Spectrum and Antibiotic Resistance of Uropathogens in Romanian Females
Abstract
1. Introduction
2. Results
3. Discussion
3.1. The Importance of Presenting Population Specific AMR Reports
3.2. Differences and Trends Regarding the Prevalence of Uropathogens
3.3. Antimicrobial Resistance in Relation to Patient Age
3.4. Comparison of Resistance Pattern for E. coli with Other Studies
3.5. Rationale for Reporting Gender-Specific Uropathogens AMR
3.6. Empiric Antibiotic Treatment in Female UTIs
3.7. Limitations
4. Materials and Methods
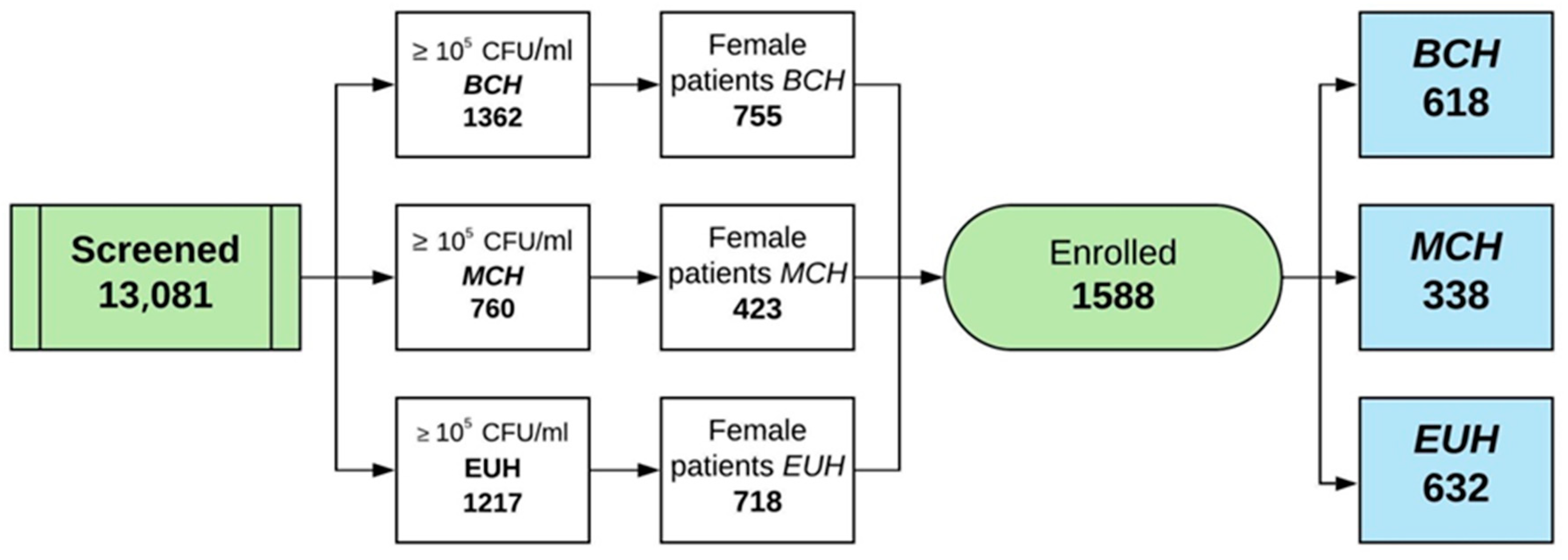
4.1. Study Design and Sample Population
4.2. Inclusion and Exclusion Criteria
- Positive uroculture ≥105 CFU/mL;
- Single bacteria strain on uroculture;
- Female patients;
- Age ≥18 years.
- Uroculture <105 CFU/mL;
- Multiple bacteria strain on uroculture;
- Presence of a urological catheter.
