Antibiotic Prophylaxis on Third Molar Extraction: Systematic Review of Recent Data
Abstract
1. Introduction
2. Results
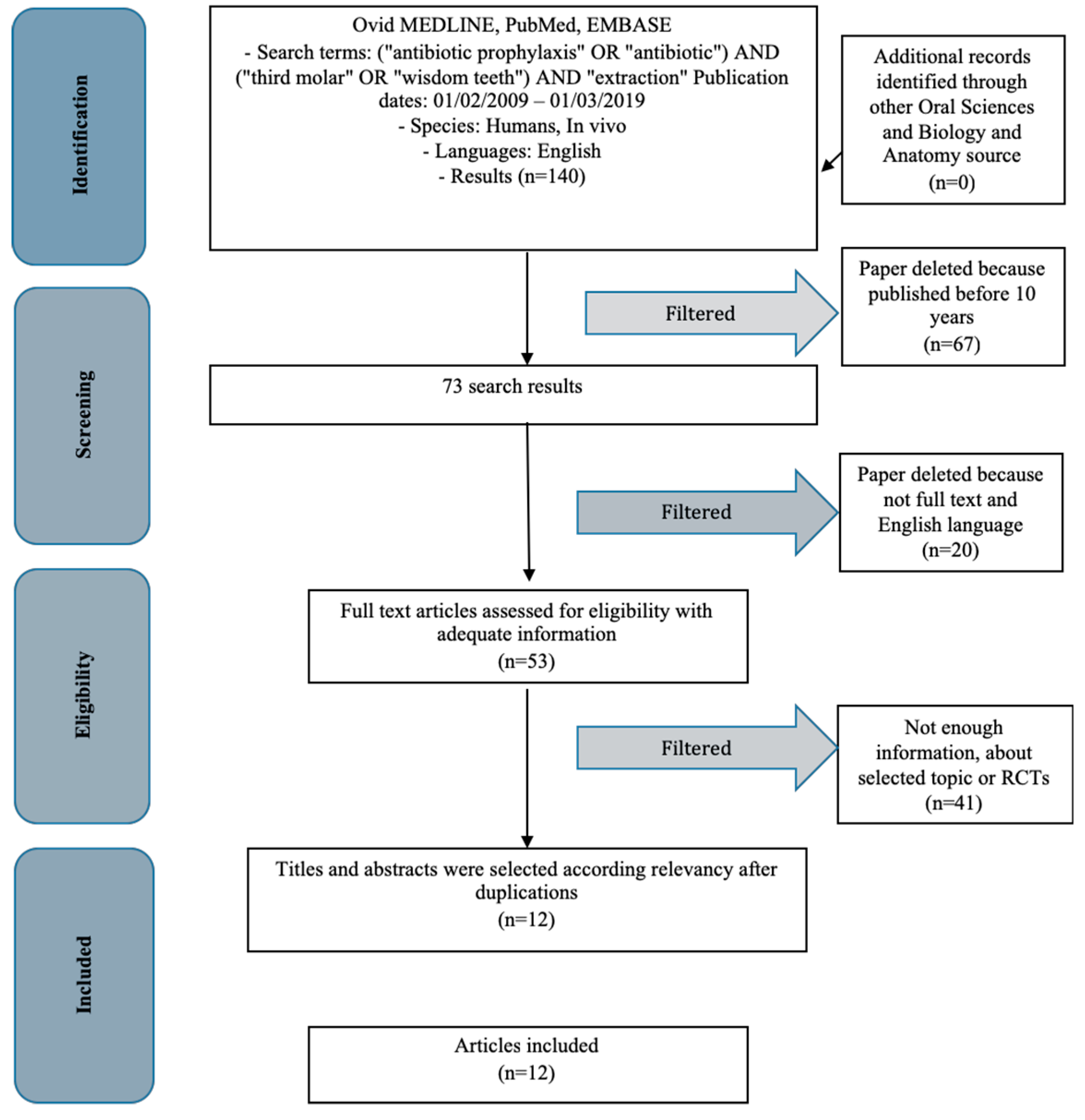
2.1. Manuscript Collection and Search Strategy
2.2. Study Characteristics
2.3. Risk of Bias Within the Studies
2.4. Risk of Bias Across the Studies
2.5. Evaluation of Studies
3. Discussion
3.1. Context of Extractive Surgery
3.2. Review Study Discussion
4. Materials and Methods
4.1. Application Protocol and Website Recording Data
4.2. Target Questions
- What are the most widely used antibiotic protocols during wisdom tooth extraction surgery?
- Are there any alternatives? Are these more beneficial for the patient?
