Historical Overview of the Evolution of Multidrug-Resistant Gram-Negative Infections in Tunisia from 1999 to 2019
Abstract
1. Introduction
2. Results
2.1. Distribution of Gram-Negative Bacilli
2.2. Overall Frequency of Antibiotic Resistance
2.3. Antibiotic Resistance Frequency by Samples and Type of Resistant Strains
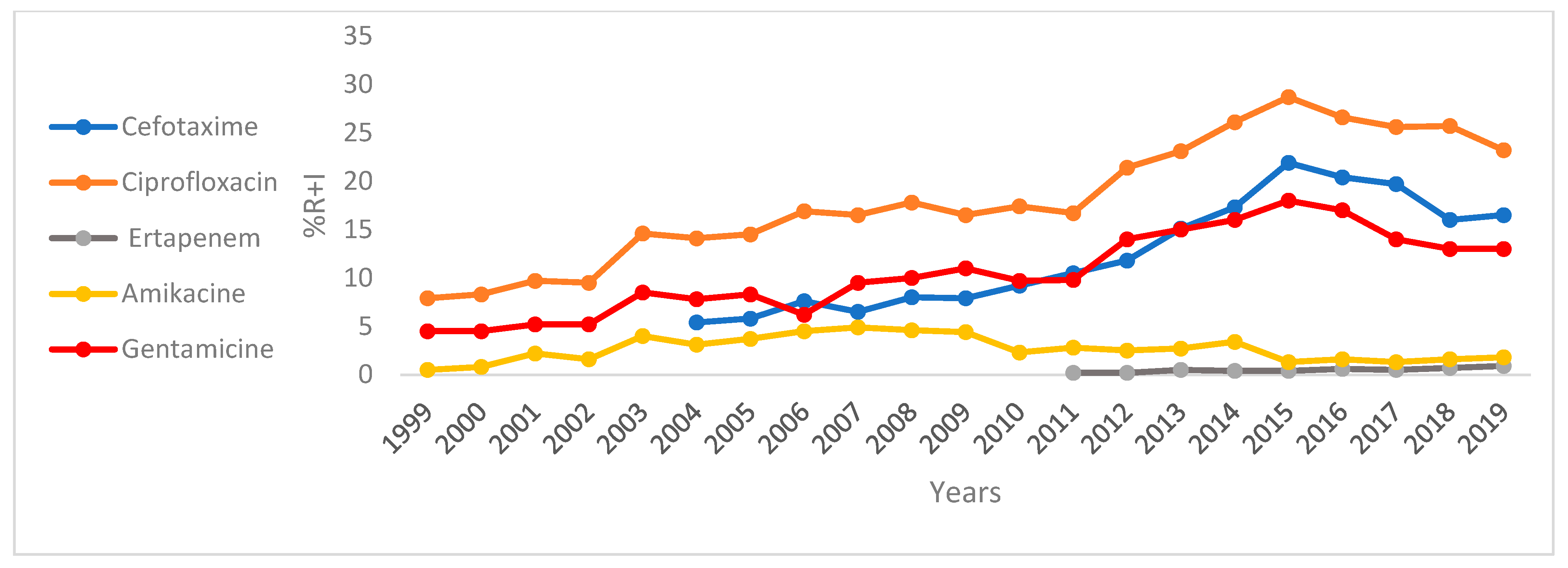
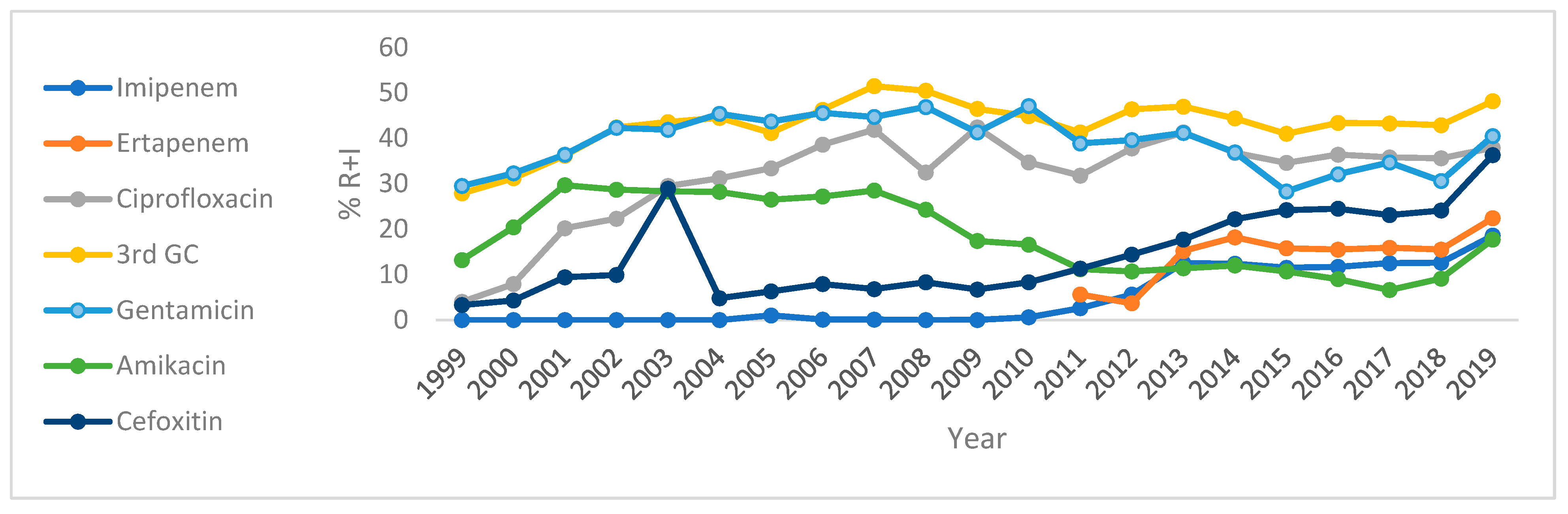
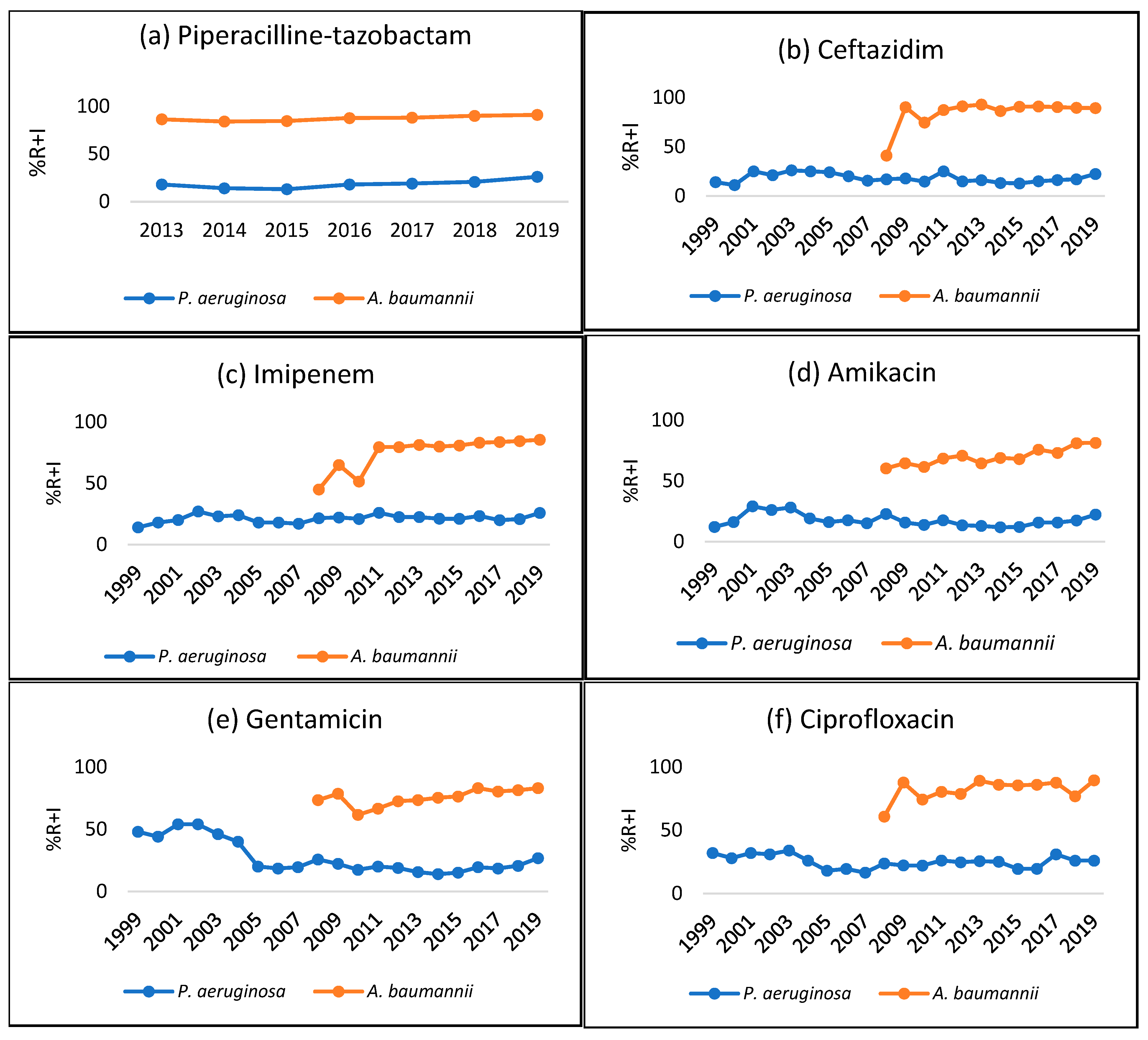
2.4. Antimicrobial Susceptibility Trends
3. Discussion
4. Conclusions
5. Materials and Methods
5.1. Study Sites and Inclusion
5.2. Antimicrobial Susceptibility Testing
5.3. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AMR | antimicrobial resistance |
| AMC | amoxicillin–clavulanic acid |
| AMK | amikacin |
| AMX | amoxicillin |
| AST | antimicrobial susceptibility testing |