4.3. Antibiotics Policy in UTIs in Study Centers
4.4. Sample Collection, Bacterial Culture, and Identification
4.5. Antibiotic Susceptibility Test
4.6. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Medina, M.; Castillo-Pino, E. An introduction to the epidemiology and burden of urinary tract infections. Ther. Adv. Urol. 2019, 11, 1756287219832172. [Google Scholar] [CrossRef]
- Gupta, K.; Hooton, T.M.; Stamm, W.E. Increasing antimicrobial resistance and the management of uncomplicated community-acquired urinary tract infections. Ann. Intern. Med. 2001, 135, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Stamm, W.E.; Norrby, S.R. Urinary tract infections: Disease panorama and challenges. J. Infect. Dis. 2001, 183 (Suppl. 1), S1–S4. [Google Scholar] [CrossRef] [PubMed]
- Flores-Mireles, A.L.; Walker, J.N.; Caparon, M.; Hultgren, S.J. Urinary tract infections: Epidemiology, mechanisms of infection and treatment options. Nat. Rev. Microbiol. 2015, 13, 269–284. [Google Scholar] [CrossRef] [PubMed]
- Tandogdu, Z.; Wagenlehner, F.M. Global epidemiology of urinary tract infections. Curr. Opin. Infect. Dis. 2016, 29, 73–79. [Google Scholar] [CrossRef]
- Schmiemann, G.; Kniehl, E.; Gebhardt, K.; Matejczyk, M.M.; Hummers-Pradier, E. The diagnosis of urinary tract infection: A systematic review. Dtsch. Arztebl. Int. 2010, 107, 361–367. [Google Scholar] [CrossRef]
- Chu, C.M.; Lowder, J.L. Diagnosis and treatment of urinary tract infections across age groups. Am. J. Obstet. Gynecol. 2018, 219, 40–51. [Google Scholar] [CrossRef]
- Mehedintu, C.; Bratila, E.; Cirstoiu, M.; Petca, A.; Brinduse, L.A.; Berceanu, C.; Barac, R.I.; Andreescu, C.V.; Petca, R.C.; Sandru, F.; et al. Evaluation of effectiveness and tolerability of boric acid in the treatment of vaginal infection with Candida Species. Rev. Chim. 2019, 70, 2375–2378. [Google Scholar] [CrossRef]
- Foxman, B. Recurring urinary tract infection: Incidence and risk factors. Am. J. Public Health 1990, 80, 331–333. [Google Scholar] [CrossRef]
- Petca, R.C.; Salaheddin, Y.; Petca, A.; Popescu, R.I.; Mehedintu, C.; Maru, N.; Jinga, V. Could chemical composition of stone influence percutaneous nephrolithotomy in the management of staghorn calculi? Rev. Chim. 2019, 70, 3872–3877. [Google Scholar] [CrossRef]
- Alós, J.I. Epidemiología y etiología de la infección urinaria comunitaria. Sensibilidad antimicrobiana de los principales patógenos y significado clínico de la resistencia. Enferm. Infecc. Microbiol. Clin. 2005, 23, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Nielubowicz, G.R.; Mobley, H.L. Host-pathogen interactions in urinary tract infection. Nat. Rev. Urol. 2010, 7, 430–441. [Google Scholar] [CrossRef] [PubMed]
