Abstract
Stenotrophomonas maltophilia is an opportunistic pathogen that produces respiratory infections in immunosuppressed and cystic fibrosis patients. The therapeutic options to treat S. maltophilia infections are limited since it exhibits resistance to a wide variety of antibiotics such as β-lactams, aminoglycosides, tetracyclines, cephalosporins, macrolides, fluoroquinolones, or carbapenems. The antibiotic combination trimethoprim/sulfamethoxazole (SXT) is the treatment of choice to combat infections caused by S. maltophilia, while ceftazidime, ciprofloxacin, or tobramycin are used in most SXT-resistant infections. In the current study, experimental evolution and whole-genome sequencing (WGS) were used to examine the evolutionary trajectories of S. maltophilia towards resistance against tobramycin, ciprofloxacin, and SXT. The genetic changes underlying antibiotic resistance, as well as the evolutionary trajectories toward that resistance, were determined. Our results determine that genomic changes in the efflux pump regulatory genes smeT and soxR are essential to confer resistance to ciprofloxacin, and the mutation in the rplA gene is significant in the resistance to tobramycin. We identified mutations in folP and the efflux pump regulator smeRV as the basis of SXT resistance. Detailed and reliable knowledge of ciprofloxacin, tobramycin, and SXT resistance is essential for safe and effective use in clinical settings. Herein, we were able to prove once again the extraordinary ability that S. maltophilia has to acquire resistance and the importance of looking for alternatives to combat this resistance.
1. Introduction
Stenotrophomonas maltophilia is a cosmopolitan, ubiquitous, intrinsically multidrug-resistant Gram-negative bacterium with an environmental origin [1] that has been isolated in clinical [2,3,4,5,6] and non-clinical settings [7,8,9,10]. Its prevalence as a nosocomial pathogen increases every day, being mainly associated with respiratory infections in immunosuppressed and cystic fibrosis patients [7]. The increasing rate of antibiotic resistance has limited the therapeutic options and strategies to treat Gram-negative pathogens [11] such as S. maltophilia. This microorganism is considered a prototype of antibiotic-resistant bacteria. It exhibits an intrinsic low susceptibility to a wide variety of antibiotics such as β-lactams, aminoglycosides, tetracyclines, cephalosporins, macrolides, fluoroquinolones, and carbapenems [12]. For this reason, the World Health Organization (WHO) lists S. maltophilia as one of the main pathogens with interest in public health in hospitals worldwide [13]. Currently, the antibiotics’ combination trimethoprim/sulfamethoxazole (SXT) is the treatment of choice, with ceftazidime, ciprofloxacin, and tobramycin being the agents used in the majority of SXT-resistant infections [14,15,16]. With the number of antibiotics of choice restricted, predicting the mechanisms by which this bacterium may acquire resistance becomes important in preventing and treating infections [17,18]. S. maltophilia exhibits numerous mechanisms of antibiotic resistance that contribute to its multidrug-resistant phenotype, including the low permeability of its membrane as well as the presence in its genome of β-lactamases, enzymes that modify aminoglycosides, SmQnr (an enzyme that protects DNA gyrase from quinolones), and multidrug resistance (MDR) efflux pumps [19]. The primary cause of antibiotic resistance in this bacterial species is these efflux systems [20,21].
In the present work, we explore the evolution of resistance to ciprofloxacin (which inhibits bacterial topoisomerases, fundamental for DNA replication [22]), tobramycin (a ribosome-targeting antimicrobial), and SXT (an inhibitor of folic acid synthesis) in S. maltophilia. Ciprofloxacin is the most potent fluoroquinolone against Gram-negative bacilli [23]. The main mechanisms conferring resistance to this antibiotic are alterations in its target enzymes, the DNA topoisomerases GyrA and ParC [24], as well as the overproduction of MDR efflux pumps in most bacterial species [25]. Nevertheless, S. maltophilia is the only microorganism in which resistance to quinolones is not the consequence of mutations in the genes encoding these bacterial topoisomerases but of mutations that lead to the overexpression of efflux pumps [26]. Tobramycin is an aminoglycoside that induces miscoding during protein synthesis and the disruption of the bacterial membrane [27,28,29]. Resistance to tobramycin can result from different mechanisms involving mutations (like those leading to the overproduction of MDR efflux pumps), methylations, or enzymatic modifications of the antibiotic [30,31]. SXT is a fixed-dose combination antibiotic including sulfamethoxazole (a sulfonamide that inhibits folate synthesis) and trimethoprim (a direct competitor of the enzyme dihydrofolate reductase that produces a bactericidal effect) [32]. Bacterial resistance to SXT has been mainly attributed to the acquisition of resistance genes such as dhfr, folP, sul1, and sul2; the latter two are present in the core of ubiquitously distributed integrons. However, target mutations and mutations leading to the overproduction of MDR efflux pumps [33] also confer SXT resistance.
A previous analysis of single-step selected mutants in S. maltophilia detected that resistance to either ciprofloxacin or SXT was due to the overproduction of both the SmeDEF and the SmeVWX efflux pumps [33,34]. Nevertheless, this one-step selection only identifies mutations that can independently confer resistance to the antibiotic of selection. It does not provide information about the evolutionary dynamics, including the mutations (frequently low-level resistance mutations) that can jointly render resistance and those that can be relevant in clinics. For this purpose, experimental evolution and whole-genome sequencing (WGS) were used to examine the evolutionary trajectories of S. maltophilia toward resistance against these three antibiotics to determine the genetic changes underlying antibiotic resistance, as well as the evolutionary trajectories toward that resistance.
2. Results
2.1. Experimental Evolution in the Presence of Ciprofloxacin, Tobramycin, and Trimethoprim/Sulfamethoxazole Leads to High Levels of Resistance in S. maltophilia
To ascertain if distinct populations exhibit similar potential evolutionary trajectories, four biological replicates were subjected to selective pressure exerted by ciprofloxacin (CIP-A, CIP-B, CIP-C, and CIP-D), tobramycin (TOB-A, TOB-B, TOB-C, and TOB-D), and SXT (SXT-A, SXT-B32, SXT-B64, SXT-C, and SXT-D), and four were maintained without any selective pressure (A, B, C and D). All of them were serially passaged for 21 days, increasing the antibiotic concentration to track the progression of resistance during the selection period. The initial concentration of each antibiotic used in these experimental evolutions was the baseline minimal inhibitory concentration (MIC): 0.75 μg/mL of ciprofloxacin, 4 μg/mL of tobramycin, and 0.5 μg/mL of SXT. When bacteria are exposed to escalating antibiotic concentrations, one phenotypic trajectory can be anticipated: a gradual selection of mutants displaying progressively higher resistance levels. All the evolved populations, in the presence of the selective pressure exerted by each antibiotic, reached high levels of resistance (Table 1). All the populations that evolved in the absence of the drug had final MICs of 0.75 μg/mL to ciprofloxacin, 4 μg/mL to tobramycin, and 0.5 μg/mL to SXT.

Table 1.
MICs (μg/mL) of the seventeen populations evolved in the presence of the selective pressure exerted by each antibiotic. The populations reached high levels of resistance in comparison with the populations that evolved in the absence of the drugs.
