A Topical Desiccant Agent in Association with Manual Debridement in the Initial Treatment of Peri-Implant Mucositis: A Clinical and Microbiological Pilot Study
Abstract
1. Introduction
2. Results
2.1. Demographics
2.2. Clinical Outcomes
2.3. Microbiological Results
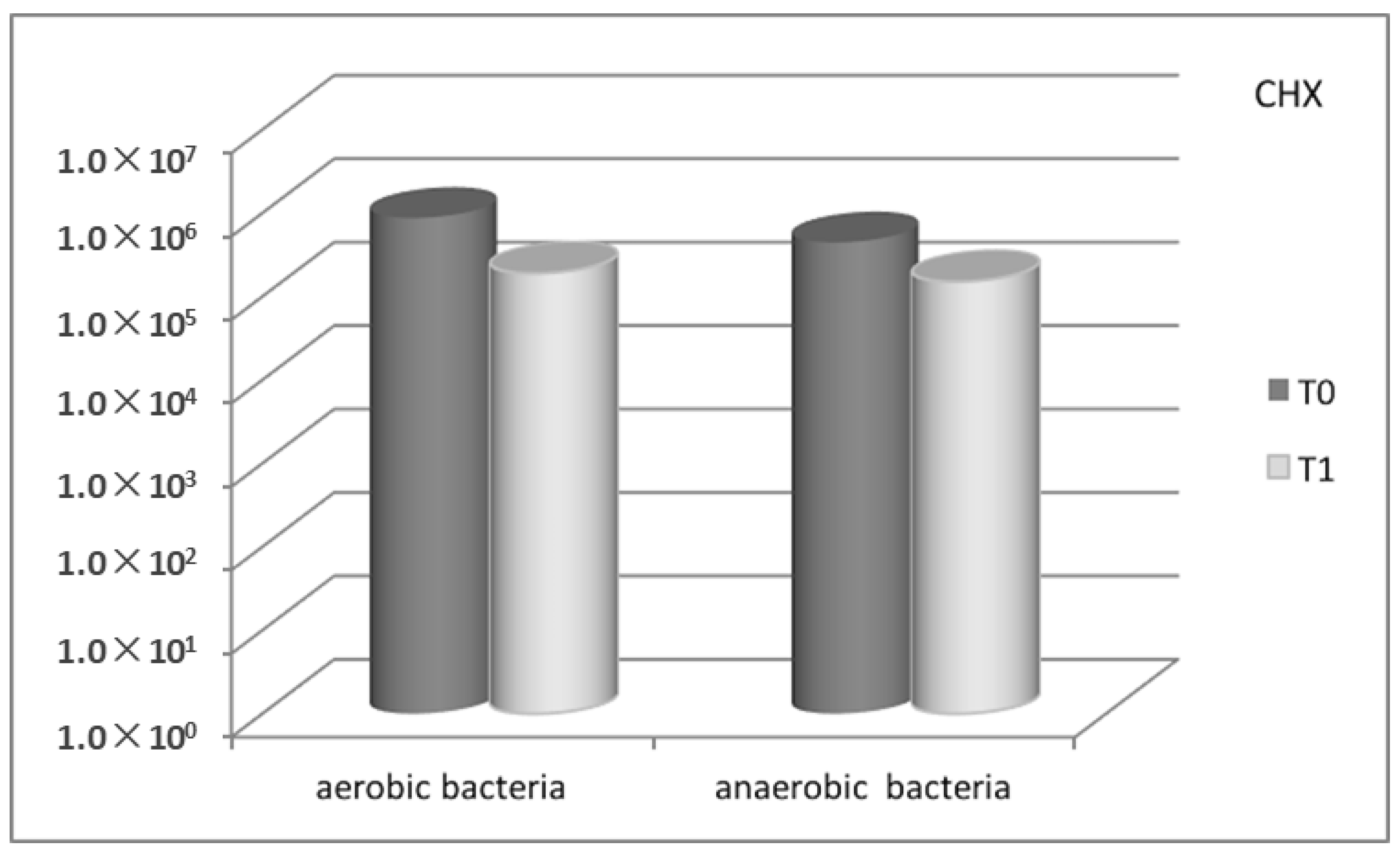
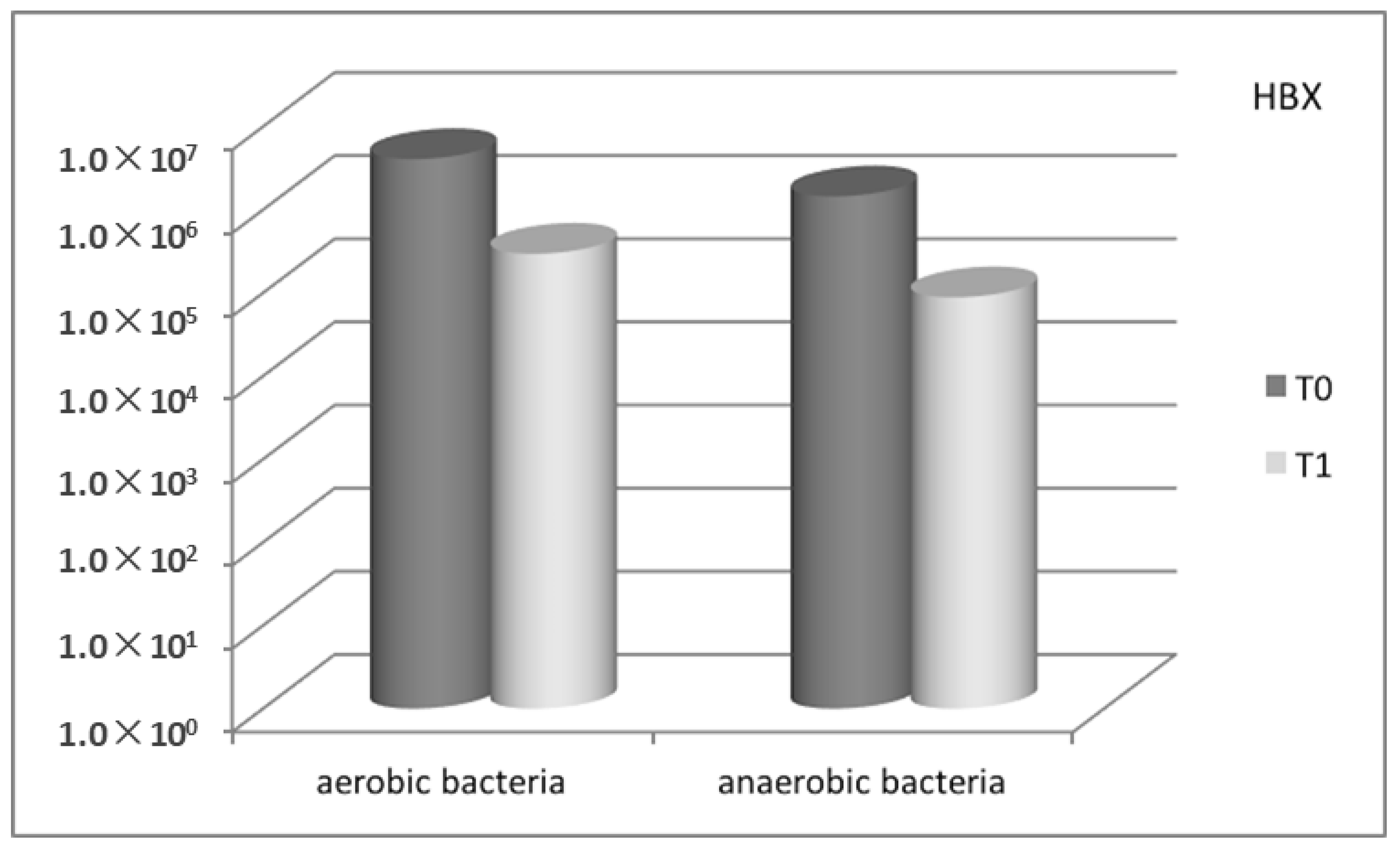
2.3.1. Bacterial Count Evaluation
2.3.2. Molecular Biology—Multiplex PCR (Polymerase Chain Reaction)
2.4. Patients’ Degree of Satisfaction
3. Discussion
4. Materials and Methods
4.1. Study Design
4.2. Soft Tissues Assessment
- -
- PPD, recorded in mm as the distance between the gingival margin and the base of the periodontal pocket;
- -
- BOP, recorded as 0 (no bleeding) or 1 (bleeding) after probing for PPD;
- -
- Modified Bleeding Index (mBI), recorded as 0, 1, 2, 3 according to Mombelli et al. [38];
- -
- Visible Plaque Index (VPI), recorded as 0 (no plaque) or 1 (plaque) after probing for PPD;
- -
- Modified Plaque Index (mPLI), recorded as 0, 1, 2, 3 according to Mombelli et al. [38].
