Prescriber Commitment Posters to Increase Prudent Antibiotic Prescribing in English General Practice: A Cluster Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
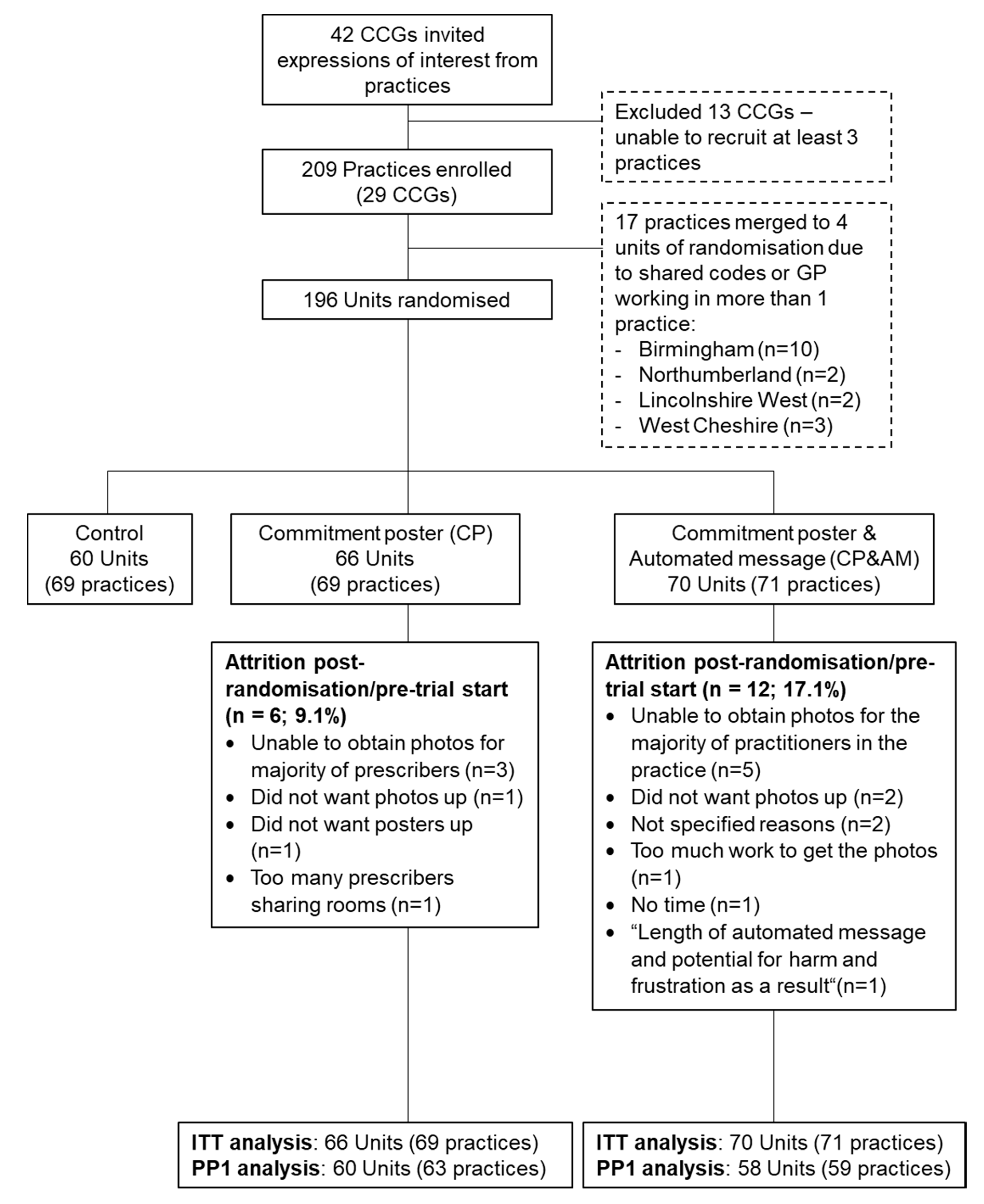
2.1. Study Design, Participants, and Setting
2.2. Randomization
2.3. Procedure and Interventions
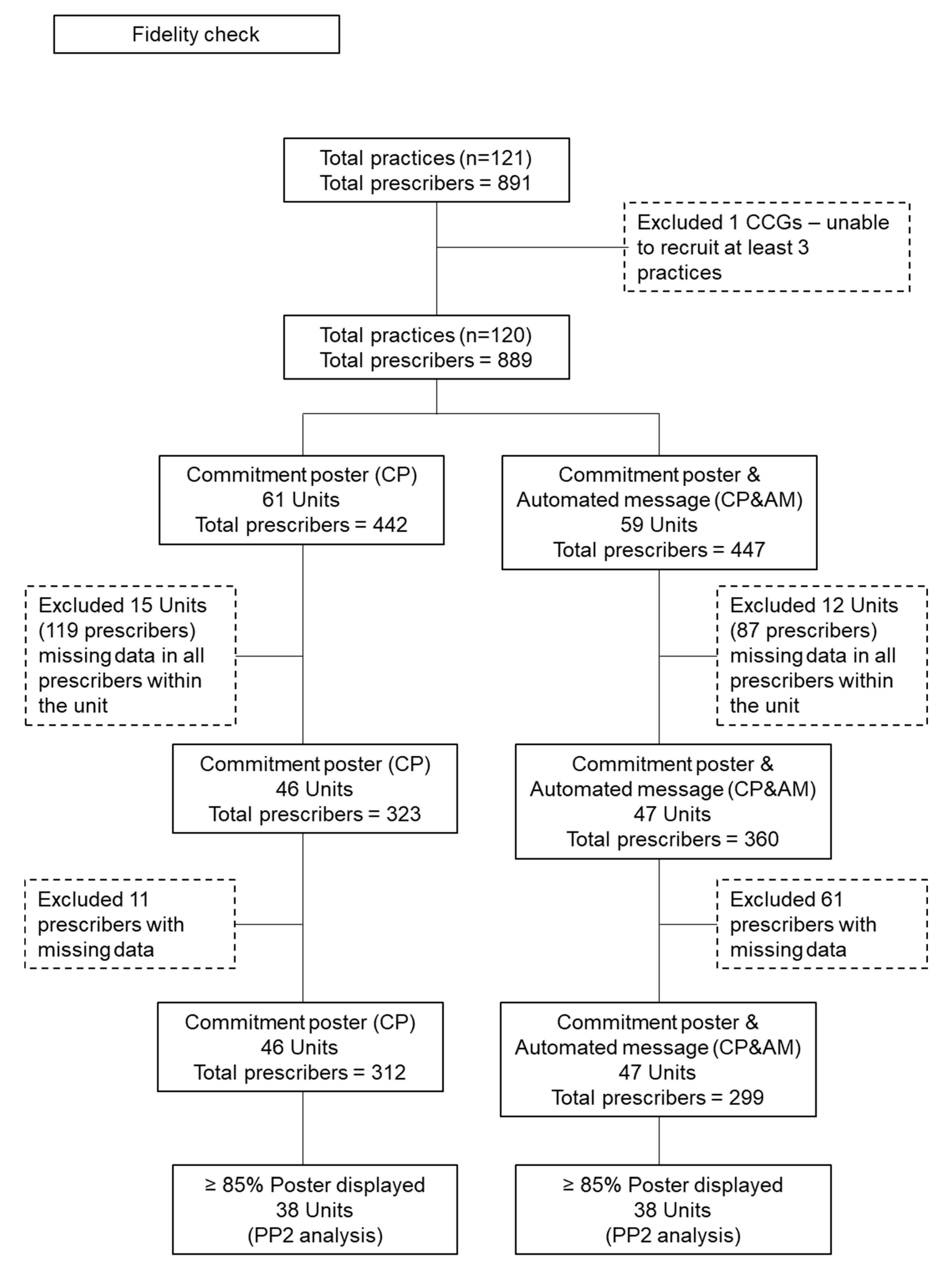
2.4. Fidelity Checks
2.5. Data Collection and Outcome Measures
2.6. Power Calculation
2.7. Statistical Analysis
3. Results
3.1. Fidelity Checks
3.2. Overall Effect of Interventions Compared to the Control
3.3. Effect of Interventions on Antibiotics Commonly Prescribed for URTI and Broad Spectrum Prescribing
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Ethical Statement
Availability of Data and Materials
Abbreviations
| AM | Antimicrobial stewardship message |
| AMR | Antimicrobial resistance |
| BCT-T V1 | Behaviour Change Technique Taxonomy Version 1 |
| CCG | Clinical Commissioning Groups |
| CP | Commitment poster |
| MDES | Minimum detectable effect size |
| PHE | Public Health England |
| PHEBI | Public Health England Behavioural Insights |
| URTI | Upper respiratory tract infections |
References
- World Health Organisation. Antibiotic Resistance. Available online: http://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance (accessed on 13 May 2020).
