Effectiveness of a Combination of Nasturtium Herb and Horseradish Root (Angocin® Anti-Infekt N) Compared to Antibiotics in Managing Acute and Recurrent Urinary Tract Infections: A Retrospective Real-world Cohort Study
Abstract
1. Introduction
2. Methods
2.1. Data Source
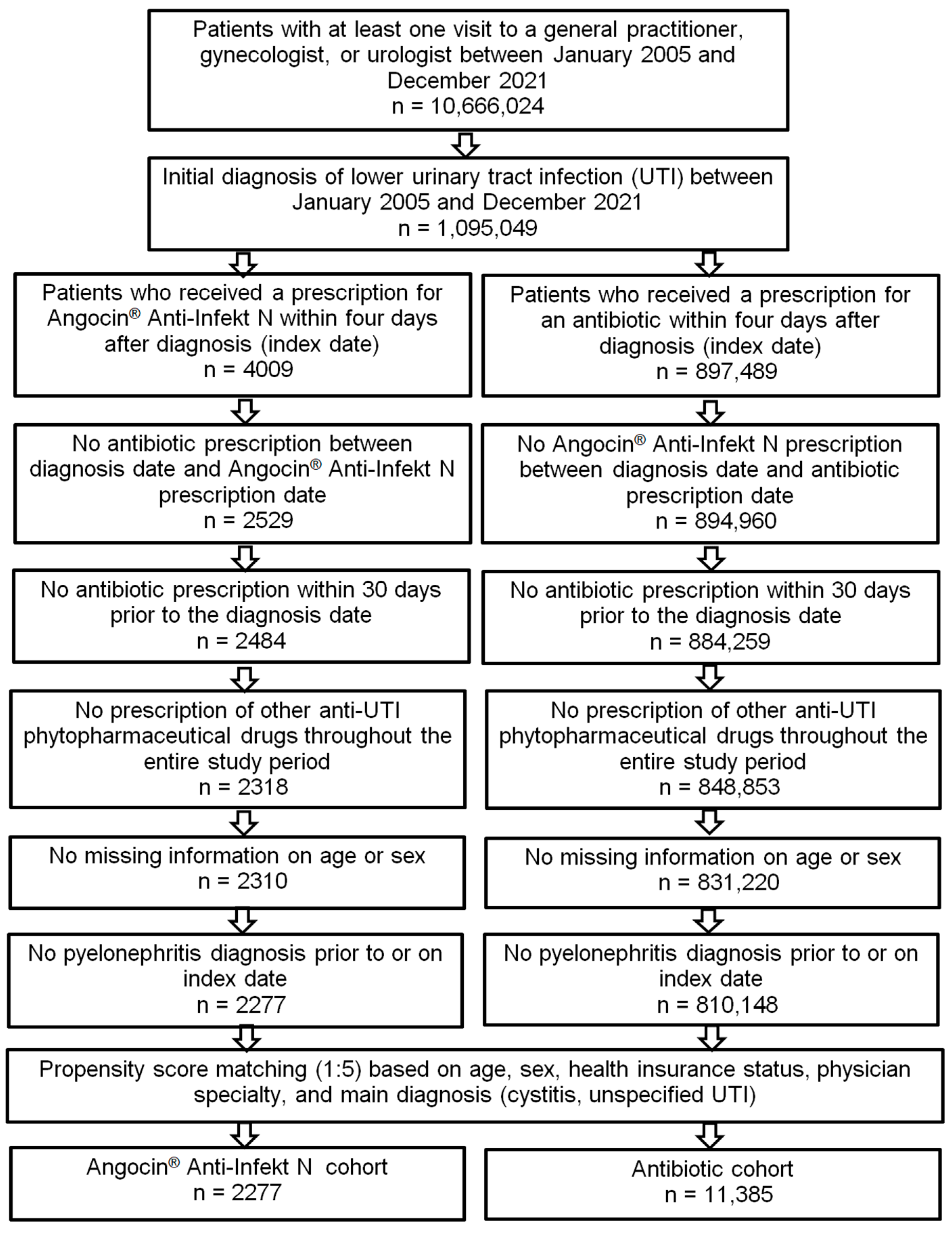
2.2. Study Population
- Acute cystitis (ICD-10: N30.0).
- Other cystitis (ICD-10: N30.8).
- Cystitis, unspecified (ICD-10: N30.9).
- Urinary tract infection, site not specified (ICD-10: N39.0).
