Monoclonal Antibodies as an Antibacterial Approach Against Bacterial Pathogens
Abstract
1. Introduction
2. Antibacterial Antibodies—Previous Success
3. Previous Failures Lead to Current Success
4. Future and Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Hubbert, W.R. Comparative Statistics of Antitoxin Horses. A Study of the Records of One Hundred Horses Immunized To Diphtheria Toxin, With Composite of Curves. J. Exp. Med. 1905, 7, 176–182. [Google Scholar] [CrossRef] [PubMed]
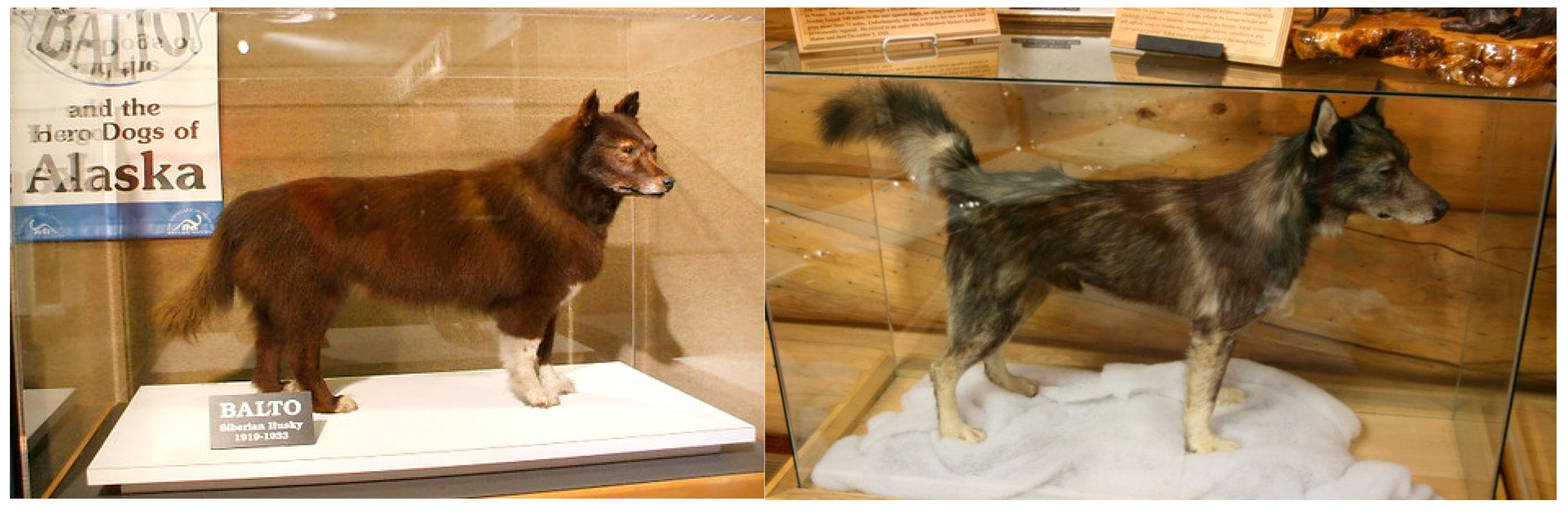
- Crane, L. In 1925, a Remote Town Was Saved from Lethal Disease by Dogs. Available online: http://www.bbc.com/earth/story/20161014-in-1925-a-remote-town-was-saved-from-lethal-disease-by-dogs (accessed on 13 January 2020).