- Cassini, A.; Högberg, L.D.; Plachouras, D.; Quattrocchi, A.; Hoxha, A.; Simonsen, G.S.; Colomb-Cotinat, M.; Kretzschmar, M.E.; Devleesschauwer, B.; Cecchini, M.; et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: A population-level modelling analysis. Lancet Infect. Dis. 2019, 19, 56–66. [Google Scholar] [CrossRef]
- O’Neill, J. Tackling Drug-Resistant Infections Globally: Final Report and Recommendations; Review on Antimicrobial Resistance: London, UK, 2016. [Google Scholar]
- Laxminarayan, R.; Duse, A.; Wattal, C.; Zaidi, A.K.M.; Wertheim, H.; Sumpradit, N.; Vlieghe, E.; Hara, G.L.; Gould, I.M.; Goossens, H.; et al. Antibiotic resistance—The need for global solutions. Lancet Infect. Dis. 2013, 13, 1057–1098. [Google Scholar] [CrossRef]
- Chatterjee, A.; Modarai, M.; Naylor, N.R.; Boyd, S.E.; Atun, R.; Barlow, J.; Holmes, A.H.; Johnson, A.; Robotham, J.V. Quantifying drivers of antibiotic resistance in humans: A systematic review. Lancet Infect. 2018, 18, e368–e378. [Google Scholar] [CrossRef]
- Goossens, H.; Ferech, M.; Vander Stichele, R.; Elseviers, M.; ESAC Project Group. Outpatient antibiotic use in Europe and association with resistance: A cross-national database study. Lancet 2005, 365, 579–587. [Google Scholar] [CrossRef]
- England, P.H. English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR); PHE Publications: London, UK, 2018. [Google Scholar]
- Dolk, F.C.K.; Pouwels, K.B.; Smith, D.R.; Robotham, J.V.; Smieszek, T. Antibiotics in primary care in England: Which antibiotics are prescribed and for which conditions? J. Antimicrob. Chemother. 2018, 73, ii2–ii10. [Google Scholar] [CrossRef] [PubMed]
- Fleming-Dutra, K.E.; Hersh, A.L.; Shapiro, D.J.; Bartoces, M.; Enns, E.A.; File, T.M.; Finkelstein, J.A.; Gerber, J.S.; Hyun, D.Y.; Linder, J.A.; et al. Prevalence of inappropriate antibiotic prescriptions among US ambulatory care visits, 2010–2011. JAMA 2016, 315, 1864–1873. [Google Scholar] [CrossRef] [PubMed]
- Smieszek, T.; Pouwels, K.B.; Dolk, F.C.K.; Smith, D.R.; Hopkins, S.; Sharland, M.; Hay, A.D.; Moore, M.V.; Robotham, J.V. Potential for reducing inappropriate antibiotic prescribing in English primary care. J. Antimicrob. Chemother. 2018, 73, ii36–ii43. [Google Scholar] [CrossRef]
- Fredericks, I.; Hollingworth, S.; Pudmenzky, A.; Rossato, L.; Syed, S.; Kairuz, T. Consumer knowledge and perceptions about antibiotics and upper respiratory tract infections in a community pharmacy. Int. J. Clin. Pharm. 2015, 37, 1213–1221. [Google Scholar] [CrossRef]
- McDermott, L.; Leydon, G.M.; Halls, A.; Kelly, J.; Nagle, A.; White, J.; Little, P. Qualitative interview study of antibiotics and self-management strategies for respiratory infections in primary care. BMJ Open 2017, 7, e016903. [Google Scholar]
- European Commission. Special Eurobarometer 478—November 2018. Antimicrobial Resistance. Available online: https://data.europa.eu/euodp/en/data/dataset/S2190_90_1_478_ENG (accessed on 12 May 2020).
