Susceptibility of Multidrug-Resistant and Biofilm-Forming Uropathogens to Mexican Oregano Essential Oil
Abstract
:1. Introduction
2. Results
2.1. Bacterial Isolates from UTI Patients
2.2. Antibiotic Resistance of Bacterial Isolates from the Urine of UTI Patients
2.3. Biofilm Formation of Multidrug-Resistant Bacterial Isolates
2.4. The Antimicrobial Capacity of Mexican Oregano Essential Oil Against Selected Isolates
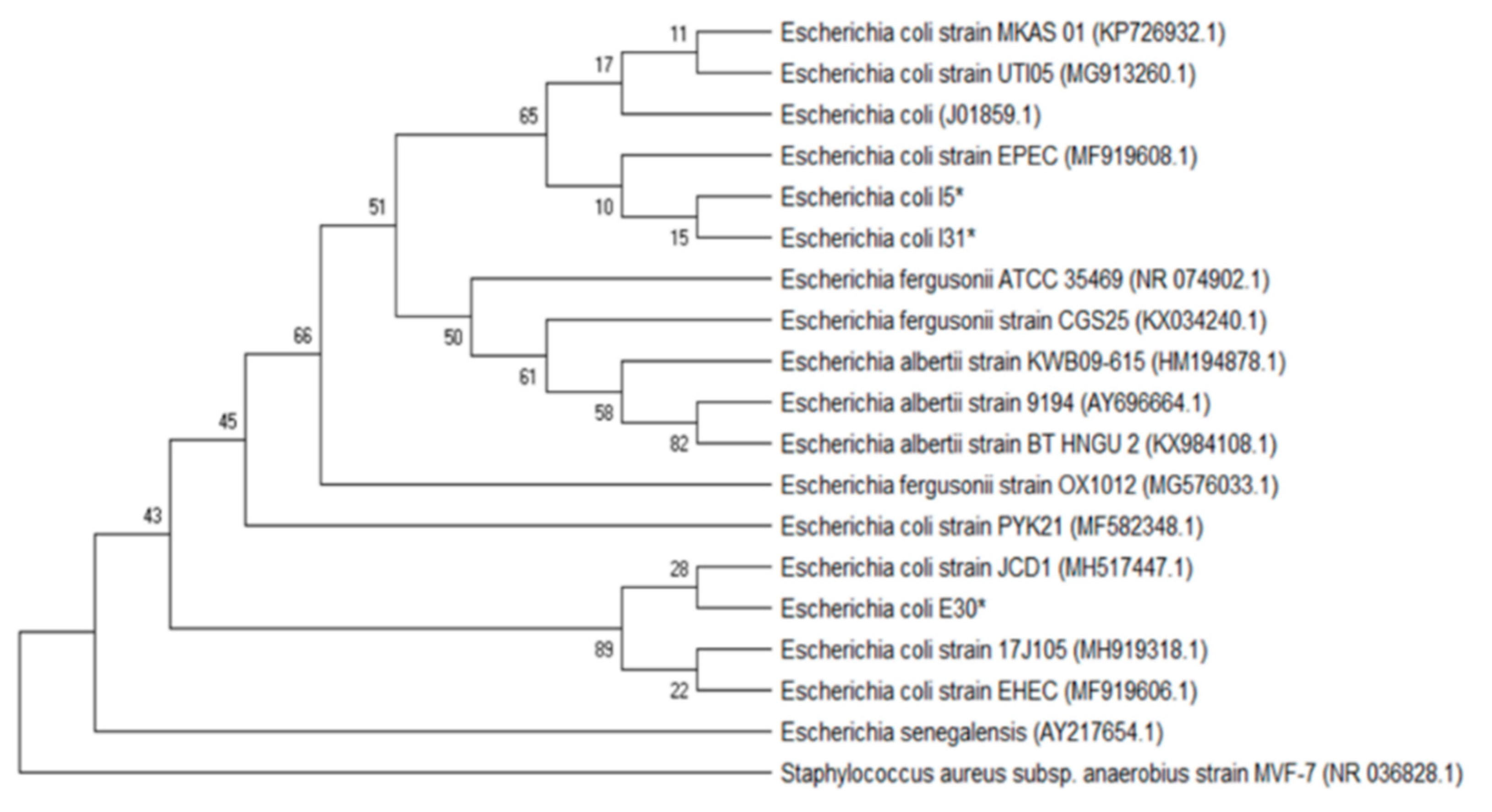
2.5. Molecular Identification of Multidrug-Resistant, Biofilm-Forming Isolates from the Urine of UTI Patients
3. Discussion
4. Materials and Methods
4.1. Bacterial Isolates
4.2. Antibiotic Susceptibility Test
4.3. Biofilm Formation Test
4.4. Oregano Essential Oil Extraction and Analysis
4.5. Antimicrobial Activity of Mexican Oregano Essential Oil
4.6. Bacterial Isolates Molecular Identification
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Bouacha, M.; Ayed, H.; Grara, N. Honey bee as alternative medicine to treat eleven multidrug-resistant bacteria causing urinary tract infection during pregnancy. Sci. Pharm. 2018, 86, 14. [Google Scholar] [CrossRef] [PubMed]
- Ma, A.H.; Hughes, G.J. Updates in Management of Complicated Urinary Tract Infections: A Focus on Multidrug-Resistant Organisms. Am. J. Ther. 2018, 25, e53–e66. [Google Scholar] [CrossRef]
- Römling, U.; Balsalobre, C. Biofilm infections, their resilience to therapy and innovative treatment strategies. J. Intern. Med. 2012, 272, 541–561. [Google Scholar] [CrossRef] [PubMed]
- Flores-Mireles, A.L.; Walker, J.N.; Caparon, M.; Hultgren, S.J. Urinary tract infections: Epidemiology, mechanisms of infection and treatment options. Nat. Rev. Microbiol. 2015, 13, 269–284. [Google Scholar] [CrossRef] [PubMed]
- González, M.J.; Robino, L.; Iribarnegaray, V.; Zunino, P.; Scavone, P. Effect of different antibiotics on biofilm produced by uropathogenic Escherichia coli isolated from children with urinary tract infection. Pathog. Dis. 2017, 75, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Castillo, F.Y.; Moreno-Flores, A.C.; Avelar-González, F.J.; Márquez-Díaz, F.; Harel, J.; Guerrero-Barrera, A.L. An evaluation of multidrug-resistant Escherichia coli isolates in urinary tract infections from Aguascalientes, Mexico: Cross-sectional study. Ann. Clin. Microbiol. Antimicrob. 2018, 17, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Dumaru, R.; Baral, R.; Shrestha, L.B. Study of biofilm formation and antibiotic resistance pattern of gram-negative Bacilli among the clinical isolates at BPKIHS, Dharan. BMC Res. Notes 2019, 12, 1–7. [Google Scholar] [CrossRef]
- Shridhar, S.; Dhanashree, B. Antibiotic Susceptibility Pattern and Biofilm Formation in Clinical Isolates of Enterococcus spp. Interdiscip. Perspect. Infect. Dis. 2019, 2019, 1–6. [Google Scholar] [CrossRef]