- Casadevall, A.; Scharff, M.D. Serum Therapy Revisited: Animal Models of Infection and Development of Passive Antibody Therapy. Antimicrob. Agents Chemother. 1994, 38, 1695–1702. [Google Scholar] [CrossRef] [PubMed]
- Casadevall, A. Antibody-based therapies for emerging infectious diseases. Emerg. Infect. Dis. 1996, 2, 200–208. [Google Scholar] [CrossRef] [PubMed]
- Lewis, K. Platforms for antibiotic discovery. Nat. Rev. Drug Discov. 2013, 12, 371–387. [Google Scholar] [CrossRef] [PubMed]
- Köhler, G.; Milstein, C. Continuous Cultures of Fused Cells Secreting Antibody of predefined specificity. Nature 1975, 256, 495–497. [Google Scholar] [CrossRef] [PubMed]
- Zurawski, V.R., Jr.; Haber, E.; Black, P.H. Production of Antibody to Tetanus Toxoid by Continuous Human Lymphoblastoid Cell Lines. Science 1978, 199, 1439–1441. [Google Scholar] [CrossRef]
- Riechmann, L.; Clark, M.; Waldmann, H.; Winter, G. Reshaping human antibodies for therapy. Nature 1988, 332, 323–327. [Google Scholar] [CrossRef]
- Wright, A.; Shin, S.; Morrison, S.L. Genetically engineered antibodies: Progress and prospects. Crit. Rev. Immunol. 1992, 12, 125–168. [Google Scholar]
- Robert-Guroff, M.; Brown, M.; Gallo, R.C. HTLV-III-neutralizing Antibodies in Patients With AIDS and AIDS-related Complex. Nature 1985, 316, 72–74. [Google Scholar] [CrossRef]
- Hey, A. History and Practice: Antibodies in Infectious Diseases. Microbiol. Spectr. 2015, 3, 2. [Google Scholar] [CrossRef]
- Glanville, J.; Zhai, W.; Berka, J.; Telman, D.; Huerta, G.; Mehta, G.R.; Ni, I.; Mei, L.; Sundar, P.D.; Day, G.M.R. Precise determination of the diversity of a combinatorial antibody library gives insight into the human immunoglobulin repertoire. Proc. Natl. Acad. Sci. USA 2009, 106, 20216–20221. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Nowak, C.; Andrien, B.; Shao, M.; Ponniah, G.; Neill, A. Impact of IgG Fc-Oligosaccharides on Recombinant Monoclonal Antibody Structure, Stability, Safety, and Efficacy. Biotechnol. Prog. 2017, 33, 1173–1181. [Google Scholar] [CrossRef]
- Walker, L.M.; Burton, D.R. Passive immunotherapy of viral infections: ‘super-antibodies’ enter the fray. Nat. Rev. Immunol. 2018, 18, 297–308. [Google Scholar] [CrossRef] [PubMed]
- Liikanen, I.; Tähtinen, S.; Guse, K.; Gutmann, T.; Savola, P.; Oksanen, M.; Kanerva, A.; Hemminki, A. Oncolytic Adenovirus Expressing Monoclonal Antibody Trastuzumab for Treatment of HER2-Positive Cancer. Mol. Cancer Ther. 2016, 15, 2259–2269. [Google Scholar] [CrossRef] [PubMed]
- Limberis, M.P. Intranasal antibody gene transfer in mice and ferrets elicits broad protection against pandemic influenza. Sci. Transl. Med. 2013, 5, 187. [Google Scholar] [CrossRef] [PubMed]