- Godycki-Ćwirko, M.; Cals, J.W.C.; Francis, N.; Verheij, T.; Butler, C.; Goossens, H.; Zakowska, I.; Panasiuk, L. Public Beliefs on Antibiotics and Symptoms of Respiratory Tract Infections among Rural and Urban Population in Poland: A Questionnaire Study. PLoS ONE 2014, 9, e109248. [Google Scholar]
- Fletcher-Lartey, S.; Yee, M.; Gaarslev, C.; Khan, R. Why do general practitioners prescribe antibiotics for upper respiratory tract infections to meet patient expectations: A mixed methods study. BMJ Open 2016, 6, 012244. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, R.; O’Doherty, J.; O’Regan, A.; Dunne, C.P. Antibiotic use for acute respiratory tract infections (ARTI) in primary care; what factors affect prescribing and why is it important? A narrative review. Ir. J. Med. Sci. 2018, 187, 969–986. [Google Scholar] [CrossRef] [PubMed]
- Kianmehr, H.; Sabounchi, N.S.; Sabounchi, S.S.; Cosler, L.E.; Sabounchi, S.S. Patient expectation trends on receiving antibiotic prescriptions for respiratory tract infections: A systematic review and meta-regression analysis. Int. J. Clin. Pr. 2019, 73, e13360. [Google Scholar] [CrossRef] [PubMed]
- McParland, J.L.; Williams, L.; Gozdzielewska, L.; Young, M.; Smith, F.; MacDonald, J.; Langdridge, D.; Davis, M.; Price, L.; Flowers, P. What are the ‘active ingredients’ of interventions targeting the public’s engagement with antimicrobial resistance and how might they work? Br. J. Health Psychol. 2018, 23, 804–819. [Google Scholar] [CrossRef]
- Haynes, C.; McLeod, C. A Review of Reviews of Educational Interventions Designed to Change the Public’s Knowledge and Behaviour in Relation to Antimicrobial Use and Antimicrobial Resistance That Target Healthcare Professionals and Patients; NICE: London, UK.
- Pinder, R.; Sallis, A.; Berry, D.; Chadborn, T. Behaviour Change and Antibiotic Prescribing in Healthcare Settings. Literature Review and Behavioural Analysis; Public Health England: London, UK, 2015. [Google Scholar]
- Huttner, B.; Saam, M.; Moja, L.; Mah, K.; Sprenger, M.; Harbarth, S.; Magrini, N. How to improve antibiotic awareness campaigns: Findings of a WHO global survey. BMJ Glob. Heal. 2019, 4, e001239. [Google Scholar] [CrossRef]
- Fletcher-Miles, H.; Gammon, J.; Williams, S.; Hunt, J. A scoping review to assess the impact of public education campaigns to affect behavior change pertaining to antimicrobial resistance. Am. J. Infect. Control 2020, 48, 433–442. [Google Scholar] [CrossRef]
- King, S.; Exley, J.; Taylor, J.; Kruithof, K.; Larkin, J.; Pardal, M. Antimicrobial stewardship: The effectiveness of educational interventions to change risk-related behaviours in the general population: A systematic review. Rand Health Q. 2016, 5, 2. [Google Scholar]
- Lawrence, C.; Ferguson, E. Public health messages about antibiotic treatment for respiratory tract infection may increase perceived symptom severity reporting. J. Health. Psychol. 2016, 24, 623–627. [Google Scholar] [CrossRef]
- Charani, E.; Castro-Sánchez, E.; Holmes, A. The Role of Behavior Change in Antimicrobial Stewardship. Infect. Dis. Clin. N. Am. 2014, 28, 169–175. [Google Scholar] [CrossRef]
- Meeker, D.; Knight, T.K.; Friedberg, M.; Linder, J.; Goldstein, N.J.; Fox, C.R.; Rothfeld, A.; Díaz, G.; Doctor, J.N. Nudging guideline-concordant antibiotic prescribing: A randomized clinical trial. JAMA Intern. Med. 2014, 174, 425–431. [Google Scholar] [CrossRef]
