Optimizing the Dosing Regimens of Daptomycin Based on the Susceptible Dose-Dependent Breakpoint against Vancomycin-Resistant Enterococci Infection
Abstract
1. Introduction
2. Results
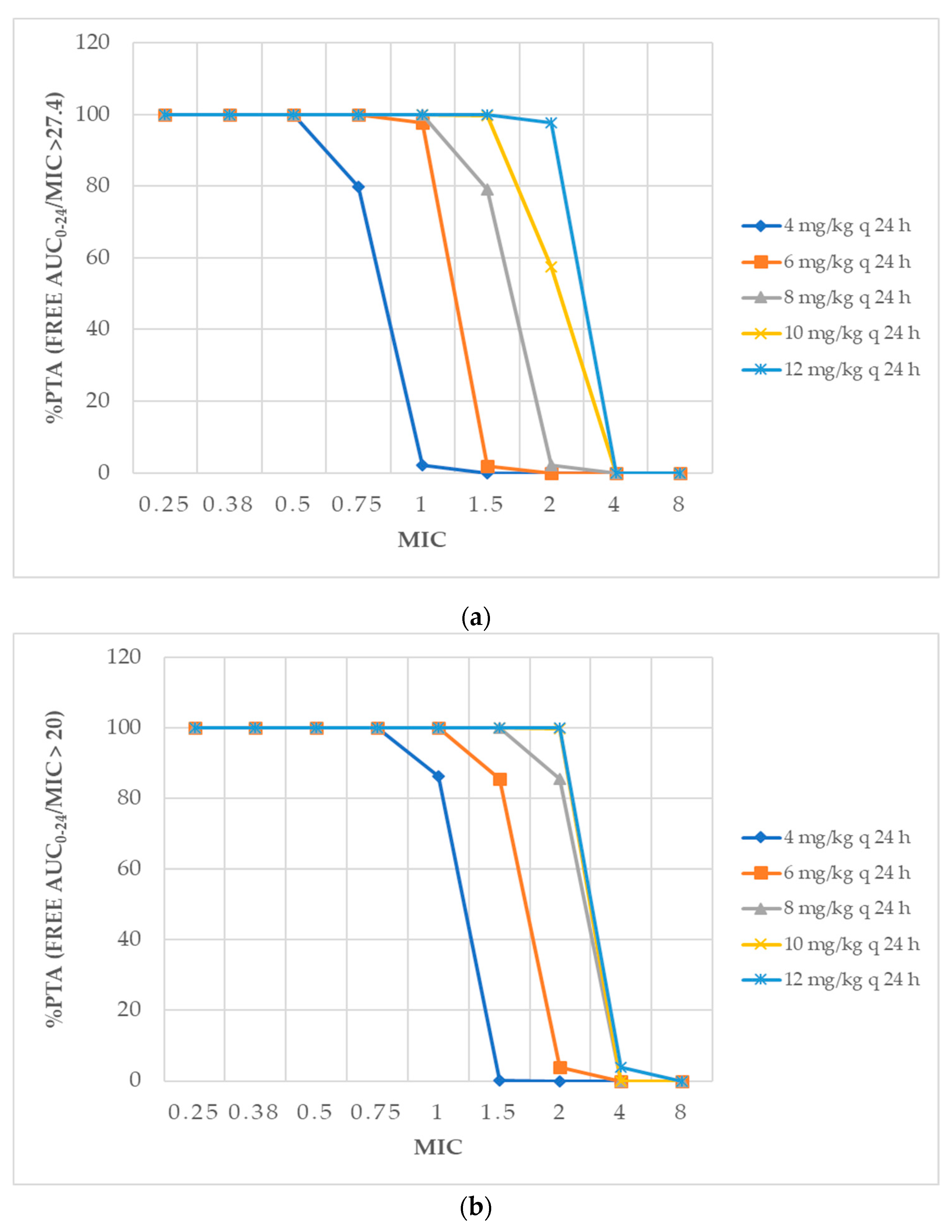
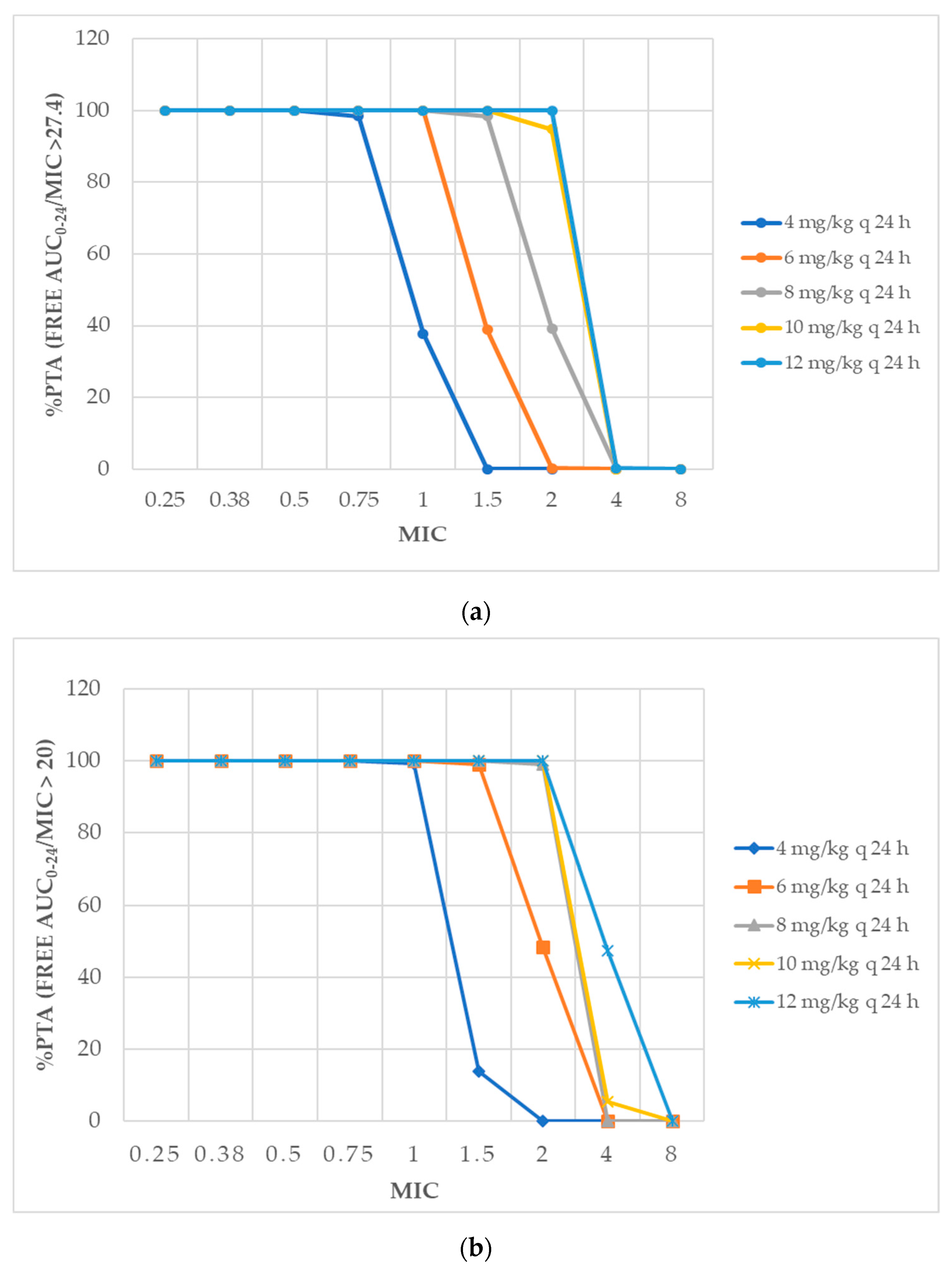
2.1. Pharmacodynamic Profiling
2.2. Pharmacokinetic and Pharmacodynamic Analysis and Dosing Simulations
3. Discussion
4. Materials and Methods
4.1. Microbiological Analysis
4.2. Pharmacokinetic and Pharmacodynamic Analysis and Dosing Simulations
4.3. Ethical Approval
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Hemapanpairoa, J.; Changpradub, D.; Thunyaharn, S.; Santimaleeworagun, W. Vancomycin-resistant enterococcal infection in a Thai university hospital: Clinical characteristics, treatment outcomes, and synergistic effect. Infect. Drug Resist. 2019, 12, 2049–2057. [Google Scholar] [CrossRef] [PubMed]
- Chiang, H.Y.; Perencevich, E.N.; Nair, R.; Nelson, R.E.; Samore, M.; Khader, K.; Chorazy, M.L.; Herwaldt, L.A.; Blevins, A.; Ward, M.A.; et al. Incidence and Outcomes Associated with Infections Caused by Vancomycin-Resistant Enterococci in the United States: Systematic Literature Review and Meta-Analysis. Infect. Control Hosp. Epidemiol. 2017, 38, 203–215. [Google Scholar] [CrossRef] [PubMed]
- National Antimicrobial Resistance Surveillance Center. Thailand. Available online: http://narst.dmsc.moph.go.th/ (accessed on 9 September 2019).
