Antibacterial Drug Development: A New Approach Is Needed for the Field to Survive and Thrive
Abstract
1. The Broken Antibiotic Marketplace
2. The Carbapenem-Resistant Enterobacteriaceae Threat
3. Phage Therapies, Virulence Inhibitors, Bacterial Growth Rate Modulators, and Monoclonal Antibodies
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Centers for Disease Control and Prevention (CDC). Antibiotic Resistance Threats in the United States, 2019; U.S. Department of Health and Human Services, CDC: Atlanta, GA, USA, 2019.
- Burnham, J.P.; Olsen, M.A.; Kollef, M.H. Re-estimating annual deaths due to multidrug-resistant organism infections. Infect. Control Hosp. Epidemiol. 2019, 40, 112–113. [Google Scholar] [CrossRef] [PubMed]
- Outterson, K.; Powers, J.H.; Daniel, G.W.; McClellan, M.B. Repairing the broken market for antibiotic innovation. Health Aff. 2015, 34, 277–285. [Google Scholar] [CrossRef] [PubMed]
- Shlaes, D.M.; Bradford, P.A. Antibiotics–From there to where? How the antibiotic miracle is threatened by resistance and a broken market and what we can do about it. Pathog. Immun. 2018, 3, 19–43. [Google Scholar] [CrossRef] [PubMed]
- Lack of New Antibiotics Threatens Global Efforts to Contain Drug-Resistant Infections [News Release]; World Health Organization: Geneva, Switzerland, 17 January 2020; Available online: https://www.who.int/news-room/detail/17-01-2020-17-01-2020-lack-of-new-antibiotics-threatens-global-efforts-to-contain-drug-resistant-infections (accessed on 28 May 2020).
- Jacobs, A. Crisis Looms in antibiotics as drug makers go bankrupt. New York Times. 26 December 2019. Section A Page 1. Available online: https://www.nytimes.com/2019/12/25/health/antibiotics-new-resistance.html (accessed on 28 May 2020).
- Achaogen Inc. United States Securities and Exchange Commission Filing. Form 10-K. 1 April 2019. Available online: https://seekingalpha.com/filing/4427413 (accessed on 10 June 2020).
- GlobeNewswire. Achaogen Reports Fourth Quarter and Full Year 2018 Financial Results and Provides Corporate Update. 28 March 2019. Available online: https://www.globenewswire.com/news-release/2019/03/28/1783626/0/en/Achaogen-Reports-Fourth-Quarter-and-Full-Year-2018-Financial-Results-and-Provides-Corporate-Update.html (accessed on 29 May 2020).
- GlobeNewswire. Achaogen Plans for Near-Term Sale Using Structured Process through Chapter 11 of the U.S. Bankruptcy Code. 15 April 2019. Available online: https://www.globenewswire.com/news-release/2019/04/15/1803906/0/en/Achaogen-Plans-for-Near-Term-Sale-Using-Structured-Process-Through-Chapter-11-of-the-U-S-Bankruptcy-Code.html (accessed on 29 May 2020).
- In the United States Bankruptcy Court for the District of Delaware v. Achaogen Inc. Chapter 11. Case No. 19-10844 (BLS). Docket #0295. 22 June 2019. Available online: http://www.kccllc.net/achaogen/document/1910844190622000000000002 (accessed on 10 June 2020).
- European Medicines Agency. Available online: https://www.ema.europa.eu/en/documents/withdrawal-letter/withdrawal-letter-zemdri_en.pdf (accessed on 14 July 2020).
- European Medicines Agency. Available online: https://www.ema.europa.eu/en/medicines/human/withdrawn-applications/zemdri (accessed on 14 July 2020).
- CARB-X. Annual Report 2018–2019. 2019. Available online: https://carb-x.org/wp-content/uploads/2019/09/Carbx_AR_2018_forweb2.pdf (accessed on 28 May 2020).
