The Pharmaceutical Ability of Pistacia lentiscus L. Leaves Essential Oil Against Periodontal Bacteria and Candida sp. and Its Anti-Inflammatory Potential
Abstract
1. Introduction
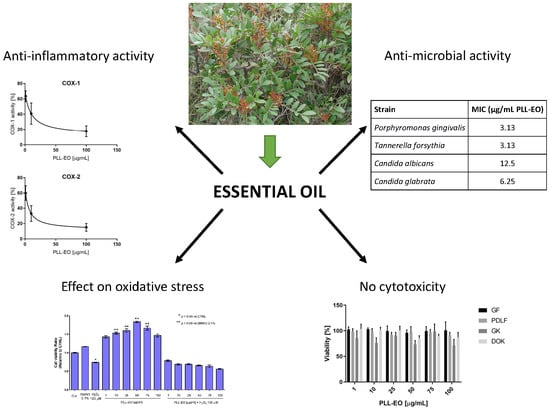
2. Results
2.1. Essential Oil Yield and Chemical Fingerprinting
2.2. Minimal Inhibitory Concentrations Against Oral Bacteria and Candida sp.
2.3. Anti-inflammatory Assays
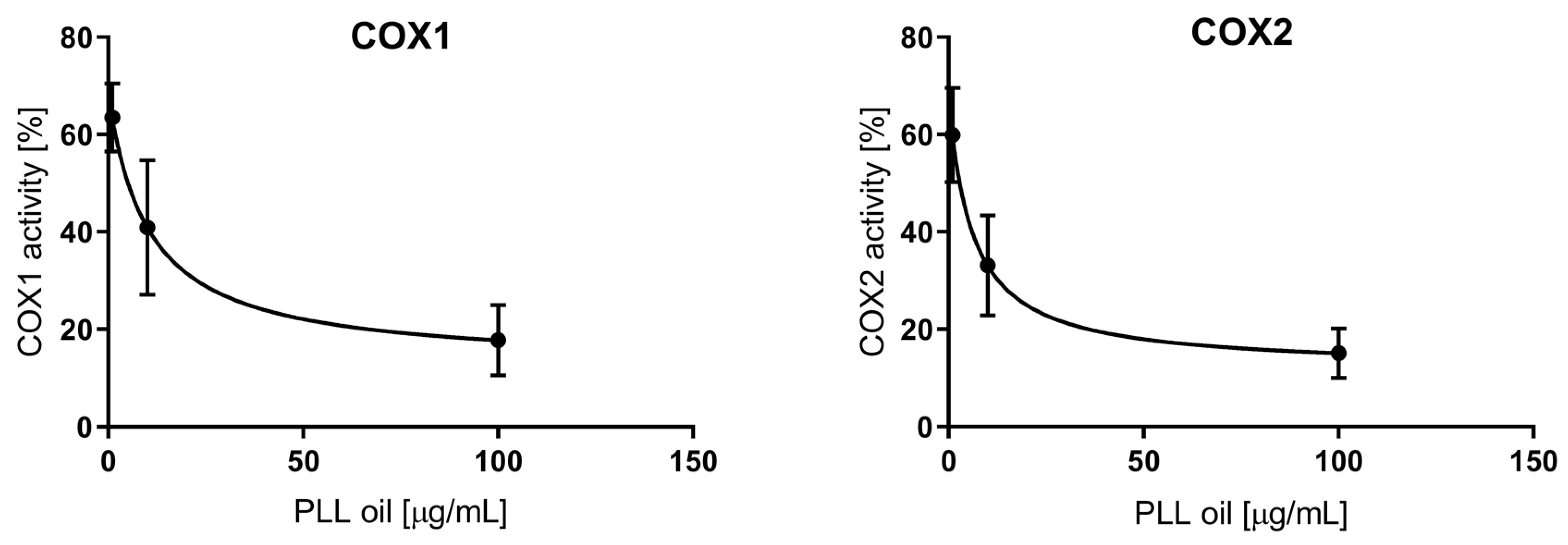
2.3.1. COX-1/2 Inhibition
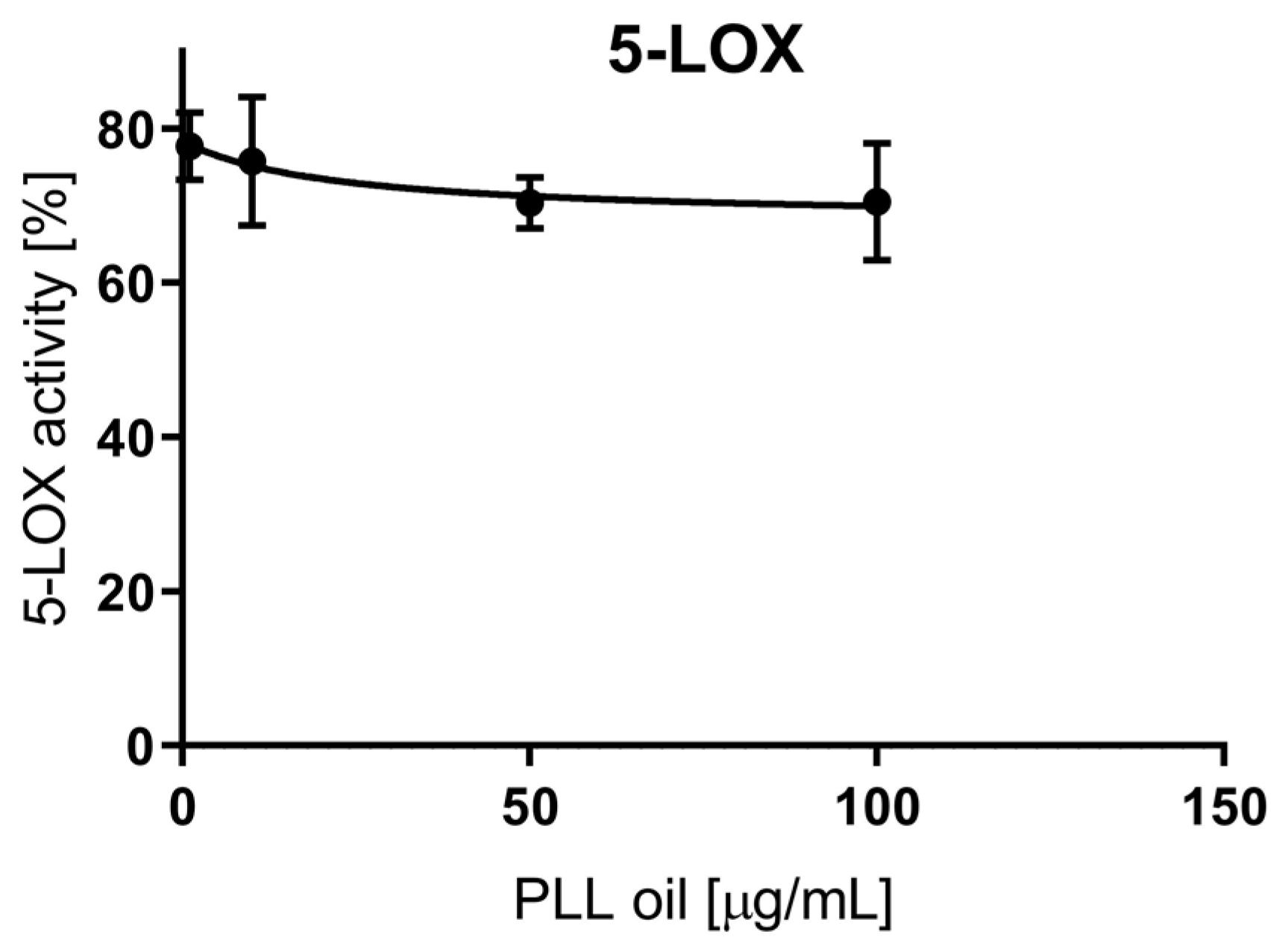
2.3.2. LOX Inhibition
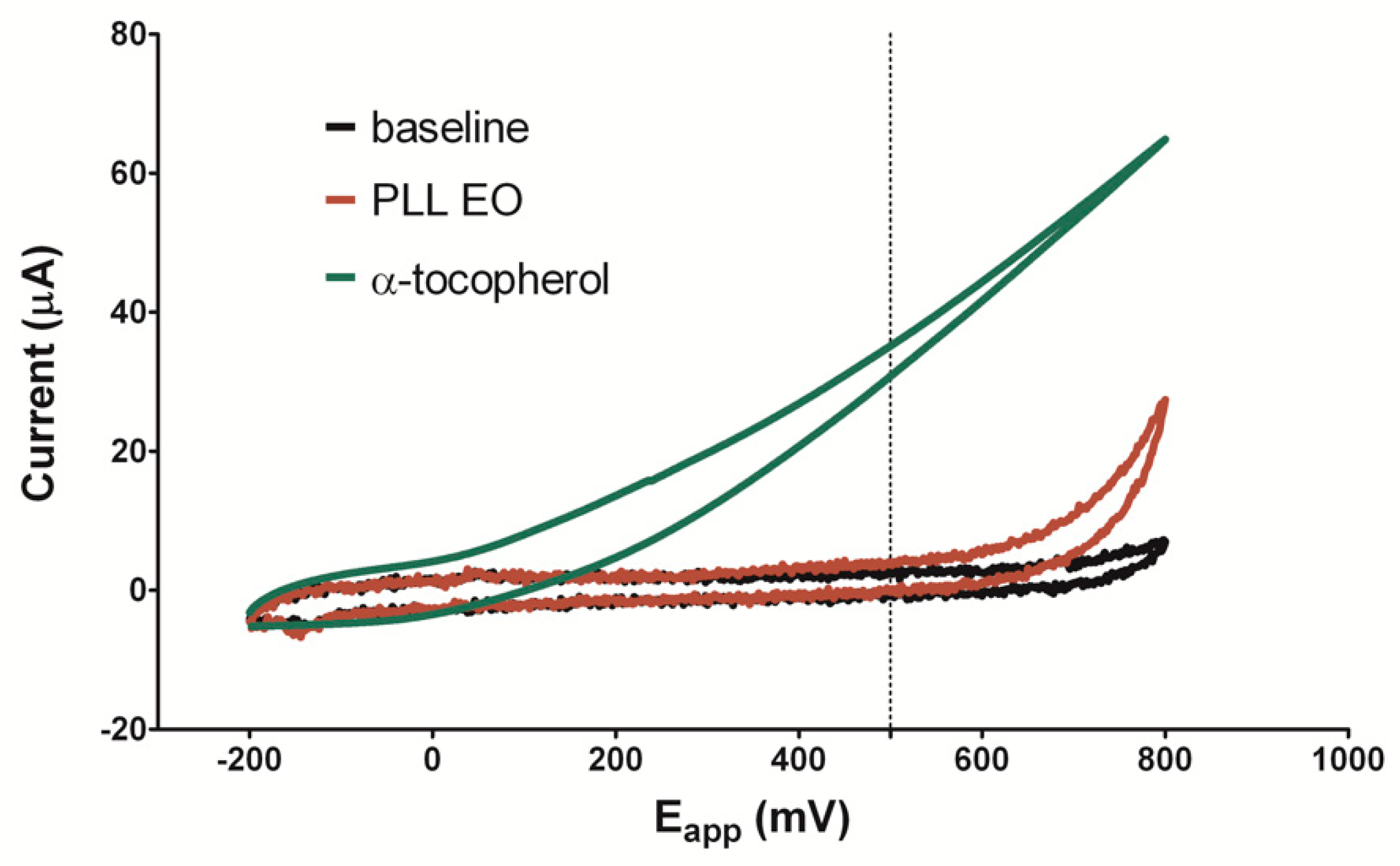
2.3.3. Electro-Chemical Determination of the Antioxidant Activity
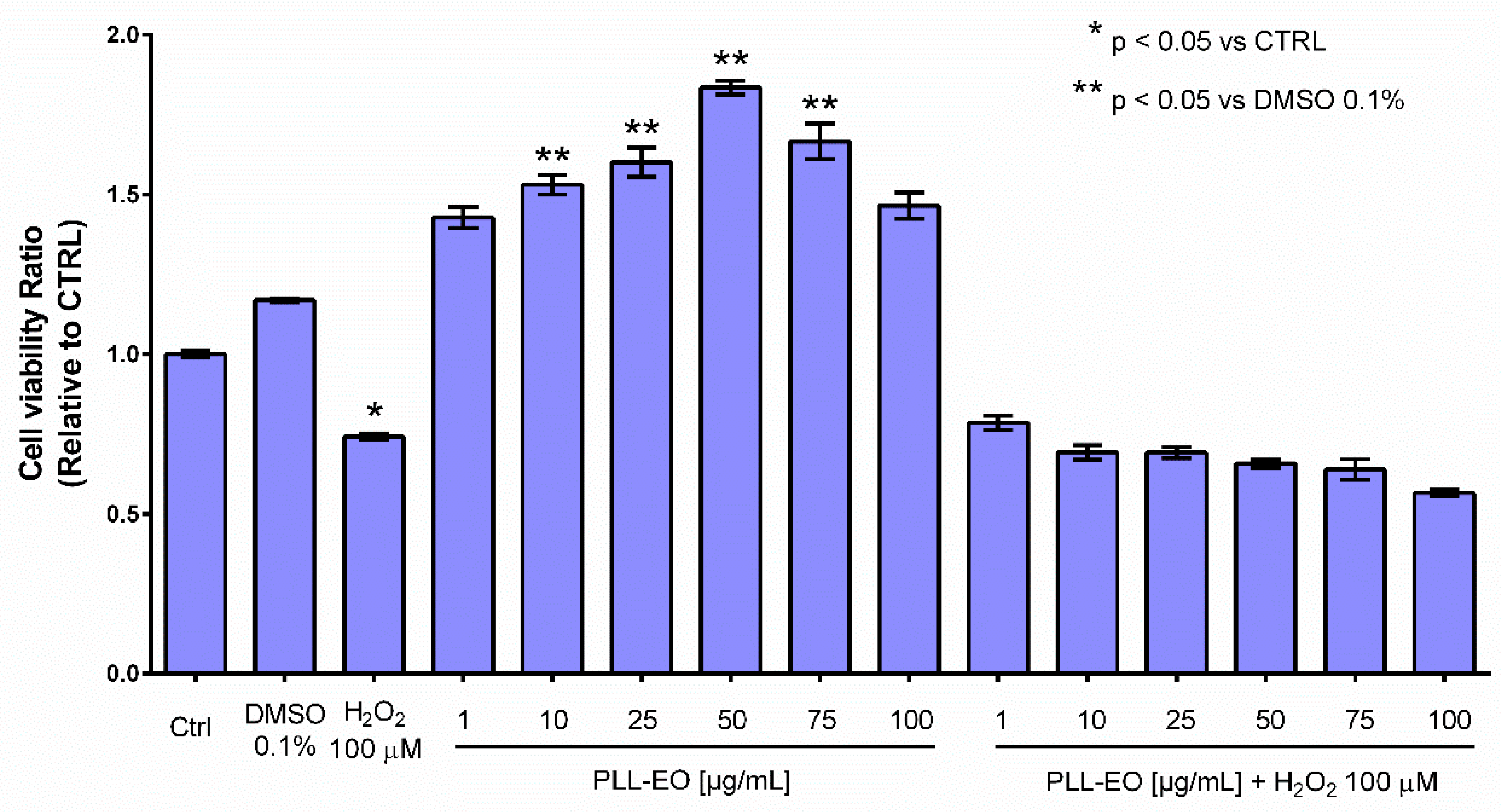
2.4. Viability Assay
2.5. Cytotoxicity Assay
3. Discussion
4. Materials and Methods
4.1. Chemicals and Abbreviations
4.2. Plant Material, Essential Oil Extraction, and GC/MS Characterization
4.3. Gas Chromatography -Mass Spectrometry (GC-MS) Analysis
4.4. Minimal Inhibitory Concentration Assay
4.5. Anti-Inflammatory Assays
4.5.1. COX-1/2 Inhibition
4.5.2. LOX Inhibition
4.5.3. Antioxidant Activity
4.6. Viability Assay
4.6.1. Cell origin, Culture, and Treatments
4.6.2. MTT Assay
4.7. Cytotoxicity Assay
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Papapanou, P.N.; Sanz, M.; Buduneli, N.; Dietrich, T.; Feres, M.; Fine, D.H.; Flemmig, T.F.; Garcia, R.; Giannobile, W.V.; Graziani, F.; et al. Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Periodontol. 2018, 89 (Suppl. 1), S173–S182. [Google Scholar] [CrossRef] [PubMed]
- Pinna, R.; Campus, G.; Cumbo, E.; Mura, I.; Milia, E. Xerostomia induced by radiotherapy: An overview of the physio-pathology, clinical evidence and management of the oral damage. Ther. Clin. Risk Manag. 2015, 4, 171–188. [Google Scholar] [CrossRef] [PubMed]
- Murakami, S.; Mealey, B.L.; Mariotti, A.; Chapple, I.L.C. Dental plaque-induced gingival conditions. J. Periodontol. 2018, 89 (Suppl. 1), S17–S27. [Google Scholar]
- Sharma, A. Virulence mechanisms of Tannerella forsythia. Periodontology 2000, 54, 106–116. [Google Scholar] [CrossRef]
- Chukkapalli, S.S.; Rivera-Kweh, M.F.; Velsko, I.M.; Chen, H.; Zheng, D.; Bhattacharyya, I.; Gangula, P.R.; Lucas, A.R.; Kesavalu, L. Chronic oral infection with major periodontal bacteria Tannerella forsythia modulates systemic atherosclerosis risk factors and inflammatory markers. FEMS Path. Dis. 2015, 73, ftv009. [Google Scholar] [CrossRef] [PubMed]
- Low, C.Y.; Rotstein, C. Emerging fungal infections in immunocompromised patients. F1000 Med. Rep. 2011, 3, 14. [Google Scholar] [CrossRef] [PubMed]