- Baddour Larry, M.; Wilson Walter, R.; Bayer Arnold, S.; Fowler Vance, G.; Tleyjeh Imad, M.; Rybak Michael, J.; Barsic, B.; Lockhart Peter, B.; Gewitz Michael, H.; Levison Matthew, E.; et al. Infective Endocarditis in Adults: Diagnosis, Antimicrobial Therapy, and Management of Complications. Circulation 2015, 132, 1435–1486. [Google Scholar] [CrossRef] [PubMed]
- Mermel, L.A.; Allon, M.; Bouza, E.; Craven, D.E.; Flynn, P.; O’Grady, N.P.; Raad, I.I.; Rijnders, B.J.A.; Sherertz, R.J.; Warren, D.K. Clinical Practice Guidelines for the Diagnosis and Management of Intravascular Catheter-Related Infection: 2009 Update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2009, 49, 1–45. [Google Scholar] [CrossRef] [PubMed]
- Stevens, D.L.; Bisno, A.L.; Chambers, H.F.; Dellinger, E.P.; Goldstein, E.J.C.; Gorbach, S.L.; Hirschmann, J.V.; Kaplan, S.L.; Montoya, J.G.; Wade, J.C. Practice Guidelines for the Diagnosis and Management of Skin and Soft Tissue Infections: 2014 Update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2014, 59, e10–e52. [Google Scholar] [CrossRef]
- Berbari, E.F.; Kanj, S.S.; Kowalski, T.J.; Darouiche, R.O.; Widmer, A.F.; Schmitt, S.K.; Hendershot, E.F.; Holtom, P.D.; Huddleston, P.M., III; Petermann, G.W.; et al. 2015 Infectious Diseases Society of America (IDSA) Clinical Practice Guidelines for the Diagnosis and Treatment of Native Vertebral Osteomyelitis in Adultsa. Clin. Infect. Dis. 2015, 61, e26–e46. [Google Scholar] [CrossRef]
- Waller, D.G.; Sampson, A.P. 51—Chemotherapy of infections. In Medical Pharmacology and Therapeutics, 5th ed.; Waller, D.G., Sampson, A.P., Eds.; Elsevier: Amsterdam, The Netherlands, 2018; pp. 581–629. [Google Scholar] [CrossRef]
- American Thoracic Society and Infectious Diseases Society of America. Guidelines for the Management of Adults with Hospital-acquired, Ventilator-associated, and Healthcare-associated Pneumonia. Am. J. Respir. Crit. Care Med. 2005, 171, 388–416. [Google Scholar] [CrossRef]
- Foolad, F.; Taylor, B.D.; Shelburne, S.A.; Arias, C.A.; Aitken, S.L. Association of daptomycin dosing regimen and mortality in patients with VRE bacteraemia: A review. J. Antimicrob. Chemother. 2018, 73, 2277–2283. [Google Scholar] [CrossRef]
- Chuang, Y.C.; Lin, H.Y.; Chen, P.Y.; Lin, C.Y.; Wang, J.T.; Chen, Y.C.; Chang, S.C. Effect of Daptomycin Dose on the Outcome of Vancomycin-Resistant, Daptomycin-Susceptible Enterococcus faecium Bacteremia. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2017, 64, 1026–1034. [Google Scholar] [CrossRef]
- Britt, N.S.; Potter, E.M.; Patel, N.; Steed, M.E. Comparative Effectiveness and Safety of Standard-, Medium-, and High-Dose Daptomycin Strategies for the Treatment of Vancomycin-Resistant Enterococcal Bacteremia among Veterans Affairs Patients. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2017, 64, 605–613. [Google Scholar] [CrossRef]
- Humphries, R.M. The New, New Daptomycin Breakpoint for Enterococcus spp. J. Clin. Microbiol. 2019, 57, e00600–e00619. [Google Scholar] [CrossRef] [PubMed]
- Satlin, M.J.; Nicolau, D.P.; Humphries, R.M.; Kuti, J.L.; Campeau, S.A.; Lewis, J.S., II; Weinstein, M.P.; Jorgensen, J.H.; Clinical and Laboratory Standards Institute Subcommittee on Antimicrobial Susceptibility Testing and Ad Hoc Working Group on Revision of Daptomycin Enterococcal Breakpoints. Development of Daptomycin Susceptibility Breakpoints for Enterococcus faecium and Revision of the Breakpoints for other Enterococcal species by the Clinical and Laboratory Standards Institute. Clin. Infect. Dis. 2019. [Google Scholar] [CrossRef] [PubMed]