| BSI | bloodstream infections |
| CAZ | ceftazidime |
| CDC | Centers for Disease Control and Prevention |
| CIP | ciprofloxacin |
| CTX | cefotaxime |
| COL | colistin |
| EUCAST | European Committee on Antimicrobial Susceptibility Testing |
| ESBLs | extended-spectrum β-lactamases |
| ETP | ertapenem |
| FEP | cefepime |
| FOS | fosfomycin |
| FOX | cefoxitin |
| GEN | gentamicin |
| GNBs | Gram-negative bacteria |
| IAI | intra-abdominal infections |
| IMP | imipenem |
| IQC | internal quality control |
| LART | L’AntibioRésistance en Tunisie |
| MEM | meropenem |
| MDR | multidrug-resistant |
| NAL | nalidixic acid |
| PIP | piperacillin |
| RTIs | respiratory tract infections |
| SXT | trimethoprim–sulfamethoxazole |
| TIC | ticarcillin |
| TIM | ticarcillin–clavulanic acid |
| TZP | piperacillin-tazobactam |
| UTIs | urinary tract infections |
| 3GCs | 3rd-generation cephalosporins |
References
- Oli, A.N.; Itumo, C.J.; Okam, P.C.; Ezebialu, I.U.; Okeke, K.N.; Ifezulike, C.C.; Ezeobi, I.; Emechebe, G.O.; Okezie, U.M.; Adejumo, S.A.; et al. Carbapenem-Resistant Enterobacteriaceae Posing a Dilemma in Effective Healthcare Delivery. Antibiotics 2019, 8, 156. [Google Scholar] [CrossRef] [PubMed]
- Bassetti, M.; Garau, J. Current and future perspectives in the treatment of multidrug-resistant Gram-negative infections. J. Antimicrob. Chemother. 2021, 76 (Suppl. S4), iv23–iv37. [Google Scholar] [CrossRef]
- Antimicrobial Resistance Threats in the United States, 2021–2022|Antimicrobial Resistance|CDC. Available online: https://www.cdc.gov/antimicrobial-resistance/data-research/threats/update-2022.html (accessed on 25 May 2025).