- Meeker, D.; Linder, J.; Fox, C.R.; Friedberg, M.; Persell, S.D.; Goldstein, N.J.; Knight, T.K.; Hay, J.W.; Doctor, J.N. Effect of Behavioral Interventions on Inappropriate Antibiotic Prescribing Among Primary Care Practices: A Randomized Clinical Trial. JAMA 2016, 315, 562–570. [Google Scholar] [CrossRef] [PubMed]
- Hallsworth, M.; Chadborn, T.; Sallis, A.; Sanders, M.; Berry, D.; Greaves, F.; Clements, L.; Davies, S.C. Provision of social norm feedback to high prescribers of antibiotics in general practice: A pragmatic national randomised controlled trial. Lancet 2016, 387, 1743–1752. [Google Scholar] [CrossRef]
- Butler, C.; Simpson, S.A.; Dunstan, F.; Rollnick, S.; Cohen, D.; Gillespie, D.; Evans, M.; Alam, M.F.; Bekkers, M.-J.; Moore, L.; et al. Effectiveness of multifaceted educational programme to reduce antibiotic dispensing in primary care: Practice based randomised controlled trial. BMJ 2012, 344, d8173. [Google Scholar] [CrossRef] [PubMed]
- Little, P.; Stuart, B.; Francis, N.; Douglas, E.; Tonkin-Crine, S.; Anthierens, S.; Cals, J.W.L.; Melbye, H.; Santer, M.; Moore, M.; et al. Effects of internet-based training on antibiotic prescribing rates for acute respiratory-tract infections: A multinational, cluster, randomised, factorial, controlled trial. Lancet 2013, 382, 1175–1182. [Google Scholar] [CrossRef]
- Cals, J.; Ament, A.J.H.A.; Hood, K.; Butler, C.; Hopstaken, R.; Wassink, G.F.; Dinant, G.-J. C-reactive protein point of care testing and physician communication skills training for lower respiratory tract infections in general practice: Economic evaluation of a cluster randomized trial. J. Eval. Clin. Pr. 2010, 17, 1059–1069. [Google Scholar] [CrossRef]
- Pallak, M.S.; Cook, D.A.; Sullivan, J.J. Commitment and energy conservation. Appl. Soc. Psychol. Annu. 1980, 1, 235–253. [Google Scholar]
- Cialdini, R.B. The Science of Persuasion. Sci. Am. 2001, 284, 76–81. [Google Scholar] [CrossRef]
- Baca-Motes, K.; Brown, A.; Gneezy, A.; Keenan, E.A.; Nelson, L.D. Commitment and Behavior Change: Evidence from the Field. J. Consum. Res. 2013, 39, 1070–1084. [Google Scholar] [CrossRef]
- Kerr, J.; Eves, F.F.; Carroll, U. The influence of poster prompts on stair use: The effects of setting, poster size and content. Br. J. Health Psychol. 2001, 6, 397–405. [Google Scholar] [CrossRef]
- AntibioticGuardian.com. Antibiotic Guardian. Available online: https://antibioticguardian.com/ (accessed on 1 October 2019).
- NHS Business Authority. Available online: https://www.nhsbsa.nhs.uk/ (accessed on 1 January 2018).
- Cioffi, D.; Garner, R. On Doing the Decision: Effects of Active versus Passive Choice on Commitment and Self-Perception. Pers. Soc. Psychol. Bull. 1996, 22, 133–147. [Google Scholar] [CrossRef]
- Allison, S.T.; Messick, D.M. The Feature-Positive Effect, Attitude Strength, and Degree of Perceived Consensus. Pers. Soc. Psychol. Bull. 1988, 14, 231–241. [Google Scholar] [CrossRef] [PubMed]
- Cialdini, R.B.; Cacioppo, J.T.; Bassett, R.; Miller, J.A. Low-ball procedure for producing compliance: Commitment then cost. J. Personal. Soc. Psychol. 1978, 36, 463. [Google Scholar] [CrossRef]
- Germeni, E.; Frost, J.; Garside, R.; Rogers, M.; Valderas, J.M.; Britten, N. Antibiotic prescribing for acute respiratory tract infections in primary care: An updated and expanded meta-ethnography. Br. J. Gen. Pr. 2018, 68, e633–e645. [Google Scholar] [CrossRef] [PubMed]
- Ashdown, H.F.; Räisänen, U.; Wang, K.; Ziebland, S.; Harnden, A. Prescribing antibiotics to ‘at-risk’ children with influenza-like illness in primary care: Qualitative study. BMJ Open 2016, 6, e011497. [Google Scholar] [CrossRef] [PubMed]