2.2. Mutations Selected in the Presence of Ciprofloxacin, Tobramycin, and Trimethoprim/Sulfamethoxazole in S. maltophilia D457
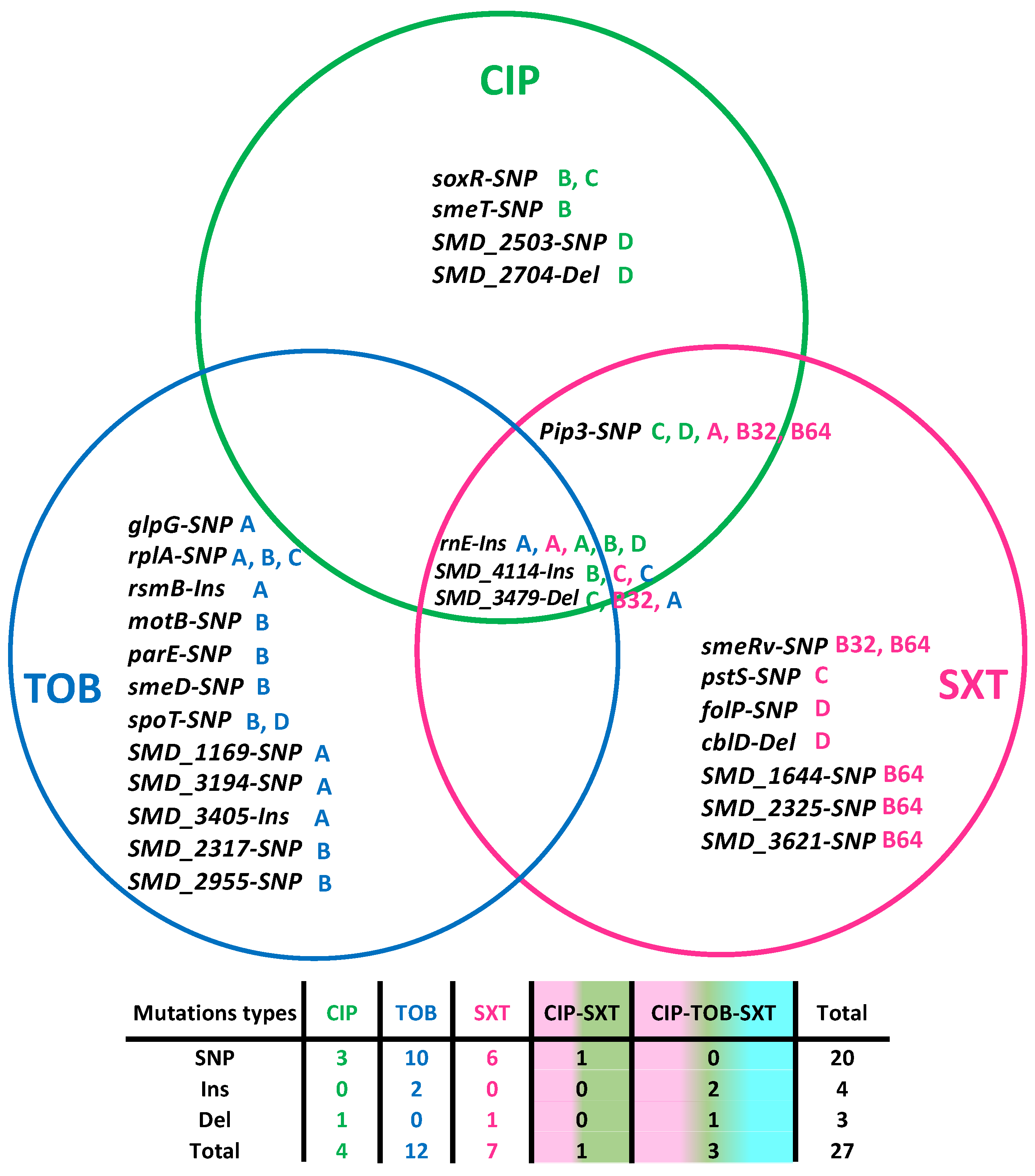
To better understand the genetic events linked to the emergence of resistance in the evolved populations, the genome of each final population was sequenced. In addition to antibiotic resistance mutations, mutations increasing the fitness of the population for growing in the medium can also be selected. Therefore, only those mutations in the populations evolving under antibiotic selective pressure, but not in the control populations, were considered. Twenty-seven mutations were identified (Table 2 and Figure 1). Notably, three mutations were identified in different populations that evolved in the three antibiotics used. Firstly, insertions in the gene rnE that encodes the ribonuclease E. RnE plays a central role in RNA processing and metabolism [35], and it has been previously linked to high-level ciprofloxacin resistance in Pseudomonas aeruginosa and Pseudomonas fluorescens [36]. Secondly, three base pair insertions were found in the gene SMD_4114. This gene is proposed to encode an S9 family peptidase DAP2. Since endopeptidases have been predicted to function as space makers that trigger peptidoglycan enlargement due to the insertion of a new glycan strand and can be genetically associated with PBPs (penicillin-binding proteins), this mutation could be related to cross-resistance to beta-lactams (see below), such as ceftazidime [37]. Thirdly, single-nucleotide polymorphisms (SNP) or short deletions were detected in the gene SMD_3479, a YiiG family protein with unknown function and predicted to be a lipoprotein [38]. Another SNP was shared between ciprofloxacin and SXT-evolved populations in the gene pip3, a prolyl aminopeptidase. This protein is involved in the surveillance mechanism inducing the DNA-repair pathways [39].

Table 2.
WGS-identified mutations in the ciprofloxacin, tobramycin, and SXT-evolved lineages.
Figure 1.
Distributions of mutations in the evolved lineages: twenty-seven mutations were identified. Among them, three were found in populations that evolved in the three antibiotics used. One extra mutation was shared between ciprofloxacin (CIP) and SXT and the other were specific for the antibiotic used for selection. Four were found in ciprofloxacin-evolved populations, twelve in the tobramycin (TOB) populations, and seven in the SXT. The white boxes indicate the population in which that mutation was found. The table below indicates the type of mutation according to the antibiotic in which the populations evolved. SNP: single-nucleotide variant, Ins: insertions, Del: deletions. Green A, B, C, and D correspond to the CIP-evolved populations in the antibiotics CIP; Blue A, B, C, and D correspond to the TOB-evolved population; and A, B32, B64, C, and D to the SXT-evolved populations.
Moving to ciprofloxacin-evolved populations, four mutations were exclusively identified in the populations that evolved in the presence of this drug. Genomic changes in the genes soxR (a redox-sensitive transcriptional activator that contributes to the multidrug resistant phenotypes of clinical strains) [40], SMD_2503, and SMD_2704 (both of unknown function), and smeT were found. SmeT is a regulator of smeDEF expression. Mutations in this regulator deal to the overproduction of the SmeDEF efflux pump, and hence to MDR in this bacterial species [19].
Twelve genetic changes were found exclusively in the tobramycin-evolved populations. SNPs in the gene that encodes the L1 50S ribosomal protein, rplA, were detected, which is consistent with the tobramycin mechanism of action. Again, mutations related to the SmeDEF efflux pump were found; in this case, an SNP in the gene encoding SmeD, the periplasmic adaptor subunit of the multidrug efflux transporter SmeDEF. Furthermore, we identified mutations in genes not previously related to aminoglycosides resistance: glpG, which encodes an intramembrane serine protease of the rhomboid family; rsmB, an RNA regulator that interacts with rsmA, and which overexpression increases the production of N-acyl-homoserine lactone, pyocyanin, and elastase [41]; motB, which encodes a protein that integrates into the cell membrane and is part of the flagellar motor protein complex [42]; parE, encoding the DNA topoisomerase IV subunit B and whose mutation renders to quinolone resistance in E. coli [43], S. typhi [44] or R. anatipestifer [45]; spoT, a synthetase-hydrolase that regulates the concentration of (p)ppGpp [46]; SMD_3194, an ATP-binding protein of unknown function; SMD_3405, a putative membrane protein of unknown function; SMD_1169, an acetyltransferase; SMD_2317, an ABC transporter; and SMD_2955, an PepSY-associated TM helix domain-containing protein that has been suggested to function as a controller of peptidase activity within the immediate environmental and, in addition, protect the cell from lysis.