4.3. Search Strategy
4.4. Collection Data
4.5. Manuscript Selections
4.6. Research Classifications
4.7. Exclusion and Inclusion Criteria
- Investigated pharmacological prophylaxis or third molar extraction
- Clinical human randomized controlled trials
- Patients with other specific disease as osteoporosis, immunologic disorders, uncontrolled diabetes mellitus, or other surgical risk-related systemic conditions
- Not enough information regarding the topic
- Animal or in vitro studies
- Articles published prior to 1 February 2009
- No access to the title and abstract
4.8. Strategy for Collecting Data
4.9. Record of the Extracted and Collected Data Extraction
- “Author”—revealed the first author of publication
- “Year”—Year of publication
- “Type of study”—indicated the method of the research and some additional information
- “Sample size”—described the number of patients, animals or models examined
- “Protocols”—described types of groups or antibiotic protocols used
4.10. Risk of Bias Assessment
- Selection bias
- Performance bias and detection bias
- Attrition bias
- Reporting bias
- Examiner blinding, examiner calibration, standardized follow-up description, standardized residual graft measurement, standardized radiographic assessment
4.11. Third Molar Surgery
4.12. Used Antibiotics in Dentistry and Antibiotics Properties
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Fiorillo, L.; Cervino, G.; Herford, A.S.; Lauritano, F.; D’Amico, C.; Lo Giudice, R.; Laino, L.; Troiano, G.; Crimi, S.; Cicciu, M. Interferon Crevicular Fluid Profile and Correlation with Periodontal Disease and Wound Healing: A Systemic Review of Recent Data. Int. J. Mol. Sci. 2018, 19, 1908. [Google Scholar] [CrossRef] [PubMed]
- Singh Gill, A.; Morrissey, H.; Rahman, A. A Systematic Review and Meta-Analysis Evaluating Antibiotic Prophylaxis in Dental Implants and Extraction Procedures. Medicina (Kaunas) 2018, 54, 95. [Google Scholar] [CrossRef] [PubMed]
- Mercier, P.; Precious, D. Risks and benefits of removal of impacted third molars. A critical review of the literature. Int. J. Oral Maxillofac. Surg. 1992, 21, 17–27. [Google Scholar] [CrossRef]
- Bui, C.H.; Seldin, E.B.; Dodson, T.B. Types, Frequencies, and Risk Factors for Complications after Third Molar Extraction. J. Oral Maxillofac. Surg. 2003, 61, 1379–1389. [Google Scholar] [CrossRef]
- Isola, G.; Alibrandi, A.; Pedulla, E.; Grassia, V.; Ferlito, S.; Perillo, L.; Rapisarda, E. Analysis of the Effectiveness of Lornoxicam and Flurbiprofen on Management of Pain and Sequelae Following Third Molar Surgery: A Randomized, Controlled, Clinical Trial. J. Clin. Med. 2019, 8, 325. [Google Scholar] [CrossRef]
- Troiano, G.; Laino, L.; Cicciu, M.; Cervino, G.; Fiorillo, L.; D’Amico, C.; Zhurakivska, K.; Lo Muzio, L. Comparison of Two Routes of Administration of Dexamethasone to Reduce the Postoperative Sequelae After Third Molar Surgery: A Systematic Review and Meta-Analysis. Open Dent. J. 2018, 12, 181–188. [Google Scholar] [CrossRef]
- Laino, L.; Troiano, G.; Dioguardi, M.; Perillo, L.; Laino, G.; Lo Muzio, L.; Cicciu, M. Patient Discomfort During and After Surgically Assisted Rapid Maxillary Expansion Under Local Anaesthesia. J. Craniofac. Surg. 2016, 27, 772–775. [Google Scholar] [CrossRef]
- Isola, G.; Matarese, M.; Ramaglia, L.; Cicciu, M.; Matarese, G. Evaluation of the efficacy of celecoxib and ibuprofen on postoperative pain, swelling, and mouth opening after surgical removal of impacted third molars: a randomized, controlled clinical trial. Int. J. Oral Maxillofac. Surg. 2019. [Google Scholar] [CrossRef] [PubMed]
- Sortino, F.; Cicciu, M. Strategies used to inhibit postoperative swelling following removal of impacted lower third molar. Dent. Res. J. (Isfahan) 2011, 8, 162–171. [Google Scholar]