4.3. Microbial Sampling and Analysis
4.3.1. Culture Investigation
4.3.2. DNA Extraction and Multiplex PCR Condition
4.4. Study Protocol and Treatment
4.5. Test Substances and Administration
4.6. Patients’ Degree of Satisfaction
4.7. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Pjetursson, B.E.; Karoussis, I.; Bürgin, W.; Brägger, U.; Lang, N.P. Patients’ satisfaction following implant therapy. A 10-year prospective cohort study. Clin. Oral Implant. Res. 2005, 16, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Berglundh, T.; Lindhe, J.; Ericsson, I.; Marinello, C.P.; Liljenberg, B.; Thomsen, P. The soft tissue barrier at implants and teeth. Clin. Oral Implant. Res. 1991, 2, 81–90. [Google Scholar] [CrossRef]
- Zitzmann, N.U.; Berglundh, T. Definition and prevalence of peri-implant diseases. J. Clin. Periodontol. 2008, 35, 286–291. [Google Scholar] [CrossRef] [PubMed]
- Atieh, M.A.; Alsabeeha, N.H.; Faggion, C.M., Jr.; Duncan, W.J. The frequency of peri-implant diseases: A systematic review and meta- analysis. J. Periodontol. 2013, 84, 1586–1598. [Google Scholar] [CrossRef] [PubMed]
- Derks, J.; Tomasi, C. Peri-implant health and disease. A systematic review of current epidemiology. J. Clin. Periodontol. 2015, 42, S158–S171. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.T.; Huang, Y.W.; Zhu, L.; Weltman, R. Prevalences of peri-implantitis and peri-implant mucositis: Systematic review and meta-analysis. J. Dent. 2017, 62, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Jepsen, S.; Berglundh, T.; Genco, R.; Aass, A.M.; Demirel, K.; Derks, J.; Figuero, E.; Giovannoli, J.L.; Goldstein, M.; Lambert, F.; et al. Primary prevention of peri-implantitis: Managing peri-implant mucositis. J. Clin. Periodontol. 2015, 42, S152–S157. [Google Scholar] [CrossRef]
- Salvi, G.E.; Zitzmann, N.U. The effects of anti-infective preventive measures on the occurrence of biologic implant complications and implant loss: A systematic review. Int. J. Oral Maxillofac. Implant. 2014, 29, 292–307. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, F.; Sculean, A.; Rothamel, D.; Schwenzer, K.; Georg, T.; Becker, J. Clinical evaluation of an Er: YAG laser for nonsurgical treatment of peri-implantitis: A pilot study. Clin. Oral Implant. Res. 2005, 16, 44–52. [Google Scholar] [CrossRef] [PubMed]
- Renvert, S.; Lindahl, C.; Roos Jansåker, A.M.; Persson, G.R. Treatment of peri-implantitis using an Er:YAG laser or an air-abrasive device: A randomized clinical trial. J. Clin. Periodontol. 2011, 38, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Schenk, G.; Flemmig, T.F.; Betz, T.; Reuther, J.; Klaiber, B. Controlled local delivery of tetracycline HCl in the treatment of peri implant mucosal hyperplasia and mucositis. A controlled case series. Clin. Oral Implant. Res. 1997, 8, 427–433. [Google Scholar] [CrossRef]
- Porras, R.; Anderson, G.B.; Caffesse, R.; Narendran, S.; Trejo, P.M. Clinical response to 2 different therapeutic regimens to treat peri-implant mucositis. J. Periodontol. 2002, 73, 1118–1125. [Google Scholar] [CrossRef] [PubMed]