- Scott, S.G. Filler Candida–host cell receptor–ligand interactions. Curr. Opin. Microbiol. 2006, 9, 333–339. [Google Scholar]
- Richardson, J.P.; Moyes, D.L.; Ho, J.; Naglik, J.R. Candida innate immunity at the mucosa. Semin. Cell Dev. Biol. 2019, 89, 58–70. [Google Scholar] [CrossRef]
- Liu, X.; Wang, D.; Yu, C.; Li, T.; Liu, J.; Sun, S. Potential antifungal targets against a Candida biofilm based on an enzyme in the arachidonic acid cascade—A review. Front. Microbiol. 2016, 7, 1925. [Google Scholar] [CrossRef]
- Sanz, M.; Beighton, D.; Curtis, M.A.; Cury, J.A.; Dige, I.; Dommisch, H.; Ellwood, R.; Giacaman, R.A.; Herrera, D.; Herzberg, M.C.; et al. Role of microbial biofilms in the maintenance of oral health and in the development of dental caries and periodontal diseases. Consensus report of group 1 of the Joint EFP/ORCA workshop on the boundaries between caries and periodontal disease. J. Clin. Periodontol. 2017, 44 (Suppl. 18), S5–S11. [Google Scholar] [CrossRef]
- Cavaillon, J.M.; Adib-Conquy, M. The Pro-Inflammatory Cytokine Cascade. In Immune Response in the Critically Ill. Update in Intensive Care Medicine; Marshall, J.C., Cohen, J., Eds.; Springer: Berlin/Heidelberg, Germany, 2002; Volume 31, pp. 37–66. [Google Scholar]
- Rådmark, O.; Samuelsson, B. 5-Lipoxygenase: Mechanisms of regulation. J. Lipid Res. 2009, 50, S40–S45. [Google Scholar] [CrossRef] [PubMed]
- Miguel, M.G. Antioxidant and anti-inflammatory activities of essential oils: A short review. Molecules 2010, 15, 9252–9287. [Google Scholar] [CrossRef]
- Valeriani, F.; Protano, C.; Gianfranceschi, G.; Cozza, P.; Campanella, V.; Liguori, G.; Vitali, M.; Divizia, M.; Spica, V.R. Infection control in healthcare settings: Perspectives for mfDNA analysis in monitoring sanitation procedures. BMC Infect. Dis. 2016, 16, 394. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Maida, C.; Campus, G.; Piana, A.; Solinas, G.; Milia, E.; Castiglia, P. Periodontal status in an Italian young adult population. Prevalence and relationship with periodontopathic bacteria. New Microbiol. 2003, 26, 47–56. [Google Scholar] [PubMed]
- Bender, P.; Egger, A.; Westermann, M.; Taudte, N.; Sculean, A.; Potempa, J.; Möllerf, B.; Buchholz, M.; Eick, S. Expression of human and Porphyromonas gingivalis glutaminyl cyclases in periodontitis and rheumatoid arthritis–A pilot study. Arch. Oral Biol. 2019, 97, 223–230. [Google Scholar] [CrossRef]
- Campanella, V.; Oberti, L.; Gabrione, F.; González-Valero, L.; Hernández-Martínez, V.; Silvestre-Rangil, J. Periodontitis and cerebrovascular disease: A new novel in medicine. J. Biol. Regul. Homeost. Agents 2019, 33, 135–144. [Google Scholar]
