The Impact of a Structured Outpatient Parenteral Antimicrobial Therapy (OPAT) Programme on Quality of Care, Optimisation of Antimicrobial Use, and Healthcare Costs: A Retrospective Cohort Study
Abstract
1. Introduction
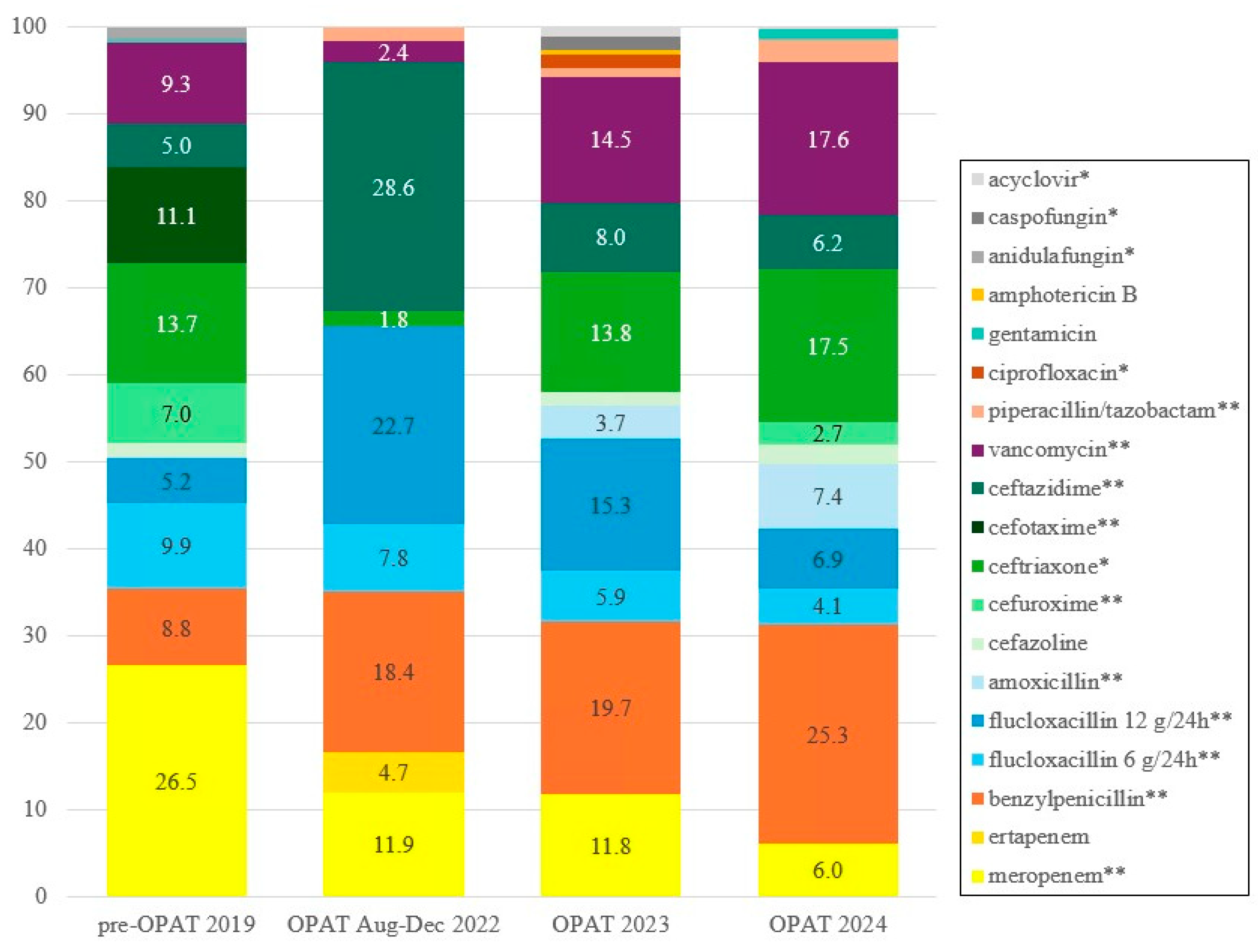
2. Results
2.1. Patient Characteristics
2.2. Patient Outcomes
2.3. The Impact of the ID Specialist Assessment
2.4. Costs
3. Discussion
4. Materials and Methods
4.1. Study Design
4.2. OPAT Programme Procedure
4.3. Study Population
4.4. Data Collection
4.5. Variables
- Clinical response: Assessed by the study team based on documentation of treating physicians when antimicrobial therapy was completed, categorized into four groups: good (no residual symptoms/negative culture), reasonable (minor symptoms requiring no additional treatment), poor (severe symptoms/readmission), or deceased.