- Levison, M.E.; Kaye, D. Treatment of complicated urinary tract infections with an emphasis on drug-resistant Gram-negative uropathogens. Curr. Infect. Dis. Rep. 2013, 15, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Chenoweth, C.E.; Gould, C.V.; Saint, S. Diagnosis, management, and prevention of catheter-associated urinary tract infections. Infect. Dis. Clin. N. Am. 2014, 28, 105–119. [Google Scholar] [CrossRef]
- Gales, A.C.; Sader, H.S.; Jones, R.N.; SENTRY Participants Group (Latin America). Urinary tract infection trends in Latin American hospitals: Report from the SENTRY antimicrobial surveillance program (1997–2000). Diagn. Microbiol. Infect. Dis. 2002, 44, 289–299. [Google Scholar] [CrossRef]
- Minardi, D.; d’Anzeo, G.; Cantoro, D.; Conti, A.; Muzzonigro, G. Urinary tract infections in women: Etiology and treatment options. Int. J. Gen. Med. 2011, 4, 333–343. [Google Scholar] [CrossRef]
- Wagenlehner, F.M.; Niemetz, A.H.; Weidner, W.; Naber, K.G. Spectrum and antibiotic resistance of uropathogens from hospitalised patients with urinary tract infections: 1994–2005. Int. J. Antimicrob. Agents. 2008, 31, S25–S34. [Google Scholar] [CrossRef]
- Petca, R.C.; Popescu, R.I.; Mares, C.; Petca, A.; Mehedintu, C.; Sandu, I.; Maru, N. Antibiotic resistance profile of common uropathogens implicated in urinary tract infections in Romania. Farmacia 2019, 67, 994–1004. [Google Scholar] [CrossRef]
- Chibelean, C.B.; Petca, R.-C.; Mareș, C.; Popescu, R.-I.; Enikő, B.; Mehedințu, C.; Petca, A. A clinical perspective on the antimicrobial resistance spectrum of uropathogens in a Romanian male population. Microorganisms 2020, 8, 848. [Google Scholar] [CrossRef]
- Schito, G.C.; Naber, K.G.; Botto, H.; Palou, J.; Mazzei, T.; Gualco, L.; Marchese, A. The ARESC study: An international survey on the antimicrobial resistance of pathogens involved in uncomplicated urinary tract infections. Int. J. Antimicrob. Agents 2009, 34, 407–413. [Google Scholar] [CrossRef]
- World Health Organization. Global Antimicrobial Resistance Surveillance System (GLASS) Report: Early Implementation 2020; World Health Organization: Geneva, Switzerland, 2020; pp. 1–132. [Google Scholar]
- Bonkat, G.; Pickard, R.; Bartoletti, R.; Cai, T.; Bruyere, F.; Geerlings, S.E.; Köves, B.; Wagenlehner, F. EAU Guidelines on Urological Infections; European Association of Urology: Arnhem, The Netherlands, 2018. [Google Scholar]
- Gupta, K.; Hooton, T.M.; Naber, K.G.; Wullt, B.; Colgan, R.; Miller, L.G.; Moran, G.J.; Nicolle, L.E.; Raz, R.; Schaeffer, A.J.; et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: A 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin. Infect. Dis. 2011, 52, e103–e120. [Google Scholar] [CrossRef] [PubMed]
- Kahlmeter, G.; Åhman, J.; Matuschek, E. Antimicrobial resistance of Escherichia coli causing uncomplicated urinary tract infections: A European update for 2014 and comparison with 2000 and 2008. Infect. Dis. Ther. 2015, 4, 417–423. [Google Scholar] [CrossRef] [PubMed]