- Flingai, S.; Plummer, E.M.; Patel, A.; Shresta, S.; Mendoza, J.M.; Broderick, K.E.; Sardesai, N.Y.; Muthumani, K.; Weiner, D.B. Protection Against Dengue Disease by Synthetic Nucleic Acid Antibody Prophylaxis/Immunotherapy. Sci. Rep. 2015, 5, 12616. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.; DiGiandomenico, A.; Keller, A.E.; Smith, T.R.F.; Park, D.H.; Ramos, S.; Schultheis, K.; Elliott, S.T.C.; Mendoza, J.; Broderick, K.E. An Engineered Bispecific DNA-encoded IgG Antibody Protects against Pseudomonas aeruginosa in a Pneumonia Challenge Model. Nat. Commun. 2017, 8, 637. [Google Scholar] [CrossRef]
- Heesterbeek, D.A.C.; Angelier, M.L.; Harrison, R.A.; Rooijakkers, S.H.M. Complement and Bacterial Infections: From Molecular Mechanisms to Therapeutic Applications. J. Innate Immun. 2018, 10, 455–464. [Google Scholar] [CrossRef]
- Storek, K.M.; Auerbach, M.R.; Shi, H.; Garcia, N.K.; Sun, D.; Nickerson, N.N.; Vij, R.; Lin, Z.; Chiang, N.; Schneider, K.; et al. Monoclonal antibody targeting the β-barrel assembly machine of Escherichia coli is bactericidal. Proc. Natl. Acad. Sci. USA 2018, 115, 3692–3697. [Google Scholar] [CrossRef]
- Dunn-Siegrist, I.; Leger, O.; Daubeuf, B.; Poitevin, Y.; Dépis, F.; Herren, S.; Kosco-Vilbois, M.; Dean, Y.; Pugin, J.; Elson, G. Pivotal involvement of Fcgamma receptor IIA in the neutralization of lipopolysaccharide signaling via a potent novel anti-TLR4 monoclonal antibody 15C1. J. Biol. Chem. 2007, 282, 34817–34827. [Google Scholar] [CrossRef]
- Vij, R.; Lin, Z.; Chiang, N.; Vernes, J.M.; Storek, K.M.; Park, S.; Chan, J.; Meng, Y.G.; Comps-Agrar, L.; Luan, P.; et al. A targeted boost-and-sort immunization strategy using Escherichia coli BamA identifies rare growth inhibitory antibodies. Sci. Rep. 2018, 8, 7136. [Google Scholar] [CrossRef] [PubMed]
- Tursi, S.A.; Puligedda, R.D.; Szabo, P.; Nicastro, L.K.; Miller, A.L.; Qiu, C.; Gallucci, S.; Relkin, N.R.; Buttaro, B.A.; Dessain, S.K.; et al. Salmonella Typhimurium biofilm disruption by a human antibody that binds a pan-amyloid epitope on curli. Nat. Commun. 2020, 11, 1007. [Google Scholar] [CrossRef]
- Novotny, L.A.; Jurcisek, J.A.; Goodman, S.D.; Bakaletz, L.O. Monoclonal antibodies against DNA-binding tips of DNABII proteins disrupt biofilms in vitro and induce bacterial clearance in vivo. EBioMedicine 2016, 10, 33–44. [Google Scholar] [CrossRef] [PubMed]
- Kaizuka, K.; Hosogi, Y.; Hayakawa, M.; Shibata, Y.; Abiko, Y. Human monoclonal antibody inhibits Porphyromonas gingivalis hemagglutinin activity. J. Periodontol. 2003, 74, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, W.; Sethi, S.; Darji, A.; Mraheil, M.A.; Hain, T.; Chakraborty, T. Antibody targeting the ferritin-like protein controls Listeria infection. Infect. Immun. 2010, 78, 3306–3314. [Google Scholar] [CrossRef][Green Version]
- Bennett, M.R.; Dong, J.; Bombardi, R.G.; Soto, C.; Parrington, H.M.; Nargi, R.S.; Schoeder, C.T.; Nagel, M.B.; Schey, K.L.; Meiler, J.; et al. Human VH1-69 Gene-Encoded Human Monoclonal Antibodies against Staphylococcus aureus IsdB Use at Least Three Distinct Modes of Binding to Inhibit Bacterial Growth and Pathogenesis. mBio 2019, 10. [Google Scholar] [CrossRef]