Finally, seven mutations were found in the SXT-evolved populations. Importantly, this includes an SNP in the gene smeRv, a transcriptional regulator whose mutation leads to the overproduction of the SmeVWX efflux pump, whose contribution to the acquisition of resistance to SXT in single-step selected mutans was previously described in S. maltophilia [47]. Additionally, an SNP in the gene folP, that encodes a dihydropteroate synthase, the target enzyme of the sulfonamides, was detected. This enzyme confers sulfonamide resistance by preventing the inhibition of folate synthesis by sulfonamide antibiotics, such as SXT [48]. Another SNP in the gene SMD_3621, a pteridine reductase related to the synthesis of folates in bacteria, was also found [49]. Moreover, mutational changes in pstS (the substrate-binding component of the ABC-type transporter complex pstSACB, involved in phosphate import [50]), cblD (a pilus assembly protein that is required for surface expression of cable pili but is not related to antibiotic resistance [51]), and SMD_1644 and SMD_2325 (two hypothetical proteins with unknown function and for which participation in antibiotic resistance has not been reported yet) were identified.
Among the mutations, there were 20 SNPs, 4 insertions, and 3 deletions. Notably, almost all mutant alleles selected in the presence of antibiotics had coverages of >90%, (Table 2). The identified mutations show the versatility of the resistance mechanisms of S. maltophilia. We identified mutations in genes encoding RND efflux pumps, oxidative stress response proteins, outer membrane regulators, resistance regulators, and virulence determinants. Below, we discuss their functions according to our results.
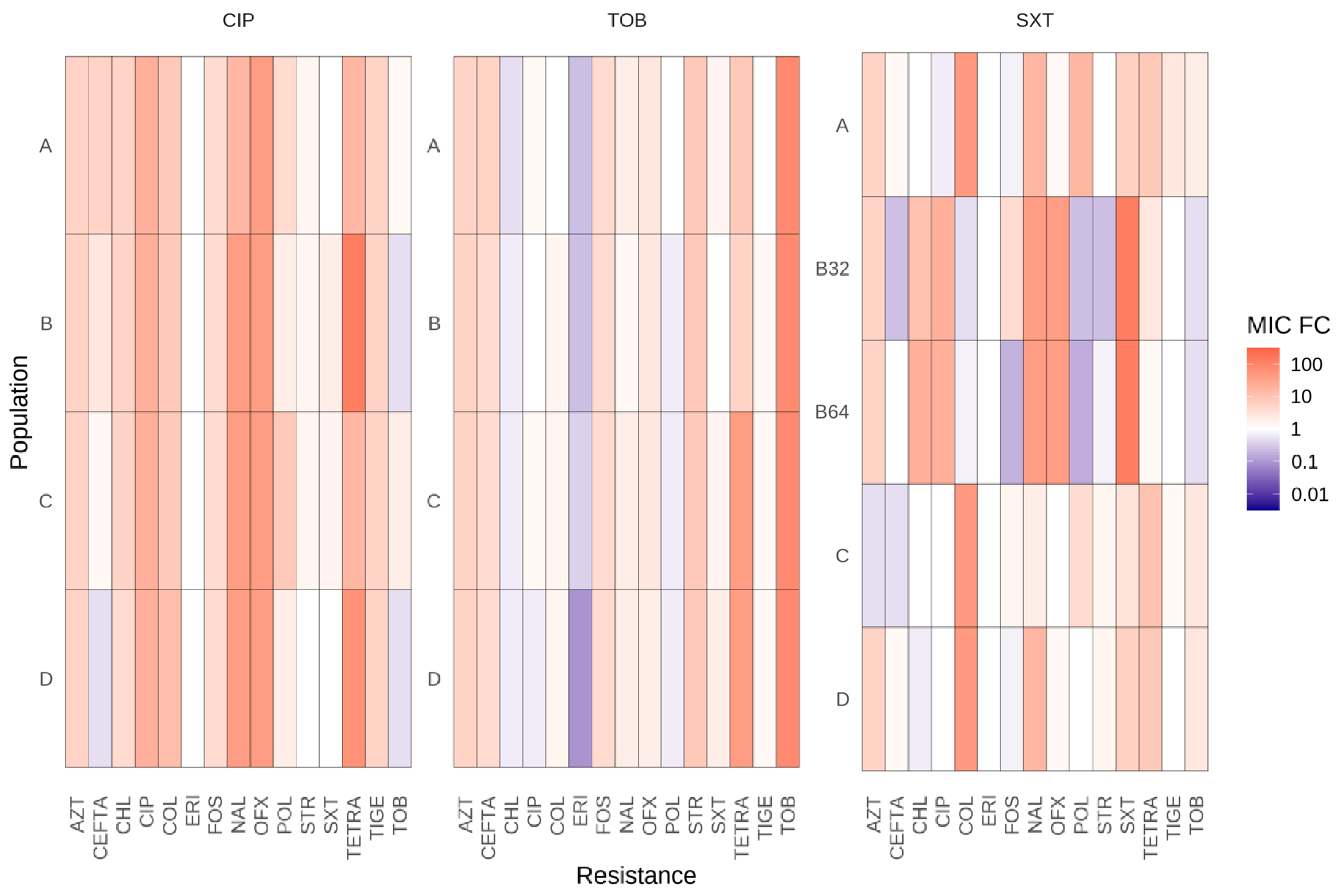
2.3. Adaptative Trajectories, Cross-Resistance, and Collateral Sensitivity of Evolved Populations
To assess whether the development of antibiotic resistance was specific to the antibiotic used for selection or impacted the susceptibility to other antibiotics, the resistance levels to other antibiotics were measured. Nine families of antibiotics (beta-lactams, fluoroquinolones, tetracyclines, macrolides, aminoglycosides, polymyxins, phenols, monobactam, and phosphonic) were tested. Almost all evolved populations demonstrated increased resistance or susceptibility to other antibiotics from various structural families, indicating that some resistance mutations are not specific to ciprofloxacin, tobramycin, and SXT (Figure 2).
Figure 2.
Collateral susceptibility of the evolved S. maltophilia populations to antibiotics from different families. MICs fold changes in the 17 fosfomycin-evolved populations, with respect to the populations that evolved in the absence of antibiotics. Values of at least double or half the control populations’ MIC were considered significant. CIP, ciprofloxacin; TOB, tobramycin; SXT, trimethoprim/sulfamethoxazole; TIGE, tigecycline; STR, streptomycin; TETRA, tetracycline; OFX, ofloxacin; AZT, aztreonam; NAL, nalidixic acid; CEFTA, ceftazidime; CHL, chloramphenicol; FOS, fosfomycin; ERI, erythromycin; COL, colistin; POL, polymyxin B. A, B, C, and D correspond to the CIP and TOB-evolved populations in the first two panels. A, B32, B64, C, and D to the SXT-evolved populations in the third panel.
The evolved populations in ciprofloxacin (CIP-A, CIP-B, CIP-C, and CIP-D) showed cross-resistance to tetracycline, nalidixic acid, and ofloxacin and collateral susceptibility to SXT and tobramycin. The four tobramycin-evolved populations (TOB-A, TOB-B, TOB-C, and TOB-D) displayed cross-resistance to tetracycline and collateral sensibility to chloramphenicol, erythromycin, and ciprofloxacin. Additionally, two tobramycin-evolved populations (TOB-B, TOB-D) were hypersusceptible to SXT.
Concerning evolved populations in SXT, three populations (SXT-A, SXT-C, and SXT-D) were unable to acquire high levels of resistance to SXT but presented cross-resistance to tigecycline, tetracycline, aztreonam, nalidixic acid, or colistin. Furthermore, the two populations acquiring high levels of SXT resistance (SXT-B32 and SXT-B64) showed cross-resistance to ciprofloxacin, ofloxacin, aztreonam, nalidixic acid, tetracycline, and chloramphenicol. These results are consistent with the mutation in smeRV identified in these two populations that would lead to an overproduction of the SmeVWX efflux pump, which contributes to the acquisition of resistance to the aforementioned antibiotics [33]. SXT-B32 and SXT-B64 also demonstrated collateral susceptibility to tobramycin, streptomycin, ceftazidime, fosfomycin, polymyxin B, and colistin.
