibiotic use in periodontal and implant practices. Int. J. Periodontics Restor. Dent. 2015, 35, 481–487. [Google Scholar] [CrossRef]
- Ireland, R.S.; Palmer, N.O.; Lindenmeyer, A.; Mills, N. An investigation of antibiotic prophylaxis in implant practice in the UK. Br. Dent. J. 2012, 213, E14. [Google Scholar] [CrossRef]
- Barden, L.S.; Dowell, S.F.; Schwartz, B.; Lackey, C. Current attitudes regarding use of antimicrobial agents: Results from physician’s and parents’ focus group discussions. Clin. Pediatr. 1998, 37, 665–671. [Google Scholar] [CrossRef]
- Gonzalez-Gonzalez, C.; López-Vázquez, P.; Vázquez-Lago, J.M.; Piñeiro-Lamas, M.; Herdeiro, M.T.; Arzamendi, P.C.; Figueiras, A. Effect of physicians’ attitudes and knowledge on the quality of antibiotic prescription: A cohort study. PLoS ONE 2015, 10, e0141820. [Google Scholar] [CrossRef]
- Martin, M.; Kanatas, A.; Hardy, P. Antibiotic prophylaxis and third molar surgery. Br. Dent. J. 2005, 198, 327–330. [Google Scholar] [CrossRef] [PubMed]
- Munckhof, W. Antibiotics for surgical prophylaxis. Aust. Prescr 2005, 28, 38–40. [Google Scholar] [CrossRef]
- Rajasuo, A.; Perkki, K.; Nyfors, S.; Jousimies-Somer, H.; Meurman, J.H. Bacteremia following surgical dental extraction with an emphasis on anaerobic strains. J. Dent. Res. 2004, 83, 170–174. [Google Scholar] [CrossRef]
- Poeschl, P.W.; Eckel, D.; Poeschl, E. Postoperative prophylactic antibiotic treatment in third molar surgery—A necessity? J. Oral Maxillofac. Surg. 2004, 62, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Sekhar, C.H.; Narayanan, V.; Baig, M.F. Role of antimicrobials in third molar surgery: Prospective, double blind, randomized, placebo-controlled clinical study. J. Oral Maxillofac. Surg. 2001, 39, 134–137. [Google Scholar] [CrossRef] [PubMed]
- Barie, P.S. Modern surgical antibiotic prophylaxis and therapy--less is more. Surg. Infect. (Larchmt) 2000, 1, 23–29. [Google Scholar] [CrossRef]
- Bulut, E.; Bulut, S.; Etikan, I.; Koseoglu, O. The value of routine antibiotic prophylaxis in mandibular third molar surgery: Acute-phase protein levels as indicators of infection. J. Oral Sci. 2001, 43, 117–122. [Google Scholar] [CrossRef][Green Version]
- Barbosa, M.; Prada-López, I.; Álvarez, M.; Amaral, B.; Tomás, I. Post-tooth extraction bacteraemia: A randomized clinical trial on the efficacy of chlorhexidine prophylaxis. PLoS ONE 2015, 10, e0124249. [Google Scholar] [CrossRef]
- Spagnuolo, G.; De Vito, D.; Rengo, S.; Tatullo, M. COVID-19 Outbreak: An Overview on Dentistry. Int. J. Environ. Res. Public Health 2020, 17, 2094. [Google Scholar] [CrossRef]
- Daly, C.G. Antibiotic prophylaxis for dental procedures. Aust. Prescr. 2017, 40, 184–188. [Google Scholar] [CrossRef]
- Tong, H.J.; Hu, S.; Mok, B.Y.Y.; Islam, I.; Hong, C.H.L. Antibiotic prophylaxis prescribing practices of dentists in Singapore. Int. Dent. J. 2014, 64, 108–114. [Google Scholar] [CrossRef] [PubMed]
- Segura-Egea, J.J.; Velasco-Ortega, E.; Torres-Lagares, D.; Velasco-Ponferrada, M.C.; Monsalve-Guil, L.; Llamas-Carreras, J.M. Pattern of antibiotic prescription in the management of endodontic infections amongst Spanish oral surgeons. Int. Endod. J. 2010, 43, 342–350. [Google Scholar] [CrossRef] [PubMed]
- Oral and Dental Expert Group. Therapeutic Guidelines: Oral and Dental. Version 2; Therapeutic Guidelines Limited: Melbourne, MEL, Australia, 2012. [Google Scholar]
- Oral and Dental Expert Group. Therapeutic Guidelines: Oral and Dental. Version 3; Therapeutic Guidelines Limited: Melbourne, MEL, Australia, 2019. [Google Scholar]
- Antibiotic Expert Group. Therapeutic Guidelines: Antibiotic. Version 15; Therapeutic Guidelines Limited: Melbourne, MEL, Australia, 2014. [Google Scholar]
- The Dental Directory: 2016 Edition; Australian Dental Association: St Leonards, NSW, Australia, 2016.