- Biomedical Advanced Research and Development Authority (BARDA). Available online: https://www.phe.gov/about/barda/Pages/default.aspx (accessed on 1 June 2020).
- Food and Drug Administration. Limited Population Pathway for Antibacterial and Antifungal Drugs: Guidance for Industry; U.S. Department of Health and Human Services, Food and Drug Administration: Silver Spring, MD, USA, 2018.
- Centers for Disease Control and Prevention (CDC). Antibiotic Resistance Threats in the United States, 2013; U.S. Department of Health and Human Services, CDC: Atlanta, GA, USA, 2013.
- Castanheira, M.; Deshpande, L.M.; Mendes, R.E.; Canton, R.; Sader, H.S.; Jones, R.N. Variations in the occurrence of resistance phenotypes and carbapenemase genes among Enterobacteriaceae isolates in 20 years of the SENTRY Antimicrobial Surveillance Program. Open Forum Infect. Dis. 2019, 6, S23–S33. [Google Scholar] [CrossRef]
- Castanheira, M.; Doyle, T.B.; Kantro, V.; Mendes, R.E.; Shortridge, D. Meropenem-vaborbactam activity against carbapenem-resistant Enterobacterales isolates collected in U.S. hospitals during 2016 to 2018. Antimicrob. Agents Chemother. 2020, 64, e01951-19. [Google Scholar] [CrossRef]
- Fernebro, J. Fighting bacterial infections–Future treatment options. Drug Resist. Update 2011, 14, 125–139. [Google Scholar] [CrossRef]
- Kutateladze, M.; Adamia, R. Bacteriophages as potential new therapeutics to replace or supplement antibiotics. Trends Biotechnol. 2010, 28, 591–595. [Google Scholar] [CrossRef]
- Baron, C. Antivirulence drugs to target bacterial secretion systems. Curr. Opin. Microbiol. 2010, 13, 100–105. [Google Scholar] [CrossRef]
- Ambrose, P.G.; VanScoy, B.; Conde, H.; McCauley, J.; Rubino, C.M.; Bhavnani, S.M. Bacterial replication rate modulation in combination with antimicrobial therapy: Turning the microbe against itself. Antimicrob. Agents Chemother. 2016, 61, e01605-16. [Google Scholar] [CrossRef]
- Ambrose, P.G.; VanScoy, B.D.; Adams, J.; Fikes, S.; Bader, J.C.; Bhavnani, S.M.; Rubino, C.M. Norepinephrine in combination with antimicrobial therapy increases both the bacterial replication rate and bactericidal activity. Antimicrob. Agents Chemother. 2018, 62, e02257-17. [Google Scholar] [CrossRef]
- Ambrose, P.G.; VanScoy, B.D.; Luna, B.M.; Yan, J.; Ulhaq, A.; Nielsen, T.B.; Rudin, S.; Hujer, K.; Bonomo, R.A.; Actis, L.; et al. Apotransferrin in Combination with Ciprofloxacin Slows Bacterial Replication, Prevents Resistance Amplification, and Increases Antimicrobial Regimen Effect. Antimicrob. Agents Chemother. 2019, 63, e00112-19. [Google Scholar] [CrossRef] [PubMed]
- Nagy, E.; Nagy, G.; Power, C.A.; Badarau, A.; Szijarto, V. Anti-bacterial monoclonal antibodies. In Recombinant Antibodies for Infectious Diseases. Advances in Experimental Medicine and Biology; Springer: Cham, Switzerland, 2017; Volume 1053, pp. 119–153. [Google Scholar]
- DiGiandomenico, A.; Sellman, B.R. Antibacterial monoclonal antibodies: The next generation? Curr. Opin. Microbiol. 2015, 27, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Zurawski, D.V.; McLendon, M.K. Monoclonal antibodies as an antibacterial approach against bacterial pathogens. Antibiotics 2020, 9, 155. [Google Scholar] [CrossRef] [PubMed]
- CARB-X. Available online: https://carb-x.org/portfolio/gallery/ (accessed on 30 June 2020).