3. Discussion
In this work, we identified that all the evolved populations reached high levels of resistance in the presence of the selective pressure exerted by each antibiotic, in comparison with the populations that evolved in the absence of the drugs. Since the purpose of this work was to identify stable mutations that can be fixed, only the final evolved populations were sequenced. We are aware that sequencing intermediate evolved populations will also provide information on the dynamics of the evolution of antibiotic resistance; however, this study is beyond the focus of the current work. Twenty-seven mutations were identified. Among them, twenty correspond to SNPs, three to deletions, and four to insertions. The mutations affect elements of the outer membrane, oxidative stress response, previously known resistance determinants, and virulence. We also studied the cross-resistance and collateral sensitivity of these evolved populations.
Among the mutations found during the course of these evolutions, insertions in the gene rnE (Ribonuclease E) were identified in populations selected in the presence of the three antibiotics. This gene plays a central role in RNA processing and metabolism [35], and it is emerging as a potential antibacterial target in Acinetobacter baumanni [52]. rnE is required for the maturation of the 5S and 16S rRNAs and the majority of tRNAs, including the mRNA processing and cleaving of the 5’ leader of the ompA mRNA [53]. We have found that the S. maltophilia genome encodes a porin orthologous to the Escherichia coli OpmA and the P. aeruginosa OprF (SMD_2502) [54]. Clinical isolates of P. aeruginosa that are antibiotic-resistant to imipenem and polymyxin B and deficient in the major outer membrane protein OprF have been isolated in a previous work [36]. This result suggests that the lack of processing of the OpmA mRNA would lead to a decrease of this porin in the outer membrane, increasing antibiotic resistance to multiple antibiotics. This might suggest that OmpA/OprF could be a major outer membrane antibiotic transporter in S. maltophilia as it is in P. aeruginosa [36], since its blockage is enough to confer high-level ciprofloxacin resistance. This resistance could lead to erythromycin susceptibility too, leading to increased binding of this antibiotic to its target site in the 50S ribosomal subunit, since RnE is required for the maturation of rRNAs.
Ciprofloxacin-evolved population CIP-D presented an SNP in a gene encoding a protein that shows 95% identity with YadA, an adhesin precursor from P. aeruginosa. This collagen-binding outer membrane protein forms a fibrillar matrix on the bacterial cell surface that promotes initial attachment and invasion of eukaryotic cells. Although it also protects the bacteria by being responsible for agglutination, serum resistance, complement inactivation, and phagocytosis resistance, this change has not been related to antibiotic resistance.
Populations CIP-B and CIP-C shared an SNP in soxR. This redox-sensitive transcriptional activator induces the expression of the RND efflux pump-encoding operon mexGHI-opmD in P. aeruginosa [55]. Moreover, the constitutive soxS expression caused by single point mutations in the soxR gene has been shown to contribute to the MDR phenotypes of clinical strains, and it is sufficient to confer multiple-antibiotic resistance in a fresh genetic background. The increased soxS expression in E. coli leads to the downregulation of the expression of the gene encoding the outer membrane porin OmpF [56,57], to a decrease in cell permeability, and to an increased expression of the genes encoding the AcrAB efflux pump [58]. All in all, soxRS-mediated antibiotic resistance is a result of the combination of an increased efflux pump activity and decreased cell permeability [40]. Hence, our results indicate that SoxR is important for ciprofloxacin resistance in S. maltophilia, as has been previously described for other organisms like A. baumannii [59], E. coli [40], and K. pneumoniae [60].
A SNP in the smeDEF regulator, smeT, was found in a ciprofloxacin-evolved population (CIP-B). Since SmeDEF is a main determinant of MDR in S. maltophilia, the observed cross-resistance to tigecycline, chloramphenicol, erythromycin, SXT, or tetracycline is consistent with the fact that these antibiotics are substrates of SmeDEF [61]. Further, the same substitution, L166Q, has been previously associated with antibiotic resistance in clinical isolates of S. maltophilia, supporting the reliability of our results [61].
All in all, these results suggest that decreased permeability and the overproduction of MDR efflux pumps are the main mechanisms driving ciprofloxacin resistance, as well as the broad cross-resistance caused by this selection.
Regarding tobramycin-evolved populations, populations TOB-A, TOB-B, and TOB-C presented different SNPs in the gene rplA, encoding the 50S ribosomal protein L1, which has been previously related to the aminoglycosides’ resistance in S. maltophilia [62].
The populations TOB-B and TOB-D showed molecular changes in spoT. SpoT regulates the nutritional starvation stringent response [63,64,65]. Although this synthetase-hydrolase of the alarmone ppGpp has not been previously related to antibiotic resistance, it has been proposed that the stringent response can modulate antibiotic resistance and tolerance [66]. It is important to notice that the population TOB-D only presents the spoT mutation and that the coverage of the mutation was 100%. The fact that no further mutations are found in the evolved population strongly suggests that this mutation is responsible for the acquired tobramycin resistance in this population, although more work would be needed to fully support this statement.
In the population TOB-A, an SNP was found in a gene related to metabolism: glpG. This gene encodes a rhomboid family intramembrane serine protease required to produce an extracellular signaling molecule that regulates cellular functions, including peptidoglycan acetylation, methionine transport, and cysteine biosynthesis. Previously, a glpG mutant of E. coli exhibited a slight increase in resistance to β-lactams [67]. Interestingly, the tobramycin-evolved population TOB-A presents greater cross-resistance levels to ceftazidime than the other populations that evolved on tobramycin.
Another important change in this TOB-A population is an insertion in the gene encoding the ribosomal RNA small subunit methyltransferase B (RsmB), a regulatory RNA of the global repressor RsmA in P. aeruginosa [41]. RsmA regulates the Type III Secretion System (T3SS) in P. aeruginosa. This system has been proposed to play a role in the expression of MDR efflux pumps in P. aeruginosa. A reduction in T3SS expression in this bacterial species is associated with the overproduction of MexCD-OprJ and MexEF-OprN [68]. Hence, compared to the P. aeruginosa wild-type strain, the rsmA mutant presents increased resistance to amikacin, nalidixic acid, trimethoprim, gentamicin, and ceftazidime. The confirmed role of RsmA in antibiotic resistance implies that RsmA could be a possible global regulator involved in regulating the cross-talk between antibiotic resistance and the virulence associated with T3SS [69]. Thus, this mutation could lead to an unregulated RsmA that produces increased antibiotic resistance.
Furthermore, we identified an SNP in smeD in the population TOB-B. To date, only mutations in the SmeDEF regulator protein (SmeT) have been described to be related to an MDR phenotype. However, it is also known that mutations involving the subunits of efflux pumps in this bacterial species (changes in the SmeH structural element of the SmeGH efflux pump) are involved in the acquisition of resistance [70], suggesting that this mutation could be related to an enhanced efflux of antibiotics such as ofloxacin or tetracycline.
Moving to SXT-evolved populations, we achieved a final concentration of 3MIC in three populations (A, C, and D) and final concentrations of 32MIC (SXT-B32) and 64MIC (SXT-B64) in two other populations. These technical issues might indicate that the acquired resistance to this antibiotic is complex and dependent on a leading mutation. The two highly resistant populations shared a mutation in the smeRv regulator. This mutation would lead to an overproduction of the SmeVWX efflux pump, which contributes to the acquisition of resistance to SXT, ciprofloxacin, ofloxacin, nalidixic acid, levofloxacin, tetracycline, and chloramphenicol [33], antibiotics to which these two populations are cross-resistant.
Population SXT-C presented a mutation in the gene pstS, the substrate-binding component of the ABC-type transporter complex PstSACB involved in phosphate import [50]. The Pst system encoded by the pst operon (pstSCAB-phoU) forms a phosphate transporter across the cytoplasmic membrane. Mutations in this operon have been shown to influence antibiotic susceptibility to polymyxin in E. coli. This effect is due to changes in the expression of RND, MFS, and ABC transporters influenced by pstC disruption [71]. In addition, mutations in this gene significantly decrease bacterial adherence, invasion, motility, and biofilm-forming ability in A. baumannii [72].