- Mummolo, S.; Severino, M.; Campanella, V.; Barlattani, A., Jr.; Quinzi, V.; Marchetti, E. Chlorhexidine gel used as antiseptic in periodontal pockets. J. Biol. Regul. Homeost. Agents 2019, 33, 83–88. [Google Scholar]
- Hidalgo, E.; Dominguez, C. Mechanisms underlying chlorhexidine-induced cytotoxicity. Toxicol. In Vitro 2001, 15, 271–276. [Google Scholar] [CrossRef]
- Azzimonti, B.; Cochis, A.; El Beyrouthy, M.; Iriti, M.; Uberti, F.; Sorrentino, R.; Landini, M.M.; Rimondini, L.; Varoni, E.M. Essential oil from berries of Lebanese Juniperus excelsa M. Bieb displays similar antibacterial activity to chlorhexidine but higher cytocompatibility with human oral primary cells. Molecules 2015, 20, 9344–9357. [Google Scholar] [CrossRef]
- Müller, H.D.; Eick, S.; Moritz, A.; Lussi, A.; Gruber, R. Cytotoxicity and antimicrobial activity of oral rinses in vitro. Biomed. Res. Int. 2017, 2017, 4019723. [Google Scholar] [CrossRef]
- Coxib and Traditional NSAID Trialists’ (CNT) Collaboration; Bhala, N.; Emberson, J.; Merhi, A.; Abramson, S.; Arber, N.; Baron, J.A.; Bombardier, C.; Cannon, C.; Farkouh, M.E.; et al. Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: Meta-analyses of individual participant data from randomised trials. Lancet 2013, 382, 769–779. [Google Scholar]
- Clavé, S.; Rousset-Rouvière, C.; Daniel, L.; Tsimarotos, M. The invisible threat of non-steroidal anti-inflammatory drugs for kidneys. Front. Pediatr. 2019, 7, 520. [Google Scholar] [CrossRef] [PubMed]
- Blobaum, A.L.; Marnett, L.J. Structural and functional basis of cyclooxygenase inhibition. J. Med. Chem. 2007, 50, 1425–1441. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Antimicrobial Resistance: Global Report on Surveillance; World Health Organization: Geneva, Switzerland, 2014; ISBN 9789241564748. [Google Scholar]
- El-Meleigy, M.A.; Ahmed, M.E.; Arafa, R.A.; Ebrahim, N.A.; El-Kholany, E.E. Cytotoxicity of four oils on some human and bacterial cells. J. Appl. Sci. Environ. Sanit. 2010, 5, 143–159. [Google Scholar]
- Langhansova, L.; Landa, P.; Kutil, Z.; Tauchen, J.; Marsik, P.; Rezek, J.; Dong, L.J.; Yun, Z.L.; Vanek, T. Myrica rubra leaves as a potential source of a dual 5-LOX/COX inhibitor. Food Agric. Immunol. 2017, 28, 343–353. [Google Scholar] [CrossRef]
- Manconi, M.; Petretto, G.; D’hallewin, G.; Escribanod, E.; Milia, E.; Pinna, R.; Palmieri, A.; Firoznezhadg, M.; Perish, J.E.; Usachh, I.; et al. Thymus essential oil extraction, characterization and incorporation in phospholipid vesicles for the antioxidant/antibacterial treatment of oral cavity diseases. Colloids Surf. B Biointerfaces 2018, 171, 115–122. [Google Scholar] [CrossRef]