2.3. Descriptive and Statistical Analyses
3. Results
3.1. Baseline Characteristics of Study Patients
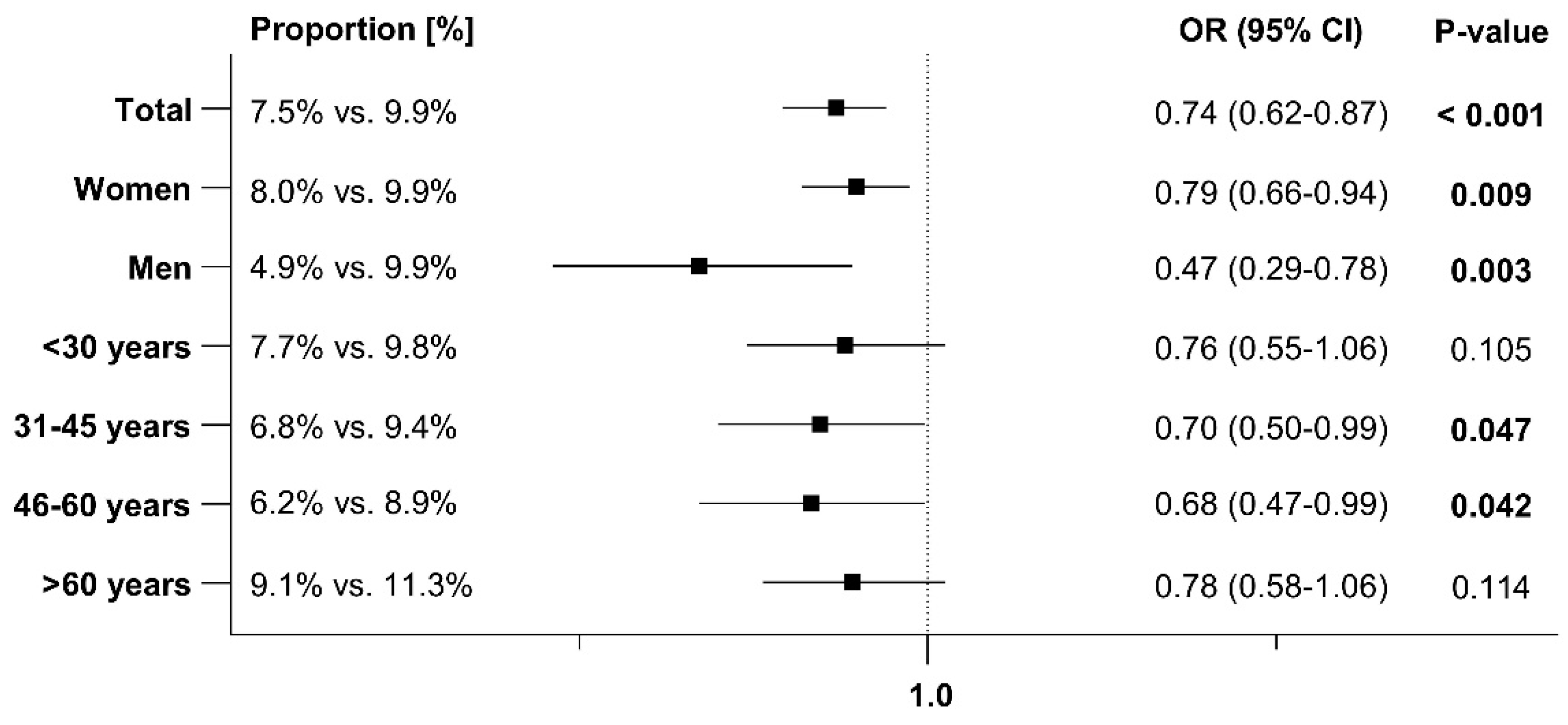
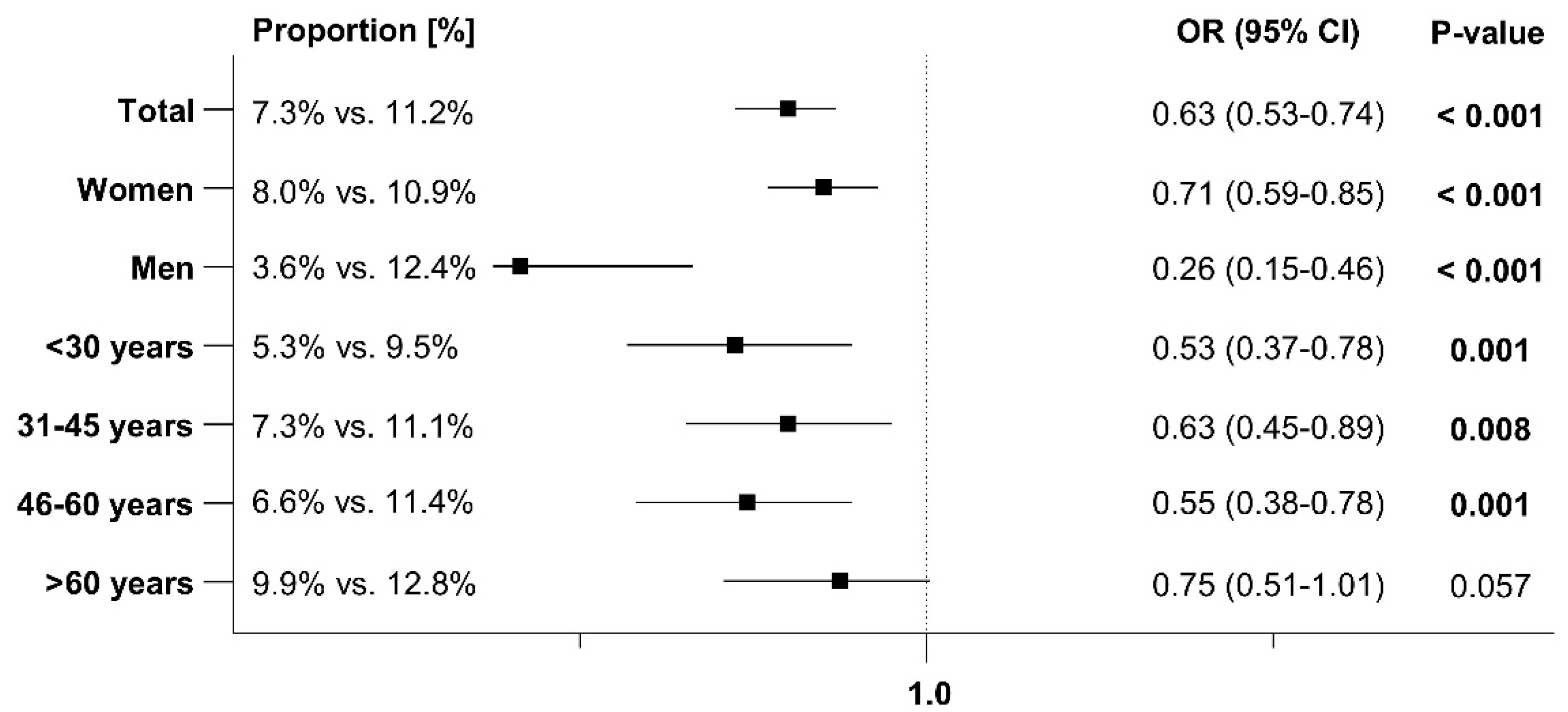
3.2. Early and Sporadic UTI
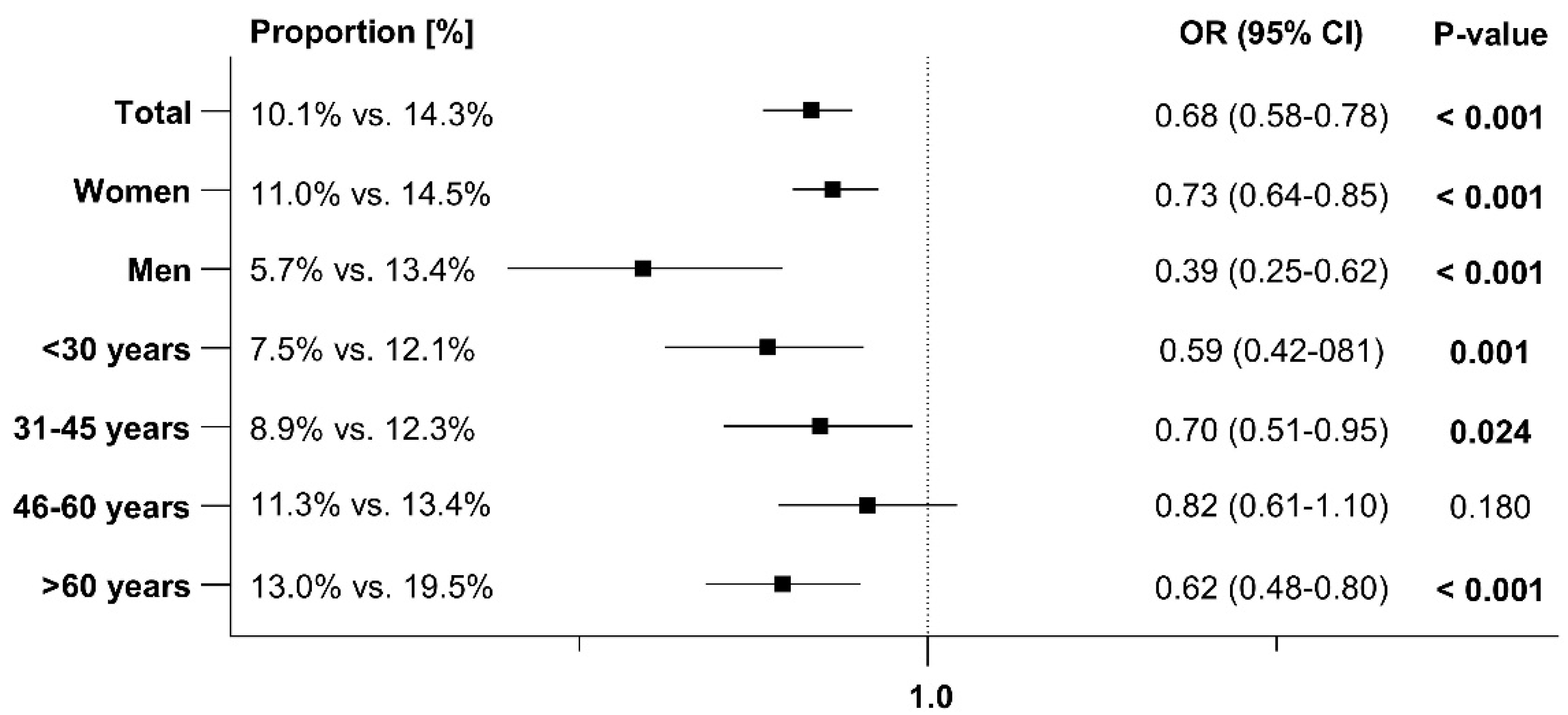
3.3. Recurrent Urinary Tract Infections (rUTI)
3.4. Antibiotic Prescriptions After the Index Date
3.5. Sick Leave After the Index Date
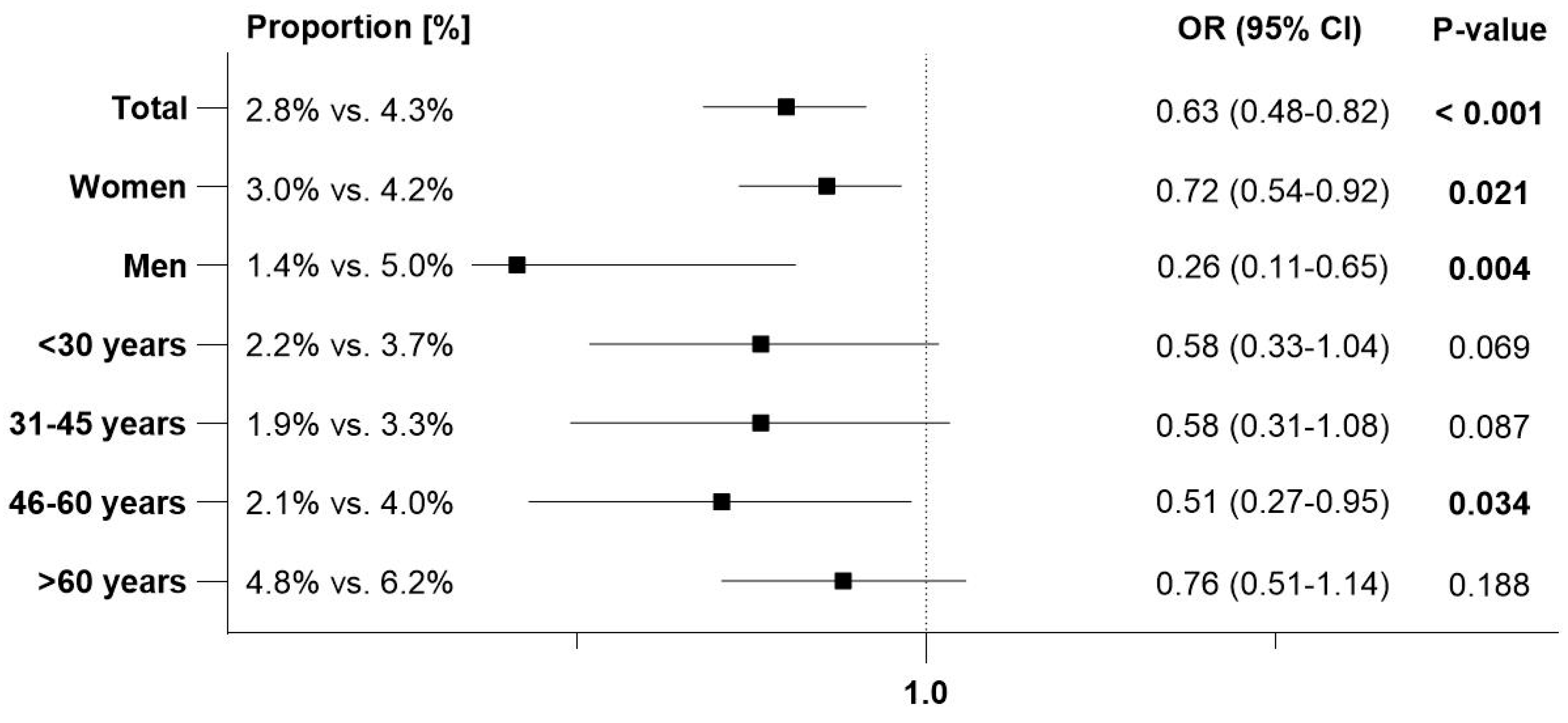
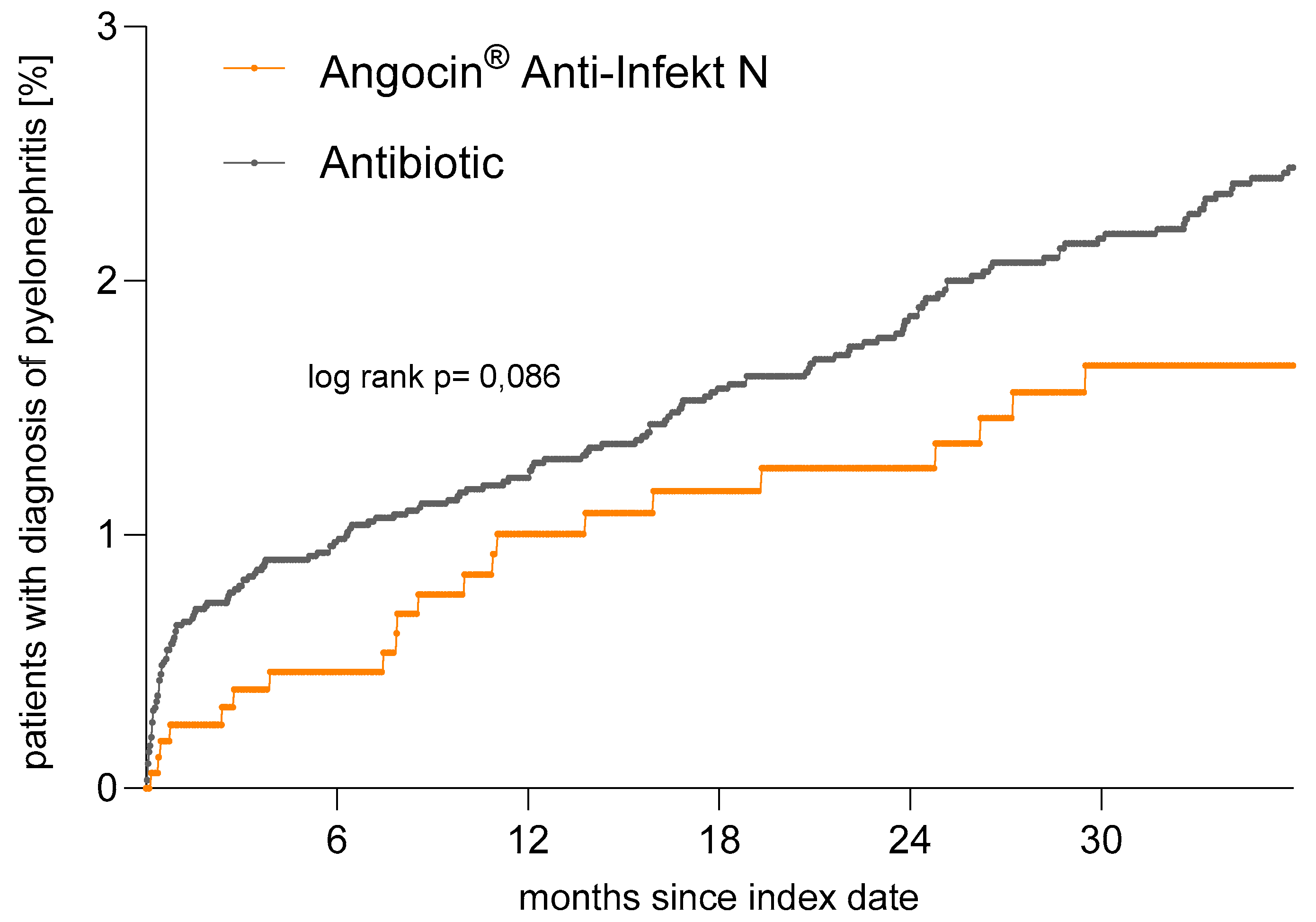
3.6. Incidence of Pyelonephritis
4. Strengths and Limitations
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Statement of Ethics
References
- Flores-Mireles, A.L.; Walker, J.N.; Caparon, M.; Hultgren, S.J. Urinary tract infections: Epidemiology, mechanisms of infection and treatment options. Nat. Rev. Microbiol. 2015, 13, 269–284. [Google Scholar] [CrossRef] [PubMed]
- Kranz, J.; Schmidt, S.; Lebert, C.; Schneidewind, L.; Mandraka, F.; Kunze, M.; Helbig, S.; Vahlensieck, W.; Naber, K.; Schmiemann, G.; et al. The 2017 Update of the German Clinical Guideline on Epidemiology, Diagnostics, Therapy, Prevention, and Management of Uncomplicated Urinary Tract Infections in Adult Patients. Part II: Therapy and Prevention. Urol. Int. 2018, 100, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Naber, K.G.; Tiran-Saucedo, J.; Wagenlehner, F.M.E.; RECAP Group. Psychosocial burden of recurrent uncomplicated urinary tract infections. GMS Infect. Dis. 2022, 10, Doc01. [Google Scholar] [CrossRef]
- Kranz, J.; Bartoletti, R.; Bruyere, F.; Cai, T.; Geerlings, S.; Koves, B.; Schubert, S.; Pilatz, A.; Veeratterapillay, R.; Wagenlehner, F.M.E.; et al. European Association of Urology Guidelines on Urological Infections: Summary of the 2024 Guidelines. Eur. Urol. 2024, 86, 27–41. [Google Scholar] [CrossRef]