- Stapleton, P.J.; Lundon, D.J.; McWade, R.; Scanlon, N.; Hannan, M.M.; O’Kelly, F.; Lynch, M. Antibiotic resistance patterns of Escherichia coli urinary isolates and comparison with antibiotic consumption data over 10 years, 2005–2014. Ir. J. Med. Sci. 2017, 186, 733–741. [Google Scholar] [CrossRef] [PubMed]
- Seitz, M.; Stief, C.; Waidelich, R. Local epidemiology and resistance profiles in acute uncomplicated cystitis (AUC) in women: A prospective cohort study in an urban urological ambulatory setting. BMC Infect. Dis. 2017, 17, 685. [Google Scholar] [CrossRef]
- Honsbeek, M.; Tjon-A.-Tsien, A.; Stobberingh, E.; de Steenwinkel, J.; Melles, D.C.; Lous, J.; Richardus, J.H.; Voeten, H. Low antimicrobial resistance in general practice patients in Rotterdam, the city with the largest proportion of immigrants in the Netherlands. Eur. J. Clin. Microbiol. Infect. Dis. 2020, 39, 929–935. [Google Scholar] [CrossRef] [PubMed]
- Bientinesi, R.; Murri, R.; Sacco, E. Efficacy and safety of levofloxacin as a treatment for complicated urinary tract infections and pyelonephritis. Expert. Opin. Pharmacother. 2020, 21, 637–644. [Google Scholar] [CrossRef]
- Folliero, V.; Caputo, P.; Della Rocca, M.T.; Chianese, A.; Galdiero, M.; Iovene, M.R.; Hay, C.; Franci, G.; Galdiero, M. Prevalence and antimicrobial susceptibility patterns of bacterial pathogens in urinary tract infections in University Hospital of Campania “Luigi Vanvitelli” between 2017 and 2018. Antibiotics 2020, 9, 215. [Google Scholar] [CrossRef]
- Adeghate, J.; Juhász, E.; Pongrácz, J.; Rimanóczy, É.; Kristóf, K. Does Staphylococcus Saprophyticus cause acute cystitis only in young females, or is there more to the story? A one-year comprehensive study done in Budapest, Hungary. Acta Microbiol. Immunol. Hung. 2016, 63, 57–67. [Google Scholar] [CrossRef]
- Stefaniuk, E.; Suchocka, U.; Bosacka, K.; Hryniewicz, W. Etiology and antibiotic susceptibility of bacterial pathogens responsible for community-acquired urinary tract infections in Poland. Eur. J. Clin. Microbiol. Infect. Dis. 2016, 35, 1363–1369. [Google Scholar] [CrossRef]
- Tandogdu, Z.; Cek, M.; Wagenlehner, F.; Naber, K.; Tenke, P.; van Ostrum, E.; Johansen, T.B. Resistance patterns of nosocomial urinary tract infections in urology departments: 8-year results of the global prevalence of infections in urology study. World J. Urol. 2014, 32, 791–801. [Google Scholar] [CrossRef]
- Schaffer, J.N.; Pearson, M.M. Proteus mirabilis and Urinary Tract Infections. In Urinary Tract Infections: Molecular Pathogenesis and Clinical Management, 2nd ed.; Mulvey, M.A., Klumpp, D.J., Stapleton, A.E., Eds.; ASM Press: Washington, DC, USA, 2017; pp. 383–434. [Google Scholar] [CrossRef]
- Bouza, E.; San Juan, R.; Muñoz, P.; Voss, A.; Kluytmans, J. Co-operative Group of the European Study Group on Nosocomial Infections. A European perspective on nosocomial urinary tract infections I. Report on the microbiology workload, etiology and antimicrobial susceptibility (ESGNI-003 study). European Study Group on Nosocomial Infections. Clin. Microbiol. Infect. 2001, 7, 523–531. [Google Scholar] [CrossRef] [PubMed]