- Pinna, R.; Filigheddu, E.; Juliano, C.; Palmieri, A.; Manconi, M.; D’hallewin, G.; Petretto, G.; Maioli, M.; Caddeo, C.; Manca, M.L.; et al. Antimicrobial effect of Thymus capitatus and Citrus limon var. pompia as raw extracts and nanovesicles. Pharmaceutics 2019, 11, 234. [Google Scholar] [CrossRef]
- Gertsch, J.; Leonti, M.; Raduner, S.; Racz, I.; Chen, J.Z.; Xie, X.Q.; Altmann, K.H.; Karsak, M.; Zimmer, A. Beta caryophyllene is a dietary cannabinoid. Proc. Natl. Acad. Sci. USA 2008, 105, 9099–9104. [Google Scholar] [CrossRef]
- Russo, E.B. Taming THC: Potential cannabis synergy and phytocannabinoid- terpenoid entourage effects. Br. J. Pharmacol. 2011, 163, 1344–1364. [Google Scholar] [CrossRef]
- Nguyen, L.T.; Myslivečková, Z.; Szotáková, B.; Špičáková, A.; Lněničková, K.; Ambrož, M.; Kubíček, V.; Krasulová, K.; Anzenbacher, P.; Skálová, L. The inhibitory effects of β-caryophyllene, β-caryophyllene oxide and α-humulene on the activities of the main drug-metabolizing enzymes in rat and human liver in vitro. Chem. Biol. Interact. 2017, 25, 123–128. [Google Scholar] [CrossRef]
- Barra, A.; Coroneo, V.; Dessì, S.; Cabras, P.; Angioni, A. Characterization of the volatile constituents in the essential oil of Pistacia lentiscus L. from different origins and its antifungal and antioxidant activity. J. Agric. Food Chem. 2007, 22, 7093–7098. [Google Scholar] [CrossRef] [PubMed]
- Di Rosa, A. Erbe e Piante Medicinali in Sardegna, 3rd ed.; Carlo Delfino Ed.: Sassari, Italy, 2018. [Google Scholar]
- Quartu, M.; Serra, M.P.; Boi, M.; Pillolla, G.; Melis, T.; Poddighe, L.; Del Fiacco, M.; Falconieri, D.; Carta, G.; Murru, E.; et al. Effect of acute administration of Pistacia lentiscus L. essential oil on rat cerebral cortex following transient bilateral common carotid artery occlusion. Lipids Health Dis. 2012, 11, 8. [Google Scholar] [CrossRef] [PubMed]
- Orrù, G.; Demontis, C.; Mameli, A.; Tuveri, E.; Coni, P.; Pichiri, G.; Coghe, F.; Rosa, A.; Rossi, P.; D’hallewin, G. The selective interaction of Pistacia lentiscus Oil vs. human Streptococci, an old functional food revisited with new tools. Front. Microbiol. 2017, 8, 2067. [Google Scholar] [CrossRef] [PubMed]
- Barberis, A.; Spissu, Y.; Bazzu, G.; Fadda, A.; Azara, E.; Sanna, D.; Schirra, M.; Serra, P.A. Development and characterization of an ascorbate oxidase-based sensor–bio-sensor system for telemetric detection of AA and antioxidant capacity in fresh orange juice. Anal. Chem. 2014, 86, 8727–8734. [Google Scholar] [CrossRef]