- Deutsche Gesellschaft für Urologie. S3 Leitlinie: Epidemiologie, Diagnostik, Therapie, Prävention und Management Unkomplizierter, Bakterieller, Ambulant Erworbener Harnwegsinfektionen bei Erwachsenen—Aktualisierung 2024. Langversion, 3.0, AWMF Registernummer: 043/044. 3 Guideline: Epidemiology, Diagnosis, Therapy, Prevention and Management of Uncomplicated Bacterial Community-Acquired Urinary Tract Infections in Adults—Update 2024. Long Version, 3.0, AWMF Register Number: 043/044; Deutsche Gesellschaft für Urologie e.V., Ed.; Deutsche Gesellschaft für Urologie: Düsseldorf, Germany, 2024. [Google Scholar]
- Kaussner, Y.; Rover, C.; Heinz, J.; Hummers, E.; Debray, T.P.A.; Hay, A.D.; Heytens, S.; Vik, I.; Little, P.; Moore, M.; et al. Reducing antibiotic use in uncomplicated urinary tract infections in adult women: A systematic review and individual participant data meta-analysis. Clin. Microbiol. Infect. 2022, 28, 1558–1566. [Google Scholar] [CrossRef]
- Rodriguez-Manas, L. Urinary tract infections in the elderly: A review of disease characteristics and current treatment options. Drugs Context 2020, 9, 1–8. [Google Scholar] [CrossRef]
- Ehrenberg, C.; Kalder, M.; Kostev, K. Prevalence of and factors associated with the prescription of phytopharmaceuticals in outpatients with urinary tract infections. Int. J. Clin. Pharmacol. Ther. 2021, 59, 654–661. [Google Scholar] [CrossRef] [PubMed]
- Vahlensieck, W., Jr.; Westenfelder, M. Nitrofurantoin versus trimethoprim for low-dose long-term prophylaxis in patients with recurrent urinary tract infections. A prospective randomized study. Int. Urol. Nephrol. 1992, 24, 3–10. [Google Scholar] [CrossRef]
- Stewardson, A.J.; Gaia, N.; Francois, P.; Malhotra-Kumar, S.; Delemont, C.; Martinez de Tejada, B.; Schrenzel, J.; Harbarth, S.; Lazarevic, V.; Saturn, W.P.; et al. Collateral damage from oral ciprofloxacin versus nitrofurantoin in outpatients with urinary tract infections: A culture-free analysis of gut microbiota. Clin. Microbiol. Infect. 2015, 21, 344.e1–344.e11. [Google Scholar] [CrossRef]
- Cizman, M.; Plankar Srovin, T. Antibiotic consumption and resistance of gram-negative pathogens (collateral damage). GMS Infect. Dis. 2018, 6, Doc05. [Google Scholar] [CrossRef]
