Country-Specific Approaches to Preventing Infections in Cataract Surgery
Abstract
1. Introduction
2. Results
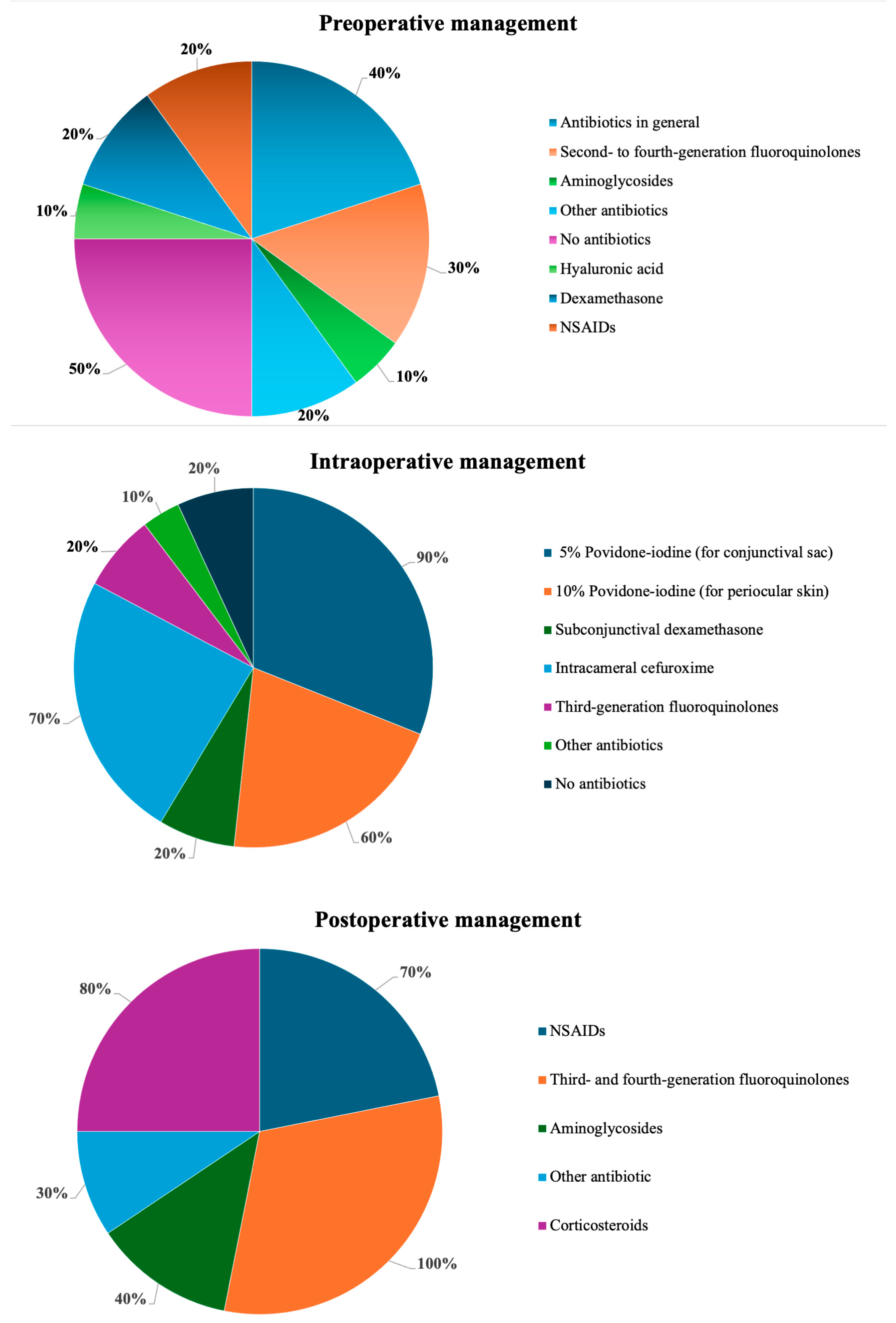
2.1. Preoperative Management
2.2. Intraoperative Management
2.3. Postoperative Management
3. Discussion
Limitations
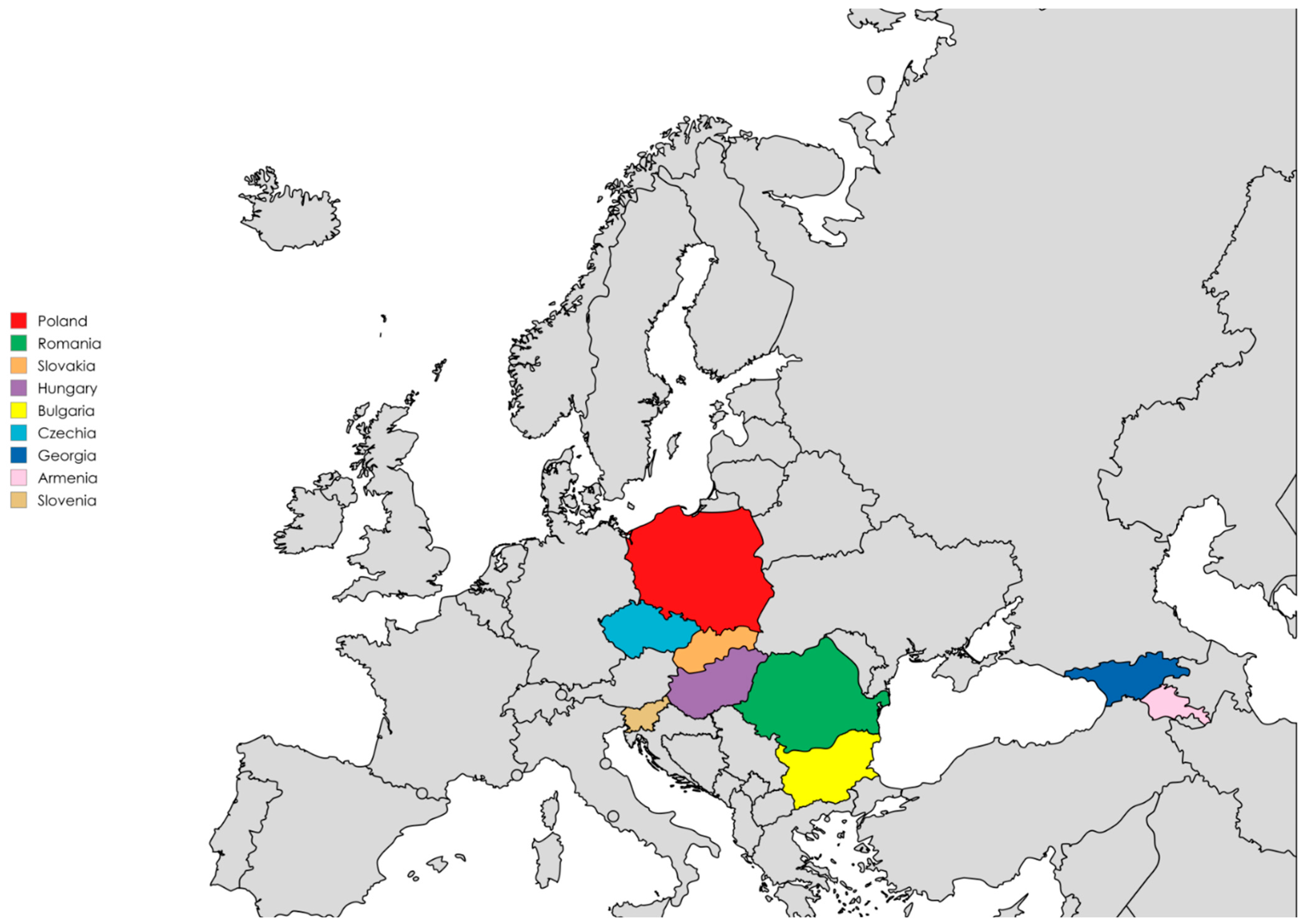
4. Materials and Methods
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AMR | antimicrobial resistance |
| ESCRS | European Society of Cataract and Refractive Surgeons |
| FDC | Fixed-dose combination |
| MRSA | methicillin-resistant S. aureus |
| MRSE | methicillin-resistant S. epidermidis |
| NICE | National Institute for Health and Care Excellence |
| NSAIDs | non-steroidal anti-inflammatory drugs |
References
- Murray, C.J.L.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Robles Aguilar, G.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E.; et al. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef] [PubMed]
- GBD 2021 Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance 1990–2021: A systematic analysis with forecasts to 2050. Lancet 2024, 404, 1199–1226. [Google Scholar] [CrossRef] [PubMed]
- Moshirfar, M.; Milner, D.; Patel, B.C. Cataract Surgery; StatPearls: St. Petersburg, FL, USA, 2025. [Google Scholar]
- Hashemi, H.; Fayaz, F.; Hashemi, A.; Khabazkhoob, M. Global prevalence of cataract surgery. Curr. Opin. Ophthalmol. 2025, 36, 10–17. [Google Scholar] [CrossRef]
- Lin, L.; Liang, Y.; Jiang, G.; Gan, Q.; Yang, T.; Liao, P.; Liang, H. Global, regional, and national burden of cataract: A comprehensive analysis and projections from 1990 to 2021. PLoS ONE 2025, 20, e0326263. [Google Scholar] [CrossRef]