- Recurrence: Reinfection with the same microorganism within 3 months of therapy completion.
- Complications: Included both adverse drug reactions and catheter-associated complications (infection and thrombosis). Categorized as mild, severe (hospitalization, discontinuation of therapy, or death) or none.
- Readmission: Unplanned admission during or ≤3 months after completing antimicrobial therapy.
- Timely PICC removal: Within 3 days of IV completion, or not placed, or needed for other medical treatments.
4.6. Evaluation of ID Specialist Assessment
4.7. Cost Analysis
4.8. Statistical Analyses
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CI | Confidence Intervals |
| EHR | Electronic Health Record |
| ID | Infectious Disease |
| IQR | Interquartile Ranges |
| IV | Intravenous |
| MDRO’s | Multidrug-resistant Organisms |
| OPAT | Outpatient Parenteral Antimicrobial Therapy |
| OR | Odds Ratios |
| PICC | Peripherally Inserted Central Catheters |
| RPHLK | Regional Public Health Laboratory Kennemerland |
| SD | Standard Deviation |
| SG | Spaarne Gasthuis (hospital) |
| S-OPAT | Self-administered Outpatient Parenteral Antimicrobial Therapy |
| TDM | Therapeutic Drug Monitoring |
References
- Berrevoets, M.A.H.; Oerlemans, A.J.M.; Tromp, M.; Kullberg, B.J.; Ten Oever, J.; Schouten, J.A.; Hulscher, M.E. Quality of Outpatient Parenteral Antimicrobial Therapy (OPAT) Care from the Patient’s Perspective: A Qualitative Study. BMJ Open 2018, 8, e024564. [Google Scholar] [CrossRef]
- Chapman, A.L.N.; Dixon, S.; Andrews, D.; Lillie, P.J.; Bazaz, R.; Patchett, J.D. Clinical Efficacy and Cost-Effectiveness of Outpatient Parenteral Antibiotic Therapy (OPAT): A UK Perspective. J. Antimicrob. Chemother. 2009, 64, 1316–1324. [Google Scholar] [CrossRef] [PubMed]
- Stichting Werkgroep Antibioticabeleid (SWAB). Praktijkgids Implementatie Van Een OPAT-Programma in Het Ziekenhuis; Stichting Werkgroep Antibioticabeleid (SWAB): Leiden, The Netherlands, 2023. [Google Scholar]
- Tice, A.D.; Rehm, S.J.; Dalovisio, J.R.; Bradley, J.S.; Martinelli, L.P.; Graham, D.R.; Gainer, R.B.; Kunkel, M.J.; Yancey, R.W.; Williams, D.N. Practice Guidelines for Outpatient Parenteral Antimicrobial Therapy. Clin. Infect. Dis. 2004, 38, 1651–1671. [Google Scholar] [CrossRef] [PubMed]
- Paladino, J.A.; Poretz, D. Outpatient Parenteral Antimicrobial Therapy Today. Clin. Infect. Dis. 2010, 51, S198–S208. [Google Scholar] [CrossRef]
- Minton, J.; Murray, C.C.; Meads, D.; Hess, S.; Vargas-Palacios, A.; Mitchell, E.; Wright, J.; Hulme, C.; Raynor, D.K.; Gregson, A.; et al. The Community IntraVenous Antibiotic Study (CIVAS): A Mixed-Methods Evaluation of Patient Preferences for and Cost-Effectiveness of Different Service Models for Delivering Outpatient Parenteral Antimicrobial Therapy. Health Serv. Deliv. Res. 2017, 5, 1–272. [Google Scholar] [CrossRef] [PubMed]
- Browning, S.; Loewenthal, M.R.; Freelander, I.; Dobson, P.M.; Schneider, K.; Davis, J.S. Safety of Prolonged Outpatient Courses of Intravenous Antibiotics: A Prospective Cohort Study. Clin. Microbiol. Infect. 2022, 28, 832–837. [Google Scholar] [CrossRef]