- Sabir, N.; Ikram, A.; Zaman, G.; Satti, L.; Gardezi, A.; Ahmed, A.; Ahmed, P. Bacterial biofilm-based catheter-associated urinary tract infections: Causative pathogens and antibiotic resistance. Am. J. Infect. Control 2017, 45, 1101–1105. [Google Scholar] [CrossRef]
- Fasugba, O.; Das, A.; Mnatzaganian, G.; Mitchell, B.G.; Collignon, P.; Gardner, A. Incidence of single-drug resistant, multidrug-resistant and extensively drug-resistant Escherichia coli urinary tract infections: An Australian laboratory-based retrospective study. J. Glob. Antimicrob. Resist. 2019, 16, 254–259. [Google Scholar] [CrossRef]
- Lagha, R.; Ben Abdallah, F.; AL-Sarhan, B.O.; Al-Sodany, Y. Antibacterial and Biofilm Inhibitory Activity of Medicinal Plant Essential Oils Against Escherichia coli Isolated from UTI Patients. Molecules 2019, 24, 1161. [Google Scholar] [CrossRef] [PubMed]
- Avila-Sosa, R.; Gastélum-Franco, M.G.; Camacho-Dávila, A.; Torres-Muñoz, J.V.; Nevárez-Moorillón, G.V. Extracts of Mexican Oregano (Lippia berlandieri Schauer) with Antioxidant and Antimicrobial Activity. Food Bioprocess Technol. 2010, 3, 434–440. [Google Scholar] [CrossRef]
- Cid-Pérez, T.; Ávila-Sosa, R.; Ochoa-Velasco, C.; Rivera-Chavira, B.; Nevárez-Moorillón, G.V. Antioxidant and Antimicrobial Activity of Mexican Oregano (Poliomintha longiflora) Essential Oil, Hydrosol and Extracts from Waste Solid Residues. Plants 2019, 8, 22. [Google Scholar] [CrossRef] [PubMed]
- Magiorako, A.-P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef] [PubMed]
- Stepanovic, R.; Vukovic, D.; Dakic, I.; Savic, B.; Svabic-Vlahovic, M. A modified microtiter-plate test for quantification of staphylococcal biofilm formation. J. Microbiol. Methods 2000, 40, 175–179. [Google Scholar] [CrossRef]
- Cid-Pérez, T.S.; Nevárez-Moorillón, G.V.; Torres-Muñoz, J.V.; Palou, E.; López-Malo, A. Mexican oregano (Lippia berlandieri and Poliomintha longiflora) oils. Essent. Oils Food Preserv. Flavor Saf. 2015. [Google Scholar] [CrossRef]
- Kraemer, S.A.; Ramachandran, A.; Perron, G.G. Antibiotic Pollution in the Environment: From Microbial Ecology to Public Policy. Microorganisms 2019, 7, 180. [Google Scholar] [CrossRef]
- Walker, E.; Lyman, A.; Gupta, K.; Mahoney, M.V.; Snyder, G.M.; Hirsch, E.B. Clinical Management of an Increasing Threat: Outpatient Urinary Tract Infections Due to Multidrug-Resistant Uropathogens. Clin. Infect. Dis. 2016, 63, 960–965. [Google Scholar] [CrossRef]
- Ukah, U.V.; Glass, M.; Avery, B.; Daignault, D.; Mulvey, M.R.; Reid-Smith, R.J.; Parmley, E.J.; Portt, A.; Boerlin, P.; Manges, A.R. Risk factors for acquisition of multidrug-resistant Escherichia coli and development of community-acquired urinary tract infections. Epidemiol. Infect. 2018, 146, 46–57. [Google Scholar] [CrossRef]
- Fallah, F.; Yousefi, M.; Pourmand, M.R.; Hashemi, A.; Nazari Alam, A.; Afshar, D. Phenotypic and genotypic study of biofilm formation in Enterococci isolated from urinary tract infections. Microb. Pathog. 2017, 108, 85–90. [Google Scholar] [CrossRef]