- Ciulla, T.A.; Starr, M.B.; Masket, S. Bacterial endophthalmitis prophylaxis for cataract surgery: An evidence-based update. Ophthalmology 2002, 109, 13–24. [Google Scholar] [CrossRef] [PubMed]
- Speaker, M.G.; Milch, F.A.; Shah, M.K.; Eisner, W.; Kreiswirth, B.N. Role of external bacterial flora in the pathogenesis of acute postoperative endophthalmitis. Ophthalmology 1991, 98, 639–649. [Google Scholar] [CrossRef]
- Gunalda, J.; Williams, D.; Koyfman, A.; Long, B. High risk and low prevalence diseases: Endophthalmitis. Am. J. Emerg. Med. 2023, 71, 144–149. [Google Scholar] [CrossRef]
- Ting, M.Y.L.; Pocobelli, G.; Butu, D.M.; Mandal, N.; Nicholson, L.; Khan, S.R. Incidence and outcomes of post-operative endophthalmitis following elective phacoemulsification cataract surgery, between 2015 and 2022. Eye 2024, 38, 3429–3433. [Google Scholar] [CrossRef]
- Ferrara, M.; Gatti, F.; Lockington, D.; Iaria, A.; Kaye, S.; Virgili, G.; Aragona, P.; Semeraro, F.; Romano, V. Antimicrobials and antiseptics: Lowering effect on ocular surface bacterial flora—A systematic review. Acta Ophthalmol. 2024, 102, e215–e228. [Google Scholar] [CrossRef]
- Szaflik, J.P.; Bakunowicz-Łazarczyk, A.; Dobrowolski, D.; Grabska-Liberek, I.; Kałużny, B.; Kałużny, J.; Lubiński, W.; Mackiewicz, J.; Michalska-Małecka, K.; Misiuk-Hojło, M.; et al. Guidelines for perioperative care in cataract surgery in Poland. Klin. Ocz. Acta Ophthalmol. Pol. 2024, 126, 115–118. [Google Scholar] [CrossRef]
- Mather, R.; Karenchak, L.M.; Romanowski, E.G.; Kowalski, R.P. Fourth generation fluoroquinolones: New weapons in the arsenal of ophthalmic antibiotics. Am. J. Ophthalmol. 2002, 133, 463–466. [Google Scholar] [CrossRef]