Population SXT-D presented a mutation in the gene folP that encodes a dihydropteroate synthase, the target enzyme of sulfonamide. As mentioned, this enzyme prevents the inhibition of folate biosynthesis by sulfonamide antibiotics, such as the one included in SXT, thus conferring sulfonamide resistance. Previous studies related folP point mutations with SXT resistance in Streptococcus mutans [48].
In order to raise high-level SXT resistance, the population SXT-B64 presented a mutation in two hypothetical proteins with unknown function, SMD_1644 and SMD_2325, and in a pteridine reductase. It has been previously studied that overproduction of the pteridine reductase 1 (Ptr1) by gene amplification confers methotrexate resistance in Leishmania promastigotes [73]. However, the reasons why mutations in this gene are selected by SXT in S. maltophilia remain to be clarified.
Finally, in some of the populations involved in ciprofloxacin (CIP-C and CIP-D) and SXT (SXT-A, SXT-B32, and SXT-B64) resistance, mutations in the gene pip3, encoding a prolyl aminopeptidase, were detected. Pip3 is a regulator of a major facilitator antiporter involved in pristinamycin resistance in Streptomyces coelicolor [39]. Whether or not it plays a similar role in S. maltophilia antibiotic resistance, regulating the expression of a drug efflux pump, remains to be established.
In conclusion, resistance to all these antibiotics is related to permeability changes and overexpression of the genes encoding MDR efflux pumps. This result would indicate the need to introduce new antibiotics or new combinatory therapies, together with the development of efflux pump inhibitors, to treat S. maltophilia [19] since high-level resistance is rapidly acquired. Significantly, all the populations that evolved in ciprofloxacin showed collateral susceptibility to tobramycin, and all populations that evolved in tobramycin were susceptible to ciprofloxacin. Reciprocal collateral sensitivity is not a frequent situation [74]. When found, it favors the use of combinations of the antibiotics involved. Our findings support that the sequential combinatory use of ciprofloxacin and tobramycin might improve the treatment outcome of S. maltophilia infections. Nevertheless, we are aware that the translation of these results into clinical practice requires the analysis of the robustness of the observed evolution pathways in clinical isolates presenting different genomic backgrounds [74], a study that is beyond the purposes of the current work.
4. Materials and Methods
4.1. Bacterial Strains and Growth Conditions
The wild-type clinical isolate S. maltophilia D457 was used as the parental strain for the evolution experiments [75]. All the experiments were performed at 37 °C in Mueller–Hinton broth with shaking at 250 rpm in glass tubes.
4.2. Experimental Evolution
Experimental evolution was performed with the wild-type strain D457 [75] growing in the presence of increasing concentrations of ciprofloxacin, tobramycin, and SXT. Sixteen independent bacterial populations (four controls without antibiotics, four populations challenged with ciprofloxacin, four populations challenged with tobramycin, and four populations challenged with SXT). Cultures were grown in parallel in Mueller-Hilton broth at 37 °C and 250 rpm in independent glass tubes. Cultures were initially grown at the maximum concentration of the antibiotics that allowed growth in Mueller–Hinton broth. Serial passages were performed by inoculating 1 μL of bacterial cell cultures in fresh medium containing the same antibiotic concentration every 24 h for 2 days. The initial concentrations used were 0.5 μg/mL ciprofloxacin, 0.5 μg/mL tobramycin, and 0.25 or 0.5 μg/mL SXT. Every three days, the concentration of the drugs was doubled. Ciprofloxacin and tobramycin concentrations increased over the evolution from the initial MIC up to 32MIC. As stated, MIC is defined as the lowest concentration of an antibiotic that inhibits the growth of a specific bacterial strain [76]. From SXT, 5 populations were started in 0.5 μg/mL SXT (3 grew until a final concentration of 3MIC and 1 until 32MIC). An extra population started at 0.25 μg/mL was grown until a final concentration of 64MIC. Every three days, samples from each culture were taken and preserved at −80 ◦C for future investigation. The procedure was repeated for 21 consecutive days.
4.3. DNA Extraction and Whole-Genome Sequencing
At the end of the evolution assays, the total genomic DNAs from the evolved populations were extracted. The genomic DNA extraction was performed with the Chemagic DNA H96 bacterial kit (CMG-799 Chemagic) using the Chemagic 360/MSMI instrument (PerkinElmer, Waltham, MA, USA). The DNA quality assay was performed with an Agilent 2200 TapeStation system from the Translational Genomics Unit (Ramón y Cajal Institute in Madrid, Spain). Library construction and WGS were performed by the Oxford Genomics Centre (Oxford, United Kingdom). Pair End Libraries (2 × 150 bp) were sequenced using an Illumina NovaSeq6000 system (San Diego, CA, USA). The coverage was greater than 150× for all the samples.
4.4. Identification of Mutations
The variant calling and VCF (Variant Call Format) file were created with Bactmap v1.0. [77] against the reference genome of the strain S. maltophilia D457 (GenBank accession number NC_017671.1). BCFtools v1.19. [78] were used for filtering and binding individual CVFs. Variants were then filtered against the D457 laboratory wild-type strain.
4.5. Antimicrobial Susceptibility Assays
MICs for the antibiotics ciprofloxacin, tobramycin, SXT, tigecycline, streptomycin, tetracycline, ofloxacin, aztreonam, nalidixic acid, ceftazidime, chloramphenicol, fosfomycin, and erythromycin were determined on Mueller–Hinton agar plates. MIC of colistin and polymyxin B were determined on Mueller–Hinton II agar plates. MIC test strips (Liofilchem, Roseto degli Abruzzi, Italia) were used in all the cases, and the plates were incubated for 20 h at 37 °C.