- Isola, G.; Cicciu, M.; Fiorillo, L.; Matarese, G. Association Between Odontoma and Impacted Teeth. J. Craniofac. Surg 2017, 28, 755–758. [Google Scholar] [CrossRef]
- Terauchi, M.; Akiya, S.; Kumagai, J.; Ohyama, Y.; Yamaguchi, S. An Analysis of Dentigerous Cysts Developed around a Mandibular Third Molar by Panoramic Radiographs. Dent. J. (Basel) 2019, 7, 13. [Google Scholar] [CrossRef]
- Cervino, G.; Fiorillo, L.; Herford, A.S.; Romeo, U.; Bianchi, A.; Crimi, S.; Amico, C.; De Stefano, R.; Troiano, G.; Santoro, R.; et al. Molecular Biomarkers Related to Oral Carcinoma: Clinical Trial Outcome Evaluation in a Literature Review. Dis. Markers 2019, 2019, 11. [Google Scholar] [CrossRef]
- Monaco, G.; Tavernese, L.; Agostini, R.; Marchetti, C. Evaluation of antibiotic prophylaxis in reducing postoperative infection after mandibular third molar extraction in young patients. J. Oral Maxillofac. Surg. 2009, 67, 1467–1472. [Google Scholar] [CrossRef]
- Luaces-Rey, R.; Arenaz-Bua, J.; Lopez-Cedrun-Cembranos, J.L.; Martinez-Roca, C.; Pertega-Diaz, S.; Sironvalle-Soliva, S. Efficacy and safety comparison of two amoxicillin administration schedules after third molar removal. A randomized, double-blind and controlled clinical trial. Med. Oral Patol. Oral Cir. Bucal. 2010, 15, e633–638. [Google Scholar] [CrossRef]
- Siddiqi, A.; Morkel, J.A.; Zafar, S. Antibiotic prophylaxis in third molar surgery: A randomized double-blind placebo-controlled clinical trial using split-mouth technique. Int. J. Oral Maxillofac. Surg 2010, 39, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Bezerra, T.P.; Studart-Soares, E.C.; Scaparo, H.C.; Pita-Neto, I.C.; Batista, S.H.; Fonteles, C.S. Prophylaxis versus placebo treatment for infective and inflammatory complications of surgical third molar removal: a split-mouth, double-blind, controlled, clinical trial with amoxicillin (500 mg). J. Oral Maxillofac. 2011, 69, e333–e339. [Google Scholar] [CrossRef]
- Adde, C.A.; Soares, M.S.; Romano, M.M.; Carnaval, T.G.; Sampaio, R.M.; Aldarvis, F.P.; Federico, L.R. Clinical and surgical evaluation of the indication of postoperative antibiotic prescription in third molar surgery. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2012, 114, S26–S31. [Google Scholar] [CrossRef] [PubMed]
- Sisalli, U.; Lalli, C.; Cerone, L.; Maida, S.; Manzoli, L.; Serra, E.; Dolci, M. Amoxicillin and clavulanic acid vs. ceftazidime in the surgical extraction of impacted third molar: a comparative study. Int. J. Immunopathol. Pharmacol. 2012, 25, 771–774. [Google Scholar] [CrossRef]
- Duvall, N.B.; Fisher, T.D.; Hensley, D.; Hancock, R.H.; Vandewalle, K.S. The comparative efficacy of 0.12% chlorhexidine and amoxicillin to reduce the incidence and magnitude of bacteremia during third molar extractions: a prospective, blind, randomized clinical trial. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2013, 115, 752–763. [Google Scholar] [CrossRef] [PubMed]
- Crincoli, V.; Di Comite, M.; Di Bisceglie, M.B.; Petruzzi, M.; Fatone, L.; De Biase, C.; Tecco, S.; Festa, F. Which route of antibiotic administration should be used for third molar surgery? A split-mouth study to compare intramuscular and oral intake. Clin. Ter. 2014, 165, e12–e16. [Google Scholar]
- Arteagoitia, I.; Ramos, E.; Santamaria, G.; Barbier, L.; Alvarez, J.; Santamaria, J. Amoxicillin/clavulanic acid 2000/125 mg to prevent complications due to infection following completely bone-impacted lower third molar removal: a clinical trial. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2015, 119, 8–16. [Google Scholar] [CrossRef]
- Milani, B.A.; Bauer, H.C.; Sampaio-Filho, H.; Horliana, A.C.; Perez, F.E.; Tortamano, I.P.; Jorge, W.A. Antibiotic therapy in fully impacted lower third molar surgery: randomized three-arm, double-blind, controlled trial. Oral Maxillofac. Surg. 2015, 19, 341–346. [Google Scholar] [CrossRef]