- Tan, C.S.H.; Wong, H.K.; Yang, F.P. Epidemiology of postoperative endophthalmitis in an Asian population: 11-year incidence and effect of intracameral antibiotic agents. J. Cataract. Refract. Surg. 2012, 38, 425–430. [Google Scholar] [CrossRef]
- Orfeo, V.; Aragona, P.; Alessio, G.; Drago, L.; Mastropasqua, L.; Rossi, S.; Vinciguerra, P.; Ciprandi, G.; Tognetto, D. Expert consensus on the management of patients undergoing cataract surgery: A Delphi study. Eur. J. Ophthalmol. 2024, 34, 747–753. [Google Scholar] [CrossRef]
- Izdebska, J.; Wróblewska, M.; Piechal, A.; Misiuk-Hojło, M. Infections prophylaxis after cataract surgery: Fluroquinolones and anti-inflammatory drugs ? alone or in combined medications? Ophthatherapy 2023, 10, 135–141. [Google Scholar] [CrossRef]
- Garcia O’Farrill, N.; Abi Karam, M.; Villegas, V.M.; Flynn, H.W., Jr.; Grzybowski, A.; Schwartz, S.G. New Approaches to Overcoming Antimicrobial Resistance in Endophthalmitis. Pharmaceuticals 2024, 17, 321. [Google Scholar] [CrossRef]
- Barry, P.; Cordoves, L.; Gardner, A. ESCRS Guidelines for Prevention and Treatment of Endophthalmitis Following Cataract Surgery: Data, Dilemmas and Conclusions; European Society of Cataract and Refractive Surgeons: London, UK, 2013. [Google Scholar]
- European Society of Cataract and Refractive Surgeons (ESCRS) Guideline for Cataract Surgery (Draft Version). Available online: https://www.escrs.org/escrs-guideline-for-cataract-surgery/ (accessed on 28 April 2025).
- Institute for Health Metrics and Evaluation (IHME). Antimicrobial Resistance Collaborators: Global Burden of Bacterial AMR 1990–2021; IHME: Seattle, WA, USA, 2023; Available online: https://www.healthdata.org/sites/default/files/2023-09/Armenia.pdf (accessed on 22 July 2025).