- Kline, K.; Lewis, A. Gram-positive uropathogens, polymicrobial urinary tract infection, and the emerging microbiota of the urinary tract. Microbiol. Spectr. 2016, 4. [Google Scholar] [CrossRef] [PubMed]
- Mody, L.; Juthani-Mehta, M. Urinary tract infections in older women: A clinical review. JAMA 2014, 311, 844–854. [Google Scholar] [CrossRef] [PubMed]
- Foxman, B. Urinary tract infection syndromes: Occurrence, recurrence, bacteriology, risk factors, and disease burden. Infect. Dis. Clin. N. Am. 2014, 28, 1–13. [Google Scholar] [CrossRef]
- Perrotta, C.; Aznar, M.; Mejia, R.; Albert, X.; Ng, C.W. Oestrogens for preventing recurrent urinary tract infection in postmenopausal women. Cochrane Database Syst. Rev. 2008, 2, CD005131. [Google Scholar] [CrossRef]
- Miotla, P.; Romanek-Piva, K.; Bogusiewicz, M.; Markut-Miotla, E.; Adamiak, A.; Wróbel, A.; Zebrowska, M.; Wawrysiuk, S.; Mendyk, K.; Rechberger, E.; et al. Antimicrobial resistance patterns in women with positive urine culture: Does menopausal status make a significant difference? Biomed. Res. Int. 2017, 2017, 4192908. [Google Scholar] [CrossRef]
- Heytens, S.; Boelens, J.; Claeys, G.; DeSutter, A.; Christiaens, T. Uropathogen distribution and antimicrobial susceptibility in uncomplicated cystitis in Belgium, a high antibiotics prescribing country: 20-year surveillance. Eur. J. Clin. Microbiol. Infect. Dis. 2017, 36, 105–113. [Google Scholar] [CrossRef]
- Ny, S.; Edquist, P.; Dumpis, U.; Gröndahl-Yli-Hannuksela, K.; Hermes, J.; Kling, A.M.; Klingeberg, A.; Kozlov, R.; Källman, O.; Lis, D.O.; et al. Antimicrobial resistance of Escherichia coli isolates from outpatient urinary tract infections in women in six European countries including Russia. J. Glob. Antimicrob. Resist. 2019, 17, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Gobernado, M.; Valdés, L.; Alós, J.I.; García-Rey, C.; Dal-Ré, R.; García-de-Lomas, J.; Spanish Surveillance Group for Urinary Pathogens. Antimicrobial susceptibility of clinical Escherichia coli isolates from uncomplicated cystitis in women over a 1-year period in Spain. Rev. Esp. Quimioter. 2007, 20, 68–76. [Google Scholar] [PubMed]
- Falagas, M.E.; Polemis, M.; Alexiou, V.G.; Marini-Mastrogiannaki, A.; Kremastinou, J.; Vatopoulos, A.C. Antimicrobial resistance of Esherichia coli urinary isolates from primary care patients in Greece. Med. Sci. Monit. 2008, 14, CR75–CR79. [Google Scholar] [PubMed]
- Magyar, A.; Köves, B.; Nagy, K.; Dobák, A.; Arthanareeswaran, V.; Bálint, P.; Wagenlehner, F.; Tenke, P. Spectrum and antibiotic resistance of uropathogens between 2004 and 2015 in a tertiary care hospital in Hungary. J. Med. Microbiol. 2017, 66, 788–797. [Google Scholar] [CrossRef] [PubMed]