Author Contributions
Conceptualization, J.L.M.; Formal analysis, L.E.O.-S.; Funding acquisition, J.L.M.; Investigation, L.E.O.-S. and T.G.-G.; Resources, J.L.M.; Supervision, J.L.M. and T.G.-G.; Writing—original draft, L.E.O.-S. and T.G.-G.; Writing—review and editing, L.E.O.-S., J.L.M. and T.G.-G. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by MCIN/AEI/10.13039/501100011033, grant PID2020-113521RB-I00.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All the data generated are available in this manuscript. Copies of the genome sequence here have been made available under the NCBI BioProject ID PRJNA933546.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Sanz-García, F.; Gil-Gil, T.; Laborda, P.; Ochoa-Sánchez, L.E.; Martínez, J.L.; Hernando-Amado, S. Coming from the Wild: Multidrug Resistant Opportunistic Pathogens Presenting a Primary, Not Human-Linked, Environmental Habitat. Int. J. Mol. Sci. 2021, 22, 8080. [Google Scholar] [CrossRef] [PubMed]
- Rogues, A.M.; Maugein, J.; Allery, A.; Fleureau, C.; Boulestreau, H.; Surcin, S.; Bebear, C.; Janvier, G.; Gachie, J.P. Electronic Ventilator Temperature Sensors as a Potential Source of Respiratory Tract Colonization with Stenotrophomonas maltophilia. J. Hosp. Infect. 2001, 49, 289–292. [Google Scholar] [CrossRef] [PubMed]
- De Mauri, A.; Torreggiani, M.; Chiarinotti, D.; Andreoni, S.; Molinari, G.; De Leo, M. Stenotrophomonas maltophilia: An Emerging Pathogen in Dialysis Units. J. Med. Microbiol. 2014, 63, 1407–1410. [Google Scholar] [CrossRef] [PubMed]
- Stigt, J.A.; Wolfhagen, M.J.; Smulders, P.; Lammers, V. The Identification of Stenotrophomonas maltophilia Contamination in Ultrasound Endoscopes and Reproduction of Decontamination Failure by Deliberate Soiling Tests. Respiration 2015, 89, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Riquena, B.; Monte, L.d.F.V.; Lopes, A.J.; da Silva-Filho, L.V.R.F.; Damaceno, N.; Aquino, E.d.S.; Marostica, P.J.C.; Ribeiro, J.D. Microbiological Contamination of Nebulizers Used by Cystic Fibrosis Patients: An Underestimated Problem. J. Bras. Pneumol. 2019, 45, e20170351. [Google Scholar] [CrossRef] [PubMed]
- Zainulabid, U.A.; Siew, S.W.; Musa, S.M.; Soffian, S.N.; Periyasamy, P.; Ahmad, H.F. Whole-Genome Sequence of a Stenotrophomonas maltophilia Isolate from Tap Water in an Intensive Care Unit. Microbiol. Resour. Announc. 2023, 12, e00995-22. [Google Scholar] [CrossRef] [PubMed]
- An, S.; Berg, G. Stenotrophomonas maltophilia. Trends Microbiol. 2018, 26, 637–638. [Google Scholar] [CrossRef]
- Li, X.; McLaughlin, R.W.; Grover, N.A. Characterization of Antibiotic-Resistant Stenotrophomonas Isolates from Painted Turtles Living in the Wild. Curr. Microbiol. 2023, 80, 93. [Google Scholar] [CrossRef]
- Jägevall, S.; Rabe, L.; Pedersen, K. Abundance and Diversity of Biofilms in Natural and Artificial Aquifers of the Äspö Hard Rock Laboratory, Sweden. Microb. Ecol. 2011, 61, 410–422. [Google Scholar] [CrossRef]
- Ochoa-Sánchez, L.E.; Vinuesa, P. Evolutionary Genetic Analysis Uncovers Multiple Species with Distinct Habitat Preferences and Antibiotic Resistance Phenotypes in the Stenotrophomonas maltophilia Complex. Front. Microbiol. 2017, 8, 1548. [Google Scholar] [CrossRef]
- Yassin, A.; Huralska, M.; Pogue, J.M.; Dixit, D.; Sawyer, R.G.; Kaye, K.S. Executive Summary: State-of-the-Art Review: State of the Management of Infections Caused by Multidrug-Resistant Gram-Negative Organisms. Clin. Infect. Dis. 2023, 77, 1223–1225. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, M.B. Antibiotic Resistance in the Opportunistic Pathogen Stenotrophomonas maltophilia. Front. Microbiol. 2015, 6, 140723. [Google Scholar] [CrossRef] [PubMed]
- Rello, J.; Kalwaje Eshwara, V.; Lagunes, L.; Alves, J.; Wunderink, R.G.; Conway-Morris, A.; Rojas, J.N.; Alp, E.; Zhang, Z. A Global Priority List of the TOp TEn Resistant Microorganisms (TOTEM) Study at Intensive Care: A Prioritization Exercise Based on Multi-Criteria Decision Analysis. Eur. J. Clin. Microbiol. Infect. Dis. 2019, 38, 319–323. [Google Scholar] [CrossRef] [PubMed]
- Li, X.-Z. Role of the Acetyltransferase AAC(6′)-Iz Modifying Enzyme in Aminoglycoside Resistance in Stenotrophomonas maltophilia. J. Antimicrob. Chemother. 2003, 51, 803–811. [Google Scholar] [CrossRef] [PubMed]
- Rojas, P.; Garcia, E.; Calderón, G.M.; Ferreira, F.; Rosso, M. Successful Treatment of Stenotrophomonas maltophilia Meningitis in a Preterm Baby Boy: A Case Report. J. Med. Case Rep. 2009, 3, 7389. [Google Scholar] [CrossRef]
- Toleman, M.A.; Bennett, P.M.; Bennett, D.M.C.; Jones, R.N.; Walsh, T.R. Global Emergence of Trimethoprim/Sulfamethoxazole Resistance in Stenotrophomonas maltophilia Mediated by Acquisition of Sul Genes. Emerg. Infect. Dis. 2007, 13, 559–565. [Google Scholar] [CrossRef] [PubMed]
- Hernández, A.; Ruiz, F.M.; Romero, A.; Martínez, J.L. The Binding of Triclosan to SmeT, the Repressor of the Multidrug Efflux Pump SmeDEF, Induces Antibiotic Resistance in Stenotrophomonas maltophilia. PLoS Pathog. 2011, 7, e1002103. [Google Scholar] [CrossRef] [PubMed]
- Martínez, J.L.; Baquero, F.; Andersson, D.I. Predicting Antibiotic Resistance. Nat. Rev. Microbiol. 2007, 5, 958–965. [Google Scholar] [CrossRef] [PubMed]
- Gil-Gil, T.; Martínez, J.L.; Blanco, P. Mechanisms of Antimicrobial Resistance in Stenotrophomonas maltophilia: A Review of Current Knowledge. Expert Rev. Anti Infect. Ther. 2020, 18, 335–347. [Google Scholar] [CrossRef]
- Li, X.-Z.; Nikaido, H. Efflux-Mediated Drug Resistance in Bacteria. Drugs 2004, 64, 159–204. [Google Scholar] [CrossRef]
- Zhang, L.; Li, X.-Z.; Poole, K. Multiple Antibiotic Resistance in Stenotrophomonas maltophilia: Involvement of a Multidrug Efflux System. Antimicrob. Agents Chemother. 2000, 44, 287–293. [Google Scholar] [CrossRef]
- Redgrave, L.S.; Sutton, S.B.; Webber, M.A.; Piddock, L.J.V. Fluoroquinolone Resistance: Mechanisms, Impact on Bacteria, and Role in Evolutionary Success. Trends Microbiol. 2014, 22, 438–445. [Google Scholar] [CrossRef] [PubMed]
- Campoli-Richards, D.M.; Monk, J.P.; Price, A.; Benfield, P.; Todd, P.A.; Ward, A. Ciprofloxacin: A Review of Its Antibacterial Activity, Pharmacokinetic Properties and Therapeutic Use. Drugs 1988, 35, 373–447. [Google Scholar] [CrossRef] [PubMed]
- Laponogov, I.; Veselkov, D.A.; Crevel, I.M.-T.; Pan, X.-S.; Fisher, L.M.; Sanderson, M.R. Structure of an ‘Open’ Clamp Type II Topoisomerase-DNA Complex Provides a Mechanism for DNA Capture and Transport. Nucleic Acids Res. 2013, 41, 9911–9923. [Google Scholar] [CrossRef]