- World Health Organization (WHO). Antimicrobial Resistance TrACSS Armenia 2022 Country Profile. Available online: https://www.who.int/publications/m/item/Antimicrobial-resistance-tracss-arm-2022-country-profile (accessed on 24 July 2025).
- World Health Organization (WHO). Antimicrobial Resistance TrACSS Georgia 2021 Country Profile. Available online: https://www.who.int/publications/m/item/antimicrobial-resistance-tracss-geo-2021-country-profile (accessed on 20 July 2025).
- Kessel, L.; Flesner, P.; Andresen, J.; Erngaard, D.; Tendal, B.; Hjortdal, J. Antibiotic prevention of postcataract endophthalmitis: A systematic review and meta-analysis. Acta Ophthalmol. 2015, 93, 303–317. [Google Scholar] [CrossRef]
- Bowen, R.C.; Zhou, A.X.; Bondalapati, S.; Lawyer, T.W.; Snow, K.B.; Evans, P.R.; Bardsley, T.; McFarland, M.; Kliethermes, M.; Shi, D.; et al. Comparative analysis of the safety and efficacy of intracameral cefuroxime, moxifloxacin and vancomycin at the end of cataract surgery: A meta-analysis. Br. J. Ophthalmol. 2018, 102, 1268–1276. [Google Scholar] [CrossRef]
- Kato, A.; Horita, N.; Namkoong, H.; Nomura, E.; Masuhara, N.; Kaneko, T.; Mizuki, N.; Takeuchi, M. Prophylactic antibiotics for postcataract surgery endophthalmitis: A systematic review and network meta-analysis of 6.8 million eyes. Sci. Rep. 2022, 12, 17416. [Google Scholar] [CrossRef] [PubMed]
- Felfeli, T.; Miranda, R.N.; Kaur, J.; Chan, C.C.; Naimark, D.M.J. Cost-Effectiveness of Preoperative Topical Antibiotic Prophylaxis for Endophthalmitis Following Cataract Surgery. Am. J. Ophthalmol. 2023, 247, 152–160. [Google Scholar] [CrossRef] [PubMed]
- Aprokam. Summary of Product Characteristics. 2019. Available online: https://www.medicines.org.uk/emc/product/2963/smpc (accessed on 20 July 2025).