- Buratti, S.; Scampicchio, M.; Giovanelli, G.; Mannino, S. A low-cost and low-tech electrochemical flow system for the evaluation of total phenolic content and antioxidant power of tea infusions. Talanta 2008, 75, 312–316. [Google Scholar] [CrossRef]
- Barroso, F.; de lo Santos Alvarez, N.; Delerue-Matos, C.; Oliveira, M.B. Towards a reliable technology for antioxidant capacity and oxidative damage evaluation: Electrochemical (bio) sensors. Biosens. Bioelectron. 2011, 30, 1–12. [Google Scholar] [CrossRef]
- Hughes, D.; Andersson, D.I. Evolutionary consequences of drug resistance: Shared principles across diverse targets and organisms. Nat. Rev. Genet. 2015, 16, 459–471. [Google Scholar] [CrossRef]
- Joshia, V.; Venkatesha, S.H.; Ramakrishnan, C.; Nanjaraj Urs, A.N.; Hiremath, V.; Moudgil, K.D.; Velmurugan, D.; Vishwanath, B.S. Celastrol modulates inflammation through inhibition of the catalytic activity of mediators of arachidonic acid pathway: Secretory phospholipase A2 group IIA, 5-lipoxygenase and cyclooxygenase-2. Pharmacol. Res. 2016, 113, 265–275. [Google Scholar] [CrossRef]
- Barberis, A.; Bazzu, G.; Calia, G.; Puggioni, G.M.; Rocchitta, G.G.; Migheli, R.; Schirra, M.; Desole, M.S.; Serra, P.A. New ultralow-cost telemetric system for a rapid electronchemical detection of vitamin C in fresch orange juice. Anal. Chem. 2010, 82, 5134–5140. [Google Scholar] [CrossRef]
- Fadda, A.; Sanna, D. Advantages and pitfalls of the methods for the antioxidant activity evaluation. In Advances in Food Analysis Research; Nova Science Publisher, Inc.: Hauppauge, NY, USA, 2015; pp. 65–88. [Google Scholar]
- Bullitta, S.; Piluzza, G.; Manunta, M.D.I. Cell-based and chemical assays of the ability to modulate the production of intracellular Reactive Oxygen Species of eleven Mediterranean plant species related to ethnobotanic traditions. Genet. Resour. Crop Evol. 2013, 60, 403–412. [Google Scholar] [CrossRef]
- Duru, M.E.; Cakir, A.; Kordali, S.; Zengin, H.; Harmandar, M.; Izumi, S.; Hirata, T. Chemical composition and antifungal properties of essential oils of three Pistacia species. Fitoterapia 2003, 74, 170–176. [Google Scholar] [CrossRef]
- Sharma, S.; Gupta, J.; Prabhakar, P.K.; Gupta, P.; Solanki, P.; Rajput, A. Phytochemical repurposing of natural molecule: Sabinene for identification of novel therapeutic benefits using in silico and in vitro approaches. Assay Drug Dev. Technol. 2019, 17, 339–351. [Google Scholar] [CrossRef] [PubMed]
- de Sousa, E.L.; Farias, T.C.; Ferreira, S.B.; Ferreira, P.B.; Lima, Z.N.; Ferreira, S.B. Antibacterial Activity and Time-kill Kinetics of Positive Enantiomer of α-pinene Against Strains of Staphylococcus aureus and Escherichia coli. Curr. Top. Med. Chem. 2018, 18, 917–924. [Google Scholar] [CrossRef] [PubMed]