- Singh, K.V.; Pinkston, K.L.; Gao, P.; Harvey, B.R.; Murray, B.E. Anti-Ace monoclonal antibody reduces Enterococcus faecalis aortic valve infection in a rat infective endocarditis model. Pathog. Dis. 2018, 76, 8. [Google Scholar] [CrossRef]
- Aye, R.; Weldearegay, Y.B.; Lutta, H.O.; Chuma, F.; Pich, A.; Jores, J.; Meens, J.; Naessens, J. Identification of targets of monoclonal antibodies that inhibit adhesion and growth in Mycoplasma mycoides subspecies mycoides. Vet. Immunol. Immunopathol. 2018, 204, 11–18. [Google Scholar] [CrossRef]
- Aguilar, J.L.; Varshney, A.K.; Pechuan, X.; Dutta, K.; Nosanchuk, J.D.; Fries, B.C. Monoclonal antibodies protect from Staphylococcal Enterotoxin K (SEK) induced toxic shock and sepsis by USA300 Staphylococcus aureus. Virulence 2017, 8, 741–750. [Google Scholar] [CrossRef]
- Iwamoto, R.; Senoh, H.; Okada, Y.; Uchida, T.; Mekada, E. An antibody that inhibits the binding of diphtheria toxin to cells revealed the association of a 27-kDa membrane protein with the diphtheria toxin receptor. J. Biol. Chem. 1991, 266, 20463–20469. [Google Scholar]
- Diago-Navarro, E.; Calatayud-Baselga, I.; Sun, D.; Khairallah, C.; Mann, I.; Ulacia-Hernando, A.; Sheridan, B.; Shi, M.; Fries, B.C. Antibody-Based Immunotherapy To Treat and Prevent Infection with Hypervirulent Klebsiella pneumoniae. Clin. Vaccine Immunol. 2017, 24. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, T.B.; Pantapalangkoor, P.; Luna, B.M.; Bruhn, K.W.; Yan, J.; Dekitani, K.; Hsieh, S.; Yeshoua, B.; Pascual, B.; Vinogradov, E.; et al. Monoclonal Antibody Protects Against Acinetobacter baumannii Infection by Enhancing Bacterial Clearance and Evading Sepsis. J. Infect. Dis. 2017, 216, 489–501. [Google Scholar] [CrossRef] [PubMed]
- Gulati, S.; Beurskens, F.J.; de Kreuk, B.J.; Roza, M.; Zheng, B.; DeOliveira, R.B.; Shaughnessy, J.; Nowak, N.A.; Taylor, R.P.; Botto, M.; et al. Complement alone drives efficacy of a chimeric antigonococcal monoclonal antibody. PLoS Biol. 2019, 17, e3000323. [Google Scholar] [CrossRef]
- Visan, L.; Rouleau, N.; Proust, E.; Peyrot, L.; Donadieu, A.; Ochs, M. Antibodies to PcpA and PhtD protect mice against Streptococcus pneumoniae by a macrophage- and complement-dependent mechanism. Hum. Vaccines Immunother. 2018, 14, 489–494. [Google Scholar] [CrossRef]
- Resch, B. Product Review on the Monoclonal Antibody Palivizumab for Prevention of Respiratory Syncytial Virus Infection. Hum. Vaccines Immunother. 2017, 13, 2138–2149. [Google Scholar] [CrossRef]
- Nagy, C.F.; Leach, T.S.; Hoffman, J.H.; Czech, A.; Carpenter, S.E.; Guttendorf, R. Pharmacokinetics and Tolerability of Obiltoxaximab: A Report of 5 Healthy Volunteer Studies. Clin. Ther. 2016, 38, 2083–2097. [Google Scholar] [CrossRef]
- Allio, T. The FDA Animal Rule and its role in protecting human safety. Exp. Opin. Drug Saf. 2018, 17, 971–973. [Google Scholar] [CrossRef] [PubMed]
- Biron, B.; Beck, K.; Dyer, D.; Mattix, M.; Twenhafel, N.; Nalca, A. Efficacy of ETI-204 monoclonal antibody as an adjunct therapy in a New Zealand white rabbit partial survival model for inhalational anthrax. Antimicrob. Agents Chemother. 2015, 59, 2206–2214. [Google Scholar] [CrossRef] [PubMed]