- Omole, A.; Awosika, A.; Patel, P. Cefuroxime. In StatPearls; StatPearls: Treasure Island, FL, USA, 2025. [Google Scholar]
- Barry, P.; Seal, D.; Gettinby, G.; Lees, F.; Peterson, M.; Revie, C. Prophylaxis of postoperative endophthalmitis following cataract surgery: Results of the ESCRS multicenter study and identification of risk factors. J. Cataract. Refract. Surg. 2007, 33, 978–988. [Google Scholar] [CrossRef] [PubMed]
- de Sousa Casavechia, L.N.; Meireles, A.C.; Schapira, E.; Fernandes, R.A.B.; Fernandes, A.G. The impact of antibiotic prophylaxis with intracameral cefuroxime on postoperative infectious endophthalmitis rates in a high-volume cataract surgery center. Sci. Rep. 2023, 13, 18031. [Google Scholar] [CrossRef]
- Rathi, V.M.; Sharma, S.; Das, T.; Khanna, R.C. Endophthalmitis Prophylaxis Study, Report 2: Intracameral antibiotic prophylaxis with or without postoperative topical antibiotic in cataract surgery. Indian J. Ophthalmol. 2020, 68, 2451–2455. [Google Scholar] [CrossRef]
- Chen, S.P.; Woreta, F.; Chang, D.F. Cataracts: A Review. JAMA 2025, 333, 2093–2103. [Google Scholar] [CrossRef]
- Aragona, P.; Postorino, E.I.; Aragona, E. Post-surgical management of cataract: Light and dark in the 2020s. Eur. J. Ophthalmol. 2021, 31, 287–290. [Google Scholar] [CrossRef]
- Witkin, A.J.; Chang, D.F.; Jumper, J.M.; Charles, S.; Eliott, D.; Hoffman, R.S.; Mamalis, N.; Miller, K.M.; Wykoff, C.C. Vancomycin-Associated Hemorrhagic Occlusive Retinal Vasculitis: Clinical Characteristics of 36 Eyes. Ophthalmology 2017, 124, 583–595. [Google Scholar] [CrossRef]
- Clinical Alert: HORV Association with Intraocular Vancomycin. Available online: https://ascrs.org/-/media/files/clinical-committee-reports/clinical-alert-horv-association-with-intraocular-vancomycin.pdf (accessed on 12 August 2025).
- Friling, E.; Bro, T.; Lundström, M.; Montan, P. Endophthalmitis after cataract surgery and effect of different intracameral antibiotic regimes in Sweden 2011-2017: National registry study. J. Cataract. Refract. Surg. 2024, 50, 828–835. [Google Scholar] [CrossRef] [PubMed]
- Samudio, M.; Abente, S.; Fariña, N.; López, Y.; Duré, C.; Laspina, F.; Guillén, R.; Salinas, C.; Castillo, V.; Palacios, J.; et al. Analysis of antibiotic resistance and genetic profile of conjunctival bacteria flora before and after cataract surgery. Int. Ophthalmol. 2023, 43, 519–530. [Google Scholar] [CrossRef]
- NICE. Cataracts in Adults: Management; National Institute for Health and Care Excellence: London, UK, 2017. [Google Scholar]
- Grzybowski, A.; Kupidura-Majewski, K. The role of topical antibiotics in perioperative endophthalmitis prevention in cataract surgery. Ophthatherapy 2019, 6, 147–151. [Google Scholar] [CrossRef]
- Grzybowski, A.; Kanclerz, P.; Myers, W.G. The use of povidone-iodine in ophthalmology. Curr. Opin. Ophthalmol. 2018, 29, 19–32. [Google Scholar] [CrossRef]
- Lepelletier, D.; Maillard, J.Y.; Pozzetto, B.; Simon, A. Povidone Iodine: Properties, Mechanisms of Action, and Role in Infection Control and Staphylococcus aureus Decolonization. Antimicrob. Agents Chemother. 2020, 64, 10–1128. [Google Scholar] [CrossRef]