- Mackow, N.A. and van Duin, D. Reviewing novel treatment options for carbapenem-resistant Enterobacterales. Expert Rev. Anti-Infect. Ther. 2024, 22, 71–85. [Google Scholar] [CrossRef] [PubMed]
- Ponce-de-Leon, A.; Rodríguez-Noriega, E.; Morfín-Otero, R.; Cornejo-Juárez, D.P.; Tinoco, J.C.; Martínez-Gamboa, A.; Gaona-Tapia, C.J.; Guerrero-Almeida, M.L.; Martin-Onraët, A.; Cervantes, J.L.V.; et al. Antimicrobial susceptibility of gram-negative bacilli isolated from intra-abdominal and urinary-tract infections in Mexico from 2009 to 2015: Results from the Study for Monitoring Antimicrobial Resistance Trends (SMART). PLoS ONE 2018, 13, e0198621. [Google Scholar] [CrossRef]
- Breijyeh, Z.; Jubeh, B.; Karaman, R. Resistance of Gram-Negative Bacteria to Current Antibacterial Agents and Approaches to Resolve It. Molecules 2020, 25, 1340. [Google Scholar] [CrossRef] [PubMed]
- Mancuso, G.; Midiri, A.; Gerace, E.; Biondo, C. Bacterial Antibiotic Resistance: The Most Critical Pathogens. Pathogens 2021, 10, 1310. [Google Scholar] [CrossRef]
- Gauba, A.; Rahman, K.M. Evaluation of Antibiotic Resistance Mechanisms in Gram-Negative Bacteria. Antibiotics 2023, 12, 1590. [Google Scholar] [CrossRef]
- Yassin, A.; Huralska, M.; Pogue, J.M.; Dixit, D.; Sawyer, R.G.; Kaye, K.S. State of the Management of Infections Caused by Multidrug-Resistant Gram-Negative Organisms. Clin. Infect. Dis. 2023, 77, e46–e56. [Google Scholar] [CrossRef]
- Bassetti, M.; Peghin, M.; Vena, A.; Giacobbe, D.R. Treatment of Infections Due to MDR Gram-Negative Bacteria. Front. Med. 2019, 6, 74. [Google Scholar] [CrossRef]
- Larcher, R.; Laffont-Lozes, P.; Roger, C.; Doncesco, R.; Groul-Viaud, C.; Martin, A.; Loubet, P.; Lavigne, J.-P.; Pantel, A.; Sotto, A. Last resort beta-lactam antibiotics for treatment of New-Delhi Metallo-Beta-Lactamase producing Enterobacterales and other Difficult-to-Treat Resistance in Gram-negative bacteria: A real-life study. Front. Cell. Infect. Microbiol. 2022, 12, 1048633. [Google Scholar] [CrossRef]
- Browne, A.J.; Chipeta, M.G.; Haines-Woodhouse, G.; Kumaran, E.P.A.; Hamadani, B.H.K.; Zaraa, S.; Henry, N.J.; Deshpande, A.; Reiner, R.C.; Day, N.P.J.; et al. Global antibiotic consumption and usage in humans, 2000–2018: A spatial modelling study. Lancet Planet. Health 2021, 5, e893–e904. [Google Scholar] [CrossRef] [PubMed]
- Kasbi, Y.; Sellami, F.; Ferjani, A.; Abbassi, A.; Ben Boubaker, I.B. Pharmaco-Epidemiological Study and Correlation Between Antibiotic Resistance and Antibiotic Consumption in a Tunisian Teaching Hospital from 2010 to 2022. Antibiotics 2025, 14, 135. [Google Scholar] [CrossRef]
- Sallem, N.; Ben Mansour, N.; Amri, H.; Boudaoura, M.; Gargouri, O.; Mahjoubi, F.; Hammami, A.; Mnif, B.; Chow, S.-K. Extended-spectrum beta-lactamase- and carbapenemase-producing Escherichia coli isolates causing hospital- and community-acquired infections in Tunisia (2001–2019): Expansion of CTX-M-15-C2 and CTX-M-27-C1 ST131 subclades. Microbiol. Spectr. 2024, 12, e0147124. [Google Scholar] [CrossRef]
- Mansour, W. Tunisian antibiotic resistance problems: Three contexts but one health. Afr. Health Sci. 2018, 18, 1202–1203. [Google Scholar] [CrossRef]