- Henning, L.N.; Carpenter, S.; Stark, G.V.; Serbina, N.V. Development of Protective Immunity in New Zealand White Rabbits Challenged with Bacillus anthracis Spores and Treated with Antibiotics and Obiltoxaximab, a Monoclonal Antibody against Protective Antigen. Antimicrob. Agents Chemother. 2018, 62. [Google Scholar] [CrossRef]
- Wilcox, M.H.; Gerding, D.N.; Poxton, I.R.; Kelly, C.; Nathan, R.; Birch, T.; Cornely, O.A.; Rahav, G.; Bouza, E.; Lee, C.; et al. Bezlotoxumab for Prevention of Recurrent Clostridium difficile Infection. N. Engl. J. Med. 2017, 376, 305–317. [Google Scholar] [CrossRef]
- Yang, Z.; Ramsey, J.; Hamza, T.; Zhang, Y.; Li, S.; Yfantis, H.G.; Lee, D.; Hernandez, L.D.; Seghezzi, W.; Furneisen, J.M.; et al. Mechanisms of protection against Clostridium difficile infection by the monoclonal antitoxin antibodies actoxumab and bezlotoxumab. Infect. Immun. 2015, 83, 822–831. [Google Scholar] [CrossRef] [PubMed]
- Džunková, M.; D’Auria, G.; Xu, H.; Huang, J.; Duan, Y.; Moya, A.; Kelly, C.P.; Chen, X. The Monoclonal Antitoxin Antibodies (Actoxumab-Bezlotoxumab) Treatment Facilitates Normalization of the Gut Microbiota of Mice with Clostridium difficile Infection. Front. Cell Infect. Microbiol. 2016, 6, 119. [Google Scholar] [CrossRef] [PubMed]
- Baer, M.; Sawa, T.; Flynn, P.; Luehrsen, K.; Martinez, D.; Wiener-Kronish, J.P.; Yarranton, G.; Bebbington, C. An engineered human antibody fab fragment specific for Pseudomonas aeruginosa PcrV antigen has potent antibacterial activity. Infect. Immun. 2009, 77, 1083–1090. [Google Scholar] [CrossRef] [PubMed]
- Jain, R.; Beckett, V.V.; Konstan, M.W.; Accurso, F.J.; Burns, J.L.; Mayer-Hamblett, N.; Milla, C.; VanDevanter, D.R.; Chmiel, J.F. KB001-A Study Group. KB001-A, a novel anti-inflammatory, found to be safe and well-tolerated in cystic fibrosis patients infected with Pseudomonas aeruginosa. J. Cyst. Fibros. 2018, 17, 484–491. [Google Scholar] [CrossRef] [PubMed]
- Sause, W.E.; Buckley, P.T.; Strohl, W.R.; Lynch, A.S.; Torres, V.J. Antibody-Based Biologics and Their Promise to Combat Staphylococcus aureus Infections. Trends Pharmacol. Sci. 2016, 37, 231–241. [Google Scholar] [CrossRef]
- Del Pozo, J.L. Biofilm-related disease. Exp. Rev. Anti Infect. Ther. 2018, 16, 51–65. [Google Scholar] [CrossRef]
- Gollan, B.; Grabe, G.; Michaux, C.; Helaine, S. Bacterial Persisters and Infection: Past, Present, and Progressing. Ann. Rev. Microbiol. 2019, 73, 359–385. [Google Scholar] [CrossRef]
- Ryser, S.; Tenorio, E.; Estellés, A.; Kauvar, L.M. Human antibody repertoire frequently includes antibodies to a bacterial biofilm associated protein. PLoS ONE 2019, 14, e0219256. [Google Scholar] [CrossRef]
- Diep, B.A.; Hilliard, J.J.; Le, V.T.; Tkaczyk, C.; Le, H.N.; Tran, V.G.; Rao, R.L.; Dip, E.C.; Pereira-Franchi, E.P.; Cha, P.; et al. Targeting Alpha Toxin To Mitigate Its Lethal Toxicity in Ferret and Rabbit Models of Staphylococcus aureus Necrotizing Pneumonia. Antimicrob. Agents Chemother. 2017, 61. [Google Scholar] [CrossRef]