- Cabral, C.; Ingram, J.; Lucas, P.J.; Redmond, N.M.; Kai, J.; Hay, A.D.; Horwood, J. Influence of Clinical Communication on Parents’ Antibiotic Expectations for Children With Respiratory Tract Infections. Ann. Fam. Med. 2016, 14, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, A.T.; Roque, F.; Falcão, A.; Figueiras, A.; Herdeiro, M.T. Understanding physician antibiotic prescribing behaviour: A systematic review of qualitative studies. Int. J. Antimicrob. Agents 2013, 41, 203–212. [Google Scholar] [CrossRef]
- Tonkin-Crine, S.; Yardley, L.; Little, P. Antibiotic prescribing for acute respiratory tract infections in primary care: A systematic review and meta-ethnography. J. Antimicrob. Chemother. 2011, 66, 2215–2223. [Google Scholar] [CrossRef]
- Chattopadhyay, A.; Mondal, T.; Saha, T.K.; Dey, I.; Sahu, B.K.; Bhattacharya, J. An audit of prescribing practices in CGHS dispensaries of Kolkata, India. IOSR J Dent. Med. Sci. 2013, 8, 32–37. [Google Scholar] [CrossRef]
- Jin, G.; Zhao, Y.; Chen, C.; Wang, W.; Du, J.; Lu, X. The Length and Content of General Practice Consultation in Two Urban Districts of Beijing: A Preliminary Observation Study. PLoS ONE 2015, 10, e0135121. [Google Scholar] [CrossRef]
- Nizami, S.; Khan, I.; Bhutta, Z. Drug prescribing practices of general practitioners and paediatricians for childhood diarrhoea in Karachi, Pakistan. Soc. Sci. Med. 1996, 42, 1133–1139. [Google Scholar] [CrossRef]
- Sheeran, P.; Gollwitzer, P.M.; Bargh, J.A. Nonconscious processes and health. Heal. Psychol. 2013, 32, 460–473. [Google Scholar] [CrossRef] [PubMed]
- Presseau, J.; Johnston, M.; Heponiemi, T.; Elovainio, M.; Francis, J.J.; Eccles, M.P.; Steen, N.; Hrisos, S.; Stamp, E.; Grimshaw, J.M.; et al. Reflective and Automatic Processes in Health Care Professional Behaviour: A Dual Process Model Tested Across Multiple Behaviours. Ann. Behav. Med. 2014, 48, 347–358. [Google Scholar] [CrossRef] [PubMed]
- Nilsen, P.; Roback, K.; Broström, A.; Ellström, P.-E. Creatures of habit: Accounting for the role of habit in implementation research on clinical behaviour change. Implement. Sci. 2012, 7, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Potthoff, S.; Presseau, J.; Sniehotta, F.F.; Johnston, M.; Elovainio, M.; Avery, L. Planning to be routine: Habit as a mediator of the planning-behaviour relationship in healthcare professionals. Implement. Sci. 2017, 12, 24. [Google Scholar] [CrossRef] [PubMed]
- Centre for Disease Control. A Commitment to Our Patients about Antibiotics. Available online: https://www.cdc.gov/antibiotic-use/community/downloads/A-Commitment-to-Our-Patients-about-Antibiotics-poster-version-1.pdf (accessed on 18 April 2020).
- Centre for Disease Control. Antibiotic Prescribing and Use in Doctor’s Offices. Available online: https://www.cdc.gov/antibiotic-use/community/index.html (accessed on 18 April 2020).
- Zanichelli, V.; Tebano, G.; Gyssens, I.; Vlahović-Palčevski, V.; Monnier, A.A.; Benić, M.S.; Harbarth, S.; Hulscher, M.; Pulcini, C.; Huttner, B.D. Patient-related determinants of antibiotic use: A systematic review. Clin. Microbiol. Infect. 2019, 25, 48–53. [Google Scholar] [CrossRef] [PubMed]
| Prescribing Rate per 1000 Population a | Coefficient (β1) | Robust Standard Error | p-Value | 95% C.I. |
|---|---|---|---|---|
| Commitment poster | 5.67 | 7.54 | 0.46 | −9.77 to 21.11 |
| Baseline prescribing rate | 0.78 | 0.03 | <0.001 | 0.71 to 0.84 |