- Ben Hassena, A.; Guermazi-Toumi, S.; Amor, M.G.-B.; Saidani, M.; Tlili, S.; Khannous, L.; Gdoura, R.; Siala-Trigui, M. Detection of AmpC and ESBL-producing Enterobacterales isolated from urinary tract infections in Tunisia. Acta Microbiol. Et Immunol. Hung. 2022, 69, 46–55. [Google Scholar] [CrossRef]
- Sola, M.; Mani, Y.; Saras, E.; Drapeau, A.; Grami, R.; Aouni, M.; Madec, J.-Y.; Haenni, M.; Mansour, W. Prevalence and Characterization of Extended-Spectrum β-Lactamase- and Carbapenemase-Producing Enterobacterales from Tunisian Seafood. Microorganisms 2022, 10, 1364. [Google Scholar] [CrossRef] [PubMed]
- Ben Said, L.; Jouini, A.; Klibi, N.; Dziri, R.; Alonso, C.A.; Boudabous, A.; Ben Slama, K.; Torres, C. Detection of extended-spectrum beta-lactamase (ESBL)-producing Enterobacteriaceae in vegetables, soil and water of the farm environment in Tunisia. Int. J. Food Microbiol. 2015, 203, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Hassen, B.; Abbassi, M.S.; Ruiz-Ripa, L.; Mama, O.M.; Hassen, A.; Torres, C.; Hammami, S. High prevalence of mcr-1 encoding colistin resistance and first identification of blaCTX-M-55 in ESBL/CMY-2-producing Escherichia coli isolated from chicken faeces and retail meat in Tunisia. Int. J. Food Microbiol. 2020, 318, 108478. [Google Scholar] [CrossRef]
- Moser, K.A.; Zhang, L.; Spicknall, I.; Braykov, N.P.; Levy, K.; Marrs, C.F.; Foxman, B.; Trueba, G.; Cevallos, W.; Goldstick, J.; et al. The Role of Mobile Genetic Elements in the Spread of Antimicrobial-Resistant Escherichia coli from Chickens to Humans in Small-Scale Production Poultry Operations in Rural Ecuador. Am. J. Epidemiol. 2018, 187, 558–567. [Google Scholar] [CrossRef]
- Partridge, S.R.; Kwong, S.M.; Firth, N.; Jensen, S.O. Mobile genetic elements associated with antimicrobial resistance. Clin. Microbiol. Rev. 2018, 31, e00088-17. [Google Scholar] [CrossRef]
- Dziri, O.; Dziri, R.; El Salabi, A.A.; Chouchani, C. Carbapenemase Producing Gram-Negative Bacteria in Tunisia: History of Thirteen Years of Challenge. Infect. Drug Resist. 2020, 13, 4177–4191. [Google Scholar] [CrossRef]
- Tamma, P.D.; Heil, E.L.; Justo, J.A.; Mathers, A.J.; Satlin, M.J.; Bonomo, R.A. Infectious Diseases Society of America 2024 Guidance on the Treatment of Antimicrobial-Resistant Gram-Negative Infections. Clin. Infect. Dis. 2024, 78, ciae403. [Google Scholar] [CrossRef] [PubMed]
- Résistance Bactérienne. Available online: https://www.infectiologie.org.tn/resistance.php (accessed on 31 May 2025).
- Daoud, N.; Hamdoun, M.; Hannachi, H.; Gharsallah, C.; Mallekh, W.; Bahri, O. Antimicrobial Susceptibility Patterns of Escherichia coli among Tunisian Outpatients with Community-Acquired Urinary Tract Infection (2012–2018). Curr. Urol. 2020, 14, 200–205. [Google Scholar] [CrossRef]
- Guermazi-Toumi, S.; Boujlel, S.; Assoudi, M.; Issaoui, R.; Tlili, S.; Hlaiem, M.E. Susceptibility profiles of bacteria causing urinary tract infections in Southern Tunisia. J. Glob. Antimicrob. Resist. 2018, 12, 48–52. [Google Scholar] [CrossRef]
- Jadoon, R.J.; Jalal-Ud-Din, M.; Khan, S.A.E. Coli Resistance to Ciprofloxacin and Common Associated Factors. J. Coll Physicians Surg Pak. 2015, 25, 824–827. [Google Scholar] [PubMed]