- Bugeja, S.J.; Stewart, D.; Vosper, H. Clinical Benefits and Costs of an Outpatient Parenteral Antimicrobial Therapy Service. Res. Soc. Adm. Pharm. 2021, 17, 1758–1763. [Google Scholar] [CrossRef]
- Lai, T.; Thiele, H.; Rogers, B.A.; Hillock, N.; Adhikari, S.; McNamara, A.; Rawlins, M. Exploring the Advancements of Australian OPAT. Ther. Adv. Infect. Dis. 2023, 10, 20499361231199582. [Google Scholar] [CrossRef]
- Reidy, P.; Breslin, T.; Muldoon, E. Outpatient Parenteral Antimicrobial Therapy (OPAT) across the World: A Comparative Analysis—What Lessons Can We Learn? JAC-Antimicrob. Resist. 2024, 6, dlae111. [Google Scholar] [CrossRef]
- Durojaiye, O.C.; Fiori, C.; Cartwright, K. Delivery of Outpatient Parenteral Antimicrobial Therapy (OPAT) in an Ever-Changing National Health Service (UK): Benefits, Barriers, and Opportunities. Antibiotics 2025, 14, 451. [Google Scholar] [CrossRef]
- Hassanzai, M.; Adanç, F.; Koch, B.C.P.; Verkaik, N.J.; van Oldenrijk, J.; de Bruin, J.L.; de Winter, B.C.M.; van Onzenoort, H.A.W. Best Practices, Implementation and Challenges of Outpatient Parenteral Antimicrobial Therapy: Results of a Worldwide Survey among Healthcare Providers. Ther. Adv. Infect. Dis. 2023, 10, 20499361231214901. [Google Scholar] [CrossRef]
- Stoorvogel, H.H.; Hulscher, M.E.J.L.; Wertheim, H.F.L.; Yzerman, E.P.F.; Scholing, M.; Schouten, J.A.; ten Oever, J. Current Practices and Opportunities for Outpatient Parenteral Antimicrobial Therapy in Hospitals: A National Cross-Sectional Survey. Antibiotics 2022, 11, 1343. [Google Scholar] [CrossRef]
- Chopra, V.; Anand, S.; Hickner, A.; Buist, M.; Rogers, M.A.; Saint, S.; Flanders, S.A. Risk of Venous Thromboembolism Associated with Peripherally Inserted Central Catheters: A Systematic Review and Meta-Analysis. Lancet Lond. Engl. 2013, 382, 311–325. [Google Scholar] [CrossRef] [PubMed]
- Mermel, L.A. Prevention of Intravascular Catheter–Related Infections. Ann. Intern. Med. 2000, 132, 391–402. [Google Scholar] [CrossRef] [PubMed]
- Li, H.-K.; Rombach, I.; Zambellas, R.; Walker, A.S.; McNally, M.A.; Atkins, B.L.; Lipsky, B.A.; Hughes, H.C.; Bose, D.; Kümin, M.; et al. Oral versus Intravenous Antibiotics for Bone and Joint Infection. N. Engl. J. Med. 2019, 380, 425–436. [Google Scholar] [CrossRef] [PubMed]
- Kaasch, A.J.; López-Cortés, L.E.; Rodríguez-Baño, J.; Cisneros, J.M.; Navarro, M.D.; Fätkenheuer, G.; Jung, N.; Rieg, S.; Lepeule, R.; Coutte, L.; et al. Efficacy and Safety of an Early Oral Switch in Low-Risk Staphylococcus Aureus Bloodstream Infection (SABATO): An International, Open-Label, Parallel-Group, Randomised, Controlled, Non-Inferiority Trial. Lancet Infect. Dis. 2024, 24, 523–534. [Google Scholar] [CrossRef]
- Patel, J.; Saeedi Moghaddam, S.; Ranganathan, S.; Vezeau, N.; O’Neill, E.; Harant, A. Global Policy Responses to Antimicrobial Resistance, 2021–2022: A Systematic Governance Analysis of 161 Countries and Territories. Lancet Infect. Dis. 2025; Online ahead of print. [Google Scholar] [CrossRef]
- Centraal Bureau Voor de Statistiek Inflatie 3,3 Procent in 2024. Available online: https://www.cbs.nl/nl-nl/nieuws/2025/03/inflatie-3-3-procent-in-2024 (accessed on 21 July 2025).