- Renvert, S.; Lessem, J.; Dahlén, G.; Lindahl, C.; Svensson, M. Topical minocycline microspheres versus topical chlorhexidine gel as an adjunct to mechanical debridement of incipient peri-implant infections: A randomized clinical trial. J. Clin. Periodontol. 2006, 33, 362–369. [Google Scholar] [CrossRef] [PubMed]
- Renvert, S.; Lessem, J.; Dahlén, G.; Renvert, H.; Lindahl, C. Mechanical and repeated antimicrobial therapy using a local drug delivery system in the treatment of peri-implantitis: A randomized clinical trial. J. Periodontol. 2008, 79, 836–844. [Google Scholar] [CrossRef] [PubMed]
- Hallström, H.; Persson, G.R.; Lindgren, S.; Olofsson, M.; Renvert, S. Systemic antibiotics and debridement of peri-implant mucositis. A randomized clinical trial. J. Clin. Periodontol. 2012, 39, 574–581. [Google Scholar] [CrossRef] [PubMed]
- Walker, C.B.; Godowski, K.C.; Borden, L.; Lennon, J.; Nangò, S.; Stone, C.; Garrett, S. The effects of sustained release doxycycline on the anaerobic flora and antibiotic-resistant patterns in subgingival plaque and saliva. J. Periodontol. 2000, 71, 768–774. [Google Scholar] [CrossRef]
- Heitz-Mayfield, L.J.; Lang, N.P. Antimicrobial treatment of peri-implant diseases. Int. J. Oral Maxillofac. Implant. 2004, 19, 128–139. [Google Scholar]
- Heitz-Mayfield, L.J.; Salvi, G.E.; Botticelli, D.; Mombelli, A.; Faddy, M.; Lang, N.P. Implant Complication Research Group. Anti-infective treatment of peri-implant mucositis: A randomised controlled clinical trial. Clin. Oral Implant. Res. 2011, 22, 237–241. [Google Scholar] [CrossRef]
- Lombardo, G.; Signoretto, C.; Corrocher, G.; Pardo, A.; Pighi, J.; Rovera, A.; Caccuri, F.; Nocini, P.F. A topical desiccant agent in association with ultrasonic debridement in the initial treatment of chronic periodontitis: A clinical and microbiological study. New Microbiol. 2015, 38, 393–407. [Google Scholar]
- Isola, G.; Matarese, G.; Williams, R.C.; Siciliano, V.I.; Alibrandi, A.; Cordasco, G.; Ramaglia, L. The effects of a desiccant agent in the treatment of chronic periodontitis: A randomized, controlled clinical trial. Clin. Oral Investig. 2018, 22, 791–800. [Google Scholar] [CrossRef]
- Porter, S.R.; Al-Johani, K.; Fedele, S.; Moles, D.R. Randomised controlled trial of the efficacy of HybenX in the symptomatic treatment of recurrent aphthous stomatitis. Oral Dis. 2009, 15, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Bracke, J.; Basara, M.; Savord, E.; Dunaway, A.; Watkins, M. Pilot evaluation of a simple adjunctive method for improved removal of oral biofilm during conventional scaling and root planing therapy. J. Biol. Regul. Homeost. Agents 2015, 29, 6–9. [Google Scholar] [PubMed]
- Lombardo, G.; Corrocher, G.; Rovera, A.; Pighi, J.; Marincola, M.; Lehrberg, J.; Nocini, P.F. Decontamination using a desiccant with air powder abrasion followed by biphasic calcium sulfate grafting: A new treatment for peri-implantitis. Case Rep. Dent. 2015, 2015, 474839. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Huang, R.; Li, M.; Gregory, L.C. Bacterial interactions in dental biofilm. Virulence 2011, 2, 435–444. [Google Scholar] [CrossRef] [PubMed]