- Chen, S.L.; Yu, H.; Luo, H.M.; Wu, Q.; Li, C.F.; Steinmetz, A. Conservation and sustainable use of medicinal plants: Problems, progress, and prospects. Chinese Med. (UK) 2016, 11, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Zhou, F.; Ji, B.P.; Pei, R.S.; Xu, N. The antibacterial mechanism of carvacrol and thymol against Escherichia coli. Lett. Appl. Microbiol. 2008, 47, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Oussalah, M.; Caillet, S.; Lacroix, M. Mechanism of action of Spanish oregano, Chinese cinnamon, and savory essential oils against cell membranes and walls of Escherichia coli O157: H7 and Listeria monocytogenes. J. Food Prot. 2006, 69, 1046–1055. [Google Scholar] [CrossRef] [PubMed]
- Kumar, M.S.; Das, A.P. Molecular identification of multi drug resistant bacteria from urinary tract infected urine samples. Microb. Pathog. 2016, 98, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Procop, G.W.; Church, D.L.; Hall, G.S.; Janda, W.M.; Koneman, E.W.; Schreckenberger, P.C.; Woods, G.L. Koneman’s Color Atlas and Textbook of Diagnostic Microbiology; Wolters Kluwer Health: Philadelphia, PA, USA, 2016; ISBN 978-1-451-11659-5. [Google Scholar]
- Biemer, J.J. Antimicrobial Susceptibility Testing by the Kirby-Bauer Disc Diffusion Method. Ann. Clin. Lab. Sci. 1973, 3, 135–140. [Google Scholar]
- Sambrook, J.; Russell, D.W. Molecular Cloning: A Laboratory Manual, 3rd ed.; Cold Spring Harbor Laboratory Press: New York, NY, USA, 2001. [Google Scholar]
- Merzoug, M.; Dalache, F.; Karam, H.Z.; Karam, N.E. Isolation and preliminary characterisation of bacteriocin produced by Enterococcus faecium GHB21 isolated from Algerian paste of dates “ghars”. Ann. Microbiol. 2016, 66, 795–805. [Google Scholar] [CrossRef]
- Kumar, S.; Stecher, G.; Li, M.; Knyaz, C.; Tamura, K. MEGA X: Molecular evolutionary genetics analysis across computing platforms. Mol. Biol. Evol. 2018, 35, 1547–1549. [Google Scholar] [CrossRef]
- Kimura, M. A Simple Method for Estimating Evolutionary Rates of Base Substitutions Through Comparative Studies of Nucleotide Sequences. J. Mol. Evol. 1980, 16, 111–120. [Google Scholar] [CrossRef]






| Isolates ID | Isolates Identification | Antibiotic Resistance a | Biofilm Formation Test in Glass Tubes b | Biofilm Formation Microplate Test c |
|---|---|---|---|---|
| E2 | Staphylococcus sp. coagulase negative | VA, E, OX, P | − | Non-adherent |
| I3 | Pseudomonas aeruginosa | AM, CIP, CRO, CL | ++ | Strongly adherent |
| I5 | E. coli | AM, CIP, GM | + | Strongly adherent |
| I7 | E. coli | AM, CIP, CRO, GM | + | Non-adherent |
| E9 | E. coli | AM, CRO, GM | − | Non-adherent |
| E10 | E. coli | AM, CRO, CTX | − | Non-adherent |
| I13 | E. coli | AM, CRO, GM, CTX | + | Non-adherent |
| E21 | E. coli | AM, CIP, CRO, CTX | − | Non-adherent |
| I24 | Staphylococcus sp. coagulase negative | VA, E, OX, P | +++ | Moderately adherent |