- Xue, P.; Wang, J.; Wu, B.; Ma, Y.; Wu, F.; Hou, R. Efficacy of antibiotic prophylaxis on postoperative inflammatory complications in Chinese patients having impacted mandibular third molars removed: A split-mouth, double-blind, self-controlled, clinical trial. Br. J. Oral Maxillofac. Surg. 2015, 53, 416–420. [Google Scholar] [CrossRef]
- Braimah, R.O.; Ndukwe, K.C.; Owotade, J.F.; Aregbesola, S.B. Impact of oral antibiotics on health-related quality of life after mandibular third molar surgery: An observational study. Niger. J. Clin. Pract. 2017, 20, 1189–1194. [Google Scholar] [CrossRef]
- Oteri, G.; Cicciu, M.; Peditto, M.; Catalano, A.; Loddo, S.; Pisano, M.; Lasco, A. Does Vitamin D3 Have an Impact on Clinical and Biochemical Parameters Related to Third Molar Surgery. J. Craniofac. Surg. 2016, 27, 469–476. [Google Scholar] [CrossRef]
- Moore, R.A.; Derry, S.; Wiffen, P.J.; Banerjee, S.; Karan, R.; Glimm, E.; Wiksten, A.; Aldington, D.; Eccleston, C. Estimating relative efficacy in acute postoperative pain: network meta-analysis is consistent with indirect comparison to placebo alone. Pain 2018, 159, 2234–2244. [Google Scholar] [CrossRef]
- Kim, J.-W.; Jo, Y.-Y.; Kim, J.-Y.; Oh, J.-h.; Yang, B.-E.; Kim, S.-G. Clinical Study for Silk Mat Application into Extraction Socket: A Split-Mouth, Randomized Clinical Trial. Appl. Sci. 2019, 9, 1208. [Google Scholar] [CrossRef]
- Ho, K.N.; Salamanca, E.; Chang, K.C.; Shih, T.C.; Chang, Y.C.; Huang, H.M.; Teng, N.C.; Lin, C.T.; Feng, S.W.; Chang, W.J. A Novel HA/beta-TCP-Collagen Composite Enhanced New Bone Formation for Dental Extraction Socket Preservation in Beagle Dogs. Materials (Basel) 2016, 9, 191. [Google Scholar] [CrossRef] [PubMed]
- Cicciu, M.; Cervino, G.; Herford, A.S.; Fama, F.; Bramanti, E.; Fiorillo, L.; Lauritano, F.; Sambataro, S.; Troiano, G.; Laino, L. Facial Bone Reconstruction Using both Marine or Non-Marine Bone Substitutes: Evaluation of Current Outcomes in a Systematic Literature Review. Mar. Drugs 2018, 16, 27. [Google Scholar] [CrossRef] [PubMed]
- Poli, P.P.; Beretta, M.; Cicciù, M.; Maiorana, C. Alveolar ridge augmentation with titanium mesh. A retrospective clinical study. Open Dent. J. 2014, 8, 148–158. [Google Scholar] [CrossRef] [PubMed]
- Cervino, G.; Terranova, A.; Briguglio, F.; De Stefano, R.; Famà, F.; D’Amico, C.; Amoroso, G.; Marino, S.; Gorassini, F.; Mastroieni, R.; et al. Diabetes: Oral health related quality of life and oral alterations. BioMed Res. Int. 2019, 2019. [Google Scholar] [CrossRef]
- Isola, G.; Ramaglia, L.; Cordasco, G.; Lucchese, A.; Fiorillo, L.; Matarese, G. The effect of a functional appliance in the management of temporomandibular joint disorders in patients with juvenile idiopathic arthritis. Minerva Stomatol. 2017, 66, 1–8. [Google Scholar] [PubMed]
- Cervino, G.; Fiorillo, L.; Laino, L.; Herford, A.S.; Lauritano, F.; Giudice, G.L.; Fama, F.; Santoro, R.; Troiano, G.; Iannello, G.; et al. Oral Health Impact Profile in Celiac Patients: Analysis of Recent Findings in a Literature Review. Gastroenterol. Res. Pract. 2018, 2018, 7848735. [Google Scholar] [CrossRef]
- Gagliano, A.; Aricò, I.; Calarese, T.; Condurso, R.; Germanò, E.; Cedro, C.; Spina, E.; Silvestri, R. Restless Leg Syndrome in ADHD children: Levetiracetam as a reasonable therapeutic option. Brain Dev. 2011, 33, 480–486. [Google Scholar] [CrossRef]
- Stacchi, C.; Berton, F.; Fiorillo, L.; Nicolin, V.; Lombardi, T.; Cicciù, M.; Di Lenarda, R. Fresh frozen allogeneic bone block in maxillary sinus floor elevation: Histomorphometric analysis of a bone specimen retrieved 15 years after grafting procedure. Appl. Sci. 2019, 9, 1119. [Google Scholar] [CrossRef]