- Klingeberg, A.; Willrich, N.; Schneider, M.; Schmiemann, G.; Gagyor, I.; Richter, D.; Noll, I.; Eckmanns, T. The Percentage of Antibiotic Resistance in Uncomplicated Community-Acquired Urinary Tract Infections. Dtsch. Arztebl. Int. 2024, 121, 175–181. [Google Scholar] [CrossRef]
- Kronenberg, A.; Koenig, S.; Droz, S.; Muhlemann, K. Active surveillance of antibiotic resistance prevalence in urinary tract and skin infections in the outpatient setting. Clin. Microbiol. Infect. 2011, 17, 1845–1851. [Google Scholar] [CrossRef] [PubMed]
- Schmiemann, G.; Hoffmann, F.; Hamprecht, A.; Jobski, K. Patterns and trends of antibacterial treatment in patients with urinary tract infections, 2015–2019: An analysis of health insurance data. BMC Prim. Care 2022, 23, 204. [Google Scholar] [CrossRef] [PubMed]
- Conrad, A. In-vitro-Untersuchungen zur antibakteriellen Wirksamkeit einer Kombination aus Kapuzinerkressekraut (Tropaeoli majoris herba) und Meerrettichwurzel (Armoraciae rusticanae radix). Drug Res. 2006, 56, 842–849. [Google Scholar]
- Conrad, A.; Biehler, D.; Nobis, T.; Richter, H.; Engels, I.; Biehler, K.; Frank, U. Broad spectrum antibacterial activity of a mixture of isothiocyanates from nasturtium (Tropaeoli majoris herba) and horseradish (Armoraciae rusticanae radix). Drug Res. 2013, 63, 65–68. [Google Scholar] [CrossRef]
- Herz, C.; Tran, H.T.; Marton, M.R.; Maul, R.; Baldermann, S.; Schreiner, M.; Lamy, E. Evaluation of an Aqueous Extract from Horseradish Root (Armoracia rusticana Radix) against Lipopolysaccharide-Induced Cellular Inflammation Reaction. Evid. Based Complement. Alternat Med. 2017, 2017, 1950692. [Google Scholar] [CrossRef]
- Tran, H.T.; Marton, M.R.; Herz, C.; Maul, R.; Baldermann, S.; Schreiner, M.; Lamy, E. Nasturtium (Indian cress, Tropaeolum majus nanum) dually blocks the COX and LOX pathway in primary human immune cells. Phytomedicine 2016, 23, 611–620. [Google Scholar] [CrossRef]