- Bouzenna, H.; Hfaiedh, N.; Giroux-Metges, M.A.; Elfeki, A.; Talarmin, H. Potential protective effects of alpha-pinene against cytotoxicity caused by aspirin in the IEC-6 cells. Biomed. Pharmacother. 2017, 93, 961–968. [Google Scholar] [CrossRef] [PubMed]
- Turchetti, P.; Pinelli, P.; Buzzini, A.; Romani, D.; Heimler, F.; Franconi, F.; Martini, A. In vitro antimycotic activity of some plant extracts towards yeast and yeast-like strains. Phytother. Res. 2005, 19, 44–49. [Google Scholar] [CrossRef]
- Karygianni, L.; Cecere, M.; Argyropoulou, A.; Hellwig, E.; Skaltsounis, A.L.; Wittmer, A.; Tchorz, J.P.; Al-Ahmad, A. Compounds from Olea europaea and Pistacia lentiscus inhibit oral microbial growth. BMC Complement. Altern. Med. 2019, 26, 51. [Google Scholar] [CrossRef]
- Tabenski, L.; Maisch, T.; Santarelli, F.; Hiller, K.A. Schmalz Individual growth detection of bacterial species in an in vitro oral polymicrobial biofilm model. Arch. Microbiol. 2014, 196, 819–828. [Google Scholar] [CrossRef]
- Rajendran, R.; Sherry, L.; Deshpande, A.; Johnson, E.M.; Hanson, M.F.; Williams, C.; Munro, C.A.; Jones, B.L.; Ramage, G. A prospective surveillance study of Candidaemia: Epidemiology, risk factors, antifungal treatment and outcome in hospitalized patients. Front. Microbiol. 2016, 7, 915. [Google Scholar] [CrossRef]
- Zhou, Y.; Wang, G.; Li, Y.; Liu, Y.; Song, Y.; Zheng, W.; Zhang, N.; Hu, X.; Yan, S.; Jia, J. In vitro interactions between aspirin and amphotericin B against planktonic cells and biofilm cells of Candida albicans and C. parapsilosis. Antimicrob. Agents Chemother. 2012, 56, 3250–3260. [Google Scholar] [CrossRef]
- Farmacopea Ufficiale della Repubblica Italiana, 12th ed.; Istituto Poligrafico e Zecca dello Stato: Roma, Italy, 2008.
- Adams, R.P. Identification of Essential Oil Components by Gas Chromatography/Quadrupole Mass Spectrometry, 3rd ed.; Allured Publ. Corp.: Carol Stream, IL, USA, 2007; pp. 7093–7098. [Google Scholar]
- Milia, E.; Castelli, G.; Bortone, A.; Sotgiu, G.; Manunta, A.; Pinna, R.; Gallina, G. Short-term response of three resin-based materials as desensitizing agents under oral environmental exposure. Acta Odontol. Scand. 2013, 71, 599–609. [Google Scholar] [CrossRef]
- Ruzza, P.; Siligardi, G.; Hussain, R.; Marchiani, A.; Islami, M.; Bubacco, L.; Delogu, G.; Fabbri, D.; Dettori, M.A.; Sechi, M.; et al. Ceftriaxone blocks the polymerization of α-synuclein and exerts neuroprotective effects in vitro. ACS Chem. Neurosci. 2014, 15, 30–38. [Google Scholar] [CrossRef] [PubMed]