- Hamad, C.D.; Sheppard, W.L.; Chun, R.F.; Mamouei, Z.; Lloyd, T.S.; Li, A.K.; Sobti, R.; Pearce, J.W.; Hernandez, A.; Dipane, M.V.; et al. Comparing the in Vitro Efficacy of Commonly Used Surgical Irrigants for the Treatment of Implant-Associated Infections. J. Bone Jt. Surg. Am. 2025, 107, 1818–1824. [Google Scholar] [CrossRef]
- Majalekar, P.P.; Shirote, P.J. Fluoroquinolones: Blessings Or Curses. Curr. Drug Targets 2020, 21, 1354–1370. [Google Scholar] [CrossRef]
- Khoo, P.; McCluskey, P.; Cabrera-Aguas, M.; Watson, S.L. Bacterial eye infections. In Encyclopedia of Infezction and Immunity; Rezaei, N., Ed.; Elsevier: Amsterdam, The Netherlands, 2022; pp. 204–218. [Google Scholar]
- Cabrera-Aguas, M.; Chidi-Egboka, N.; Kandel, H.; Watson, S.L. Antimicrobial resistance in ocular infection: A review. Clin. Exp. Ophthalmol. 2024, 52, 258–275. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, S.; Agrawal, D.; Gomase, S.N.; Parchand, S.M.; Gangwe, A.B.; Mishra, M. Fluoroquinolone resistance in bacterial isolates from ocular infections: Trend in antibiotic susceptibility patterns between 2005–2020. Indian J. Ophthalmol. 2022, 70, 4391–4398. [Google Scholar] [CrossRef]
- Drago, L. Topical Antibiotic Therapy in the Ocular Environment: The Benefits of Using Moxifloxacin Eyedrops. Microorganisms 2024, 12, 649. [Google Scholar] [CrossRef]
- Fernández-Rubio, E.; Urcelay, J.L.; Cuesta-Rodriguez, T. The antibiotic resistance pattern of conjunctival bacteria: A key for designing a cataract surgery prophylaxis. Eye 2009, 23, 1321–1328. [Google Scholar] [CrossRef]
- Hsu, H.Y.; Lind, J.T.; Tseng, L.; Miller, D. Ocular flora and their antibiotic resistance patterns in the midwest: A prospective study of patients undergoing cataract surgery. Am. J. Ophthalmol. 2013, 155, 36–44.e32. [Google Scholar] [CrossRef] [PubMed]
- Tabatabaei, S.A.; Masoumi, A.; Mirzaei, A.; Mirshahi, R.; Momenaei, B.; Bijani, F.M.; Rashidinia, A.; Nazari, M.; Ahadifard, M.; Mahdizad, Z.; et al. Infectious Endophthalmitis: An Overview of Clinical Features, Microbiology Profile, and Antibiotic Sensitivity Pattern. J. Curr. Ophthalmol. 2024, 36, 284–290. [Google Scholar] [CrossRef]
- Shi, Q.; Mao, D.; Zhang, Z.; Qudsi, A.I.; Wei, M.; Cheng, Z.; Zhang, Y.; Wang, Z.; Chen, K.; Xu, X.; et al. Epidemiological and Antimicrobial Resistance Trends in Bacterial Keratitis: A Hospital-Based 10-Year Study (2014–2024). Microorganisms 2025, 13, 670. [Google Scholar] [CrossRef]
- Norrby, S.R. Levofloxacin. Expert. Opin. Pharmacother. 1999, 1, 109–119. [Google Scholar] [CrossRef]
- Schwab, I.R.; Friedlaender, M.; McCulley, J.; Lichtenstein, S.J.; Moran, C.T. A phase III clinical trial of 0.5% levofloxacin ophthalmic solution versus 0.3% ofloxacin ophthalmic solution for the treatment of bacterial conjunctivitis. Ophthalmology 2003, 110, 457–465. [Google Scholar] [CrossRef]
- Kim, S.J.; Flach, A.J.; Jampol, L.M. Nonsteroidal anti-inflammatory drugs in ophthalmology. Surv. Ophthalmol. 2010, 55, 108–133. [Google Scholar] [CrossRef]