- Marsh, P.D. Dental plaque: Biological significance of a biofilm and community life-style. J. Clin. Periodontol. 2005, 32, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Stoodley, P.; Sauer, K.; Davies, D.G.; Costerton, J.W. Biofilms as complex differentiated communities. Annu. Rev. Microbiol. 2002, 56, 187–209. [Google Scholar] [CrossRef]
- Zijnge, V.; van Leeuwen, M.B.; Degener, J.E.; Abbas, F.; Thurnheer, T.; Gmür, R.; Harmsen, H.J. Oral biofilm architecture on natural teeth. PLoS ONE 2010, 5, e9321. [Google Scholar] [CrossRef]
- Renvert, S.; Lessem, J.; Lindahl, C.; Svensson, M. Treatment of incipient peri-implant infections using topical minocycline microspheres versus topical chlorhexidine gel as an adjunct to mechanical debridement. J. Int. Acad. Periodontol. 2004, 6, 154–159. [Google Scholar]
- Herrera, D.; Matesanz, P.; Bascones-Martìnez, A.; Sanz, M. Local and systemic antimicrobial therapy in periodontics. J. Evid. Based Dent. Pract. 2012, 12, 50–60. [Google Scholar] [CrossRef]
- Paolantonio, M.; D’Ercole, S.; Pilloni, A.; D’Archivio, D.; Lisanti, L.; Graziani, F.; Femminella, B.; Sanmartino, G.; Perillo, L.; Tetè, S.; et al. Clinical, microbiologic, and biochemical effects of subgingival administration of a Xanthan-based chlorhexidine gel in the treatment of periodontitis: A randomized multicenter trial. J. Periodontol. 2009, 80, 1479–1492. [Google Scholar] [CrossRef]
- Thöne-Mühling, M.; Swierkot, K.; Nonnenmacher, C.; Mutters, R.; Flores-de-Jacoby, L.; Mengel, R. Comparison of two full-mouth approaches in the treatment of peri-implant mucositis: A pilot study. Clin. Oral Implant. Res. 2010, 21, 504–512. [Google Scholar] [CrossRef] [PubMed]
- Menezes, K.M.; Fernandes-Costa, A.N.; Silva-Neto, R.D.; Calderon, P.S.; Gurgel, B.C. Efficacy of 0.12% chlorhexidine gluconate for non-surgical treatment of peri-implant mucositis. J. Periodontol. 2016, 87, 1305–1313. [Google Scholar] [CrossRef] [PubMed]
- Pini-Prato, G.; Magnani, C.; Rotundo, R. Nonsurgical treatment of peri-implantitis using the biofilm decontamination approach: A case report study. Int. J. Periodontics Restor. Dent. 2016, 36, 383–391. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Costa, F.O.; Ferreira, S.D.; Cortelli, J.R.; Lima, R.P.E.; Cortelli, S.C.; Cota, L.O.M. Microbiological profile associated with peri-implant diseases in individuals with and without preventive maintenance therapy: A 5-year follow-up. Clin. Oral Investig. 2018, 1. [Google Scholar] [CrossRef] [PubMed]
- Hultin, M.; Gustafsson, A.; Hallström, H.; Johansson, L.A.; Ekfeldt, A.; Klinge, B. Microbiological findings and host response in patients with peri-implantitis. Clin. Oral Implant. Res. 2002, 13, 349–358. [Google Scholar] [CrossRef]
- CONSORT Transparent Reporting of Trials. Available online: http://www.consort-statement.org (accessed on 10 June 2018).