| Practice population b | 0.01 | 0.00 | <0.001 | 0.00 to 0.01 |
| Number of GPs c | −0.67 | 0.43 | 0.13 | −1.55 to 0.22 |
| February (reference) | - | - | - | - |
| March | 32.54 | 4.13 | <0.001 | 24.09 to 40.99 |
| April | −24.16 | 3.06 | <0.001 | −30.43 to −17.88 |
| May | −62.63 | 4.80 | <0.001 | −72.47 to −52.79 |
| June | −59.80 | 4.18 | <0.001 | −68.36 to −51.25 |
| July | −58.35 | 3.69 | <0.001 | −65.91 to −50.80 |
| Year 2016 (reference 2015) | 22.60 | 6.77 | 0.00 | 8.74 to 36.46 |
| Prescribing Rate per 1000 Population | Coefficient (β1) | Robust Standard Error | p-Value | 95% C.I. |
|---|---|---|---|---|
| Commitment poster and automated message a | −12.58 | 8.86 | 0.17 | −30.73 to 5.58 |
| Baseline prescribing rate | 0.75 | 0.05 | <0.001 | 0.64 to 0.86 |
| Practice population b | 0.01 | 0.00 | 0.01 | 0.00 to 0.01 |
| Number of GPs c | −0.29 | 0.68 | 0.68 | −1.68 to 1.10 |
| February (reference) | - | - | - | - |
| March | 33.66 | 3.83 | <0.001 | 25.81 to 41.50 |
| April | −25.80 | 3.92 | <0.001 | −33.83 to −17.77 |
| May | −67.17 | 4.16 | <0.001 | −75.68 to −58.65 |
| June | −58.82 | 4.03 | <0.001 | −67.07 to −50.57 |
| July | −58.69 | 4.25 | <0.001 | −67.38 to −49.99 |
| Year 2016 (reference 2015) | 23.71 | 7.38 | 0.00 | 8.60 to 38.83 |
| Prescribing Rate per 1000 Population a | Coef. (β1) | Robust Standard Error | p-Value | 95% C.I. |
|---|---|---|---|---|
| Commitment Poster | 5.90 | 7.21 | 0.42 | −8.86 to 20.67 |
| Intervention: Automated message a | −18.444 | 6.91 | 0.01 | −32.60 to −4.29 |
| Baseline prescribing rate | 0.77 | 0.03 | <0.001 | 0.70 to 0.82 |
| Practice population b | 0.01 | 0.00 | 0.00 | 0.00 to 0.01 |
| Number of GPs c | −0.13 | 0.35 | 0.72 | −0.85 to 0.59 |
| February (reference) | - | - | - | - |
| March | 31.87 | 3.07 | <0.001 | 25.59 to 38.15 |
| April | −26.74 | 3.11 | <0.001 | −33.10 to −20.38 |
| May | −65.71 | 4.00 | <0.001 | −73.90 to −57.52 |
| June | −60.30 | 3.55 | <0.001 | −67.58 to −53.02 |
| July | −60.14 | 3.49 | <0.001 | −67.30 to −52.99 |
| Year 2016 (reference 2015) | 22.24 | 7.12 | 0.00 | 7.64 to 36.82 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sallis, A.; Bondaronek, P.; Sanders, J.G.; Yu, L.-M.; Harris, V.; Vlaev, I.; Sanders, M.; Tonkin-Crine, S.; Chadborn, T. Prescriber Commitment Posters to Increase Prudent Antibiotic Prescribing in English General Practice: A Cluster Randomized Controlled Trial. Antibiotics 2020, 9, 490. https://doi.org/10.3390/antibiotics9080490
Sallis A, Bondaronek P, Sanders JG, Yu L-M, Harris V, Vlaev I, Sanders M, Tonkin-Crine S, Chadborn T. Prescriber Commitment Posters to Increase Prudent Antibiotic Prescribing in English General Practice: A Cluster Randomized Controlled Trial. Antibiotics. 2020; 9(8):490. https://doi.org/10.3390/antibiotics9080490
Chicago/Turabian StyleSallis, Anna, Paulina Bondaronek, Jet G. Sanders, Ly-Mee Yu, Victoria Harris, Ivo Vlaev, Michael Sanders, Sarah Tonkin-Crine, and Tim Chadborn. 2020. "Prescriber Commitment Posters to Increase Prudent Antibiotic Prescribing in English General Practice: A Cluster Randomized Controlled Trial" Antibiotics 9, no. 8: 490. https://doi.org/10.3390/antibiotics9080490
APA StyleSallis, A., Bondaronek, P., Sanders, J. G., Yu, L.-M., Harris, V., Vlaev, I., Sanders, M., Tonkin-Crine, S., & Chadborn, T. (2020). Prescriber Commitment Posters to Increase Prudent Antibiotic Prescribing in English General Practice: A Cluster Randomized Controlled Trial. Antibiotics, 9(8), 490. https://doi.org/10.3390/antibiotics9080490