- Wittpenn, J.R.; Silverstein, S.; Heier, J.; Kenyon, K.R.; Hunkeler, J.D.; Earl, M. A randomized, masked comparison of topical ketorolac 0.4% plus steroid vs steroid alone in low-risk cataract surgery patients. Am. J. Ophthalmol. 2008, 146, 554–560. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Schoenberger, S.D.; Thorne, J.E.; Ehlers, J.P.; Yeh, S.; Bakri, S.J. Topical Nonsteroidal Anti-inflammatory Drugs and Cataract Surgery: A Report by the American Academy of Ophthalmology. Ophthalmology 2015, 122, 2159–2168. [Google Scholar] [CrossRef]
- Yang, C.; Yang, J.; Lu, A.; Gong, J.; Yang, Y.; Lin, X.; Li, M.; Xu, H. Nanoparticles in ocular applications and their potential toxicity. Front. Mol. Biosci. 2022, 9, 931759. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Santonja, J.J.; Güell, J.L.; Gris, O.; Vázquez Dorrego, X.M.; Pellicer, E.; Benítez-Del-Castillo, J.M. Liposomal Ozonated Oil in Ocular Infections: A Review of Preclinical and Clinical Studies, Focusing on Its Antiseptic and Regenerative Properties. Clin. Ophthalmol. 2022, 16, 1953–1962. [Google Scholar] [CrossRef]
- Cao, Y.; Samy, K.E.; Bernards, D.A.; Desai, T.A. Recent advances in intraocular sustained-release drug delivery devices. Drug Discov. Today 2019, 24, 1694–1700. [Google Scholar] [CrossRef]
- WHO. Global Action Plan on Antimicrobial Resistance. Available online: https://iris.who.int/server/api/core/bitstreams/1a487887-e162-46a0-8aef-802907c66070/content (accessed on 18 October 2025).
- McEwen, S.A.; Collignon, P.J. Antimicrobial Resistance: A One Health Perspective. Microbiol. Spectr. 2018, 6, 521–547. [Google Scholar] [CrossRef] [PubMed]
- Kuzman, T.; Gabric, I.; Meter, A.; Skegro, I.; Masnec, S.; Kalauz, M.; Pupic-Bakrac, A. Clinical Experience of Using a Combination of Dexamethasone and Levofloxacin After Cataract Surgery. Med. Arch. 2024, 78, 127–130. [Google Scholar] [CrossRef]
- Bandello, F.; Coassin, M.; Di Zazzo, A.; Rizzo, S.; Biagini, I.; Pozdeyeva, N.; Sinitsyn, M.; Verzin, A.; De Rosa, P.; Calabrò, F.; et al. One week of levofloxacin plus dexamethasone eye drops for cataract surgery: An innovative and rational therapeutic strategy. Eye 2020, 34, 2112–2122. [Google Scholar] [CrossRef]
- Phung, T.L.; Ngo, N.T.; Pham, T.T.; Nguyen, H.T.; Duong, K.N.; Dang, M.T.N.; Alcusky, M.J.; Amante, D.J.; Nguyen, H.L. Economic evaluation of fixed-dose drug combinations: A systematic review. J. Appl. Pharm. Sci. 2024, 14, 001–026. [Google Scholar] [CrossRef]
- World Health Organization. Global Guidelines for the Prevention of Surgical Site Infection; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- American Academy of Ophtalmology. Cataract in the Adult Eye Preferred Practice Pattern; American Academy of Ophthalmology: Francisco, CA, USA, 2021. [Google Scholar]
- WHO. Global Antimicrobial Resistance and Use Surveillance System (GLASS) Report: 2022 Global Antimicrobial Resistance and Use Surveillance System (GLASS). Available online: https://www.who.int/publications/i/item/9789240062702 (accessed on 17 October 2025).