- Schuts, E.; Hulscher, M.; Mouton, J.; Verduin, C.; Cohen Stuart, J.; Overdiep, H.; Van der Linden, P.; Natsch, S.; Hertogh, C.; Wolfs, T.; et al. Current Evidence on Hospital Antimicrobial Stewardship Objectives: A Systematic Review and Meta-Analysis. Lancet Infect. Dis. 2016, 16, 847–856. [Google Scholar] [CrossRef]
- Murray, C.J.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Aguilar, G.R.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E.; et al. Global Burden of Bacterial Antimicrobial Resistance in 2019: A Systematic Analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef]
- Mohammed, S.A.; Roberts, J.A.; Cotta, M.O.; Rogers, B.; Pollard, J.; Assefa, G.M.; Erku, D.; Sime, F.B. Safety and Efficacy of Outpatient Parenteral Antimicrobial Therapy: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Int. J. Antimicrob. Agents 2024, 64, 107263. [Google Scholar] [CrossRef]
- Conant, M.; Erdman, S.; Osterholzer, D. Mandatory Infectious Diseases Approval of Outpatient Parenteral Antimicrobial Therapy (OPAT): Clinical and Economic Outcomes of Averted Cases. J. Antimicrob. Chemother. 2014, 69, 1695–1700. [Google Scholar] [CrossRef]
- Veerman, K.; Goosen, J.; Spijkers, K.; Jager, N.; Heesterbeek, P.; Telgt, D. Prolonged Use of Linezolid in Bone and Joint Infections: A Retrospective Analysis of Adverse Effects. J. Antimicrob. Chemother. 2023, 78, 2660–2666. [Google Scholar] [CrossRef]
- Ten Doesschate, T.; Van Mens, S.P.; Van Nieuwkoop, C.; Geerlings, S.E.; Hoepelman, A.I.M.; Bonten, M.J.M. Oral Fosfomycin versus Ciprofloxacin in Women with E.Coli Febrile Urinary Tract Infection, a Double-Blind Placebo-Controlled Randomized Controlled Non-Inferiority Trial (FORECAST). BMC Infect. Dis. 2018, 18, 626. [Google Scholar] [CrossRef] [PubMed]
- Burch, A.R.; Ledergerber, B.; Ringer, M.; Padrutt, M.; Reiber, C.; Mayer, F.; Zinkernagel, A.S.; Eberhard, N.; Kaelin, M.B.; Hasse, B. Improving Antimicrobial Treatment in Terms of Antimicrobial Stewardship and Health Costs by an OPAT Service. Infection 2024, 52, 1367–1376. [Google Scholar] [CrossRef]
- Lanckohr, C.; Bracht, H. Antimicrobial Stewardship. Curr. Opin. Crit. Care 2022, 28, 551–556. [Google Scholar] [CrossRef] [PubMed]
- Dyar, O.J.; Huttner, B.; Schouten, J.; Pulcini, C. What Is Antimicrobial Stewardship? Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2017, 23, 793–798. [Google Scholar] [CrossRef]
- Wijnakker, R.; Visser, L.E.; Schippers, E.F.; Visser, L.G.; van Burgel, N.D.; van Nieuwkoop, C. The Impact of an Infectious Disease Expert Team on Outpatient Parenteral Antimicrobial Treatment in the Netherlands. Int. J. Clin. Pharm. 2019, 41, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Cassettari, V.; Novato, N.; Onuchic, M.H.F. Antimicrobial Stewardship in the Outpatient Parenteral Antimicrobial Therapy (OPAT) Setting: The Impact of Prescription Assessment by an Infectious Diseases Specialist. Braz. J. Infect. Dis. 2021, 25, 101560. [Google Scholar] [CrossRef]
- Maaskant, J.M.; de Vries, T.; Volle, L.; Jamaludin, F.S.; Geerlings, S.E.; Sigaloff, K.C.E. Clinical and Patient-Reported Outcomes of Self-Administered Outpatient Parenteral Antimicrobial Treatment (S-OPAT): A Scoping Review. Infection 2025, 53, 2083–2102. [Google Scholar] [CrossRef]