| RI apol Sper | RI apol Lett | Constituents | % | ID * |
|---|---|---|---|---|
| 924 | 927 | tricyclene | 0.24 ± 0.01 | MS-RI |
| 930 | 931 | α-thujene | 0.23 ± 0.01 | Std |
| 939 | 937 | α-pinene | 16.89 ± 0.15 | Std |
| 955 | 956 | camphene | 1.04 ± 0.04 | Std |
| 977 | 975 | sabinene | 7.73 ± 0.11 | Std |
| 981 | 979 | β-pinene | 4.30 ± 0.05 | Std |
| 992 | 991 | β-myrcene | 0.87 ± 0.02 | Std |
| 1005 | 1003 | α-phellandrene | 7.39 ± 0.12 | Std |
| 1015 | 1017 | α-terpinene | 4.79 ± 0.04 | Std |
| 1025 | 1025 | p-cymene | 1.10 ± 0.03 | Std |
| 1027 | 1029 | limonene | 3.89 ± 0.07 | Std |
| 1031 | 1030 | β-phellandrene | 4.71 ± 0.05 | MS-RI |
| 1035 | 1037 | Cis-β-ocimene | 0.24 ± 0.02 | MS-RI |
| 1056 | 1056 | isoamyl isobutyrate | 0.55 ± 0.02 | MS-RI |
| 1056 | 1056 | 2-methylbuthyl butanoate | 0.18 ± 0.01 | Std |
| 1064 | 1060 | γ-terpinene | 6.30 ± 0.09 | Std |
| 1087 | 1089 | terpinolene | 3.25 ± 0.02 | MS-RI |
| 1090 | 1091 | p-cymenene | 0.12 ± 0.01 | MS-RI |
| 1094 | 1094 | isopentyl isivalerate | 0.13 ± 0.01 | MS-RI |
| 1108 | 1108 | n-amyl isovalerate | 0.04 ± 0.01 | MS-RI |
| 1115 | 1117 | fenchol | 0.11 ± 0.01 | MS-RI |
| 1147 | 1144 | Cis-β-terpineol | 0.13 ± 0.01 | Std |
| 1166 | 1169 | borneol-endo | 0.16 ± 0.01 | Std |
| 1181 | 1177 | terpinen-4-ol | 16.49 ± 0.18 | MS-RI |
| 1187 | 1189 | α-terpineol | 3.98 ± 0.07 | MS-RI |
| 1194 | 1199 | γ-terpineol | 0.07 ± 0.01 | MS-RI |
| 1242 | 1238 | isopentyl hexanoate | 0.24 ± 0.02 | MS-RI |
| 1247 | 1247 | 2-methylbuthyl hexanoate | 0.17 ± 0.01 | Std |
| 1258 | 1253 | piperitone | 0.05 ± 0.01 | Std |
| 1294 | 1294 | 2-undecanone | 0.85 ± 0.03 | MS-RI |
| 1355 | 1351 | α-cubebene | 0.05 ± 0.01 | Std |
| 1378 | 1377 | α-copaene | 0.24 ± 0.01 | MS-RI |
| 1380 | 1382 | β-maaliene | 0.33 ± 0.02 | MS-RI |
| 1407 | 1409 | (Z)-caryophyllene | 1.39 ± 0.06 | MS-RI |
| 1419 | 1419 | (E)-caryophyllene | 0.07 ± 0.01 | Std |
| 1457 | 1460 | alloaromadendrene | 0.14 ± 0.01 | Std |
| 1480 | 1480 | γ-muurolene | 0.57 ± 0.03 | Std |
| 1485 | 1485 | α-amorfene | 0.07 ± 0.01 | MS-RI |
| 1486 | 1485 | germacrene D | 2.73 ± 0.11 | MS-RI |
| 1497 | 1499 | Cis-dihydro apofarnesal | 0.14 ± 0.01 | MS-RI |
| 1502 | 1500 | α-muurolene | 0.53 ± 0.02 | Std |
| 1509 | 1506 | β-bisabolene | 0.19 ± 0.01 | MS-RI |
| 1521 | 1523 | δ-cadinene | 1.43 ± 0.04 | MS-RI |
| 1535 | 1535 | Trans-cadina-1(2),4-diene | 0.15 ± 0.01 | Std |
| 1539 | 1539 | α-cadinene | 0.07 ± 0.01 | Std |
| 1552 | 1552 | Cis-muurol-5-en-4-β-ol | 0.07 ± 0.01 | Std |
| 1535 | 1535 | Trans-cadin-4-en-7-ol | 0.31 ± 0.02 | Std |
| 1639 | 1640 | epi-α-cadinol | 1.22 ± 0.08 | Std |