- Safdar, N.; Andes, D.; Craig, W.A. In vivo pharmacodynamic activity of daptomycin. Antimicrob. Agents Chemother. 2004, 48, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Avery, L.M.; Kuti, J.L.; Weisser, M.; Egli, A.; Rybak, M.J.; Zasowski, E.J.; Arias, C.A.; Contreras, G.A.; Chong, P.P.; Aitken, S.L.; et al. Pharmacodynamic Analysis of Daptomycin-treated Enterococcal Bacteremia: It Is Time to Change the Breakpoint. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2019, 68, 1650–1657. [Google Scholar] [CrossRef] [PubMed]
- Bhavnani, S.M.; Rubino, C.M.; Ambrose, P.G.; Drusano, G.L. Daptomycin exposure and the probability of elevations in the creatine phosphokinase level: Data from a randomized trial of patients with bacteremia and endocarditis. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2010, 50, 1568–1574. [Google Scholar] [CrossRef] [PubMed]
- Boucher, B.; Wood, G.; Swanson, J. Pharmacokinetic Changes in Critical Illness. Crit. Care Clin. 2006, 22, 255–271. [Google Scholar] [CrossRef]
- Pea, F. Plasma pharmacokinetics of antimicrobial agents in critically ill patients. Curr. Clin. Pharmacol. 2013, 8, 5–12. [Google Scholar]
- Roberts, J.A.; Abdul-Aziz, M.H.; Lipman, J.; Mouton, J.W.; Vinks, A.A.; Felton, T.W.; Hope, W.W.; Farkas, A.; Neely, M.N.; Schentag, J.J.; et al. Individualised antibiotic dosing for patients who are critically ill: Challenges and potential solutions. Lancet Infect. Dis. 2014, 14, 498–509. [Google Scholar] [CrossRef]
- O’Driscoll, T.; Crank, C.W. Vancomycin-resistant enterococcal infections: Epidemiology, clinical manifestations, and optimal management. Infect. Drug Resist. 2015, 8, 217–230. [Google Scholar] [CrossRef]
- Streit, J.M.; Jones, R.N.; Sader, H.S. Daptomycin activity and spectrum: A worldwide sample of 6737 clinical Gram-positive organisms. J. Antimicrob. Chemother. 2004, 53, 669–674. [Google Scholar] [CrossRef]
- Cantón, R.; Ruiz-Garbajosa, P.; Chaves, R.L.; Johnson, A.P. A potential role for daptomycin in enterococcal infections: What is the evidence? J. Antimicrob. Chemother. 2010, 65, 1126–1136. [Google Scholar] [CrossRef] [PubMed]
- Patel, J.B.; Jevitt, L.A.; Hageman, J.; McDonald, L.C.; Tenover, F.C. An association between reduced susceptibility to daptomycin and reduced susceptibility to vancomycin in Staphylococcus aureus. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2006, 42, 1652–1653. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Zhang, J.; Chen, Y.; Liang, X.; Guo, Y.; Yu, J.; Zhu, D.; Zhang, Y. Optimization of linezolid treatment regimens for Gram-positive bacterial infections based on pharmacokinetic/pharmacodynamic analysis. Future Microbiol. 2017, 12, 39–50. [Google Scholar] [CrossRef] [PubMed]
- Humphries, R.M.; Pollett, S.; Sakoulas, G. A current perspective on daptomycin for the clinical microbiologist. Clin. Microbiol. Rev. 2013, 26, 759–780. [Google Scholar] [CrossRef] [PubMed]
- Shukla, B.S.; Shelburne, S.; Reyes, K.; Kamboj, M.; Lewis, J.D.; Rincon, S.L.; Reyes, J.; Carvajal, L.P.; Panesso, D.; Sifri, C.D.; et al. Influence of Minimum Inhibitory Concentration in Clinical Outcomes of Enterococcus faecium Bacteremia Treated with Daptomycin: Is it Time to Change the Breakpoint? Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2016, 62, 1514–1520. [Google Scholar] [CrossRef] [PubMed]