- Yilmaz, N.; Agus, N.; Bayram, A.; Samlioglu, P.; Sirin, M.C.; Derici, Y.K.; Hanci, S.Y. Antimicrobial susceptibilities of Escherichia coli isolates as agents of community-acquired urinary tract infection (2008–2014). Urol. Res. Pr. 2016, 42, 32–36. [Google Scholar] [CrossRef]
- Veeraraghavan, B.; Jesudason, M.R.; Prakasah, J.A.J.; Anandan, S.; Sahni, R.D.; Pragasam, A.K.; Bakthavatchalam, Y.D.; Selvakumar, R.J.; Dhole, T.; Rodrigues, C.; et al. Antimicrobial susceptibility profiles of gram-negative bacteria causing infections collected across India during 2014–2016: Study for monitoring antimicrobial resistance trend report. Indian J. Med Microbiol. 2018, 36, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Ayari, K.; Bourouis, A.; Chihi, H.; Mahrouki, S.; Naas, T.; Belhadj, O. Dissemination and genetic support of broad-spectrum beta-lactam-resistant Escherichia coli strain isolated from two Tunisian hospitals during 2004–2012. Afr. Health Sci. 2017, 17, 346–355. [Google Scholar] [CrossRef]
- Yan, M.; Zheng, B.; Li, Y.; Lv, Y. Antimicrobial Susceptibility Trends Among Gram-Negative Bacilli Causing Bloodstream Infections: Results from the China Antimicrobial Resistance Surveillance Trial (CARST) Program, 2011–2020. Infect. Drug Resist. 2022, 15, 2325–2337. [Google Scholar] [CrossRef]
- Lin, W.-P.; Wang, J.-T.; Chang, S.-C.; Chang, F.-Y.; Fung, C.-P.; Chuang, Y.-C.; Chen, Y.-S.; Shiau, Y.-R.; Tan, M.-C.; Wang, H.-Y.; et al. The Antimicrobial Susceptibility of Klebsiella pneumoniae from Community Settings in Taiwan, a Trend Analysis. Sci. Rep. 2016, 6, 36280. [Google Scholar] [CrossRef]
- Bouchillon, S.K.; Badal, R.E.; Hoban, D.J.; Hawser, S.P. Antimicrobial susceptibility of inpatient urinary tract isolates of gram-negative bacilli in the United States: Results from the study for monitoring antimicrobial resistance trends (SMART) program: 2009–2011. Clin. Ther. 2013, 35, 872–877. [Google Scholar] [CrossRef]
- Mansour, W.; Haenni, M.; Saras, E.; Grami, R.; Mani, Y.; Khalifa, A.B.H.; Atrouss, S.E.; Kheder, M.; Hassen, M.F.; Boujâafar, N.; et al. Outbreak of colistin-resistant carbapenemase-producing Klebsiella pneumoniae in Tunisia. J. Glob. Antimicrob. Resist. 2017, 10, 88–94. [Google Scholar] [CrossRef]
- Monography-Ceftazidime Avibactam-Stabilis 4.0. Available online: https://www.stabilis.org/Monographie.php?IdMolecule=997 (accessed on 17 June 2025).
- Megdiche, Z.; Lamloumi, M.; Maamar, B.; Dhraief, S.; Messadi, A.A.; Thabet, L. In vitro activity of ceftazidime- avibactam and ceftolozane- tazobactam against clinical isolates of Enterobacteriaceae and Pseudomonas æruginosa: Results from a trauma center and burn unit in Tunisia. Ann Burn. Fire Disasters 2025, 38, 31–37. [Google Scholar]
- Fethi, M.; Rojo-Bezares, B.; Arfaoui, A.; Dziri, R.; Chichón, G.; Barguellil, F.; López, M.; El Asli, M.S.; Toledano, P.; Ouzari, H.-I.; et al. High Prevalence of GES-5 Variant and Co-Expression of VIM-2 and GES-45 among Clinical Pseudomonas aeruginosa Strains in Tunisia. Antibiotics 2023, 12, 1394. [Google Scholar] [CrossRef]
- Abdallah, H.B.; Noomen, S.; Khélifa, A.B.E.; Sahnoun, O.; Elargoubi, A.; Mastouri, M. Susceptibility patterns of Pseudomonas aeruginosa strains isolated in the Monastir region, Tunisia. Med. Et Mal. Infect. 2008, 38, 554–556. [Google Scholar] [CrossRef] [PubMed]