- Marcon, J.; Schubert, S.; Stief, C.G.; Magistro, G. In vitro efficacy of phytotherapeutics suggested for prevention and therapy of urinary tract infections. Infection 2019, 47, 937–944. [Google Scholar] [CrossRef]
- Mutters, N.T.; Mampel, A.; Kropidlowski, R.; Biehler, K.; Gunther, F.; Balu, I.; Malek, V.; Frank, U. Treating urinary tract infections due to MDR E. coli with Isothiocyanates—A phytotherapeutic alternative to antibiotics? Fitoterapia 2018, 129, 237–240. [Google Scholar] [CrossRef]
- Kaiser, S.J.; Mutters, N.T.; Blessing, B.; Gunther, F. Natural isothiocyanates express antimicrobial activity against developing and mature biofilms of Pseudomonas aeruginosa. Fitoterapia 2017, 119, 57–63. [Google Scholar] [CrossRef]
- Goos, K.-H.; Albrecht, U.; Schneider, B. Wirksamkeit und Verträglichkeit eines pflanzlichen Arzneimittels mit Kapuzinerkressenkraut und Meerrettich bei akuter Sinusitis, akuter Bronchitis und akuter Blasenentzündung im Vergleich zu anderen Therapien unter den Bedingungen der täglichen Praxis. Arzneimittelforschung 2006, 56, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Albrecht, U.; Goos, K.-H.; Schneider, B. A randomised, double-blind, placebo-controlled trial of a herbal medicinal product containing Tropaeoli majoris herba (Nasturtium) and Armoraciae rusticanae radix (Horseradish) for the prophylactic treatment of patients with chronically recurrent lower urinary tract infections. Curr. Med. Res. Opin. 2007, 23, 2415–2422. [Google Scholar] [CrossRef] [PubMed]
- Rathmann, W.; Bongaerts, B.; Carius, H.J.; Kruppert, S.; Kostev, K. Basic characteristics and representativeness of the German Disease Analyzer database. Int. J. Clin. Pharmacol. Ther. 2018, 56, 459–466. [Google Scholar] [CrossRef]
- Holler, M.; Steindl, H.; Abramov-Sommariva, D.; Wagenlehner, F.; Naber, K.G.; Kostev, K. Treatment of Urinary Tract Infections with Canephron ((R)) in Germany: A Retrospective Database Analysis. Antibiotics 2021, 10, 685. [Google Scholar] [CrossRef] [PubMed]