- Hua, L.; Cohen, T.S.; Shi, Y.; Datta, V.; Hilliard, J.J.; Tkaczyk, C.; Suzich, J.; Stover, C.K.; Sellman, B.R. MEDI4893* Promotes Survival and Extends the Antibiotic Treatment Window in a Staphylococcus aureus Immunocompromised Pneumonia Model. Antimicrob. Agents Chemother. 2015, 59, 4526–4532. [Google Scholar] [CrossRef]
- Hilliard, J.J.; Datta, V.; Tkaczyk, C.; Hamilton, M.; Sadowska, A.; Jones-Nelson, O.; O’Day, T.; Weiss, W.J.; Szarka, S.; Nguyen, V.; et al. Anti-alpha-toxin monoclonal antibody and antibiotic combination therapy improves disease outcome and accelerates healing in a Staphylococcus aureus dermonecrosis model. Antimicrob. Agents Chemother. 2015, 59, 299–309. [Google Scholar] [CrossRef]
- Ortines, R.V.; Wang, Y.; Liu, H.; Dikeman, D.A.; Pinsker, B.L.; Miller, R.J.; Kim, S.E.; Ackerman, N.E.; Rizkallah, J.F.; Marcello, L.T.; et al. Efficacy of a Multimechanistic Monoclonal Antibody Combination against Staphylococcus aureus Surgical Site Infections in Mice. Antimicrob. Agents Chemother. 2019, 63. [Google Scholar] [CrossRef]
- Ortines, R.V.; Liu, H.; Cheng, L.I.; Cohen, T.S.; Lawlor, H.; Gami, A.; Wang, Y.; Dillen, C.A.; Archer, N.K.; Miller, R.J.; et al. Neutralizing Alpha-Toxin Accelerates Healing of Staphylococcus aureus-Infected Wounds in Nondiabetic and Diabetic Mice. Antimicrob. Agents Chemother. 2018, 62. [Google Scholar] [CrossRef]
- DiGiandomenico, A.; Keller, A.E.; Gao, C.; Rainey, G.J.; Warrener, P.; Camara, M.M.; Bonnell, J.; Fleming, R.; Bezabeh, B.; Dimasi, N.; et al. A multifunctional bispecific antibody protects against Pseudomonas aeruginosa. Sci. Transl. Med. 2014, 6, 262. [Google Scholar] [CrossRef]
- Zegans, M.E.; DiGiandomenico, A.; Ray, K.; Naimie, A.; Keller, A.E.; Stover, C.K.; Lalitha, P.; Srinivasan, M.; Acharya, N.R.; Lietman, T.M. Association of Biofilm Formation, Psl Exopolysaccharide Expression, and Clinical Outcomes in Pseudomonas aeruginosa Keratitis: Analysis of Isolates in the Steroids for Corneal Ulcers Trial. JAMA Ophthalmol. 2016, 134, 383–389. [Google Scholar] [CrossRef]
- Byrd, M.S.; Pang, B.; Hong, W.; Waligora, E.A.; Juneau, R.A.; Armbruster, C.E.; Weimer, K.E.; Murrah, K.; Mann, E.E.; Lu, H.; et al. Direct evaluation of Pseudomonas aeruginosa biofilm mediators in a chronic infection model. Infect. Immun. 2011, 79, 3087–3095. [Google Scholar] [CrossRef]
- Ali, S.O.; Yu, X.Q.; Robbie, G.J.; Wu, Y.; Shoemaker, K.; Yu, L.; DiGiandomenico, A.; Keller, A.E.; Anude, C.; Hernandez-Illas, M.; et al. Phase 1 study of MEDI3902, an investigational anti-Pseudomonas aeruginosa PcrV and Psl bispecific human monoclonal antibody, in healthy adults. Clin. Microbiol. Infect. 2019, 25, 629. [Google Scholar] [CrossRef] [PubMed]
- Le, H.N.; Tran, V.G.; Vu, T.T.T.; Gras, E.; Le, V.T.M.; Pinheiro, M.G.; Aguiar-Alves, F.; Schneider-Smith, E.; Carter, H.C.; Sellman, B.R.; et al. Treatment Efficacy of MEDI3902 in Pseudomonas aeruginosa Bloodstream Infection and Acute Pneumonia Rabbit Models. Antimicrob. Agents Chemother. 2019, 63. [Google Scholar] [CrossRef] [PubMed]