- Sisk, A.L.; Hammer, W.B.; Shelton, D.W.; Joy, E.D. Complications following removal of impacted third molars: The role of the experience of the surgeon. J. Oral Maxillofac. Surg. 1986, 44, 855–859. [Google Scholar] [CrossRef]
- Pahlevan, R.; Keyhanlou, F.; Fazel, S.; Shahsavari, F. Keratocystic odontogenic tumor associated with impacted maxillary third molar extending to the antrum: A challenging diagnosis. Hum. Pathol. 2019, 15, 59–63. [Google Scholar] [CrossRef]
- Brignardello-Petersen, R. Antibiotic prophylaxis probably reduces the risk of developing postoperative infections but may increase the risk of experiencing adverse events in patients undergoing third-molar surgical extraction. J. Am. Dent. Assoc. 2019, 150, e30. [Google Scholar] [CrossRef]
- Cordero, E.; Vallejos, D.; Sadovnik, I.; Romo, L. Study of prevalence of third molar according to Pell and Gregory classification. Int.J. Oral Maxillofac. Surg. 2011, 40, 1127. [Google Scholar] [CrossRef]
- Pol, R.; Ruggiero, T.; Gallesio, G.; Riso, M.; Bergamasco, L.; Mortellaro, C.; Mozzati, M. Efficacy of Anti-Inflammatory and Analgesic of Superpulsed Low Level Laser Therapy After Impacted Mandibular Third Molars Extractions. J. Craniofac. Surg. 2016, 27, 685–690. [Google Scholar] [CrossRef]
- Cervino, G.; Fiorillo, L.; Spagnuolo, G.; Bramanti, E.; Laino, L.; Lauritano, F.; Cicciu, M. Interface Between MTA and Dental Bonding Agents: Scanning Electron Microscope Evaluation. J. Int. Soc. Prev. Community Dent. 2017, 7, 64–68. [Google Scholar]
- Marghalani, A. Antibiotic prophylaxis reduces infectious complications but increases adverse effects after third-molar extraction in healthy patients. J. Am. Dent. Assoc. 2014, 145, 476–478. [Google Scholar] [CrossRef] [PubMed]
- Savovic, J.; Turner, R.M.; Mawdsley, D.; Jones, H.E.; Beynon, R.; Higgins, J.P.T.; Sterne, J.A.C. Association Between Risk-of-Bias Assessments and Results of Randomized Trials in Cochrane Reviews: The ROBES Meta-Epidemiologic Study. Am. J. Epidemiol. 2018, 187, 1113–1122. [Google Scholar] [CrossRef] [PubMed]
- Mansournia, M.A.; Higgins, J.P.; Sterne, J.A.; Hernan, M.A. Biases in Randomized Trials: A Conversation Between Trialists and Epidemiologists. Epidemiology (Cambridge, Mass.) 2017, 28, 54–59. [Google Scholar] [CrossRef]
- Higgins, J.P.; Altman, D.G.; Gotzsche, P.C.; Juni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- Coburn, K.M.; Vevea, J.L. Publication bias as a function of study characteristics. Psychol. methods 2015, 20, 310–330. [Google Scholar] [CrossRef]
- Widek, T.; Genet, P.; Merkens, H.; Boldt, J.; Petrovic, A.; Vallis, J.; Scheurer, E. Dental age estimation: The chronology of mineralization and eruption of male third molars with 3T MRI. Forensic Sci. Int. 2019, 297, 228–235. [Google Scholar] [CrossRef]
- Suwa, G.; Kono, R.T.; Simpson, S.W.; Asfaw, B.; Lovejoy, C.O.; White, T.D. Paleobiological implications of the Ardipithecus ramidus dentition. Science 2009, 326, 94–99. [Google Scholar] [CrossRef]
- Staderini, E.; Patini, R.; Guglielmi, F.; Camodeca, A.; Gallenzi, P. How to Manage Impacted Third Molars: Germectomy or Delayed Removal? A Systematic Literature Review. Medicina (Kaunas) 2019, 55, 79. [Google Scholar] [CrossRef]
- Ryan, J.; Piercy, J.; James, P. Assessment of NICE guidance on two surgical procedures. Lancet 2004, 363, 1525–1526. [Google Scholar] [CrossRef]
- Garn, S.M.; Lewis, A.B.; Kerewsky, R.S. Third Molar Agenesis and Variation in Size of the Remaining Teeth. Nature 1964, 201, 839. [Google Scholar] [CrossRef]
- Garn, S.M.; Lewis, A.B.; Kerewsky, R.S. Third Molar Agenesis and Size Reduction of the Remaining Teeth. Nature 1963, 200, 488–489. [Google Scholar] [CrossRef]