- Francois, B.; Mercier, E.; Gonzalez, C.; Asehnoune, K.; Nseir, S.; Fiancette, M.; Desachy, A.; Plantefeve, G.; Meziani, F.; de Lame, P.-A.; et al. Safety and tolerability of a single administration of AR-301, a human monoclonal antibody, in ICU patients with severe pneumonia caused by Staphylococcus aureus: First-in-human trial. Intensive Care Med. 2018, 44, 1787–1796. [Google Scholar] [CrossRef] [PubMed]
- Armata Pharmaceuticals. Available online: https://www.armatapharma.com/pipeline/ap-pa02/ (accessed on 7 July 2020).
- Armata Pharmaceuticals. Available online: https://www.armatapharma.com/pipeline/ap-sa02/ (accessed on 7 July 2020).
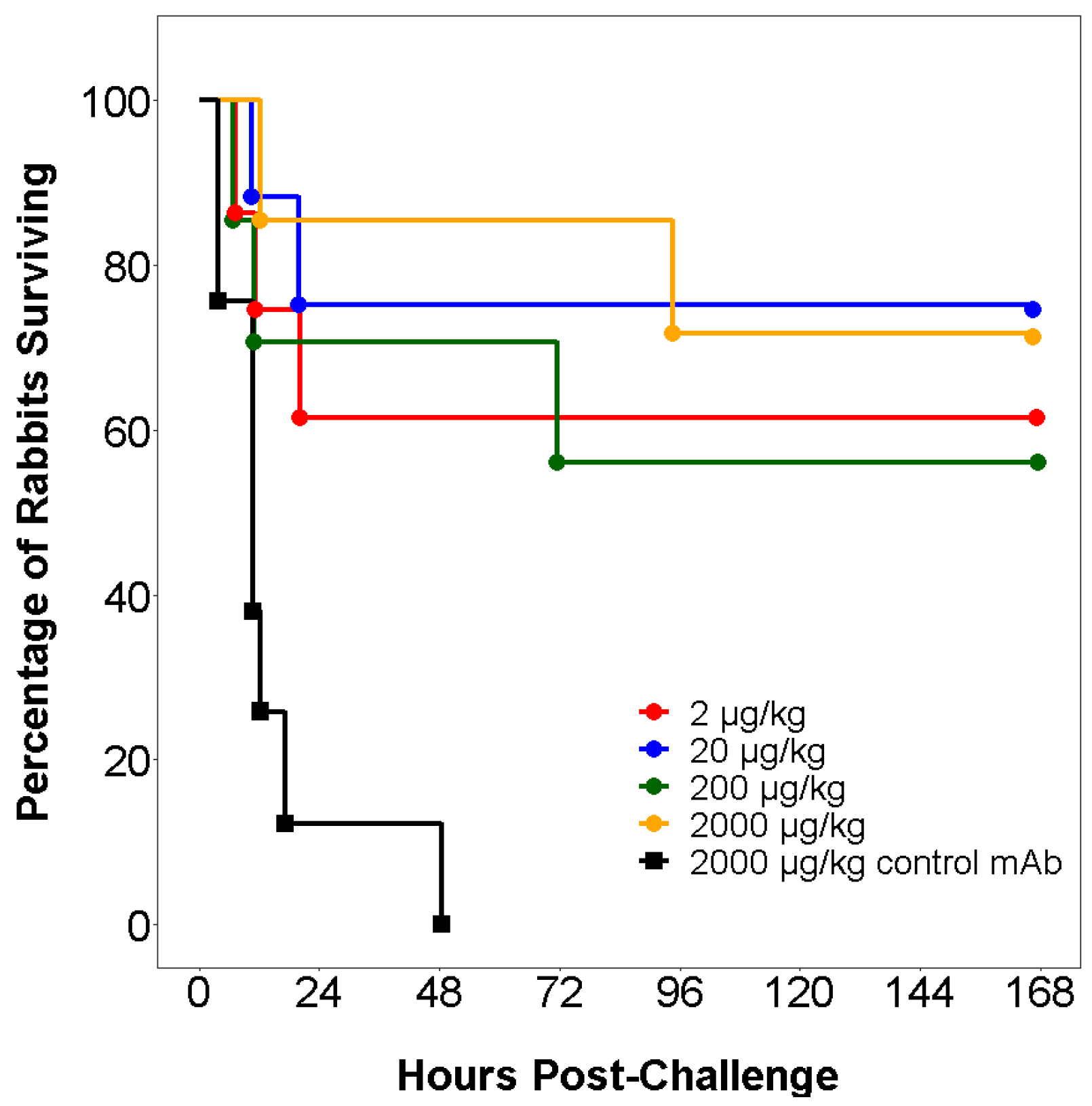
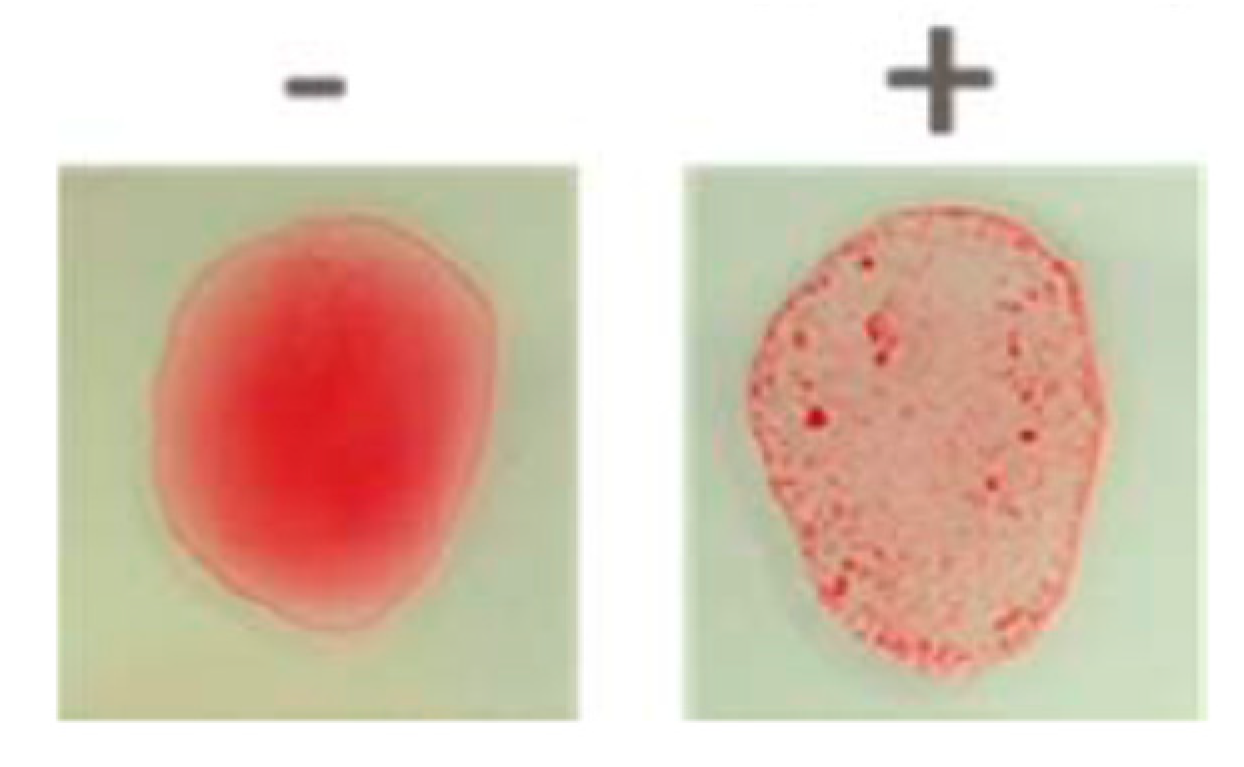
- Szijarto, V.; Guachalla, L.M.; Hartl, K.; Varga, C.; Badarau, A.; Mirkina, I.; Visram, Z.C.; Stulik, L.; Power, C.A.; Nagy, E.; et al. Endotoxin neutralization by an O-antigen specific monoclonal antibody: A potential novel therapeutic approach against Klebsiella pneumoniae ST258. Virulence 2017, 8, 1203–1215. [Google Scholar] [CrossRef] [PubMed]
- Ghose, C. Development of BH01, a peptide lysin for the treatment of Acinetobacter infections. Presented at the ASM/ESCMID Conference on Drug Development to Meet the Challenge of Antimicrobial Resistance, Boston, MA, USA, 6 September 2019. [Google Scholar]