| 1644 | 1646 | α-muurolol | 0.94 ± 0.04 | Std |
| 1648 | 1652 | cedr-8(15)-en-9-α-ol | 0.12 ± 0.01 | Std |
| 96.96 |
| Strain | Origin | MIC (µg/mL PLL-EO) |
|---|---|---|
| Streptococcus gordonii ATCC 10558 | Laboratory | 12.5 |
| Actinomyces naeslundii ATCC 12104 | Laboratory | 3.13 |
| Fusobacterium nucleatum ATCC 25586 | Laboratory | 6.25 |
| Porphyromonas gingivalis ATCC 33277 | Laboratory | 3.13 |
| P. gingivalis BeOR6 | Clinical isolate | 1.63 |
| P. gingivalis BeOR14 | Clinical isolate | 1.63 |
| Tannerella forsythia ATCC 43330 | Laboratory | 3.13 |
| T. forsythia Be13237 | Clinical isolate | 1.63 |
| T. forsythia Be13216 | Clinical isolate | 3.13 |
| Candida albicans ATCC 76615 | Laboratory | 12.5 |
| C. albicans BeT41 | Clinical isolate | 12.5 |
| C. albicans BeT603 | Clinical isolate | 12.5 |
| Candida glabrata DSM 6425 | Laboratory | 6.25 |
| C. glabrata Be10183 | Clinical isolate | 6.25 |
| C. glabrata Be184 | Clinical isolate | 6.25 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Milia, E.; Usai, M.; Szotáková, B.; Elstnerová, M.; Králová, V.; D’hallewin, G.; Spissu, Y.; Barberis, A.; Marchetti, M.; Bortone, A.; et al. The Pharmaceutical Ability of Pistacia lentiscus L. Leaves Essential Oil Against Periodontal Bacteria and Candida sp. and Its Anti-Inflammatory Potential. Antibiotics 2020, 9, 281. https://doi.org/10.3390/antibiotics9060281
Milia E, Usai M, Szotáková B, Elstnerová M, Králová V, D’hallewin G, Spissu Y, Barberis A, Marchetti M, Bortone A, et al. The Pharmaceutical Ability of Pistacia lentiscus L. Leaves Essential Oil Against Periodontal Bacteria and Candida sp. and Its Anti-Inflammatory Potential. Antibiotics. 2020; 9(6):281. https://doi.org/10.3390/antibiotics9060281
Chicago/Turabian StyleMilia, Egle, Marianna Usai, Barbora Szotáková, Marie Elstnerová, Věra Králová, Guy D’hallewin, Ylenia Spissu, Antonio Barberis, Mauro Marchetti, Antonella Bortone, and et al. 2020. "The Pharmaceutical Ability of Pistacia lentiscus L. Leaves Essential Oil Against Periodontal Bacteria and Candida sp. and Its Anti-Inflammatory Potential" Antibiotics 9, no. 6: 281. https://doi.org/10.3390/antibiotics9060281
APA StyleMilia, E., Usai, M., Szotáková, B., Elstnerová, M., Králová, V., D’hallewin, G., Spissu, Y., Barberis, A., Marchetti, M., Bortone, A., Campanella, V., Mastandrea, G., Langhansová, L., & Eick, S. (2020). The Pharmaceutical Ability of Pistacia lentiscus L. Leaves Essential Oil Against Periodontal Bacteria and Candida sp. and Its Anti-Inflammatory Potential. Antibiotics, 9(6), 281. https://doi.org/10.3390/antibiotics9060281