- Garn, S.M.; Lewis, A.B.; Bonne, B. Third molar polymorphism and the timing of tooth formation. Nature 1961, 192, 989. [Google Scholar] [CrossRef]
- Evans, A.R.; Daly, E.S.; Catlett, K.K.; Paul, K.S.; King, S.J.; Skinner, M.M.; Nesse, H.P.; Hublin, J.J.; Townsend, G.C.; Schwartz, G.T.; et al. A simple rule governs the evolution and development of hominin tooth size. Nature 2016, 530, 477–480. [Google Scholar] [CrossRef] [PubMed]
- Menditti, D.; Laino, L.; Cicciu, M.; Mezzogiorno, A.; Perillo, L.; Menditti, M.; Cervino, G.; Lo Muzio, L.; Baldi, A. Kissing molars: report of three cases and new prospective on aetiopathogenetic theories. Int. J. Clin. Exp. Pathol. 2015, 8, 15708–15718. [Google Scholar]
- Vader, J.P. Retractor design and the lingual nerve. Lancet 1992, 339, 1117. [Google Scholar]
- Rancitelli, D.; Borgonovo, A.E.; Cicciù, M.; Re, D.; Rizza, F.; Frigo, A.C.; Maiorana, C. Maxillary sinus septa and anatomic correlation with the Schneiderian membrane. J. Craniofac. Surg. 2015, 26, 1394–1398. [Google Scholar] [CrossRef]
- Maridati, P.; Stoffella, E.; Speroni, S.; Cicciu, M.; Maiorana, C. Alveolar antral artery isolation during sinus lift procedure with the double window technique. Open Dent. J. 2014, 8, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Genc, A.; Cakarer, S.; Yalcin, B.K.; Kilic, B.B.; Isler, S.C.; Keskin, C. A comparative study of surgical drain placement and the use of kinesiologic tape to reduce postoperative morbidity after third molar surgery. Clin. Oral Investig. 2019, 23, 345–350. [Google Scholar] [CrossRef] [PubMed]
- Alkadi, S.; Stassen, L. Effect of One-Suture and Sutureless Techniques on Postoperative Healing After Third Molar Surgery. J. Oral Maxillofac. Surg. 2019, 77, e1–e703. [Google Scholar] [CrossRef] [PubMed]
- Nimcenko, T.; Omerca, G.; Bramanti, E.; Cervino, G.; Laino, L.; Cicciu, M. Autogenous wisdom tooth transplantation: A case series with 6-9 months follow-up. Dent. Res. J. (Isfahan) 2014, 11, 705–710. [Google Scholar]
- Laino, L.; Menditti, D.; Lo Muzio, L.; Laino, G.; Lauritano, F.; Cicciu, M. Extraoral surgical approach of ectopic mandibular third molar to the lower border of mandible. J. Craniofac. Surg. 2015, 26, e256–260. [Google Scholar] [CrossRef] [PubMed]
- Lombardi, T.; Bernardello, F.; Berton, F.; Porrelli, D.; Rapani, A.; Camurri Piloni, A.; Fiorillo, L.; Di Lenarda, R.; Stacchi, C. Efficacy of Alveolar Ridge Preservation after Maxillary Molar Extraction in Reducing Crestal Bone Resorption and Sinus Pneumatization: A Multicenter Prospective Case-Control Study. Biomed. Res. Int. 2018, 2018, 9352130. [Google Scholar] [CrossRef]
- Laino, L.; Cicciù, M.; Fiorillo, L.; Crimi, S.; Bianchi, A.; Amoroso, G.; Monte, I.P.; Herford, A.S.; Cervino, G. Surgical Risk on Patients with Coagulopathies: Guidelines on Hemophiliac Patients for Oro-Maxillofacial Surgery. Int. J. Environ. Res. Public Health 2019, 16, 1386. [Google Scholar] [CrossRef]
- Fiorillo, L.; De Stefano, R.; Cervino, G.; Crimi, S.; Bianchi, A.; Campagna, P.; Herford, A.S.; Laino, L.; Cicciù, M. Oral and Psychological Alterations in Haemophiliac Patients. Biomedicines 2019, 7, 33. [Google Scholar] [CrossRef] [PubMed]
- Rullo, R.; Scalzone, P.; Laino, L.; Russo, A.; Festa, V.M.; Fiorillo, L.; Cicciu, M. Solitary Plasmacytoma of the Mandible: Early Diagnosis and Surgical Management. J. Craniofac. Surg. 2019. [Google Scholar] [CrossRef]
- Cervino, G.; Fiorillo, L.; Herford, A.S.; Laino, L.; Troiano, G.; Amoroso, G.; Crimi, S.; Matarese, M.; D’Amico, C.; Nastro Siniscalchi, E.; et al. Alginate Materials and Dental Impression Technique: A Current State of the Art and Application to Dental Practice. Mar. Drugs 2018, 17, 18. [Google Scholar] [CrossRef]