- Laterre, P.-F.; Colin, G.; Dequin, P.-F.; Dugernier, T.; Boulain, T.; Azeredo da Silveira, S.; Lajaunais, F.; Perez, A.; Francois, B. CAL02, a novel antitoxin liposomal agent, in severe pneumococcal pneumonia: A first-in-human, double-blind, placebo-controlled, randomised trial. Lancet Infect. Dis. 2019, 19, 620–630. [Google Scholar] [CrossRef]
- Channabasappa, S.; Durgaiah, M.; Chikkamadaiah, R.; Kumar, S.; Joshi, A.; Sriram, B. Efficacy of novel antistaphylococcal ectolysin P128 in a rat model of methicillin-resistant Staphylococcus aureus bacteremia. Antimicrob. Agents Chemother. 2018, 62, e01358-17. [Google Scholar] [CrossRef] [PubMed]
- Peck, M.; Rothenberg, M.E.; Deng, R.; Lewin-Koh, N.; She, G.; Kamath, A.R.; Carrasco-Triguero, M.; Saad, O.; Castro, A.; Teufel, L.; et al. A Phase 1, randomized, single-ascending-dose study to investigate the safety, tolerability, and pharmacokinetics of DSTA4637S, an anti-Staphylococcus aureus Thiomab antibody-antibiotic conjugate, in healthy volunteers. Antimicrob. Agents Chemother. 2019, 63, e02588-18. [Google Scholar] [CrossRef]
- ClinicalTrials.gov [Internet]. Bethesda (MD): National Library of Medicine (US). Identifier NCT03089697, Phase IIa Clinical Study of N-Rephasin® SAL200. 24 March 2017. Available online: https://clinicaltrials.gov/ct2/show/NCT03089697?term=sal200&draw=2&rank=2 (accessed on 14 July 2020).