- Shariati, A.; Arshadi, M.; Khosrojerdi, M.A.; Abedinzadeh, M.; Ganjalishahi, M.; Maleki, A.; Heidary, M.; Khoshnood, S. The resistance mechanisms of bacteria against ciprofloxacin and new approaches for enhancing the efficacy of this antibiotic. Front. Public Health 2022, 10, 1025633. [Google Scholar] [CrossRef] [PubMed]
- Aramă, V. Topical antibiotic therapy in eye infections—Myths and certainties in the era of bacterial resistance to antibiotics. Rom. J. Ophthalmol. 2020, 64, 245–260. [Google Scholar] [CrossRef]
- Ghita, A.M.; Iliescu, D.A.; Ghita, A.C.; Ilie, L.A. Susceptibility of Ocular Surface Bacteria to Various Antibiotic Agents in a Romanian Ophthalmology Clinic. Diagnostics 2023, 13, 3409. [Google Scholar] [CrossRef]
- Kümmerer, K. Antibiotics in the aquatic environment—A review—Part I. Chemosphere 2009, 75, 417–434. [Google Scholar] [CrossRef] [PubMed]
- Bengtsson-Palme, J.; Kristiansson, E.; Larsson, D.G.J. Environmental factors influencing the development and spread of antibiotic resistance. FEMS Microbiol. Rev. 2018, 42, fux053. [Google Scholar] [CrossRef]
- Rizzo, L.; Manaia, C.; Merlin, C.; Schwartz, T.; Dagot, C.; Ploy, M.C.; Michael, I.; Fatta-Kassinos, D. Urban wastewater treatment plants as hotspots for antibiotic resistant bacteria and genes spread into the environment: A review. Sci. Total Environ. 2013, 447, 345–360. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Toro, M.D.; Popa-Cherecheanu, A.; Majtanova, N.; Rusňák, Š.; Labauri, N.; Pfiefer, V.; Dakov, N.; Németh, G.; Nanyan, V.; Korona-Głowniak, I.; et al. Country-Specific Approaches to Preventing Infections in Cataract Surgery. Antibiotics 2025, 14, 1192. https://doi.org/10.3390/antibiotics14121192
Toro MD, Popa-Cherecheanu A, Majtanova N, Rusňák Š, Labauri N, Pfiefer V, Dakov N, Németh G, Nanyan V, Korona-Głowniak I, et al. Country-Specific Approaches to Preventing Infections in Cataract Surgery. Antibiotics. 2025; 14(12):1192. https://doi.org/10.3390/antibiotics14121192
Chicago/Turabian StyleToro, Mario Damiano, Alina Popa-Cherecheanu, Nora Majtanova, Štěpán Rusňák, Nikoloz Labauri, Vladimir Pfiefer, Nikolai Dakov, Gábor Németh, Vahe Nanyan, Izabela Korona-Głowniak, and et al. 2025. "Country-Specific Approaches to Preventing Infections in Cataract Surgery" Antibiotics 14, no. 12: 1192. https://doi.org/10.3390/antibiotics14121192
APA StyleToro, M. D., Popa-Cherecheanu, A., Majtanova, N., Rusňák, Š., Labauri, N., Pfiefer, V., Dakov, N., Németh, G., Nanyan, V., Korona-Głowniak, I., & Rejdak, R. (2025). Country-Specific Approaches to Preventing Infections in Cataract Surgery. Antibiotics, 14(12), 1192. https://doi.org/10.3390/antibiotics14121192