- Ferjani, S.; Maamar, E.; Ferjani, A.; Kanzari, L.; Ben Boubaker, I.B. Evaluation of Three Carbapenemase-Phenotypic Detection Methods and Emergence of Diverse VIM and GES Variants among Pseudomonas aeruginosa Isolates in Tunisia. Antibiotics 2022, 11, 858. [Google Scholar] [CrossRef]
- Sastre-Femenia, M.À.; Fernández-Muñoz, A.; Gomis-Font, M.A.; Taltavull, B.; López-Causapé, C.; Arca-Suárez, J.; Martínez-Martínez, L.; Cantón, R.; Larrosa, N.; Oteo-Iglesias, J.; et al. Pseudomonas aeruginosa antibiotic susceptibility profiles, genomic epidemiology and resistance mechanisms: A nation-wide five-year time lapse analysis. Lancet Reg. Health-Eur. 2023, 34, 100736. [Google Scholar] [CrossRef] [PubMed]
- Nadia, J.; Wejdene, M.; Bonnin, R.A.; Meriam, G.; Cherifa, C.; Rachida, G.; Nesrine, K.; Noureddine, B.; Olfa, B.; Thierry, N. Temporal Variation in Antibiotic Resistance of Acinetobacter baumannii in a Teaching Hospital in Tunisia: Correlation with Antimicrobial Consumption. Open Microbiol. J. 2019, 13, 106–111. [Google Scholar] [CrossRef]
- Ferjani, S.; Kanzari, L.; Maamar, E.; Hamzaoui, Z.; Rehaiem, A.; Ferjani, A.; Boubaker, I.B.-B. Extensively drug-resistant Acinetobacter baumannii co-producing VIM-2 and OXA-23 in intensive care units: Results of a one-day point prevalence in a Tunisian hospital. Infect. Dis. Now 2022, 52, 426–431. [Google Scholar] [CrossRef]
- Tunisia in Figures 2022. Institut National de Statistiques/Publications|INS. Available online: https://www.ins.tn/publication (accessed on 29 May 2025).
- Eucast: Clinical Breakpoints and Dosing of Antibiotics. Available online: http://www.eucast.org/clinical_breakpoints (accessed on 1 January 2020).
| Pathogen | Total (n) | Urine | Pulmonary | Punctures | Blood Cultures | Pus | Other * |
|---|---|---|---|---|---|---|---|
| E. coli | 125,552 | 107,088 | - | 1735 | 4010 | 7680 | 5039 |
| K. pneumoniae | 47,062 | 27,690 | 4040 | 766 | 6450 | 6202 | 1914 |
| P. aeruginosa | 30,681 | 6328 | 8565 | 1041 | 1913 | 9361 | 3473 |
| A. baumannii | 10,139 | 1630 | 4204 | 207 | 1745 | 1262 | 1091 |
| Total | 213,434 | 142,736 | 16,809 | 3749 | 14,118 | 24,505 | 11,517 |
| Pathogen | K. pneumoniae (n = 47,062) | E. coli (n= 125,552) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Resistance | Overall (1999–2019) | Urine (2004–2019) n = 27,690 | Blood Culture (2004–2019) n = 6450 | Overall (1999–2019) | Urine 1999–2019 n = 107,088 | Blood Culture (2004–2019) n = 4010 | ||||||
| n | (%R) | n | (%R) | n | (%R) | n | (%R) | n | (%R) | n | (%R) | |
| AMC | 12,934 | (27%) | 5917 | (25%) | 2165 | (39%) | 23,813 | (19%) | 20,144 | (19%) | 547 | (21%) |
| PTZ | 1911 | (4%) | - | - | 329 | (6%) | 1135 | (1%) | 917 | (1%) | 49 | (2%) |
| FOX | 6295 | (13%) | 3014 | (13%) | 1092 | (20%) | 2350 | (2%) | 1664 | (2%) | 159 | (6%) |
| CTX | 18,773 | (40%) | 8268 | (35%) | 3353 | (60%) | 13,598 | (11%) | 11,269 | (11%) | 613 | (24%) |
| CAZ | 18,330 | (39%) | 8044 | (34%) | 3230 | (58%) | 11,602 | (9%) | 9647 | (9%) | 522 | (20%) |
| IMP | 2353 | (5%) | 750 | (3%) | 610 | (11%) | 86 | (0%) | 35 | (0%) | 10 | (0%) |