- Locus Biosciences. Available online: https://www.locus-bio.com/media/locus-biosciences-initiates-worlds-first-controlled-clinical-trial/ (accessed on 14 July 2020).
- Shuptrine, C.; Surana, R.; Weiner, L.M. Monoclonal antibodies for the treatment of cancer. Semin. Cancer Biol. 2012, 22, 3–13. [Google Scholar] [CrossRef]
- Falzone, L.; Salomone, S.; Libra, M. Evolution of cancer pharmacological treatments at the turn of the third millennium. Front. Pharmacol. 2018, 9, 1300. [Google Scholar] [CrossRef]
- Campochiaro, C.; Della-Torre, E.; Cavalli, G.; De Luca, G.; Ripa, M.; Boffini, N.; Tomelleri, A.; Baldissera, E.; Rovere-Querini, P.; Ruggeri, A.; et al. Efficacy and safety of tocilizumab in severe COVID-19 patients: A single-centre retrospective cohort study. Eur. J. Int. Med. 2020, 76, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Han, M.; Li, T.; Sun, W.; Wang, D.; Fu, B.; Zhou, Y.; Zheng, X.; Yang, Y.; Li, X.; et al. Effective treatment of severe COVID-19 patients with tocilizumab. Proc. Natl. Acad. Sci. USA 2020, 117, 10970–10975. [Google Scholar] [CrossRef] [PubMed]
- ClinicalTrials.gov [Internet]. Bethesda (MD): National Library of Medicine (US). Identifier NCT04315298, Evaluation of the Efficacy and Safety of Sarilumab in Hospitalized Patients with COVID-19. 19 March 2020. Available online: https://clinicaltrials.gov/ct2/show/NCT04315298?term=sarilumab&cond=covid-19&draw=2 (accessed on 6 June 2020).