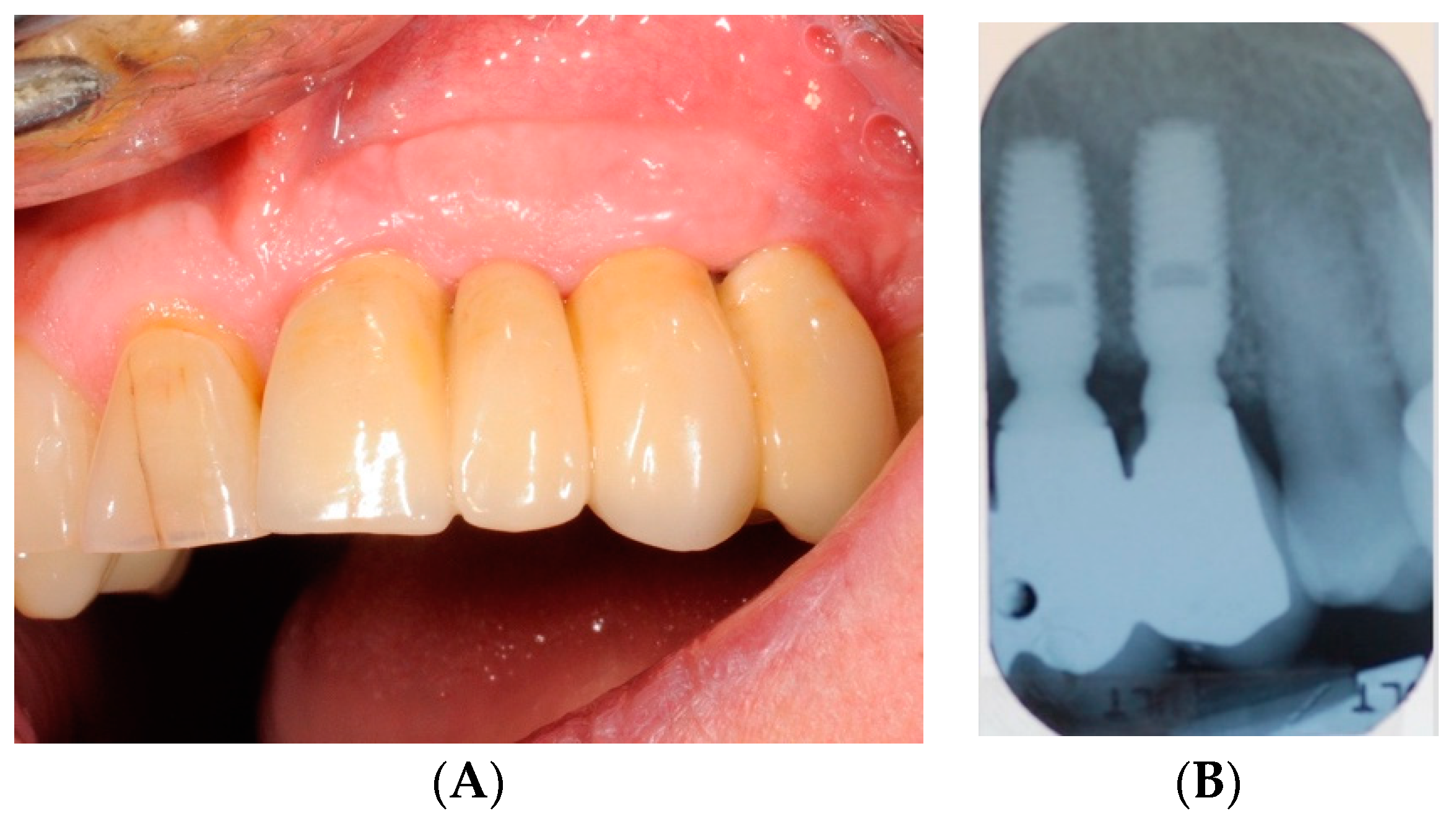
- Lombardo, G.; Pighi, J.; Marincola, M.; Corrocher, G.; Simancas-Pallares, M.; Nocini, P.F. Cumulative success rate of short and ultrashort implants supporting single crowns in the posterior maxilla: A 3-year retrospective study. Int. J. Dent. 2017, 2017, 8434281. [Google Scholar] [CrossRef]
- Mombelli, A.; Lang, N.P. Clinical parameter for the evaluation of dental implants. Periodontol. 2000 1994, 4, 81–86. [Google Scholar] [CrossRef]
- Galgali, S.R.; Gontiya, G. Evaluation of an innovative radiographic technique-parallel profile radiography to determine the dimensions of dentogingival unit. Indian J. Dent. Res. 2011, 22, 237–241. [Google Scholar]
- Signoretto, C.; Marchi, A.; Bertoncelli, A.; Burlacchini, G.; Milli, A.; Tessarolo, F.; Caola, I.; Papetti, A.; Pruzzo, C.; Zaura, E.; et al. Effects of mushroom and chicory extracts on the shape, physiology and proteome of the cariogenic bacterium Streptococcus mutans. BMC Complement. Altern. Med. 2013, 13, 117. [Google Scholar] [CrossRef] [PubMed]
- García, L.; Tercero, J.C.; Legido, B.; Ramos, J.A.; Alemany, J.; Sanz, M. Rapid detection of Actinobacillus actinomycetemcomitans, Prevotella intermedia and Porphyromona gingivalis by multiplex PCR. J. Periodontal Res. 1998, 33, 59–64. [Google Scholar] [CrossRef]






| Variable | Overall (n) | Test Group HBX (n) | Control Group CHX (n) | p Value |
|---|---|---|---|---|
| Number of patients | 23 | 12 | 11 | NS 1 |
| Age 2 | 58.97 (10.09) | 60.55 (6.59) | 55.92 (14.45) | NS |
| Number of implants | 52 | 27 | 25 | NS |
| Sex | ||||
| Implants placed in Male | 27 | 16 | 11 | NS |
| Implants placed in Female | 25 | 11 | 14 | |
| Smoking habit | ||||
| Implants placed in Non-Smokers | 45 | 23 | 22 | NS |
| Implants placed in Smokers | 7 | 4 | 3 | |
| ASA status | ||||
| Implants placed in ASA 1 patients | 32 | 18 | 14 | NS |