- Bonkat, G.; Pilatz, A.; Wagenlehner, F. Time to adapt our practice? The European Commission has restricted the use of Fluoroquinolones since March 2019. Eur. Urol. 2019, 76, 273–275. [Google Scholar] [CrossRef] [PubMed]
- Benea, E.O.; Gavriliu, L.C.; Popescu, C.; Popescu, G.A. Ghidul Angelescu. Terapie Antimicrobiana 2018, 3rd ed.; Editura Bucuresti: Bucharest, Romania, 2018; pp. 181–192. [Google Scholar]
- World Health Organization. Guidelines for the Collection of Clinical Specimens during Field Investigation of Outbreaks; World Health Organization: Geneva, Switzerland, 2000; pp. 1–51. [Google Scholar]
- Lee, P.S. Quantification of microorganisms. In Practical Handbook of Microbiology, 2nd ed.; Goldman, E., Green, L.H., Eds.; CRC Press Taylor & Francis Group: Boca Raton, FL, USA, 2009; pp. 11–30. [Google Scholar]
- Pincus, D.H. Microbial Identification Using the Biomérieux Vitek® 2 System. Available online: https://store.pda.org/tableofcontents/ermm_v2_ch01.pdf (accessed on 12 May 2020).
- Clinical and Laboratory Standards Institute® (CLSI). M 100 Performance Standards for Antimicrobial Susceptibility Testing, 28th ed. Available online: https://clsi.org/standards/products/microbiology/documents/m100/ (accessed on 10 May 2020).
| Isolated Bacteria | BCH | MCH | EUH | Total | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Gram Negative | 482 | 77.99 | 283 | 83.72 | 578 | 91.45 | 1343 | 84.57 |
| Escherichia coli | 327 | 52.91 | 156 | 46.15 | 444 | 70.25 | 927 | 58.37 |
| Klebsiella spp. | 95 | 15.37 | 71 | 21.05 | 103 | 16.29 | 269 | 16.93 |
| Pseudomonas aeruginosa | 14 | 2.26 | 32 | 9.46 | 11 | 1.74 | 57 | 3.58 |
| Proteus spp. | 46 | 7.44 | 24 | 7.1 | 20 | 3.16 | 90 | 5.66 |
| Gram Positive | 136 | 22.0 | 55 | 16.27 | 54 | 8.54 | 245 | 15.42 |
| Enterococcus spp. | 114 | 18.44 | 47 | 13.9 | 51 | 8.06 | 212 | 13.35 |
| Staphylococcus spp. | 22 | 3.55 | 8 | 2.36 | 3 | 0.47 | 33 | 2.07 |
| Isolated Bacteria | BCH | MCH | EUH | Total | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ≤40 | 41–55 | >55 | ≤40 | 41–55 | >55 | ≤40 | 41–55 | >55 | ≤40 | 41–55 | >55 | |||||||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| Escherichia coli | 51 | 8.25 | 48 | 7.76 | 228 | 36.89 | 22 | 6.5 | 23 | 6.8 | 111 | 32.84 | 49 | 7.75 | 31 | 4.9 | 364 | 57.59 | 122 | 7.68 | 102 | 6.42 | 703 | 44.26 |
| Klebsiella spp. | 13 | 2.1 | 14 | 2.26 | 68 | 11.0 | 8 | 2.36 | 13 | 3.84 | 50 | 14.79 | 7 | 1.1 | 6 | 0.94 | 90 | 14.24 | 28 | 1.76 | 33 | 2.07 | 208 | 13.09 |
| Pseudomonas aeruginosa | 2 | 0.32 | 1 | 0.16 | 11 | 1.77 | 2 | 0.59 | 3 | 0.88 | 27 | 7.98 | - | - | 3 | 0.47 | 8 | 1.26 | 4 | 0.25 | 7 | 0.44 | 46 | 2.89 |
| Proteus spp. | 7 | 1.13 | 7 | 1.13 | 32 | 5.17 | 5 | 1.47 | 4 | 1.18 | 15 | 4.43 | - | - | 2 | 0.31 | 18 | 2.84 | 12 | 0.75 | 13 | 0.81 | 65 | 4.09 |
| Enterococcus spp. | 19 | 3.07 | 23 | 3.72 | 72 | 11.65 | 9 | 2.66 | 7 | 2.07 | 31 | 9.17 | 6 | 0.94 | 2 | 0.31 | 43 | 6.8 | 34 | 2.14 | 32 | 2.01 | 146 | 9.19 |