- ClinicalTrials.gov [Internet]. Bethesda (MD): National Library of Medicine (US). Identifier NCT04357808, Efficacy of Subcutaneous Sarilumab in Hospitalized Patients with Moderate-Severe COVID-19 Infection (SARCOVID). 22 April 2020. Available online: https://clinicaltrials.gov/ct2/show/NCT04357808?term=sarilumab&cond=covid-19&draw=2 (accessed on 6 June 2020).
- Zinplava (Bezlotoxumab) [Package Insert]; Merck & Co. Inc.: Whitehouse Station, NJ, USA, 2016; Available online: https://www.merck.com/product/usa/pi_circulars/z/zinplava/zinplava_pi.pdf (accessed on 9 June 2020).
- ANTHIM (Obiltoxaximab) [Package Insert]; Elusys Therapeutics Inc.: Pine Brook, NJ, USA, 2016. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/125509lbl.pdf (accessed on 12 June 2020).
- Raxibacumab [Package Insert]; GlaxoSmithKline: Research Triangle Park, NC, USA, 2012. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/125349s000lbl.pdf (accessed on 12 June 2020).
- Wilcox, M.H.; Gerding, D.N.; Poxton, I.R.; Kelly, C.; Nathan, R.; Birch, T.; Cornely, O.A.; Rahav, G.; Bouza, E.; Lee, C.; et al. Bezlotoxumab for prevention of recurrent Clostridium difficile infection. N. Engl. J. Med. 2017, 376, 305–317. [Google Scholar] [CrossRef] [PubMed]
- Choi, M.; Hegerle, N.; Nkeze, J.; Sen, S.; Jamindar, S.; Nasrin, S.; Sen, S.; Permala-Booth, J.; Sinclair, J.; Tapia, M.D.; et al. The diversity of lipopolysaccharide (O) and capsular polysaccharide (K) antigens of invasive Klebsiella pneumoniae in a multi-country collection. Front. Microbiol. 2020, 11, 1249. [Google Scholar] [CrossRef] [PubMed]
- Kortright, K.E.; Chan, B.K.; Koff, J.L.; Turner, P.E. Phage therapy: A renewed approach to combat antibiotic-resistant bacteria. Cell Host Microbe 2019, 25, 2019–2232. [Google Scholar] [CrossRef]
- Cisek, A.A.; Dabrowska, I.; Gregorczyk, K.P.; Wyzewski, Z. Phage therapy in bacterial infections treatment: One hundred years after the discovery of bacteriophages. Curr. Microbiol. 2017, 74, 277–283. [Google Scholar] [CrossRef]
- Gill, J.J.; Hyman, P. Phage choice, isolation, and preparation for phage therapy. Curr. Pharm. Biotechnol. 2010, 11, 2–14. [Google Scholar] [CrossRef]
- Moradpour, Z.; Yousefi, N.; Sadeghi, D.; Ghasemian, A. Synergistic bactericidal activity of a naturally isolated phage and ampicillin against urinary tract infecting Escherichia coli O157. Iran. J. Basic Med. Sci. 2019, 23, 257–263. [Google Scholar]
- Styles, K.M.; Thummeepak, R.; Leungtongkam, U.; Smith, S.E.; Christie, G.S.; Millard, A.; Moat, J.; Dowson, C.G.; Wellington, E.M.H.; Sitthisak, S.; et al. Investigating bacteriophages targeting the opportunistic pathogen Acinetobacter baumanii. Antibiotics 2020, 9, 200. [Google Scholar] [CrossRef]
- Kebriaei, R.; Lev, K.; Morrisette, T.; Stamper, K.C.; Abdul-Mutakabbir, J.C.; Lehman, S.M.; Morales, S.; Rybak, M.J. Bacteriophage-antibiotic combination strategy: An alternative against methicillin-resistant phenotypes of Staphylococcus aureus. Antimicrob. Agents Chemother. 2020, 64, e00461-20. [Google Scholar] [CrossRef]
- Eliava Phage Therapy Center. Available online: https://eliavaphagetherapy.com/ (accessed on 2 July 2020).