- Thanabalasuriar, A.; Scott, B.N.V.; Peiseler, M.; Willson, M.E.; Zeng, Z.; Warrener, P.; Keller, A.E.; Surewaard, B.G.J.; Dozier, E.A.; Korhonen, J.T.; et al. Neutrophil Extracellular Traps Confine Pseudomonas aeruginosa Ocular Biofilms and Restrict Brain Invasion. Cell Host Microbe 2019, 25, 526–536. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Conover, M.; Lu, H.; Parsek, M.R.; Bayles, K.; Wozniak, D.J. Assembly and development of the Pseudomonas aeruginosa biofilm matrix. PLoS Pathog. 2009, 5, e1000354. [Google Scholar] [CrossRef]
- Recio, R.; Mancheño, M.; Viedma, E.; Villa, J.; Orellana, M.Á.; Lora-Tamayo, J.; Chaves, F. Predictors of Mortality in Bloodstream Infections Caused by Pseudomonas aeruginosa and Impact of Antimicrobial Resistance and Bacterial Virulence. Antimicrob. Agents Chemother. 2020, 64. [Google Scholar] [CrossRef]
- Tabor, D.E.; Oganesyan, V.; Keller, A.E.; Yu, L.; McLaughlin, R.E.; Song, E.; Warrener, P.; Rosenthal, K.; Esser, M.; Qi, Y.; et al. Pseudomonas aeruginosa PcrV and Psl, the Molecular Targets of Bispecific Antibody MEDI3902, Are Conserved Among Diverse Global Clinical Isolates. J. Infect. Dis. 2018, 218, 1983–1994. [Google Scholar] [CrossRef] [PubMed]
- Abel, J.; Goldmann, O.; Ziegler, C.; Höltje, C.; Smeltzer, M.S.; Cheung, A.L.; Bruhn, D.; Rohde, M.; Medina, E. Staphylococcus aureus evades the extracellular antimicrobial activity of mast cells by promoting its own uptake. J. Innate Immun. 2011, 3, 495–507. [Google Scholar] [CrossRef]
- Zhou, C.; Lehar, S.; Gutierrez, J.; Rosenberger, C.M.; Ljumanovic, N.; Dinoso, J.; Koppada, N.; Hong, K.; Baruch, A.; Carrasco-Triguero, M.; et al. Pharmacokinetics and pharmacodynamics of DSTA4637A: A novel THIOMAB™ antibody antibiotic conjugate against Staphylococcus aureus in mice. MAbs 2016, 8, 1612–1619. [Google Scholar] [CrossRef]
- Linghu, X.; Segraves, N.L.; Abramovich, I.; Wong, N.; Müller, B.; Neubauer, N.; Fantasia, S.; Rieth, S.; Bachmann, S.; Jansen, M.; et al. Highly Efficient Synthesis of a Staphylococcus aureus Targeting Payload to Enable the First Antibody-Antibiotic Conjugate. Chemistry 2018, 24, 2837–2840. [Google Scholar] [CrossRef] [PubMed]
- Lehar, S.M.; Pillow, T.; Xu, M.; Staben, L.; Kajihara, K.K.; Vandlen, R.; DePalatis, L.; Raab, H.; Hazenbos, W.L.; Morisaki, J.H.; et al. Novel antibody-antibiotic conjugate eliminates intracellular S. aureus. Nature 2015, 527, 323–328. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, J. Tackling Drug-Resistant Infections Globally: Final Report and Recommendations. 2016. Available online: https://amrreview.org/sites/default/files/160525_Final%20paper_with%20cover.pdf (accessed on 30 December 2019).
- World Health Organization. Global Action Plan on Antimicrobial Resistance. 2015. Available online: https://apps.who.int/iris/bitstream/handle/10665/193736/9789241509763_eng.pdf?sequence=1&isAllowed=y (accessed on 30 December 2019).