| Staphylococcus spp. | 4 | 0.64 | 7 | 1.13 | 11 | 1.77 | - | - | 1 | 0.29 | 7 | 2.07 | 2 | 0.31 | - | - | 1 | 0.15 | 6 | 0.37 | 8 | 0.5 | 19 | 1.19 |
| Total | 96 | 15.53 | 100 | 16.18 | 422 | 68.28 | 46 | 13.6 | 51 | 15.08 | 241 | 71.3 | 64 | 6.96 | 44 | 6.96 | 524 | 82.91 | 206 | 12.97 | 195 | 12.27 | 1187 | 74.74 |
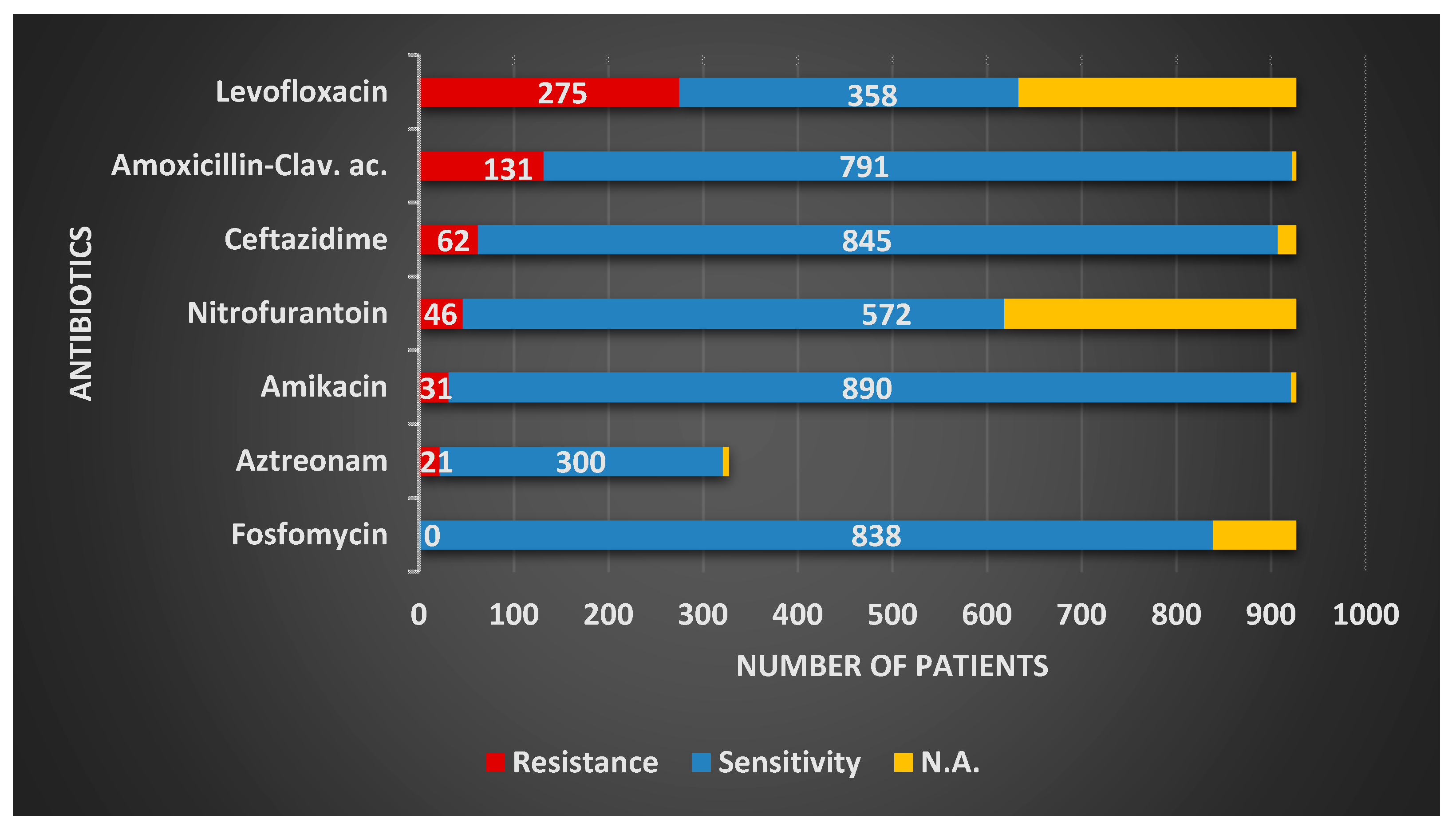
| Antibiotics | Gram-Negative Organism Isolated | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Escherichia coli | Klebsiella spp. | Pseudomonas aeruginosa | Proteus spp. | |||||||||||||||||
| R | S | NA | R | S | NA | R | S | NA | R | S | NA | |||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | |||||
| Amikacin | 31 | 3.34 | 890 | 96.0 | - | 31 | 11.52 | 238 | 88.47 | - | 8 | 14.03 | 46 | 80.7 | - | 8 | 8.88 | 77 | 85.55 | - |
| Amoxicillin-Clavulanic ac. | 131 | 14.13 | 791 | 85.32 | - | 77 | 28.62 | 199 | 73.97 | - | 12 | 21.05 | 21 | 36.84 | - | 24 | 26.66 | 63 | 70.0 | - |
| Aztreonam | 21 | 6.42 | 300 | 91.74 | 600(M + E) | 20 | 21.05 | 71 | 74.73 | 174(M + E) | 3 | 21.42 | 11 | 78.57 | 43(M + E) | 4 | 8.69 | 41 | 89.13 | 44(M + E) |
| Ceftazidime | 62 | 6.68 | 845 | 91.15 | - | 41 | 15.24 | 220 | 81.78 | - | 14 | 24.56 | 41 | 71.92 | - | 13 | 14.44 | 76 | 84.44 | - |
| Fosfomycin | 0 | 0 | 838 | 90.39 | - | - | - | - | - | 4 | 12.5 | 15 | 46.87 | 25(B + E) | 16 | 66.66 | 5 | 20.83 | 66(B+E) | |
| Imipenem | 0 | 0 | 321 | 98.16 | 600(M + E) | 9 | 4.54 | 186 | 93.93 | 71(M) | 4 | 16.0 | 20 | 80.0 | 32(M) | 0 | 0 | 45 | 97.82 | 44(M + E) |
| Levofloxacin | 275 | 29.66 | 358 | 38.61 | - | 42 | 15.61 | 224 | 83.27 | 18 | 31.57 | 38 | 66.66 | - | 22 | 24.44 | 63 | 70.0 | - | |
| Meropenem | 1 | 0.3 | 321 | 98.16 | 600(M + E) | 15 | 7.57 | 182 | 91.91 | 71(M) | 4 | 16.9 | 20 | 80.0 | 32(M) | 1 | 2.17 | 42 | 91.32 | 44(M + E) |
| Nitrofurantoin | 46 | 4.96 | 572 | 61.7 | - | 42 | 15.61 | 113 | 42.0 | - | 8 | 18.6 | 26 | 60.46 | 14(B) | 9 | 37.5 | 11 | 45.83 | 66(B + E) |
| Antibiotics | Gram-Positive Organism Isolated | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Enterococcus spp. | Staphylococcus spp. | |||||||||
| R | S | NA | R | S | NA | |||||
| n | % | n | % | n | % | n | % | |||
| Amikacin | 5 | 10.63 | 15 | 31.91 | 165(B + E) | 2 | 6.06 | 30 | 90.9 | - |
| Ampicillin | 31 | 14.62 | 166 | 78.3 | - | - | - | - | - | - |
| Trimethoprim–Sulfamethoxazole | 5 | 10.63 | 18 | 38.29 | 165(B + E) | 7 | 21.21 | 21 | 63.63 | - |
| Ceftazidime | 2 | 4.25 | 19 | 40.42 | 165(B + E) | 5 | 22.72 | 17 | 77.27 | 11(M + E) |
| Fosfomycin | 1 | 0.62 | 152 | 94.4 | 51(E) | 0 | 0 | 5 | 62.5 | 25(B + E) |
| Levofloxacin | 68 | 32.07 | 141 | 66.5 | - | 9 | 27.27 | 21 | 63.63 | - |
| Nitrofurantoin | 7 | 3.3 | 189 | 89.15 | - | 2 | 0.8 | 19 | 76.0 | 8(M) |
| Penicillin | 68 | 32.07 | 129 | 60.84 | - | 11 | 50.0 | 10 | 45.45 | 11(M + E) |