| Total n = 529 | Pre-OPAT n = 118 | OPAT n = 411 | p-Value | |
|---|---|---|---|---|
| Sex n (%) | 0.360 | |||
| Male | 335 (63.3%) | 70 (59.3%) | 265 (64.5%) | |
| Female | 194 (36.7%) | 48 (40.7%) | 146 (35.5%) | |
| Age mean (SD) | 67.3 (17.5) | 65.3 (16.5) | 67.8 (17.7) | 0.155 |
| Department n (%) | 0.002 | |||
| Internal medicine (incl. Nephrology, Oncology) | 152 (28.7%) | 39 (33.1%) | 113 (27.5%) | |
| Surgery (incl. Vascular Surgery and Trauma Surgery) | 76 (14.4%) | 18 (15.3%) | 58 (14.1%) | |
| Cardiology | 82 (15.5%) | 10 (8.5%) | 72 (17.5%) | |
| Pulmonology | 41 (7.8%) | 11 (9.3%) | 30 (7.3%) | |
| Orthopedics | 22 (4.2%) | 1 (0.8%) | 21 (5.1%) | |
| Urology | 59 (11.2%) | 24 (20.3%) | 35 (8.5%) | |
| Geriatrics | 30 (5.7%) | 2 (1.7%) | 28 (6.8%) | |
| Neurology (incl. Neurosurgery) | 38 (7.2%) | 7 (5.9%) | 31 (7.5%) | |
| Pediatrics | 13 (2.5%) | 3 (2.5%) | 10 (2.4%) | |
| Other departments 1 | 16 (3.0%) | 3 (2.5%) | 13 (3.2%) | |
| Primary indication n (%) | 0.001 | |||
| Endocarditis | 108 (20.4%) | 14 (11.9%) | 94 (22.9%) | |
| Urinary tract infection | 94 (17.8%) | 35 (29.7%) | 59 (14.4%) | |
| Pulmonary infection | 43 (8.1%) | 12 (10.2%) | 31 (7.5%) | |
| Abscess/soft tissue infection | 30 (5.7%) | 3 (2.5%) | 27 (6.6%) | |
| Neurological infection/eye infection | 39 (7.4%) | 11 (9.3%) | 28 (6.8%) | |
| Osteomyelitis/spondylodiscitis/arthritis | 98 (18.5%) | 25 (21.2%) | 73 (17.8%) | |
| Vascular infection/aortitis/mycotic aneurysm | 26 (4.9%) | 5 (4.2%) | 21 (5.1%) | |
| Bloodstream infection (without focus, or associated with phlebitis or intravascular catheter-related origin) | 64 (12.1%) | 7 (5.9%) | 57 (13.9%) | |
| Other infections 2 | 27 (5.1%) | 6 (5.1%) | 21 (5.1%) | |
| Additional indication n (%) | ||||
| S. aureus bacteraemia | 120 (22.7%) | 15 (12.7%) | 105 (25.5%) | 0.005 |
| Other bacteraemia or candidemia | 152 (28.7%) | 33 (28.0%) | 119 (29.0%) | 0.925 |
| Device related infections 3 | 107 (20.2%) | 21 (17.8%) | 86 (20.9%) | 0.538 |
| Multidrug-resistant organisms | 64 (12.1%) | 22 (18.6%) | 42 (10.2%) | 0.021 |
| Duration of IV antibiotics (days) mean (SD) | 24.7 (24.7) | 34.4 (38.5) | 21.8 (18.1) | 0.001 |
| Clinical response n (%) | 0.313 | |||
| Good | 356 (67.3%) | 81 (68.6%) | 275 (66.9%) | |
| Reasonable (still some symptoms) | 87 (16.4%) | 20 (16.9%) | 67 (16.3%) | |
| Poor | 54 (10.2%) | 14 (11.9%) | 40 (9.7%) | |
| Deceased 4 | 32 (6.0%) | 3 (2.5%) | 29 (7.1%) | |
| Recurrence (<3 months) n (%) | 0.011 | |||
| No | 471 (89.0%) | 97 (82.2%) | 374 (91.0%) | |
| Yes | 58 (11.0%) | 21 (17.8%) | 37 (9.0%) | |
| Complications n (%) | 0.009 | |||
| No complications | 457 (86.4%) | 93 (78.8%) | 364 (88.6%) | |
| Mild complications | 50 (9.5%) | 15 (12.7%) | 35 (8.5%) | |
| Severe complications | 22 (4.2%) | 10 (8.5%) | 12 (2.9%) | |
| Readmissions (<3 months) n (%) | 0.184 | |||
| No | 424 (80.2%) | 89 (75.4%) | 335 (81.5%) | |
| Yes | 105 (19.8%) | 29 (24.6%) | 76 (18.5%) | |
| Timely removal of PICC n (%) * | 0.002 | |||
| Yes | 336 (90.8%) | 58 (80.6%) | 278 (93.3%) | |
| No | 34 (9.2%) | 14 (19.4%) | 20 (6.7%) | |
| Days waiting for discharge mean (SD) ** | 4.8 (6.0) | 4.7 (6.3) | 4.8 (5.8) | 0.836 |
| Baseline | Model | Adjusted | Model * | |||||