| Implants placed in ASA 2 patients | 20 | 9 | 11 | |
| Number of TPS 3 sessions /year | ||||
| = 1/Year | 15 | 7 | 8 | NS |
| > 1/Year | 37 | 20 | 17 | |
| Interproximal oral hygiene | ||||
| No | 21 | 12 | 9 | NS |
| Yes | 31 | 15 | 16 |
| PPD | All Sites/Implant (n = 162) | All Sites/Implant (n = 150) | p Value | Qualifying Site/Implant (n = 27) | Qualifying Site/Implant (n = 25) | p Value |
| Observation Interval | HBX Group | CHX Group | HBX Group | CHX Group | ||
| T0 (Day 0) | 3.70 (0.83) | 3.78 (0.81) | NS 1 | 4.85 (0.99) | 5.64 (1.50) | NS |
| T1 (Day 90) | 3.29 (0.72) | 3.55 (0.83) | NS | 4.37 (1.04) | 5.14 (1.61) | NS |
| p value | NS | NS | NS | NS | ||
| mBI | All Sites/Implant (n = 162) | All Sites/Implant (n = 150) | p Value | Qualifying Site/Implant (n = 27) | Qualifying Site/Implant (n = 25) | p Value |
| Observation Interval | HBX Group | CHX Group | HBX Group | CHX Group | ||
| T0 (Day 0) | 1.53 (0.55) | 1.53 (0.59) | NS | 2.67 (0.48) | 2.43 (0.51) | NS |
| T1 (Day 90) | 0.43 (0.34) | 0.93 (0.51) | NS | 1.48 (0.70) | 1.57 (0.65) | NS |
| p value | <0.05 * | NS | <0.05 * | <0.05 * | ||
| BOP | All Sites/Implant (n = 162) | All Sites/Implant (n = 150) | p Value | Qualifying Site/Implant (n = 27) | Qualifying Site/Implant (n = 25) | p Value |
| Observation Interval | HBX Group | CHX Group | HBX Group | CHX Group | ||
| T0 (Day 0) | 75.92% | 68.66% | NS | 100% | 100% | NS |
| T1 (Day 90) | 42.23% | 52.57% | NS | 42.78% | 57.63% | NS |
| p value | <0.05 * | NS | <0.05 * | <0.05 * | ||
| mPLI | All Sites/Implant (n = 162) | All Sites/Implant (n = 150) | p Value | Qualifying Site/Implant (n = 27) | Qualifying Site/Implant (n = 25) | p Value |
| Observation Interval | HBX Group | CHX Group | HBX Group | CHX Group | ||
| T0 (Day 0) | 0.38 (0.46) | 0.75 (0.68) | NS | 0.67 (0.43) | 1.21 (1.05) | NS |
| T1 (Day 90) | 0.09 (0.20) | 0.39 (0.36) | <0.05 * | 0.26 (0.53) | 1.14 (0.86) | <0.05 * |