- Kidd, J.M.; Abdelraouf, K.; Asempa, T.E.; Humphries, R.M.; Nicolau, D.P. Pharmacodynamics of Daptomycin against Enterococcus faecium and Enterococcus faecalis in the murine thigh infection model. Antimicrob. Agents Chemother. 2018, 62, e00506–e00518. [Google Scholar] [CrossRef] [PubMed]
- Falcone, M.; Russo, A.; Venditti, M.; Novelli, A.; Pai, M.P. Considerations for higher doses of daptomycin in critically ill patients with methicillin-resistant Staphylococcus aureus bacteremia. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2013, 57, 1568–1576. [Google Scholar] [CrossRef]
- Bubalo, J.S.; Munar, M.Y.; Cherala, G.; Hayes-Lattin, B.; Maziarz, R. Daptomycin pharmacokinetics in adult oncology patients with neutropenic fever. Antimicrob. Agents Chemother. 2009, 53, 428–434. [Google Scholar] [CrossRef]
- Soraluce, A.; Asin-Prieto, E.; Rodriguez-Gascon, A.; Barrasa, H.; Maynar, J.; Carcelero, E.; Soy, D.; Isla, A. Population pharmacokinetics of daptomycin in critically ill patients. Int. J. Antimicrob. Agents 2018, 52, 158–165. [Google Scholar] [CrossRef]
- Kebriaei, R.; Rice, S.A.; Singh, K.V.; Stamper, K.C.; Dinh, A.Q.; Rios, R.; Diaz, L.; Murray, B.E.; Munita, J.M.; Tran, T.T.; et al. Influence of Inoculum Effect on the Efficacy of Daptomycin Monotherapy and in Combination with beta-Lactams against Daptomycin-Susceptible Enterococcus faecium Harboring LiaSR Substitutions. Antimicrob. Agents Chemother. 2018, 62. [Google Scholar] [CrossRef]
- Smith, J.R.; Barber, K.E.; Raut, A.; Aboutaleb, M.; Sakoulas, G.; Rybak, M.J. beta-Lactam combinations with daptomycin provide synergy against vancomycin-resistant Enterococcus faecalis and Enterococcus faecium. J. Antimicrob. Chemother. 2015, 70, 1738–1743. [Google Scholar] [CrossRef] [PubMed]
- Metwali, H.; Elder, K. Dose-independent daptomycin associated rhabdomyolysis: Case report. J. Basic Clin. Pharm. 2018, 9, 286–288. [Google Scholar]

| Daptomycin Dosing | % CFR of AUC/MIC | % Probability of Cmin < 24.3 mg/L | |||
|---|---|---|---|---|---|
| >27.4 | >20 | ||||
| First 24 h | Steady State | First 24 h | Steady State | ||
| 4 mg/kg q 24 h | 41.47 | 57.24 | 72.86 | 79.42 | 100 |
| 6 mg/kg q 24 h | 76.74 | 84.37 | 93.22 | 96.68 | 100 |
| 8 mg/kg q 24 h | 91.98 | 96.35 | 97.61 | 97.9 | 100 |
| 10 mg/kg q 24 h | 96.99 | 97.81 | 97.91 | 98.03 | 100 |
| 12 mg/kg q 24 h | 97.87 | 97.92 | 98.0 | 99.0 | 99.99 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santimaleeworagun, W.; Changpradub, D.; Thunyaharn, S.; Hemapanpairoa, J. Optimizing the Dosing Regimens of Daptomycin Based on the Susceptible Dose-Dependent Breakpoint against Vancomycin-Resistant Enterococci Infection. Antibiotics 2019, 8, 245. https://doi.org/10.3390/antibiotics8040245
Santimaleeworagun W, Changpradub D, Thunyaharn S, Hemapanpairoa J. Optimizing the Dosing Regimens of Daptomycin Based on the Susceptible Dose-Dependent Breakpoint against Vancomycin-Resistant Enterococci Infection. Antibiotics. 2019; 8(4):245. https://doi.org/10.3390/antibiotics8040245
Chicago/Turabian StyleSantimaleeworagun, Wichai, Dhitiwat Changpradub, Sudaluck Thunyaharn, and Jatapat Hemapanpairoa. 2019. "Optimizing the Dosing Regimens of Daptomycin Based on the Susceptible Dose-Dependent Breakpoint against Vancomycin-Resistant Enterococci Infection" Antibiotics 8, no. 4: 245. https://doi.org/10.3390/antibiotics8040245
APA StyleSantimaleeworagun, W., Changpradub, D., Thunyaharn, S., & Hemapanpairoa, J. (2019). Optimizing the Dosing Regimens of Daptomycin Based on the Susceptible Dose-Dependent Breakpoint against Vancomycin-Resistant Enterococci Infection. Antibiotics, 8(4), 245. https://doi.org/10.3390/antibiotics8040245