- Shariati, A.; Arshadi, M.; Khosrojerdi, M.A.; Abedinzadeh, M.; Ganjalishahi, M.; Maleki, A.; Heidary, M.; Khoshnood, S. The Resistance Mechanisms of Bacteria against Ciprofloxacin and New Approaches for Enhancing the Efficacy of This Antibiotic. Front. Public Health 2022, 10, 1025633. [Google Scholar] [CrossRef] [PubMed]
- Valdezate, S.; Vindel, A.; Saéz-Nieto, J.A.; Baquero, F.; Cantón, R. Preservation of Topoisomerase Genetic Sequences during in Vivo and in Vitro Development of High-Level Resistance to Ciprofloxacin in Isogenic Stenotrophomonas maltophilia Strains. J. Antimicrob. Chemother. 2005, 56, 220–223. [Google Scholar] [CrossRef]
- Vicens, Q.; Westhof, E. Crystal Structure of a Complex between the Aminoglycoside Tobramycin and an Oligonucleotide Containing the Ribosomal Decoding A Site. Chem. Biol. 2002, 9, 747–755. [Google Scholar] [CrossRef] [PubMed]
- Wright, G.D.; Berghuis, A.M.; Mobashery, S. Aminoglycoside Antibiotics. Structures, Functions, and Resistance. Adv. Exp. Med. Biol. 1998, 456, 27–69. [Google Scholar] [PubMed]
- Davies, J.; Davis, B.D. Misreading of Ribonucleic Acid Code Words Induced by Aminoglycoside Antibiotics. The Effect of Drug Concentration. J. Biol. Chem. 1968, 243, 3312–3316. [Google Scholar] [CrossRef]
- Walsh, C. Molecular Mechanisms That Confer Antibacterial Drug Resistance. Nature 2000, 406, 775–781. [Google Scholar] [CrossRef]
- Kotra, L.P.; Haddad, J.; Mobashery, S. Aminoglycosides: Perspectives on Mechanisms of Action and Resistance and Strategies to Counter Resistance. Antimicrob. Agents Chemother. 2000, 44, 3249–3256. [Google Scholar] [CrossRef]
- Kemnic, T.R.; Coleman, M. Trimethoprim Sulfamethoxazole. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- García-León, G.; Ruiz De Alegría Puig, C.; García De La Fuente, C.; Martínez-Martínez, L.; Martínez, J.L.; Sánchez, M.B. High-Level Quinolone Resistance Is Associated with the Overexpression of smeVWX in Stenotrophomonas maltophilia Clinical Isolates. Clin. Microbiol. Infect. 2015, 21, 464–467. [Google Scholar] [CrossRef] [PubMed]
- García-León, G.; Salgado, F.; Oliveros, J.C.; Sánchez, M.B.; Martínez, J.L. Interplay between Intrinsic and Acquired Resistance to Quinolones in Stenotrophomonas maltophilia. Environ. Microbiol. 2014, 16, 1282–1296. [Google Scholar] [CrossRef] [PubMed]
- Mardle, C.E.; Shakespeare, T.J.; Butt, L.E.; Goddard, L.R.; Gowers, D.M.; Atkins, H.S.; Vincent, H.A.; Callaghan, A.J. A Structural and Biochemical Comparison of Ribonuclease E Homologues from Pathogenic Bacteria Highlights Species-Specific Properties. Sci. Rep. 2019, 9, 7952. [Google Scholar] [CrossRef] [PubMed]
- Brinkman, F.S.L.; Schoofs, G.; Hancock, R.E.W.; De Mot, R. Influence of a Putative ECF Sigma Factor on Expression of the Major Outer Membrane Protein, OprF, in Pseudomonas aeruginosa and Pseudomonas fluorescens. J. Bacteriol. 1999, 181, 4746–4754. [Google Scholar] [CrossRef] [PubMed]
- Park, S.H.; Kim, Y.J.; Lee, H.B.; Seok, Y.-J.; Lee, C.-R. Genetic Evidence for Distinct Functions of Peptidoglycan Endopeptidases in Escherichia coli. Front. Microbiol. 2020, 11, 565767. [Google Scholar] [CrossRef] [PubMed]
- The UniProt Consortium; Bateman, A.; Martin, M.-J.; Orchard, S.; Magrane, M.; Ahmad, S.; Alpi, E.; Bowler-Barnett, E.H.; Britto, R.; Bye-A-Jee, H.; et al. UniProt: The Universal Protein Knowledgebase in 2023. Nucleic Acids Res. 2023, 51, D523–D531. [Google Scholar] [CrossRef]
- Folcher, M.; Morris, R.P.; Dale, G.; Salah-Bey-Hocini, K.; Viollier, P.H.; Thompson, C.J. A Transcriptional Regulator of a Pristinamycin Resistance Gene in Streptomyces Coelicolor. J. Biol. Chem. 2001, 276, 1479–1485. [Google Scholar] [CrossRef] [PubMed]
- Koutsolioutsou, A.; Peña-Llopis, S.; Demple, B. Constitutive soxR Mutations Contribute to Multiple-Antibiotic Resistance in Clinical Escherichia coli Isolates. Antimicrob. Agents Chemother. 2005, 49, 2746–2752. [Google Scholar] [CrossRef]
- Burrowes, E.; Abbas, A.; O’Neill, A.; Adams, C.; O’Gara, F. Characterisation of the Regulatory RNA RsmB from Pseudomonas aeruginosa PAO1. Res. Microbiol. 2005, 156, 7–16. [Google Scholar] [CrossRef]
- Morimoto, Y.V.; Namba, K.; Minamino, T. GFP Fusion to the N-Terminus of MotB Affects the Proton Channel Activity of the Bacterial Flagellar Motor in Salmonella. Biomolecules 2020, 10, 1255. [Google Scholar] [CrossRef]
- Sorlozano, A.; Gutierrez, J.; Jimenez, A.; De Dios Luna, J.; Martínez, J.L. Contribution of a New Mutation in parE to Quinolone Resistance in Extended-Spectrum-β-Lactamase-Producing Escherichia coli Isolates. J. Clin. Microbiol. 2007, 45, 2740–2742. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Nathania, I.; Nainggolan, I.M.; Yasmon, A.; Nusatia, A.C.M.; Tjoa, E.; Gunardi, W.D.; Moehario, L.H. Hotspots Sequences of gyrA, gyrB, parC, and parE Genes Encoded for Fluoroquinolones Resistance from Local Salmonella Typhi Strains in Jakarta. BMC Microbiol. 2022, 22, 250. [Google Scholar] [CrossRef] [PubMed]
- Zhu, D.; Zheng, M.; Xu, J.; Wang, M.; Jia, R.; Chen, S.; Liu, M.; Zhao, X.; Yang, Q.; Wu, Y.; et al. Prevalence of Fluoroquinolone Resistance and Mutations in the gyrA, parC and parE Genes of Riemerella anatipestifer Isolated from Ducks in China. BMC Microbiol. 2019, 19, 271. [Google Scholar] [CrossRef] [PubMed]
- Ronneau, S.; Hallez, R. Make and Break the Alarmone: Regulation of (p)ppGpp Synthetase/Hydrolase Enzymes in Bacteria. FEMS Microbiol. Rev. 2019, 43, 389–400. [Google Scholar] [CrossRef] [PubMed]
- Alonso, A.; Martinez, J.L. Expression of Multidrug Efflux Pump SmeDEF by Clinical Isolates of Stenotrophomonas maltophilia. Antimicrob. Agents Chemother. 2001, 45, 1879–1881. [Google Scholar] [CrossRef]
- Buwembo, W.; Aery, S.; Rwenyonyi, C.M.; Swedberg, G.; Kironde, F. Point Mutations in the folP Gene Partly Explain Sulfonamide Resistance of Streptococcus mutans. Int. J. Microbiol. 2013, 2013, 367021. [Google Scholar] [CrossRef]
- Feirer, N.; Fuqua, C. Pterin Function in Bacteria. Pteridines 2017, 28, 23–36. [Google Scholar] [CrossRef]
- Aguena, M.; Ferreira, G.M.; Spira, B. Stability of the pstS Transcript of Escherichia coli. Arch. Microbiol. 2009, 191, 105–112. [Google Scholar] [CrossRef]
- Sajjan, U.S.; Xie, H.; Lefebre, M.D.; Valvano, M.A.; Forstner, J.F. Identification and Molecular Analysis of Cable Pilus Biosynthesis Genes in Burkholderia cepacia. Microbiology 2003, 149, 961–971. [Google Scholar] [CrossRef]
- Nejad, A.J.; Shahrokhi, N.; Nielsen, P.E. Targeting of the Essential acpP, ftsZ, and Rne Genes in Carbapenem-Resistant Acinetobacter baumannii by Antisense PNA Precision Antibacterials. Biomedicines 2021, 9, 429. [Google Scholar] [CrossRef]