- Isola, G.; Matarese, M.; Ramaglia, L.; Iorio-Siciliano, V.; Cordasco, G.; Matarese, G. Efficacy of a drug composed of herbal extracts on postoperative discomfort after surgical removal of impacted mandibular third molar: a randomized, triple-blind, controlled clinical trial. Clin. Oral Investig. 2019, 23, 2443–2453. [Google Scholar] [CrossRef]
- Stein, K.; Farmer, J.; Singhal, S.; Marra, F.; Sutherland, S.; Quiñonez, C. The use and misuse of antibiotics in dentistry: A scoping review. J. Am. Dent. Assoc. 2018, 149, 869–884. [Google Scholar] [CrossRef] [PubMed]
- Patini, R.; Coviello, V.; Riminucci, M.; Corsi, A.; Cicconetti, A. Early-stage diffuse large B-cell lymphoma of the submental region: a case report and review of the literature. Oral Surg. 2017, 10, 56–60. [Google Scholar] [CrossRef]
- Coviello, V.; Zareh Dehkhargani, S.; Patini, R.; Cicconetti, A. Surgical ciliated cyst 12 years after Le Fort I maxillary advancement osteotomy: a case report and review of the literature. Oral Surg. 2017, 10, 165–170. [Google Scholar] [CrossRef]
- Facciolo, M.-T.; Riva, F.; Gallenzi, P.; Patini, R.; Gaglioti, D. A rare case of oral multisystem Langerhans cell histiocytosis. J. Clin. Exp. Dent. 2017, 9, e820–e824. [Google Scholar] [CrossRef][Green Version]
- Patini, R.; Gallenzi, P.; Spagnuolo, G.; Cordaro, M.; Cantiani, M.; Amalfitano, A.; Arcovito, A.; Calla, C.; Mingrone, G.; Nocca, G. Correlation Between Metabolic Syndrome, Periodontitis and Reactive Oxygen Species Production. A Pilot Study. Open Dent. J. 2017, 12, 621–627. [Google Scholar] [CrossRef]
- Patini, R.; Staderini, E.; Lajolo, C.; Lopetuso, L.; Mohammed, H.; Rimondini, L.; Rocchetti, V.; Franceschi, F.; Cordaro, M.; Gallenzi, P. Relationship between oral microbiota and periodontal disease: a systematic review. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 5775–5788. [Google Scholar]
- Ferlazzo, N.; Currò, M.; Zinellu, A.; Caccamo, D.; Isola, G.; Ventura, V.; Carru, C.; Matarese, G.; Ientile, R. Influence of MTHFR Genetic Background on p16 and MGMT Methylation in Oral Squamous Cell Cancer. Int. J. Mol. Sci. 2017, 18, 724. [Google Scholar] [CrossRef]
- Lo Giudice, G.; Cutroneo, G.; Centofanti, A.; Artemisia, A.; Bramanti, E.; Militi, A.; Rizzo, G.; Favaloro, A.; Irrera, A.; Lo Giudice, R.; et al. Dentin morphology of root canal surface: A quantitative evaluation based on a scanning electronic microscopy study. BioMed. Res. Int. 2015, 2015. [Google Scholar] [CrossRef]
- Bramanti, E.; Matacena, G.; Cecchetti, F.; Arcuri, C.; Cicciù, M. Oral health-related quality of life in partially edentulous patients before and after implant therapy: A 2-year longitudinal study. Oral Implantol. (Rome) 2013, 6, 37–42. [Google Scholar] [CrossRef]
- Herford, A.S.; Cicciù, M.; Eftimie, L.F.; Miller, M.; Signorino, F.; Famà, F.; Cervino, G.; Lo Giudice, G.; Bramanti, E.; Lauritano, F.; et al. rhBMP-2 applied as support of distraction osteogenesis: A split-mouth histological study over nonhuman primates mandibles. Int. J. Clin. Exp. Med. 2016, 9, 17187–17194. [Google Scholar]
- Fama, F.; Cicciu, M.; Sindoni, A.; Nastro-Siniscalchi, E.; Falzea, R.; Cervino, G.; Polito, F.; De Ponte, F.; Gioffre-Florio, M. Maxillofacial and concomitant serious injuries: An eight-year single center experience. Chin. J. Traumatol. 2017, 20, 4–8. [Google Scholar] [CrossRef]
- Herford, A.S.; Miller, M.; Lauritano, F.; Cervino, G.; Signorino, F.; Maiorana, C. The use of virtual surgical planning and navigation in the treatment of orbital trauma. Chin. J. Traumatol. 2017, 20, 9–13. [Google Scholar] [CrossRef]
- Pippi, R.; Pietrantoni, A.; Patini, R.; Santoro, M.; Santoro, M. Is telephone follow-up really effective in early diagnosis of inflammatory complications after tooth extraction? Med. Oral Patol. Oral Cir. Bucal 2018, 23, e707–e715. [Google Scholar] [CrossRef] [PubMed]