- Ludwik Hirszfeld Institute of Immunology and Experimental Therapy. Available online: https://www.iitd.pan.wroc.pl/en/OTF/ZasadyTerapiiFagowej.html (accessed on 2 July 2020).
- CARB-X. Available online: https://carb-x.org/carb-x-news/carb-x-funds-eligo-bioscience-to-develop-crispr-based-therapeutics-derived-from-bacteriophages-to-kill-superbugs-and-prevent-deadly-infections-in-transplant-patients (accessed on 2 July 2020).
- Fowler, V.G.; Das, A.F.; Lipka-Diamond, J.; Schuch, R.; Pomerantz, R.; Jauregui-Peredo, L.; Bressler, A.; Evans, D.; Moran, G.J.; Rupp, M.E.; et al. Exebacase for patients with Staphylococcus aureus bloodstream infection and endocarditis. J. Clin. Investig. 2020, 130, 3750–3760. [Google Scholar] [CrossRef] [PubMed]
- ClinicalTrials.gov [Internet]. Bethesda (MD): National Library of Medicine (US). Identifier NCT04160468, Direct Lysis of Staph aureus Resistant Pathogen Trial of Exebacase (DISRUPT). 13 November 2019. Available online: https://clinicaltrials.gov/ct2/show/NCT04160468?term=exebacase&draw=1&rank=1 (accessed on 2 July 2020).
| Approved Agent | Class | Developmental Agent | Class |
|---|---|---|---|
| Ceftazidime-avibactam | β-lactam-β-lactamase inhibitor | Apramycin | Aminoglycoside |
| Cefiderocol | Siderophore cephalosporin | Arbekacin inhalation | Aminoglycoside |
| Ciprofloxacin | Fluoroquinolone | BOS-228 | Monobactam |
| Colistin | Polymyxin | Cefepime-AAI101 | β-lactam-β-lactamase inhibitor |
| Doxycycline | Tetracycline | Cefepime-VNRX5133 | β-lactam-β-lactamase inhibitor |
| Imipenem-relebactam | β-lactam-β-lactamase inhibitor | Cefepime-zidebactam | β-lactam-PBP2 inhibitor |
| Levofloxacin | Fluoroquinolone | Ceftibuten-VNRX7145 | β-lactam-β-lactamase inhibitor |
| Meropenem-vaborbactam | β-lactam-β-lactamase inhibitor | Cefpodoxime-ETX0282 | β-lactam- β-lactamase inhibitor |
| Plazomicin | Aminogycoside | FG-LpxC-UTI | LpxC inhibitor |
| Tigecycline | Tetracycline | Fosfomycin 1 | Phosphoenolpyruvate synthetase inhibitor |
| KBP-7072 | Tetracycline | ||
| Meropenem-nacubactam | β-lactam-β-lactamase inhibitor | ||
| QPX2015-QPX7728 | β-lactam-β-lactamase inhibitor | ||
| SPR206 | Polymyxin |
| Sponsor | Product | Class/Mechanism of Action | Reference |
|---|---|---|---|
| Amicrobe, Inc. | Amicidin-β | Amicidin | [28] |
| Antabio SAS | PEi | Pseudomonas elastase inhibitor | [28] |
| Aridis Pharmaceuticals | Aerumab 1, AR-401, Salvecin 2 | Monoclonal antibodies | [25,26,27,29] |
| Armata Pharmaceuticals | AP-PA02, AP-SA02 | Phage cocktails | [30,31] |
| AstraZeneca PLC | Suvratoxumab 3 | Monoclonal antibodies | [25,26,27] |
| Bravos BioSciences | BB100 4, BB200 5 | Monoclonal antibodies | [27,28,32] |
| Bioharmony Therapeutics | BH01 | Lysin | [33] |