- Heidemann, J.; Kalder, M.; Kostev, K. Association between contraceptive use and risk of lower urinary tract infection (LUTI): A case-control study. Int. J. Clin. Pharmacol. Ther. 2022, 60, 167–175. [Google Scholar] [CrossRef]
- Rassen, J.A.; Shelat, A.A.; Myers, J.; Glynn, R.J.; Rothman, K.J.; Schneeweiss, S. One-to-many propensity score matching in cohort studies. Pharmacoepidemiol. Drug Saf. 2012, 21 (Suppl. S2), 69–80. [Google Scholar] [CrossRef]
- Stuart, E.A.; Lee, B.K.; Leacy, F.P. Prognostic score-based balance measures can be a useful diagnostic for propensity score methods in comparative effectiveness research. J. Clin. Epidemiol. 2013, 66, S84–S90. [Google Scholar] [CrossRef]
- Bertsche, T.; Alexa, J.M.; Eickhoff, C.; Schulz, M. Self-care and self-medication as central components of healthcare in Germany—On the way to evidence-based pharmacy. Explor. Res. Clin. Soc. Pharm. 2023, 9, 100257. [Google Scholar] [CrossRef]
- Goos, K.-H.; Albrecht, U.; Schneider, B. Aktuelle Untersuchungen zur Wirksamkeit und Verträglichkeit eines pflanzlichen Arzneimittels mit Kapuzinerkressenkraut und Meerrettich bei akuter Sinusitis, akuter Bronchitis und akuter Blasenentzündung bei Kindern im Vergleich zu anderen Antibiotika. Arzneimittelforschung 2007, 57, 238–246. [Google Scholar] [CrossRef]
- Marton, M.R.; Krumbein, A.; Platz, S.; Schreiner, M.; Rohn, S.; Rehmers, A.; Lavric, V.; Mersch-Sundermann, V.; Lamy, E. Determination of bioactive, free isothiocyanates from a glucosinolate-containing phytotherapeutic agent: A pilot study with in vitro models and human intervention. Fitoterapia 2013, 85, 25–34. [Google Scholar] [CrossRef]
- Deltourbe, L.; Lacerda Mariano, L.; Hreha, T.N.; Hunstad, D.A.; Ingersoll, M.A. The impact of biological sex on diseases of the urinary tract. Mucosal Immunol. 2022, 15, 857–866. [Google Scholar] [CrossRef] [PubMed]