| E26 | Pseudomonas aeruginosa | AM, CRO, CTX, OX | +++ | Strongly adherent |
| I27 | Enterococcus faecalis | VA, E, OX | + | Strongly adherent |
| E30 | E. coli | AM, FEP, CRO, CTX | + | Strongly adherent |
| I31 | E. coli | AM, FEP, CRO, CTX | ++ | Strongly adherent |
| E36 | E. coli | AM, FEP, CRO, CTX | +++ | Moderately adherent |
| I38 | E. coli | AM, FEP, CRO, CTX | + | Non-adherent |
| E40 | E. coli | AM, FEP, CRO, CTX | − | Weakly adherent |
| E50 | E. coli | AM, FEP, CRO, CTX | + | Non-adherent |
| E51 | E. coli | AM, FEP, CRO, CTX | + | Non-adherent |
| I52 | E. coli | AM, FEP, CRO, CTX | − | Non-adherent |
| E53 | E. coli | AM, FEP, CRO, CTX | + | Non-adherent |
| Isolates ID | Lippia berlandieri EO1 | Lippia berlandieri EO2 | Poliomintha longiflora | |||
|---|---|---|---|---|---|---|
| MIC (mg/L) | MBC (mg/L) | MIC (mg/L) | MBC (mg/L) | MIC (mg/L) | MBC (mg/L) | |
| I3 Pseudomonas aeruginosa | >2000 | >2000 | >2000 | >2000 | >2000 | >2000 |
| I5 E. coli | 500 | 500 | 500 | 500 | 500 | 500 |
| E26 Pseudomonas aeruginosa | >2000 | >2000 | >2000 | >2000 | >2000 | >2000 |
| I27 Enterococcus faecalis | <250 | <250 | <250 | <250 | <250 | <250 |
| E30 E. coli | 750 | 750 | 750 | 750 | 1000 | 1000 |
| I31 E. coli | 500 | 500 | 500 | 500 | 750 | 750 |
| I3 Pseudomonas aeruginosa | >2000 | >2000 | >2000 | >2000 | >2000 | >2000 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zapién-Chavarría, K.A.; Plascencia-Terrazas, A.; Venegas-Ortega, M.G.; Varillas-Torres, M.; Rivera-Chavira, B.E.; Adame-Gallegos, J.R.; González-Rangel, M.O.; Nevárez-Moorillón, G.V. Susceptibility of Multidrug-Resistant and Biofilm-Forming Uropathogens to Mexican Oregano Essential Oil. Antibiotics 2019, 8, 186. https://doi.org/10.3390/antibiotics8040186
Zapién-Chavarría KA, Plascencia-Terrazas A, Venegas-Ortega MG, Varillas-Torres M, Rivera-Chavira BE, Adame-Gallegos JR, González-Rangel MO, Nevárez-Moorillón GV. Susceptibility of Multidrug-Resistant and Biofilm-Forming Uropathogens to Mexican Oregano Essential Oil. Antibiotics. 2019; 8(4):186. https://doi.org/10.3390/antibiotics8040186
Chicago/Turabian StyleZapién-Chavarría, Karen Arely, Alejandro Plascencia-Terrazas, María Georgina Venegas-Ortega, Mauricio Varillas-Torres, Blanca Estela Rivera-Chavira, Jaime Raúl Adame-Gallegos, María Olga González-Rangel, and Guadalupe Virginia Nevárez-Moorillón. 2019. "Susceptibility of Multidrug-Resistant and Biofilm-Forming Uropathogens to Mexican Oregano Essential Oil" Antibiotics 8, no. 4: 186. https://doi.org/10.3390/antibiotics8040186
APA StyleZapién-Chavarría, K. A., Plascencia-Terrazas, A., Venegas-Ortega, M. G., Varillas-Torres, M., Rivera-Chavira, B. E., Adame-Gallegos, J. R., González-Rangel, M. O., & Nevárez-Moorillón, G. V. (2019). Susceptibility of Multidrug-Resistant and Biofilm-Forming Uropathogens to Mexican Oregano Essential Oil. Antibiotics, 8(4), 186. https://doi.org/10.3390/antibiotics8040186