| BioVersys AG | AVATAR-SA | Antivirulent (inhibits AgrA) | [28] |
| Centauri Therapeutics | ABX01 | Dual-acting immunotherapy | [28] |
| Combioxin SA | CAL02 | Antivirulent liposome | [34] |
| ContraFect Corporation | Exebacase 6, Gram-negative lysins | Direct lytic agents | [28] |
| Eligo Bioscience | EB004 | Bacteriophage | [28] |
| Facile Therapeutics | Ebselen | Anti-toxin | [28] |
| GangaGen, Inc. | P128 | Lysin | [35] |
| Genentech, Inc. | DSTA4637S | Monoclonal antibody-antibiotic conjugate | [36] |
| Integrated BioTherapeutics Inc. | IBT-V02 | Multivalent toxoid vaccine targeting Staphylococcus aureus | [28] |
| iNtRON Biotechnology, Inc. | N-Rephasin SAL200 7 | Lysin | [37] |
| Locus Biosciences | LBP-EC01 | Bacteriophage | [38] |
| Lytica Therapeutics | StAMPs | Stapled antimicrobial peptides | [28] |
| Microbiotix, Inc. | Trans translational inhibitor | Trans translational inhibitor antibiotic | [28] |
| Microbiotix, Inc. | T3SS inhibitor | T3SS inhibitor, virulence modifier | [28] |
| MicroPharm Ltd. | PolyCAb | Polyclonal antibody | [27] |
| Roche | RG7861 | Monoclonal antibody | [27] |
| Seres Therapeutics | SER-155 | Microbiome transplant | [28] |
| Techulon Inc. | PPNA-XPA | Peptide-peptide nucleic acid | [28] |
| Trellis Bioscience | TRL1068 | Monoclonal antibody | [27,28] |
| Vaxcyte, Inc. 8 | VAX-A1 | Carbohydrate conjugate vaccine targeting Group A Streptococcus | [28] |
| Vaxxilon AG | VXN-319 | Multivalent vaccine targeting K. pneumoniae | [28] |
| VaxDyn, S.L. | VXD-003 | Monoclonal antibody | [27] |
| Vedanta Biosciences, Inc. | VE707 | Live biotherapeutic | [27] |
| XBiotech Inc. | 514G3 | Monoclonal antibody | [25,27] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Safir, M.C.; Bhavnani, S.M.; Slover, C.M.; Ambrose, P.G.; Rubino, C.M. Antibacterial Drug Development: A New Approach Is Needed for the Field to Survive and Thrive. Antibiotics 2020, 9, 412. https://doi.org/10.3390/antibiotics9070412
Safir MC, Bhavnani SM, Slover CM, Ambrose PG, Rubino CM. Antibacterial Drug Development: A New Approach Is Needed for the Field to Survive and Thrive. Antibiotics. 2020; 9(7):412. https://doi.org/10.3390/antibiotics9070412
Chicago/Turabian StyleSafir, M. Courtney, Sujata M. Bhavnani, Christine M. Slover, Paul G. Ambrose, and Christopher M. Rubino. 2020. "Antibacterial Drug Development: A New Approach Is Needed for the Field to Survive and Thrive" Antibiotics 9, no. 7: 412. https://doi.org/10.3390/antibiotics9070412
APA StyleSafir, M. C., Bhavnani, S. M., Slover, C. M., Ambrose, P. G., & Rubino, C. M. (2020). Antibacterial Drug Development: A New Approach Is Needed for the Field to Survive and Thrive. Antibiotics, 9(7), 412. https://doi.org/10.3390/antibiotics9070412