- Buyel, J.F.; Twyman, R.M.; Fischer, R. Very-large-scale production of antibodies in plants: The biologization of manufacturing. Biotechnol. Adv. 2017, 35, 458–465. [Google Scholar] [CrossRef] [PubMed]
- Simon, M.S.; Sfeir, M.M.; Calfee, D.P.; Satlin, M.J. Cost-effectiveness of ceftazidime-avibactam for treatment of carbapenem-resistant Enterobacteriaceae bacteremia and pneumonia. Antimicrob. Agents Chemother. 2019. [Google Scholar] [CrossRef] [PubMed]
- Tkaczyk, C.; Semenova, E.; Shi, Y.Y.; Rosenthal, K.; Oganesyan, V.; Warrener, P.; Stover, C.K.; Sellman, B.R. Alanine scanning mutagenesis of the MEDI4839 (Suvratoxumab) epitope reduces alpha toxin lytic activity in vitro and S. aureus fitness in infection models. Antimicrob. Agents Chemother. 2018, 62. [Google Scholar] [CrossRef]
- Riazi, A.; Strong, P.C.; Coleman, R.; Chen, W.; Hirama, T.; van Faassen, H.; Henry, M.; Logan, S.M.; Szymanski, C.M.; Mackenzie, R.; et al. Pentavalent single-domain antibodies reduce Campylobacter jejuni motility and colonization in chickens. PLoS ONE 2013, 8, e83928. [Google Scholar] [CrossRef]
- Vu, T.T.T.; Nguyen, N.T.Q.; Tran, V.G.; Gras, E.; Mao, Y.; Jung, D.H.; Tkaczyk, C.; Sellman, B.R.; Diep, B.A. Protective Efficacy of Monoclonal Antibodies Neutralizing Alpha-Hemolysin and Bicomponent Leukocidins in Rabbit Model of Staphylococcus aureus Necrotizing Pneumonia. Antimicrob. Agents Chemother. 2019, 64. [Google Scholar] [CrossRef]
- DiGiandomenico, A.; Sellman, B.R. Antibacterial monoclonal antibodies: The next generation? Curr. Opin. Microbiol. 2015, 27, 78–85. [Google Scholar] [CrossRef] [PubMed]
| Antibacterial Mechanism | Reference |
|---|---|
| Bactericidal | [20,22] |
| Biofilm | [23,24] |
| Iron acquisition | [25,26,27] |
| Attachment/Adhesion | [28,29] |
| Anti-toxin/Anti-virulence | [30,31] |
| Opsonophagocytosis | [32,33] |
| Complement | [34,35] |
| Name | Bacterial Species Targeted | Company | Development Phase |
|---|---|---|---|
| AR301 | Staphylococcus aureus | Aridis Pharmaceuticals | Phase 2 Complete Ongoing Phase 3 |
| MEDI4893 | Staphylococcus aureus | Medimmune | Phase 2 Complete |
| MEDI3902 | Pseudomonas aeruginosa | Medimmune | Phase 1 Complete Ongoing Phase 2 |
| AR101 | Pseudomonas aeruginosa | Aridis Pharmaceuticals | Phase 1 Complete Ongoing Phase 2 |
| 514G3 | Staphylococcus aureus | XBiotech | Phase 2 |
| ARN-100 | Staphylococcus aureus | Arsansis | Phase 2 Halted |
| PolyCAb | Clostridium difficile | MicroPharm | Phase 1 |
| RG7861 | Staphylococcus aureus | Roche | Phase 1 |
| TRL1068 | Biofilm—multiple species | Trellis Bioscience | Preclinical Entering Phase 1 |
| AR401-mAb | Acinetobacter baumannii | Aridis Pharmaceuticals | Preclinical |
| VXD-003 | Acinetobacter baumannii | VaxDyn | Preclinical |
| Cd-ISTAb | Clostridium difficile | Integrated BioTherapeutics | Preclinical |
| ASN-4 | Escherichia coli (ST131) | Arsansis—Outlicensed to BB100 | Preclinical |
| ASN-5 | K. pneumoniae | Arsansis—Outlicensed to BB200 | Preclinical |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zurawski, D.V.; McLendon, M.K. Monoclonal Antibodies as an Antibacterial Approach Against Bacterial Pathogens. Antibiotics 2020, 9, 155. https://doi.org/10.3390/antibiotics9040155
Zurawski DV, McLendon MK. Monoclonal Antibodies as an Antibacterial Approach Against Bacterial Pathogens. Antibiotics. 2020; 9(4):155. https://doi.org/10.3390/antibiotics9040155
Chicago/Turabian StyleZurawski, Daniel V., and Molly K. McLendon. 2020. "Monoclonal Antibodies as an Antibacterial Approach Against Bacterial Pathogens" Antibiotics 9, no. 4: 155. https://doi.org/10.3390/antibiotics9040155
APA StyleZurawski, D. V., & McLendon, M. K. (2020). Monoclonal Antibodies as an Antibacterial Approach Against Bacterial Pathogens. Antibiotics, 9(4), 155. https://doi.org/10.3390/antibiotics9040155