| ERT | 7530 | (16%) | 1806 | (11%) | 936 | (25%) | 291 | (0%) | 200 | (0%) | 22 | (1%) |
| GEN | 16,808 | (36%) | 6921 | (29%) | 2935 | (53%) | 13,224 | (11%) | 10,843 | (10%) | 478 | (18%) |
| AMK | 4948 | (11%) | 1929 | (8%) | 933 | (17%) | 1766 | (1%) | 1413 | (1%) | 78 | (3%) |
| NAL | 14,564 | (31%) | 7590 | (32%) | 2009 | (36%) | 30,085 | (24%) | 25,119 | (23%) | 824 | (32%) |
| CIP | 14,577 | (31%) | 7753 | (33%) | 2049 | (37%) | 23,572 | (19%) | 19,915 | (19%) | 670 | (26%) |
| SXT | 20,142 | (43%) | 19,295 | 41% | 18,824 | 44% | 52,731 | (42%) | 51,476 | 41% | 62,776 | 50% |
| Pathogen | P. aeruginosa (n = 30,681) | A. baumannii (n= 10,139) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Resistance | Overall (1999–2019) | Pulmonary Samples (2004–2019) n = 8056 | Blood Culture (2004–2019) n = 1858 | Overall (1999–2019) | Pulmonary Samples (2008–2019) n = 4204 | Blood Culture (2008–2019) n = 1745 | ||||||
| n | (%R) | n | (%R) | n | (%R) | n | (%R) | n | (%R) | n | (%R) | |
| PTZ | 2666 | (9%) | 1039 | (14%) | 280 | (18%) | 5413 | (53%) | 2423 | (58%) | 848 | (49%) |
| CAZ | 4868 | (16%) | 1319 | (18%) | 318 | (20%) | 8245 | (81%) | 3652 | (87%) | 1382 | (79%) |
| FEP | 2079 | (7%) | 1010 | (14%) | 187 | (12%) | 5443 | (54%) | 2403 | (57%) | 896 | (51%) |
| IMP | 5798 | (19%) | 1745 | (23%) | 394 | (25%) | 7117 | (70%) | 3233 | (77%) | 1176 | (67%) |
| MEM | 698 | (2%) | 269 | (4%) | 48 | (3%) | - | - | - | - | - | - |
| GEN | 7615 | (25%) | 1554 | (21%) | 340 | (22%) | 7576 | (75%) | 3241 | (77%) | 1217 | (70%) |
| AMK | 4459 | (15%) | 1013 | (14%) | 263 | (17%) | 7049 | (70%) | 3171 | (75%) | 1117 | (64%) |
| CIP | 6916 | (23%) | 1750 | (23%) | 320 | (20%) | 8320 | (82%) | 3688 | (88%) | 1374 | (79%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kanzari, L.; Ferjani, S.; Mnif, B.; Mahjoubi, F.; Zribi, M.; Meftah, K.; Ferjani, A.; Mhiri, E.; Ben Lamine, Y.; Kadri, Y.; et al. Historical Overview of the Evolution of Multidrug-Resistant Gram-Negative Infections in Tunisia from 1999 to 2019. Antibiotics 2025, 14, 657. https://doi.org/10.3390/antibiotics14070657
Kanzari L, Ferjani S, Mnif B, Mahjoubi F, Zribi M, Meftah K, Ferjani A, Mhiri E, Ben Lamine Y, Kadri Y, et al. Historical Overview of the Evolution of Multidrug-Resistant Gram-Negative Infections in Tunisia from 1999 to 2019. Antibiotics. 2025; 14(7):657. https://doi.org/10.3390/antibiotics14070657
Chicago/Turabian StyleKanzari, Lamia, Sana Ferjani, Basma Mnif, Faouzia Mahjoubi, Mariem Zribi, Khaoula Meftah, Asma Ferjani, Emna Mhiri, Yomna Ben Lamine, Yosr Kadri, and et al. 2025. "Historical Overview of the Evolution of Multidrug-Resistant Gram-Negative Infections in Tunisia from 1999 to 2019" Antibiotics 14, no. 7: 657. https://doi.org/10.3390/antibiotics14070657
APA StyleKanzari, L., Ferjani, S., Mnif, B., Mahjoubi, F., Zribi, M., Meftah, K., Ferjani, A., Mhiri, E., Ben Lamine, Y., Kadri, Y., Naija, H., Hamdoun, M., Chebbi, Y., Dhraief, S., Mohamed, N., Zaghden, H., Thabet, L., Achour, W., Bahri, O., ... Boutiba-Ben Boubaker, I. (2025). Historical Overview of the Evolution of Multidrug-Resistant Gram-Negative Infections in Tunisia from 1999 to 2019. Antibiotics, 14(7), 657. https://doi.org/10.3390/antibiotics14070657