| p value | <0.05 * | NS | NS | NS | ||
| VPI | All Sites/Implant (n = 162) | All Sites/Implant (n = 150) | p Value | Qualifying Site/Implant (n = 27) | Qualifying Site/Implant (n = 25) | p Value |
| Observation Interval | HBX Group | CHX Group | HBX Group | CHX Group | ||
| T0 (Day 0) | 31.48% | 54.76% | NS | 44.54% | 29.01% | NS |
| T1 (Day 90) | 8.64% | 26.19% | <0.05 * | 7.43% | 10.74% | NS |
| p value | <0.05 * | <0.05 * | <0.05 * | NS |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lombardo, G.; Signoriello, A.; Corrocher, G.; Signoretto, C.; Burlacchini, G.; Pardo, A.; Nocini, P.F. A Topical Desiccant Agent in Association with Manual Debridement in the Initial Treatment of Peri-Implant Mucositis: A Clinical and Microbiological Pilot Study. Antibiotics 2019, 8, 82. https://doi.org/10.3390/antibiotics8020082
Lombardo G, Signoriello A, Corrocher G, Signoretto C, Burlacchini G, Pardo A, Nocini PF. A Topical Desiccant Agent in Association with Manual Debridement in the Initial Treatment of Peri-Implant Mucositis: A Clinical and Microbiological Pilot Study. Antibiotics. 2019; 8(2):82. https://doi.org/10.3390/antibiotics8020082
Chicago/Turabian StyleLombardo, Giorgio, Annarita Signoriello, Giovanni Corrocher, Caterina Signoretto, Gloria Burlacchini, Alessia Pardo, and Pier Francesco Nocini. 2019. "A Topical Desiccant Agent in Association with Manual Debridement in the Initial Treatment of Peri-Implant Mucositis: A Clinical and Microbiological Pilot Study" Antibiotics 8, no. 2: 82. https://doi.org/10.3390/antibiotics8020082
APA StyleLombardo, G., Signoriello, A., Corrocher, G., Signoretto, C., Burlacchini, G., Pardo, A., & Nocini, P. F. (2019). A Topical Desiccant Agent in Association with Manual Debridement in the Initial Treatment of Peri-Implant Mucositis: A Clinical and Microbiological Pilot Study. Antibiotics, 8(2), 82. https://doi.org/10.3390/antibiotics8020082