| Characteristics | All | GDs | OMFSs | Significance (p Value) 3 |
|---|---|---|---|---|
| (n = 77) | (n = 60) | (n = 17) 1 | ||
| Primary dental degree | ||||
| Graduation (year) 2 | - | |||
| Mean | 1990.1 | 1992.6 | 1981.6 | |
| SD | 13.1 | 12.4 | 12.5 | |
| Range | 1659–2015 | 1964–2014 | 1959–1998 | |
| Obtained in Australia, n (%) | p > 0.05 | |||
| Yes | 69 (89.6) | 55 (91.7) | 14 (82.4) | |
| No | 8 (10.4) | 5 (8.3) | 3 (17.7) | |
| Specialist experience | ||||
| Years of practice experience as a specialist (years) | - | - | - | |
| Mean | 23 | |||
| SD | 12.5 | |||
| Range | 5–23 | |||
| Workplace environment | ||||
| Private sector only | 71 (79.2) | 55 (91.7) | 6 (35.3) | p < 0.001 |
| Public sector only | 3 (3.9) | 3 (5.0) | 0 (0.0) | |
| Both private and public | 2 (2.6) | 2 (3.3) | 11 (64.7) |
| Procedure | Respondent Type | Disinfection of Oral Cavity (%) | Prescribed Antibiotics (%) | Most Frequent Timing of Antibiotic Administration | Most Frequently Prescribed Antibiotic Agent | |
|---|---|---|---|---|---|---|
| Third molar surgical extraction | Total | n = 69 | 49.3 | 33.3 | Postoperative only 60.9% | Amoxicillin only 78.3% |
| GDs | n = 51 | 43.1 | 23.5 1 | |||
| OMFSs | n = 18 | 66.7 | 61.1 1 | |||
| Single implant placement | Total | n = 47 | 87.2 | 66.0 | Postoperative only 38.7% | Amoxicillin only 77.4% |
| GDs | n = 29 | 93.1 | 62.1 | |||
| OMFSs | n = 18 | 77.8 | 72.2 | |||
| Procedure | Respondent Type | Preferred Timing of Antibiotic Administration (%) | |||||
|---|---|---|---|---|---|---|---|
| Preoperative Only | Perioperative Only | Postoperative Only | Pre- and Postoperative | Peri- and Postoperative | |||
| Third molar surgical extraction | Total | n = 23 | 21.7 | 4.2 | 60.9 | 4.3 | 8.7 |
| GDs | n = 12 | 9.1 | 9.1 | 63.6 | 9.1 | 9.1 | |
| OMFSs | n = 11 | 33.3 | 0.0 | 58.3 | 0.0 | 8.3 | |
| Single implant placement | Total | n = 31 | 25.8 | 9.7 | 38.7 | 12.9 | 12.9 |
| GDs | n = 18 | 15.4 | 15.4 | 46.2 | 7.7 | 15.4 | |
| OMFSs | n = 13 | 33.3 | 5.6 | 33.3 | 16.7 | 11.1 | |
| Procedure | Respondent Type | Preferred Antibiotic Agent/s (%) | |||||
|---|---|---|---|---|---|---|---|
| Amoxicillin Only | Phenoxymethylpenicillin Only | Cephalexin Only | Metronidazole Plus Amoxicillin | Amoxicillin/Clavulanic Acid | |||
| Third molar surgical extraction | Total | n = 23 | 78.3 | 8.7 | 4.3 | 4.3 | 0.0 |
| GDs 1 | n = 12 | 75 | 8.3 | 0.0 | 8.3 | 0.0 | |
| OMFSs | n = 11 | 81.8 | 9.1 | 9.2 | 0.0 | 0.0 | |
| Single implant placement | Total | n = 31 | 77.4 | 0.0 | 6.5 | 9.7 | 6.5 |
| GDs | n = 18 | 83.3 | 0.0 | 5.6 | 11.1 | 0.0 | |
| OMFSs | n = 13 | 69.2 | 7.7 | 7.7 | 7.7 | 15.4 | |
| Medical History | Third Molar Surgical Extraction | Single Implant Placement | ||
|---|---|---|---|---|
| % of practitioners providing antibiotic prophylaxis for the procedures listed | ||||
| GDs (n = 50) | OMFSs (n = 18) | GDs (n = 27) | OMFSs (n = 17) | |
| Patients on oral anticoagulants or platelet inhibitors | 4.0 | 5.6 | 11.1 | 17.7 |
| HIV positive | 24.0 1 | 55.6 1 | 37.0 | 47.1 |
| History of injecting drug use | 8.0 2 | 38.9 2 | 14.8 | 41.2 |
| Chronic hepatitis B or C | 14.0 | 33.3 | 22.2 | 41.2 |
| Uncontrolled diabetes mellitus | 56.0 3 | 100.0 3 | 63.0 2 | 100.0 2 |
| Cardiac valve replacement or mitral valve prolapse | 92.0 | 83.3 | 85.2 | 88.2 |
| Prosthetic joint in past two years | 48.0 | 72.2 | 59.3 | 76.5 |
| History of head and neck cancer and radiotherapy | 48.0 | 55.6 | 48.2 | 64.7 |
| Oral bisphosphonate therapy for the past three years | 66.0 | 83.3 | 63.0 | 82.4 |
| History of intravenous bisphosphonate therapy | 68.0 | 88.9 | 55.6 1 | 88.2 1 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, C.; Gilpin, N.; Walsh, L. Discrepancy in Therapeutic and Prophylactic Antibiotic Prescribing in General Dentists and Maxillofacial Specialists in Australia. Antibiotics 2020, 9, 492. https://doi.org/10.3390/antibiotics9080492
Chen C, Gilpin N, Walsh L. Discrepancy in Therapeutic and Prophylactic Antibiotic Prescribing in General Dentists and Maxillofacial Specialists in Australia. Antibiotics. 2020; 9(8):492. https://doi.org/10.3390/antibiotics9080492
Chicago/Turabian StyleChen, Cheryl, Nicole Gilpin, and Laurence Walsh. 2020. "Discrepancy in Therapeutic and Prophylactic Antibiotic Prescribing in General Dentists and Maxillofacial Specialists in Australia" Antibiotics 9, no. 8: 492. https://doi.org/10.3390/antibiotics9080492
APA StyleChen, C., Gilpin, N., & Walsh, L. (2020). Discrepancy in Therapeutic and Prophylactic Antibiotic Prescribing in General Dentists and Maxillofacial Specialists in Australia. Antibiotics, 9(8), 492. https://doi.org/10.3390/antibiotics9080492