- Sabih, A.; Leslie, S.W. Complicated Urinary Tract Infections. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Kolman, K.B. Cystitis and Pyelonephritis: Diagnosis, Treatment, and Prevention. Prim. Care 2019, 46, 191–202. [Google Scholar] [CrossRef] [PubMed]
- Herness, J.; Buttolph, A.; Hammer, N.C. Acute Pyelonephritis in Adults: Rapid Evidence Review. Am. Fam. Physician 2020, 102, 173–180. [Google Scholar] [PubMed]

| Prior to Matching | After Matching | |||||
|---|---|---|---|---|---|---|
| Variable | Patients with Angocin® Prescription | Patients with Antibiotic Prescription | p-Value | Patients with Angocin® Prescription | Patients with Antibiotic Prescription | p-Value |
| n | 2277 | 810,148 | 2277 | 11,385 | ||
| Age (mean, SD) | 45.7 (19.8) | 49.8 (21.6) | <0.001 | 45.7 (19.8) | 45.7 (19.7) | 0.985 |
| <30 years (n, %) | 587 (25.8) | 187,446 (23.1) | <0.001 | 587 (25.8) | 2995 (26.3) | 0.946 |
| 31–45 years (n, %) | 572 (25.1) | 166,550 (20.6) | 572 (25.1) | 2827 (24.8) | ||
| 46–60 years (n, %) | 533 (23.4) | 171,438 (21.2) | 533 (23.4) | 2679 (23.5) | ||
| >60 years (n, %) | 585 (25.7) | 284,714 (35.1) | 585 (25.7) | 2884 (25.3) | ||
| Sex: female (%) | 1911 (83.9) | 647,128 (79.9) | <0.001 | 1911 (83.9) | 9555 (83.9) | 1.000 |
| Private health insurance coverage (n, %) | 450 (19.8) | 69,625 (8.6) | <0.001 | 450 (19.8) | 2250 (19.8) | 1.000 |
| Cystitis (n, %) | 715 (31.4) | 263,374 (32.5) | <0.001 | 715 (31.4) | 3575 (31.4) | 1.000 |
| Therapy by general practitioner (n, %) | 947 (41.6) | 540,168 (66.7) | <0.001 | 947 (41.6) | 4735 (41.6) | 1.000 |
| Therapy by gynecologist (n, %) | 227 (10.0) | 123,139 (15.2) | 227 (10.0) | 1135 (10.0) | ||
| Therapy by urologist (n, %) | 1103 (48.4) | 146,841 (18.1) | 1103 (48.4) | 5515 (48.4) | ||
| Patient Group | Events per 1000 Person-Years in Patients with Angocin® Prescription (%) | Events per 1000 Person-Years in Patients with Antibiotic Prescription (%) | Hazard Ratio (95% CI) | p-Value |
|---|---|---|---|---|