|---|---|---|---|---|---|---|---|---|
| Regression Coefficient | Odds Ratio | CI 95% | p-Value | Regression Coefficient | Odds Ratio | CI 95% | p-Value | |
| Duration of IV therapy | −12.58 | [−17.55; −7.62] | <0.001 | −13.97 | [−18.79; −9.15] | <0.001 | ||
| Clinical response | 1.20 | [0.69–2.19] | 0.537 | 1.22 | [0.67–2.32] | 0.527 | ||
| Recurrences | 0.46 | [0.26–0.83] | 0.008 | 0.74 | [0.38–1.48] | 0.353 | ||
| Readmissions | 0.70 | [0.43–1.15] | 0.145 | 0.75 | [0.44–1.29] | 0.287 | ||
| Complications | 0.48 | [0.28–0.83] | 0.007 | 0.44 | [0.24–0.81] | 0.007 | ||
| Timely PICC removal ** | 0.30 | [0.14–0.63] | 0.001 | 0.29 | [0.12–0.68] | 0.004 | ||
| Combination variable *** | 0.48 | [0.31–0.73] | 0.001 | 0.58 | [0.37–0.92] | 0.021 |
| Pre-OPAT | OPAT | Difference | ||||
|---|---|---|---|---|---|---|
| Per patient | Per 100 patients | Per patient | Per 100 patients | Per patient | Per 100 patients | |
| IV preparations | 5,201.18 | 520,117.76 | 1,879.38 | 187,938.08 | 3,321.80 | 332,179.68 |
| Oral antibiotics | 24.14 | 2,414.00 | - 24.14 | - 2,414.00 | ||
| TDM 1 | 1.24 | 124.40 | 1.16 | 115.70 | 0.08 | 8.70 |
| Ertapenem * | 15.59 | 1,559.12 | - 15.59 | - 1,559.12 | ||
| OPAT team | 23.43 | 2,343.00 | - 23.43 | - 2,343.00 | ||
| PICC placements | 234.53 | 23,453.39 | 186.13 | 18,613.13 | 48.40 | 4,840.26 |
| Days waiting for discharge | 2,928.67 | 292,867.44 | 2,892.46 | 289,246.02 | 36.21 | 3,621.42 |
| Total | 8,365.62 | 836,562.99 | 5,022.29 | 502,229.05 | 3,343.33 | 334,333.94 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manders, I.G.; Comello, D.; Souverein, D.; Euser, S.; Herpers, B.L.; Vetten, J.; Kalpoe, J.S.; Goeijenbier, M.; van Lelyveld, S.F.L. The Impact of a Structured Outpatient Parenteral Antimicrobial Therapy (OPAT) Programme on Quality of Care, Optimisation of Antimicrobial Use, and Healthcare Costs: A Retrospective Cohort Study. Antibiotics 2025, 14, 1103. https://doi.org/10.3390/antibiotics14111103
Manders IG, Comello D, Souverein D, Euser S, Herpers BL, Vetten J, Kalpoe JS, Goeijenbier M, van Lelyveld SFL. The Impact of a Structured Outpatient Parenteral Antimicrobial Therapy (OPAT) Programme on Quality of Care, Optimisation of Antimicrobial Use, and Healthcare Costs: A Retrospective Cohort Study. Antibiotics. 2025; 14(11):1103. https://doi.org/10.3390/antibiotics14111103
Chicago/Turabian StyleManders, Irene G., Darya Comello, Dennis Souverein, Sjoerd Euser, Bjorn L. Herpers, Judith Vetten, Jayant S. Kalpoe, Marco Goeijenbier, and Steven F. L. van Lelyveld. 2025. "The Impact of a Structured Outpatient Parenteral Antimicrobial Therapy (OPAT) Programme on Quality of Care, Optimisation of Antimicrobial Use, and Healthcare Costs: A Retrospective Cohort Study" Antibiotics 14, no. 11: 1103. https://doi.org/10.3390/antibiotics14111103
APA StyleManders, I. G., Comello, D., Souverein, D., Euser, S., Herpers, B. L., Vetten, J., Kalpoe, J. S., Goeijenbier, M., & van Lelyveld, S. F. L. (2025). The Impact of a Structured Outpatient Parenteral Antimicrobial Therapy (OPAT) Programme on Quality of Care, Optimisation of Antimicrobial Use, and Healthcare Costs: A Retrospective Cohort Study. Antibiotics, 14(11), 1103. https://doi.org/10.3390/antibiotics14111103