| Author | Year | Type of Study | Sample Size | Protocols |
|---|---|---|---|---|
| Monaco et al. [13] | 2009 | RCT | 59 | Amoxicillin vs. placebo |
| Luaces-Rey et al. [14] | 2010 | RCT | 160 | Two amoxicillin different protocols |
| Siddiqi et al. [15] | 2010 | RCT, split mouth | 100 | Amoxicillin vs. placebo |
| Bezerra et al. [16] | 2011 | RCT, split mouth | 800 | Amoxicillin vs. placebo |
| Adde et al. [17] | 2012 | RCT | 71 | Amoxicillin vs. clindamycin vs. placebo |
| Sisalli et al. [18] | 2012 | RCT | 107 | Amoxicillin clavulanate vs. ceftazidime |
| Duvall et al. [19] | 2013 | RCT | 30 | Chlorhexidine 0.12% rinse vs. amoxicillin vs. placebo |
| Crincoli et al. [20] | 2014 | RCT, split mouth | 24 | Amoxicillin clavulanate vs. cefazolin |
| Arteagoitia et al. [21] | 2015 | RCT | 118 | Amoxicillin vs. placebo |
| Milani et al. [22] | 2015 | RCT | 80 | Two different routes of amoxicillin vs. placebo |
| Xue et al. [23] | 2015 | RCT, slit mouth | 207 | Amoxicillin vs. placebo |
| Braimah et al. [24] | 2017 | RCT | 135 | Two different routes of amoxicillin vs. levofloxacin |
| Risk of Bias | [13] | [14] | [15] | [16] | [17] | [18] | [19] | [20] | [21] | [22] | [23] | [24] |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low Risk | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||
| Medium Risk | ✓ | |||||||||||
| High Risk | ||||||||||||
| Unclear Risk | ✓ | ✓ | ✓ | ✓ |
| Author | Drug Side Effects | Quality of Life | Dysphagia | Trismus and Mouth Opening | Pain | Swelling | Fever | Wound Infection | Purulent Discharge | Edema and Abscess | Bacteremia | Lympha Deno Pathy |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Monaco et al. | NS | NS | NS | NS | ||||||||
| Luaces-Rey et al. | NS | NS | NS | NS | NS | |||||||
| Siddiqi et al. | NS | NS p >0.05 | NS p >0.05 | NS | NS | NS | NS | |||||
| Bezerra et al. | NS | NS p = 0.21 | NS | NS | ||||||||
| Adde et al. | NS | NS p >0.05 | ||||||||||
| Sisalli et al. | NS | NS | NS | NS | NS | |||||||
| Duvall et al. | NS | |||||||||||
| Crincoli et al. | NS | NS | NS | NS | NS | NS | ||||||
| Arteagoitia et al. | S | S | NS | S | ||||||||
| Milani et al. | NS p = 0.99 | NS | NS | NS p = 0.06 | ||||||||
| Xue et al. | S p = 0.005 | NS | ||||||||||
| Braimah et al. | S |
| Active Principle Formulation | Before Surgery | After Surgery |
|---|---|---|
| Amoxicillin | 2 g 1 h before surgery | 500 mg every 8 h after surgery for 7 days |
| Amoxicillin clavulanate | 500 + 125 mg 2 days before surgery | 500 + 125 mg every 12 h for another 4 days. |
| Amoxicillin clavulanate | 875 + 125 mg 2 days before surgery | 875 + 125 mg every 12 h for another 4 days. |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cervino, G.; Cicciù, M.; Biondi, A.; Bocchieri, S.; Herford, A.S.; Laino, L.; Fiorillo, L. Antibiotic Prophylaxis on Third Molar Extraction: Systematic Review of Recent Data. Antibiotics 2019, 8, 53. https://doi.org/10.3390/antibiotics8020053
Cervino G, Cicciù M, Biondi A, Bocchieri S, Herford AS, Laino L, Fiorillo L. Antibiotic Prophylaxis on Third Molar Extraction: Systematic Review of Recent Data. Antibiotics. 2019; 8(2):53. https://doi.org/10.3390/antibiotics8020053
Chicago/Turabian StyleCervino, Gabriele, Marco Cicciù, Antonio Biondi, Salvatore Bocchieri, Alan Scott Herford, Luigi Laino, and Luca Fiorillo. 2019. "Antibiotic Prophylaxis on Third Molar Extraction: Systematic Review of Recent Data" Antibiotics 8, no. 2: 53. https://doi.org/10.3390/antibiotics8020053
APA StyleCervino, G., Cicciù, M., Biondi, A., Bocchieri, S., Herford, A. S., Laino, L., & Fiorillo, L. (2019). Antibiotic Prophylaxis on Third Molar Extraction: Systematic Review of Recent Data. Antibiotics, 8(2), 53. https://doi.org/10.3390/antibiotics8020053