| Total | 6.2 | 9.2 | 0.67 (0.43–1.06) | 0.073 |
| Women | 7.2 | 10.2 | 0.70 (0.44–1.11) | 0.125 |
| Men | 1.7 | 4.1 | 0.42 (0.06–3.21) | 0.403 |
| Age groups | ||||
| <30 years | 7.4 | 17.6 | 0.42 (0.17–1.04) | 0.060 |
| 31–45 years | 7.8 | 9.8 | 0.76 (0.33–1.79) | 0.531 |
| 46–60 years | 5.4 | 6.6 | 0.82 (0.32–2.09) | 0.670 |
| >60 years | 5.1 | 5.0 | 1.02 (0.39–2.66) | 0.966 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kassner, N.; Wonnemann, M.; Ziegler, Y.; Vahlensieck, W.; Kranz, J.; Kostev, K. Effectiveness of a Combination of Nasturtium Herb and Horseradish Root (Angocin® Anti-Infekt N) Compared to Antibiotics in Managing Acute and Recurrent Urinary Tract Infections: A Retrospective Real-world Cohort Study. Antibiotics 2024, 13, 1036. https://doi.org/10.3390/antibiotics13111036
Kassner N, Wonnemann M, Ziegler Y, Vahlensieck W, Kranz J, Kostev K. Effectiveness of a Combination of Nasturtium Herb and Horseradish Root (Angocin® Anti-Infekt N) Compared to Antibiotics in Managing Acute and Recurrent Urinary Tract Infections: A Retrospective Real-world Cohort Study. Antibiotics. 2024; 13(11):1036. https://doi.org/10.3390/antibiotics13111036
Chicago/Turabian StyleKassner, Nina, Meinolf Wonnemann, Yvonne Ziegler, Winfried Vahlensieck, Jennifer Kranz, and Karel Kostev. 2024. "Effectiveness of a Combination of Nasturtium Herb and Horseradish Root (Angocin® Anti-Infekt N) Compared to Antibiotics in Managing Acute and Recurrent Urinary Tract Infections: A Retrospective Real-world Cohort Study" Antibiotics 13, no. 11: 1036. https://doi.org/10.3390/antibiotics13111036
APA StyleKassner, N., Wonnemann, M., Ziegler, Y., Vahlensieck, W., Kranz, J., & Kostev, K. (2024). Effectiveness of a Combination of Nasturtium Herb and Horseradish Root (Angocin® Anti-Infekt N) Compared to Antibiotics in Managing Acute and Recurrent Urinary Tract Infections: A Retrospective Real-world Cohort Study. Antibiotics, 13(11), 1036. https://doi.org/10.3390/antibiotics13111036