| Vancomycin | 3 | 1.41 | 195 | 91.98 | - | - | - | - | - | - |
| Antibiotics | Gram-Negative | Gram-Positive | Total | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| R | S | R | S | R | S | |||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| Amikacin | 78 | 5.8 | 1251 | 93.14 | 7 | 8.75 | 45 | 56.25 | 85 | 5.97 | 1296 | 91.07 |
| Amoxicillin–Clavulanic ac. | 244 | 18.16 | 1074 | 79.97 | - | - | - | - | 244 | 18.16 | 1074 | 79.97 |
| Ampicillin | - | - | - | - | 31 | 14.62 | 166 | 78.3 | 31 | 14.62 | 166 | 78.3 |
| Aztreonam | 48 | 9.95 | 423 | 87.75 | - | - | - | - | 48 | 9.95 | 423 | 87.75 |
| Trimethoprim-Sulfamethoxazole | - | - | - | - | 12 | 15.0 | 39 | 48.75 | 12 | 15.0 | 39 | 48.75 |
| Ceftazidime | 130 | 9.67 | 1182 | 88.01 | 7 | 10.14 | 36 | 52.17 | 137 | 9.7 | 1218 | 86.26 |
| Fosfomycin | 20 | 2.03 | 858 | 87.28 | 1 | 0.59 | 157 | 92.89 | 21 | 1.82 | 1015 | 88.10 |
| Imipenem | 13 | 2.18 | 572 | 95.97 | - | - | - | - | 13 | 2.18 | 572 | 95.97 |
| Levofloxacin | 357 | 26.58 | 683 | 50.85 | 77 | 31.42 | 162 | 66.12 | 434 | 27.32 | 845 | 53.21 |
| Meropenem | 21 | 3.52 | 565 | 94.79 | - | - | - | - | 21 | 3.52 | 565 | 94.79 |
| Nitrofurantoin | 105 | 8.31 | 722 | 57.16 | 9 | 3.79 | 208 | 87.76 | 114 | 7.6 | 930 | 62.0 |
| Penicillin | - | - | - | - | 79 | 33.76 | 139 | 59.4 | 79 | 33.76 | 139 | 59.40 |
| Vancomycin | - | - | - | - | 3 | 1.22 | 195 | 79.59 | 3 | 1.22 | 195 | 79.59 |
| Antibiotics | Quantity (mcG) | Disk Diffusion Ranges (mm) |
|---|---|---|
| Amikacin | 30 | 15–16 |
| Amoxicillin–Clavulanic ac. | 20/10 | 14–17 |
| Aztreonam | 30 | 18–20 |
| Ceftazidime | 30 | 18–20 |
| Fosfomycin | 200 | 13–15 |
| Imipenem | 10 | 20–22 |
| Levofloxacin | 5 | 14–16 |
| Meropenem | 10 | 20–22 |
| Nitrofurantoin | 300 | 15–16 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Petca, R.-C.; Mareș, C.; Petca, A.; Negoiță, S.; Popescu, R.-I.; Boț, M.; Barabás, E.; Chibelean, C.B. Spectrum and Antibiotic Resistance of Uropathogens in Romanian Females. Antibiotics 2020, 9, 472. https://doi.org/10.3390/antibiotics9080472
Petca R-C, Mareș C, Petca A, Negoiță S, Popescu R-I, Boț M, Barabás E, Chibelean CB. Spectrum and Antibiotic Resistance of Uropathogens in Romanian Females. Antibiotics. 2020; 9(8):472. https://doi.org/10.3390/antibiotics9080472
Chicago/Turabian StylePetca, Răzvan-Cosmin, Cristian Mareș, Aida Petca, Silvius Negoiță, Răzvan-Ionuț Popescu, Mihaela Boț, Enikő Barabás, and Călin Bogdan Chibelean. 2020. "Spectrum and Antibiotic Resistance of Uropathogens in Romanian Females" Antibiotics 9, no. 8: 472. https://doi.org/10.3390/antibiotics9080472
APA StylePetca, R.-C., Mareș, C., Petca, A., Negoiță, S., Popescu, R.-I., Boț, M., Barabás, E., & Chibelean, C. B. (2020). Spectrum and Antibiotic Resistance of Uropathogens in Romanian Females. Antibiotics, 9(8), 472. https://doi.org/10.3390/antibiotics9080472