- Georgellis, D.; Arvidson, S.; Von Gabain, A. Decay of ompA mRNA and Processing of 9S RNA Are Immediately Affected by Shifts in Growth Rate, but in Opposite Manners. J. Bacteriol. 1992, 174, 5382–5390. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cullen, P.A.; Haake, D.A.; Adler, B. Outer Membrane Proteins of Pathogenic Spirochetes. FEMS Microbiol. Rev. 2004, 28, 291–318. [Google Scholar] [CrossRef] [PubMed]
- Rozner, M.; Nukarinen, E.; Wolfinger, M.T.; Amman, F.; Weckwerth, W.; Bläsi, U.; Sonnleitner, E. Rewiring of Gene Expression in Pseudomonas aeruginosa During Diauxic Growth Reveals an Indirect Regulation of the MexGHI-OpmD Efflux Pump by Hfq. Front. Microbiol. 2022, 13, 919539. [Google Scholar] [CrossRef] [PubMed]
- Chou, J.H.; Greenberg, J.T.; Demple, B. Posttranscriptional Repression of Escherichia coli OmpF Protein in Response to Redox Stress: Positive Control of the micF Antisense RNA by the soxRS Locus. J. Bacteriol. 1993, 175, 1026–1031. [Google Scholar] [CrossRef] [PubMed]
- Miller, P.F.; Sulavik, M.C. Overlaps and Parallels in the Regulation of Intrinsic Multiple-Antibiotic Resistance in Escherichia coli. Mol. Microbiol. 1996, 21, 441–448. [Google Scholar] [CrossRef] [PubMed]
- White, D.G.; Goldman, J.D.; Demple, B.; Levy, S.B. Role of the acrAB Locus in Organic Solvent Tolerance Mediated by Expression of marA, soxS, or robA in Escherichia coli. J. Bacteriol. 1997, 179, 6122–6126. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Wang, Q.; Wang, R.; Zhang, Y.; Wang, X.; Wang, H. Global Regulator SoxR Is a Negative Regulator of Efflux Pump Gene Expression and Affects Antibiotic Resistance and Fitness in Acinetobacter baumannii. Medicine 2017, 96, e7188. [Google Scholar] [CrossRef] [PubMed]
- Bialek-Davenet, S.; Marcon, E.; Leflon-Guibout, V.; Lavigne, J.-P.; Bert, F.; Moreau, R.; Nicolas-Chanoine, M.-H. In Vitro Selection of ramR and soxR Mutants Overexpressing Efflux Systems by Fluoroquinolones as Well as Cefoxitin in Klebsiella Pneumoniae. Antimicrob. Agents Chemother. 2011, 55, 2795–2802. [Google Scholar] [CrossRef] [PubMed]
- Alonso, A.; Martínez, J.L. Cloning and Characterization of SmeDEF, a Novel Multidrug Efflux Pump from Stenotrophomonas maltophilia. Antimicrob. Agents Chemother. 2000, 44, 3079–3086. [Google Scholar] [CrossRef]
- Calvopiña, K.; Dulyayangkul, P.; Avison, M.B. Mutations in Ribosomal Protein RplA or Treatment with Ribosomal Acting Antibiotics Activates Production of Aminoglycoside Efflux Pump SmeYZ in Stenotrophomonas maltophilia. Antimicrob. Agents Chemother. 2020, 64, e01524-19. [Google Scholar] [CrossRef]
- Potrykus, K.; Cashel, M. (P)ppGpp: Still Magical? Annu. Rev. Microbiol. 2008, 62, 35–51. [Google Scholar] [CrossRef]
- Sy, J. Reversibility of the Pyrophosphoryl Transfer from ATP to GTP by Escherichia coli Stringent Factor. Proc. Natl. Acad. Sci. USA 1974, 71, 3470–3473. [Google Scholar] [CrossRef] [PubMed]
- Fitzsimmons, L.F.; Liu, L.; Kant, S.; Kim, J.-S.; Till, J.K.; Jones-Carson, J.; Porwollik, S.; McClelland, M.; Vazquez-Torres, A. SpoT Induces Intracellular Salmonella Virulence Programs in the Phagosome. mBio 2020, 11, e03397-19. [Google Scholar] [CrossRef] [PubMed]
- Das, B.; Bhadra, R.K. (P)ppGpp Metabolism and Antimicrobial Resistance in Bacterial Pathogens. Front. Microbiol. 2020, 11, 563944. [Google Scholar] [CrossRef]
- Clemmer, K.M.; Sturgill, G.M.; Veenstra, A.; Rather, P.N. Functional Characterization of Escherichia coli GlpG and Additional Rhomboid Proteins Using an aarA Mutant of Providencia Stuartii. J. Bacteriol. 2006, 188, 3415–3419. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Linares, J.F.; López, J.A.; Camafeita, E.; Albar, J.P.; Rojo, F.; Martínez, J.L. Overexpression of the Multidrug Efflux Pumps MexCD-OprJ and MexEF-OprN Is Associated with a Reduction of Type III Secretion in Pseudomonas aeruginosa. J. Bacteriol. 2005, 187, 1384–1391. [Google Scholar] [CrossRef] [PubMed]
- Mulcahy, H.; O’Callaghan, J.; O’Grady, E.P.; Adams, C.; O’Gara, F. The Posttranscriptional Regulator RsmA Plays a Role in the Interaction between Pseudomonas aeruginosa and Human Airway Epithelial Cells by Positively Regulating the Type III Secretion System. Infect. Immun. 2006, 74, 3012–3015. [Google Scholar] [CrossRef]
- Blanco, P.; Corona, F.; Martínez, J.L. Involvement of the RND Efflux Pump Transporter SmeH in the Acquisition of Resistance to Ceftazidime in Stenotrophomonas maltophilia. Sci. Rep. 2019, 9, 4917. [Google Scholar] [CrossRef]
- Lamarche, M.G.; Dozois, C.M.; Daigle, F.; Caza, M.; Curtiss, R.; Dubreuil, J.D.; Harel, J. Inactivation of the Pst System Reduces the Virulence of an Avian Pathogenic Escherichia coli O78 Strain. Infect. Immun. 2005, 73, 4138–4145. [Google Scholar] [CrossRef]
- Gil-Marqués, M.L.; Labrador Herrera, G.; Miró Canturri, A.; Pachón, J.; Smani, Y.; Pachón-Ibáñez, M.E. Role of PstS in the Pathogenesis of Acinetobacter baumannii under Microaerobiosis and Normoxia. J. Infect. Dis. 2020, 222, 1204–1212. [Google Scholar] [CrossRef]
- Kheirandish, F.; Bandehpour, M.; Davoudi, N.; Mosaffa, N.; Dawood, S.; Kazemi, B.; Haghighi, A.; Khamesipour, A.; Masjedi, H.; Mohebali, M.; et al. Gene Regulation of Pteridine Reductase 1 in Leishmania promastigotes and Amastigotes Using a Full-Length Antisense Construct. Iran. J. Parasitol. 2013, 8, 190–196. [Google Scholar] [PubMed]
- Hernando-Amado, S.; Laborda, P.; Valverde, J.R.; Martínez, J.L. Mutational Background Influences P. aeruginosa Ciprofloxacin Resistance Evolution but Preserves Collateral Sensitivity Robustness. Proc. Natl. Acad. Sci. USA 2022, 119, e2109370119. [Google Scholar] [CrossRef] [PubMed]
- Lira, F.; Hernández, A.; Belda, E.; Sánchez, M.B.; Moya, A.; Silva, F.J.; Martínez, J.L. Whole-Genome Sequence of Stenotrophomonas maltophilia D457, a Clinical Isolate and a Model Strain. J. Bacteriol. 2012, 194, 3563–3564. [Google Scholar] [CrossRef] [PubMed]
- European Committee for Antimicrobial Susceptibility Testing (EUCAST) of the European Society of Clinical Microbiology and Infectious Diseases (ESCMID). Terminology Relating to Methods for the Determination of Susceptibility of Bacteria to Antimicrobial Agents. Clin. Microbiol. Infect. 2000, 6, 503–508. [Google Scholar] [CrossRef] [PubMed]
- Ewels, P.A.; Peltzer, A.; Fillinger, S.; Patel, H.; Alneberg, J.; Wilm, A.; Garcia, M.U.; Di Tommaso, P.; Nahnsen, S. The Nf-Core Framework for Community-Curated Bioinformatics Pipelines. Nat. Biotechnol. 2020, 38, 276–278. [Google Scholar] [CrossRef]
- Danecek, P.; Bonfield, J.K.; Liddle, J.; Marshall, J.; Ohan, V.; Pollard, M.O.; Whitwham, A.; Keane, T.; McCarthy, S.A.; Davies, R.M.; et al. Twelve Years of SAMtools and BCFtools. GigaScience 2021, 10, giab008. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).